Abstract
Background: The positive impact of the outdoors on physical and mental health is increasingly being evidenced. However, the impact on vulnerable and disadvantaged individuals engaging in group based sustainable building construction has not been examined.
Aim: To provide the first pragmatic examination of the impact of engaging in a brief (8 days over 8 weeks) outdoor sustainable construction project on the mental health and social connectedness of hard to reach and disadvantaged groups.
Methods: In study 1, 93 young people not in education, employment or training took part whilst study 2 comprised 55 adults who were asylum seekers, long-term unemployed or men with longstanding depression. Self-report data were collected at baseline and towards the end of the programme.
Results: Those with poor mental health and social connection at baseline showed statistically and clinically significant improvements in depression, anxiety, resilience and social connection by the end of the brief intervention.
Conclusion: Engagement in a group based sustainable construction project can provide significant mental health and social benefits to a range of vulnerable and hard to reach groups with difficulties in these areas. Building on these findings could be important for health and social care policy for marginalised groups.
Introduction
The health and wellbeing benefits of the outdoors have long been recognised. Greenspace exposure has been associated with a range of general physical health benefits (Twohig-Bennett & Jones, Citation2018) especially for some specific groups (e.g. pregnant women, children and older adults) and particularly amongst those from the lowest socioeconomic groups (World Health Organization Regional Office for Europe, Citation2016).
In recent years, there has been increased interest in harnessing such possible benefits through deliberate and structured use of the outdoors. This has led to two broad ways individuals engage with the outdoors being identified: “experiencing a natural environment” (looking at nature or an activity taking place in a natural environment e.g. jogging) and “interacting with natural elements” (e.g. being active with nature or animals such as through horticulture) (Haubenhofer, Elings, Hassink, & Hine, Citation2010). The benefits of such use of structured green space activity have been reported with an array of groups (Rogerson, Barton, Bragg, & Pretty, Citation2017) including those with depression (e.g. Frühauf et al., Citation2016; Townsend, Citation2006); severe mental illness (schizophrenia spectrum disorder; bipolar or major depression; Kam & Siu, Citation2010); dementia (Whear et al., Citation2014); acquired brain injury (Thomas, Citation2004); those in secure mental health services (e.g. Roberts, Davies, & Maggs, Citation2015) and young people (Tillmann, Tobin, Avison, & Gilliland, Citation2018). A recent review also concluded that nature-based interventions (e.g. horticulture; care farms) offer ways to support the wellbeing of those in institutional settings (e.g. prisons, care homes and inpatient mental health facilities) (Moeller, King, Burr, Gibbs, & Gomersall, Citation2018).
While there are a multitude of terms used, “green care” has been suggested to encompass “interventions” (e.g. care farming, horticultural therapy and wilderness therapy) that aim “to maintain or promote a person’s social, physical, mental and even educational wellbeing” (Haubenhofer et al., Citation2010, p. 106) although the broader phrase “green care, nature-based interventions for vulnerable groups” (p. 17) has been recommended when using of the outdoors in relation to mental health (Bragg & Atkins, Citation2016). Additionally, blue space interventions (activities in a natural water setting such as canoeing, fishing and surfing) have also been shown to have impacts on mental health and wellbeing (Britton, Kindermann, Domegan, & Carlin, Citation2018). However, the evidence base for the impact of the outdoors on wellbeing is still in its infancy with most studies relying on qualitative methods or quantitative approaches with small participant numbers (commonly <20).
Within the “green care” literature, participation in woodland settings has been a popular area for research. For example, gaining a sense of purpose, meaning and togetherness has been reported for volunteers with mental health problems (Christie & Cole, Citation2017) while physical, mental health and social benefits have been reported (including fewer visits to the doctor and feeling safer in the community) amongst those with problems such as depression (Townsend, Citation2006).
