Abstract
Background: Mental health policies advocate service user participation in care planning. However, service users often feel they’re not fully involved and direct access to users’ own electronic care plans in the community can be an obstacle. To address this, an electronic care pathway tool (CPT) was co-designed by service users, staff and software developers, to facilitate co-production of care and crisis plans.
Aims: To investigate the feasibility and acceptability of the pilot implementation of the CPT in professionals’ practice to co-produce care plans and enable efficient working.
Method: Qualitative interviews with fifteen mental health practitioners, and five service development/management staff. Normalisation process theory, which outlines the social processes involved in implementing technology, and co-production theory, informed interviews and data analysis.
Results: Multiple factors influenced CPT usage, including people’s views of technology, practitioners’ relationships with service users, service users’ mental health needs, and their capacity for reflective thinking. The CPT’s visual and interactive features could enable co-production of care plans. The CPT supported practitioners’ efficiency, but its features did not easily streamline with electronic patient records.
Conclusions: CPT interactive touchpoints supported service users’ therapeutic reflection and facilitated care planning involvement. Information technology system interoperability was an obstacle.
Background
Mental health policies highlight the importance of involving service users in developing and reviewing their care plans (Department of Health, Citation2008; NHS England, Citation2016), which can facilitate recovery (Bee, Price, Baker, & Lovell, Citation2015). Yet in practice, service users often feel they are not fully engaged in care planning (Bee et al., Citation2015; Brooks, Lovell, Bee, Sanders, & Rogers, Citation2018; Grundy et al., Citation2016). Care planning can prioritise organisational needs and risk prevention, yet service users want a holistic approach that reflects their everyday lives (Brooks et al., Citation2018; Simpson et al., Citation2016a). There is a need for greater co-production in care planning (Simpson et al., Citation2016b), where service users work in equal partnerships with staff and build on their strengths and capabilities (Nesta, Citation2012). Care plans should be in an accessible format where service users can include their own written text, identified recovery needs, priorities and goals (Bee et al., Citation2015; Grundy et al., Citation2016; Simpson et al., Citation2016b). Electronic records and inflexible electronic care plan formats can limit community-based practitioners’ ability to work directly on care plans with service users (Brooks et al., Citation2018; Simpson et al., Citation2016b). Solutions may lie in “more integrated IT systems and the use of modern, mobile technology” (Simpson et al., Citation2016b, p. 106).
The study of mental health information technology (IT), hosted by institutions, where both practitioners and service users interact with technology through a shared interface to encourage collaborative decision-making is at an early stage (Henshall et al., Citation2017). Previous mental health IT research has focussed on access and engagement with IT (Ennis, Rose, Denis, Pandit, & Wykes, Citation2012; Schrank, Sibitz, Unger, & Amering, Citation2010); service user owned electronic personal mental health records (Ennis et al., Citation2014); digital psychological interventions (Tunney, Cooney, Coyle, & O'Reilly, Citation2017) and mobile apps for self-management (Goodwin, Cummins, Behan, & O’Brien, Citation2016; Naslund, Marsch, McHugo, & Bartels, Citation2015). A systematic review of mental health IT implementation studies recommends that service users and staff should co-develop and implement digital health interventions (Aref-Adib et al., Citation2019). This study contributes to literature gaps by focussing on: the use of mental health technology where service users and staff were involved in its development, design and implementation (Ennis et al., Citation2014; Wykes & Brown, Citation2016); how this technology was used by practitioners within services (Hill et al., Citation2017; Hollis et al., Citation2018; Wykes & Brown, Citation2016) and the effects of this technology on service user-practitioner consultations and shared decision-making from staff perspectives (Mair et al., Citation2012; Wykes & Brown, Citation2016). Implementing IT interventions into routine practice can be difficult (Hill et al., Citation2017); and research is needed to understand how mental health technologies are used in everyday practice (Hollis et al., Citation2015; Wykes & Brown, Citation2016).
