Abstract
Background
Substance use amongst young people poses developmental and clinical challenges, necessitating early detection and treatment. Considering the widespread use of technology in young people, delivering interventions digitally may help to reduce and monitor their substance use.
Aims
We conducted a systematic review and two meta-analyses to assess the effectiveness of digital interventions for reducing substance use (alcohol, smoking, and other substances) among young people aged 10 to 24 years old.
Method
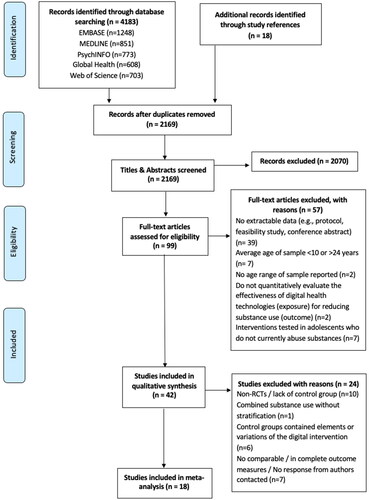
Embase, Global Health, Medline, PsychINFO, Web of Science and reference lists of relevant papers were searched in November 2020. Studies were included if they quantitatively evaluated the effectiveness of digital health technologies for treating substance use. A narrative synthesis and meta-analysis were conducted.
Results
Forty-two studies were included in the systematic review and 18 in the meta-analyses. Digital interventions showed small, but statistically significant reductions in weekly alcohol consumption compared to controls (SMD= −0.12, 95% CI= −0.17 to −0.06, I2=0%), but no overall effect was seen on 30-day smoking abstinence (OR = 1.12, 95% CI = 0.70 to 1.80, I2=81%). The effectiveness of digital interventions for reducing substance use is generally weak, however, promising results such as reducing alcohol use were seen. Large-scale studies should investigate the viability of digital interventions, collect user feedback, and determine cost-effectiveness.
Prisma/Prospero
This systematic review was conducted following Cochrane methodology PRISMA guidelines. The review was registered with PROSPERO in November 2020 (CRD42020218442).
1. Introduction
In high-income countries, substance use is one of the leading causes for healthy life years lost in young people and represents a major public health challenge (Dick & Ferguson, Citation2015; Griswold et al., Citation2018; Peacock et al., Citation2018). Substance use most frequently co-occurs with psychiatric problems such as depression, suicide and psychosis (Patton et al., Citation2002; Sussman et al., Citation2008) and clusters with other adverse childhood experiences (ACEs) such as low socioeconomic status, incarceration and homelessness (Hughes et al., Citation2017; Kessler et al., Citation2006; Low et al., Citation2012; Settipani et al., Citation2018). Each of these circumstances can trigger an increase in current substance use to ‘self-medicate’ co-occurring psychiatric symptoms and/or create a stressful environment that can trigger a relapse in substance use.
The peak time for initiation of substance use is during adolescence and young adulthood, with tobacco and alcohol usually preceding the use of highly addictive and illegal substances such as heroin and methamphetamine (Degenhardt et al., Citation2016). Whilst there is no international consensus on the age range for adolescence and young adulthood, the World Health Organisation (WHO) recognises that adolescents include persons aged 10–19 years and youth includes those between 15–24 years for statistical purposes (WHO, Citation2022). Together, ‘young people’ are between the ages of 10–24 years, which is the definition we use in this paper. Young people undergo a period of key psychosocial transitions occur as the brain undergoes cognitive and emotional development that begins with the onset of puberty (approximately aged 10) and ends in the mid-20s (Squeglia et al., Citation2009). Therefore. preventing and reducing substance use during this time is critical.
The recent COVID-19 pandemic separated young people from some of the protective factors against substance use like school and family connectedness, strong neighbourhood attachment and academic competence (Nawi et al., Citation2021), which could have created conditions for substance use to begin or continue (Dumas et al., Citation2020). Alternatively, the pandemic demonstrated the value of digital health to address people’s health needs. The term ‘digital health interventions’ denotes interventions that are responsive to user input and are delivered with the support of technology including targeted client communication; personal health tracking; and on-demand information services (Isioma et al., Citation2022; Quilty et al., Citation2021; WHO, Citation2019). Specifically, Web/Internet/Computer-based health interventions are primarily self-guided programmes that are executed by means of a “prescriptive online programme operated through a website and delivered through a computer” (Barak et al., Citation2009) and mobile phone-based health interventions are those delivered through a mobile/smart phone – including applications (apps) and text messages (WHO, Citation2011).
Young people are the most digitally connected age group worldwide − 70% use the internet, compared to 48% of the total population (United Nations Children’s Fund, Citation2017). Digital health interventions could promote positive behaviour changes and potentially increase treatment engagement in this population, which might be more cost-effective than current methods, but there is a need to summarise their effectiveness to decide whether they are worth investing in.
There is currently no systematic review and meta-analysis that synthesises data on different types of digital interventions for the treatment of dependency, addiction or substance use disorder in young people aged 10–24 years. To add, this systematic review uses a broader search strategy to capture studies that may have tested digital interventions for e-cigarette use/vaping, since the uptake of these has increased considerably in recent years across the globe (Perikleous et al., Citation2018). This work comprises of a systematic review and two meta-analyses of randomised controlled trials (RCTs) with outcomes associated with smoking and alcohol use.
Previous systematic reviews and meta-analyses which have investigated the effect of digital health interventions on changing substance use behaviours among young people have produced conflicting results (Carey et al., Citation2012; Champion et al., Citation2013; Civljak et al., Citation2013; Dick et al., Citation2019; Hutton et al., Citation2011; Oosterveen et al., Citation2017; Tait & Christensen, Citation2010). Digital interventions show weak efficacy for smoking cessation (Civljak et al., Citation2013; Hutton et al., Citation2011), but seem to be more promising for reducing alcohol use. A 2012 meta-analysis by Carey et al. compared face-to-face interventions with computer-delivered alcohol interventions between 1998–2010 and conluded tthat face-to-face interventions ultimately provided the most effective and enduring effects (Carey et al., Citation2012). Apps and text messaging have alos been found to be acceptable and potentially effective ways to deliver messages about reducing alcohol consumption to young people (Hutton et al., Citation2020; Kazemi et al., Citation2021). However, each of these reviews did not investigate young people with dependency, or a pre-existing substance use disorder, therefore clinical relevance is difficult to determine.
The addiction field has experienced a rapid increase in digital health interventions. This review and meta-analysis aims to examine:
The effectiveness of digital treatments for young people (10–24 years) with problematic substance use, dependency or addiction.
Whether the type of substance, the type of digital intervention or particular features explain variability in effects.
The feasibility and acceptability of digital interventions in this age group.
Furthermore, we hope to aid researchers in evaluating new literature, give new directions for future research, and help to create useful digital treatments.
2. Material and methods
2.1. Design
This systematic review was conducted following Cochrane methodology and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (Moher et al., Citation2009). The review was registered with PROSPERO in November 2020 (CRD42020218442).
2.2. Search strategy
Embase, Global Health, Medline, PsychINFO and Web of Science databases were searched in November 2020 to identify peer-reviewed studies in English. No limits were placed on the dates that papers were published, as we wanted to provide an exhaustive overview of the literature by capturing any studies which previous reviews might have missed.
Search terms were based on a preliminary search of the relevant literature and reviewed and approved by all of the authors in a meeting. We combined the following search terms and their associated wildcard variants using Boolean operators:
Adolescents, teenagers, youth, young people/person/adult
Digital health, Telehealth, telemedicine, eHealth, mHealth, Internet, uHealth, smartphone, apps, mobile health, electronic health
Drugs, alcohol, smoking, substance use/abuse/misuse
The search terms within groups were combined with OR whereas each domain was combined with AND. The search coding was defined by two of the authors (AW and DL), PhD scholars who have experience with search strategies from previous systematic reviews. The full search strategy can be found in Table A in O’Logbon et al., Citation2023. Reference lists of relevant studies and systematic reviews were also searched.
2.3. Eligibility criteria
Articles were eligible for inclusion if they (i) were published in English, (ii) quantitatively evaluated the effectiveness of a digital health intervention (exposure) for substance use (outcome), (iii) included participants who were between 10–24 years of age, and (iv) included participants with self‐reported current problematic substance use at baseline (one-off consumption such as using a substance once a year or once in their lifetime did not apply) or a formally diagnosed substance use disorder. Randomised controlled trials (RCTs) and non-RCTs were both included in the systematic review. Non-RCTs were not included in meta-analyses.
Digital health interventions were defined as interventions delivered with the support of computers, mobile phones or portable devices with the primary aim of changing substance use-related behaviours. Examples include binge drinking (drinking more than the recommend weekly allowance in a single session), smoking (tobacco, cannabis, other substances, or e-cigarettes) and illicit drug use. Interventions targeting additional behaviours (e.g. eating habits and exercise) or co-occurring conditions (e.g. depression) were only included if participants were screened into the trial as using substances and if substance use behaviours were reported separately.
