ABSTRACT
Acquired Brain Injury (ABI) often results in significant challenges, yet it may also facilitate Post-Traumatic Growth (PTG). This review explores a critical question: “What are the main factors contributing to PTG following ABI, and what potential barriers to its development are perceived by ABI survivors?” Here we aim to systematically uncover these contributors and barriers to PTG through a meta-synthesis, involving a comprehensive review of previously published qualitative research on this topic. A literature search was conducted across PsycINFO, CINAHL, and MEDLINE up to December 2022 to identify studies for inclusion. From an initial pool of 1,946 records, eleven articles were selected for inclusion. Reflexive thematic analysis yielded three analytical themes including “Journey to Self-Rediscovery”, “Strength in Connection” and “Overcoming Obstacles”. Our findings also revealed facilitators and barriers across multiple levels of scale including personal (e.g., acceptance versus resignation), interpersonal (e.g., positive social ties versus difficulties making social connections), and systemic (e.g., new meaning and purpose versus financial constraints) scales. Our research extends existing knowledge in ABI rehabilitation, providing a more nuanced understanding of the dynamics influencing PTG with implications for clinicians seeking to promote wellbeing following brain injury.
Acquired Brain Injury (ABI) is defined as damage to the brain occurring after birth, either due to external forces causing head trauma (Traumatic Brain Injury, TBI) or internal and external causes like stroke, hypoxia, brain tumours, infections, and toxic exposure (non-TBI) (Cattelani et al., Citation2010; Grace et al., Citation2015; Seeto et al., Citation2017). ABI represents a significant public health issue globally (Kamalakannan et al., Citation2015). TBI and stroke rank among the top ten causes of death and disability worldwide, with an estimated sixty-nine million individuals sustaining TBI annually (Dewan et al., Citation2018) and a lifetime stroke risk of 1 in 4 people (Feigin et al., Citation2022). The healthcare costs for TBI and stroke are substantial (Humphreys et al., Citation2013); in Europe and the UK alone, the total cost of stroke was around €60 billion in 2017 (Luengo-Fernandez et al., Citation2020). In the UK, each year, over 1 million people visit emergency departments for head injury, which is the leading cause of death and disability in people under 40 (National Institute for Health and Care Excellence, Citation2023). The effects of ABI account for 10% of the annual NHS budget (Barber et al., Citation2018), and although many ABI survivors are able to recover, over 40% of survivors face long-term disability, and require acute and post-acute neurorehabilitation (Corrigan et al., Citation2010). Survivors often struggle with cognitive impairments, physical difficulties, and lifestyle challenges (Karagiorgou et al., Citation2018; Rabinowitz & Levin, Citation2014; Reinkensmeyer et al., Citation2014). The injury itself, coupled with these resulting challenges, can lead to psychological distress, anxiety, depression, and suicide risk, impacting on a person’s quality of life and wellbeing (Graff et al., Citation2018; Karagiorgou et al., Citation2018; Nochi, Citation2000; Osborn et al., Citation2014; Roundhill et al., Citation2007). Additionally, ABI can disrupt independent functioning, autonomy, social relationships, and community integration (Baker et al., Citation2018; de Freitas Cardoso et al., Citation2019; Kuenemund et al., Citation2016).
Historically, neurorehabilitation has focused on managing the negative aspects of ABI (Grace et al., Citation2015; Graff et al., Citation2018). However, since ABI is not a condition that can be “fixed” and it is not always possible for a person to return to premorbid levels of functioning (Fisher et al., Citation2020), there is a need for broader approaches to rehabilitation that focus on supporting people to live fulfilling lives within the limitations imposed by the condition. These include opportunities for psychological growth to support recovery and enhance psychological wellbeing (Lyon et al., Citation2021). For example, our previous research has shown that holistic interventions like surf therapy and group-based activities focused on personal growth can improve psychological wellbeing (Gibbs et al., Citation2022b; Wilkie et al., Citation2021). Positive psychology interventions have also been reported to increase happiness and reduce anxiety symptoms (Andrewes et al., Citation2014;; Tulip et al., Citation2020). Our research and service evaluations, developed around the GENIAL model (Fisher et al., Citation2024; Kemp & Fisher, Citation2022; Mead et al., Citation2019, Citation2021), focus on building wellbeing for people with chronic conditions like ABI. This model integrates physical and psychological approaches and embeds rehabilitation with the persons social context whilst attempting to reduce health inequalities and socio-structural barriers to wellbeing. Our work highlights the importance of positive psychological experiences, health behaviours, social relationships, and community reintegration in promoting health and wellbeing. These elements are crucial in facilitating Post-Traumatic Growth (PTG) in ABI survivors, as evidenced by prior research (Collicutt McGrath & Linley, Citation2006; Lyon et al., Citation2021; Powell et al., Citation2012; Silva et al., Citation2011). PTG is defined as subjective perceptions of positive psychological growth following a traumatic event that exceed levels of pre-trauma functioning (Lyon et al., Citation2021; Tedeschi & Calhoun, Citation2004). It differs from resilience, optimism, or coping, as it indicates a higher state of psychological development.
Our study moves beyond the work of Bannon et al. (Citation2022) – which focused on resilience post-TBI – by focusing on PTG to better understand how survivors may achieve higher levels of functioning than before the injury. Literature suggests that individuals experiencing PTG undergo subjective changes in self-perception, life and relationships following trauma (Sekely & Zakzanis, Citation2019; Tedeschi & Calhoun, Citation2004). PTG typically arises from struggles and re-definition of identity, involving integrating the traumatic event into a person’s life narrative (Kuenemund et al., Citation2016; Ownsworth & Fleming, Citation2011; Sekely & Zakzanis, Citation2019). Cognitive strategies associated with PTG represent a progression beyond pre-injury functioning (Rogan et al., Citation2013; Tedeschi & Calhoun, Citation2004). Reported associations between aspects of PTG including new possibilities and personal strength and return to work in ABI populations are also promising (Sekely & Zakzanis, Citation2019). Critically, a significant percentage of ABI survivors report PTG are those with more severe injuries or longer recovery periods (Goldberg et al., Citation2019; Gould & Ponsford, Citation2014; Sawyer et al., Citation2010; Sekely & Zakzanis, Citation2019). PTG is linked to lower distress levels, increased coping strategies, and positive treatment beliefs (Karagiorgou et al., Citation2018; Rogan et al., Citation2013). Grace et al. (Citation2015) found correlations between PTG and factors like employment, education duration, injury duration, life satisfaction, and subjective beliefs about post-injury change. Gender, age, injury severity, and community activity are also predictors of PTG (Pais-Hrit et al., Citation2019; Sawyer et al., Citation2010).
Qualitative studies have shown that ABI survivors experience positive changes in self-perception, life meaning, social relationships, life priorities, and fulfilment (Karagiorgou et al., Citation2018; Levack et al., Citation2014). Factors contributing to PTG include active engagement, willingness to change, social support, physical and mental activity, spirituality, and meaning-making strategies (Downing et al., Citation2021; Kersten et al., Citation2018; Lyon et al., Citation2021; Pais-Hrit et al., Citation2019; Seeto et al., Citation2017; Sekely & Zakzanis, Citation2019). Acceptance and self-awareness are also key, as is the individuality of the recovery process (Graff et al., Citation2018; Lyon et al., Citation2021). Despite valuable insights from qualitative research on PTG post-ABI, a systematic synthesis is lacking. Our meta-synthesis aims to bridge this gap by reviewing the literature comprehensively to identify facilitating factors and potential barriers to PTG. This work aims to provide greater insight into factors that predict PTG to inform professionals and rehabilitation provision, ultimately improving the recovery, quality of life, and sense of wellbeing of ABI survivors.
