Abstract
High sodium intake increases cardiovascular risk by increasing blood pressure. The intake of coffee elevates blood pressure acutely. Preclinical evidence shows that this action of caffeine is enhanced by high salt intake. We hypothesised that high sodium intake augments the acute blood pressure response to coffee in humans. A randomised cross-over study (n = 15) was performed comparing the effect of lower (6 g/d; LS) with higher (12 g/d; HS) sodium chloride diet on blood pressure before and 2 h after regular coffee intake. Baseline blood pressure was 115 ± 4/84 ± 2/68 ± 1 during LS and 121 ± 4/89 ± 2/69 ± 1 mmHg during HS (SBP/Mean Arterial Pressure (MAP)/DBP; mean ± SE, p < 0.05 for SBP). During LS, blood pressure increased to 121 ± 4/91 ± 2/73 ± 1 (p < 0.05 for SBP, MAP, DBP versus baseline). HS did not significantly affect the impact of coffee on blood pressure (p > 0.3 for SBP, DBP; p > 0.05 for MAP). Sodium intake does not relevantly modulate the impact of regular coffee consumption on blood pressure.
Introduction
Lifestyle has an important impact on cardiovascular health. Smoking, inactivity and high caloric diet are well-accepted risk factors for cardiovascular disease. In addition, in population-based cohorts daily sodium intake is associated with cardiovascular risk (O'Donnell et al. Citation2014). Sodium intake is positively correlated with blood pressure, an established determinant of cardiovascular risk (He et al. Citation1998, Citation2013; Intersalt Cooperative Research Group Citation1988; Sacks et al. Citation2001; Obarzanek et al. Citation2003; Mente et al. Citation2014). Reduction in sodium intake has been associated with reduced cardiovascular events (Cook et al. Citation2007; Strazzullo et al. Citation2009; Aburto et al. Citation2013). Thus, it seems likely that blood pressure, at least in part, mediates the association between sodium take and cardiovascular events. The World Health Organisation advices a daily intake of 2 g of sodium (87 mmol Na+) per day. Globally, the actual salt intake is much higher and may be responsible for 1.65 million deaths from cardiovascular causes annually (Mozaffarian et al. Citation2014).
After at least 24 h of caffeine abstinence, caffeine-containing beverages acutely raise blood pressure. This effect is mediated, at least in part, by antagonism of the vasodilator actions of endogenous adenosine (Smits et al. Citation1987; van Dusseldorp et al. Citation1989). In contrast to salt intake, the relation between the use of caffeine-containing beverages and cardiovascular events is much more controversial. While most retrospective observational studies report a positive association between patient-reported coffee use and cardiovascular events, prospective studies do not confirm this relationship (Riksen et al. Citation2009; Guessous et al. Citation2014). Several reasons for this ambiguity have been suggested. Prospective studies may underestimate the potential impact of the transient and acute effects of coffee intake as triggers of a cardiovascular event, such as adrenal release of epinephrine, increase in blood pressure and increased susceptibility from ischaemia and reperfusion (Riksen et al. Citation2009, Citation2011). Furthermore, population-based observational studies have largely neglected potential interactions between lifestyle factors such as salt and coffee intake.
Preclinical evidence in animals has indicated that high sodium intake augments the vasodilator actions of adenosine (Liclican et al. Citation2005; Dobrowolski et al. Citation2007; Nayeem et al. Citation2010, Citation2011). In addition, some older evidence suggests that high sodium intake increases endogenous extracellular adenosine formation (Siragy and Linden Citation1996). Further, inhibition of the adenosine A2A receptor has been shown to cause hypertension (Poucher et al. Citation1995; Liclican et al. Citation2009; Carroll Citation2012).
Thus, the pressor effect of high salt intake may be counteracted by increased adenosine formation and subsequent adenosine receptor-mediated vasodilation. Since caffeine antagonises the vasodilator action of adenosine, we hypothesised that the acute pressor effect of caffeinated coffee is potentiated by high salt intake. According to this hypothesis, the impact of coffee consumption on cardiovascular risk should be higher in those who use more salt in their diet. If true, this interaction between salt and coffee intake on blood pressure should be taken into account in population-based observational studies on the relation between coffee intake and cardiovascular disease. Because of this potential high societal impact, we decided to explore the modulating effect of salt intake on the coffee-induced rise in blood pressure in humans.
