Corona virus disease (Covid-19) is a global pandemic. The novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) that causes Covid-19 is reported to have originated in a seafood market in the Chinese city of Wuhan. It is hypothesised the virus was transmitted from live animals to humans at the market. The virus subsequently spread worldwide via human to human transmission (Lu et al., Citation2020). Covid-19 symptoms include fever (85.6%), a new and persistent cough (65.7%), fatigue (42.4%), dyspnoea (21.4%) and loss of sense of taste and/or smell (Hu et al., Citation2020). Neurological and gastrointestinal symptoms have also been reported. These include diarrhoea, vomiting, nausea, abdominal pain (Smyk et al., Citation2020) dizziness, as well as headache which may be part of a systemic illness rather than a specific neurological syndrome (Rogers et al., Citation2020).
Beyond the most commonly reported covid-19 symptoms, calls to action have been made to address the psychological impact of the disease (Byrne & Wykes, Citation2020; Kumar & Rajasekharan Nayar, Citation2020; Moreno et al., 2020). These include direct effects of covid-19 infection on the central nervous system such as encephalitis, Intensive Care Unit (ICU) related trauma, exacerbation of existing psychiatric disorder (Rogers et al., Citation2020) and the wider pandemic impact of isolation and distress incurred with social distancing, lock downs and quarantine (Jia et al., Citation2020; Lima et al., Citation2020). A systematic review assessed the psychiatric and neuropsychiatric presentations of severe acute respiratory syndrome (SARS), middle east respiratory syndrome (MERS) and Covid-19 and identified delirium as a common acute symptom (Rogers et al., Citation2020). Depression, anxiety, fatigue and post-traumatic stress disorder (PTSD) were common in the months after MERS and SARS. Rogers et al. (Citation2020) suggest patients with Covid-19 may also experience these conditions and symptoms, as well as insomnia following acute stages of infection.
People may also be at risk of persistent physical symptoms (PPS). Generally, these are defined as persistent bodily symptoms with functional disability but no explanatory structural pathology. Somatic Symptom Disorder (SSD) is the corresponding diagnosis in the Diagnostic and Statistics Manual-V (DSM-V). It refers to persistent (6 months or more) and clinically significant somatic complaints accompanied by excessive and disproportionate health-related thoughts, feelings and behaviours regarding the symptoms (American Psychiatric Association, Citation2013). Bodily Distress Disorder (BDD) is the diagnostic term used in the eleventh version of the International Classification of Diseases (ICD-11). It requires both the presence of one or more distressing bodily symptoms, that can either be “medically unexplained” or caused by a general medical condition, with “excessive, disproportionate or maladaptive” responses to the symptoms. Most importantly, both diagnostic terms include people with symptoms of distress related to medical conditions, for example, cancer, diabetes and heart disease. SSD describes a positive conceptualisation of symptoms based on presence of symptoms rather than absence of them. In addition, it moves beyond mind/body dualism, such that inexplicability does not equal psychiatric disorder, potentially leading to a better therapeutic alliance. Symptoms are not considered to be “in the mind” or solely due to distress (Chalder & Willis, Citation2018). For these reasons we prefer the diagnostic term SSD and will use it in the remainder of this article.
Despite there being a large body of literature investigating the psychological impact of covid-19, there is little mention of covid-19 related SSD, with the exception of some studies that investigate covid-19 related anxiety and its association with somatisation (Colizzi et al., Citation2020; Shevlin et al., Citation2020; Yifan et al., Citation2020). This may be due to ongoing, dualistic conceptualisations of health as either physical or psychological, despite efforts to provide more integrated care (Chalder, Citation2005; Deary, Citation2005). It could also be too early for reports given SSD diagnostic criteria states that symptoms should persist for 6 months or more. Unfortunately, the pandemic effects of covid-19 infection such as anxiety, social isolation, adverse media exposure, worry about significant others, limited access to health services are not only associated with a rise in mental health problems (Jia et al., Citation2020; Luo et al., Citation2020; Yao et al., Citation2020), they also create a “perfect storm” for the development of persistent symptoms.