Studies were excluded from the review if they (i) assessed passive digital health technologies, such as those developed for the sole purpose of screening, assessment or lacked any user input, (ii) the mean age of participants was <10 years or >24 years, or (iii) <50% of the participant population was between 10–24 years old.
2.4. Study selection and data extraction
Duplicate references were removed in Mendeley reference manager, then titles and abstracts of articles were independently reviewed for eligibility in November 2020 by JO and CW. Percentage agreement was high (Cohen’s kappa: 0.81). Where disagreement existed, JO and CW agreed on an outcome through discussion. JO screened the full-texts and CW was responsible for second rating them – both agreed on all of the full-texts to be included in the final review. JO completed data extraction using the Cochrane Data Extraction and Assessment form as a guide and conducted the meta-analyses.
2.5. Outcomes
Our primary outcome was abstinence or reduction in substance use as reported by the trial authors. For secondary outcomes, we sought data on feasibility and acceptability. However, these were reported inconsistently, and so were included in a narrative synthesis.
2.6. Statistical analysis
The meta-analyses were conducted using RevMan 5.4.1. Studies were not included if they were not an RCT; lacked a control group; combined substance use was measured without stratification by the different types of substances; control groups contained elements or variations of the digital intervention, and if there were no outcome measures comparable to the other studies (). The remaining 18 studies targeted either smoking or alcohol consumption.
The most common outcome measure for alcohol use was weekly alcohol consumption (continuous variable). Studies reported this in standard drink units, number of drinks, or grams of ethanol. Results from intention-to-treat analysis were used where available. If not already provided, means and standard deviations were converted from available confidence intervals, standard errors, medians, ranges, and sample sizes (Higgins et al., Citation2022; Hozo et al., Citation2005).
For smoking studies, the most common outcome measure was 30-day continuous abstinence (dichotomous variable). Percentages or fractions were converted to whole numbers based on the sample size, provided an intention-to-treat analysis had been used. If intention-to-treat results were not available, we used reported results for completers.
Outcomes were reported over a wide range of time points so we used the results reported at the last time point from each study. Authors of studies with missing or inconclusive results were contacted to provide additional information.
Due to anticipated heterogeneity in the study designs and scales used, we used a random-effects model to pool Standardised Mean Differences (SMD) between treatment and control arms for alcohol studies and odds ratios (OR) for smoking studies. For the main meta-analyses, if studies reported on multiple relevant study arms, we combined them to ensure that in each study a single treatment arm result was being compared to a single control arm result (Cochrane Handbook section 16.5.4) (Higgins et al., Citation2022). We calculated a mean average to combine study arms in the alcohol meta-analysis, and summed frequencies to combine study arms in the smoking meta-analysis. Heterogeneity was investigated using Cochran’s Q and the I2 statistic, and publication bias was explored using funnel plots.
Post hoc sensitivity analyses were conducted to investigate whether the pooled effect sizes varied according to the type of control group under study: face-to-face intervention, assessment only/no intervention, and passive intervention (e.g. leaflets, helplines). For these analyses, we did not combine multiple control arms as described above, such that studies could appear twice if they included multiple relevant control arms.
Due to journal restrictions on the number of figures that can be included in manuscripts, the remaining figures can be found on the Open Science Framework (O’Logbon et al., Citation2023).
2.7. Narrative synthesis
Findings which could not be included in the meta-analysis were summarised in a narrative synthesis. Effectiveness, acceptability, and feasibility were explored.
3. Results
The PRISMA diagram for this review can be found in .
3.1. Study characteristics
Characteristics from 32 RCTs are summarised in and 10 non-RCTs in . Most of the studies were conducted in the USA (n = 29) and the mean ages of the samples ranged from 15 to 24 years. Studies investigated digital health interventions for the following substances: alcohol (n = 17), smoking (n = 19), and polydrug use (combination of marijuana, methamphetamine, cocaine, heroin, prescription drugs and other including alcohol or smoking) (n = 6). Various digital platforms were used: Web/Internet/Computer-based (n = 23), Mobile phone-based (n = 16) and both web- and mobile phone-based (n = 3).
Table 1. Summary of included RCTs (n = 32).
Table 2. Summary of included non-RCTs (n = 10).
All the studies used self-reported substance use outcomes and 12 used biochemical validation of abstinence (Alfonso et al., Citation2013; An et al., Citation2008; Carey et al., Citation2009; Doumas et al., Citation2009; Gonzales et al., Citation2014; Kong et al., Citation2017; Obermayer et al., Citation2004; Pbert et al., Citation2020; Ramo et al., Citation2018; Riley et al., Citation2008; Simmons et al., Citation2013; Walters et al., Citation2007). For smoking, this was determined by urine or saliva cotinine levels or carbon monoxide breath testing. For alcohol consumption, peak blood alcohol concentrations (BAC) were measured.
All the studies assessed substance use outcomes using variants of the surveys noted in (Collins et al., Citation1985; Fagerström, Citation1978; Heatherton et al., Citation1991; Hurlbut & Sher, Citation1992; Khadjesari et al., Citation2009; Raskin White & Labouvie, Citation1989; Saunders et al., Citation1993; Shiffman et al., Citation2004; Sobell & Sobell, Citation1992). Intervention periods ranged from 2 weeks to 12 months, with most studies conducting follow-ups via online questionnaires or telephone interviews.
3.2. Quality assessment
The Cochrane risk of bias tool (Higgins et al., Citation2011) was used to assess risk of bias for RCTs (see Table B in O’Logbon et al., Citation2023) and the ROBINS-I tool was used for non-RCTs (Sterne et al., Citation2016) (see Table C in O’Logbon et al., Citation2023).
Ten studies were non-RCTs () and lacked randomisation and a control group, leading to confounders which were not controlled for. Eight were potentially underpowered, with small sample sizes (<100) (Dennis et al., Citation2015; Hussey & Flynn, Citation2019; Kong et al., Citation2017; Mays et al., Citation2020; Obermayer et al., Citation2004; Riley et al., Citation2008; Shrier et al., Citation2014; Woodruff et al., Citation2001).
A loss to follow up was seen in most studies. We took a good response rate as 60%, which four RCTs (Bewick et al., Citation2010; Deady et al., Citation2016; Ekman et al., Citation2011; Skov-Ettrup et al., Citation2014) and one non-RCT (Baskerville et al., Citation2016) failed to achieve, suggesting high attrition rates. Their statistical analyses sought to minimise attrition bias in analyses, using methods such as multiple imputation, last observation carried forward, and sensitivity analysis.
All studies were vulnerable to response bias because they used self-reported measures of substance use and intervention adherence, although some used biochemical validation. Further biases could have arisen due to the settings where participants were sampled, such as outside clubs and bars (Carrà et al., Citation2016) or in rehabilitation centres (Hussey & Flynn, Citation2019; Trudeau et al., Citation2017). Finally, there were limited discussions of participant and investigator blinding, perhaps because the concealment of group allocation is challenging for these types of interventions.
3.3. Alcohol meta-analysis
depicts the characteristics of the studies that were included in the meta-analysis.
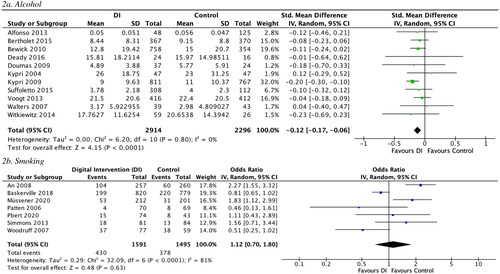
Eleven of these studies measured the effectiveness of a digital intervention on alcohol consumption (Alfonso et al., Citation2013; Bertholet et al., Citation2015; Bewick et al., Citation2010; Deady et al., Citation2016; Doumas et al., Citation2009; Kypri et al., Citation2004, Citation2009; Suffoletto et al., Citation2015; Voogt et al., Citation2013; Walters et al., Citation2007; Witkiewitz et al., Citation2014). The pooled SMD demonstrated a small but statistically significant effect of digital interventions on reducing weekly alcohol consumption at follow-up compared to control arms (SMD= −0.12, 95% CI= −0.17 to −0.06) ().
Table 3. Studies included in meta-analyses.
There was evidence of low heterogeneity (I2=0%; Q (10) =6.20, P=.80). Visual inspection of the funnel plot (see Figure A in O’Logbon et al., Citation2023) showed symmetry, indicating little publication bias.
Digital interventions yielded stronger reductions in alcohol use than assessment only/no intervention, and comparable reductions to passive interventions and face-to-face therapy ().
Table 4. Sensitivity analyses.
3.4. Smoking meta-analysis
Seven studies were included in the smoking meta-analysis (An et al., Citation2008; Baskerville et al., Citation2018; Müssener et al., Citation2020; Patten et al., Citation2006; Pbert et al., Citation2020; Simmons et al., Citation2013; Woodruff et al., Citation2001) (). There was no statistically significant effect of digital interventions on 30-day smoking abstinence (OR = 1.12, 95% CI = 0.70 to 1.80) (). There was evidence for considerable and statistically significant heterogeneity (I2=81%; Q (6) =32.09, P < 0.0001). Visual inspection of the funnel plot (see Figure B in O’Logbon et al., Citation2023) also showed asymmetry, indicating potential publication bias.
