ABSTRACT
Stroke inpatients in rehabilitation clinics are highly inactive in their free time and often depend on staff members to transport them to scheduled therapies. This study examines how distances between spaces in rehabilitation clinics impact patients’ mobility. Seventy patients were shadowed over the course of one ordinary day in rehabilitation. Shadowing was accompanied by patient and staff questionnaires. Both patients and staff members described the labyrinthine built environment with long corridors that all look similar. Patients covered substantial daily distances in the clinics, and longer distances were significantly related to encountering more mobility barriers and dependence on staff. Compact layouts with vertically separate wards and main therapy areas resulted in reduced travel distances compared to more complex building layouts. Patients’ mobility abilities were occasionally observed to change on different distances and even throughout the day. As distances result from the building's layout, greater attention needs to be paid to this aspect of the built environment in the early design stages. This is especially the case since other built-environment barriers were found to be intertwined with long distances. All patients may be independently mobile if distances between their most important areas (wards, therapy areas and dining spaces) are carefully planned.
Introduction
Infection control, recovery speed and success, as well as patient activity levels, well-being and overall satisfaction, are all positively influenced by various built environment aspects of healthcare facilities (Alfonsi et al., Citation2014; Brambilla et al., Citation2019; Ulrich et al., Citation2008). However, much of this research is conducted in acute care hospitals, leaving rehabilitation clinics relatively underrepresented. Rehabilitation clinics are an important setting to investigate for their significance in patients’ rehabilitation. This is an environment where, after a hospital stay, many patients need to re-learn the impaired skills needed to return home. Given the differences between a hospital and a rehabilitation environment, applying evidence-based design concepts from other healthcare settings to a rehabilitation setting is unlikely to completely meet their specific goals and purposes (Lipson-Smith et al., Citation2019).
Stroke patients are among the most common patient groups that continue their recovery in rehabilitation clinics. Their length of stay in these facilities in Germany ranges from several weeks (Bussmann et al., Citation2018; Nikolaus et al., Citation2006) to several months in some instances. Because stroke causes complex motor, cognitive and other impairments (Adamson et al., Citation2004), rehabilitation includes multidisciplinary therapy, most commonly physiotherapy and occupational therapy (Hempler et al., Citation2018). Inpatients stay on the wards and attend multiple therapies each day, sometimes in different parts of the building. The physical environment of rehabilitation clinics and its role in patient recovery deserve special attention due to the extended length of stay compared to other healthcare facilities such as hospitals. However, this research field is still in its early stages (Lipson-Smith et al., Citation2021). Much remains unknown about the spatial needs of stroke patients in rehabilitation and how the design of rehabilitation clinics can better support the care processes.
Rehabilitation environment and patients’ needs
Even though the physical environment should be regarded as an active component in neurological rehabilitation (Shannon et al., Citation2018), little is known about how rehabilitation settings affect stroke patients’ recovery and well-being. These environments are important because: (1) stroke patients spend a substantial amount of time in them during rehabilitation; (2) these patients are in different rehabilitation stages and use different mobility aids (e.g. a wheelchair or a walker), which impacts their interactions with space; and (3) they are expected to find their way around the clinic to attend daily therapies independently.
Complex rehabilitation programmes require large multistorey buildings. Their built environment usually consists of patient wards, therapy rooms, communal areas (such as a living room, a library, or a game room), a shared cafeteria, diagnostic facilities, administration offices and other staff offices. The existing buildings are often not purposely built for rehabilitation, and new clinics are planned without sufficient evidence-based design knowledge (Lipson-Smith et al., Citation2020). These vastly different approaches in each facility's built environment design are unlikely always to be suitable for stroke patients’ rehabilitation goals and recovery.
The main goals of stroke rehabilitation are mobility and daily activities (ADL) independence (Luker et al., Citation2015). The sudden loss of control, complex post-stroke impairments and the long recovery process can contribute to depression and anxiety in patients (Gaete Moncayo & Bogousslavsky, Citation2008; Pohjasvaara et al., Citation1998), which have been linked to delays in stroke rehabilitation and increased functional dependence (Pohjasvaara et al., Citation2001). Regaining independence in mobility and daily activities typically signifies recovery for patients who believe they have regained control and made significant rehabilitation progress (Luker et al., Citation2015). This process of recovering mobility and ADL autonomy occurs not just in therapies but also through physical, cognitive and social activities that patients engage in during their free time.
At the same time, the size and spatial configuration of rehabilitation clinics can create wayfinding challenges and other mobility barriers for patients (Kevdzija & Marquardt, Citation2018), who often experience navigation (Claessen et al., Citation2017) and motor (Langhorne et al., Citation2009) impairments after a stroke. Patients also describe the lack of places to meet others and the sterility and emptiness of the existing communal spaces in stroke unit wards (Anåker et al., Citation2019). Even though most rehabilitation facilities include a communal area for patients, their location in the building, distance from patient rooms, and design are not based on evidence-based knowledge about patients’ spatial needs (Kevdzija & Marquardt, Citation2021). Thus, there appears to be a discrepancy between the way rehabilitation environments are designed and their intended purpose: to support stroke patients’ recovery, activity and mobility.
Activity levels during rehabilitation
Although stroke patients, physicians and therapists highly prioritize mobility and activity during rehabilitation, the common conclusion of research studies conducted in different stroke rehabilitation environments is that patients are inactive in general (Anåker et al., Citation2018; Janssen et al., Citation2014a; Kārkliņa et al., Citation2021; Kevdzija & Marquardt, Citation2021; West & Bernhardt, Citation2012). Stroke patients undergoing rehabilitation spend most of their free time inactive and in bed, which contrasts with the recommendations for stroke care (Billinger et al., Citation2014). Besides the factors such as various post-stroke cognitive and physical impairments (Van De Port et al., Citation2006) and post-stroke fatigue (Duncan et al., Citation2015; MacIntosh et al., Citation2017), which can influence their mobility and activity levels, the physical environment could also be a contributor to patients’ inactivity. Previous investigations in different settings for neurological rehabilitation indicate that their physical environment is hindering for stroke patients (Anåker et al., Citation2017; Kevdzija & Marquardt, Citation2018; Newall et al., Citation1997) and promotes loneliness (Anåker et al., Citation2019).
Due to the importance of patient activity during rehabilitation, recent research has focused on using the concept of an enriched environment to increase their activity levels. In the context of rehabilitation, environmental enrichment refers to the provision of a stimulating setting with a variety of materials for patients to exercise their cognitive and physical abilities, such as books, puzzles, newspapers, games, music (Janssen et al., Citation2014b), usually without modifying the built environment. Several studies were conducted using similar principles of an enriched environment with mixed results on the effect of this intervention on patients’ activity levels (Janssen et al., Citation2014b, Citation2021; Rosbergen et al., Citation2017). The authors of the latest study identified its negligible effect on activity levels. They concluded that the re-design of the built environment might be necessary to support and promote patients’ activities, in addition to environmental enrichment (Janssen et al., Citation2021). Based on the available research that highlights the inactivity of stroke patients and the activity-hindering built environment, it is necessary to examine the built environment's various aspects to better understand how they impact patients’ activity and mobility.