Methods
A meta-synthesis was conducted following guidelines by Lachal et al. (Citation2017), which build upon Thomas and Harden's (Citation2008) methodology. We also drew on guidelines for reflexive thematic analysis (Braun & Clarke, Citation2013, Citation2020, Citation2022), complimenting and enhancing the methodology outlined by Lachal et al. (Citation2017), as well as the updated PRISMA – guidelines (Page et al., Citation2021), to ensure that our systematic review process is clear and accessible. A formal protocol for the study was not pre-registered, aligning with recommendations that qualitative research should remain flexible to adapt, adjust, and respond to emerging issues during the research process (Braun & Clarke, Citation2020; Haven et al., Citation2020; Tong et al., Citation2007).
Literature search
A comprehensive search was conducted by Arroyo (first author) and Davies using the following databases: PsycINFO (Ebscohost), CINAHL (Ebscohost) and MEDLINE (Ebscohost). The search strategy focused on a combination of title and abstract searching as well as subject headings, while adapting the search to each database. Arroyo and Davies used three clusters of search terms to ensure adequate inclusion of articles. These search terms were related to (a) the topic of interest, (b) the population and (c) the research method. The CINAHL search strategy is presented in as an example. The databases were searched from the earliest available records to December 2022. Collaboration with Davies, a skilled information retrieval librarian, and regular meetings with Kemp (a Professor of Psychology and corresponding author) ensured a high level of accuracy and reliability throughout the process.
Table 1. Search strategy: CINAHL (Ebscohost) date run: 27th December 2022.
Inclusion and exclusion criteria
The inclusion and exclusion criteria for our study were discussed and approved by all authors before conducting the screening process began. These criteria were guided by the SPIDER framework (Cooke et al., Citation2012), characterizing the Sample, Phenomenon of Interest, Design, Evaluation, and Research Type. The sample included individuals aged 18 or older with Acquired Brain Injury (ABI) as a primary diagnosis. ABI refers to brain damage occurring post-birth due to external and internal causes like head trauma or stroke (Grace et al., Citation2015; Powell et al., Citation2012). The phenomenon of interest focused on perceived experiences of post-traumatic growth, including personal or psychological growth following ABI. Research designs encompassed qualitative studies reporting results from individual and focus group interviews or surveys, and mixed method designs that included qualitative findings. To ensure a comprehensive search and avoid bias, grey literature was included if relevant studies met inclusion criteria (McAuley et al., Citation2000; Thomas & Harden, Citation2008). All studies had to be in English and published in peer-reviewed journals. Exclusion criteria were: populations under 18, diagnoses other than ABI, studies focusing on non-survivors such as carers or relatives, purely quantitative designs, or studies not focusing on PTG. Comorbidity, defined as the presence of one or more chronic conditions alongside ABI (Jackson et al., Citation2020), was not a criterion for exclusion, acknowledging the complex nature of ABI and its frequent co-occurrence with other difficulties including mental health issues.
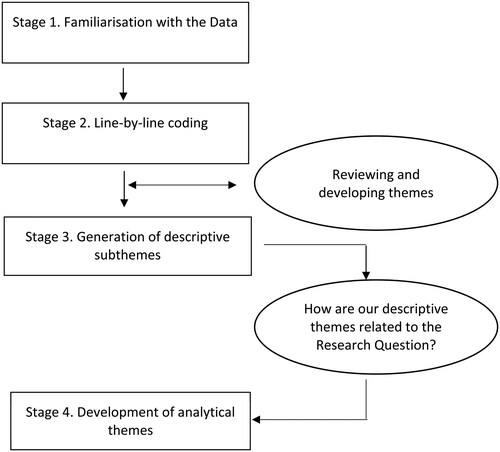
Thematic analysis
In this study, we synthesized the findings from identified studies using the procedures outlined by Lachal et al. (Citation2017) and Thomas and Harden (Citation2008), while also drawing on developments in reflexive thematic analysis (Braun & Clarke, Citation2013, Citation2020, Citation2022). This approach leveraged the researcher's knowledge and expertise to explore the deeper meaning of the data, guiding interpretation (Fisher et al., Citation2024; Kemp & Fisher, Citation2022; Mead et al., Citation2019, Citation2021). The synthesis began with a meticulous reading and re-reading of the identified studies, essential for effectively collecting, combining, and interpreting the data. Line-by-line coding of the findings was employed using NVivo 12 software, translating identified concepts into shared meanings across the studies. This process involved extensive labelling and categorizing of the data, leading to the development of descriptive subthemes. Consistent with Braun and Clarke's guidelines, the first author (Arroyo) was the only coder, supported by discussions and consensus meetings with co-authors. This collaborative practice provided a platform for challenging and refining emerging analytical themes, ensuring accuracy and mindfulness of biases and theoretical positions.
Reflexivity and positionality were central to our research process, given the clinical experiences of working with ABI survivors at a Community Brain Injury Service. Our experiences in applying positive psychology in rehabilitation contexts (e.g., Gibbs et al., Citation2022; Tulip et al., Citation2020; Wilkie et al., Citation2021) have shaped our perspectives. To enhance the trustworthiness of our data analysis and findings, we adopted a collaborative approach involving a diverse team that included graduate research students (PA, LW), a Consultant Clinical Psychologist (ZF), a Professor of Psychology (AHK), and a librarian skilled in information retrieval (ED). This diverse expertise enriched our understanding of the data, ensuring a balanced and comprehensive analysis. Our team engaged in group reflexivity, critically reflecting on our experiences and their impact on data interpretation. These practices of a multidisciplinary collaborative approach and active reflexivity were vital in maintaining the integrity and validity of our research, ensuring that our conclusions reflected the data and the diverse insights of our research team.
Quality assessment
The quality of the chosen studies was evaluated to critically assess the value and integrity of the data. As recommended by the Cochrane Collaboration, the CASP (Citation2018) checklist for qualitative research was chosen to aid quality and risk of bias assessment, addressing all of the components and assumptions of qualitative research (Lachal et al., Citation2017). A three-point scale (0 = not met, 1 = partially met and 2 = totally met) was used to assess each of the ten criteria included in the checklist (max total score = 20) (see ). Assessment determined that study quality was good with scores ranging from 15 to 20 out of a possible 20 (). All articles had a clear statement about their aims, findings and had taken ethical issues into consideration. However, description of data collection, analytical methods, inclusion criteria and considerations regarding the relationship between the researcher and the participants were sometimes insufficient. However, following discussion, it was concluded that the information provided was sufficient for our purposes and no studies were excluded on the basis of this assessment.
Table 2. Summary information of studies included in the meta-synthesis.
Results and discussion
Search results
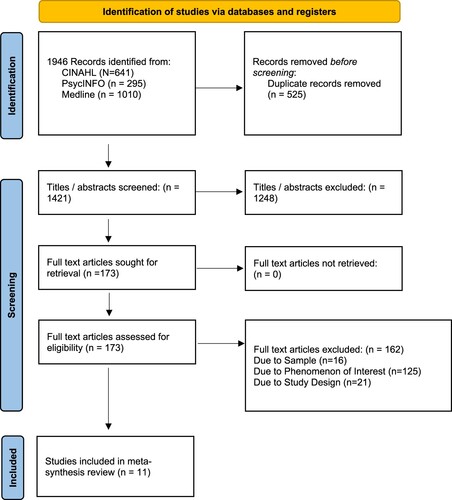
The selection process is shown in the PRISMA flow diagram in . All database search results were imported into the online software, Covidence, for managing and streamlining systematic reviews. All identified studies were initially screened by title and abstract, considering predefined inclusion and exclusion criteria. When abstracts did not provide sufficient information, the full text of individual studies were then read. Next, a second selection took place after examining the articles that passed the screening. Finally, the reference lists of the remaining articles were examined to look for studies that may have been missed in the previous search.