Sensitivity analyses yielded similar, non-significant effect sizes when limiting the meta-analysis to different control arms ().
3.5. Narrative synthesis
Non-RCTs (in ) and the 14 RCTs that could not be included in the meta-analyses are discussed below.
3.5.1. Effectiveness
3.5.1.1. Alcohol use
A total of six studies could not be included in the alcohol meta-analysis (Bryant et al., Citation2013; Carey et al., Citation2009; Carrà et al., Citation2016; Cunningham et al., Citation2015; Ekman et al., Citation2011; Hides et al., Citation2018). Carrà et al. (Citation2016) was not an RCT; Bryant et al. (Citation2013) and Hides et al. (Citation2018) included elements or variations of the digital intervention in their control groups and there were no comparable outcome measures in the other three studies despite authors being contacted (Carey et al., Citation2009; Cunningham et al., Citation2015; Ekman et al., Citation2011).
Overall, digital interventions for alcohol use did not show significant long-term effects on young people’s drinking habits. Carrà et al. (Citation2016) piloted an app to reduce binge drinking in young adults which showed a reduction in binge drinking (37% at baseline vs. 18% at 2-week follow-up), however longer-term effects were not studied and there was a lack of control group.
Three studies investigated electronic screening brief interventions (e-SBIs) (Bertholet et al., Citation2015; Carey et al., Citation2009; Ekman et al., Citation2011). SBIs are completed in primary care settings and consist of a conversation with a healthcare professional to screen for substance‐related risk or harm and provide personalised feedback and coping strategies to reduce use. Cunningham et al. (Citation2015) compared the e-SBI to an in-person SBI and an information brochure (control group). At three months, both SBIs significantly decreased alcohol consumption compared to the control but this was not maintained at six months. These results are echoed in Ekman et al.’s (Citation2011) study that compared an e-SBI to a control group receiving generic feedback on their alcohol use. Carey, Henson, et al. (Citation2009) compared an e-SBI to an in-person SBI among college students sanctioned for alcohol violations. The in-person SBI was more effective after one month but neither intervention predicted additional drinking change beyond what was already achieved post-sanction.
Personalised feedback and interactive monitoring interventions were also investigated. Bryant et al. (Citation2013) trialled personalised feedback sent via email to undergraduate students on their drinking (generated from information gathered at baseline). Students consumed significantly fewer drinks per week and spent less days being drunk compared to their previous 30 days. Conversely, interactive monitoring and feedback of drinking behaviour via the Ray’s Night Out app in Hides et al.’s (Citation2018) study produced no differences in alcohol use or related problems but improved young people’s alcohol knowledge, which was maintained at the one-year follow-up.
3.5.1.2. Smoking
A total of twelve studies could not be included in the smoking meta-analysis (An et al., Citation2013; Baskerville et al., Citation2016; Kong et al., Citation2017; Mason et al., Citation2015; Mays et al., Citation2020; Obermayer et al., Citation2004; Ramo et al., Citation2018; Riley et al., Citation2008; Shrier et al., Citation2014; Skov-Ettrup et al., Citation2014; Woodruff et al., Citation2001; Ybarra et al., Citation2013). Seven were excluded because they were non-RCTs (Baskerville et al., Citation2016; Kong et al., Citation2017; Mays et al., Citation2020; Obermayer et al., Citation2004; Riley et al., Citation2008; Shrier et al., Citation2014; Woodruff et al., Citation2001) and three studies contained elements or variations of the digital intervention (An et al., Citation2013; Skov-Ettrup et al., Citation2014; Ybarra et al., Citation2013). There were no comparable outcome measures in the other two studies despite authors being contacted (Mason et al., Citation2015; Ramo et al., Citation2018).
Combined web- and mobile-based interventions involved the completion of educational modules and tools to monitor progress. This helped generate text messages which either reminded participants of quit dates or were health/lifestyle related (An et al., Citation2013; Riley et al., Citation2008). Increased abstinence rates were seen in these studies. In particular, in An et al.’s (Citation2013) 3-arm RCT, the addition of online peer coaching to the web-based modules and text messages showed the highest abstinence rate.
Mays et al. (Citation2020) and Obermayer et al. (Citation2004) trialled mobile phone text-messaging interventions that informed participants on the short- and long-term harm of their smoking habits. Mays et al. (Citation2020) found that six participants (30%) reported quitting smoking completely and four participants (20%) had decreased frequency of smoking at the six-week follow-up. In Obermayer et al.’s (Citation2004) study, nearly half (43%) of the 46 participants reported a 24-hour quit attempt, and 22% had quit smoking after six weeks in the programme (17% validated by cotinine).
The other studies reported no significant effects on smoking rates (Baskerville et al., Citation2016; Kong et al., Citation2017; Mason et al., Citation2015; Ramo et al., Citation2018; Shrier et al., Citation2014; Skov-Ettrup et al., Citation2014; Woodruff et al., Citation2001).
3.5.1.3. Other substances and combined drug use
Five studies (Dennis et al., Citation2015; Gonzales et al., Citation2014; Hussey & Flynn, Citation2019; Trudeau et al., Citation2017; Walton et al., Citation2013) investigated the effects of digital interventions for combined drug use including marijuana, methamphetamine, cocaine, heroin, prescription drugs and alcohol. Unfortunately, all were excluded from the meta-analysis because they were either non-RCTs (Dennis et al., Citation2015; Hussey & Flynn, Citation2019) or had no comparable outcome measures, despite contacting authors (Gonzales et al., Citation2014; Trudeau et al., Citation2017; Walton et al., Citation2013).
In Gonzales et al.’s (Citation2014) study of a 12-week text messaging intervention, the participants who received texts (to monitor relapse and recovery, provide feedback, reminders, support, and education) were significantly less likely to relapse compared to control participants in community-based treatment programs (OR = 0.52, p = 0.002). Primary drug use was detected from urinalysis which bolsters these results.
Trudeau et al. (Citation2017) compared an online relapse-prevention programme to face-to-face therapy. Participants who used the website indicated a greater decrease drug use at 3-month follow up compared to controls, but this was not maintained at the 6-month follow-up.
Two studies (Dennis et al., Citation2015; Hussey & Flynn, Citation2019) assessed the effectiveness of ACHESS (Addiction Comprehensive Health Enhancement Support System) (Gustafson et al., Citation2014), a mobile app that includes substance use monitoring, educational tools, and ecological momentary assessments and interventions (EMA/Is). A high rate of participants completed the prompted EMAs (87%) and reported lower substance use in the next week after accessing an EMI (Dennis et al., Citation2015). Hussey & Flynn (Citation2019) found that ACHESS led to approximately the same proportion of young people achieving abstinence compared to those receiving treatment at a rehabilitation centre (58.3% vs 60.7%).
Finally, an e-SBI for cannabis use showed a short-term decrease in cannabis-related consequences (at 3 and 6 months) (Walton et al., Citation2013), but did not significantly reduce use, compared to a therapist-delivered SBI and a brochure.
3.5.2. Feasibility & acceptability
Seven studies reported on feasibility and acceptability in detail (Hides et al., Citation2018; Kong et al., Citation2017; Trudeau et al., Citation2017; Witkiewitz et al., Citation2014; Woodruff et al., Citation2001; Ybarra et al., Citation2013). We comment on the overall findings by each digital platform type.
3.5.2.1. Mobile phone-based interventions
Mobile phone-based interventions showed high acceptability and engagement. Hides et al.’s (Citation2018) Ray’s Night Out app was rated 3 out of 5 stars. The uMARS (Mobile application rating scale – user version (Stoyanov et al., Citation2016)) indicated that the app had high quality, functionality, aesthetics and information. There was an acceptable level of engagement, but participants reported they were unlikely to pay for the app.
In Ybarra et al.’s (Citation2013) study of an mHealth smoking cessation programme, Stop My Smoking (SMS) USA, at the 3-month follow-up, the intervention appeared to be most helpful for quitting smoking in men (44% intervention vs. 29% control; p = .14), young adults not currently enrolled in higher education (45% vs. 26% control; p = .07), and participants of non-White race (42% intervention vs. 23% control; p = .14). This may suggest that a digital intervention like SMS USA is particularly acceptable among this sub-population (Ybarra et al., Citation2013).
Participants of Kong et al.’s (Citation2017) mobile phone-based contingency management programme expressed that they enjoyed being in the programme and would recommend it to a friend. Appealing aspects were quality of support received, being on a quit schedule, setting goals and monetary incentives. Suggested areas for improvement included more in-person support, more incentives, and making it easier to send videos and provide saliva samples remotely.
In Dennis et al.’s (Citation2015) pilot study of an app for EMAs, high acceptability was seen, measured by the number of EMAs completed by adolescents. When surveyed on their experience of the app, most felt that the EMA “was not too long” (95%), “easy to learn how to do” (100%), and it was “easy to complete 6 per day” (94%).