In the United Kingdom (UK) general population, covid-19 related anxiety has been found to predict general somatic symptoms, particularly fatigue, followed by gastrointestinal (GI) symptoms (Shevlin et al., Citation2020). In China, several somatic symptoms were identified in 140 ICU nurses: (a) dyspnoea (30.7%), dizziness (17.9%), (b) headache (19.3%), nausea (21.4%); (c) chest discomfort/palpitation (31.4%), xerostomia (15.7%) and fatigue (15%) (Yifan et al., Citation2020). They were significantly associated with accidents and personal protective equipment (PPE) failure, giving rise to fears of covid-19 infection. In Italy, an adolescent boy presented with somatic symptoms suggestive of covid-19 (fever, increased heart rate to 130 bpm, delirium, breathing difficulty, altered taste and smell and general malaise) despite testing negative (Colizzi et al., Citation2020). Lowered mood and severe anxiety about his somatic symptoms with delusional intensity were also evident. A diagnosis of SSD was appropriate given history of functional neurological disorder (FND) and eating disorder onset in February 2019 in response to GI discomfort. However, there is no comment on the reliability of the covid-19 test i.e., if the test was repeated and found negative. There is also a lack of report on any covid-19 testing in the other studies. As such, we cannot be certain that participants were not experiencing symptoms of actual covid-19 infection as opposed to the somatising effects of covid-19 related anxiety.
Previous research suggests that people may in fact be at risk of SSD following actual infection with covid-19. Symptoms such as fatigue, have been shown to persist following the acute stages of a number of different viruses. Glandular fever, meningitis and hepatitis are significant risk factors for post-infectious chronic fatigue (Berelowitz et al., Citation1995; Candy et al., Citation2003; Cope et al., Citation1994; Hotopf et al., Citation1996; White et al., Citation2001). The previous coronavirus pandemic viruses, (MERS) and (SARS) were also associated with fatigue. 40.3% of SARS survivors reported a chronic fatigue problem, with 27.1% meeting the Centre for Disease Control (CDC) criteria for chronic fatigue syndrome (CFS) (Lam et al., Citation2009). Fatigue was also reported as a long-term chronic outcome up to 40 months post-infection, in at least one-third of MERS patients (Ahmed et al., Citation2020).
Given the development of fatigue following infection with a range of viruses, including the previous coronavirus pandemics, it is reasonable to assume that covid-19 infection will pose a similar threat. At the time of writing, fatigue and other symptoms are in fact being reported as ongoing, months after covid-19 infection (Carfì et al., Citation2020; Nabavi, Citation2020).
Previous research on post-infectious fatigue development shows it follows a temporal course that consists of defined phases. It is a common symptom in the acute stages of viral infections. It may then persist in a subacute phase of ≤3 months duration. A chronic phase refers to fatigue that persists beyond 6 months, long after the initial viral infection (CDC, 2015).
Risk factors that are associated with these phases can be categorised into biological, behavioural, cognitive, emotional and social domains. Elevated inflammatory markers such as CD4 and CD8 are associated with sub-acute fatigue (Candy et al., Citation2003; White et al., Citation2001). Fatigue at infection onset, prolonged bed rest, GP sick certification and psychological distress were significant risk factors for chronic fatigue in prospective cohort studies (Berelowitz et al., Citation1995; Candy et al., Citation2003; Cope et al., Citation1994; Hotopf et al., Citation1996; White et al., Citation2001). In contrast, physical fitness at infection onset was found to be protective (Candy et al., Citation2003; White et al., Citation2001). Cognitive and behavioural responses to symptoms can be associated with both sub-acute and chronic fatigue. These include reduced activity, all or nothing behaviour, negative perfectionism and beliefs of a prolonged, serious illness prognosis (Candy et al., Citation2003; Cope et al., Citation1994; Moss-Morris et al., Citation2011; White et al., Citation2001).
Models of persistent fatigue in a number of diseases have also identified risk factors that can be differentiated in accordance with a temporal course. These include human immuno deficiency virus (HIV), breast cancer, arthritis and multiple sclerosis. Similarly, they all recognise biological processes that initially trigger fatigue but suggest that additional psychological, social and behavioural factors maintain fatigue once triggered. Hughes et al. (Citation2020), provide a good example of a biopsychosocial model for HIV-related fatigue. Given the overlap of risk factors in both post-infectious and condition-specific fatigue models, it is reasonable to assume they also apply to the possible development of fatigue following covid-19 infection.
