Abstract
Background
The current moment is characterised by deep-rooted uncertainties, such as climate change and COVID-19. Uncertainty has been reported to be associated with negative mental health outcomes, such as stress and anxiety. However, no comprehensive review on the association between uncertainty and mental health exists.
Aim
The aim of the current scoping review was to systematically explore and describe the literature on the link between uncertainty and mental health.
Methods
A scoping review was undertaken following guidelines by Arksey and O’Malley (2005).
Results
One hundred and one papers addressing the association between uncertainty and mental health were identified. Most were cross-sectional studies (67%) conducted in the fields of medicine or nursing (59%), in high-income countries, among adult populations (74%), and in medical settings. Substantial heterogeneity was identified in the measurements of uncertainty and mental health. Most studies (79%) reported a positive association between uncertainty and mental health problems.
Conclusions
Research is needed in more diverse contexts and populations. More robust designs are required to provide insight into the directionality and strength of the association between uncertainty and mental health. Few studies reported how individuals coped with uncertainty. Future studies should address the identified gaps and investigate interventions to address uncertainty and its determinants.
Keywords:
Introduction
The current global scenario is being described as one characterized by systemic and deep-rooted uncertainties. Uncertainty has been identified as a defining characteristic of modernity (Bauman, Citation2007; Muggah & Goldin, Citation2019), with economist Barry Eichengreen arguing that we are living in an “age of hyper-uncertainty” (Eichengreen, Citation2016). Climate change, the rise in armed conflict and natural hazards, displacement and large flows of refugees, and austerity, are all believed to contribute to triggering widespread uncertainty at the individual, communal, and societal levels (Cange et al., Citation2019; Moloney et al., Citation2014). Currently, the COVID-19 pandemic has further exacerbated pre-existing uncertainties and generated new ones, with media outlets going as far as talking of a “pandemic of uncertainty” (Rogoff, Citation2020).
Uncertainty is often referred to as a trigger for several negative mental health outcomes, such as stress (Greco & Roger, Citation2003) and anxiety (Grupe & Nitschke, Citation2013). Recently, this narrative has been particularly evident in the context of COVID-19. The World Health Organization’s page on mental health and COVID-19 states that “fear, worry, and stress are normal responses […] at times when we are faced with uncertainty or the unknown” (WHO, 2020). Self-help articles with tips on how to deal and cope with uncertainty have boomed in recent months, both in the popular media (HelpGuide, Citation2020; Thomson, Citation2020), as well as within national health services (NHS, Citation2020) and professional mental health organizations (APA, Citation2020; BACP, Citation2020).
Never before has the link between uncertainty and mental health been more central in public and academic discourses. Yet, there is little systematic evidence concerning the link between uncertainty and mental health (Anderson et al., Citation2019). Furthermore, it is not yet clear what types of uncertainty have been investigated, in relation to what kind of uncertainty-generating events, and among which populations. There is also a need to clarify which kind of psychiatric and psychosocial issues have been addressed and whether any specific coping mechanisms to manage uncertainty have been identified. To be able to provide adequate clinical and social support to people whose mental health is negatively impacted by uncertainty, it is crucial to systematically investigate what causes uncertainty, how uncertainty affects mental health and well-being, what coping mechanisms are available to people and their families, and what support can be offered to improve mental health and well-being. Initiated before the COVID-19 pandemic, the rationale for this review was to systematically explore and characterize the quantitative literature on the association between uncertainty and mental health to critically investigate the effects of uncertainty on mental health and to make recommendations for research, policy, and practice.
Uncertainty and mental health
The definitions of uncertainty vary and include a state taking place when “details of the situation are ambiguous, complex, unpredictable, or probabilistic; when information is unavailable or inconsistent; and when people feel insecure in their own state of knowledge or the state of knowledge in general” (Brashers, Citation2001, p. 478). Other definitions include uncertainty as a state characterized by lack of control (Afifi et al., Citation2014), by an incapacity to foresee future outcomes (Penrod, Citation2007), by entropy and disorder (Hirsh et al., Citation2012), or by the inability to determine the meaning of an event (Mishel, Citation1988).
The term uncertainty has often been used interchangeably with similar, albeit conceptually distinct, terms such as “ambiguity” and “risk” (Wakeham, Citation2015), contributing further to the instability of the concept. The likely cause for this complexity and diversity of definitions is in part due to the use of the term across a variety of disparate fields for different purposes, ranging from behavioural economics (Tversky & Kahneman, Citation1974) and communication studies (Afifi & Afifi, Citation2016), to mental health sciences (Grupe & Nitschke, Citation2013) and medical disciplines (Szulczewski et al., Citation2017). The current heterogeneous conceptualisations of uncertainty represent a challenge as slightly distinct constructs are being addressed under the same term. This is predicted to lead to poor operationalisation in measurement, lack of clarity concerning appropriate definitions, and difficulty in generalising findings across different disciplines.
Research from various disciplines has shown that uncertainty is an experience associated with worsened mental health across various populations (Phillimore & Cheung, Citation2021; Santacroce, Citation2003; Stewart & Mishel, Citation2000; Wu et al., Citation2020). One of the most popular early models of stress and coping suggested that appraising a situation as uncertain can lead to an increase in perceived stress and inhibit effective coping (Lazarus & Folkman, Citation1984), therefore linking stress and uncertainty together. Since then, several strands of research have investigated the impact that different types and degrees of uncertainty can have on mental health. For instance, experimental evidence suggests that humans and other mammals display intrinsic aversive reactions when exposed to uncertainty (de Berker et al., Citation2016). Some research has found uncertainty to be positively associated with higher rates of mental health problems in relation to a variety of psychiatric conditions, such as depression (Sharkey et al., Citation2018), anxiety disorders (Tarhani et al., Citation2020) and post-traumatic stress disorder (PTSD) (Moreland & Santacroce, Citation2018). Additionally, uncertainty has been linked to a worsening of several psychosocial outcomes, such as quality of life (Niv et al., Citation2017), psychological distress (Hoff et al., Citation2002), and psychosocial adjustment (Mauro, Citation2008).
However, this conceptualisation of uncertainty as intrinsically pathogenic has also been the object of criticism (Schiltz et al., Citation2019), with Mishel’s theory of uncertainty in illness (Mishel, Citation1988) highlighting how, depending on the context, uncertainty can be appraised not only as a threat but also as an opportunity. Indeed, some authors have failed to find a relationship between uncertainty and poor mental health (Arroll et al., Citation2012), and some have even found an association with certain positive psychosocial variables, such as hope (Gill & Morgan, Citation2011) or argued that uncertainty can allow people to remain optimistic in the face of adversity (Brashers, Citation2001).