Distance and wayfinding
Stroke patients and medical staff identified wayfinding as the most common mobility barrier in the built environment of rehabilitation clinics, followed by insufficient width of corridors and long distances (Kevdzija & Marquardt, Citation2018). Wayfinding can be a challenging topic to investigate since it is dependent on an interplay of various cognitive functions (Van Asselen et al., Citation2005) and the overall influence of post-stroke impairments on wayfinding ability is difficult to determine. It is also challenging to conduct rigorous comparative research in existing facilities because of the unique character of each facility and the logistical constraints (Kalantari & Snell, Citation2017; Ulrich et al., Citation2008). This is likely why there is a lack of empirical research on the topic and why recent studies on wayfinding in healthcare facilities rely on virtual reality, which might not be comparable with patients’ real-world experiences (Kalantari et al., Citation2021).
However, while wayfinding as a mobility barrier is complex and challenging to investigate, another related barrier in the built environment that deserves attention is the distance between spaces. Long distances are a common design issue in many healthcare facilities due to large and complex programmes, expansion over time, or adaptation from other functions. Distances between spaces are determined by the spatial configuration of the building, which is difficult to modify after the building is completed, making it a crucial factor to address early in the design process. Because most studies on the relationship between the built environment and stroke patients focus on smaller settings such as stroke units or rehabilitation wards, it's unknown how much distance stroke patients cover daily in rehabilitation clinics.
Research studies examining walking distance in healthcare facilities have been primarily focused on nursing staff in hospitals (Real et al., Citation2017; Seo et al., Citation2011; Welton et al., Citation2006). Most studies that measured patients’ walking distances/activity levels did not use distance as a primary measure. Rather, the research focused on walking ability and activity levels during various rehabilitation and therapeutic measures or activity levels following discharge (Killey & Watt, Citation2006; Mansfield et al., Citation2015; Rand et al., Citation2009). The main findings show that the majority of participants did not meet the recommended physical activity levels (Rand et al., Citation2009), even for patients whose physiotherapists received feedback from their accelerometers (Mansfield et al., Citation2015); and that extra walking enhanced mobility and independence (Killey & Watt, Citation2006). The authors argued that one of the reasons why individuals attending inpatient stroke rehabilitation had limited capacity to increase overall walking time could have been the ‘limited space or suboptimal environmental layout’ (Mansfield et al., Citation2015, p. 853). The adopted methodological approach of using pedometers and step activity monitors lacks insight into how patients interact with the built environment, the mobility barriers they encounter and the strategies they use to overcome them.
Because of the usually long distances between patient rooms and therapy rooms, rehabilitation clinics often employ staff members who bring patients from their rooms to therapies, contributing to their feelings of dependence and loss of control. Long distances could potentially negatively impact patients’ mobility and activity in the form of increased dependence on staff members, exhaustion and decreased activity due to distance acting as a barrier. So far, it is unclear how much distance patients cover during one day in large facilities such as rehabilitation clinics and how the distances between crucial spaces (patient rooms and therapy areas) impact their mobility independence. Therefore, more knowledge is needed about how the building's spatial configuration and resulting distances affect stroke patients’ daily life in rehabilitation clinics.
Objectives
Since much is still unknown about the spatial aspects that might impact stroke patients’ mobility, activities and recovery in rehabilitation clinics, this research study investigates distance as an essential component of the built environment. The aim is to examine the relationship between distance and patients’ independent mobility in rehabilitation clinics: how much distance stroke patients cover each day during inpatient recovery and how these distances impact their mobility independence. The findings intend to inform the actors involved in the process of planning rehabilitation clinics about the impact of distances resulting from different building layouts on stroke patients’ everyday lives during rehabilitation.
Materials and methods
This study used patient shadowing as the primary research method supported with patient and staff questionnaires to examine the impact of distance on stroke patients’ mobility in seven rehabilitation clinics in Germany. The complete research study entitled ‘Mobility of stroke patients in neurological rehabilitation clinics’ was approved by the Ethical Committee at the Technische Universität Dresden (approval number: EK 452102016).
Settings
The study was conducted in seven rehabilitation clinics with different layout organizations. Out of between 50 and 60 contacted rehabilitation clinics (all identified clinics for neurology patients in Germany), 11 responded positively, invited the first author (hereafter: the researcher), and were visited in the preliminary research phase. The initial assessment at each visited clinic consisted of a tour of the facility given by a staff member and an informal interview with the clinic's medical director. During conversations with medical directors, further information was obtained about the operational patterns of neurological clinics, how patients were accommodated in the clinics, and how their rehabilitation was organized.
In the next stage, seven clinics were selected for the study to ensure the inclusion of distinctive and different types of building layouts. This selection was made to assess a variety of spatial configurations and to analyse the travel distances resulting from them. The characteristics of each participating rehabilitation clinic are shown in . They were predominantly neurological rehabilitation clinics with a capacity ranging from 188 to 250 beds. The physical environment accessible to patients consisted of their patient ward, therapy rooms (concentrated in one or various areas of the building depending on the clinic), diagnostic facilities, the main cafeteria and various communal areas (not present in every clinic) such as a living room, a library or a café. These clinics had different strategies for allocating patient wards, therapy rooms and other facilities. Some clinics had a hotel-like configuration with patient wards and main therapy areas separated vertically. Others had patient rooms and therapy rooms combined on the same level. Several clinics had a mix of the two: therapy rooms combined with patient rooms, and others separated vertically.
Table 1. Characteristics of the participating rehabilitation clinics.
Inpatients undergoing rehabilitation in all these clinics were expected to attend meals and therapies independently, meaning that patients had to cover the distances between their patient rooms, various therapy rooms and the cafeteria multiple times per day. Aside from scheduled meals and therapy appointments, patients covered the additional distance to visit communal and other spaces in their free time.
Participant recruitment
The medical staff selected the potential participants in each clinic based on the given inclusion and exclusion criteria, their health status and psychological state (). The study included 70 patients of neurological rehabilitation clinics that: (1) suffered a stroke, (2) were able to move independently in the clinic (with or without the use of wheelchair, walker or other equipment) and (3) gave their consent for the study. Patients diagnosed with dementia, severe communication and cognitive impairments, severe multi-morbidity (somatic, psychiatric or psycho/geriatric), significant mobility impairment before the stroke, and/or orthopaedic, neurological or other condition of consequence for the study were excluded from participation. All patients included in the analysis were over 60 years old due to the availability of participants during the observation weeks, as stroke is commonly a condition of advanced age. Only one patient younger than 60 (aged 31) satisfied the inclusion criteria, accepted to participate, and was shadowed during 12 consecutive hours. The observations revealed that this patient did not encounter any challenges in the built environment and was highly active compared to other patients, most likely due to being much younger and adaptable to changes and barriers. This one patient was excluded from the analysis to ensure that the participating patients shared similar characteristics, namely that they were older, independently mobile stroke patients.