Witkiewitz et al. (Citation2014) assessed the effectiveness and feasibility of BASICS-Mobile (Brief Alcohol Screening and Intervention for College Students programme (Hanewinkel & Wiborg, Citation2005)) – an e-SBI for college students that incorporates personalised feedback about drinking behaviour with components of cognitive behavioural therapy. Many participants reported that they learned something new about alcohol or smoking and that it helped them develop a goal to change their habits (Witkiewitz et al., Citation2014). However, five participants reported that participation in the study made them want to smoke or drink more than usual, suggesting that reactivity to repeated assessment may be an issue for digital interventions. Yet analysis of the smoking and drinking behaviour of these individuals indicated that they reported similar reductions in drinking and smoking as those who did not provide this feedback.
3.5.2.2. Web-based interventions
Notable positive aspects of web-based interventions included ease of use and ability to interact with a counsellor and other smokers (Woodruff et al., Citation2001). In Trudeau et al.’s (Citation2017) relapse-prevention website, ‘Navigating My Journey’, participants wanted “actual footage” of addicts in situations to be added to the site (the website already included video interviews with former users); guest speakers; and additional content on family issues.
4. Discussion
4.1. Main findings
We found evidence that digital interventions produced a small but significant overall reduction in alcohol consumption compared to no intervention controls, whilst digital interventions were not effective for smoking abstinence. Overall, improvements were short-lived and inconsistent.
4.2. Comparison to wider literature
4.2.1. Abstinence vs harm reduction
Addiction recovery is a personal journey and different strategies work for different people. The two most common approaches are abstinence and harm reduction. Abstinence-based addiction treatment focuses on quitting the substance whilst harm reduction focuses on educating people about safer substance use and tends to be more appropriate for an individual who is not ready to commit to abstinence by meeting them ‘where they are at’ (Marlatt & Witkiewitz, Citation2010). This is easier with alcohol since there are national maximimum recommended units, whilst there is no such ‘recommended allowance’ for smoking or illicit drug use. Learning about how to drink more safely and the dangerous consequences of binge drinking rather than enforcing abstinence is consistent with findings that most adolescents see drinking as normative (Borsari & Carey, Citation2001; Jenkins et al., Citation2017), which may explain the results seen.
It is important to acknowledge that primary prevention programmes for substance use need to differ in focus from those aimed at secondary prevention (where substance use is already established) – the latter was the focus in this systematic review. This requires careful consideration of the intended target population and the context in which the digital intervention and treatment approach are used. Future research could be done to compare abstinence-based and harm reduction-based digital interventions and determine which has longer-term effects.
4.2.2. Alcohol
Overall, digital interventions may help people reduce binge drinking better than doing nothing or providing only general health information but may have similar effects in reducing drinking when compared to face‐to‐face treatment, as concluded in other reviews (Cadigan et al., Citation2015; Dotson et al., Citation2015; Leeman et al., Citation2015). Yet, they do have the advantage that they can be delivered to a far larger proportion of the target population (Tait & Christensen, Citation2010). Effect sizes similar to those presented in our meta-analyses were found in Kaner et al.’s (Citation2017) systematic review and meta-analysis which investigated personalised digital interventions for reducing harmful alcohol use (Kaner et al., Citation2017).
4.2.3. Smoking
We found weak evidence to support the efficacy of digital interventions for smoking cessation which coincides with two systematic reviews (Civljak et al., Citation2013; Hutton et al., Citation2011). Conversely, a meta-analysis that compared internet smoking cessation interventions to face-to-face or no support found that digital interventions were superior, however, the types of Internet interventions were highly heterogeneous – e.g. photo-aging software, a list of Internet resources and a telehealth clinic with accompanying in-person support (Kant et al., Citation2021).
Mobile text-messaging may be particularly powerful for smoking behaviours such as abstinence and reduction of use, particularly automated reminders and motivating messages that can be sent during times of cravings (Scott-Sheldon et al., Citation2016). However, further work is needed to detect specific moderators of interventions such as follow-up length and message frequency.
4.2.4. Notable features of digital interventions
A personalised or tailored component was highlighted in most included studies (Bryant et al., Citation2013; Doumas et al., Citation2009; Skov-Ettrup et al., Citation2014; Suffoletto et al., Citation2015, Bewick et al., Citation2010). Personalised feedback, for example, aims to reduce negative substance use outcomes by providing feedback and tracking progress of substance use behaviours. Typically, personalised feedback is used in counselling sessions delivered using the principles of motivational interviewing (Miller & Rollnick, Citation2013) and often requires trained providers, clinical training, and supervision.
Providing personalised feedback digitally is an appealing alternative as it is can be automated, delivered in a variety of formats such as texts, apps or emails, and may be quicker to disseminate (e.g. app algorithms can analyse and track data provided by the young person to generate personalised messages at times when they may need it most). These features are thought to maintain abstinence for longer (Cadigan et al., Citation2015; Civljak et al., Citation2013). However, a lack of efficacy has been shown for illicit drug use (Saxton et al., Citation2021). The limited number of studies on digital interventions for illicit drug use suggest further research is needed to ascertain their efficacy for this substance type.
Online peer coaching was another particularly useful component highlighted in An et al.’s (Citation2013) study. There is limited evidence for the use of digital peer-based interventions for substance use, but face-to-face mentoring has shown positive effects (DuBois et al., Citation2011; Macarthur et al., Citation2016; Thomas et al., Citation2011). Across adolescence, young people tend to seek support from peers to solve problems more often than from their parents and teachers (Bokhorst et al., Citation2010). Innovative ways to connect young people to one another and effectively communicate substance use behaviour change to the target population at scale can be facilitated by technology. Studies are now underway to investigate the use of a digital peer-led approach to influence substance use behaviour change (Musyoka et al., Citation2021; Quilty et al., Citation2022).
Other desirable features of digital interventions for young people include the ability to receive information confidentially and anonymously for free, 24-hour availability and convenience of access (Franklin et al., Citation2006; Hawke et al., Citation2021; Wickersham et al., Citation2019).
4.2.5. Acceptability and engagement
High attrition rates indicate a potential challenge for implementing digital health technologies. They are likely to depend on factors associated with the participant (such as personal motivation) and the intervention (such as user experience design). Substance use disorders require long-term treatment and there is currently a lack of long-term efficacy data on digital interventions to suggest they can fulfil this. Even when interventions are well-designed, engagement hovers at ‘acceptable’ levels and attrition rates remain high. While clinical trials often try to keep drop-out rates low by frequent clinician contact and cash incentives (the latter of which majority of studies in this review provided), this is unlikely to be sustainable in a real-life clinical setting. Finally, if the costs associated with maintaining adherence equals that of face-to-face treatment then digital interventions may not be as low-cost or scalable as anticipated.
Fortunately, there are several emerging features that have increased engagement such as ease of use, gamification, personalisation, symptom monitoring, numerical feedback (ratings, scores), ability to chart progress, socialisation within the app (such as forums and peer support) and integration with clinical services (Nwosu et al., Citation2022). However, fears around privacy and data security, particularly surrounding susbtance use and addiction, can also cause attrition and should be addressed upfront (Huckvale et al., Citation2019).
4.2.6. Implications for clinical practice
The use of digital interventions to change behaviour is a necessary area of research to help develop and implement these tools to enhance current substance use treatment for young people. This review provides an assessment of the effectiveness of a broad range of digital health interventions and useful features. Digital interventions may have a role in monitoring substance use habits short-term, which could be useful when adolescents do not currently have an assigned counsellor, are on a waiting list for treatment, or do not want to seek help face-to-face. Data collected by EMAs/EMIs, or apps could inform therapist-led CBT and be used alongside it. Nevertheless, future digital interventions must be designed with input from young people, collect user feedback, remain free of charge wherever possible, and be easy to use so engagement is maximised. It may also be worth considering which treatment approaches work best for the adolescent age range – perhaps focusing on harm reduction as a first step towards abstinence could be initiated and maintained by digital interventions.
4.3. Limitations
This review is subject to some limitations. Firstly, our age range for substance use was 10 − 24 years to capture ‘young people’, but this is a wide age range with a number of heterogenous developmental periods that can affect the extent of substance use and the uptake of interventions. In addition, our meta-analysis did not include all of the RCTs due to lack of comparable outcomes, even when attempts to contact authors were made. Some of the included studies also very short follow-up periods between the use of the digital intervention and the substance use outcome, and this is important to keep in mind when looking at pooled estimates. Nevertheless, we used the longest follow-up period provided. We also only included studies published in the English language, which may limit generalisability of results. Finally, the range of studies included in this review, the variability between measurement of participants’ substance use outcomes, the unadjusted estimates used in the meta-analyses, and the small number of studies in the stratified analyses, should be considered when interpreting results.