Despite these insights, the relationship between uncertainty and mental health remains ambiguous as no comprehensive review of the literature has been conducted to capture the association between these two constructs. Evidence collected through this scoping review will result in an important contribution at both research and implementation levels and contribute to filling this gap in knowledge. Firstly, it will allow us to identify important gaps in the literature and shed light on possible mechanisms behind the association between uncertainty and mental health. Secondly, we will be able to highlight possible issues and incongruencies in the conceptualisation, operationalisation, and measurement of the construct. Finally, considering the dearth of interventions targeted at managing uncertainty, providing a systematic overview of the extant literature represents an important benchmark for future implementation work and more targeted research on the political, social, and economic determinants of poor mental health.
Methods
This scoping review forms part of a larger mixed-methods research project investigating the experience of uncertainty and its link to mental health in the occupied Palestinian territory. The aim is to develop, pilot, and validate a relevant metric for uncertainty that takes into consideration local realities and experiences. To gain an overview of the existing evidence-base, it was considered appropriate to conduct a scoping review to take into account the heterogeneous nature of the literature as well as our exploratory research question (Colquhoun et al., Citation2014). Indeed, scoping reviews have been defined as “exploratory projects that systematically map the literature available on a topic, identifying key concepts, theories, sources of evidence, and gaps in the research” (Candian Institutes of Health Research, Citation2010).
We followed the methodological recommendations for conducting a scoping review as outlined by Arksey and O’Malley (Citation2005) and by the Joanna Briggs Institute manual for scoping reviews methodology (Peters et al., Citation2015). The methodological framework proposed by Arksey and O’Malley (Citation2005) identifies five different stages when conducting a scoping review: (i) Identifying the research question; (ii) Identifying relevant studies; (iii) Study selection; (iv) Charting the data; and (v) Collating, summarizing, and reporting the results. The five different stages are reported below. A protocol was produced for internal use but was not submitted to PROSPERO due to PROSPERO not accepting to date protocols for scoping reviews.
Identifying the research question
Through preliminary engagement with key literature and discussion among team members on the conceptualization and characteristics of uncertainty, we identified the main objective of the review as that of mapping the available evidence on the link between uncertainty and mental health. To address this main objective, six different related research questions were identified:
Among which populations has the association between uncertainty and mental health been studied?
What is the reported event/entity that generated uncertainty in which populations?
How is uncertainty measured?
What is the mental health outcome under investigation?
What is the direction of the relationship between uncertainty and mental health?
What are the coping mechanisms to deal with uncertainty reported in the literature?
Identifying relevant studies
The current scoping review identified, selected, and evaluated evidence from peer-reviewed articles that examined the association between uncertainty and mental health. Following the Joanna Briggs Institute manual for conducting scoping reviews, we conducted a first broad, unstructured search to identify key literature on the association between uncertainty and mental health. Familiarization with these key papers allowed for a narrowing of the research questions and informed the structured search strategy. In the structured search, we focused on studies published between 2000 and 2018 and published in English. Key papers identified using the first unstructured search published before 2000 were still noted down to be used for the introduction and discussion sections to provide a wider and more accurate representation of the field.
We searched five different databases (i.e., MEDLINE, PubMed, PsycINFO, EMBASE, and EBSCO Global Health). The structured search took place between September and October 2018. An example of the search strategy used on the PubMed database is shown in Supplementary Appendix 1.
This search strategy was applied across the five different databases. As suggested by the Joanna Briggs Institute manual (2015), in addition to the systematic search on databases, we also identified relevant literature through hand searches of reference lists of included studies and of other key references to keep the search strategy broad. Furthermore, although included in the search terms, we ended up excluding findings that only focused on quality of life due to the specific focus of the current review on mental health and because of the high number of studies identified.
Selecting studies
We undertook two different stages of study selection: 1. Screening title and abstract and 2. Full-text screening. Across these screenings we applied the following exclusion criteria:
Study did not focus on uncertainty. We excluded studies focusing on related but distinct concepts, such as risk or insecurity,Footnote1 and those focusing on the intolerance of uncertainty construct
Study did not focus on mental health
Study did not focus on the association between uncertainty and mental health
Study was not peer-reviewed (e.g., conference abstracts or unpublished thesis)
Study was not quantitative
Study was not in English
Study was published before 2000
Study subjects were not human (i.e., animal studies)
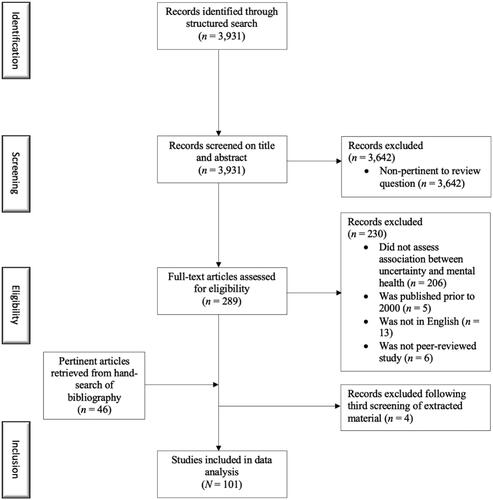
summarizes the selection process. The initial quantitative database search yielded 3931 articles. A total of 289 were retained following the initial screening of abstract and title (93% of studies were removed following initial screening). The 289 retained articles underwent a second full-text screening. A total of 59 articles were retained following the second full-text screening (80% of studies removed). All screening was conducted blindly by two different researchers and discrepancies were highlighted, discussed, and resolved. Bibliographies of all accepted studies were hand-searched for relevant literature that had been omitted by the structured search. This led to the inclusion of 46 relevant articles. Due to the ambiguity inherent in the construct of uncertainty, a third and final screening of the extracted material was conducted to confirm the inclusion of the paper after data extraction. This final screening was conducted blindly by two authors and focused on whether the paper had clearly measured uncertainty (vs. only mentioning it in passing at the introduction or discussion stages) and had linked it to a mental health variable(s). Discrepancies between the two researchers were discussed until an agreement was reached and 4 papers were excluded. The final number of accepted studies was therefore 101. All references for included studies are reported in Supplementary Appendix 2.
Charting the data
A data charting sheet was created to extract data relevant to our question. Various versions of different charting sheets were tested before reaching consensus on a final version. Two researchers independently tested the final data charting sheet on 10 randomly selected papers. Data charting sheets for each paper were then compared to ensure consistency in the data extraction procedure. All articles went through a double charting process undertaken separately by two different reviewers. Discrepancies between the information extracted were highlighted, discussed, and resolved. All extracted data from the charting sheets was transferred to a Google sheet for synthesis. The final version of the data charting sheet is reported in Supplementary Appendix 3 and includes all the data points that were extracted for the current review.