This article examines the acceptability and perceived effectiveness of the pilot implementation of a care pathway tool (CPT) into clinical practice from staff perspectives. The CPT was co-designed by software developers (Otsuka Health Solutions), mental health staff (from Avon and Wiltshire Mental Health Partnership NHS Trust) and a group of service users and aimed to enable service users and staff to co-produce care plans, crisis plans and progress notes. The CPT was hosted on a touchscreen tablet computer. Its features are outlined in , with examples in and .
Figure 1. CPT feature ‘People in my life’. The copyright and all other intellectual property rights in the Care Pathway Tool are owned by Otsuka Health Solutions.
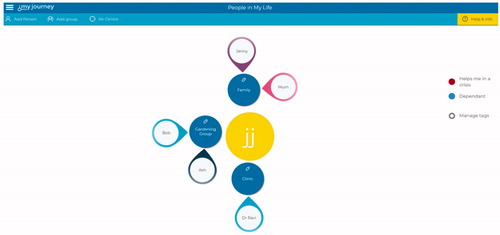
Figure 2. CPT feature ‘Managing my warning signs’. This feature was developed with kind permission of the authors of the card sorting approach by Birchwood et al (Birchwood et al., Citation2000), who retain the intellectual property rights to it. The copyright and all other intellectual property rights in the Care Pathway Tool are owned by Otsuka Health Solutions.
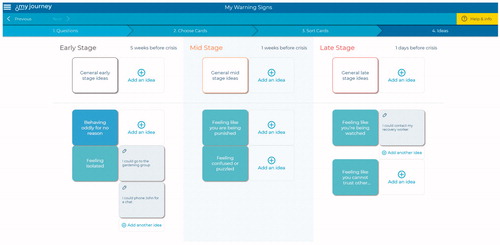
Table 1. CPT features.
The CPT was part of a wider IT project to facilitate integrated care records and system management overseen by a Joint Project Board, whose members included service users, practitioners, managers and software developer staff. They actively used co-production principles (Nesta, Citation2012), where service users were partners in IT tool design and development. Co-production training and support was provided by Rethink. Supplementary file 1 illustrates how the CPT was co-developed with service users. The independent evaluation was undertaken by NIHR CLAHRC West. Research questions asked how the CPT may: (a) facilitate working in co-production and impact on practitioners’ interactions with service users; (b) enable the development and recording of service user co-produced care planning, risk and progress records and (c) support efficient working.
Methods
Interview sampling and recruitment
The CPT pilot implementation took place between March and December 2016. Potential interview participants were identified by service provider and software developer members of the Joint Project Board who oversaw the IT project and were invited to take part in an interview with researchers via emails from the software developers, with a participant information sheet. Potential interviewees were asked to contact the researchers to take part. All practitioners who took part in the CPT pilot (n = 30) were invited as potential interviewees. Fifteen CPT practitioners (Recovery navigators, Peer support workers, Psychiatrists, Occupational therapists, Specialist Recovery Practitioners and Social workers) responded and an interview was organised; fifteen did not respond. Fifteen managers and senior clinicians involved in the wider IT project to facilitate integrated care records and system management were invited to take part. Four did not respond, six responded saying that they did not know enough about the project to take part. Five managers were interviewed (team managers, quality leads, development managers and a senior manager).
Interview procedures
In-depth interviews were conducted between October and November 2016. All interviews were conducted by experienced social scientists MF and CP by telephone to enable busy community-based professionals to take part. Recorded verbal consent was gained before the interviews. Interviews took between 13 and 60 min (average 32 min). The fifteen practitioners who used the CPT were asked about (i) their views and experiences of the CPT; (ii) acceptability and feasibility of using the CPT including service users’ reactions and interactions when using it; (iii) impact on working practice and ability to co-produce care plans and (iv) suggested improvements. A topic guide was developed in collaboration with software developers, members of the Joint Project Board and service user members of this Board who expressed an interest. Questions to the five managers interviewed included strategic perspectives affecting the adoption of new IT innovations, IT implementation and the organisational context within which the CPT was developed. Interview questions (Supplementary file 2) were structured around normalisation process theory (NPT) (Murray et al., Citation2010). NPT outlines the social processes involved in technological implementation ().