Materials and methods
Study population
This study was approved by the institutional ethics review board (CMO Arnhem-Nijmegen; registration number 2012/113) and was performed according to the declaration of Helsinki.
Fifteen healthy volunteers (eight females) were recruited at the university campus. After informed consent, all participants were screened for in- and exclusion criteria. Inclusion criteria were: unremarkable medical history, ≥18 years of age and signed informed consent. Exclusion criteria were: current medication or recreational drug use (except use of oral contraceptives), a body mass index >25 kg/m2, hypertension (defined as systolic blood pressure >140 mmHg and/or diastolic blood pressure >90 mmHg), a difference in systolic blood pressure of ≥10 mmHg between two arms, intake of >2 alcohol consumptions per day, cardiovascular abnormalities detected by routine history and physical examination.
Study design
This study was performed in a university hospital (Radboudumc) and designed as a cross-over study. In all participating volunteers, a three-day food diary was obtained. Each food diary contained one weekend day. Based on this diary, a dietician (RL) extracted two unique individual diets per participant: a diet relatively lower (6 g/24 h) and higher (12 g/24 h) in sodium chloride. We chose for a 6 g/24 h diet because compliance to the diet was extremely important and we presumed that a lower <5 g/24 h sodium chloride diet (as is advised by the World Health Organisation (WHO)) would be difficult to follow in daily practice for most participants. Subsequently, all volunteers were randomly assigned to “group A” or “group B”. Group A started on a lower sodium chloride diet for five consecutive days followed by a test day and a wash-out period of at least 4 days, during which the volunteer used his or her regular diet. Thereafter, a higher sodium chloride diet was taken for 5 days, finished by a test day. Group B followed the protocol in reversed order (higher salt intake first). During the final 24 h of each period of regulated sodium intake the participants abstained from nicotine, alcohol and caffeine containing products, to exclude these as possible confounders. The last 2 h before the experiment on the test day they abstained from all food and drinks, except water. Physical activity was not recorded, but we asked participants to stick to their normal lifestyle during the entire study. Two procedures were performed to verify compliance to the diet. At the end of each period of regulated sodium intake, all participants collected a 24 h urine sample, which was analysed for volume, sodium and creatinine excretion to check for compliance to sodium intake. Furthermore, at arrival on each test day venous blood was sampled to determine the baseline plasma caffeine concentration to check appropriate caffeine abstinence.
After emptying the bladder, the baseline blood pressure was recorded in sitting position on the non-dominant arm at 5 min intervals for 15 min with an oscillometric automatic blood pressure device (Dinamap, 1846 SX; Critikon, Portanje Electronica BV, Utrecht, The Netherlands). Subsequently 350 ml of regular black coffee was taken orally within 15 min. After this, blood pressure recording was resumed at 5-min intervals for another 2 h. Two hours after coffee ingestion, another 5 ml venous blood sample was obtained to measure the plasma caffeine concentration.
Coffee preparation
Before each coffee administration, coffee was freshly prepared according to a standardised procedure using the same coffee brewer; 350 ml water was dripped on 24 g of ground coffee (Douwe Egberts Gold, Douwe Egberts, Utrecht, The Netherlands). This is a mixture of beans of the plants Coffea Arabica and Coffea Robusta.
Analytical procedures
Determination of the plasma caffeine concentration was done by using a reversed-phase high-performance liquid chromatography (HPLC) method with UV-detection set at 273 mm according to Schreiber-Deturmeny and Brugerolle (Citation1996). Urinary sodium was measured using an ion-selective electrode (ISE) method and creatinine was measured using an enzymatic colorimetric method. Both measurements were performed using an automized platform (Architect C16000, Abbott Diagnostics Nederland BV, Hoofddorp, the Netherlands).
Sample size calculation
Based on a previous study (Smits et al. Citation1983, Citation1985a) we anticipated that the intake of two cups of caffeine containing coffee prepared as in this study increased systolic blood pressure by 5 ± 5 (SD), mean arterial pressure by 9 ± 5 and diastolic blood pressure by 11 ± 7 mmHg. We assumed a between-test correlation in blood pressure response of 0.8. Based on these assumptions we calculated a group size of 10 volunteers to allow the detection of a 4 mmHg difference in blood pressure response to coffee between lower and higher salt intake conditions for systolic and mean arterial blood pressure and 15 volunteers for diastolic blood pressure (power 0.9; two-sided alpha of 0.05).