Figure 1. Flowchart for thematic analysis process from familiarization to identification of analytical themes.
A total of 1946 studies were identified through database searching, from which 1421 remained once duplicates were removed (). A total of 1248 articles were then excluded after screening titles and abstracts. One hundred and fifty-five studies were then excluded for reasons relating to inclusion criteria (e.g., participant age and methodology). Finally, a total of 11 studies were included in this meta-synthesis, two of which were identified within the grey literature. describes the characteristics of these studies, including study details, location, aim, method of data collection, analysis and details about the participants and their injuries. ()
Figure 2. PRISMA flow diagram showing the study selection process for the meta-synthesis.
Identified literature was published between 2000 and 2021; one was conducted in Ireland (Allen et al., Citation2022), four in the United States (Gillespie, Citation2019; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020), one was conducted in Denmark (Graff et al., Citation2018), another one in Germany (Kuenemund et al., Citation2016) and the remaining four were conducted in the United Kingdom (Karagiorgou et al., Citation2018; Lyon et al., Citation2021; Roundhill et al., Citation2007; Seeto et al., Citation2017). Five articles were designed to evaluate the experiences of PTG in ABI survivors (Allen et al., Citation2022; Karagiorgou et al., Citation2018; Lyon et al., Citation2021; McGinnis, Citation2011; Preble, Citation2020). One of these explored the experiences of living with ABI in individuals reporting low or high PTG (Allen et al., Citation2022). Another, focused on understanding the experiences of PTG after completing a positive psychotherapy pilot study (Karagiorgou et al., Citation2018), while three others sought to understand the development of PTG among ABI populations (Lyon et al., Citation2021; McGinnis, Citation2011; Preble, Citation2020). The remaining six (Gillespie, Citation2019; Graff et al., Citation2018; Kuenemund et al., Citation2016; Nochi, Citation2000; Roundhill et al., Citation2007; Seeto et al., Citation2017) had wider aims (e.g., impact of spirituality and understanding changes in identity following ABI) and PTG was one of their key findings. Ten studies used semi-structured individual or group interviews to collect their data (Allen et al., Citation2022; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017) whereas one study asked open questions to the participants by telephone or in person (Gillespie, Citation2019). In this study, questions focused on spirituality, in particular. Participant age varied between 18 and 77 years and time since injury ranged from 9 months to 60 years. Sample sizes ranged from 6 to 42 participants with a total of 167 participants across all eleven studies. Nine studies (Allen et al., Citation2022; Gillespie, Citation2019; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Preble, Citation2020; Roundhill et al., Citation2007) reported findings from males and females, while two studies did not provide details (Nochi, Citation2000; Seeto et al., Citation2017). Regarding recruitment, three studies (Lyon et al., Citation2021; Roundhill et al., Citation2007; Seeto et al., Citation2017) used community-based charities (e.g., Headway UK), one study (Karagiorgou et al., Citation2018) recruited participants through a variety of NHS clinics and another drew participants from acute rehabilitation facilities (Kuenemund et al., Citation2016). One study recruited participants from a single rehabilitation facility (Gillespie, Citation2019), another from a national rehabilitation hospital in Dublin (Allen et al., Citation2022) and another from the Copenhagen University Hospital (Graff et al., Citation2018). Other participants were recruited from post-acute inpatient rehabilitation facilities (McGinnis, Citation2011), local TBI support groups (Nochi, Citation2000) and online platforms (Preble, Citation2020). It is not clear if participants in Gillespie’s (Citation2019) study were living in the community. Two out of eleven studies (Allen et al., Citation2022; Lyon et al., Citation2021) included several types of ABI such as TBI, abscess and hematoma; two focused on stroke (Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016), five focused on TBI (Gillespie, Citation2019; Graff et al., Citation2018; McGinnis, Citation2011; Nochi, Citation2000; Roundhill et al., Citation2007), one focused on encephalitis, while another did not specify ABI type (Seeto et al., Citation2017). In one study (Karagiorgou et al., Citation2018) all participants reported emotional distress with scores at moderate levels or above on at least one sub-scale of the Depression Anxiety Stress Scale (DASS-21).
Findings
Three analytical themes including “Journey to Self-Rediscovery”, “Strength in Connection” and “Overcoming Obstacles”, emerged from the grouping descriptive subthemes (). Facilitating factors of Post-Traumatic Growth (PTG) following Acquired Brain Injury (ABI) were categorized into two primary groups: “Journey to Self-Rediscovery: Individual Pathways in Post-Traumatic Growth” and “Strength in Connection: The Role of Community and Relationships in Healing.” Additionally, the obstacles that appear to impede PTG were encapsulated in the theme “Overcoming Obstacles: Identifying and Navigating Barriers to Growth.” For a detailed breakdown of these themes, including all descriptive subthemes sorted by analytical category, refer to .
Figure 3. Pathway from acquired brain injury to post-traumatic growth and associated facilitators and barriers along that pathway.
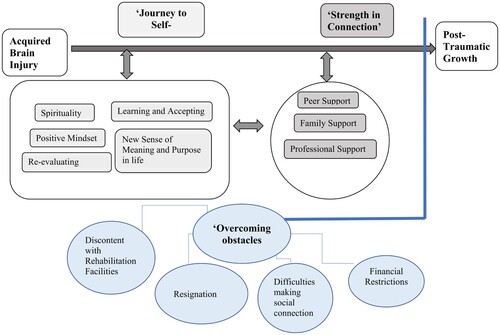
Table 3. Sub-themes identified in each study sorted by analytical theme.
Theme 1: “journey to self-rediscovery: individual pathways in post-traumatic growth”
Our research uncovered five factors at the level of the individual that are pivotal in the development of PTG following ABI. This journey, deeply rooted in self-reflection, involves redefining personhood and identity in the wake of the profound impact of ABI (Lyon et al., Citation2021; Roundhill et al., Citation2007). The journey is explored through five sub-themes: “Building a Positive Mindset,” “Re-evaluating Myself,” “Learning, Adjustment, and Acceptance,” “Finding New Meaning and Purpose,” and “Transformed Perspectives on Spirituality,” each playing a crucial role in the survivors’ path toward growth and rediscovery.
Building a positive mindset
Survivors who fostered a positive outlook on life demonstrated significant resilience. Focusing on strengths rather than weaknesses and setting achievable goals facilitated a sense of empowerment. Survivors found that immersing themselves in positive environments and engaging in uplifting social experiences, particularly with fellow ABI survivors, contributed significantly to maintaining this positive mindset. These interactions not only offered emotional support but also paved the way for setting and achieving new life goals, underlining an important link between the individual and the transformative potential of a supportive community (Allen et al., Citation2022; Karagiorgou et al., Citation2018; Lyon et al., Citation2021; Roundhill et al., Citation2007).