Table 2. NPT constructs related to CPT implementation.
Data analysis
Interviews were audio recorded, fully transcribed (including recorded verbal consent), anonymised, checked for accuracy and imported into NVivo 10 qualitative data analysis software. Transcripts were thematically analysed using a data-driven approach (Braun & Clarke, Citation2006) until saturation within the confines of the number of people participating in the pilot (Sandelowski, Citation1995). Themes were ordered using NPT as a framework (Supplementary file 3). Two researchers (MF and CP) conducted the analysis, double-coding the initial interviews to ensure rigour. Where there were differences, these were discussed, and ways to develop the thematic codes were agreed. The wider research team discussed key themes to ensure credibility and external validity, considering emerging findings, alternative explanations and diverse cases. The CPT practitioners and managers interview data sets were analysed separately, and then synthesised within different themes.
Touchpoint analysis
NPT has previously been integrated with co-production theory, analysing touchpoints to understand people’s interactions with technology (Farr et al., Citation2018). Touchpoints are where service users come into contact with a service and can include interactions with people, technology or physical environments. Touchpoints are points of service interaction that affect users’ experiences and feelings about that service (both positively and negatively). Touchpoint analysis has been used in healthcare improvement methods (Bate & Robert, Citation2007) and has been employed to understand how to improve healthcare technology design (Farr et al., Citation2018). In this study, technological touchpoints included the hardware device that the CPT was hosted on (mobile computer tablet with detachable keyboard) and the different CPT software features ( ). Different touchpoints were analysed to understand how CPT features affected practitioners’ interactions with service users and its perceived effectiveness.
Table 3. How CPT touchpoints affected practitioner and service user interactions.
Results
Data are presented below, using the four NPT constructs () and technological touchpoints of the CPT.
Coherence
Staff perceived that the CPT could potentially facilitate more collaborative care:
[It gives the] opportunity to try and improve the service for service users so that it was less… dictated to them what their care plan was, what their recovery plan was…. It's a way of getting their voice heard and having their involvement right from the start (Practitioner 03).
Practitioners were keen to write electronic care plans with service users, rather than the usual practice of writing them up after meetings. Other anticipated CPT benefits included: using time more effectively; accessing information more easily; quicker administrative duties and better ways of presenting information without relying on handwritten notes. Training was provided to practitioners to functionally use the tool and introduce it to service users, further training suggestions included sharing different ways that practitioners had worked with the CPT with service users.
Cognitive participation
In analysing what promoted participation with the CPT, issues were related to organisational context; using an IT tablet computer in mental health consultations and how practitioners introduced the CPT to service users.
Organisational context
Sufficient time and resources affected the extent to which practitioners were able to learn about and use the CPT:
It’s just down to how busy people are, that’s the biggest barrier (Practitioner 11).
Cultural issues such as the extent to which technology was used in everyday practice also affected CPT implementation:
No-one uses Outlook calendars and people still use faxes… it's still a very paper heavy mindset (Practitioner 03).
Service reorganisation may also have affected the degree to which staff were willing to engage:
There’ve been a huge number of changes to mental health services… I think staff have got change fatigue, they don’t necessarily always embrace things in the way that you might hope that they would (Manager 01).
The organisational culture surrounding the development and use of care plans, was perceived as needing to change, with the CPT potentially having a role in this:
Half of [service users] haven't seen their care plan or it was done at a time when they were in a difficult place or it's changed a lot since… the culture isn't there yet in terms of putting that front and centre of their recovery.… This tool [CPT] will certainly help to readdress that (Practitioner 03).