Table 2. Participants’ characteristics.
Patients’ mobility levels
The participating patients were divided into three mobility level categories based on the mobility aid that they were using to move around within the clinics: using a wheelchair (level 1), using a walker (level 2) or independently walking (level 3). Instead of using the Barthel Index for Mobility (from 0 = immobile to 15 = independent, but may use any aid; Mahoney & Barthel, Citation1965) or another assessment scale, the mobility aid was used to sort patients into mobility level categories. This decision was taken since it was observed that the mobility aid had a major impact on how patients moved and interacted with space. The exact number of patients with the same mobility level and health condition in each clinic was impossible to obtain due to the unique nature of stroke, where no two strokes are alike and leave the same impairments. Another reason is the nature of the research design, where the selection had to be made from the consenting patients available in the clinic during the field study's two weeks.
Following the explanation of the research study and the requirements to each potential participant by one of the clinic's staff members, patients received a large-print information sheet to read and a large-print consent form to sign in case they wanted to participate. The patients were able to drop out of the study at any time. All 70 participants gave their written or verbal consent for the study.
Research methods
Patient shadowing was used to gain an insight into the daily life of stroke inpatients in rehabilitation clinics and to examine the impact of distance on their mobility. Shadowing was chosen as a method for observing and recording a single individual's everyday activities (Mcdonald, Citation2005). During patient shadowing, an empathetic observer follows patients across various care experiences while recording information gathered through observations (Shaw et al., Citation2014). The role of an observer is challenging since it requires balancing in-depth insight into patients’ experiences with respect for their privacy (Liberati, Citation2017). To effectively use this method, the researcher must be aware of what is required of them at any given time and be able to improvize to maintain or modify their methodological commitments while being open and flexible (Quinlan, Citation2008). Even so, shadowing enables ethnographic observation of various stages and touchpoints in the care process (Gallan et al., Citation2021). The purpose of shadowing can be threefold depending on the aims of a researcher: to learn themselves, to record behaviour and to investigate roles and perspectives in a detailed, qualitative way (Quinlan, Citation2008).
In this study, the shadowing method was adopted to record patients’ daily covered distances and their interactions with space. The ‘observe only’ approach was employed because of typical post-stroke speech impairments and a language barrier between the researcher and many participating patients. The researcher observed patients, avoided interfering with their activities and did not initiate a discussion with the patient but did answer their questions and requests when possible. Therefore, shadowing was used to objectively observe patients’ activities and remain somewhat invisible (Vásquez et al., Citation2012). However, due to the nature of shadowing (an individual carefully following a subject for an extended period) and due to ethical considerations, the researcher could not remain a completely secret observer. Consequently, the Hawthorne effect (individuals changing their conduct in response to being observed) may have influenced the behaviour of the participants. The study's goals were not disclosed to patients to minimize the Hawthorne effect. Patients were only told that their usual daily paths in the clinic were being observed.
Patients’ paths in the clinics were recorded on the previously prepared and then printed building floor plans with an extra sheet for the activity time log. This allowed for precise mapping of locations and the nature of patients’ paths. One researcher observed patients in all corridors and communal areas. Because the focus was on distances between spaces, it was decided not to follow patients inside the therapy rooms and their patient rooms to protect their privacy. Three complimentary types of notes were taken during the patient shadowing:
paths on the floor plans;
time log of all activities;
notable encounters with the built environment, sometimes accompanied by sketches.
Each patient was observed for 12 h on a typical clinic day, from 07:00 h to 19:00 h. The exact observation times differed somewhat between clinics due to different meal times. The 12-h observation usually began immediately before patients’ breakfast and ended after dinner. Total observation time in all clinics was 840 h.
Shadowing was supplemented with patient and staff questionnaires to gain additional insights into their spatial experiences. The observed patients (n = 60) and medical staff that cared for them (55 nurses and four physicians, n = 59) completed the questionnaires. Not all patients were able to complete the questionnaire due to post-stroke impairments. In the questionnaires, patients were asked about the barriers they experienced in the built environment, while staff members were asked about the barriers they witnessed patients encountering.
Data analysis
Data from floor plans and time log sheets were digitalized after data collection. Autodesk AutoCAD software was used to digitally re-draw all the patient paths on the prepared digital floor plans. The travel distances were calculated using these digitally documented patient paths. A path was defined as the distance a patient covered to get from one to another location (from point A to point B). Due to the patient's confusion and wandering, one of the 70 shadowed patients had to be excluded from the analysis. The total number of measured paths for all 69 included patients was n = 1322. These were their usual daily paths (such as going from their room to therapy or cafeteria) and were not a part of training supervised by a physical therapist or another healthcare professional.
Four different aspects were recorded and analysed:
daily distances covered by patients in clinics,
relationship between distance and encountering mobility barriers/needing help from staff,
comparison of path distances with and without encountered mobility barriers/needing help,
patients’ observed paths and interactions with space.
The mobility barrier categories emerged from shadowing data analysis. Patients encountered barriers in these five key categories:
wayfinding issues (e.g. patient choosing a wrong turn in the corridor, asking other patients/or staff which way to go)
problems with long distances (e.g. stopping to rest on the way, asking the researcher to push their wheelchair)
insufficient dimensions of corridors (e.g. not enough space to pass with a wheelchair, no room to park a wheelchair)
physical obstacles (e.g. not being able to open a heavy door, hitting the equipment on the side of the corridor)
flooring (e.g. difficulty to control a wheelchair on a floor slope, rolling a wheelchair backwards on the carpet flooring)
Each path was categorized according to the patient's level of dependence with the help of time log sheets. One of the three possible codes was used for each path, which signified the levels of dependence and severity of the mobility issue that the patient encountered. A path was categorized as category A if the patient faced no mobility barriers. Type B was defined as a path where the patient faced a mobility barrier but was able to overcome it without help. When a patient encountered a barrier and needed help on a path (verbal or physical, such as pushing a wheelchair), it was classed as type C, the highest level of dependence.
NVivo Pro 11 was used to analyse patient and medical staff open-ended questionnaire responses. Their responses were translated from the German language to English before analysis.
Results
Average daily distances
Since patients need to attend therapies between three and seven times per day, the daily covered distance in the clinics can be substantial, ranging from 912 to 2108 m on average (). Mobile patients are usually expected to cover these distances independently, with no assistance from medical staff. The daily distances in clinics likely vary due to differences in spatial configurations, zonal distribution of functions, such as patient rooms and treatment areas (), and therapy quantity.
Table 3. Average daily distance covered in each clinic per patient.
The clinics with the shortest covered distances had compact layouts with a single central building containing all patient and therapy rooms. The exception is Clinic D, where, despite the compact layout, the covered daily distance was longer. The most likely cause is the complex configuration of the basement level where all therapy rooms are concentrated, which is shared with another clinic. The two types of functional layouts were the most efficient in terms of distance: patient rooms and therapy areas separated vertically (hotel-like configuration), and patient rooms and therapy rooms mixed on the same floor, with the main therapy area separated vertically (mixed hotel-like configuration). Patients in the clinics with more complex functional configurations (mixed configurations) covered considerably longer distances during one day.