Re-evaluating myself
A key aspect of PTG was the survivors’ ability to compare their pre – and post-injury lives. This introspection often led to a newfound understanding of self, with many survivors realizing improvements and positive changes in their perspectives and priorities. This re-evaluation helped in developing a new sense of identity, reshaping life values, and cultivating new life perspectives, which were crucial in the journey toward growth (Allen et al., Citation2022; Graff et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Learning, adjustment, and acceptance
Embracing their new reality was essential for survivors in developing PTG. This phase involved a challenging yet transformative process of relearning old skills and acquiring new ones to adapt to a lifestyle with newfound limitations. For many, this period represented a “reset button,” providing an opportunity to learn about the impact of their brain injury and to recalibrate their lives accordingly (Allen et al., Citation2022; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Finding new meaning and purpose
The experience of ABI often led survivors to a profound reorganization of life priorities and the development of a renewed sense of purpose. This reorientation included the adoption of positive thinking strategies and problem-solving techniques, which played a significant role in overcoming challenges and fostering hope for the future. Survivors who successfully navigated this journey often reported an enhanced appreciation of life, a renewed sense of fulfilment, and gratitude (Allen et al., Citation2022; Gillespie, Citation2019; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Transformed perspectives on spirituality
ABI had a profound impact on their spiritual beliefs. This transformation often led to a strengthened or newly developed faith, providing a source of motivation and a deeper sense of connection to a higher power. Participants expressed feelings of gratitude and a newfound connection to spirituality, viewing their experience as an opportunity for a second chance at life (Gillespie, Citation2019; Karagiorgou et al., Citation2018; McGinnis, Citation2011; Preble, Citation2020).
In summary, our findings indicate that the process of self-rediscovery following ABI is a multifaceted journey involving positive mindset development, self-re-evaluation, learning and adaptation, finding new meaning, and often, a transformation in spiritual beliefs. Engaging in this journey enables survivors to embrace their new realities, leading to growth and positivity in their post-ABI lives.
Theme 2: “strength in connection: the role of community and relationships in healing”
The “Strength in Connection” theme emphasizes the crucial role of social ties and community support in fostering PTG after ABI. It underscores how positive interactions and relationships with peers, family, and professionals are instrumental in the healing journey. This theme is explored through three sub-themes: “Peer Support,” emphasizing the power of shared experiences and community among survivors; “Family Support,” highlighting the role of familial relationships in recovery; and “Professional Support,” focusing on the influence of healthcare professionals in guiding and empowering ABI survivors.
Peer support
Engagement with fellow ABI survivors through group activities and social gatherings has proven vital in developing a supportive community. This sense of belonging helps counteract feelings of isolation and societal judgment. For many survivors, peer support was a key factor in coming to terms with their injury and adapting to the changes it brought. Interacting with others who share similar experiences fosters mutual understanding and acceptance, contributing significantly to building a positive, forward-looking mindset (Allen et al., Citation2022; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Preble, Citation2020; Roundhill et al., Citation2007).
Family support
Positive support from family members, including partners and siblings, offers invaluable emotional and practical assistance. However, this support can be a double-edged sword, as some survivors worry about becoming a burden on their loved ones. The importance of family involvement in rehabilitation and healthcare decisions is crucial, as it can significantly enhance the recovery process and overall wellbeing of the survivor (Allen et al., Citation2022; Graff et al., Citation2018; Kuenemund et al., Citation2016; McGinnis, Citation2011; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Professional support
Healthcare professionals play a critical role in the survivors’ understanding of their injury and its limitations. Positive reinforcement from these professionals has been found to be incredibly impactful, encouraging survivors to adopt a proactive and hopeful approach to their new reality. Services such as the UK-wide brain injury charity, Headway, provide essential opportunities for connection and socialization, furthering the survivors’ understanding of their condition and fostering the development of adaptive coping skills and self-efficacy (Allen et al., Citation2022; Gillespie, Citation2019; Karagiorgou et al., Citation2018; Lyon et al., Citation2021; Roundhill et al., Citation2007; Seeto et al., Citation2017).
In summary, the research suggests that fostering social connections, particularly through peer support, is a major facilitator of PTG following ABI. Maintaining positive familial relationships and receiving professional guidance are also crucial in this regard. Findings also indicate that disruptions in family or romantic relationships can adversely affect survivors’ wellbeing and sense of social connectedness. Thus, providing comprehensive support to the entire family, including respite care and interventions aimed at strengthening relationships, can significantly enhance survivors’ social connections, wellbeing, and potential for PTG (Karagiorgou et al., Citation2018; Lyon et al., Citation2021; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Theme 3: “overcoming obstacles: identifying and navigating barriers to growth”
The “Overcoming Obstacles” theme delves into the challenges that can impede the development of PTG following ABI, highlighting four key barriers.
Resignation
A significant barrier identified was the struggle with accepting the new reality post-ABI. Acceptance was often a long, challenging, and complicated process, with many survivors grappling with the changes in their lives. It often emerged after realizing that returning to previous ways was no longer feasible. However, for some, this acceptance leaned more towards resignation than a wholehearted embrace of the new reality, leading to an internal conflict between longing for the past and adapting to the present (Allen et al., Citation2022; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; Lyon et al., Citation2021; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
Difficulties making social connections
Survivors often faced challenges in forming and maintaining social connections due to cognitive impairments and personality changes resulting from ABI. These difficulties negatively impacted their relationships and social life, leading to feelings of impatience, frustration, and isolation when interacting with those who could not understand their experience. The loss of friendships, ruptures in relationships with family members and subsequent isolation highlighted the importance of social support in the recovery journey (Allen et al., Citation2022; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Kuenemund et al., Citation2016; McGinnis, Citation2011; Preble, Citation2020; Roundhill et al., Citation2007).
Financial restrictions
Financial constraints emerged as a significant barrier, with some participants feeling limited in their recovery options due to lack of funds. Unemployment and insufficient support from the government and family exacerbated the sense of being overwhelmed, impacting both their rehabilitation opportunities and overall well-being (Allen et al., Citation2022; Nochi, Citation2000; Seeto et al., Citation2017).
Discontent with the rehabilitation process
Dissatisfaction with the rehabilitation process was a common theme among participants. Prolonged stays in care facilities, uncertainty about the recovery process, feelings of passivity in the rehabilitation process, and excessive assistance that compromised independence were sources of frustration. The need for more active involvement in the rehabilitation process was emphasized, highlighting the importance of empowering survivors to take control of their recovery. Additionally, some participants felt misunderstood by the healthcare system, as they considered that their condition should qualify for ongoing tailored support rather than short-term one-size-fits all recovery programmes (Allen et al., Citation2022; Graff et al., Citation2018; Karagiorgou et al., Citation2018; Lyon et al., Citation2021; McGinnis, Citation2011; Nochi, Citation2000; Preble, Citation2020; Roundhill et al., Citation2007; Seeto et al., Citation2017).
In summary, this theme sheds light on the complex challenges faced by ABI survivors on their journey towards PTG. The struggle with accepting their condition, often verging on resignation, highlights the internal conflict many survivors experience in reconciling their past and present selves. The difficulties in forming and maintaining social connections illuminate the critical role of empathy and understanding from those around the survivors. Financial constraints and dissatisfaction with the rehabilitation process further underscore the multifaceted nature of recovery, where practical, emotional, and financial support are all crucial. These findings emphasize the need for a holistic approach to neurorehabilitation and support for ABI survivors. Addressing these barriers requires not only individual resilience but also a supportive environment where survivors’ autonomy is respected, their challenges are understood, and their strengths are harnessed. This approach can significantly enhance the potential for PTG, ensuring that survivors not only overcome these obstacles but also find new paths to personal growth and fulfilment.