In order to explain the possible mental health value of natural environments two complementary theories have been used (Mantler & Logan, Citation2015). First, the Stress Recovery Theory (Ulrich, Citation1983) posits that being in the outdoors elicits positive emotions which consequently lower stress. Second, Attention Restoration Theory (Kaplan, Citation1995) argues that natural environments are “restorative” because they do not require the cognitive effort (e.g. to filter information) experienced in man-made (built) environments. Whilst there is some evidence to support both of these theories, it is not clear what “dose” might be required or whether active or passive engagement with the outdoors is likely to have the greatest benefits (Berto, Citation2014). It is also possible that there are additional mechanisms at play especially when individuals are active within an outdoor setting.
Sustainable construction (sometimes referred to as eco building or green building) is the process of “creating structures and using processes that are environmentally responsible and resource-efficient throughout a building’s life-cycle from siting to design, construction, operation, maintenance, renovation and deconstruction” (https://archive.epa.gov/greenbuilding/web/html/about.html; accessed 16/8/19). Research has identified that there may be a number of benefits associated with living and working in structures of this type (e.g. Allen et al., Citation2015; Colton et al., Citation2014). However, reviews of nature-based interventions (Bragg & Atkins, Citation2016; Moeller et al., Citation2018), greenspace exposure (Twohig-Bennett & Jones, Citation2018) and green care (Haubenhofer et al., Citation2010) that describe various activities have no examples of or research reporting the impact of sustainable construction (SC) as a “green activity”. This indicates that SC is a new area of outdoor participation research. Examples of SC projects being delivered by a workforce of vulnerable and “hard to reach” participants exist, such as the Down to Earth Project (https://www.downtoearthproject.org.uk/; accessed 22/08/19), a not for profit social enterprise. In this model, SC is used to deliver community buildings and housing while fostering skills development and wellbeing amongst the volunteer workforce. While skills development has be quantified (e.g. through recognised certification and assessment, Roberts et al., Citation2015) there is no published research that examines the impact of SC on the wellbeing of a participant workforce from vulnerable and “hard to reach” groups.
The current research
The aim of this research is to provide the first pragmatic examination of the impact of engaging in a brief outdoor SC project on the mental health and social connectedness of “hard to reach” and disadvantaged groups. Specifically it was hypothesised that, participation in outdoor sustainable building projects would lead to improvements in self-reported depression; anxiety; wellbeing; social connection (generally and within the programme) and resilience amongst those with difficulties in these areas.
Methods
Design
A quantitative design was adopted using pre-post self-report measurement. It was intended that this would allow an examination of the size of any impact related to participation in social construction while addressing limitations with the existing wider green care literature (e.g. small sample sizes).
Participants
All those who attended Down to Earth groups (see intervention below) during the period September 2016 to March 2017 were invited to participate (n = 158). In total, 123 individuals agreed to provide data and did so at both time points. All participants were considered “disadvantaged” and “hard to reach” namely, young adults not in education, employment or training (study 1) and adults from a number of groups including asylum seekers, the long-term unemployed and men with longstanding depression (study 2). For study 1, data from 93 young people (68 men: 20 women: 5 did not disclose their gender; average age 19 years) were collected, although one cohort completed only the PHQ-4 (n = 28; 21 men: 7 women). Study 2 comprised data from 55 adults (40 men: 15 women; average age 36). Although this second study group included a small number of younger people (18–25) their route to accessing the scheme was because they belonged to another “excluded group” (e.g. asylum seekers). Typically more male than female participants engaged with the project although some female only groups have been introduced since this study. None of the participants currently had any paid employment and all participants were in receipt of some form of state or charitable support.