Other somatic symptoms that are known to persist following infections such as norovirus and campylobacter include the GI symptoms of irritable bowel syndrome (IBS) (Spiller & Garsed, Citation2009). The developmental course of post-infectious IBS is also understood to be initially triggered by infection but maintained by social, psychological and behavioural factors. These include prolonged duration of initial infection, toxicity of infection, mucosal inflammation, high levels of perceived stress, negative illness beliefs, all or nothing behaviour, anxiety and depression (Moss-Morris et al., Citation2011; Spiller & Garsed, Citation2009). GI symptoms are not as widely reported as other acute covid-19 symptoms such as fever and cough. However, where they are identified there is risk of prolonged infection duration, as they may present before respiratory distress and can mimic other GI disorders such as inflammatory bowel disease (IBD) (Smyk et al., Citation2020).
PTSD is also a known risk factor for the development of persistent somatic symptoms (Afari et al., Citation2014). However, there is no mention of somatic symptoms in relation to covid-19 related PTSD. Boyraz and Legros (Citation2020) warn PTSD could develop following exposure to stressful lockdown/quarantine conditions, bereavement, anxiety about, as well as infection with covid-19 and ICU admission. Health professionals working in ICU are also vulnerable. Given that people are 2.7 times more likely to develop persistent somatic symptoms following exposure to trauma, we expect a synonymous increase in SSD (Afari et al., Citation2014).
We are now learning more about covid-19 and its long-term impact. The term “long covid” has been coined to describe symptoms such as breathlessness, fatigue and joint pain that last for months after the initial infection has subsided (Nabavi, Citation2020). People who have “long covid” are also known as “long-haulers” and report their daily functioning is impaired, with some unable to return to work and resume their previously active lifestyles. It is important to identify and classify these symptoms to facilitate management and treatment. However, the term “long hauler” may be doing more damage than good. It implies a serious, chronic disease timeline and identity. Perceptions of serious illness consequences and prolonged recovery beliefs are risk factors for sub-acute and chronic fatigue (Candy et al., Citation2003; Moss-Morris et al, Citation2011). An empirically driven and operationally defined diagnosis that is recognised by healthcare services, employers and government agencies could counter the development of a “chronic illness” identity which may not be helpful. Appropriate diagnostic criteria could also facilitate appropriate rehabilitative care and support (NIHR, Citation2020).
The acute phases of covid-19 infection have involved stays in ICU with bed rest and for some this has been prolonged. Previously, patients with acute lung injury have developed muscle weakness during ICU treatment associated with substantial impairments in physical function beyond 24 months (Fan et al., Citation2014). Covid-19 patients may also be at risk from such long-term complications. Acute and post multi-disciplinary rehabilitation in hospitals and respiratory units may be effective for prevention of post-infectious fatigue and other symptoms (Ahmed et al., Citation2020). Educational interventions to limit bed rest and gradually increase activity have demonstrated effectiveness in reducing post-infectious fatigue associated with EBV (Candy et al., Citation2004). Similar interventions may therefore help medium to long term prevention of fatigue beyond the acute stages of covid-19 infection. Evidence-based treatments for fatigue and other persistent somatic symptoms are also well established and moderately effective. Cognitive behavioural therapy (CBT) demonstrates some of the strongest evidence for SSD (van Dessel et al., Citation2014). CBT is recommended as part of multidisciplinary treatment for high risk patients with SSD, whereas, low to moderate risk cases can be managed in primary care with a stepped-care disease management approach (van der Feltz-Cornelis et al., Citation2012). The SSD scale (SSD-12) demonstrates good psychometric properties and may assist clinicians with diagnosis and assessment (Toussaint et al., Citation2017). In the UK, persistent somatic symptoms are now managed in a stepped-care approach that includes the primary care based Improving Access to Psychological Therapies (IAPT) programme (McCrae et al., Citation2015), with step up referrals to secondary and tertiary care multi-disciplinary services (Chalder & Willis, Citation2017).