Relationship between distance and encountering mobility barriers
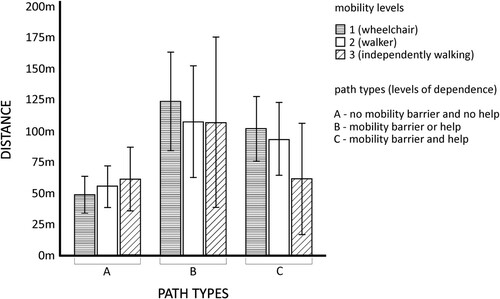
It is common for stroke patients to experience mobility issues related to distance, such as needing to rest often, not having enough strength to reach a specific place, and needing assistance to get around. Patients (n = 69) encountered distance-related issues on 57 of 1322 paths (4.3%). The paths where patients encountered a distance issue were significantly longer than those on which they did not experience any mobility barriers or needed help ().
Table 4. Lengths of paths with and without distance issues and/or needing help.
The paths with observed distance issues belonged to only seven out of 69 patients, five were wheelchair users, and two were using a walker. Hence, the sample size was insufficient to compare the path lengths with encountered distance issues between the three mobility levels.
There was a significant effect of distance on the number of all categories of previously defined mobility barriers (wayfinding, distance, dimensions, physical obstacles, flooring) that patients encountered in the built environment (Wilks’ Λ = 0.379, F(2,15) = 12.271, p = 0.01). When all mobility barrier categories were observed in this sample, the longer distance was related to more barriers encountered and more help from medical staff needed (). A total of 45 patients (65.2%) and their paths were included in the analysis with the General Linear Model (general multivariate regression model). Other 24 patients (34.8%) did not encounter any mobility barriers and did not need help on any of their paths during the observations.
Relationship between mobility levels and encountering mobility barriers
There was no statistically significant effect of mobility level on encountering mobility barriers and needing help on longer distances in this sample (Wilks’ Λ = 0.723, F (4.30) = 1.319, p = 0.286). Increased distance increased the number of encountered mobility barriers in the built environment for all patients, with no significant difference between mobility levels (). Longer distances increased the likelihood that a patient would encounter a mobility barrier or require help from staff to reach a specific location, independent of the patients’ mobility level.
Comparison of paths with and without mobility barriers
The path lengths of patients with varying levels of mobility were compared to examine whether there were any considerable differences. There were 163 paths out of 1322 in total (12.3%) where patients encountered one of the five identified mobility barriers and/or needed help. Patients experienced distance-related issues on 57 of the 163 paths and the other four categories of mobility barriers on the rest. The overall number of paths where patients encountered a barrier and/or needed help varied greatly. Patients using wheelchairs experienced a mobility barrier, needed help, or both twice as often as those using a walker or walking independently ().
Table 5. Comparison of numbers of paths with encountered barriers and/or needed help for each mobility level (n = 163).
The paths where patients did not encounter any mobility barriers and did not need help were significantly shorter than those with barriers and/or needed help for all mobility levels together (). Patients encountered mobility barriers and needed help more often on distances that were around 110 m on average. An average distance of about 60 m was less challenging for patients to cover independently.
Table 6. Lengths of paths with and without encountered mobility barriers and/or needed help (n = 1322).
The intertwined barriers
Even though separating distance as a single aspect of the built environment might be more straightforward for data analysis, many of the spatial features are intertwined and can influence each other and the patient's experience of space. The same is true for spatial distances. Two cases are presented in narrative style, described based on shadowing notes, to illustrate how stroke patients use and interact with space and overcome long distances independently.
In the first example, a patient of Clinic A was returning to his room following physical therapy. His length of stay in the clinic was 35 days on the observation day, and he used a wheelchair for mobility. This patient had hemiplegia on the left side of the body (paralysis of arm and leg), which made using a wheelchair challenging. Additionally, the building of clinic A is specific for its growth in phases. Over time, the building grew into separate ‘houses’, causing certain parts to be disconnected. The patient's physical therapy room was on the building's basement level. The patient had to use the elevator next to this room to arrive at the clinics’ ground floor. Then, he had to travel to another elevator around 55 m away, which took him to the second floor, where his patient ward was located. The patient's path between the therapy room and patient room was 216.4 m long and spread over three building levels.
On the first part of the path, the patient encountered a wayfinding issue upon reaching the ground floor: he chose the wrong corridor upon exiting the elevator. After 26.5 m, the patient realized his error and used backtracking to find the right way. He grew increasingly tired, stopped to rest in the corridor and asked the researcher to push his wheelchair until the elevator (another 25 m). Upon exiting the elevator on the second building floor, he continued independently. After another 22.6 m, he lost control of the wheelchair and hit the seating furniture on the side of the corridor. He regained balance and control of the wheelchair on his own and finally arrived in his room.
The second example is from Clinic B and shows how even shorter distances can be challenging for older stroke patients using a wheelchair. This patient was also returning from therapy to her room. Her length of stay was 24 days on the observation day. She suffered hemiparesis (muscle weakness) on the right side of her body and required a wheelchair for mobility. The patient ward was on the same floor as the therapy rooms, just across a wide corridor.
The distance of 78.03 m was demanding for this patient following physical therapy. She had to stop and rest many times on the way to her room. She also used the handrail on the wall to pull herself forward on several occasions. This patient had to repeat the same path while attending different therapies throughout the day, each time passing through the same therapy corridor and showing a similar mobility pattern.
This case is problematic since it happened in the main therapy corridor, where all 210 patients receive therapy. The high patient traffic and narrow corridor created difficulties for other patients. During this patient's journey through the corridor, other wheelchair users could not pass and reach therapy rooms. Despite the patient's mobility independence, the difficulties in reaching her room hindered the movement of other patients, especially those with limited mobility. The distance and insufficient corridor width created a mobility barrier for this specific patient and other patients attending or finishing therapies at that time.
The presented examples show how various aspects of the built environment may be interconnected and, in combination, present barriers to patients’ mobility. Moreover, patients’ needs vary depending on their mobility ability. No patients who could walk independently were observed to encounter such distance-related issues, whereas those in wheelchairs were the most vulnerable to the built environment's barriers. The interplay of barriers in the built environment is different for each patient, but their mobility needs and abilities can also change on different distances. Two additional examples are discussed to illustrate this phenomenon.
Changing mobility needs
In some situations, it was observed that patients’ reliance on staff members and various forms of mobility aids varied across different distances in clinics and even over the course of a single day.
In one case, a patient of clinic D who was using a wheelchair was brought to all therapies and appointments by staff during the observation day. Still, she could independently visit the communal room on the ward, which was around 38 m away from her room. All therapy areas and diagnostic facilities where she attended appointments were much farther from her room, ranging from 74.4 to 136.75 m. Therefore, while this patient could be independent on short distances, she needed assistance to visit places farther away from her room.