Clinical implications
We have presented a comprehensive synthesis of perspectives from individuals living with ABI, shedding light on critical factors influencing their potential for PTG, alongside perceived barriers to its attainment. Within ABI neurorehabilitation, facilitating PTG is considered an optimal outcome, which necessitates a thorough understanding of its underlying elements. These insights are essential for shaping the development or refinement of rehabilitation services that foster environments conducive to PTG whilst also addressing individual and systemic obstacles.
While PTG may not be universal, existing research, including our own, demonstrates a strong correlation between PTG and wellbeing (Wilkie et al., Citation2021 & Citation2023). Therefore, interventions aimed at enhancing wellbeing among individuals with ABI may act as catalysts for PTG, establishing a positive, mutually reinforcing relationship between the two. Our findings highlight a need for integrating different therapeutic approaches within models of neurorehabilitation, allowing for personal and systemic dimensions of ABI to be addressed. For instance, therapies such as Acceptance and Commitment Therapy (ACT), Positive Psychotherapy (PPT), and Meaning-Centred Cognitive Therapy (MCCT) would serve to enhance psychological flexibility, positive emotions and existential adaptation post-ABI respectively, all of which contribute to PTG (Hayes et al., Citation2006; Kangas & McDonald, Citation2011; Karagiorgou et al., Citation2018; Seligman et al., Citation2006; Wong, Citation2011, Citation2019). Additionally, social support networks, including peer groups and mentoring programmes, are crucial for emotional and social recovery, as well as systemic approaches that consider ABI within the context of an individual’s relationships and broader environment (Kersten et al., Citation2018; Lefkovits et al., Citation2020). An important caveat here is that survivors often feel a lack of autonomy and independence, and social and family connections with good intentions may instead disempower the individual as people are recategorized as “carers” and “cared for”, (Muldoon et al., Citation2019), which may pose barriers to PTG. This observation highlights the importance of working with the support networks of ABI survivors to ensure that such support provides a “social cure” rather than a “curse”.
The “Gold Standard” Holistic Neurorehabilitation Model (Ben-Yishay, Citation2000; Ben-Yishay & Daniels-Zide, Citation2000; Prigatano, Citation2000; Tate & Pledger, Citation2003; Wilson et al., Citation2009), lays the foundations for the experience of PTG as reported in this study, with its focus on the therapeutic milieu, shared understanding, meaningful, functional, goal-directed activities, psychological interventions, and working with carers and families. Our findings and previous work, highlight opportunities to further enhance the Holistic Model Neurorehabilitation by integrating insights from Wellbeing Science and Systems-Informed Thinking (Fisher et al., Citation2020; Gibbs, et al., Citation2022; Kemp & Fisher, Citation2022; Kern et al., Citation2020). For example, over recent years, we have developed a new theoretical framework of wellbeing (Fisher et al., Citation2020; Kemp et al., Citation2017; Kemp & Fisher, Citation2022; Mead et al., Citation2021), which, in conjunction with the Holistic Model of Neurorehabilitation, has guided the redesign of our community neurorehabilitation services. Our aim was to establish more effective models of care that prioritize the facilitation of health and wellbeing, rather than solely focusing on deficit reduction and distress alleviation. Additionally, we have employed “systems-informed thinking” (Kern et al., Citation2020; Gibbs et al., Citation2022a) to foster sustainable opportunities for social connection, meaning-making, and community reintegration through collaborative partnerships with community providers (Gibbs et al., Citation2022b; Tulip et al., Citation2020; Wilkie et al., Citation2021). This creates the long-term community infrastructure to support participants’ need for immersing themselves in positive environments and engaging in uplifting social experiences, which significantly contributed to maintaining a positive mindset. Our work shows that these environments and the social connections they promote not only offer emotional support but also facilitate the setting of and achieving new life goals, underlining an important link between the individual and the transformative potential of a wider supportive community (Gibbs et al., Citation2022; Kemp & Fisher, Citation2022).
Our approach also takes a “top-down” approach by working with partners to reduce the impact of socio-structural factors on health outcomes. For example, by working with providers to develop grants and secure additional funding for community partner involvement, there is no economic barrier toward accessing sustainable community interventions that promote wellbeing long after discharge. This is necessary for PTG, given that time since injury has been found to be a predictor of PTG, whereby the longer the time since injury, the higher the levels of PTG. Accordingly, we argue that in order to avoid the reported barrier of “resignation”, it is important that community neurorehabilitation services act as a steppingstone to bridge the gap between rehabilitation and longer-term community integration, ensuring there are sustainable opportunities for environments and social experiences that promote PTG and wellbeing more generally.
Finally, it must be acknowledged that access to neurorehabilitation remains limited for many ABI patients (McKevitt et al., Citation2011). Moreover, our findings suggest that even for those who do receive care, it often falls short of expected standards and gold standard models. Our work highlights the unmet need for quality neurorehabilitation services that supports people to achieve optimal functioning, and advocates for models that promote active patient participation and shared decision-making (NICE Guidelines, Citation2022; Valderas Martinez et al., Citation2016), consistent with the WHO’s “Rehabilitation Call for Action”. Our findings expose the gap between aspirational guidelines and the reality many people with ABI face and provide insights into the elements needed to promote optimal functioning.
Study limitations and future directions
In conducting our meta-synthesis, we faced several methodological limitations, which not only informed the direction of our current study but have also help to identify distinct pathways for future research. Acknowledging the subjective nature of thematic analysis, a characteristic that enriches quantitative research by providing depth and context, we employed a multi-layered approach for data interpretation. This approach, involving cross-validation and refinement by a diverse research team, aimed to harness the strengths of thematic subjectivity while ensuring a comprehensive and nuanced understanding of our findings. Our analysis, primarily focused on Western-centric studies, highlights the need for broader cultural inclusion in future research. This presents an opportunity to expand our understanding of PTG in ABI survivors across a wider cultural spectrum, incorporating perspectives from non-Western and non-English speaking communities. We also identified gaps in the reporting of ethical considerations and detailed population demographics in source articles, pointing to limitations in existing research and pave the way for more comprehensive reporting in future studies, including a focus on detailed participant demographics, injury types, severity, and more transparent accounts of ethical considerations and researcher reflexivity. Furthermore, the relationship between PTG and wellbeing in ABI survivors, currently understood through a limited temporal lens, opens avenues for further longitudinal research. Such studies could explore the sustainability and long-term impacts of PTG, particularly how interventions targeting wellbeing might support and sustain PTG over time. Our findings also suggest that aspects relating to wellbeing may facilitate PTG, providing a fertile ground for future research to clarify and expand upon these observations, thereby contributing to a more nuanced understanding of recovery and growth in ABI survivors.
Conclusions
Our meta-synthesis has illuminated the multifaceted journey of self-rediscovery, the strength derived from connections, and the obstacles faced by ABI survivors, and has also underscored the critical role of holistic neurorehabilitation in facilitating Post-Traumatic Growth (PTG). Our findings and reflections highlight the necessity of incorporating varied therapeutic approaches, along with acknowledging the vital role of social support systems. Future studies are needed to explore the long-term sustainability of PTG and how interventions targeting wellbeing might support its continuity. The insights gained from this synthesis provide a foundation for future research activities, advocating for a holistic approach to neurorehabilitation that not only addresses the complex challenges faced by ABI survivors but also enhances their capacity for growth and contributes positively to the broader community.