To address the question concerned with the association between uncertainty and mental health problems we categorized each study based on the directionality of the statistical relationship between the uncertainty variable and the mental health variable. Each study could be categorized as positive (i.e., positive association between uncertainty and mental health problems), negative (i.e., negative association between uncertainty and mental health problems), mixed (i.e., different analyses reported different types of directionality), or non-significant (i.e., the association was not statistically significant).
Collating, summarizing, and reporting the results
A narrative review approach (Courtin & Knapp, Citation2017) was used to synthesize and report the results. When the outcome was numerical (e.g., mean sample size across studies, mean gender distribution across studies), descriptive statistics were calculated to provide a general estimate across studies. When calculating percentages, decimals were rounded to the closest whole number. For more qualitative information (e.g., type of population, type of uncertainty-generating event/entity, reported coping mechanisms), a narrative approach was taken by categorizing under themes generated by the authors the different studies and results reported in a narrative form. This allowed us to capture numerical data and also provide an account of data that was not quantifiable.
Results
Descriptive information on studies
The vast majority of papers reviewed consisted of original research studies entailing the collection of primary data (91%) (see ). Original research studies were followed by review articles (6%) and by a smaller number of papers using secondary datasets (2%) and theoretical papers or commentaries (1%). A cross-sectional design was most commonly used in the reviewed studies (67%) (see ). A substantial number of other studies used a longitudinal design (14%) followed by psychometric assessment studies (8%), experimental studies (2%), intervention studies (2%), and one case-control study (1%).
Table 1. Descriptive information on studies.
More than half of the reviewed studies came from the fields of medicine or nursing (59%) (see ). A considerable percentage of studies also belonged to the fields of medicine and/or nursing but included authors or elements from the field of psychology (23%). One in every ten studies (11%) belonged to the fields of psychology, psychiatry, or neuroscience. Finally, a smaller number of studies were interdisciplinary studies from medicine and nursing as well as public health (4%) or the social sciences (3%).
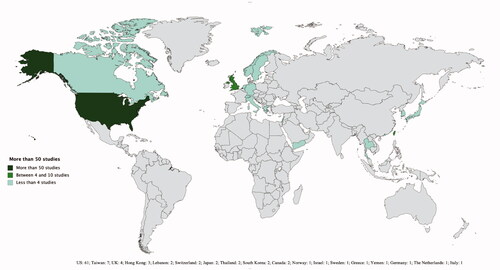
The geographical location where studies have been conducted is shown graphically in . The overwhelming majority of studies came from the United States (n = 61). The next countries for number of studies were Taiwan with seven studies and the United Kingdom with four studies. The remaining countries had from 1 to 3 studies. Most studies were concentrated in high-income countries, with some exceptions (e.g., Lebanon, Yemen, and Thailand). The geographical location of the first authors generally mirrored the geographical location of where studies had been conducted.
Among which populations has the association between uncertainty and mental health been studied?
The mean sample size across primary studies was 201 with a median of 120 participants per study. In terms of gender distribution, across original studies, the median percentage of female participants was 60% with 8 studies focusing only on men and 14 studies focusing only on women. This was often due to the focus of the study being on medical conditions more likely to take place in one sex, such as breast cancer. In terms of age distribution, the majority of original studies focusedFootnote2 on adults (18–65 years old) (74%), with a substantial number of studies focusing on children and adolescents (<18 years old) (20%) and a minority of studies focusing on older adults (>65 years old) (6%). In most studies, CaucasianFootnote3 participants were the most represented (i.e., highest percentage of total participants) ethnicity (52%), followed by Chinese participants (4%), African American participants (4%), and Taiwanese participants (2%). A significant number of studies (31%) did not report the ethnicity of their participants.
What is the reported event/entity that generated uncertainty in which populations?
Uncertainty was investigated in three different settings: (1) the medical setting; (2) disaster and conflict settings; and (3) the occupational and university settings.
Most studies focused on medical settings (n = 92) with 58 focusing on patients, 27 on carers, and seven on health professionals. The patient profile (n = 58) was very diverse featuring individuals with cancer, other non-communicable diseases, infectious diseases, high-risk pregnancies, undergoing genetic counselling, organ transplants, and receiving implanted devices. The main factor generating uncertainty was their illness. Specifically, individual studies highlighted particular uncertainties connected to treatment (n = 31), illness course (n = 15), symptoms (n = 14), prognosis (n = 12), their future (n = 10), diagnosis (n = 7), recurrence (n = 4), information (n = 4), interpersonal relationships (n = 4), life expectancy (n = 4), intensity and toxicity of treatment (n = 3), side effects of treatment (n = 3), and recovery (n = 2). Similarly, carers (n = 27) were mainly uncertain about the illness with some studies mentioning specifically treatment (n = 12), prognosis (n = 8), illness course (n = 8), information (n = 7), future (n = 6), symptoms (n = 5), life expectancy (n = 4), damaging effects of the illness (n = 2), diagnosis (n = 2), and care giving (n = 2).
Among health professionals, uncertainty was investigated among physicians (n = 4) and nurses (n = 3) all of whom felt uncertain about the medical context especially regarding decision making and diagnosing in the face of incomplete information, equipment, and tests. Physicians were particularly concerned with interpersonal relationships with patients and colleagues, misconduct, bad treatment outcomes, and patient referrals. Nurses, on the other hand, were worried about their perceived lack of experience, inadequate training, and insufficient support and guidance from physicians to make adequate treatment decisions and communicate health information to patients or families effectively.
Among the studies that focused on disaster or conflict settings (n = 4), three focused on uncertainty following natural and chemical hazards, and one focused on uncertainty in refugee settings. These studies generally reported two types of uncertainty. One is related to personal uncertainties, such as one’s future, livelihood, and the safety of oneself, one’s family members, and friends. The other is related to structural and macro-level issues, such as job insecurity, housing, and one’s country’s safety and future.
Among studies focusing on occupational and university settings (n = 4), uncertainty was explored with workers (n = 2) and students (n = 2). Uncertainty experienced by workers was related to workplace reorganization, job-related tasks, and the future of one’s job. Among students, one study focused on uncertainty generated experimentally while another study, conducted in Lebanon, reported that students felt uncertain about their future, safety, and health as well as their country’s security and future.
How is uncertainty measured?