Using an IT tablet computer in mental health consultations
It was unusual for mental health practitioners to have access to a service user’s electronic records during consultations. Usual practice was to take mental or paper notes of discussions with service users, transferring these to the organisation’s electronic patient record (EPR) afterwards (usually on a fixed desktop computer in a different room/office). Introducing a mobile tablet computer prompted data security concerns from the NHS organisation. The tablet computer that hosted the CPT was “completely locked down” (Practitioner 03). Practitioners could access their NHS email but not the internet, which could limit the CPT’s usefulness e.g. searching for community resources with service users. Practitioners spoke of problems logging on and accessing service user files, forgetting passwords or the tablet computer running out of battery. One practitioner spoke of difficulties if they met their clients outside, where sunshine could affect screen visibility. Another interviewee felt it was inappropriate to use the tablet computer in a public place as they thought it could be stigmatising. Practitioners’ relationship with technology and working routines could affect the extent to which they used a tablet computer with a service user:
I’ve not ever been someone that writes things down I think when I’m in a meeting with a service user, I find it harder to listen if I’m doing that, so putting something in between myself and a service user in some ways made it more challenging for me (Practitioner 08).
Fear of damaging existing therapeutic relationships with service users could limit use. Some service users did not want to engage with the technology:
He just said flat, 'No.' He said, 'I wanna talk to you, I wanna talk to a human being’ (Practitioner 03)
Younger service users were perceived to be more familiar with technology and how to engage with touchscreen devices, although this was not always the case, with some older people engaging with the technology.
Introducing the CPT to service users
Several practitioners highlighted the need to prepare before using the CPT, to navigate its different features, and plan sessions. Deciding when to introduce the CPT to service users was dependent on their mental health state, needs, recovery stage and capacity for therapeutic reflection. CPT features required service users to reflect on their past, personal circumstances and future goals, making reflexive links between aspects of one’s life. Practitioners thought such therapeutic practices may not always be appropriate.
They’d had a bad day or bad week and they just needed to talk and sometimes… getting the tool [CPT] out, it wasn’t appropriate (Practitioner 02)
Mistrust of technology could be an issue:
One guy he was suffering from a bit of psychosis, who didn’t want the computer in the room because he thought it would be recording him (Practitioner 01)
Conversely, one practitioner highlighted the CPT could ensure service user’s notes were open and collaborative:
One particular person… he's incredibly paranoid… he was talking about people writing all these notes about him and keeping it on file… I said, 'Well, look there's this new tool [CPT]… we can, together, go through what we've talked about and at the end spend the last five or ten minutes just typing that up so that you can see what I'm writing about you and what is kept on our NHS system about you.' And he said that that would be really useful (Practitioner 03)
If service users had low levels of English language reading skills, some interviewees thought this may limit CPT use.
Collective action
The CPT had the potential to facilitate conversations by adding structure and visual material:
Some people [service users] get really enthused by it and really like having that visual element (Practitioner 06)
Where service users may have been experiencing difficult emotions, it could provide a practical focus:
Some kind of external focus actually helps… like focusing on an activity rather than somebody’s emotions. (Practitioner 13)
Touchpoints, where service users interacted with the CPT, are analysed in . Touchpoints that were easy to use and supported reflection and discussion directly linked to users’ support needs were popular, for example Managing my Warning Signs () and People in my Life (). Features that were less popular included My Journey, which consisted of large amounts of clinical information, but with less clear ways to therapeutically interact with this.
Reflexive monitoring
Practitioner perspectives
Staff saw several advantages to using the CPT. It could help facilitate conversations:
They’ve [staff] said that it’s been really easy to approach having maybe quite challenging and difficult situations with service users through using the tool [CPT] because it’s quite interactive and… it makes it able to initiate those conversations (Manager 04).
The ability to co-produce notes was seen by some interviewees to have a wider effect on the power relations between service users and practitioners:
If you give people more control over the work that you do together, it changes the relationship…. Things feel more equal and people feel more able to be involved in what can be quite an oppressive process (Practitioner 07)
However, it was highlighted that it was also the relationship with a service user that was the basis for collaborative working, rather than the adoption of a specific tool:
The most important thing is the relationship you have with someone…. That I think is probably the most important thing and will always be… (Practitioner 12).