Procedure
Ethical approval was received from a university departmental ethics committee (Ref: 23916.1406). Participants were provided with written and verbal information about the study during the introductory briefing on day one. On day 2, those who provided informed written consent were given a booklet containing each of the measures. Due to the nature of attendance at the project, it was not possible to randomise individuals or to create a contemporary comparison group. Data were collected in the training room on-site at the start of day 2 (baseline) and 7 (post-intervention) and took approximately 5–10 min to complete. These days were selected from the 8 week programme to (a) allow for a gap between research information being given and consent being obtained and to reduce the impact of factors such as the anxiety of starting something new at baseline and (b) reduce the impact of celebrations of achievements over the course and possible sadness at the programme ending (post-intervention) on the measures. Where requested (e.g. where participants had difficulty reading or writing in English), participants were given support to complete the measures. This was in the form of items being read to them. Participants generated their own anonymous code to enable data to be linked across the two time points.
Intervention
Down to Earth (www.downtoearthproject.org.uk) is a not for profit social enterprise that works with vulnerable groups to create permanent sustainable, state of the art training venues, residential accommodation and learning spaces for future participants.
Individuals attended a group based sustainable building project at one of two sites for one full day per week over an 8 week period (maximum 8 sessions; typically 6–12 members per group). Each site has been developed over time to include a range of buildings (including classrooms, offices and kitchens) that are constructed from natural products such as timber, cob, straw and lime render, with a range of sustainable living features (e.g. solar technology, allotment gardens, animals and waste water treatment) on-site. The buildings are developed to a high standard to promote the ethos of “great spaces and buildings for everyone”. During each session participants are supported by staff to engage in group and individual tasks based on construction skills (e.g. timber frame construction; lime rendering) and outdoor skills (e.g. cooking with an open fire). Communal times included lunch. None of the attendees had worked on such projects previously. Funding to deliver the groups came from a number of sources namely Big Lottery Fund UK (Our Bright Future programme) (Study 1); Natural Resources Wales; and the BUPA UK Foundation (Study 2).
Measures
Participants completed four brief self-report measures in addition to providing their age and gender.
Mental health
The Patient Health Questionnaire (PHQ-4; Kroenke, Spitzer, Williams, & Löwe, Citation2011) is an ultra-brief (4 item) screening tool for anxiety and depression. Participants are asked to determine the extent to which they have been bothered, over the last 2 weeks, by each item, rated on a four-point scale (0=“not at all”; 3=“nearly every day”). The authors report good internal reliability for the scales (>0.8) and evidence the construct validity of the tool. The authors suggest a threshold score of 3 for screening for depression (2 items) and anxiety (2 items).
Wellbeing
The Short Warwick-Edinburgh Mental Well-being Scale (SWEMWBS; Taggard, Stewart-Brown, & Parkinson, Citation2015) is a widely used short measure of wellbeing. The seven items are rated over the past 2 weeks on a five-point scale (1=“none of the time”; 5=“all of the time”). The authors have shown that this short form is highly correlated with the longer Wellbeing measure and normative data are available from the National Household Survey: England (https://warwick.ac.uk/fac/med/research/platform/wemwbs/researchers/interpretations/; accessed 20/7/18). Data were transformed using the published procedure and a score of 19.71 (representing 1 SD below the published population mean) was used to indicate low wellbeing.
Resilience
The Brief Resilience Scale (BRS; Smith et al., Citation2008) is a six-item measure designed to measure the “ability to bounce back from stress”. Items are rated on a five-point scale (1=“strongly disagree”; 5=“strongly agree”) with three items being reverse scored. The authors have reported good internal consistency (>0.8) and adequate test retest reliability over 1 month (0.69) for the scale. A cut-off of 1 SD below the mean score (2.93; based on pooled data from Smith et al.’s studies 1–3) was used to indicate low resilience.