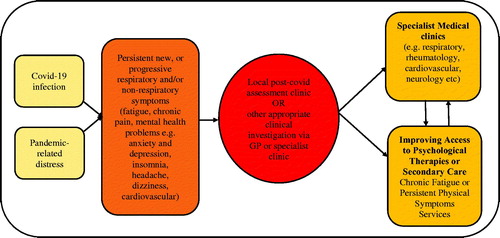
At the primary care level, General Practitioners (GP’s) will be the first port of call for most people experiencing persistent covid-19 symptoms, whether post-infectious or in relation to pandemic distress. GP’s could provide simple advice and self-help materials that target balancing activity and rest, sleep hygiene and anxiety management. At the secondary care level, a network of covid-19 rehabilitation clinics are being set up (NHS England & NHS Improvement London COVID-19, 2020). Multi-disciplinary care pathways for people who have been infected with covid-19 are advised. However, a greater number of people may be at risk of persistent symptoms due to pandemic-related distress. We recommend additional guidance and care pathways (see ).
Figure 1. Covid-19 related persistent physical symptoms care pathways (adapted from NHS England and NHS Improvement London, 2020).
The relationship between risk of SSD and covid-19 remains speculative. However, a good case definition or working diagnosis is needed, with multidisciplinary contribution including patient and public involvement (NIHR, Citation2020). Biopsychosocial models for persistent physical symptoms that move beyond dualistic concepts of illness, such as those described for fatigue could provide a plausible explanation for “long covid” and guide interventions (Chalder & Willis, Citation2018). For example, all or nothing approaches to activity (booming and busting) and marked health anxiety, although understandable responses, can exacerbate and perpetuate symptoms such as fatigue and pain that are characteristic of “long covid”. Biopsychosocial models can also account for the “long covid” experience of symptoms arising in one physiological system, which then abate only to rise in a different system (NIHR, Citation2020). Essentially, they provide a parsimonious route to the recognition that persistent multi-system symptoms can be produced by the interaction of physiological, cognitive, behavioural, emotional and social factors.
Future research might consider adequately powered, prospective designs to track a possible temporal course of somatic symptoms. Samples of covid-19 infected, covid-19 anxious and healthy subjects could be compared. Outcome evaluation will depend on the inclusion of reliable covid-19 testing at baseline and suitable follow up time points. Validated, generic measures such as the PHQ15 (Kroenke et al., Citation2002) can capture a range of somatic symptoms and measures of fatigue (Cella & Chalder, Citation2010) could track fluctuations in specific symptoms. In addition, measurement of relevant biological inflammatory markers such as CD4, CD8, IL-6 as well as psychosocial factors would provide understanding of contributing processes across time. Randomised controlled trials are needed to evaluate specific interventions designed to target covid-19 related SSD. Subsequently, mechanisms of change and moderator analyses would further our understanding of how approaches work and for whom (Hofmann & Hayes, Citation2019; Windgassen et al., Citation2016).
Acknowledgements
Trudie Chalder acknowledges the financial support of the Department of Health via the National Institute for Health Research (NIHR) Specialist Biomedical Research Centre for Mental Health award to the South London and Maudsley NHS Foundation Trust (SLaM) and the Institute of Psychiatry at King’s College London. The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Disclosure statement
Trudie Chalder has authored self-help books on chronic fatigue and received royalties.
References
- Afari, N., Ahumada, S., Wright, L., Mostoufi, S., Golnari, G., Reis, V., & Cuneo, J. (2014). Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosomatic Medicine, 76 (1), 2–11. https://doi.org/https://doi.org/10.1097/PSY.0000000000000010
- Ahmed, H., Patel, K., Greenwood, D. C., Halpin, S., Lewthwaite, P., Salawu, A., Eyre, L., Breen, A., O’Connor, R., Jones, A., & Sivan, M. (2020). Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. Journal of Rehabilitation Medicine, 52(5), jrm00063.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. (5th ed.). APA.