Most interviewees said the CPT saved them time, as they did not have to return to the office to type up notes:
It has made me more productive… I'm better able to utilise my time (Practitioner 09)
Overall, most pilot participants were positive about the CPT and wanted to continue using it. Two interviewees said they didn’t want to use it further.
System interoperability
Interoperability between CPT software and the existing NHS organisational EPR system was a barrier to use. There was no synchronous cross-system communication; records input into the CPT were not automatically transferred into the organisation’s EPR system. Until a technological fix was found, administrators manually transferred this data as an interim solution, which meant there could be a time lag of up to 48 h for the main EPR system to be updated. When a service user was in crisis, practitioners using the CPT still needed to update the main EPR system the day they saw the client. In addition, the interactive formatting of the CPT did not always map easily onto the EPR system data fields.
There are so many other little places on [the EPR system] that you have to put appointments… you have to put letters in another place and you have to put a CPA review in another place (Manager 02)
Some interactive CPT features downloaded as pdfs into the EPR, and practitioners sometimes needed to manually enter information into specific EPR fields.
Collective appraisal of the CPT
The organisation’s care plan template on the EPR included policy and organisational mandated elements. In contrast, through its co-design, the CPT reflected care planning elements that service users and staff co-designing it found most helpful. This meant that sometimes, mandatory care planning elements were not always collected, and it was decided that the CPT would not replace existing mandated care planning elements. This decision was driven by a cautionary approach to testing new electronic tools in the NHS.
When the pilot completed, financial pressures of the NHS Trust meant the partnership between the Trust and software developers came to an end. Technological development in the NHS does not always show immediate impact, and ongoing challenges of IT interoperability combined with the NHS struggling with resource and capacity issues, meant the Trust was no longer able to invest in the CPT’s further development.
Discussion
This study contributes to identified evidence gaps (Ennis et al., Citation2014; Hill et al., Citation2017; Mair et al., Citation2012; Wykes & Brown, Citation2016) to illustrate how user co-designed technology was adopted by mental health staff in everyday practice, exploring how technology use was initiated within and affected practitioner-service user consultations from staff perspectives. The CPT’s visual interactive touchpoints encouraged service user engagement and co-production of care plans and progress records. However, integrating these features into EPRs was challenging.
Some staff acknowledged that historically, service users were not fully involved in care planning, mirroring previous research (Bee et al., Citation2015; Brooks et al., Citation2018; Grundy et al., Citation2016; Simpson et al., Citation2016a). The organisation’s Care Quality Commission (CQC) inspection had highlighted that care plans needed more service user input and be more regularly updated (CQC, Citation2016). Staff perceived CPT usage could enable more service user engagement. When deciding whether to use the CPT, staff considered the potential for benefit, service users’ mental health state and care needs, and potential impact on existing therapeutic relationships. This aligns with other health technology research where clinicians can often assess only some service users as being ‘suitable’ for using a particular technology (Greenhalgh et al., Citation2017). Some staff emphasised that relationships with service users was core to involvement in care planning and recovery, as highlighted in other research (Brooks et al., Citation2018; Grundy et al., Citation2016; Simpson et al., Citation2016a, Citation2016b). Whilst previous research on technology use by people diagnosed with schizophrenia identified that ‘paranoid ideas’ about technology may be an obstacle (Schrank et al., Citation2010), this study found where service users mistrusted technology, this could both limit use, or enable it when the CPT was presented as an open way to share records.