Social connection
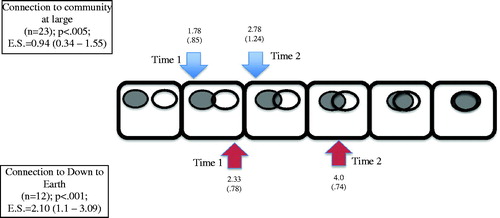
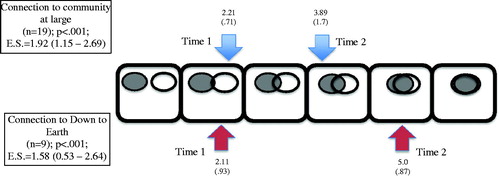
Social connection was assessed using an adaptation of the Inclusion of Community in the Self Scale (Mashek, Cannaday, & Tangney, Citation2007) designed for this study. Participants were presented with increasingly overlapping pairs of circles and asked to indicate which best reflected their level of connection. The adaptation asked participants to rate “your relationship with Down to Earth” (the study project) in addition to the original statement on the scale i.e. “your relationship with the community at large”. The authors report acceptable test retest reliability over a 2-week period (0.74) and provide good evidence of the convergent and discriminant validity of this measure. There is no established cut-off, therefore the bottom half of the scale range (3 or lower) was used to indicate difficulties in these areas.
Approach to analyses
As the creation of meaningful comparisons and participant randomisation were not possible, various means to determine the degree to which change had occurred and maximise reliability and validity were employed. Statistical significance testing and effect size change were coupled with approaches to determine the clinical significance and meaningfulness of change (e.g. Davies & Sheldon, Citation2012). This method has been adopted within the UK by the Improving Access to Psychological Therapies (IAPT) programme which has a treatment only cohort (see Community & Mental Health Team, Citation2018). Paired samples t tests were used to determine if changes over time were statistically significant. A power analysis (medium to large effect – 0.6; p<.05; power=.8) using G-Power (Faul, Erdfelder, Lang, & Buchner, Citation2007) indicated a minimum sample of 24 for a two-tailed test. Thresholds for reliable change and effect sizes were computed using online calculators (www.psyctc.org/stats/rcsc1.htm and www.psychometrica.de/effect_size.html, respectively). To examine clinically significant change for anxiety and depression, the methodology used by the IAPT programme was adopted (see Community & Mental Health Team, Citation2018). These involve identifying (a) the number of people who move from above the clinical cut-off to below it (termed “recovery”); (b) the number of individuals who change by more than the measurement error associated with the tool (termed “improvement”) and (c) those individuals who demonstrate both “recovery” and “improvement”. It is important to note that in this context, “recovery” and “improvement” are clinical significance classifications (see Jacobson & Truax, Citation1991). These very robust measures for determining change help mitigate possible threats to validity such as regression to the mean. For anxiety and depression, reliable change calculations indicated a threshold of two points (for each scale) be adopted for identifying clinical change.
Results
Baselines over time
The phased delivery of the groups over a period of 6 months allowed baseline data from those in the groups starting in the first 3 months of the study to be compared with those in the last 3 months. Analyses revealed no differences in baseline data over time suggesting that those entering the project at different time points (e.g. across seasons) did not significantly differ.
Comparison of participants from study 1 and study 2
At baseline, the young adult participants in study 1 were found to have significantly less connection to the community (t = 4.398; p<.001) and to Down to Earth (t = 2.735; p<.01) and reported lower wellbeing (t = 2.447; p<.05) than those in study 2. Using the National Household Survey of England average (of 23.6) as a benchmark, study 1 participants reported average wellbeing levels well below this (n = 60; 21.3) whilst study 2 participants were just below this level (n = 49; 23.4). No differences between the groups were observed for baseline anxiety, depression or resilience. On the basis of these findings it was decided to combine data from both studies for anxiety, depression and resilience whilst analysing the data for connection and wellbeing for each group.
Mental health: depression, anxiety and resilience
When data from all participants regardless of baseline score were analysed (n = 123), no changes over time were recorded on any of the measures. However, across the different areas measured, around a third of the group reported difficulties in each area at or above the threshold level (depression, 27%; anxiety, 42%; resilience, 35%). When inclusion in the analysis was limited to only those falling at or below the cut-off threshold described in the method section, statistically significant improvements were found (as shown in ) for depression (n = 27; t= −4.21, p<.001); anxiety (n = 43; t= −6.39, p<.001) and resilience (n = 24, t = 3.73, p<.001). As can be seen in the table, the change in anxiety and depression scores represented a large effect whilst for resilience this was in the medium to large range.