4.4. Conclusion
Evidence for the effectiveness of digital health interventions for reducing substance use was generally weak, however, a small, significant and short-lived impact on alcohol use was seen in our meta-analysis. Digital health technologies may be appropriate for short-term use and monitoring – an ideal opportunity for this could be whilst waiting for treatment. In-person treatment is likely to be supplemented, instead of replaced, by these interventions.
Their acceptability is notable and there is potential for them to overcome various barriers associated with access to substance use services. However, additional user feedback and programme development is still warranted to continue to optimise user experience and reduce attrition rates. There was high attrition with longer follow-up periods, which makes it difficult to determine if significant improvements can be maintained long-term.
Future research should continue to investigate the viability of these interventions using large-scale studies and their cost-effectiveness should also be further explored, especially since it was indicated in one study that young people would not pay to use digital interventions. Furthermore, differential effects for vulnerable groups such as homeless, single-parent and looked-after young people could yield important discussion points as to whether digital interventions could be tailored for different sub-groups. Finally, the next review on this topic should investigate the use of digital interventions to combat the trend of increasing e-cigarette use/vaping young people particularly in adolescents who have never used substances before.
Additional information
Funding
References
- Alfonso, J., Hall, T. v., & Dunn, M. E. (2013). Feedback-based alcohol interventions for mandated students: An effectiveness study of three modalities. Clinical Psychology & Psychotherapy, 20(5), 411–423. doi:10.1002/cpp.1786.
- An, L. C., Demers, M. R. S., Kirch, M. A., Considine-Dunn, S., Nair, V., Dasgupta, K., Narisetty, N., Resnicow, K., & Ahluwalia, J. (2013). A randomized trial of an avatar-hosted multiple behavior change intervention for young adult smokers. Journal of the National Cancer Institute. Monographs, 2013(47), 209–215. doi:10.1093/jncimonographs/lgt021.
- An, L. C., Klatt, C., Perry, C. L., Lein, E. B., Hennrikus, D. J., Pallonen, U. E., Bliss, R. L., Lando, H. A., Farley, D. M., Ahluwalia, J. S., & Ehlinger, E. P. (2008). The RealU online cessation intervention for college smokers: A randomized controlled trial. Preventive Medicine, 47(2), 194–199. doi:10.1016/j.ypmed.2008.04.011.
- Barak, A., Klein, B., & Proudfoot, J. G. (2009). Defining internet-supported therapeutic interventions. In Annals of Behavioral Medicine : a Publication of the Society of Behavioral Medicine, 38(1), 4–17. (IssueAnn Behav Med. doi:10.1007/s12160–009–9130–7.
- Baskerville, N. B., Azagba, S., Norman, C., McKeown, K., & Brown, K. S. (2016). Effect of a digital social media campaign on young adult smoking cessation. Nicotine & Tobacco Research : official Journal of the Society for Research on Nicotine and Tobacco, 18(3), 351–360. doi:10.1093/ntr/ntv119.
- Baskerville, N. B., Struik, L. L., Guindon, G. E., Norman, C. D., Whittaker, R., Burns, C., Hammond, D., Dash, D., & Brown, K. S. (2018). Effect of a mobile phone intervention on quitting smoking in a young adult population of smokers: Randomized controlled trial. JMIR mHealth and uHealth, 6(10), e10893. doi:10.2196/10893.
- Bertholet, N., Cunningham, J. A., Faouzi, M., Gaume, J., Gmel, G., Burnand, B., & Daeppen, J. B. (2015). Internet-based brief intervention for young men with unhealthy alcohol use: A randomized controlled trial in a general population sample. Addiction (Abingdon, England), 110(11), 1735–1743. doi:10.1111/add.13051.
- Bewick, B. M., West, R., Gill, J., O’May, F., Mulhern, B., Barkham, M., & Hill, A. J. (2010). Providing Web-based feedback and social norms information to reduce student alcohol intake: A multisite investigation. Journal of Medical Internet Research, 12(5), e59. doi:10.2196/jmir.1461.
- Bokhorst, C. L., Sumter, S. R., & Westenberg, P. M. (2010). Social support from parents, friends, classmates, and teachers in children and adolescents aged 9 to 18 years: Who is perceived as most supportive? Social Development, 19(2), 417–426. doi:10.1111/j.1467-9507.2009.00540.x.
- Borsari, B., & Carey, K. B. (2001). Peer influences on college drinking: a review of the research. Journal of Substance Abuse, 13(4), 391–424. doi:10.1016/S0899-3289(01)00098-0.
- Bryant, Z. E., Henslee, A. M., & Correia, C. J. (2013). Testing the effects of e-mailed personalized feedback on risky alcohol use among college students. Addictive Behaviors, 38(10), 2563–2567. doi:10.1016/j.addbeh.2013.06.007.
- Cadigan, J. M., Haeny, A. M., Martens, M. P., Weaver, C. C., Takamatsu, S. K., & Arterberry, B. J. (2015). Personalized drinking feedback: A meta-analysis of in-person versus computer-delivered interventions. Journal of Consulting and Clinical Psychology, 83(2), 430–437. doi:10.1037/a0038394.
- Carey, K. B., Henson, J. M., Carey, M. P., & Maisto, S. A. (2009). Computer Versus In-Person Intervention for Students Violating Campus Alcohol Policy. Journal of Consulting and Clinical Psychology, 77(1), 74–87. doi:10.1037/a0014281.
- Carey, K. B., Scott-Sheldon, L. A. J., Elliott, J. C., Garey, L., & Carey, M. P. (2012). Face-to-face versus computer-delivered alcohol interventions for college drinkers: A meta-analytic review, 1998 to 2010. In Clinical Psychology Review, 32Issue (8), 690–703. (NIH Public Access doi:10.1016/j.cpr.2012.08.001.
- Carrà, G., Crocamo, C., Bartoli, F., Carretta, D., Schivalocchi, A., Bebbington, P. E., & Clerici, M. (2016). Impact of a Mobile E-Health Intervention on Binge Drinking in Young People: The Digital-Alcohol Risk Alertness Notifying Network for Adolescents and Young Adults Project. The Journal of Adolescent Health : official Publication of the Society for Adolescent Medicine, 58(5), 520–526. doi:10.1016/j.jadohealth.2016.01.008.
- Champion, K. E., Newton, N. C., Barrett, E. L., & Teesson, M. (2013). A systematic review of school-based alcohol and other drug prevention programs facilitated by computers or the Internet. Drug and Alcohol Review, 32(2), 115–123. doi:10.1111/j.1465-3362.2012.00517.x.
- Civljak, M., Stead, L. F., Hartmann-Boyce, J., Sheikh, A., & Car, J. (2013). Internet-based interventions for smoking cessation. In The Cochrane Database of Systematic Reviews, 2013Issue(7), CD007078. (Cochrane Database Syst Rev. doi:10.1002/14651858.CD007078.pub4.
- Collins, R. L., Parks, G. A., & Marlatt, G. A. (1985). Social Determinants of Alcohol Consumption. The Effects of Social Interaction and Model Status on the Self-Administration of Alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. doi:10.1037/0022-006X.53.2.189.
- Cunningham, R. M., Chermack, S. T., Ehrlich, P. F., Carter, P. M., Booth, B. M., Blow, F. C., Barry, K. L., & Walton, M. A. (2015). Alcohol interventions among underage drinkers in the ED: A randomized controlled trial. Pediatrics, 136(4), e783–e793. doi:10.1542/peds.2015-1260.
- Deady, M., Mills, K. L., Teesson, M., & Kay-Lambkin, F. (2016). An online intervention for co-occurring depression and problematic alcohol use in young people: Primary outcomes from a randomized controlled trial. Journal of Medical Internet Research, 18(3), e71. doi:10.2196/jmir.5178.
- Degenhardt, L., Stockings, E., Patton, G., Hall, W. D., & Lynskey, M. (2016). The increasing global health priority of substance use in young people. In The Lancet. Psychiatry, 3Issue (3), 251–264. (Lancet Psychiatry. doi:10.1016/S2215-0366(15)00508-8.
- Dennis, M. L., Scott, C. K., Funk, R. R., & Nicholson, L. (2015). A Pilot Study to Examine the Feasibility and Potential Effectiveness of Using Smartphones to Provide Recovery Support for Adolescents. Substance Abuse, 36(4), 486–492. doi:10.1080/08897077.2014.970323.
- Dick, B., & Ferguson, B. J. (2015). Health for the world’s adolescents: A second chance in the second decade. The Journal of Adolescent Health : official Publication of the Society for Adolescent Medicine, 56(1), 3–6. doi:10.1016/j.jadohealth.2014.10.260.
- Dick, S., Whelan, E., Davoren, M. P., Dockray, S., Heavin, C., Linehan, C., & Byrne, M. (2019). A systematic review of the effectiveness of digital interventions for illicit substance misuse harm reduction in third-level students. BMC Public Health, 19(1), 1244. doi:10.1186/s12889-019-7583-6.