Interactional workability of healthcare technology is vital to ensure it is adopted in everyday practice (Murray et al., Citation2011). The CPT touchpoints provided several identified facilitators to increase service user-led care planning (Bee et al., Citation2015; Simpson et al., Citation2016b), illustrating where its visual interactive features could initiate constructive conversations. Computer (rather than smartphone) based health IT can be a useful format to engage mental health service users less familiar with technology (Ennis et al., Citation2012). In this study a mobile computer tablet with detachable keyboard and touchscreen were seen to facilitate service users’ engagement with the CPT. Service users could type their own words into care plans and progress notes, which facilitated more open documentation and user involved care planning (Grundy et al., Citation2016). Practitioners saw this could have a positive effect on equalising power dynamics with service users. Popular CPT touchpoints were simple to use, interactive, and provided clear prompts that facilitated therapeutic interaction and reflection on symptom management and social support mechanisms, which could enhance practitioners’ understanding of service users’ experiences. This could support shared decision-making, and enable care planning to be based on service users’ networks and resources, key principles of co-production (Nesta, Citation2012).
summarises features that can engage staff and service users to adopt new technology within mental health services.
Table 4. Facilitators supporting engagement and uptake of new technology in mental health practice.
Most interviewees wanted to continue using the CPT, as they believed it facilitated the co-production of care plans and records and saved them administrative time, features supporting technological adoption (Murray et al., Citation2011; Ross, Stevenson, Lau, & Murray, Citation2016). However, inefficiencies also occurred, because of difficulties automatically writing back information into the EPR system. Interoperability problems often occur when introducing new technologies into health systems (Ross et al., Citation2016). Interactive technologies that engage service users need to be interoperable with EPRs to support efficient working.
Service users were involved in the design and development of the CPT and whilst patients’ needs must remain at the centre of technology development (Hollis et al., Citation2015), a tension arose between the elements of care planning that service users and practitioners found most useful, and those mandated by the organisation that were not always collected by the CPT. Technological development and implementation can be hindered by different stakeholder priorities (Mair et al., Citation2012).
Strengths and limitations
This study illustrates how the CPT affected interactions with service users from practitioners’ perspectives, analysing how its different co-designed features affected mental health support sessions and co-production within care planning. Through using touchpoint analysis, this article contributes to understanding how to make mental health technologies more engaging and easier to use for people who may lack confidence or have low IT literacy (Hollis et al., Citation2018). Interviews examined a broad range of staff members’ experiences and perspectives. However, some practitioners had only recently started using the CPT and were still exploring how the CPT could be used. Service users’ uptake of the CPT was also intermittent. Staff who volunteered to take part in the CPT pilot implementation were a self-selecting sample who may have been more enthusiastic about technology use. The limited sample of managers interviewed should be considered when interpreting our findings. Service users were not interviewed as part of this study, as they were taking part in a separate evaluation organised by the software developers. However, most issues raised by service users within the separate evaluation aligned with staff perceptions, which gives greater assurance to these research findings.
Conclusion
Interactive technology can facilitate service user engagement with care planning, but different factors influenced IT adoption in consultations, including service users’ mental health state, care needs and goals, capacity for reflective thinking, practitioners’ relationship with service users, and both practitioners and service users’ attitudes toward technology. Analysing the CPT’s touchpoints shows how interactive technological interfaces could provide new therapeutic and reflective opportunities. However, these features did not neatly dovetail into existing care plans and EPRs, and IT system interoperability was a technical challenge. Engagement and uptake of mental health technology could be improved by paying attention to factors outlined in . These factors can inform the future development of interactive tools designed to support service user involvement in care planning.
Ethics approval and consent to participate
The study was reviewed by the NHS Health Research Authority (ID: 199385) and ethically reviewed by the University of Bristol, Faculty of Health Sciences, Research Ethics Committee (Application: 29045). All participants provided recorded verbal consent for their anonymised quotes to be published.
Supplemental Material
Download Zip (573.3 KB)Acknowledgements
The authors thank the Engagement & Implementation Manager for her co-ordination and communication role within the research. They also thank the service users and carers who were involved in the development of the interview topic guide, and all interviewees who took part in the study.
Disclosure statement
Otsuka Health Solutions (OHS) were paid under contract by Avon and Wiltshire Mental Health Partnership NHS Trust (AWP) to design and develop digital solutions including the Care Pathway Tool described in the publication from April 2015 to December 2016. OHS paid the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) West a fee for the evaluation project which represented 50% of the costs of the project. OHS own the software referred to in this publication as the 'Care Pathway Tool'.