Table 1. Change in scores over time for those above threshold at baseline.
Of those meeting the threshold criteria for depression at time 1 (n = 27), 15 (55%) no longer met the threshold at the end of their participation and could be considered to meet the clinical significance criteria for “recovery”. For anxiety, 21 (49%) of the 43 participants meeting the anxiety threshold would be considered to meet the clinical significance criteria for “recovery” at time 2. Using a more demanding methodology (where inclusion was determined by meeting the anxiety or depression cut-off or both at time 1, and “recovery” requires both anxiety AND depression to be below cut-off at time 2), 20 (42%) of the 48 individuals included in the analysis met this clinical significance criteria for “recovery”.
Reliable improvement for anxiety and depression required a change in score of two points or more between time 1 and time 2. Of the 43 individuals reaching the cut-off for anxiety, 23 (53%) showed reliable improvement and only 2 (5%) showed reliable deterioration. For depression, 13 (48%) of the 27 individuals meeting the cut-off at time 1 showed reliable improvement with 1 (4%) showing deterioration.
Combining these two approaches allowed the calculation of reliable “recovery”. Of the 48 individuals with elevated anxiety or depression scores (or both) at time 1, 16 (33%) met this stringent criteria for “reliable recovery”.
Wellbeing
Study 1: OBF (young people who are not in education, employment or training)
Of the 33 individuals in this group with wellbeing data at both time points, 12 individuals had scores below the threshold at time 1. Although the average wellbeing score improved over time, the level of change was not statistically significant and mean scores remained below the general population.
Study 2: Adults (asylum seekers, long-term unemployed)
Complete wellbeing data were available for 39 individuals in this group; 7 of whom showed low levels of wellbeing at baseline. As with study 1 participants, the improvement over time was not statistically significant and mean scores remained below the general population.
Social connection
Study 1: OBF (young people who are not in education, employment or training)
As can be seen in , significant changes with a large effect size can be seen over time for those who reported difficulties in this area (n = 23 community; n = 12 – Down to Earth). For the “community at large” ratings, the time 2 score approached the threshold score (3) whilst this threshold was exceeded with respect to Down to Earth.
Study 2: Adults (asylum seekers, long-term unemployed)
For study 2 participants reporting difficulties (n = 19 – community; n = 9 – Down to Earth), showed statistically significant improvements in social connection, both in general and within the project. In addition, the mean score at time 2 (for those with poor initial wellbeing) was considerably higher than the threshold score of 3 ().
Discussion
This study has demonstrated that individuals from marginalised and “hard to reach” groups with needs in relation to anxiety, depression, resilience and social connection show statistically and clinically significant gains over the course of a brief programme of sustainable construction. Although the “intervention” contained no formal or specific element of treatment designed to directly impact mental health or social problems, the findings indicate that SC can maintain or promote social and mental wellbeing in a range of areas. Together with previous research showing the educational benefits for SC attendees (Roberts et al., Citation2015) this research suggests that SC can be viewed as a green care approach (Haubenhofer et al., Citation2010).
Limitations with the exiting green care evidence base mean that it is not possible to index the significant changes reported here against other forms of green care. As an alternative, comparing SC with specialist therapeutic interventions for anxiety and depression such as the IAPT programme show that although the rates of clinically significant change are lower (where 65% reliable improvement and 47% reliable “recovery” have been reported; Community & Mental Health Team, Citation2018) the effect sizes associated with changes in anxiety and depression are encouraging when compared with a CBT (d = 0.97; Thimm & Antonsen, Citation2014) and an internet delivered physical activity programme (d = 0.67; Strom et al., Citation2013). However, it must be stressed that the methods adopted in these latter studies differ from those used here and participant inclusion may differ, so direct comparisons must be applied cautiously.