Statistical analysis
Blood pressure and heart rate measurements during the last 10 min before coffee intake were averaged and taken as baseline. After ingestion of coffee, blood pressure recordings were averaged for each subsequent 30 min. Results are given as mean ± SE unless indicated otherwise. The effect of salt, coffee and the interaction between salt and coffee intake on blood pressure (primary endpoint) was analysed using a repeated measures ANOVA with sodium intake and time after coffee intake as within subject factors. Baseline sodium excretion and plasma caffeine concentrations were compared between the two study days using paired t-tests. Two-sided p values <0.05 were considered to indicate statistical significance.
Results
Compliance to protocol
Two of the 15 participants were excluded for further analysis: one because of presumed violation of the diet instructions (on both days the same amount of urinary sodium) and one subject was withdrawn from the study due to an intercurrent illness with fever. Another participant originally allocated to group B, appeared to have switched the high and low salt diets as concluded from his urinary sodium excretion. He was reallocated afterwards to group A according to these urinary sodium results. Finally, group A and B contained 6 and 7 subjects respectively. Baseline characteristics of the remaining 13 volunteers are presented in . Relevant laboratory results for all 13 participants are presented in . In general, caffeine concentration and sodium excretion were in line with what was expected from the intake according to the protocol.
Table 1. Baseline characteristics of volunteers (n = 13).
Table 2. Laboratory values (expressed as mean ± SD).
Blood pressure and heart rate
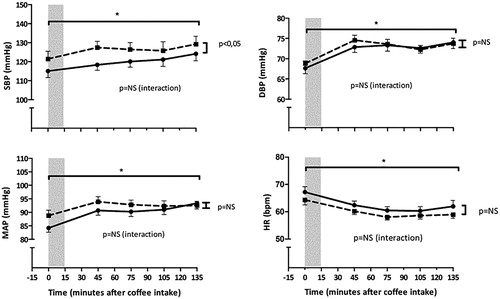
Courses in blood pressure and heart rate did not significantly differ between group A and B (data not shown). Results are presented for both groups combined (). Systolic blood pressure was significantly higher at the end of higher salt intake as compared with lower salt intake (121 ± 4 mmHg vs. 115 ± 4 mmHg; p < 0.05). Diastolic blood pressure, mean arterial pressure and heart rate were not significantly affected by salt intake, although mean arterial pressure tended to be increased (p < 0.1; see ). All three blood pressure parameters significantly increased and heart rate significantly decreased after coffee intake (p < 0.001 for all four parameters). However, salt intake did not significantly modulate the course in heart rate and blood pressure after coffee intake (interaction: p > 0.3 for heart rate, systolic and diastolic blood pressure; p > 0.05 for mean arterial pressure, see ).
Figure 1. Blood pressure and heart rate after low salt (LS) and high salt (HS) diet, at baseline and every 30 min after coffee drinking (grey area). SBP: systolic blood pressure; DBP: diastolic blood pressure; MAP: mean arterial pressure; HR: heart rate; NS: Not Significant. *Significant increase of BP and decrease of HR after coffee intake (p < 0.001).
Discussion
Based on preclinical findings, we hypothesised that salt intake modulates the blood pressure response to acute caffeinated coffee exposure. However, in our study this potential interaction was not confirmed in humans in vivo. This observation does not support our hypothesis that adenosine (A2)-receptor-induced vasodilation mitigates the salt-associated increase in blood pressure as based on previously reported studies in small rodents. Therefore, our results do not support the need to take salt intake into account when investigating the cardiovascular effect of coffee intake in epidemiological studies.