Codebook - PTG coding with quotation examples.docx
Download MS Word (42.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Allen, N., Hevey, D., Carton, S., & O'Keeffe, F. (2022). Life is about “constant evolution”: The experience of living with an acquired brain injury in individuals who report higher or lower posttraumatic growth. Disability and Rehabilitation, 44(14), 3479–3492. https://doi.org/10.1080/09638288.2020.1867654
- Andrewes, H. E., Walker, V., & O'Neill, B. (2014). Exploring the use of positive psychology interventions in brain injury survivors with challenging behaviour. Brain Injury, 28(7), 965–971. https://doi.org/10.3109/02699052.2014.888764
- Baker, F. A., Tamplin, J., Rickard, N., New, P., Ponsford, J., Roddy, C., & Lee, Y.-E. C. (2018). Meaning making process and recovery journeys explored through songwriting in early neurorehabilitation: Exploring the perspectives of participants of their self-composed songs through the interpretative phenomenological analysis. Frontiers in Psychology, 9, Article1422. https://doi.org/10.3389/fpsyg.2018.01422
- Bannon, S. M., Fishbein, N. S., Lovette, B. C., Wang, K., Waterhouse, C., Rajala, C. E., Costantini, H., Lichstein, K. H., Giacino, J. T., Vranceanu, A.-M., & Greenberg, J. (2022). A meta-synthesis of individual, interpersonal, and systemic factors impacting resilience after traumatic brain injury. Rehabilitation Psychology, 67(4), 535–545. https://doi.org/10.1037/rep0000462
- Barber, S., Bate, A., Adcock, A., Harker, R., Roberts, N., Woodhouse, J., & Mackley, A. (2018). Acquired brain injury. House of Commons Library. http://researchbriefings.files.parliament.uk/documents/CDP-2018-0145/CDP-2018-0145.pdf
- Ben-Yishay, Y. (2000). International handbook of neuropsychological rehabilitation. 127–135. https://doi.org/10.1007/978-1-4757-5569-5_8
- Ben-Yishay, Y., & Daniels-Zide, E. (2000). Examined lives: Outcomes after holistic rehabilitation. Rehabilitation Psychology, 45(2), 112–129. https://doi.org/10.1037/0090-5550.45.2.112
- Braun, V., & Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. SAGE.
- Braun, V., & Clarke, V. (2020). One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 18(3), 328–352. https://doi.org/10.1080/14780887.2020.1769238
- Braun, V., & Clarke, V. (2022). Conceptual and design thinking for thematic analysis. Qualitative Psychology, 9(1), 3–26. https://doi.org/10.1037/qup0000196
- Cattelani, R., Zettin, M., & Zoccolotti, P. (2010). Rehabilitation treatments for adults with behavioral and psychosocial disorders following acquired brain injury: A systematic review. Neuropsychology Review, 20(1), 52–85. https://doi.org/10.1007/s11065-009-9125-y
- Collicutt McGrath, J., & Linley, P. A. (2006). Post-traumatic growth in acquired brain injury: A preliminary small scale study. Brain Injury, 20(7), 767–773. https://doi.org/10.1080/02699050600664566
- Cooke, A., Smith, D., & Booth, A. (2012). Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qualitative health research, 22(10), 1435–1443. https://doi.org/10.1177/1049732312452938
- Corrigan, J. D., Selassie, A. W., & Orman, J. A. (Langlois). (2010). The epidemiology of traumatic brain injury. Journal of Head Trauma Rehabilitation, 25(2), 72–80. https://doi.org/10.1097/HTR.0b013e3181ccc8b4
- Critical Appraisal Skills Programme. (2018). CASP qualitative studies checklist. https://casp-uk.net/casp-tools-checklists/
- de Freitas Cardoso, M. G., Faleiro, R. M., de Paula, J. J., Kummer, A., Caramelli, P., Teixeira, A. L., de Souza, L. C., & Miranda, A. S. (2019). Cognitive impairment following acute mild traumatic brain injury. Frontiers in Neurology, 10(198), 1–9. https://doi.org/10.3389/fneur.2019.00198
- Dewan, M. C., Rattani, A., Gupta, S., Baticulon, R. E., Hung, Y. C., Punchak, M., Agrawal, A., Adeleye, A. O., Shrime, M. G., Rubiano, A. M., Rosenfeld, J. V., & Park, K. B. (2018). Estimating the global incidence of traumatic brain injury. Journal of Neurosurgery, 130(4), 1080–1097. https://doi.org/10.3171/2017.10.JNS17352
- Downing, M., Hicks, A., Braaf, S., Myles, D., Gabbe, B., Cameron, P., Ameratunga, S., & Ponsford, J. (2021). Factors facilitating recovery following severe traumatic brain injury: A qualitative study. Neuropsychological Rehabilitation, 31(6), 889–913. https://doi.org/10.1080/09602011.2020.1744453
- Feigin, V. L., Brainin, M., Norrving, B., Martins, S., Sacco, R. L., Hacke, W., Fisher, M., Pandian, J., & Lindsay, P. (2022). World Stroke Organization (WSO): Global stroke fact sheet 2022. International Journal of Stroke, 17(1), 18–29. https://doi.org/10.1177/17474930211065917
- Fisher, Z., Field, S., Fitzsimmons, D., Hutchings, H., Carter, K., Tod, D., Gracey, F., Knight, A., & Kemp, A. H. (2024). Group-based positive psychotherapy for people living with acquired brain injury: A protocol for a feasibility study. Pilot and Feasibility Studies, 10(1), 38. https://doi.org/10.1186/s40814-024-01459-7
- Fisher, Z., Galloghly, E., Boglo, E., Gracey, F., & Kemp, A. H. (2020). Emotion, wellbeing and the neurological disorders. In Encyclopedia of behavioral neuroscience (2nd ed., pp. 220–234). Elsevier. https://doi.org/10.1016/b978-0-12-819641-0.00013-x
- Gibbs, K., Kemp, A. H., & Fisher, Z. (2022a). Towards a culture of care for societal wellbeing: A perspective from the healthcare sector. In A. H. Kemp & D. J. Edwards (Eds.), Broadening the scope of wellbeing science (pp. 43–58). Palgrave Macmillan. https://doi.org/10.1007/978-3-031-18329-4_4
- Gibbs, K., Wilkie, L., Jarman, J., Barker-Smith, A., Kemp, A. H., & Fisher, Z. (2022b). Riding the wave into wellbeing: A qualitative evaluation of surf therapy for individuals living with acquired brain injury. PLoS One, 17(4), e0266388. https://doi.org/10.1371/journal.pone.0266388
- Gillespie, E. (2019). A qualitative pilot study of spirituality in long-term recovery in acquired brain injury. Journal of Pastoral Care & Counseling: Advancing Theory and Professional Practice Through Scholarly and Reflective Publications, 73(2), 96–105. https://doi.org/10.1177/1542305019853588