- Dotson, K. B., Dunn, M. E., & Bowers, C. A. (2015). Stand-alone personalized normative feedback for college student drinkers: A meta-analytic review, 2004 to 2014. PloS One, 10(10), e0139518. doi:10.1371/journal.pone.0139518.
- Doumas, D. M., McKinley, L. L., & Book, P. (2009). Evaluation of two Web-based alcohol interventions for mandated college students. Journal of Substance Abuse Treatment, 36(1), 65–74. doi:10.1016/j.jsat.2008.05.009.
- DuBois, D. L., Portillo, N., Rhodes, J. E., Silverthorn, N., & Valentine, J. C. (2011). How Effective Are Mentoring Programs for Youth? A Systematic Assessment of the Evidence. Psychological Science in the Public Interest : a Journal of the American Psychological Society, 12(2), 57–91. doi:10.1177/1529100611414806/ASSET/1529100611414806.FP.PNG_V03.
- Dumas, T. M., Ellis, W., & Litt, D. M. (2020). What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. The Journal of Adolescent Health : official Publication of the Society for Adolescent Medicine, 67(3), 354–361. doi:10.1016/J.JADOHEALTH.2020.06.018.
- Ekman, D. S., Andersson, A., Nilsen, P., Ståhlbrandt, H., Johansson, A. L., & Bendtsen, P. (2011). Electronic screening and brief intervention for risky drinking in Swedish university students - A randomized controlled trial. Addictive Behaviors, 36(6), 654–659. doi:10.1016/j.addbeh.2011.01.015.
- Fagerström, K. O. (1978). Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors, 3(3-4), 235–241. doi:10.1016/0306-4603(78)90024-2.
- Franklin, V. L., Waller, A., Pagliari, C., & Greene, S. A. (2006). A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabetic Medicine : a Journal of the British Diabetic Association, 23(12), 1332–1338. doi:10.1111/j.1464-5491.2006.01989.x.
- Gonzales, R., Ang, A., Murphy, D. A., Glik, D. C., & Anglin, M. D. (2014). Substance use recovery outcomes among a cohort of youth participating in a mobile-based texting aftercare pilot program. Journal of Substance Abuse Treatment, 47(1), 20–26. doi:10.1016/j.jsat.2014.01.010.
- Griswold, M. G., Fullman, N., Hawley, C., Arian, N., Zimsen, S. R. M., Tymeson, H. D., Venkateswaran, V., Tapp, A. D., Forouzanfar, M. H., Salama, J. S., Abate, K. H., Abate, D., Abay, S. M., Abbafati, C., Abdulkader, R. S., Abebe, Z., Aboyans, V., Abrar, M. M., Acharya, P., … Gakidou, E. (2018). Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 392(10152), 1015–1035. doi:10.1016/S0140-6736(18)31310-2.
- Gustafson, D. H., McTavish, F. M., Chih, M. Y., Atwood, A. K., Johnson, R. A., Boyle, M. G., Levy, M. S., Driscoll, H., Chisholm, S. M., Dillenburg, L., Isham, A., & Shah, D. (2014). A smartphone application to support recovery from alcoholism a randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. doi:10.1001/jamapsychiatry.2013.4642.
- Hanewinkel, R., & Wiborg, G. (2005). Brief alcohol screening and intervention for college students (BASICS): A German pilot study. SUCHT, 51(5), 285–290. doi:10.1463/2005.05.05.
- Haug, S., Paz Castro, R., Kowatsch, T., Filler, A., & Schaub, M. P. (2017). Efficacy of a technology-based, integrated smoking cessation and alcohol intervention for smoking cessation in adolescents: Results of a cluster-randomised controlled trial. Journal of Substance Abuse Treatment, 82, 55–66. doi:10.1016/j.jsat.2017.09.00829021116.
- Hawke, L. D., Sheikhan, N. Y., MacCon, K., & Henderson, J. (2021). Going virtual: youth attitudes toward and experiences of virtual mental health and substance use services during the COVID-19 pandemic. BMC Health Services Research, 21(1), 340. doi:10.1186/S12913-021-06321-7/TABLES/2.
- Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., & Fagerstrom, K. (1991). The Fagerström Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction, 86(9), 1119–1127. doi:10.1111/j.1360-0443.1991.tb01879.x.
- Hides, L., Quinn, C., Cockshaw, W., Stoyanov, S., Zelenko, O., Johnson, D., Tjondronegoro, D., Quek, L. H., & Kavanagh, D. J. (2018). Efficacy and outcomes of a mobile app targeting alcohol use in young people. Addictive Behaviors, 77, 89–95. doi:10.1016/j.addbeh.2017.09.020.
- Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., Welch, V. A. (editors), Cochrane Handbook for Systematic Reviews of Interventions, version 6.3 (updated February 2022), Cochrane, 2022.
- Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., Savović, J., Schulz, K. F., Weeks, L., & Sterne, J. A. C, Cochrane Statistical Methods Group. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research ed.), 343(7829), d5928. doi:10.1136/bmj.d5928.
- Hozo, S. P., Djulbegovic, B., & Hozo, I. (2005). Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology, 5(1), 13. doi:10.1186/1471-2288-5-13.
- Huckvale, K., Torous, J., & Larsen, M. E. (2019). Assessment of the Data Sharing and Privacy Practices of Smartphone Apps for Depression and Smoking Cessation. JAMA Network Open, 2(4), e192542–e192542. doi:10.1001/jamanetworkopen.2019.2542.
- Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., Jones, L., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), e356–e366. doi:10.1016/S2468-2667(17)30118-4.
- Hurlbut, S. C., & Sher, K. J. (1992). Assessing alcohol problems in college students. Journal of American College Health : J of ACH, 41(2), 49–58. doi:10.1080/07448481.1992.10392818.
- Hussey, D., & Flynn, K. C. (2019). The utility and impact of the addiction comprehensive health enhancement support system (ACHESS) on substance abuse treatment adherence among youth in an intensive outpatient program. Psychiatry Research, 281, 112580. doi:10.1016/j.psychres.2019.112580.
- Hutton, A., Prichard, I., Whitehead, D., Thomas, S., Rubin, M., Sloand, E., Powell, T. W., Frisch, K., Newman, P., & Goodwin Veenema, T. (2020). mHealth Interventions to Reduce Alcohol Use in Young People: A Systematic Review of the Literature. Comprehensive Child and Adolescent Nursing, 43(3), 171–202. doi:10.1080/24694193.2019.1616008.
- Hutton, H. E., Wilson, L. M., Apelberg, B. J., Tang, E. A., Odelola, O., Bass, E. B., & Chander, G. (2011). A systematic review of randomized controlled trials: Web-based interventions for smoking cessation among adolescents, college students, and adults. Nicotine & Tobacco Research : official Journal of the Society for Research on Nicotine and Tobacco, 13Issue (4), 227–238. In (Nicotine Tob Res. doi:10.1093/ntr/ntq252.
- Isioma, M., Id, O., Kanana, S., Id, K., Agbo, P., Kumar Id, R., & Jagugaid, F. (2022). Telehealth interventions for substance use disorders in low- and- middle income countries: A scoping review. PLOS Digital Health, 1(11), e0000125. doi:10.1371/JOURNAL.PDIG.0000125.
- Jenkins, E. K., Slemon, A., & Haines-Saah, R. J. (2017). Developing harm reduction in the context of youth substance use: Insights from a multi-site qualitative analysis of young people’s harm minimization strategies. Harm Reduction Journal, 14(1), 53. doi:10.1186/s12954-017-0180-z.
- Kaner, E. F., Beyer, F. R., Garnett, C., Crane, D., Brown, J., Muirhead, C., Redmore, J., O’Donnell, A., Newham, J. J., de Vocht, F., Hickman, M., Brown, H., Maniatopoulos, G., & Michie, S. (2017). Personalised digital interventions for reducing hazardous and harmful alcohol consumption in community-dwelling populations. The Cochrane Database of Systematic Reviews, 9(9), CD011479. doi:10.1002/14651858.CD011479.PUB2/MEDIA/CDSR/CD011479/IMAGE_N/NCD011479-CMP-002-04.PNG.
- Kant, R., Yadav, P., & Bairwa, M. (2021). Effectiveness of the Internet-Based Versus Face-to-Face Interaction on Reduction of Tobacco Use Among Adults: A Meta-Analysis. Cureus, 13(11), e19380. doi:10.7759/cureus.19380.
- Kazemi, D. M., Li, S., Levine, M. J., Auten, B., & Granson, M. (2021). Systematic Review of Smartphone Apps as a mHealth Intervention to Address Substance Abuse in Adolescents and Adults. Journal of Addictions Nursing, 32(3), 180–187. doi:10.1097/JAN.0000000000000416.
- Kessler, R. C., Walters, E. E., Aguilar-Gaxiola, S., Andrade, L., Borges, L. G., Caraveo-Anduaga, J. J., Bijl, R., DeWit, D. J., Kolody, B., Merikangas, K. R., Molnar, B. E., Vega, W. A., & Wittchen, H. U. (2006). Cross-National Comparisons of Co-Morbidities between Substance Use Disorders and Mental Disorders. In Handbooks of Sociology and Social Research. (pp. 447–472). Springer. doi:10.1007/0-387-35408-5_23.