Data availability
The datasets generated during the current study are not publicly available due to the confidential nature of the participant interviews and the data containing information that could compromise research participant privacy/consent.
Additional information
Funding
References
- Aref-Adib, G., McCloud, T., Ross, J., O'Hanlon, P., Appleton, V., Rowe, S., … Lobban, F. (2019). Factors affecting implementation of digital health interventions for people with psychosis or bipolar disorder, and their family and friends: A systematic review. The Lancet Psychiatry, 6(3), 257–266. doi:10.1016/S2215-0366(18)30302-X
- Bate, P., & Robert, G. (2007). Bringing user experience to healthcare improvement: The concepts, methods and practices of experience-based design. Oxford: Radcliffe Publishing.
- Bee, P., Price, O., Baker, J., & Lovell, K. (2015). Systematic synthesis of barriers and facilitators to service user-led care planning. British Journal of Psychiatry, 207(02), 104–114. doi:10.1192/bjp.bp.114.152447
- Birchwood, M., Spencer, E., & McGovern, D. (2000). Schizophrenia: Early warning signs. Advances in Psychiatric Treatment, 6(2), 93–101. doi:10.1192/apt.6.2.93
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. doi:10.1191/1478088706qp063oa
- Brooks, H. L., Lovell, K., Bee, P., Sanders, C., & Rogers, A. (2018). Is it time to abandon care planning in mental health services? A qualitative study exploring the views of professionals, service users and carers. Health Expectations, 21(3), 597–605. doi:10.1111/hex.12650
- CQC. (2016). Community-based mental health services for adults of working age Quality Report. Avon and Wiltshire Mental Health Partnership NHS Trust: Care Quality Commission.
- Department of Health (2008). Refocusing the care programme approach: Policy and positive practice guidance. London: Department of Health.
- Ennis, L., Robotham, D., Denis, M., Pandit, N., Newton, D., & Rose, D. (2014). Collaborative development of an electronic Personal Health Record for people with severe and enduring mental health problems. BMC Psychiatry, 14(1), 305. doi:10.1186/s12888-014-0305-9
- Ennis, L., Rose, D., Denis, M., Pandit, N., & Wykes, T. (2012). Can't surf, won't surf: The digital divide in mental health. Journal of Mental Health, 21(4), 395–403. doi:10.3109/09638237.2012.689437
- Farr, M., Banks, J., Edwards, H. B., Northstone, K., Bernard, E., & Salisbury, C. (2018). Implementing online consultations in primary care: A mixed-method evaluation extending normalisation process theory through service co-production. BMJ Open, 8(3), e019966. doi:10.1136/bmjopen-2017-019966
- Goodwin, J., Cummins, J., Behan, L., & O’Brien, S. M. (2016). Development of a mental health smartphone app: Perspectives of mental health service users. Journal of Mental Health, 25(5), 434–440. doi:10.3109/09638237.2015.1124392
- Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., A'Court, C., … Shaw, S. (2017). Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. Journal of Medical Internet Research, 19(11), e367. doi:10.2196/jmir.8775
- Grundy, A. C., Bee, P., Meade, O., Callaghan, P., Beatty, S., Olleveant, N., & Lovell, K. (2016). Bringing meaning to user involvement in mental health care planning: A qualitative exploration of service user perspectives. Journal of Psychiatric and Mental Health Nursing, 23(1), 12–21. doi:10.1111/jpm.12275
- Henshall, C., Marzano, L., Smith, K., Attenburrow, M.-J., Puntis, S., & Zlodre, J. (2017). A web-based clinical decision tool to support treatment decision-making in psychiatry: A pilot focus group study with clinicians, patients and carers. BMC Psychiatry, 17(1), 265. doi:10.1186/s12888-017-1406-z