Another patient in clinic B was using a walker as a mobility aid during the whole day and could reach all spaces independently, but he switched to using a wheelchair at the end of the day. This patient stated that he was exhausted after a long day of therapies and that using a wheelchair allowed him to rest more while using less energy for mobility.
These examples provide a glimpse into the daily life of stroke inpatients and their usual practices when going to and back from therapies. Many patients experience difficulties on long distances, such as not being able to find their way, needing to rest and relying on staff assistance. In addition to patient shadowing, both patients and medical staff shared their experiences of barriers in the built environment.
Questionnaire responses
Difficult wayfinding, long distances and inadequate visual communication (signage) were the most often mentioned barriers in the built environment by patients and medical staff. Their open-ended answers regarding these aspects are presented in . They describe a chaotic, difficult-to-navigate environment with the same appearance everywhere and long distances that are challenging for patients to cover without resting on the way. As a result of the barriers mentioned, the described built environment does not seem conducive to patients’ mobility and independence. This is shown in one of the staff members’ responses where they specifically mention personnel that brings patients to therapies. Many rehabilitation clinics adopt this approach since the built environment is not suitable for patients to find their way easily and independently. Some patients and staff suggest using colour and signage to improve wayfinding in their clinics, but minor design interventions cannot change the already existing long distances between spaces. Therefore, distance is recognized by staff and patients as a significant challenge in rehabilitation clinics. The responses offered are congruent with the findings gathered via patient shadowing.
Table 7. Questionnaire responses.
Discussion
The results of this research study demonstrate that the distance between spaces within a rehabilitation clinic has a broad range of effects on the daily mobility of patients. There were six key findings: (1) the built environment of rehabilitation clinics was described by patients and staff as difficult for orientation, with long distances and insufficient signage, (2) patients covered the shortest distances in clinics with compact hotel-like and mixed hotel-like spatial configurations, (3) patients were more dependent on staff members and encountered more mobility barriers on longer distances, regardless of their mobility level, (4) average path without any encountered mobility barriers and help needed was 60 m long (Mdn = 47.2 m), (5) long distances were intertwined with other mobility barriers in the built environment, and (6) patients’ mobility needs were changing on different distances and at different times of the day.
The impact of the built environment and distance on stroke patients’ mobility is still a topic that not much is known about, as this research field is young and developing (Lipson-Smith et al., Citation2021). This investigation aimed to contribute to this wide knowledge gap and provide insights into stroke patients’ daily experiences with distances in rehabilitation clinics. Unlike studies that use accelerometers to track patients’ mobility (Mansfield et al., Citation2015; Rand et al., Citation2009) or behavioural mapping to record their activity levels (Anåker et al., Citation2017; Janssen et al., Citation2014a; Kārkliņa et al., Citation2021), this study observed single individuals for a full day (12 h) to record their travel distances and interactions with the built environment. The adopted method allowed for observation and recording of patients’ usual daily routines in large multistorey buildings. It provided quantitative data on covered distances and qualitative descriptive data of patients’ movements through space and strategies to overcome long distances. Most importantly, it offered insights into the changing mobility needs of stroke patients depending on their mobility level, the distance between spaces and even the time of the day.
The results suggest that barriers in the built environment are frequently intertwined, can influence each other, and can be difficult to separate when analysing how the built environment affects patient mobility. Even though it is a complex topic to investigate, further research focusing on distance is needed since it can impact patients’ mobility independence and could potentially be a contributing factor to their low activity levels.
Patients’ independence and walking ability have been found to improve with increased walking activity in addition to regular therapies (Killey & Watt, Citation2006). Medical staff members also reported independent mobility as exceptionally important during patients’ recovery process (Kevdzija & Marquardt, Citation2018). Thus, rehabilitation does not only encompass standard scheduled therapies. Patients’ independent travels to therapies and their free time activities can also be an effective exercise and could contribute to their recovery (Cowdell & Garrett, Citation2003; Dixon et al., Citation2007). If independence is not achieved at the end of the rehabilitation, the extensive burden falls on caregivers to care for the patient after a stroke (Rigby et al., Citation2009). In the event of high dependence and the absence of a caregiver, the patient needs to be transferred to a long-term care facility (Ween et al., Citation1996). For this reason, independent mobility should be encouraged and promoted to decrease the dependence on others and feelings of loss of control. Furthermore, it is an additional exercise complementing regular therapies. Because of their importance, patient mobility, activity and independence are becoming the focus of numerous studies in healthcare design research.
Implications for practice
New concepts that are entirely rethinking the organization of care and the built environment of healthcare facilities are being developed based on the available research results. One example is the ‘reactivating hospital’, which focuses on activating and strengthening patients via a changed daily rhythm and a unique approach to the built environment (Feenstra, Citation2021). Furthermore, recommendations for specifically designed environments for different rehabilitation phases in stroke recovery are suggested to enable patients’ autonomy and mobility exercise (Kevdzija & Marquardt, Citation2018).
Together with implementing the enriched environment (Janssen et al., Citation2014b, Citation2021; Rosbergen et al., Citation2017), these emerging concepts for creating opportunities for patients to be more independent and active will require a response in the built environment's design. Because of this, many aspects of the built environment should be thoroughly considered for impact on patient mobility and activity. Distance between crucial functional zones in a rehabilitation clinic is one of the aspects that should be intentionally planned for enabling and supporting patients’ independent mobility. Distance is critical since it results from early decisions in the planning process and cannot be significantly altered once the building is completed. Furthermore, patient populations and their mobility abilities need to be considered when designing patient wards and their connections to other clinic areas. For patients using a wheelchair and experiencing severe motor impairments, shorter distances might offer an opportunity for autonomy during daily life in the clinic. At the same time, patients in advanced stages of rehabilitation who can already walk independently could benefit from long distances as a form of exercise.
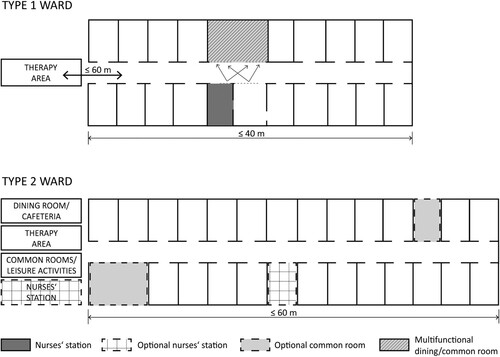
Consequently, rehabilitation clinics’ currently prevalent ‘same for all’ design should be replaced with a more targeted approach of creating the best possible environments for different patient groups and their spatial needs during recovery. The three areas in a rehabilitation clinic whose connections should be carefully planned in terms of distance are patient rooms, therapy/diagnostic areas and dining spaces. These connections are crucial since patients have to attend therapies and meals several times per day. The need for staff transport service could be reduced if the main therapy area and the dining room were located within 60 m of the wards accommodating patients who use a wheelchair (). This distance may also make it easier for patients to visit any communal and leisure spaces.