- Goldberg, L. D., McDonald, S. D., & Perrin, P. B. (2019). Predicting trajectories of posttraumatic growth following acquired physical disability. Rehabilitation Psychology, 64(1), 37–49. https://doi.org/10.1037/rep0000247
- Gould, K. R., & Ponsford, J. L. (2014). A longitudinal examination of positive changes in quality-of-life after traumatic brain injury. Brain Injury, 29(3), 283–290. https://doi.org/10.3109/02699052.2014.974671
- Grace, J. J., Kinsella, E. L., Muldoon, O. T., & Fortune, D. G. (2015). Post-traumatic growth following acquired brain injury: A systematic review and meta-analysis. Frontiers in Psychology, 6, Article 1162. https://doi.org/10.3389/fpsyg.2015.01162
- Graff, H. J., Christensen, U., Poulsen, I., & Egerod, I. (2018). Patient perspectives on navigating the field of traumatic brain injury rehabilitation: A qualitative thematic analysis. Disability and Rehabilitation, 40(8), 926–934. https://doi.org/10.1080/09638288.2017.1280542
- Haven, T. L., Errington, T. M., Gleditsch, K. S., van Grootel, L., Jacobs, A. M., Kern, F. G., Piñeiro, R., Rosenblatt, F., & Mokkink, L. B. (2020). Preregistering qualitative research: A delphi study. International Journal of Qualitative Methods, 19, 160940692097641. https://doi.org/10.1177/1609406920976417
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006
- Humphreys, I., Wood, R. L., Phillips, C. J., & Macey, S. (2013). The costs of traumatic brain injury: A literature review. ClinicoEconomics and Outcomes Research, 5, 281–287. https://doi.org/10.2147/CEOR.S44625
- Jackson, H. M., Troeung, L., & Martini, A. (2020). Prevalence, patterns, and predictors of multimorbidity in adults With acquired brain injury at admission to staged community-based rehabilitation. Archives of Rehabilitation Research and Clinical Translation, 2(4), 100089. https://doi.org/10.1016/j.arrct.2020.100089
- Kamalakannan, S. K., Gudlavalleti, A. S., Murthy Gudlavalleti, V. S., Goenka, S., & Kuper, H. (2015). Challenges in understanding the epidemiology of acquired brain injury in India. Annals of Indian Academy of Neurology, 18(1), 66–70. https://doi.org/10.4103/0972-2327.151047
- Kangas, M., & McDonald, S. (2011). Is it time to act? The potential of acceptance and commitment therapy for psychological problems following acquired brain injury. Neuropsychological Rehabilitation, 21(2), 250–276. https://doi.org/10.1080/09602011.2010.540920
- Karagiorgou, O., Evans, J. J., & Cullen, B. (2018). Post-traumatic growth in adult survivors of brain injury: A qualitative study of participants completing a pilot trial of brief positive psychotherapy. Disability and Rehabilitation, 40(6), 655–659. https://doi.org/10.1080/09638288.2016.1274337
- Kemp, A. H., Arias, J. A., & Fisher, Z. (2017). Social ties, health and wellbeing: A literature review and model. In A. Ibáñez, L. Sedeño, & A. M. García (Eds.), Neuroscience and social science: The missing link (pp. 397–427). Springer International Publishing AG. https://doi.org/10.1007/978-3-319-68421-5_17
- Kemp, A. H., & Fisher, Z. (2022). Wellbeing, whole health and societal transformation: Theoretical insights and practical applications. Global Advances in Health and Medicine, 11, 1–16. https://doi.org/10.1177/21649561211073077
- Kern, Margaret L, Williams, Paige, Spong, Cass, Colla, Rachel, Sharma, Kesh, Downie, Andrea, Taylor, Jessica A., Sharp, Sonia, Siokou, Christine, & Oades, Lindsay G. (2020). Systems informed positive psychology. The Journal of Positive Psychology, 15(6), 705–715. https://doi.org/10.1080/17439760.2019.1639799
- Kersten, P., Cummins, C., Kayes, N., Babbage, D., Elder, H., Foster, A., Weatherall, M., Siegert, R. J., Smith, G., & McPherson, K. (2018). Making sense of recovery after traumatic brain injury through a peer mentoring intervention: A qualitative exploration. BMJ Open, 8(10), e020672. https://doi.org/10.1136/bmjopen-2017-020672
- Kuenemund, A., Zwick, S., Rief, W., & Exner, C. (2016). (Re-)defining the self - enhanced posttraumatic growth and event centrality in stroke survivors: A mixed-method approach and control comparison study. Journal of Health Psychology, 21(5), 679–689. https://doi.org/10.1177/1359105314535457
- Lachal, J., Revah-Levy, A., Orri, M., & Moro, M. R. (2017). Metasynthesis: An original method to synthesize qualitative literature in psychiatry. Frontiers in Psychiatry, 8, Article 269. https://doi.org/10.3389/fpsyt.2017.00269
- Lefkovits, A. M., Hicks, A. J., Downing, M., & Ponsford, J. (2020). Surviving the “silent epidemic”: A qualitative exploration of the long-term journey after traumatic brain injury. Neuropsychological Rehabilitation, 31, 1582–1606. https://doi.org/10.1080/09602011.2020.1787849
- Levack, W. M., Boland, P., Taylor, W. J., Siegert, R. J., Kayes, N. M., Fadyl, J. K., & McPherson, K. M. (2014). Establishing a person-centred framework of self-identity after traumatic brain injury: A grounded theory study to inform measure development. BMJ Open, 4(5), e004630. https://doi.org/10.1136/bmjopen-2013-004630
- Luengo-Fernandez, R., Violato, M., Candio, P., & Leal, J. (2020). Economic burden of stroke across Europe: A population-based cost analysis. European Stroke Journal, 5(1), 17–25. https://doi.org/10.1177/2396987319883160
- Lyon, I., Fisher, P., & Gracey, F. (2021). “Putting a new perspective on life”: A qualitative grounded theory of posttraumatic growth following acquired brain injury. Disability and Rehabilitation, 43(22), 3225–3233. https://doi.org/10.1080/09638288.2020.1741699
- McAuley, L., Pham, B., Tugwell, P., & Moher, D. (2000). Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? The Lancet, 356(9237), 1228–1231. https://doi.org/10.1016/S0140-6736(00)02786-0
- McGinnis, C. K. (2011). Finding the silver lining: Posttraumatic growth after traumatic brain injury (Publication No. 3492239) [Doctoral dissertation]. Chestnut Hill College. ProQuest Dissertations & Theses Global. https://www.proquest.com/pqdtglobal1/dissertations-theses/finding-silver-lining-posttraumatic-growth-after/docview/916789621/sem-2?accountid=14680
- McKevitt, C., Fudge, N., Redfern, N., Sheldenkar, A., Crichton, A., & Wolfe, C. (2011). UK stroke survivor needs survey. Stroke Association and Kings College London.