- Khadjesari, Z., Murray, E., Kalaitzaki, E., White, I. R., McCambridge, J., Godfrey, C., & Wallace, P. (2009). Test-retest reliability of an online measure of past week alcohol consumption (the TOT-AL), and comparison with face-to-face interview. Addictive Behaviors, 34(4), 337–342. doi:10.1016/j.addbeh.2008.11.010.
- Kong, G., Goldberg, A. L., Dallery, J., & Krishnan-Sarin, S. (2017). An open-label pilot study of an intervention using mobile phones to deliver contingency management of tobacco abstinence to high school students. Experimental and Clinical Psychopharmacology, 25(5), 333–337. doi:10.1037/pha0000151.
- Kypri, K., Hallett, J., Howat, P., McManus, A., Maycock, B., Bowe, S., & Horton, N. J. (2009). Randomized controlled trial of proactive web-based alcohol screening and brief intervention for university students. Archives of Internal Medicine, 169(16), 1508–1514. doi:10.1001/archinternmed.2009.249.
- Kypri, K., Saunders, J. B., Williams, S. M., McGee, R. O., Langley, J. D., Cashell-Smith, M. L., & Gallagher, S. J. (2004). Web-based screening and brief intervention for hazardous drinking: A double-blind randomized controlled trial. Addiction (Abingdon, England), 99(11), 1410–1417. doi:10.1111/j.1360-0443.2004.00847.x.
- Leeman, R. F., Perez, E., Nogueira, C., & DeMartini, K. S. (2015). Very-brief, web-based interventions for reducing alcohol use and related problems among college students: A review. In Frontiers in Psychiatry, 6Issue(SEP), 129. (Frontiers Media SA. doi:10.3389/fpsyt.2015.00129.
- Low, N. C., Dugas, E., O’Loughlin, E., Rodriguez, D., Contreras, G., Chaiton, M., & O’Loughlin, J. (2012). Common stressful life events and difficulties are associated with mental health symptoms and substance use in young adolescents. BMC Psychiatry, 12(1), 116. doi:10.1186/1471-244X-12-116.
- Macarthur, G. J., Sean, H., Deborah M, C., Matthew, H., & Rona, C. (2016). Peer‐led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11–21 years: a systematic review and meta‐analysis. Addiction (Abingdon, England), 111(3), 391–407. doi:10.1111/ADD.13224.
- Marlatt, G. A., & Witkiewitz, K. (2010). Update on harm-reduction policy and intervention research. In Annual Review of Clinical Psychology, 6Issue(1), 591–606. (Annu Rev Clin Psychol. doi:10.1146/annurev.clinpsy.121208.131438.
- Mason, M. J., Campbell, L., Way, T., Keyser-Marcus, L., Benotsch, E., Mennis, J., Zhang, J., King, L., May, J., & Stembridge, D. R. (2015). Development and Outcomes of a Text Messaging Tobacco Cessation Intervention with Urban Adolescents. Substance Abuse, 36(4), 500–506. doi:10.1080/08897077.2014.987946.
- Mays, D., Phan, L., Johnson, A. C., Tercyak, K. P., Snow, K., Luta, G., Rehberg, K., & Lipkus, I. (2020). Results of a Single Arm Pilot Study of a Mobile Messaging Intervention for Hookah Tobacco Cessation in Young Adults. Tobacco Use Insights, 13, 1179173X20915200. doi:10.1177/1179173x20915200.
- Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change, 3rd edition. In Motivational interviewing: Helping people change., 3rd edition. Guilford Press.
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D., Antes, G., Atkins, D., Barbour, V., Barrowman, N., Berlin, J. A., Clark, J., Clarke, M., Cook, D., D’Amico, R., Deeks, J. J., Devereaux, P. J., Dickersin, K., Egger, M., Ernst, E., … Tugwell, P, PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. In Annals of Internal Medicine, 151Issue (4), 264–269, W64. (Ann Intern Med. doi:10.7326/0003-4819-151-4-200908180-00135.
- Müssener, U., Linderoth, C., Thomas, K., & Bendtsen, M. (2020). MHealth smoking cessation intervention among high school students: 3-month primary outcome findings from a randomized controlled trial. PloS One, 15(3), e0229411. doi:10.1371/journal.pone.0229411.
- Musyoka, C. M., Mbwayo, A., Donovan, D. M., & Mathai, M. (2021). mHealth-based peer mentoring for prevention of alcohol and substance abuse among first year university students: protocol for quasi-experimental intervention. Journal of Substance Use, 26(1), 53–59. doi:10.1080/14659891.2020.1766131.
- Nawi, A. M., Ismail, R., Ibrahim, F., Hassan, M. R., Manaf, M. R. A., Amit, N., Ibrahim, N., & Shafurdin, N. S. (2021). Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health, 21(1), 2088. doi:10.1186/s12889-021-11906-2.
- Nwosu, A., Boardman, S., Husain, M. M., & Doraiswamy, P. M. (2022). Digital therapeutics for mental health: Is attrition the Achilles heel? Frontiers in Psychiatry, 13, 900615. doi:10.3389/FPSYT.2022.900615/BIBTEX.
- Obermayer, J. L., Riley, W. T., Asif, O., & Jean-Mary, J. (2004). College smoking-cessation using cell phone text messaging. Journal of American College Health : J of ACH, 53(2), 71–78. doi:10.3200/JACH.53.2.71-78.
- O’Logbon, J., Williamson, C., Wickersham, A., & Leightley, D. (2023). March 17) Supplementary figures for “The effectiveness of digital health technologies for reducing substance use among young people: a systematic review & meta-analysis. doi:10.17605/OSF.IO/R6XG5.
- Oosterveen, E., Tzelepis, F., Ashton, L., & Hutchesson, M. J. (2017). A systematic review of eHealth behavioral interventions targeting smoking, nutrition, alcohol, physical activity and/or obesity for young adults. In Preventive Medicine, 99, 197–206. (Prev Med. doi:10.1016/j.ypmed.2017.01.009.
- Patten, C. A., Croghan, I. T., Meis, T. M., Decker, P. A., Pingree, S., Colligan, R. C., Dornelas, E. A., Offord, K. P., Boberg, E. W., Baumberger, R. K., Hurt, R. D., & Gustafson, D. H. (2006). Randomized clinical trial of an Internet-based versus brief office intervention for adolescent smoking cessation. Patient Education and Counseling, 64(1-3), 249–258. doi:10.1016/j.pec.2006.03.001.
- Patton, G. C., Coffey, C., Carlin, J. B., Degenhardt, L., Lynskey, M., & Hall, W. (2002). Cannabis use and mental health in young people: Cohort study. BMJ (Clinical Research ed.), 325(7374), 1195–1198. doi:10.1136/bmj.325.7374.1195.
- Pbert, L., Druker, S., Crawford, S., Frisard, C., Trivedi, M., Osganian, S. K., & Brewer, J. (2020). Feasibility of a Smartphone App with Mindfulness Training for Adolescent Smoking Cessation: Craving to Quit (C2Q)-Teen. Mindfulness, 11(3), 720–733. doi:10.1007/s12671-019-01273-w.
- Peacock, A., Leung, J., Larney, S., Colledge, S., Hickman, M., Rehm, J., Giovino, G. A., West, R., Hall, W., Griffiths, P., Ali, R., Gowing, L., Marsden, J., Ferrari, A. J., Grebely, J., Farrell, M., & Degenhardt, L. (2018). Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. In Addiction (Abingdon, England), 113Issue (10), 1905–1926. (Addiction. doi:10.1111/add.14234.
- Perikleous, E. P., Steiropoulos, P., Paraskakis, E., Constantinidis, T. C., & Nena, E. (2018). E-Cigarette Use Among Adolescents: An Overview of the Literature and Future Perspectives. Frontiers in Public Health, 6, 86. doi:10.3389/FPUBH.2018.00086.
- Quilty, L., Agic, B., Coombs, M., Kristy, B. l., Shakespeare, J., Spafford, A., Besa, R., Dematagoda, S., Patel, A., Persaud, R., & Buckley, L. (2021). Benefits of Digital Health Resources for Substance Use Concerns in Women: Scoping Review. JMIR Mental Health, 8(6):E25952 8(6), e25952. https://Mental.Jmir.Org/2021/6/E25952, doi:10.2196/25952.
- Quilty, L. C., Wardell, J. D., Garner, G., Elison-Davies, S., Davies, G., Klekovkina, E., Corman, M., Alfonsi, J., Crawford, A., de Oliveira, C., & Weekes, J. (2022). Peer support and online cognitive behavioural therapy for substance use concerns: protocol for a randomised controlled trial. BMJ Open, 12(12), e064360. doi:10.1136/bmjopen-2022-064360.