The built environment should be designed to offer patients opportunities to participate in recovery-promoting activities in their free time to support their recovery (Lipson-Smith et al., Citation2019). Achieving this requires addressing the distance between spaces, wards and therapy areas, and patient rooms and communal spaces since research suggests that patients visit communal spaces closer to their rooms (Kevdzija & Marquardt, Citation2021). Therefore, research studies attempting to improve patients’ activity levels (e.g. with the use of an enriched environment) also need to consider distance as one of the potential factors that might hinder patients’ activity and mobility, and simultaneously the use of communal spaces. Many design strategies to promote patient activity levels, such as attractive communal areas in rehabilitation clinics (common room, library, gaming room, etc.), may not be sufficient if located far from patient rooms. In this study, the hotel-like configuration was identified as the most efficient in terms of distance. Patients needed to cover considerably longer distances in the clinics with more complex configurations and therapy rooms scattered in different building areas. Although the hotel-like configuration may reduce daily patient travel distance, it is unclear how it impacts wayfinding and patient traffic in clinics.
The findings on how stroke patients experience distances between spaces may also inform design decisions at the patient ward level. Even simple considerations about the ward structure and facilities located inside or outside the ward could greatly impact patients’ mobility. A ward diagram was created to illustrate how these considerations could affect patients’ daily distances, impacting their dependence on staff and potentially even their activity levels (). The identical ward configuration is shown in two variations. The examples illustrate how ward size, locations of communal and dining spaces, and connections to therapy rooms may affect patients’ travel distances. A longer ward with the main dining room, communal spaces, optionally the nurses’ station outside the ward, and a therapy area not closely attached to the ward would result in patients travelling longer daily distances. A compact ward with most functions concentrated within or closely attached to it, on the other hand, would result in shorter distances. Taking into the account different needs of patients with varying levels of mobility, differently designed ward environments could benefit each of these groups individually.
Figure 2. Illustration of ward variations with the placement of functions inside and outside of the wards.
When designing different ward environments, many aspects other than distance need to be considered. They include, among others, the spatial configuration of the ward, the environment and types of the communal areas, and connections between locations where patients with different mobility levels are accommodated for mutual support and motivation. As a result, there is a need to reconsider how rehabilitation clinics are designed and move forward with a more tailored approach to create environments for patients’ different mobility abilities. Further research into the relationship between various aspects of the built environment and stroke patients’ mobility and activity is needed to better understand and accommodate their spatial needs during recovery.
Strengths and limitations
The strength of this study is the use of the shadowing method on a large scale (70 patients, 840 h of observations). This enabled insight into the daily routines, travelled distances and interactions with the built environment of individual stroke patients via direct observation. Although the shadowing method is the main strength of this study, this method choice also introduced certain limitations that need to be mentioned. Since the participating clinics have around 200 patients each, the sample size of 10 patients per clinic could be considered small. Because of the nature of the shadowing method, which is immensely time-consuming (Ferguson, Citation2016), the possible sample size was limited. Due to the exploratory character of this study, the sample of 70 patients was enough to study the phenomenon in question more deeply. Further studies investigating the topic only quantitatively or using mixed methods would benefit from a larger representative sample of stroke patients. Moreover, excluding the younger patient from the analysis removed the representation of young patients’ experiences, whose needs also require special attention. Additionally, the field research and data collection phase for this research study were conducted pre-COVID-19, and the influence of the pandemic on everyday life in rehabilitation clinics could not be have been observed.
Conclusion
The spatial needs of stroke patients and their relationship with the built environment have yet to be sufficiently investigated to determine which design strategies are most beneficial to the patients. The study's findings suggest that decisions made during the early design stages concerning the building's layout and distances between different locations can significantly impact patients’ mobility and independence. Shorter distances were recognized as a feature that, if carefully planned, has the potential to facilitate independent mobility for all patients, even those with limited mobility. This potential influence on patients’ mobility and the impact of other mobility barriers needs to be further examined. Future research could look into how longer distances and the presence of other mobility barriers affect patients’ activity levels, especially in their free time. Another relevant direction to be further explored is patients’ feelings and experiences with various barriers and facilitators in the built environment. Different spatial features and their interplay require special consideration since the physical environment of rehabilitation clinics shows potential for supporting the mobility and activity of stroke patients.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Adamson, J., Beswick, A., & Ebrahim, S. (2004). Is stroke the most common cause of disability? Journal of Stroke and Cerebrovascular Diseases, 13(4), 171–177. https://doi.org/https://doi.org/10.1016/j.jstrokecerebrovasdis.2004.06.003
- Alfonsi, E., Capolongo, S., & Buffoli, M. (2014). Evidence Based design and healthcare: An unconventional approach to hospital design. Annali Di Igiene : Medicina Preventiva e Di Comunità, 26(2), 137–143. https://doi.org/https://doi.org/10.7416/ai.2014.1968
- Anåker, A., von Koch, L., Heylighen, A., & Elf, M. (2019). “It's lonely”: Patients’ experiences of the physical environment at a newly built stroke unit. HERD: Health Environments Research and Design Journal, 12(3), 141–152. https://doi.org/https://doi.org/10.1177/1937586718806696
- Anåker, A., Von Koch, L., Sjöstrand, C., Bernhardt, J., & Elf, M. (2017). A comparative study of patients’ activities and interactions in a stroke unit before and after reconstruction—The significance of the built environment. PLoS ONE, 12(7), 1–12. https://doi.org/https://doi.org/10.1371/journal.pone.0177477
- Anåker, A., Von Koch, L., Sjöstrand, C., Heylighen, A., & Elf, M. (2018). The physical environment and patients’ activities and care. A comparative case study at three newly built stroke units. Journal of Advanced Nursing, 74(8), 1919–1931. https://doi.org/https://doi.org/10.1111/jan.13690
- Billinger, S. A., Arena, R., Bernhardt, J., Eng, J. J., Franklin, B. A., Johnson, C. M., Mackay-Lyons, M., Macko, R. F., Mead, G. E., Roth, E. J., Shaughnessy, M., & Tang, A. (2014). Physical activity and exercise recommendations for stroke survivors: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(8), 2532–2553. https://doi.org/https://doi.org/10.1161/STR.0000000000000022
- Brambilla, A., Rebecchi, A., & Capolongo, S. (2019). Evidence based hospital design. A literature review of the recent publications about the EBD impact of built environment on hospital occupants’ and organisational outcomes. Annali Di Igiene, 31(2), 165–180. https://doi.org/https://doi.org/10.7416/ai.2019.2269
- Bussmann, M., Neunzig, H., Gerber, J., Steinmetz, J., Jung, S., & Deck, R. (2018). Effects and quality of stroke rehabilitation of BAR phase D. Neurology International Open, 02(01), E16–E24. https://doi.org/https://doi.org/10.1055/s-0043-122193
- Claessen, M., Visser-Meily, J., Meilinger, T., Postma, A., de Rooij, N. K., & van der Ham, I. (2017). A systematic investigation of navigation impairment in chronic stroke patients: Evidence for three distinct types. Neuropsychologia, 103, 154–161. https://doi.org/https://doi.org/10.1016/j.neuropsychologia.2017.07.001
- Cowdell, F., & Garrett, D. (2003). Recreation in stroke – rehabilitation part two: Exploring patients’ views. International Journal of Therapy and Rehabilitation, 10(10), 456–462.