Substantial heterogeneity was found in terms of uncertainty measurements with a total of 20 different measures used to operationalize the construct. The most commonly used measure was the Mishel Uncertainty in Illness Scale (MUIS) (Mishel, Citation1981) (45% of all measures used) in its various versions including Mishel Uncertainty in Illness Scale (n = 22), Mishel Uncertainty in Illness Scale-Community (n = 17), Mishel Uncertainty in Illness Scale-Brain Tumour (n = 2), Short-Form Mishel Uncertainty in Illness Scale (n = 1), and Mishel Uncertainty in Illness-Survivor Version (n = 1). The other most commonly used measures to capture uncertainty were the Parental Perceptions of Uncertainty Scale (Mishel, Citation1983) (18% of all measured used, n = 18) and the Child Uncertainty in Illness Scale (Mullins & Hartman, Citation1995) (9%, n = 9). Additionally, various studies (10%, n = 10) used ad hoc measurements of uncertainty, such as single questions or short questionnaires constructed only for the study (e.g., Rybarczyk et al., Citation2007). As a result of the predominance of the MUIS scale, the vast majority of uncertainty measures appeared as having been developed in the United States (92%) within the nursing discipline (86%). A smaller number of uncertainty measures had been developed within the field of psychology (11%).
What is the mental health outcome under investigation?
Several mental health and psychosocial outcomes were investigated in relation to uncertainty across the different studies. The various mental health outcomes and their overall presence across studies are shown in . The most commonly investigated mental health and psychosocial outcomes were depression (23%), anxiety (19%), psychological distress (15%), PTSD (10%), and stress (10%).
Table 2. Mental health and psychosocial outcomes investigated across studies.
The measurements used to capture the different mental health and psychosocial outcomes were very heterogeneous with a total of 48 different measurements used. The most commonly reported mental health measurements were the State-Trait Anxiety Inventory (Spielberger et al., Citation1983) (9%), the Children’s Depression Inventory (Kovacs, Citation1992) (9%), the Brief Symptom Inventory (Derogatis & Melisaratos, Citation1983) (8%), the Impacts of Events Scale (Weiss & Marmar, Citation1996) (7%), the Centre for Epidemiological Studies Depression Scale (Radloff, Citation1977) (6%), and the Profile of Mood States (McNair et al., Citation1971) (4%). All remaining scales (51%) were used <5 times. Additionally, several studies (6%) did not use standardized mental health scales but ad hoc measurements, such as single questions enquiring about mental health status. While measurements were heterogeneous, they overwhelmingly were developed in the United States (87%). Most of the measurements originated from the fields of psychology (45%) or psychiatry (26%).
What is the direction of the relationship between uncertainty and mental health?
A substantial majority of studies identified a positive relationship between higher levels of uncertainty and worst mental health outcomes (79%). However, some studies (15%) reported mixed findings, with analyses on certain mental health outcomes yielding positive associations with uncertainty levels, while analyses on other mental health outcomes in the same study resulted in negative or non-significant associations with uncertainty levels. Additionally, a small number of studies (6%) reported a non-significant statistical relationship between uncertainty and mental health.
What strategies to cope with uncertainty are reported?
The vast majority of original studies (82%) did not investigate how people coped with uncertainty. Only 17 studies out of the 94 studies that collected primary data (18%) reported coping mechanisms for uncertainty as a variable. The types of coping explored were heterogeneous including communal coping, emotive coping, problem-focused coping, spiritual coping, avoidance, re-appraisal, seeking information, social support, denial, and hope. The measurements used reflected this heterogeneity with each study using a different measurement of coping. As a result, no firm conclusion can be drawn concerning the link between coping with uncertainty and mental health.
Discussion
Summary and discussion of key findings
To our knowledge, this scoping review represents the first systematic attempt to describe the literature on the association between uncertainty and mental health across disciplines and populations. Several key findings can be highlighted from the review. Firstly, the majority of studies were published in the field of medicine and/or nursing and generally focused on uncertainty experienced by the patient in relation to their illness, treatment, and prognosis. This literature was largely influenced by the work of Mishel on uncertainty in illness (Mishel, Citation1988).
Secondly, the vast majority of the literature reviewed (79%) found a positive association between higher levels of uncertainty and mental health problems. Uncertainty was linked to several worsened mental health outcomes, in particular depression, anxiety, distress, PTSD, and stress. However, due to the over-reliance on a cross-sectional design, we cannot make firm claims concerning the directionality of this relationship, especially in light of the impact that mental health status can have on perceptions of uncertainty and possible inverse-causality concerns (Gentes & Ruscio, Citation2011).
Thirdly, despite a few exceptions (Afifi et al., Citation2013; Al-Dubai & Rampal, Citation2012), most of the literature was produced in and by authors from high-income countries, particularly the US (60% of all studies).
The current review also highlights several gaps and limitations in the literature. Firstly, there is a lack of evidence on coping mechanisms used to manage uncertainty with only a handful of studies assessing the association between different types of coping with uncertainty and mental health. This represents a substantial limitation as evidence from qualitative work highlights how people and communities are unlikely to experience uncertainty passively but rather draw on a variety of personal and social resources to manage and navigate uncertainty (Brown et al., Citation2020). These coping mechanisms are likely to moderate the relationship between uncertainty and mental health and could provide important insights on how to reduce the detrimental impact of uncertainty on mental health in various contexts. This becomes even more salient in light of the dearth of psychosocial interventions targeting uncertainty. While certain uncertainty management interventions have been tested in medical settings and have been shown to have a positive impact on mental health (Germino et al., Citation2013; Gil et al., Citation2006), the existing literature has overwhelmingly focused on characterising and quantifying the link between uncertainty and mental health rather than on exploring how to address this link in practice. Systematic research on interventions aimed at addressing uncertainty is therefore urgently needed in a diverse number of settings beyond the medical one.
An additional limitation identified concerns the large degree of heterogeneity in the measurements of both uncertainty and mental health in the reviewed literature with 20 different uncertainty measurements and 48 different mental health measurements identified across original studies. Given the notable exception of the Mishel Uncertainty in Illness Scale (Mishel, Citation1981), which is specific to illness, there is a lack of standardised and validated measures of uncertainty in other settings. Many studies that explored the association between uncertainty and mental health in non-medical settings relied on ad hoc measurements (e.g., single item questions asking to rate perceived uncertainty on a Likert scale) (Lee et al., Citation2005; Yamanouchi et al., Citation2018; see Afifi et al., Citation2013 for an exception). Furthermore, despite their heterogeneous nature, the vast majority of measurements of uncertainty (92%) and mental health (87%) had been developed in the US and there is a lack of measurements appropriate for other settings and contexts. Drawing on previous experience with measurement development (Hammoudeh et al., Citation2013), this gap is going to be partially addressed by the authors with the development of a measurement of uncertainty relevant to war and conflict-affected settings.