- Berelowitz, G., Burgess, A., Thanabalasingham, T., Murray-Lyon, I., & Wright, D. (1995). Post-hepatitis syndrome revisited. J Viral Hepat, 2(3), 133–138. https://doi.org/https://doi.org/10.1111/j.1365-2893.1995.tb00018.x
- Boyraz, G., & Legros, D. (2020). Coronavirus Disease (COVID-19) and traumatic stress: Probable risk factors and correlates of posttraumatic stress disorder. Journal of Loss and Trauma, 25(6–7), 503–522. https://doi.org/https://doi.org/10.1080/153024.2020.1763556
- Byrne, L., & Wykes, T. (2020). A role for lived experience mental health leadership in the age of Covid-19. Journal of Mental Health, 29(3), 243–246. https://doi.org/https://doi.org/10.1080/09638237.2020.1766002
- Candy, B., Chalder, T., Cleare, A., Peakman, A., Skowera, A., Wessely, S., Weinman, J., Zuckerman, M., & Hotopf, M. (2003). Predictors of fatigue following the onset of infectious mononucleosis. Psychological Medicine, 33(5), 847–855. https://doi.org/https://doi.org/10.1017/s0033291703007554
- Candy, B., Chalder, T., Cleare, A., Wessely, S., & Hotopf, M. (2004). A randomised controlled trial of a psycho-educational intervention to aid recovery in infectious mononucleosis. Journal of Psychosomatic Research, 57(1), 89–94. https://doi.org/https://doi.org/10.1016/S0022-3999(03)00370-2
- Carfì, A., Bernabei, R., & Landi, F. (2020). Persistent symptoms in patients after acute COVID-19. JAMA, 324(6), 603–605. https://jamanetwork.com/journals/jama/fullarticle/2768351 https://doi.org/https://doi.org/10.1001/jama.2020.12603
- Cella, M., & Chalder, T. (2010). Measuring fatigue in clinical and community settings. Journal of Psychosomatic Research, 69(1), 17–22. https://doi.org/https://doi.org/10.1016/j.jpsychores.2009.10.007
- Centres for Disease Control and Prevention (CDC). (2012). CFS case definition. Retrieved June 22, 2020, from http://www.cdc.gov/cfs/case-definition/index.html.
- Chalder, T. (2005). Chronic fatigue syndrome: Focus on the provider of care rather than the consumer. Journal of Mental Health, 14(3), 209–211. https://doi.org/https://doi.org/10.1080/09638230500136522
- Chalder, T., & Willis, C. (2017). lumping” and “splitting” medically unexplained symptoms: Is there a role for a transdiagnostic approach? Journal of Mental Health, 3, 187–191.
- Chalder, T., & Willis, C. (2018). Medically unexplained symptoms. In Ayers, S., Llewellyn, C., McManus, C., Newman, S., Petrie, K., Revenson, T, Weinman, J. (eds.), Cambridge handbook of psychology, health and medicine (3rd ed.). Cambridge University Press.
- Colizzi, M., Bortoletto, R., Silvestri, M., Mondini, F., Puttini, E., Cainelli, C., Gaudino, R., Ruggeri, M., & Zoccante, L. (2020). Medically unexplained symptoms in the times of Covid-19 pandemic: A case-report. Brain, Behaviour and Immunity – Health, 5, 100073. https://doi.org/https://doi.org/10.1016/j.bbih.2020.100073
- Cope, H., David, A., Pelosi, A., & Mann, A. (1994). Predictors of chronic ‘postviral’ fatigue. Lancet, 344(8926), 864–868. https://doi.org/https://doi.org/10.1016/S0140-6736(94)92833-9
- Deary, V. (2005). Explaining the unexplained? Overcoming the distortions of a dualist understanding of medically unexplained illness. Journal of Mental Health, 14(3), 213–221. https://doi.org/https://doi.org/10.1080/09638230500136605
- Fan, E., Dowdy, D. W., Colantuoni, E., Mendez-Tellez, P. A., Sevransky, J. E., Shanholtz, C., Himmelfarb, C. R. D., Desai, S. V., Ciesla, N., Herridge, M. S., Pronovost, P. J., & Needham, D. M. (2014). Physical complications in acute lung injury survivors: A two-year longitudinal prospective study. Critical Care Medicine, 42(4), 849–859. https://doi.org/https://doi.org/10.1097/CCM.0000000000000040
- Hofmann, S., & Hayes, S. (2019). The future of intervention science: Process-based therapy. Clinical Psychological Science: A Journal of the Association for Psychological Science, 7(1), 37–50. https://doi.org/https://doi.org/10.1177/2167702618772296