- Dixon, G., Thornton, E. W., & Young, C. A. (2007). Perceptions of self-efficacy and rehabilitation among neurologically disabled adults. Clinical Rehabilitation, 21(3), 230–240. https://doi.org/https://doi.org/10.1177/0269215506071784
- Duncan, F., Lewis, S. J., Greig, C. A., Dennis, M. S., Sharpe, M., MacLullich, A. M. J., & Mead, G. E. (2015). Exploratory longitudinal cohort study of associations of fatigue after stroke. Stroke, 46(4), 1052–1058. https://doi.org/https://doi.org/10.1161/STROKEAHA.114.008079
- Feenstra, F. (2021). Reactivating hospital, active patients through special design. HERD: Health Environments Research & Design Journal, 14(1), 87–105. https://doi.org/https://doi.org/10.1177/1937586720966757
- Ferguson, K. (2016). Lessons learned from using shadowing as a qualitative research technique in education. Reflective Practice, 17(1), 15–26. https://doi.org/https://doi.org/10.1080/14623943.2015.1123683
- Gaete Moncayo, J., & Bogousslavsky, J. (2008). Post-stroke depression. Expert Review of Neurotherapeutics, 8(1), 75–92. https://doi.org/https://doi.org/10.1586/14737175.8.1.75
- Gallan, A. S., Perlow, B., Shah, R., & Gravdal, J. (2021). The impact of patient shadowing on service design: Insights from a family medicine clinic. Patient Experience Journal, 8(1), 88–98. https://doi.org/https://doi.org/10.35680/2372-0247.1449
- Hempler, I., Woitha, K., Thielhorn, U., & Farin, E. (2018). Post-stroke care after medical rehabilitation in Germany: A systematic literature review of the current provision of stroke patients. BMC Health Services Research, 18(1), 1–9. https://doi.org/https://doi.org/10.1186/s12913-018-3235-2
- Janssen, H., Ada, L., Bernhardt, J., McElduff, P., Pollack, M., Nilsson, M., & Spratt, N. (2014a). Physical, cognitive and social activity levels of stroke patients undergoing rehabilitation within a mixed rehabilitation unit. Clinical Rehabilitation, 28(1), 91–101. https://doi.org/https://doi.org/10.1177/0269215512466252
- Janssen, H., Ada, L., Bernhardt, J., McElduff, P., Pollack, M., Nilsson, M., & Spratt, N. J. (2014b). An enriched environment increases activity in stroke patients undergoing rehabilitation in a mixed rehabilitation unit: A pilot non-randomised controlled trial. Disability and Rehabilitation, 36(3), 255–262. https://doi.org/https://doi.org/10.3109/09638288.2013.788218
- Janssen, H., Ada, L., Middleton, S., Pollack, M., Nilsson, M., Churilov, L., Blennerhassett, J., Faux, S., & New, P. (2021). Altering the rehabilitation environment to improve stroke survivor activity : A phase II trial. International Journal of Stroke, 0(0), 1–9. https://doi.org/https://doi.org/10.1177/17474930211006999
- Kalantari, S., & Snell, R. (2017). Post-occupancy evaluation of a mental healthcare facility based on staff perceptions of design innovations. HERD: Health Environments Research & Design Journal, 10(4), 121–135. https://doi.org/https://doi.org/10.1177/1937586716687714
- Kalantari, S., Tripathi, V., Rounds, J. D., Mostafavi, A., Snell, R., & Cruz-Garza, J. G. (2021). Evaluating wayfinding designs in healthcare settings through EEG data and virtual response testing. bioRxiv. https://doi.org/https://doi.org/10.1101/2021.02.10.430638
- Kārkliņa, A., Chen, E., Bērziņa, G., & Stibrant Sunnerhagen, K. (2021). Patients’ physical activity in stroke units in Latvia and Sweden. Brain and Behavior, 11(5), 1–8. https://doi.org/https://doi.org/10.1002/brb3.2110
- Kevdzija, M., & Marquardt, G. (2018). Physical Barriers to mobility of stroke patients in rehabilitation clinics. In: P. Langdon, J. Lazar, A. Heylighen, & H. Dong (Eds.), Breaking down barriers CWUAAT 2018 (pp. 147–157). Springer.
- Kevdzija, M., & Marquardt, G. (2018). Physical barriers to mobility of stroke patients in rehabilitation clinics. Breaking Down Barriers, 147–157. https://doi.org/https://doi.org/10.1007/978-3-319-75028-6_13
- Kevdzija, M., & Marquardt, G. (2021). Stroke patients’ nonscheduled activity during inpatient rehabilitation and its relationship with the architectural layout : A multicenter shadowing study. Topics in Stroke Rehabilitation, 00(00), 1–7. https://doi.org/https://doi.org/10.1080/10749357.2020.1871281
- Killey, B., & Watt, E. (2006). The effect of extra walking on the mobility, independence and exercise self-efficacy of elderly hospital in-patients: A pilot study. Contemporary Nurse : A Journal for the Australian Nursing Profession, 22(1), 120–133. https://doi.org/https://doi.org/10.5172/conu.2006.22.1.120
- Langhorne, P., Coupar, F., & Pollock, A. (2009). Motor recovery after stroke: A systematic review. The Lancet Neurology, 8(8), 741–754. https://doi.org/https://doi.org/10.1016/S1474-4422(09)70150-4
- Liberati, E. G. (2017). What is the potential of patient shadowing as a patient-centred method? BMJ Quality & Safety, 26(4), 343–346. https://doi.org/https://doi.org/10.1136/bmjqs-2016-005308
- Lipson-Smith, R., Churilov, L., Newton, C., Education, D., Zeeman, H., Hons, B., Neuro, M., Bernhardt, J., & Physio, B. (2019). A framework for designing inpatient stroke rehabilitation facilities : A New approach using interdisciplinary value-focused thinking. HERD: Health Environments Research & Design Journal, 12(4), 142–158. https://doi.org/https://doi.org/10.1177/1937586719831450
- Lipson-Smith, R., Pflaumer, L., Elf, M., Blaschke, S.-M., Davis, A., White, M., Zeeman, H., & Bernhardt, J. (2021). Built environments for inpatient stroke rehabilitation services and care : a systematic literature review. BMJ Open, 11(8), 1–11. https://doi.org/https://doi.org/10.1136/bmjopen-2021-050247
- Lipson-Smith, R., Zeeman, H., & Bernhardt, J. (2020). What's in a building? A descriptive survey of adult inpatient rehabilitation facility buildings in Victoria, Australia. Archives of Rehabilitation Research and Clinical Translation, 2(1), 100040. https://doi.org/https://doi.org/10.1016/j.arrct.2020.100040
- Luker, J., Lynch, E., Bernhardsson, S., Bennett, L., & Bernhardt, J. (2015). Stroke survivors’ experiences of physical rehabilitation: A systematic review of qualitative studies. Archives of Physical Medicine and Rehabilitation, 96(9), 1698–1708.e10. https://doi.org/https://doi.org/10.1016/j.apmr.2015.03.017
- MacIntosh, B. J., Edwards, J. D., Kang, M., Cogo-Moreira, H., Chen, J. L., Mochizuki, G., Herrmann, N., & Swardfager, W. (2017). Post-stroke fatigue and depressive symptoms are differentially related to mobility and cognitive performance. Frontiers in Aging Neuroscience, 9(OCT), 1–7. https://doi.org/https://doi.org/10.3389/fnagi.2017.00343
- Mahoney, F. I., & Barthel, D. W. (1965). Functional evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Maryland State Medical Journal, 14, 61–65.