A high proportion of people in this study reported above threshold levels of difficulty in relation to the areas measured (e.g. 27% reached the threshold for depression and 42% for anxiety at time 1), providing evidence that those in “hard to reach” and marginalised groups are likely to experience rates of mental health and social difficulties which are much greater than rates within the general population for the region (10% for common mental health difficulties including anxiety and depression; Singleton, Bumpstead, O'Brien, Lee, & Meltzer, Citation2001). Combining these rates with the impact of SC shown here suggests SC could be one way to meet “sustainable wellbeing” goals such as those promoted by the Welsh Government (see https://futuregenerations.wales/about-us/future-generations-act/; accessed 1/6/18).
The changes in social connection outside the project suggest a transfer of effect from the project to the wider experiences of individuals. Given that some have argued that improving social connection should be a public health priority because of the health and wellbeing benefits associated with social connection (Holt-Lunstad, Robles, & Sbarra, Citation2017), this effect may be particularly valuable. In contrast, the specific measure of wellbeing was the only measure to show a non-significant improvement over the course of the intervention. While this may mean that SC had less of an impact in this area, it is likely that the low participant numbers in these analyses account for this. It is also possible that there is a lag between improvements in specific measures (e.g. anxiety, social connection) and more global wellbeing measures. Longitudinal research will be needed to examine these areas further.
It is recognised that there are many components to sustainable construction that could lead to the changes seen (e.g. team working, skills development, time in the outdoors) and that the active ingredients may differ from person to person (c.f. specific and general responders; Davies & Nagi, Citation2017). Qualitative methods could explore participants experiences of both SC and changes in their social and mental wellbeing as has been undertaken in other green care research. Additionally, there may be some merit in attempting to determine the impact of specific components on individuals although comparing different forms of green care in their entirety would be more feasible. To facilitate cross programme comparisons, other researchers could adopt the brief measures used here which were found to be feasible and sensitive to change with a heterogeneous group of participants. This would establish a consistent way to quantify the impact of outdoor programmes in order to enhance the green care evidence base and develop a greater understanding of “what works” with a range of groups. To enhance study inclusion, the potential limitations of using language based self-report measures could be overcome through using a simpler yet reliable and valid method of self-rating; such a tool has been developed and is available from the authors (Davies et al., in preparation).
As this research was conducted at a single setting within the UK, a replication by other sustainable construction providers would allow the generalisability of the findings to be tested along with the impact of possible cultural or societal factors. The authors would welcome contact from such services elsewhere in the world to undertake such work.
The study design and approach to analysis adopted here provided external validity of the findings, and has been used by others when comparison or control groups are not practical or ethical (e.g. IAPT). However, future research should attempt to collect further contextual and demographic information and consider including comparison or waitlist control groups to maximise internal validity. It is recognised that for interventions requiring active engagement, randomisation may be neither possible nor wanted and thus the simple application of an RCT design is unlikely to be appropriate (see Black, Citation1996 for some of the many reasons). However, it may be feasible to apply a stepped wedge design with a 3, 6 or 12 month follow up of participants. Such a design would pose several challenges (e.g. accessing participants over time; the need to minimise the assessment burden on participants; cost implications of such as study) which would need to be overcome.
Conclusion
This research provides the first evidence that group based sustainable construction with vulnerable and hard to reach groups can bring about important changes in self-reported levels of anxiety, depression and resilience, in addition to improvements in social connection. As such it contributes to the existing “green care” research by evidencing the impact of a new form of activity: sustainable construction.
Acknowledgements
The authors thank all the participants who took part.
Disclosure statement
MM is the co-founder and director of Down to Earth and JB and KD are employed by Down to Earth. The other authors report no conflict of interest.