- Hotopf, M., Noah, N., & Wessely, S. (1996). Chronic fatigue and minor psychiatric morbidity after viral meningitis: A controlled study. Journal of Neurology, Neurosurgery, and Psychiatry, 60(5), 504–509. https://doi.org/https://doi.org/10.1136/jnnp.60.5.504
- Hu, Y., Sun, J., Dai, Z., Deng, H., Li, X., Huang, Q., Wu, Y., Sun, L., & Xu, Y. (2020). Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. Journal of Clinical Virology: The Official Publication of the Pan American Society for Clinical Virology, 127, 104371. https://doi.org/https://doi.org/10.1016/j.jcv.2020.104371
- Hughes, A., Campbell, L., Graham, H., Post, F., & Chalder, T. (2020). A biopsychosocial approach to HIV fatigue: A cross-sectional and prospective analysis to identify key modifiable factors. Behavioural Medicine. Advance online publication. https://doi.org/https://doi.org/10.1080/08964289.2020.1712582
- ICD-11 for Mortality and Morbidity Statistics (ICD-11 MMS). Version 09/2020 (2020). Retrieved Accessed October 16, from https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f767044268
- Jia, R., Ayling, K., Chalder, T., Massey, A., Broadbent, E., Coupland, C., & Vedhara, K. (2020). Mental health in the UK during the COVID-19 pandemic: Cross-sectional analyses from a community cohort study. BMJ Open, 10(9), e040620. https://doi.org/https://doi.org/10.1136/bmjopen-2020-040620
- Kroenke, K., Spitzer, R., & Williams, J. (2002). The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine, 64(2), 258–266. https://doi.org/https://doi.org/10.1097/00006842-200203000-00008
- Kumar, A., & Rajasekharan Nayar, K. (2020). COVID 19 and its mental health consequences. Journal of Mental Health. Advance online publication. https://doi.org/https://doi.org/10.1080/09638237.2020.1757052
- Lam, M. H.-B., Wing, Y.-K., Yu, M. W.-M., Leung, C.-M., Ma, R. C. W., Kong, A. P. S., So, W. Y., Fong, S. Y.-Y., & Lam, S.-P. (2009). Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: Long-term follow-up. Archives of Internal Medicine, 169(22), 2142–2147. https://doi.org/https://doi.org/10.1001/archinternmed.2009.384
- Lima, C., Carvalho, P., Lima, I., Nunes, J., Saraiva, J., de Souza, R., da Silva, C., & Neto, M. (2020). The emotional impact of Coronavirus 2019-nCoV (New Coronavirus Disease). Psychiatry Research, 287, 112915. https://doi.org/https://doi.org/10.1016/j.psychres.2020.112915
- Lu, R., Zhao, X., Li, J., Niu, P., Yang, B., Wu, H., Wang, W., Song, H., Huang, B., Zhu, N., Bi, Y., Ma, X., Zhan, F., Wang, L., Hu, T., Zhou, H., Hu, Z., Zhou, W., Zhao, L., … Tan, W. (2020). Genomic characterisation and epidemiology of 2019 Novel Coronavirus: Implications for virus origins and receptor binding. Lancet, 395(10224), 565–574. https://doi.org/https://doi.org/10.1016/S0140-6736(20)30251-8
- Luo, M., Guo, L., Yu, M., Jiang, W., & Wang, H. (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – A systematic review and meta-analysis. Psychiatry Research, 291, 113190. https://doi.org/https://doi.org/10.1016/j.psychres.2020.113190
- McCrae, N., Correa, A., Chan, T., Jones, S., & Lusignan Simon, d. (2015). Long-term conditions and medically-unexplained symptoms: Feasibility of cognitive behavioural interventions within the improving access to Psychological Therapies Programme. Journal of Mental Health, 24(6), 379–384. 6, https://doi.org/https://doi.org/10.3109/09638237.2015.1022254
- Moreno, C., Wykes, T., Galderisi, S., Nordentoft, M., Crossley, N., Jones, N., Cannon, M., Correll, C. U., Byrne, L., Carr, S., Chen, E. Y. H., Gorwood, P., Johnson, S., Kärkkäinen, H., Krystal, J. H., Lee, J., Lieberman, J., López-Jaramillo, C., Männikkö, M., … Arango, C. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet. Psychiatry, 7(9), 813–824. https://doi.org/https://doi.org/10.1016/S2215-0366(20)30307-2
- Moss-Morris, R., Spence, M., & Hou, R. (2011). The pathway from glandular fever to chronic fatigue syndrome: Can the cognitive behavioural model provide the map? Psychological Medicine, 41(5), 1099–1107. https://doi.org/https://doi.org/10.1017/S003329171000139X