As is known from earlier studies, a higher salt intake increased SBP (Intersalt Cooperative Research Group Citation1988; Sacks et al. Citation2001). The increase by 140 mmol Na+/day from lower to higher salt intake in our study raised systolic blood pressure by approximately 6 mmHg. So even while the lower sodium chloride diet (6 g/24 h) intake was still higher than is advised by the WHO we found a significant difference in SBP between the two dosages of salt. This observation fits well with an observational study in 100.000 patients by Mente et al. in which an increase in sodium excretion from 1.7 g/d to 4.9 g/d (74 to 213 mmol/d) raised systolic blood pressure with 4.3 mmHg (Mente et al. Citation2014). Thus, the observed blood pressure effect of a short term increase in salt intake in our relatively small study population equals the observation in a very large cohort of chronic salt exposure. From this, we conclude that the 5-day duration of regulated sodium intake was sufficient to achieve a hemodynamic steady state. Our study was not designed to quantify the blood pressure response to coffee perse, as we did not include a placebo arm. The average increase in SBP and DBP (4.3% and 8.2%) however, was the same as in a previous study with an appropriate control group, in which SBP and DBP rose 4.4% and 11.4%, respectively, after drinking the same coffee preparation as in our study (350 ml water and 24 g coffee; Smits et al. Citation1985a). As confirmed by the plasma caffeine concentrations, the caffeine intake was highly standardised in our study. Smits et al. also described the potential confounding effect of a genetically determined slow metabolism of caffeine, which is important because an optimal blood pressure increase in response to caffeine will occur only after sufficient caffeine abstinence (Smits et al. Citation1985b). In our study, the potential impact of inter-individual variation in caffeine elimination appears neglectable since on arrival on both the test days caffeine plasma levels were low and equivalent, indicating sufficient caffeine abstinence. Thus, in our study all participants were exposed to a similar amount of coffee and caffeine on both test days and the blood pressure course after coffee intake in the present study fits with previous observations with an appropriate control group. There are some limitations to our experiment. Dietary intake apart from sodium intake during the intervention periods was not assessed. Therefore, we cannot exclude that consumption of other foods or food components (for example high potassium intake) may have interfered with the results. And although smoking and alcohol consumption was explicitly prohibited 24 h before the experiment, we were not able to verify whether abstinence took place. However, only 2 of 13 participants were regular smokers and alcohol consumption varied between volunteers from 0 to 2 beverages a day, so we assume that the possible risk of confounding the outcome is low. And although physical activity level was not objectivated during the intervention and this could have possibly influenced our data, all participants were fit adults (mean age 24 years). Also each participant served as its own control in this cross-over design further limiting the possible impact of variation in fitness.
Therefore, we conclude that the internal validity of our study in terms of salt and coffee exposure as well as external validity in terms of blood pressure response to salt and coffee were excellent. An explanation for our negative results with respect to the interaction between coffee and salt on blood pressure could be that the effect of sodium on adenosine formation and adenosine receptor stimulation that has been observed in murine models does not occur in humans. Another potential explanation is that caffeine is also believed to have a diuretic effect. A recent meta-analysis however revealed that the proposed diuretic action of caffeine is very modest and unlikely to interfere with the blood pressure response to coffee (Zhang et al. Citation2015).
In conclusion, the present study shows that high sodium intake does not relevantly augment the blood pressure response to two cups of coffee.
Disclosure statement
NP Riksen received a non-restricted grant from AstraZeneca and has served on a Scientific Advisory Board of AstraZeneca unrelated to the current subject. Otherwise, no competing interests exist. NP Riksen is supported by a grant from the Netherlands Heart Foundation [2012T051]. The other authors report no conflicts of interest.
References
- Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. 2013. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 346:f1326.
- Carroll MA. 2012. Role of the adenosine(2A) receptor-epoxyeicosatrienoic acid pathway in the development of salt-sensitive hypertension. Prostaglandins Other Lipid Mediat. 98(3–4):39–47.
- Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, Appel LJ, Whelton PK. 2007. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 334(7599):885–888.
- Dobrowolski L, Kompanowska-Jezierska E, Walkowska A, Sadowski J. 2007. Sodium intake determines the role of adenosine A2 receptors in control of renal medullary perfusion in the rat. Nephrol Dial Transplant. 22(10):2805–2809.
- Guessous I, Eap CB, Bochud M. 2014. Blood pressure in relation to coffee and caffeine consumption. Curr Hypertens Rep. 16(9):468.
- He FJ, Li J, Macgregor GA. 2013. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 346:f1325.
- He FJ, Markandu ND, Sagnella GA, MacGregor GA. 1998. Importance of the renin system in determining blood pressure fall with salt restriction in black and white hypertensives. Hypertension. 32(5):820–824.
- Intersalt Cooperative Research Group. 1988. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ. 297(6644):319–328.