Finally, there is an urgent need for more research to be conducted in low- and middle-income contexts and among populations from ethnic minorities in high-income countries. These are populations where uncertainty might be more acute and, simultaneously, people and communities might have less resources to manage it (Mokdad et al., 2016), therefore making the need to investigate its impact on mental health even more pressing.
Relevance to the mental health field
Recent years have seen a shift away from addressing mental health through a purely biomedical model and towards a more holistic understanding of mental health as a bio-psycho-social phenomenon intimately linked with social, economic, and political factors (Lund et al., Citation2018). The current review points towards the importance of investigating how uncertainty around key social determinants can impact mental health.
Mental health in the reviewed studies did not originate in a vacuum but was profoundly intertwined with the uncertainties that participants experienced as part of their day-to-day lives. Mental health was inextricable from uncertainties about one’s illness and prognosis (Reich et al., Citation2006), about the health of one’s child due to lack of information (Steele et al., Citation2009), about one’s job following a disaster (Goto et al., Citation2006), and from uncertainties about one’s safety and the security of one’s community during displacement (Afifi et al., Citation2013), to name some examples. The current review, therefore, stresses the importance of addressing poor mental health by tackling its upstream determinants and by moving beyond proximal individual predictors towards a proper consideration of meso and macro levels of the socioecological model (Rose-Clarke et al., Citation2020).
We would like to highlight several research priorities that would contribute to an improved understanding of uncertainty as a socio-political determinant of mental health as well as contributing to the identification of strategies to address uncertainty and protect mental health. Firstly, while some papers did explore uncertainty at the community and societal level (Doumit et al., Citation2015), most studies focused on the individual and family level with more research needed that goes beyond these levels.
Furthermore, additional research is needed to investigate the mechanisms through which uncertainty affects mental health. One possibility is that uncertainty might worsen mental health problems through its detrimental impact on affect and emotions (Anderson et al., Citation2019), with uncertainty generally being linked to negative affect and described as aversive (Carleton, Citation2016). A related quest is to understand whether certain aspects of uncertainty are more associated with poor mental health than other components of the construct (e.g., lack of information vs. ambiguity and unpredictability). Additionally, as our findings also highlight, uncertainty is not always significantly associated with poor mental health. Indeed, some experimental evidence indicates that uncertainty can also have positive effects (Kurtz et al., Citation2007) or intensify positive effects (Bar-Anan et al., Citation2009). More research is required to understand under which circumstances uncertainty impacts mental health positively and how these differ from circumstances in which uncertainty is associated with poor mental health.
As Anderson et al. (Citation2019) highlight, an additional important research gap concerns how affect and mental health status might impact perceptions of uncertainty itself. Despite a large amount of literature on physical health, very little research exists to date on how people with mental health conditions experience uncertainty and how that affects their condition (Wolfensberger et al., Citation2019). Furthermore, the vast majority of the reviewed literature focused on anxiety, depression, and stress and future research should investigate the impact of uncertainty on mental health outcomes that have received little to no attention in the literature, such as psychosis (Cole et al., Citation2020).
Finally, more research is needed to investigate how addressing the root causes of uncertainty (e.g., lack of information concerning treatment, safety in one’s community, job insecurity) can impact mental health (WHO, Citation2014). Only a more in-depth understanding of the ultimate drivers of uncertainty will allow for more precise recommendations to inform policy and practice in locally meaningful ways.
Limitations
The current review holds several limitations. Firstly, due to the heterogeneity of the findings, of the measurements used, and of the study designs, we were only able to summarise the results narratively and could not aggregate the results concerning the association between uncertainty and mental health using meta-analytic techniques. Additionally, a vote-counting approach (i.e., assigning a positive, negative or null outcome to a relationship) to determine directionality presents several methodological issues (Siddaway et al., Citation2019) and hinders precise inferences concerning the effect size and the directionality of the relationship between uncertainty and mental health. However, this was not the aim of our review. Furthermore, the exploratory nature of scoping reviews (Tricco et al., Citation2016) allowed us to capture a varied spectrum of evidence, therefore, providing a more comprehensive snapshot of the state of the literature to date. Similarly, we did not assess the risk of bias within studies as this is generally considered less applicable to scoping reviews (Tricco et al., Citation2018).
The current review only focused on quantitative evidence. However qualitative data is likely to provide a more nuanced picture of the relationship between uncertainty and mental health as well as yield important insights into the coping mechanisms and the context within which uncertainty emerges and is managed (Bergmans et al., Citation2017; Gill & Morgan, Citation2011). A parallel review was undertaken focusing on the link between uncertainty and mental health in the qualitative literature and will be published separately.Footnote4
Our decision to limit the inclusion of papers published in English might have led to the omission of literature produced from non-English speaking countries and might have contributed to the majority of the literature coming from the US. Furthermore, our decision to only focus on papers that specifically used the term uncertainty could have led to the omission of relevant literature on similar constructs using different terminology. Finally, our search took place before the COVID-19 pandemic and there is the possibility we might have missed some more recent publications on the link between uncertainty and mental health. However, we do not believe that a small number of more recent publications would significantly affect the overall trends within our results.
Future directions for the authors
One of the areas in which virtually no research on uncertainty and mental health has been identified is in the context of wars and armed conflict. The research conducted by Afifi et al. (Citation2013) among Palestinian refugees living in refugee camps in Lebanon represents a notable exception. The current review was, in part, motivated by the authors’ interest in empirically investigating the mental health impacts of uncertainty in the occupied Palestinian territory (oPt). In the oPt, uncertainty is a chronic, pervasive, and structural experience, given ongoing Israeli military occupation, movement restrictions, siege conditions, land confiscation, the building of Israeli settlements on Palestinian land, periodic invasions, exposure to political violence, and medical shortages. The findings of the current review highlight the urgency for more high-quality evidence to be generated on the mental health impacts of exposure to systemic and ongoing uncertainty within armed conflict. The current findings are currently informing primary data collection work that is underway in the West Bank.
Concluding remarks
Uncertainty represents one of the defining characteristics of the world in which we live and, as the current review shows, is intimately linked with the mental health of people and communities. Our findings highlight several trends as well as several gaps that warrant future research. As uncertainty is likely to accompany humanity across some of the biggest challenges of the future, an improved understanding of how it impacts mental health and what can be done to address its effects represents a crucial research priority.
Acknowledgements
We would like to thank UK Research and Innovation GCRF for their financial support. Additionally, we gratefully acknowledge the support of other members of the Research for Health in Conflict in the MENA region (R4HC-MENA) team, in particular Mathias Regent for his support in the preliminary screening of the literature, Ranim Amra and Rawan Kafri for their support in the data extraction, and Dr. Weeam Hammoudeh for her contribution in discussing the conceptualisation of the review. Finally, we would like to thank Dr. Matthew Prina for discussing with us the methodological framework for the current review.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1 Due to the ambiguity inherent in distinguishing between related and overlapping constructs, the decision was made to limit included papers only to those that specifically used the term “uncertainty”.