References
- Allen, J. G., MacNaughton, P., Laurent, J. G. C., Flanigan, S. S., Eitland, E. S., & Spengler, J. D. (2015). Green buildings and health. Current Environmental Health Reports, 2(3), 250–258. doi:10.1016/j.buildenv.2014.04.001
- Berto, R. (2014). The role of nature in coping with psycho-physiological stress: A literature review on restorativeness. Behavioral Sciences, 4(4), 394–409. doi:10.1111/j.1540-4560.2007.00497.x
- Black, N. (1996). Why we need observational studies to evaluate the effectiveness of health care. British Medical Journal, 312(7040), 1215–1218. doi:10.1136/bmj.312.7040.1215
- Bragg, R., & Atkins, G. (2016). A review of nature-based interventions for mental health care. Natural England Commissioned Reports (No. 204).
- Britton, E., Kindermann, G., Domegan, C., & Carlin, C. (2018). Blue care: A systematic review of blue space interventions for health and wellbeing. Health Promotion International, 29, 31. doi:10.1093/heapro/day103
- Christie, M. A., & Cole, F. (2017). The impact of green exercise on volunteer's mental health and wellbeing-findings from a community project in a woodland setting. Journal of Therapeutic Horticulture, 27(1), 17–33
- Colton, M. D., MacNaughton, P., Vallarino, J., Kane, J., Bennett-Fripp, M., Spengler, J. D., & Adamkiewicz, G. (2014). Indoor air quality in green vs conventional multifamily low-income housing. Environmental Science & Technology, 48(14), 7833–7841. doi:10.1021/es501489u
- Community and Mental Health Team. (2018). Psychological therapies: Annual report on the use of IAPT services. Health and Social Care Information Centre. Retrieved from https://files.digital.nhs.uk/publication/s/n/psyc-ther-ann-rep-2016-17_add.pdf.
- Davies, J., & Nagi, C. (2017). Selecting therapies and therapists. In J. Davies & C. Nagi (Eds.), Individual Psychological therapies in forensic settings: Research and practice (pp. 197–212). London: Routledge.
- Davies, J., & Sheldon, K. (2012). Single case methodologies. In K. Sheldon, J. Davies, & K. Howells (Eds.), Research in practice for forensic professionals (pp. 161–188). London: Routledge.
- Faul, F., Erdfelder, E., Lang, A.-G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. doi:10.3758/BF03193146
- Frühauf, A., Niedermeier, M., Elliott, L. R., Ledochowski, L., Marksteiner, J., & Kopp, M. (2016). Acute effects of outdoor physical activity on affect and psychological well-being in depressed patients – A preliminary study. Mental Health and Physical Activity, 10, 4–9. doi:10.1016/j.mhpa.2016.02.002
- Haubenhofer, D. K., Elings, M., Hassink, J., & Hine, R. E. (2010). The development of Green Care in Western European Countries. Explore, 6(2), 106–111. doi:10.1016/j.explore.2009.12.002
- Holt-Lunstad, J., Robles, T. F., & Sbarra, D. A. (2017). Advancing social connection as a public health priority in the United States. American Psychologist, 72(6), 517–530. doi:10.1037/amp0000103
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. doi:10.1037/0022-006X.59.1.12
- Kam, M. C. Y., & Siu, A. M. H. (2010). Evaluation of a Horticultural Activity Programme for Persons with Psychiatric Illness. Hong Kong Journal of Occupational Therapy, 20(2), 80–86. doi:10.1016/S1569-1861(11)70007-9
- Kaplan, S. (1995). The restorative benefits of nature: Toward an integrative framework. Journal of Environmental Psychology, 15(3), 169–182. doi:10.1016/0272-4944(95)90001-2
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., & Löwe, B. (2011). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. doi:10.1016/S0033-3182(09)70864-3
- Mantler, A., & Logan, A. C. (2015). Natural environments and mental health. Advances in Integrative Medicine, 2(1), 5–12. doi:10.1016/j.aimed.2015.03.002