- Nabavi, N. (2020). Long covid: How to define it and how to manage it. BMJ, 370, m3489. https://doi.org/https://doi.org/10.1136/bmj.m3489
- NHS England and NHS Improvement London COVID-19. (2020). Guidance for the commissioning of clinics for recovery and rehabilitation. Retrieved October 6, 2020, from https://s31836.pcdn.co/wp-content/uploads/COVID-19-Guidance-for-the-commissioning-of-clinics-for-recovery-and-rehabilitation-version-1-for-release_.pdf
- NIHR. (2020). Living with Covid-19. Retrieved October 16, 2020, from https://evidence.nihr.ac.uk/themedreview/living-with-covid19/
- Rogers, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P., Fusar-Poli, P., Zandi, M. S., Lewis, G., & David, A. S. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infection: A systematic review and meta-analyses with comparison to the COVID-19 pandemic. The Lancet. Psychiatry, 7(7), 611–627. https://doi.org/https://doi.org/10.1016/S2215-0366(20)30203-0
- Shevlin, M., Nolan, E., Owczarek, M., McBride, O., Murphy, J., Gibson Miller, J., Hartman, T., Levita, L., Mason, L., Martinez, A., McKay, R., Stocks, T., Bennett, K., Hyland, P., & Bentall, R. (2020). COVID‐19‐related anxiety predicts somatic symptoms in the UK population. British Journal of Health Psychology, 25(4), 875–882. https://doi.org/https://doi.org/10.1111/bjhp.12430
- Smyk, W., Janik, M., Portincasa, P., Milkiewicz, P., Lammert, F., & Krawczyk, M. (2020). COVID-19: Focus on the lungs but do not forget the gastrointestinal tract. European Journal of Clinical Investigation, 50(9), 13276. https://doi.org/https://doi.org/10.1111/eci.13276
- Spiller, R., & Garsed, K. (2009). Post infectious irritable bowel syndrome. Gastroenterology, 136(6), 1979–1988. https://doi.org/https://doi.org/10.1053/j.gastro.2009.02.074
- Toussaint, A., Löwe, B., Brähler, E., & Jordan, P. (2017). The somatic symptom disorder – B criteria scale (SSD-12): Factorial structure, validity and population-based norms. Journal of Psychosomatic Research, 97, 9–17. https://doi.org/https://doi.org/10.1016/j.jpsychores.2017.03.017
- van der Feltz-Cornelis, C., Hoedeman, R., Keuter, E., & Swinkels, J. (2012). Presentation of the multidisciplinary guideline Medically Unexplained Physical Symptoms (MUPS) and somatoform disorder in the Netherlands: Disease management according to risk profiles. Journal of Psychosomatic Research, 72(2), 168–169. https://doi.org/https://doi.org/10.1016/j.jpsychores.2011.11.007
- Van Dessel, N., Den Boeft, M., & Van der Wouden, J. (2014). Non-pharmacological interventions for somatoform disorders and medically unexplained physical symptoms (MUPS) in adults. The Cochrane Database of Systematic Reviews, 01 (11), CD011142.
- White, P. D., Thomas, J. M., Kangro, H. O., Bruce-Jones, W. D., Amess, J., Crawford, D. H., Grover, S. A., & Clare, A. W. (2001). Predictions and associations of fatigue syndromes and mood disorders that occur after infectious mononucleosis. Lancet, 358(9297), 1946–1954. https://doi.org/https://doi.org/10.1016/S0140-6736(01)06961-6
- Windgassen, S., Goldsmith, K., Moss-Morris, R., & Chalder, T. (2016). Establishing how psychological therapies work: The importance of mediation analysis. Journal of Mental Health, 25(2), 93–99. https://doi.org/https://doi.org/10.3109/09638237.2015.1124400
- Yao, H., Chen, J.-H., & Xu, Y.-F. (2020). Patients with mental health disorders in the Covid-19 epidemic. The Lancet. Psychiatry, 7(4), e21. https://doi.org/https://doi.org/10.1016/S2215-0366(20)30090-0
- Yifan, T., Ying, L., Chunhong, G., Jing, S., Rong, W., Zhenyu, L., Zejuan, G., & Peihung, L. (2020). Symptom Cluster of ICU nurses treating COVID-19 pneumonia patients in Wuhan. China. Journal of Pain Symptom Management, 60(1), e48–e53. https://doi.org/https://doi.org/10.1016/j.jpainsymman.2020.03.039