- Ramo, D. E., Thrul, J., Delucchi, K. L., Hall, S., Ling, P. M., Belohlavek, A., & Prochaska, J. J. (2018). A randomized controlled evaluation of the tobacco status project, a Facebook intervention for young adults. Addiction, 113(9), 1683–1695. doi:10.1111/add.14245.
- White, H. R., & Labouvie, E. W. (1989). Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol, 50(1), 30–37. doi:10.15288/jsa.1989.50.30.
- Riley, W., Obermayer, J., & Jean-Mary, J. (2008). Internet and mobile phone text messaging intervention for college smokers. Journal of American College Health, 57(2), 245–248. doi:10.3200/JACH.57.2.245-248.
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption‐II. Addiction (Abingdon, England), 88(6), 791–804. doi:10.1111/j.1360-0443.1993.tb02093.x.
- Saxton, J., Rodda, S. N., Booth, N., Merkouris, S. S., & Dowling, N. A. (2021). The efficacy of Personalized Normative Feedback interventions across addictions: A systematic review and meta-analysis. PloS One, 16(4), e0248262. doi:10.1371/JOURNAL.PONE.0248262.
- Scott-Sheldon, L. A. J., Lantini, R., Jennings, E. G., Thind, H., Rosen, R. K., Salmoirago-Blotcher, E., & Bock, B. C. (2016). Text Messaging-Based Interventions for Smoking Cessation: A Systematic Review and Meta-Analysis. JMIR mHealth and uHealth, 2016;4(2):E49 4(2), e5436. https://Mhealth.Jmir.Org/2016/2/E49, doi:10.2196/MHEALTH.5436.
- Settipani, C. A., Hawke, L. D., Virdo, G., Yorke, E., Mehra, K., & Henderson, J. (2018). Social Determinants of Health among Youth Seeking Substance Use and Mental Health Treatment. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27(4), 213–221. 213./pmc/articles/PMC6254257/
- Shiffman, S., Waters, A. J., & Hickcox, M. (2004). The Nicotine Dependence Syndrome Scale: A multidimensional measure of nicotine dependence. Nicotine & Tobacco Research : official Journal of the Society for Research on Nicotine and Tobacco, 6(2), 327–348. doi:10.1080/1462220042000202481.
- Shrier, L. A., Rhoads, A., Burke, P., Walls, C., & Blood, E. A. (2014). Real-time, contextual intervention using mobile technology to reduce marijuana use among youth: A pilot study. Addictive Behaviors, 39(1), 173–180. doi:10.1016/j.addbeh.2013.09.028.
- Simmons, V. N., Heckman, B. W., Fink, A. C., Small, B. J., & Brandon, T. H. (2013). Efficacy of an experiential, dissonance-based smoking intervention for college students delivered via the Internet. Journal of Consulting and Clinical Psychology, 81(5), 810–820. doi:10.1037/a0032952.
- Skov-Ettrup, L. S., Ringgaard, L. W., Dalum, P., Flensborg-Madsen, T., Thygesen, L. C., & Tolstrup, J. S. (2014). Comparing tailored and untailored text messages for smoking cessation: A randomized controlled trial among adolescent and young adult smokers. Health Education Research, 29(2), 195–205. doi:10.1093/her/cyt112.
- Sobell, L. C., & Sobell, M. B. (1992). Timeline Follow-Back. In Measuring Alcohol Consumption. (pp. 41–72). Humana Press. doi:10.1007/978-1-4612-0357-5_3.
- Squeglia, L. M., Jacobus, J., & Tapert, S. F. (2009). The influence of substance use on adolescent brain development. Clinical EEG and Neuroscience, 40(1), 31–38. doi:10.1177/155005940904000110.
- Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., Henry, D., Altman, D. G., Ansari, M. T., Boutron, I., Carpenter, J. R., Chan, A.-W., Churchill, R., Deeks, J. J., Hróbjartsson, A., Kirkham, J., Jüni, P., Loke, Y. K., Pigott, T. D., … Higgins, J. P. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ (Online), 355, i4919. doi:10.1136/bmj.i4919.
- Stoyanov, S. R., Hides, L., Kavanagh, D. J., & Wilson, H. (2016). Development and validation of the user version of the mobile application rating scale (uMARS). JMIR mHealth and uHealth, 4(2), e5849. doi:10.2196/mhealth.5849.
- Suffoletto, B., Kristan, J., Chung, T., Jeong, K., Fabio, A., Monti, P., & Clark, D. B. (2015). An interactive text message intervention to reduce binge drinking in young adults: A randomized controlled trial with 9-month outcomes. PloS One, 10(11), e0142877. doi:10.1371/journal.pone.0142877.
- Sussman, S., Skara, S., & Ames, S. L. (2008). Substance abuse among adolescents. Substance Use & Misuse, 43 Issues(12-13), 1802–1828. In (Taylor and Francis Inc. doi:10.1080/10826080802297302.
- Tait, R. J., & Christensen, H. (2010). Internet-based interventions for young people with problematic substance use: A systematic review. In Medical Journal of Australia, 192Issue(S11), S15–S21. (John Wiley & Sons, Ltd. doi:10.5694/j.1326-5377.2010.tb03687.x.
- Thomas, R. E., Lorenzetti, D., & Spragins, W. (2011). Mentoring adolescents to prevent drug and alcohol use. The Cochrane Database of Systematic Reviews, 11(11), CD007381. doi:10.1002/14651858.CD007381.PUB2.
- Trudeau, K. J., Black, R. A., Kamon, J. L., & Sussman, S. (2017). A Randomized Controlled Trial of an Online Relapse Prevention Program for Adolescents in Substance Abuse Treatment. Child & Youth Care Forum, 46(3), 437–454. doi:10.1007/s10566-016-9387-5.
- United Nations Children’s Fund. (2017). The State of the World’s Children 2017. https://www.unicef.org/reports/state-worlds-children-2017
- Voogt, C. v., Poelen, E. A. P., Kleinjan, M., Lemmers, L. A. C. J., & Engels, R. C. M. E. (2013). The effectiveness of the “what do you drink” web-based brief alcohol intervention in reducing heavy drinking among students: A two-arm parallel group randomized controlled trial. Alcohol and Alcoholism (Oxford, Oxfordshire), 48(3), 312–321. doi:10.1093/alcalc/ags133.
- Walters, S. T., Vader, A. M., & Harris, T. R. (2007). A controlled trial of web-based feedback for heavy drinking college students. Prevention Science : The Official Journal of the Society for Prevention Research, 8(1), 83–88. doi:10.1007/s11121-006-0059-9.
- Walton, M. A., Bohnert, K., Resko, S., Barry, K. L., Chermack, S. T., Zucker, R. A., Zimmerman, M. A., Booth, B. M., & Blow, F. C. (2013). Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: One year outcomes. Drug and Alcohol Dependence, 132(3), 646–653. doi:10.1016/j.drugalcdep.2013.04.020.
- Wickersham, A., Petrides, P. M., Williamson, V., & Leightley, D. (2019). Efficacy of mobile application interventions for the treatment of post-traumatic stress disorder: A systematic review. In Digital Health. (Vol. 5). SAGE PublicationsSage UK. doi:10.1177/2055207619842986.
- Witkiewitz, K., Desai, S. A., Bowen, S., Leigh, B. C., Kirouac, M., & Larimer, M. E. (2014). Development and evaluation of a mobile intervention for heavy drinking and smoking among college students. Psychology of Addictive Behaviors : journal of the Society of Psychologists in Addictive Behaviors, 28(3), 639–650. doi:10.1037/a0034747.
- Woodruff, P. G., Boushey, H. A., Dolganov, G. M., Barker, C. S., Yang, Y. H., Donnelly, S., Ellwanger, A., Sidhu, S. S., Dao-Pick, T. P., Pantoja, C., Erle, D. J., Yamamoto, K. R., & Fahy, J. V. (2007). Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proceedings of the National Academy of Sciences of the United States of America, 104(40), 15858–15863. doi:10.1073/pnas.070741310417898169
- Woodruff, S. I., Edwards, C. C., Conway, T. L., & Elliott, S. P. (2001). Pilot test of an Internet virtual world chat room for rural teen smokers. The Journal of Adolescent Health : official Publication of the Society for Adolescent Medicine, 29(4), 239–243. doi:10.1016/S1054-139X(01)00262-2.
- World Health Organisation. (2019). WHO guideline: recommendations on digital interventions for health system strengthening: evidence and recommendations. World Health Organization.
- World Health Organisation. (2022). Adolescent and Young Adult Health WHO. WHO Fact Sheet, 2022. https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions
- World Health Organization. (2011). mHealth: new Horizons for Health through Mobile Technologies: second Global Survey on eHealth, https://apps.who.int/iris/handle/10665/44607
- Ybarra, M. L., Holtrop, J. S., Prescott, T. L., Rahbar, M. H., & Strong, D. (2013). Pilot RCT results of stop my smoking USA: A text messaging-based smoking cessation program for young adults. Nicotine & Tobacco Research : official Journal of the Society for Research on Nicotine and Tobacco, 15(8), 1388–1399. doi:10.1093/ntr/nts339.