2 We defined a study as focusing on a specific age group based on the mean age group of the entire sample or on the largest proportion of a sample falling in a certain age group.
3 We report ethnic categories as they were reported in the original studies while we are aware of the critical implications of this terminology.
4 Our decision to separate the two reviews was justified by the already complex nature of the quantitative dataset and by the desire to give the appropriate weight to both reviews.
References
- Afifi, T., & Afifi, W. (Eds.). (2016). Uncertainty, information management, and disclosure decisions: Theories and applications. Routledge. https://doi.org/10.4324/9780203933046
- Afifi, W. A., Afifi, T. D., & Merrill, A. (2014). Uncertainty and control in the context of a category-five tornado. Research in Nursing & Health, 37(5), 358–366. https://doi.org/10.1002/nur.21613
- Afifi, W. A., Afifi, T. D., Robbins, S., & Nimah, N. (2013). The relative impacts of uncertainty and mothers' communication on hopelessness among Palestinian refugee youth. The American Journal of Orthopsychiatry, 83(4), 495–504. https://doi.org/10.1111/ajop.12051
- Al-Dubai, S., & Rampal, K. (2012). Psychological morbidity and sources of job stress among doctors in Yemen. Asian Journal of Psychiatry, 13(1), 1–11.
- Anderson, E. C., Carleton, R. N., Diefenbach, M., & Han, P. K. J. (2019). The relationship between uncertainty and affect. Frontiers in Psychology, 10, 2504. https://doi.org/10.3389/fpsyg.2019.02504
- APA (2020). The great unknown: 10 tips for dealing with the stress of uncertainty. American Psychological Association. https://www.apa.org/topics/stress/uncertainty
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
- Arroll, M., Dancey, C. P., Attree, E. A., Smith, S., & James, T. (2012). People with symptoms of Ménière's disease: The relationship between illness intrusiveness, illness uncertainty, dizziness handicap, and depression. Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [AND] European Academy of Otology and Neurotology, 33(5), 816–823. https://doi.org/10.1097/MAO.0b013e3182536ac6
- BACP (2020). How to cope with uncertainty during COVID-19. British Association for Counselling and Psychotherapy. https://www.bacp.co.uk/news/news-from-bacp/2020/7-august-these-are-uncertain-times-here-are-some-ways-to-cope-with-uncertainty-during-covid-19/
- Bar-Anan, Y., Wilson, T. D., & Gilbert, D. T. (2009). The feeling of uncertainty intensifies affective reactions. Emotion, 9(1), 123–127. https://doi.org/10.1037/a0014607
- Bauman, Z. (2007). Liquid times: Living in an age of uncertainty. Polity.
- Bergmans, Y., Gordon, E., & Eynan, R. (2017). Surviving moment to moment: The experience of living in a state of ambivalence for those with recurrent suicide attempts. Psychology and Psychotherapy, 90(4), 633–648. https://doi.org/10.1111/papt.12130
- Brashers, D. E. (2001). Communication and uncertainty management. Journal of Communication, 51(3), 477–497. https://doi.org/10.1111/j.1460-2466.2001.tb02892.x
- Brown, A., Hayden, S., Klingman, K., & Hussey, L. (2020). Managing uncertainty in chronic illness from patient perspectives. Journal of Excellence in Nursing and Healthcare Practice, 2(1), 1–16. https://doi.org/10.5590/JENHP.2020.2.1.01
- Candian Institutes of Health Research (2010). A guide to knowledge synthesis. Government of Canada. https://cihr-irsc.gc.ca/e/41382.html
- Cange, C. W., Brunell, C., Acarturk, C., & Fouad, F. M. (2019). Considering chronic uncertainty among Syrian refugees resettling in Europe. The Lancet Public Health, 4(1), e14. https://doi.org/10.1016/S2468-2667(18)30261-5
- Carleton, R. N. (2016). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43. https://doi.org/10.1016/j.janxdis.2016.02.007
- Cole, D. M., Diaconescu, A. O., Pfeiffer, U. J., Brodersen, K. H., Mathys, C. D., Julkowski, D., Ruhrmann, S., Schilbach, L., Tittgemeyer, M., Vogeley, K., & Stephan, K. E. (2020). Atypical processing of uncertainty in individuals at risk for psychosis. NeuroImage Clinical, 26, 102239. https://doi.org/10.1016/j.nicl.2020.102239
- Colquhoun, H. L., Levac, D., O'Brien, K. K., Straus, S., Tricco, A. C., Perrier, L., Kastner, M., & Moher, D. (2014). Scoping reviews: Time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology, 67(12), 1291–1294. https://doi.org/10.1016/j.jclinepi.2014.03.013
- Courtin, E., & Knapp, M. (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. https://doi.org/10.1111/hsc.12311
- de Berker, A. O., Rutledge, R. B., Mathys, C., Marshall, L., Cross, G. F., Dolan, R. J., & Bestmann, S. (2016). Computations of uncertainty mediate acute stress responses in humans. Nature Communications, 7(1), 10996. https://doi.org/10.1038/ncomms10996
- Derogatis, L. R., & Melisaratos, N. (1983). The Brief Symptom Inventory: An introductory report. Psychological Medicine, 13(3), 595–605.