- Mansfield, A., Wong, J. S., Bryce, J., Brunton, K., Inness, E. L., Knorr, S., Jones, S., Taati, B., & McIlroy, W. E. (2015). Use of accelerometer-based feedback of walking activity for appraising progress with walking-related goals in inpatient stroke rehabilitation: A randomised controlled trial. Neurorehabilitation and Neural Repair, 29(9), 847–857. https://doi.org/https://doi.org/10.1177/1545968314567968
- Mcdonald, S. (2005). Studying actions in context: A qualitative shadowing method for organisational research. Qualitative Research, 5(4), 455–473. https://doi.org/https://doi.org/10.1177/1468794105056923
- Newall, J. T., Wood, V. A., Hewer, R. L., & Tinson, D. J. (1997). Development of a neurological rehabilitation environment: An observational study. Clinical Rehabilitation, 11(2), 146–155. https://doi.org/https://doi.org/10.1177/026921559701100208
- Nikolaus, G., Zwingmann, C., & Jäckel, W. H. (2006). The system of rehabilitation in Germany. In J. Bengel, W. H. Jäckel, & J. Herdt (Eds.), Research in rehabilitation. Results from a research network in Southwest Germany (pp. 3–19). Schattauer.
- Pohjasvaara, T., Leppavuori, A., Siira, I., Vataja, R., Kaste, M., & Erkinjuntti, T. (1998). Frequency and clinical determinants of poststroke depression. Stroke, 29(11), 2311–2317. https://doi.org/https://doi.org/10.1161/01.STR.29.11.2311
- Pohjasvaara, T., Vataja, R., Leppävuori, A., Kaste, M., & Erkinjuntti, T. (2001). Depression is an independent predictor of poor long-term functional outcome post-stroke. European Journal of Neurology, 8(4), 315–319. https://doi.org/https://doi.org/10.1046/j.1468-1331.2001.00182.x
- Quinlan, E. (2008). Conspicuous invisibility: Shadowing as a data collection strategy. Qualitative Inquiry, 14(8), 1480–1499. https://doi.org/https://doi.org/10.1177/1077800408318318
- Rand, D., Eng, J. J., Tang, P. F., Jeng, J. S., & Hung, C. (2009). How active are people with stroke?: Use of accelerometers to assess physical activity. Stroke; a Journal of Cerebral Circulation, 40(1), 163–168. https://doi.org/https://doi.org/10.1161/STROKEAHA.108.523621
- Real, K., Bardach, S. H., & Bardach, D. R. (2017). The role of the built environment: How decentralised nurse stations shape communication, patient care processes, and patient outcomes. Health Communication, 32(12), 1557–1570. https://doi.org/https://doi.org/10.1080/10410236.2016.1239302
- Rigby, H., Gubitz, G., & Phillips, S. (2009). A systematic review of caregiver burden following stroke. International Journal of Stroke, 4(4), 285–292. https://doi.org/https://doi.org/10.1111/j.1747-4949.2009.00289.x
- Rosbergen, I. C., Grimley, R. S., Hayward, K. S., Walker, K. C., Rowley, D., Campbell, A. M., McGufficke, S., Robertson, S. T., Trinder, J., Janssen, H., & Brauer, S. G. (2017). Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: A controlled before–after pilot study. Clinical Rehabilitation, 31(11), 1516–1528. https://doi.org/https://doi.org/10.1177/0269215517705181
- Seo, H. B., Choi, Y. S., & Zimring, C. (2011). Impact of hospital unit design for patient-centered care on nurses’ behavior. Environment and Behavior, 43(4), 443–468. https://doi.org/https://doi.org/10.1177/0013916510362635
- Shannon, M. M., Elf, M., Churilov, L., Olver, J., Pert, A., Shannon, M. M., Elf, M., Churilov, L., Olver, J., & Pert, A. (2018). Can the physical environment itself influence neurological patient activity ? Disability and Rehabilitation, 41(10), 1177–1189. https://doi.org/https://doi.org/10.1080/09638288.2017.1423520
- Shaw, J., Pemberton, S., Pratt, C., & Salter, L. (2014). Shadowing: A central component of patient and family-centred care. Nursing Management, 21(3), 20–23. https://doi.org/https://doi.org/10.7748/nm.21.3.20.s24
- Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H.-B., Choi, Y.-S., Quan, X., & Joseph, A. (2008). A review of the research literature on evidence-based healthcare design. Healthcare Leadership White Paper Series #5. Health Environments Research & Design Journal, 1(Part I), 101–165. https://doi.org/https://doi.org/10.1177/193758670800100306
- Van Asselen, M., Kessels, R. P. C., Kappelle, L. J., Neggers, S. F. W., Frijns, C. J. M., & Postma, A. (2005). Neural correlates of human wayfinding in stroke patients. Brain Research, 1067(1), 229–238. https://doi.org/https://doi.org/10.1016/j.brainres.2005.10.048
- Van De Port, I. G. L., Kwakkel, G., Schepers, V. P. M., & Lindeman, E. (2006). Predicting mobility outcome one year after stroke: A prospective cohort study. Journal of Rehabilitation Medicine, 38(4), 218–223. https://doi.org/https://doi.org/10.1080/16501970600582930
- Vásquez, C., Brummans, B. H. J. M., & Groleau, C. (2012). Notes from the field on organisational shadowing as framing. Qualitative Research in Organisations and Management: An International Journal, 7(2), 144–165. https://doi.org/https://doi.org/10.1108/17465641211253075
- Ween, J. E., Alexander, M. P., D’Esposito, M., & Roberts, M. (1996). Factors predictive of stroke outcome in a rehabilitation setting. Neurology, 47(May 1994), 388–392. https://doi.org/https://doi.org/10.1212/WNL.47.2.388
- Welton, J. M., Decker, M., Adam, J., & Zone-Smith, L. (2006). How far do nurses walk? Medsurg Nursing : Official Journal of the Academy of Medical-Surgical Nurses, 15(4), 213–216.
- West, T., & Bernhardt, J. (2012, October). Physical activity in hospitalised stroke patients. Stroke Research and Treatment. 2012, 1–13. Article ID 813765. https://doi.org/https://doi.org/10.1155/2012/813765