- Mead, J., Fisher, Z., & Kemp, A. H. (2021). Moving beyond disciplinary silos towards a transdisciplinary model of wellbeing: An invited review. Frontiers in Psychology, 12, Article 642093. https://doi.org/10.3389/fpsyg.2021.642093
- Mead, J., Fisher, Z., Wilkie, L., Gibbs, K., Pridmore, J., Tree, J., & Kemp, A. H. (2019). Rethinking wellbeing: Toward a more ethical science of wellbeing that considers current and future generations. Authorea, https://doi.org/10.22541/au.156649190.08734276
- Muldoon, O. T., Walsh, R. S., Curtain, M., Crawley, L., & Kinsella, E. L. (2019). Social cure and social curse: Social identity resources and adjustment to acquired brain injury. European Journal of Social Psychology, 49(6), 1272–1282. https://doi.org/10.1002/ejsp.2564
- National Institute for Health and Care Excellence. (2022). Shared decision making. https://www.nice.org.uk/guidance/ng197
- National Institute for Health and Care Excellence. (2023). Head injury: Assessment and early management (NICE guideline NG 232). https://www.nice.org.uk/guidance/ng232
- Nochi, M. (2000). Reconstructing self-narratives in coping with traumatic brain injury. Social Science & Medicine, 51(12), 1795–1804. https://doi.org/10.1016/S0277-9536(00)00111-8
- Osborn, A. J., Mathias, J. L., & Fairweather-Schmidt, A. K. (2014). Depression following adult, non-penetrating traumatic brain injury: A meta-analysis examining methodological variables and sample characteristics. Neuroscience & Biobehavioral Reviews, 47, 1–15. https://doi.org/10.1016/j.neubiorev.2014.07.007
- Ownsworth, T., & Fleming, J. (2011). Growth through loss after brain injury. Brain Impairment, 12(2), 79–81. https://doi.org/10.1375/brim.12.2.79
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Aki, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Whiting, P. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLOS Medicine, 18(3), Article e1003583. https://doi.org/10.1371/journal.pmed.1003583
- Pais-Hrit, C., Wong, D., Gould, K. R., & Ponsford, J. (2019). Behavioural and functional correlates of post-traumatic growth following traumatic brain injury. Neuropsychological Rehabilitation, 30(7), 1205–1223. https://doi.org/10.1080/09602011.2019.1569536
- Powell, T., Gilson, R., & Collin, C. (2012). TBI 13 years on: Factors associated with post-traumatic growth. Disability and Rehabilitation, 34(17), 1461–1467. https://doi.org/10.3109/09638288.2011.644384
- Preble, C. I. (2020). Posttraumatic growth in emerging adults diagnosed with infective and autoimmune-mediated encephalitis (Publication No. 28086929) [Doctoral dissertation]. Fielding Graduate University. ProQuest Dissertations & Theses Global. https://www.proquest.com/pqdtglobal/docview/2440910929/BB71A220C54A4A41PQ/1?accountid=14680
- Prigatano, G. P. (2000). Critical issues in neuropsychology. Critical Issues in Neuropsychology, 115–125. https://doi.org/10.1007/978-1-4757-5569-5_7
- Rabinowitz, A. R., & Levin, H. S. (2014). Cognitive sequelae of traumatic brain injury. Psychiatric Clinics of North America, 37(1), 1–11. https://doi.org/10.1016/j.psc.2013.11.004
- Reinkensmeyer, D. J., Kahn, L. E., Averbuch, M., McKenna-Cole, A., Schmit, B. D., & Rymer, W. Z. (2014). Understanding and treating arm movement impairment after chronic brain injury: Progress with the ARM guide. Journal of Rehabilitation Research and Development, 37(6), 653–662.
- Rogan, C., Fortune, D. G., & Prentice, G. (2013). Post-traumatic growth, illness perceptions and coping in people with acquired brain injury. Neuropsychological Rehabilitation, 23(5), 639–657. https://doi.org/10.1080/09602011.2013.799076
- Roundhill, S. J., Williams, W. H., & Hughes, J. M. (2007). The experience of loss following traumatic brain injury: Applying a bereavement model to the process of adjustment. Qualitative Research in Psychology, 4(3), 241–257. https://doi.org/10.1080/14780880701473540
- Sawyer, A., Ayers, S., & Field, A. P. (2010). Posttraumatic growth and adjustment among individuals with cancer or HIV/AIDS: A meta-analysis. Clinical Psychology Review, 30(4), 436–447. https://doi.org/10.1016/j.cpr.2010.02.004
- Seeto, E., Scruby, K., & Greenhill, T. (2017). ‘Your whole life becomes a recovery’: Experiences of young adults following acquired brain injury. Counselling Psychology Review, 32(4), 39–48. https://doi.org/10.53841/bpscpr.2017.32.4.39
- Sekely, A., & Zakzanis, K. K. (2019). The relationship between post-traumatic growth and return to work following mild traumatic brain injury. Disability and Rehabilitation, 41(22), 2669–2675. https://doi.org/10.1080/09638288.2018.1476598
- Seligman, M., Rashid, T., & Parks, A. C. (2006). Positive psychotherapy. American Psychologist, 61(8), 774–788. https://doi.org/10.1037/0003-066X.61.8.774
- Silva, J., Ownsworth, T., Shields, C., & Fleming, J. (2011). Enhanced appreciation of life following acquired brain injury: Post-traumatic growth at 6 months postdischarge. Brain Impairment, 12(2), 93–104. https://doi.org/10.1375/brim.12.2.93
- Tate, D. G., & Pledger, C. (2003). An integrative conceptual framework of disability: New directions for research. American Psychologist, 58(4), 289–295. https://doi.org/10.1037/0003-066X.58.4.289
- Tedeschi, R. G., & Calhoun, L. G. (2004). Target ARTICLE: "posttraumatic growth: Conceptual foundations and empirical evidence". Psychological Inquiry, 15(1), 1–18. https://doi.org/10.1207/s15327965pli1501_01
- Thomas, J., & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8, Article 45. https://doi.org/10.1186/1471-2288-8-45
- Tong, A., Sainsbury, P., & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042
- Tulip, C., Fisher, Z., Bankhead, H., Wilkie, L., Pridmore, J., Gracey, F., Tree, J., & Kemp, A. H. (2020). Building wellbeing in people with chronic conditions: A qualitative evaluation of an 8-week positive psychotherapy intervention for people living with an acquired brain injury. Frontiers in Psychology, 11, Article 66. https://doi.org/10.3389/fpsyg.2020.00066
- Valderas Martinez, J., Ricci-Cabello, N., Prasopa-Plazier, N., Wensing, M., Santana, M., Kaitiritimba, R., Vazquez Curiel, E., & Murphy, M. (2016). Patient engagement: Who technical series on safer primary care. ORE Home. https://ore.exeter.ac.uk/repository/handle/10871/25108
- Wilkie, L., Arroyo, P., Conibeer, H., Kemp, A. H., & Fisher, Z. (2021). The impact of psycho-social interventions on the wellbeing of individuals with acquired brain injury during the COVID-19 pandemic. Frontiers in Psychology, 12, Article 793. https://doi.org/10.3389/fpsyg.2021.648286
- Wilkie, L., Arroyo, P., Conibeer, H., Kemp, A. H., & Fisher, Z. (2021). The Impact of Psycho-Social Interventions on the Wellbeing of Individuals With Acquired Brain Injury During the COVID-19 Pandemic. Front Psychol, 12.
- Wilkie, L., Arroyo, P., Kemp, A., & Fisher, Z. (2023). Posttraumatic growth in acquired brain injury: A narrative review. In R. Berger (Ed.), The Routledge international handbook of posttraumatic growth (pp. 367–379). Taylor & Francis.
- Wilson, B. A., Gracey, F., Evans, J. J., Bateman, A., & Malley, D. (2009). Neuropsychological Rehabilitation: Theory, Models, Therapy and Outcome. Neuropsychological Rehabilitation, 47–67. https://doi.org/10.1017/cbo9780511581083.006
- Wong, P. T. P. (2011). Meaning-centered counseling and therapy: An integrative and comprehensive approach to motivational counseling and addiction treatment. In W. M. Cox & E. Klinger (Eds.), Handbook of motivational counseling: Goal-based approaches to assessment and intervention with addiction and other problems (2nd ed., pp. 461–487). Wiley Blackwell. https://doi.org/10.1002/9780470979952.ch19
- Wong, P. T. P. (2019). Second wave positive psychology’s (PP 2.0) contribution to counselling psychology. Counselling Psychology Quarterly, 32(3–4), 275–284. https://doi.org/10.1080/09515070.2019.1671320