- Doumit, R., Afifi, R. A., & Devon, H. A. (2015). Serenity in political uncertainty. Holistic Nursing Practice, 29(2), 78–86. https://doi.org/10.1097/HNP.0000000000000077
- Eichengreen, B. (2016). Contemplating the age of hyper-uncertainty. Institute for New Economic Thinking. https://www.ineteconomics.org/perspectives/blog/contemplating-the-age-of-hyper-uncertainty
- Gentes, E. L., & Ruscio, A. M. (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive-compulsive disorder. Clinical Psychology Review, 31(6), 923–933. https://doi.org/10.1016/j.cpr.2011.05.001
- Germino, B. B., Mishel, M. H., Crandell, J., Porter, L., Blyler, D., Jenerette, C., & Gil, K. M. (2013). Outcomes of an uncertainty management intervention in younger African American and Caucasian breast cancer survivors. Oncology Nursing Forum, 40(1), 82–92. https://doi.org/10.1188/13.ONF.82-92
- Gil, K. M., Mishel, M. H., Belyea, M., Germino, B., Porter, L. S., & Clayton, M. (2006). Benefits of the uncertainty management intervention for African American and White older breast cancer survivors: 20-month outcomes. International Journal of Behavioral Medicine, 13(4), 286–294. https://doi.org/10.1207/s15327558ijbm1304_3
- Gill, E. A., & Morgan, M. (2011). Home sweet home: Conceptualizing and coping with the challenges of aging and the move to a care facility. Health Communication, 26(4), 332–342. https://doi.org/10.1080/10410236.2010.551579
- Goto, T., Wilson, J. P., Kahana, B., & Slane, S. (2006). The Miyake Island volcano disaster in Japan: Loss, uncertainty, and relocation as predictors of PTSD and depression. Journal of Applied Social Psychology, 36(8), 2001–2026. https://doi.org/10.1111/j.0021-9029.2006.00091.x
- Greco, V., & Roger, D. (2003). Uncertainty, stress, and health. Personality and Individual Differences, 34(6), 1057–1068. https://doi.org/10.1016/S0191-8869(02)00091-0
- Grupe, D. W., & Nitschke, J. B. (2013). Uncertainty and anticipation in anxiety: An integrated neurobiological and psychological perspective. Nature Reviews Neuroscience, 14(7), 488–501. https://doi.org/10.1038/nrn3524
- Hammoudeh, W., Hogan, D., & Giacaman, R. (2013). Quality of life, human insecurity, and distress among Palestinians in the Gaza Strip before and after the Winter 2008-2009 Israeli war. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 22(9), 2371–2379. https://doi.org/10.1007/s11136-013-0386-9
- HelpGuide (2020). Dealing with uncertainty during the coronavirus pandemic. HelpGuide. https://www.helpguide.org/articles/anxiety/dealing-with-uncertainty.htm
- Hirsh, J. B., Mar, R. A., & Peterson, J. B. (2012). Psychological entropy: A framework for understanding uncertainty-related anxiety. Psychological Review, 119(2), 304–320. https://doi.org/10.1037/a0026767
- Hoff, A. L., Mullins, L. L., Chaney, J. M., Hartman, V. L., & Domek, D. (2002). Illness uncertainty, perceived control, and psychological distress among adolescents with type 1 diabetes. Research and Theory for Nursing Practice, 16(4), 223–236. https://doi.org/10.1891/rtnp.16.4.223.53023
- Kovacs, M. (1992). Children’s Depression Inventory (CDI). Multi-Health Systems Inc.
- Kurtz, J. L., Wilson, T. D., & Gilbert, D. T. (2007). Quantity versus uncertainty: When winning one prize is better than winning two. Journal of Experimental Social Psychology, 43(6), 979–985. https://doi.org/10.1016/j.jesp.2006.10.020
- Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. Springer Publishing Company.
- Lee, S.-Y S., Lee, K. A., Rankin, S. H., Alkon, A., & Weiss, S. J. (2005). Acculturation and stress in Chinese-American parents of infants cared for in the intensive care unit. Advances in Neonatal Care, 5(6), 315–328. https://doi.org/10.1016/j.adnc.2005.08.011
- Lund, C., Brooke-Sumner, C., Baingana, F., Baron, E. C., Breuer, E., Chandra, P., Haushofer, J., Herrman, H., Jordans, M., Kieling, C., Medina-Mora, M. E., Morgan, E., Omigbodun, O., Tol, W., Patel, V., & Saxena, S. (2018). Social determinants of mental disorders and the sustainable development goals: A systematic review of reviews. The Lancet Psychiatry, 5(4), 357–369. https://doi.org/10.1016/S2215-0366(18)30060-9
- Mauro, A. M. P. (2008). Exploring uncertainty and psychosocial adjustment after cardioverter defibrillator implantation. The Journal of Cardiovascular Nursing, 23(6), 527–535. https://doi.org/10.1097/01.JCN.0000338932.73963.42
- McNair, D., Lorr, M., & Doppleman, L. (1971). POMS manual for the profile of mood states. Educational and Industrial Testing Service.
- Mishel, M. H. (1981). The measurement of uncertainty in illness. Nursing Research, 30(5), 258–263.
- Mishel, M. H. (1983). Parents’ perception of uncertainty concerning their hospitalized child. Nursing Research, 32(6), 324–330.
- Mishel, M. H. (1988). Uncertainty in illness. Image-The Journal of Nursing Scholarship, 20(4), 225–232. https://doi.org/10.1111/j.1547-5069.1988.tb00082.x
- Mokdad, A. H., Forouzanfar, M. H., Daoud, F., El Bcheraoui, C., Moradi-Lakeh, M., Khalil, I., Afshin, A., Tuffaha, M., Charara, R., Barber, R. M., Wagner, J., Cercy, K., Kravitz, H., Coates, M. M., Robinson, M., Estep, K., Steiner, C., Jaber, S., Mokdad, A. A., … Murray, C. J. L. (2016). Health in times of uncertainty in the eastern Mediterranean region, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet. Global Health, 4(10), e704–e713. https://doi.org/10.1016/S2214-109X(16)30168-1
- Moloney, G., Leviston, Z., Lynam, T., Price, J., Stone-Jovicich, S., & Blair, D. (2014). Using social representations theory to make sense of climate change: What scientists and nonscientists in Australia think. Ecology and Society, 19(3), 9. https://doi.org/10.5751/ES-06592-190319
- Moreland, P., & Santacroce, S. J. (2018). Illness uncertainty and posttraumatic stress in young adults with congenital heart disease. The Journal of Cardiovascular Nursing, 33(4), 356–362. https://doi.org/10.1097/JCN.0000000000000471
- Muggah, R., & Goldin, I. (2019). How to survive and thrive in our age of uncertainty. https://www.weforum.org/agenda/2019/01/how-to-survive-our-age-of-uncertainty-muggah-goldin/
- Mullins, L. L., & Hartman, V. L. (1995). Children’s uncertainty in illness scale. University of Oklahoma Health Sciences Center.