- Hill, C., Martin, J. L., Thomson, S., Scott-Ram, N., Penfold, H., & Creswell, C. (2017). Navigating the challenges of digital health innovation: Considerations and solutions in developing online and smartphone-application-based interventions for mental health disorders. British Journal of Psychiatry, 211(02), 65–69. doi:10.1192/bjp.bp.115.180372
- Hollis, C., Morriss, R., Martin, J., Amani, S., Cotton, R., Denis, M., & Lewis, S. (2015). Technological innovations in mental healthcare: Harnessing the digital revolution. British Journal of Psychiatry, 206(4), 263–265. doi:10.1192/bjp.bp.113.142612
- Hollis, C., Sampson, S., Simons, L., Davies, E. B., Churchill, R., & Betton, V. (2018). Identifying research priorities for digital technology in mental health care: Results of the James Lind Alliance Priority Setting Partnership. The Lancet Psychiatry, 5(10), 845–854. doi:10.1016/S2215-0366(18)30296-7
- Mair, F. S., May, C., O’Donnell, C., Finch, T., Sullivan, F., & Murray, E. (2012). Factors that promote or inhibit the implementation of e-health systems: An explanatory systematic review. Bulletin of the World Health Organization, 90(5), 357–364. doi:10.2471/BLT.11.099424
- Murray, E., Burns, J., May, C., Finch, T., O'Donnell, C., & Wallace, P. (2011). Why is it difficult to implement e-health initiatives? A qualitative study. Implementation Science, 6(1), 1–11. doi:10.1186/1748-5908-6-6
- Murray, E., Treweek, S., Pope, C., MacFarlane, A., Ballini, L., & Dowrick, C. (2010). Normalisation process theory: A framework for developing, evaluating and implementing complex interventions. BMC Medicine, 8, 63. doi:10.1186/1741-7015-8-63
- Naslund, J. A., Marsch, L. A., McHugo, G. J., & Bartels, S. J. (2015). Emerging mHealth and eHealth interventions for serious mental illness: A review of the literature. Journal of Mental Health, 24(5), 321–332. doi:10.3109/09638237.2015.1019054
- NHS England (2016). The five year forward view for mental health. A report from the independent Mental Health Taskforce to the NHS in England. London: NHS England.
- Nesta. (2012). People powered health: Co-production catalogue. London: National Endowment for Science, Technology and the Arts.
- Ross, J., Stevenson, F., Lau, R., & Murray, E. (2016). Factors that influence the implementation of e-health: A systematic review of systematic reviews (an update). Implementation Science, 11(1), 146. doi:10.1186/s13012-016-0510-7
- Sandelowski, M. (1995). Sample size in qualitative research. Research in Nursing & Health, 18(2), 179–183. doi:10.1002/nur.4770180211
- Schrank, B., Sibitz, I., Unger, A., & Amering, M. (2010). How patients with schizophrenia use the internet: Qualitative study. Journal of Medical Internet Research, 12(5), e70. doi:10.2196/jmir.1550
- Simpson, A., Hannigan, B., Coffey, M., Barlow, S., Cohen, R., Jones, A., et al. (2016a). Recovery-focused care planning and coordination in England and Wales: A cross-national mixed methods comparative case study. BMC Psychiatry, 16(1), 147. doi:10.1186/s12888-016-0858-x
- Simpson, A., Hannigan, B., Coffey, M., Jones, A., Barlow, S., Cohen, R., … Faulkner, A., et al. (2016b). Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP. Health Services and Delivery Research, 4(5). doi:10.3310/hsdr04050
- Tunney, C., Cooney, P., Coyle, D., & O'Reilly, G. (2017). Comparing young people's experience of technology-delivered v. face-to-face mindfulness and relaxation: two-armed qualitative focus group study. British Journal of Psychiatry, 210(04), 284–289. doi:10.1192/bjp.bp.115.172783
- Wykes, T., & Brown, M. (2016). Over promised, over-sold and underperforming? e-health in mental health. Journal of Mental Health, 25(1), 1–4. doi:10.3109/09638237.2015.1124406