- Mashek, D., Cannaday, L. W., & Tangney, J. P. (2007). Inclusion of community in self scale: A single-item pictorial measure of community connectedness. Journal of Community Psychology, 35(2), 257–275. doi:10.1002/j.1556-6676.2000.tb01932.x
- Moeller, C., King, N., Burr, V., Gibbs, G. R., & Gomersall, T. (2018). Nature based interventions in institutional and organisational settings: a scoping review. International Journal of Environmental Health Research, 28(3), 293–305. doi:10.1080/09603123.2018.1468425
- Roberts, C., Davies, J., & Maggs, R. G. (2015). Structured community activity for forensic mental health – a feasibility study. The Journal of Forensic Practice, 17(3), 180–191. doi:10.1177/030802260006300503
- Rogerson, M., Barton, J., Bragg, R., & Pretty, J. (2017). The health and wellbeing impacts of volunteering with the wildlife trusts. Report for the Wildlife Trusts. Retrieved August 29, 2019, from https://www.wildlifetrusts.org/sites/default/files/2018-05/r3_the_health_and_wellbeing_impacts_of_volunteering_with_the_wildlife_trusts_-_university_of_essex_report_3_0.pdf.
- Singleton, N., Bumpstead, R., O'Brien, M., Lee, A., & Meltzer, H. (2001). Psychiatric morbidity among adults living in private households 2000. London: The Stationery Office.
- Smith, B. W., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15(3), 194–200. doi:10.1097/00004650-200401000-00002
- Strom, M., Uckelstam, C.-J., Andersson, G., Hassmen, P., Umefjord, G., & Carlbring, P. (2013). Internet-delivered therapist-guided physical activity for mild to moderate depression: A randomized controlled trial. PeerJ, 1(3), e178. doi:10.7717/peerj.178/table-3
- Taggard, F., Stewart-Brown, S., & Parkinson, J. (2015). Warwick-Edinburgh Mental Well-being Scale (WEMWBS) (2nd ed.). Edinburgh: NHS Health Scotland.
- Thimm, J. C., & Antonsen, L. (2014). Effectiveness of cognitive behavioral group therapy for depression in routine practice. BMC Psychiatry, 14(1), 17. doi:10.1037/0022-006X.61.4.678
- Thomas, M. (2004). The potential unlimited programme: An outdoor experiential education and group work approach that facilitates adjustment to brain injury. Brain Injury, 18(12), 1271–1286. doi:10.1097/00001199-200010000-00007
- Tillmann, S., Tobin, D., Avison, W., & Gilliland, J. (2018). Mental health benefits of interactions with nature in children and teenagers: A systematic review. Journal of Epidemiology and Community Health, 72(10), 958–966. doi:10.1136/jech-2018-210436.supp2
- Townsend, M. (2006). Feel blue? Touch green! Participation in forest/woodland management as a treatment for depression. Urban Forestry & Urban Greening, 5(3), 111–120. doi:10.1016/j.ufug.2006.02.001
- Twohig-Bennett, C., & Jones, A. (2018). The health benefits of the great outdoors – A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental Research, 166, 628–637. doi:10.1016/j.envres.2018.06.030
- Ulrich, R.S. (1983). Aesthetic and affective response to natural environment. In I. Altman & J. Wohlwill (Eds.), Human behavior and environment, Vo1.6: Behavior and natural environment (pp. 85–125). New York: Plenum.
- Whear, R., Coon, J. T., Bethel, A., Abbott, R., Stein, K., & Garside, R. (2014). What is the impact of using outdoor spaces such as gardens on the physical and mental well-being of those with dementia? A systematic review of quantitative and qualitative evidence. Journal of the American Medical Directors Association, 15(10), 697–705. doi:10.1016/j.jamda.2014.05.013
- World Health Organization Regional Office for Europe (2016). Urban green spaces and health. Copenhagen: World Health Organization Regional Office for Europe.