- NHS (2020). How to deal with change and uncertainty during COVID-19. Better Health: Every Mind Matters-NHS. https://www.nhs.uk/every-mind-matters/coronavirus/how-to-manage-change-during-covid-19/
- Niv, G., Bar Josef, S., Ben Bassat, O., Avni, I., Lictenstein, L., Niv, Y., & Barnoy, S. (2017). Quality of life and uncertainty in Crohn's disease. Quality of Life Research, 26(6), 1609–1616. https://doi.org/10.1007/s11136-017-1509-5
- Penrod, J. (2007). Living with uncertainty: Concept advancement. Journal of Advanced Nursing, 57(6), 658–667. https://doi.org/10.1111/j.1365-2648.2006.04008.x
- Peters, M., Godfrey, C., McInerney, P., Soares, C. B., Khalil, H., & Parker, D. (2015). Methodology for JBI scoping reviews. In E. Aromataris (Ed.), The Joanna Briggs Institute reviewers’ manual 2015 (1st ed., pp. 3–24). Joanna Briggs Institute. https://research.monash.edu/en/publications/methodology-for-jbi-scoping-reviews
- Phillimore, J., & Cheung, S. Y. (2021). The violence of uncertainty: Empirical evidence on how asylum waiting time undermines refugee health. Social Science & Medicine, 282, 114154. https://doi.org/10.1016/j.socscimed.2021.114154
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://doi.org/10.1177/014662167700100306
- Reich, J. W., Johnson, L. M., Zautra, A. J., & Davis, M. C. (2006). Uncertainty of illness relationships with mental health and coping processes in fibromyalgia patients. Journal of Behavioral Medicine, 29(4), 307–316. https://doi.org/10.1007/s10865-006-9054-7
- Rogoff, K. (2020). After coronavirus we should be ready for an uncertainty pandemic. The Guardian.
- Rose-Clarke, K., Gurung, D., Brooke-Sumner, C., Burgess, R., Burns, J., Kakuma, R., Kusi-Mensah, K., Ladrido-Ignacio, L., Maulik, P. K., Roberts, T., Walker, I. F., Williams, S., Yaro, P., Thornicroft, G., & Lund, C. (2020). Rethinking research on the social determinants of global mental health. The Lancet Psychiatry, 7(8), 659–662. https://doi.org/10.1016/S2215-0366(20)30134-6
- Rybarczyk, B., Grady, K. L., Naftel, D. C., Kirklin, J. K., White-Williams, C., Kobashigawa, J., Chait, J., Young, J. B., Pelegrin, D., Czerr, J., McLeod, M., Rissinger, J., Higgins, R., & Heroux, A. (2007). Emotional adjustment 5 years after heart transplant: A multisite study. Rehabilitation Psychology, 52(2), 206–214. https://doi.org/10.1037/0090-5550.52.2.206
- Santacroce, S. J. (2003). Parental uncertainty and posttraumatic stress in serious childhood illness. Journal of Nursing Scholarship, 35(1), 45–51. https://doi.org/10.1111/j.1547-5069.2003.00045.x
- Schiltz, J., Vindevogel, S., Derluyn, I., & Vanderplasschen, W. (2019). Uncertainty in situations of forced displacement: A critical interpretative synthesis of refugee literature. Population Space and Place, 25(3), 3. https://doi.org/10.1002/psp.2194
- Sharkey, C. M., Bakula, D. M., Baraldi, A. N., Perez, M. N., Suorsa, K. I., Chaney, J. M., & Mullins, L. L. (2018). Grit, illness-related distress, and psychosocial outcomes in college students with a chronic medical condition: A path analysis. Journal of Pediatric Psychology, 43(5), 552–560. https://doi.org/10.1093/jpepsy/jsx145
- Siddaway, A. P., Wood, A. M., & Hedges, L. V. (2019). How to do a systematic review: A best practice guide for conducting and reporting narrative reviews, meta-analyses, and meta-syntheses. Annual Review of Psychology, 70, 747–770. https://doi.org/10.1146/annurev-psych-010418-102803
- Spielberger, C., Gorsuch, R., Lushene, R., Vagg, P., & Jacobs, G. (1983). Manual for the State-Trait Anxiety Inventory (Form Y1–Y2). Consulting Psychologists Press.
- Steele, R. G., Aylward, B. S., Jensen, C. D., & Wu, Y. P. (2009). Parent- and youth-reported illness uncertainty: Associations with distress and psychosocial functioning among recipients of liver and kidney transplantations. Children's Health Care, 38(3), 185–199. https://doi.org/10.1080/02739610903038768
- Stewart, J. L., & Mishel, M. H. (2000). Uncertainty in childhood illness: A synthesis of the parent and child literature. Scholarly Inquiry for Nursing Practice, 14(4), 299–319.
- Szulczewski, L., Mullins, L. L., Bidwell, S. L., Eddington, A. R., & Pai, A. L. H. (2017). Meta-analysis: Caregiver and youth uncertainty in pediatric chronic illness. Journal of Pediatric Psychology, 42(4), 395–421. https://doi.org/10.1093/jpepsy/jsw097
- Tarhani, M., Goudarzi, F., Hasanvand, S., Ebrahimzadeh, F., & Rassouli, M. (2020). Uncertainty, anxiety, depression and the quality of life in patients with cancer. Oncology and Radiotherapy, 46(1), 20–27.
- Thomson, S. (2020). How to deal with the anxiety of uncertainty. Wired. https://www.wired.com/story/how-to-deal-with-uncertainty-coronavirus/
- Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K., Colquhoun, H., Kastner, M., Levac, D., Ng, C., Sharpe, J. P., Wilson, K., Kenny, M., Warren, R., Wilson, C., Stelfox, H. T., & Straus, S. E. (2016). A scoping review on the conduct and reporting of scoping reviews. BMC Medical Research Methodology, 16(1), 15. https://doi.org/10.1186/s12874-016-0116-4
- Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Tversky, A., & Kahneman, D. (1974). Judgment under uncertainty: Heuristics and biases. Science, 185(4157), 1124–1131.
- Wakeham, J. (2015). Uncertainty: History of the concept. In International encyclopedia of the social & behavioral sciences (2nd ed., Vol. 24, pp. 716–721).
- Weiss, D. S., & Marmar, C. R. (1996). The impact of event scale-revised. In J. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). Guilford.
- WHO (2014). Social determinants of mental health. https://apps.who.int/iris/bitstream/handle/10665/112828/9789241506809_eng.pdf
- WHO. (2020). Mental health and COVID-19. World Health Organization.
- Wolfensberger, P., Hahn, S., van Teijlingen, E., & Thomas, S. (2019). Uncertainty in illness among people with mental ill health: A nursing perspective. British Journal of Mental Health Nursing, 8(4), 181–187. https://doi.org/10.12968/bjmh.2018.0030
- Wu, D., Yu, L., Yang, T., Cottrell, R., Peng, S., Guo, W., & Jiang, S. (2020). The impacts of uncertainty stress on mental disorders of Chinese college students: Evidence from a nationwide study. Frontiers in Psychology, 11, 243. https://doi.org/10.3389/fpsyg.2020.00243
- Yamanouchi, T., Hiroshima, M., Takeuchi, Y., Sawada, Y., Takahashi, M., & Amagai, M. (2018). Factors associated with worsened or improved mental health in the Great East Japan earthquake survivors. Archives of Psychiatric Nursing, 32(1), 103–111. https://doi.org/10.1016/j.apnu.2017.10.005