- Liclican EL, Doumad AB, Wang J, Li J, Falck JR, Stier CT Jr, Carroll MA. 2009. Inhibition of the adenosine2A receptor-epoxyeicosatrienoic acid pathway renders Dahl salt-resistant rats hypertensive. Hypertension. 54(6):1284–1290.
- Liclican EL, McGiff JC, Pedraza PL, Ferreri NR, Falck JR, Carroll MA. 2005. Exaggerated response to adenosine in kidneys from high salt-fed rats: role of epoxyeicosatrienoic acids. Am J Physiol Renal Physiol. 289(2):F386–F392.
- Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, et al. 2014. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. 371(7):601–611.
- Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, Lim S, Danaei G, Ezzati M, Powles J. 2014. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 371(7):624–634.
- Nayeem MA, Zeldin DC, Boegehold MA, Falck JR. 2011. Salt modulates vascular response through adenosine A(2A) receptor in eNOS-null mice: role of CYP450 epoxygenase and soluble epoxide hydrolase. Mol Cell Biochem. 350(1–2):101–111.
- Nayeem MA, Zeldin DC, Boegehold MA, Morisseau C, Marowsky A, Ponnoth DS, Roush KP, Falck JR. 2010. Modulation by salt intake of the vascular response mediated through adenosine A(2A) receptor: role of CYP epoxygenase and soluble epoxide hydrolase. Am J Physiol Regul Integr Comp Physiol. 299(1):R325–R333.
- Obarzanek E, Proschan MA, Vollmer WM, Moore TJ, Sacks FM, Appel LJ, Svetkey LP, Most-Windhauser MM, Cutler JA. 2003. Individual blood pressure responses to changes in salt intake: results from the DASH-Sodium trial. Hypertension. 42(4):459–467.
- O'Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, Yan H, Lee SF, Mony P, Devanath A, et al. 2014. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 371(7):612–623.
- Poucher SM, Keddie JR, Singh P, Stoggall SM, Caulkett PW, Jones G, Coll MG. 1995. The in vitro pharmacology of ZM 241385, a potent, non-xanthine A2a selective adenosine receptor antagonist. Br J Pharmacol. 115(6):1096–1102.
- Riksen NP, Rongen GA, Smits P. 2009. Acute and long-term cardiovascular effects of coffee: implications for coronary heart disease. Pharmacol Ther. 121(2):185–191.
- Riksen NP, Smits P, Rongen GA. 2011. The cardiovascular effects of methylxanthines. Handb Exp Pharmacol. (200):413–437.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG, et al. 2001. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 344(1):3–10.
- Schreiber-Deturmeny E, Bruguerolle B. 1996. Simultaneous high-performance liquid chromatographic determination of caffeine and theophylline for routine drug monitoring in human plasma. J Chromatogr B, Biomed Appl. 677(2):305–312.
- Siragy HM, Linden J. 1996. Sodium intake markedly alters renal interstitial fluid adenosine. Hypertension. 27(3):404–407.
- Smits P, Boekema P, Abreu RD, Thien T, Vanʼt Laar A. 1987. Evidence for an antagonism between caffeine and adenosine in the human cardiovascular system. J Cardiovasc Pharmacol. 10(2):136–143.
- Smits P, Hoffmann H, Thien T, Houben H, van't Laar A. 1983. Hemodynamic and humoral effects of coffee after beta 1-selective and nonselective beta-blockade. Clin Pharmacol Ther. 34(2):153–158.
- Smits P, Thien T, Van 't Laar A. 1985a. The cardiovascular effects of regular and decaffeinated coffee. Br J Clin Pharmacol. 19(6):852–854.
- Smits P, Thien T, van't Laar A. 1985b. Circulatory effects of coffee in relation to the pharmacokinetics of caffeine. Am J Cardiol. 56(15):958–963.
- Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. 2009. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ. 339:b4567.
- van Dusseldorp M, Smits P, Thien T, Katan MB. 1989. Effect of decaffeinated versus regular coffee on blood pressure. A 12-week, double-blind trial. Hypertension. 14(5):563–569.
- Zhang Y, Coca A, Casa DJ, Antonio J, Green JM, Bishop PA. 2015. Caffeine and diuresis during rest and exercise: a meta-analysis. J Sci Med Sport. 18(5):569–574.
