Abstract
Purpose: The role of the physical environment in communication between health-care professionals and persons with communication problems is a neglected area. This study provides an overview of factors in the physical environment that play a role in communication during conversations between people who are communication vulnerable and health-care professionals.
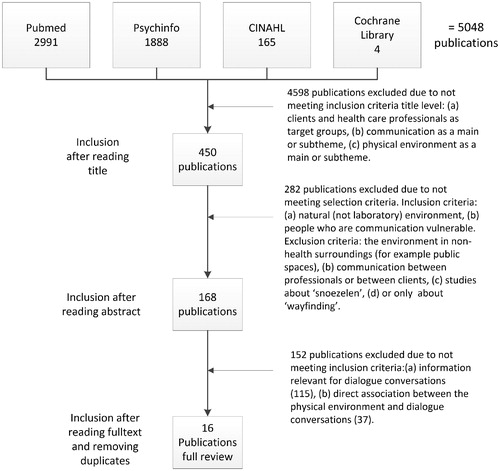
Method: A scoping review was conducted using the methodological framework of Arksey and O’Malley. The PubMed, PsycINFO, CINAHL and Cochrane Library databases were screened, and a descriptive and thematic analysis was completed.
Results: Sixteen publications were included. Six factors in the physical environment play a role in conversations between people who are communication vulnerable and health-care professionals: (1) lighting, (2) acoustic environment, (3) humidity and temperature, (4) setting and furniture placement, (5) written information, and (6) availability of augmentative and alternative communication (AAC) tools. These factors indicated barriers and strategies related to the quality of these conversations.
Conclusions: Relatively small and simple strategies to adjust the physical environment (such as adequate lighting, quiet environment, providing pen and paper) can support people who are communication vulnerable to be more involved in conversations. It is recommended that health-care professionals have an overall awareness of the potential influence of environmental elements on conversations.
The physical environment is an important feature in the success or disturbance of communication.
Small adjustments to the physical environment in rehabilitation can contribute to a communication-friendly environment for conversations with people who are communication vulnerable.
Professionals should consider adjustments with regard to the following factors in the physical environment during conversations with people who are communication vulnerable: lighting, acoustic environment, humidity and temperature, setting and furniture placement, written information, and availability of AAC (augmentative and alternative communication tools).
Implications for rehabilitation
Introduction
Effective communication in conversations between clients and professionals plays an important role in client-centred care, shared decision making and preventable adverse events in health-care.[Citation1–5] Their conversations often relate to (health-related) goals, activity choices, medical treatment, and the evaluation of treatment. Such conversations between clients and health-care professionals are often complicated and multidimensional; this is partly due to the complexity of communication itself, but is also due to time constraints, emotions, different expectations and factors in the social and physical environment.[Citation5]
Conversations are even more challenging if a client is communication vulnerable.[Citation6] There are different definitions of people who are communication vulnerable in literature.[Citation7,Citation8] We define people who are communication vulnerable as people who, due to a disease or medical condition, have difficulty expressing themselves and/or understanding information in particular environments or situations. Their communication difficulties can be mild to severe, and can be due to their sensory, emotional, physical, or cognitive (dis)abilities.[Citation9] In this paper we focus on people who are communication vulnerable due to neurological disorders.[Citation10]
According to the International Classification of Functioning, Disability and Health (ICF),[Citation11] the physical, social and attitudinal environment has an impact on conversations. A great deal of research has been conducted regarding the impact of the social and attitudinal environment on conversations, and more specifically the personal skills required to communicate effectively with clients in conversations.[Citation12–14] Less attention has been paid to the impact of the physical environment on conversations in general and in particular to the quality of conversations between people who are communication vulnerable and health-care professionals. The physical environment has an influence on people’s abilities to participate and engage in activities.[Citation11] The ICF defines the physical environment as the natural environment, human-made changes to the environment and products and technology.[Citation15] Products and technology involve naturally occurring things (e.g. trees and plants), fabricated things (e.g. chairs, written information) and technological objects (e.g. computers).[Citation11,Citation16] Research has shown that factors in the physical environment have an impact on the activities and communication of people who experience communication difficulties.[Citation17] Examples of factors influencing conversations are noise and the arrangement of furniture.[Citation17]
Since the physical environment and other ICF environmental factors (support and relationships, attitudes, and services, systems and policies) have a reciprocal relationship,[Citation18] more knowledge is needed about the impact of the physical environment in order for professionals and health-care systems to create communication friendly environments. Adapting or modifying existing physical environments, and designing new environments that promote universal communication access, is important.[Citation19]
A literature review by O’Halloran and colleagues concentrated on the acute hospital setting when describing the environmental (both social and physical) barriers and facilitators that play a role in the communication between professionals and people with communication disability.[Citation20] Other studies focus on how the physical environment can be adjusted for a group of people with a specific illness or characteristic, such as aphasia friendly environments [Citation17] or environments for people with dementia.[Citation21] O’Halloran concludes that more insights are needed about the factors in physical environments when communicating with people who have had a stroke, traumatic brain injury or who have dementia.[Citation20] Neurological disorders often lead to communication difficulties. People with different diagnoses experience different communication difficulties and needs, and therefore physical environments should be created that contribute to the communicative needs of specific individuals. Many of these communicative needs, however, may be applicable for more than one person, or for more than one diagnosis. When looking at the communicative needs of a larger target group, communication accessible environments can be created that support communication for a large group of people who are communication vulnerable, irrespective of a specific diagnosis.
The role of the physical environment in communication is a neglected area, and an up-to-date review of the literature is missing. A better understanding of communication friendly environments for conversations with health-care professionals can contribute to more accessible and empowering client-centred care for people who are communication vulnerable.[Citation20,Citation22] This literature review takes a broad look at health-care settings, and focuses on the target group of people who are communication vulnerable due to neurological disorders, since many people with neurological disorders are communication vulnerable. The aim of this scoping review is to provide an overview of factors in the physical environment that play a role in communication during conversations between people who are communication vulnerable and health-care professionals.
Methods
A scoping review was conducted to provide an extensive overview of the literature related to factors in the physical environment that play a role in communication between people who are communication vulnerable and health-care professionals. Scoping reviews are suitable for studying broad topics, are used to comprehensively and systematically map the relevant literature, and to identify key concepts and gaps in research.[Citation23,Citation24] The current scoping review was conducted using the methodological framework of Arksey and O’Malley.[Citation23] This framework identifies five stages in conducting a scoping study; the methods used in the current review will be described according to these stages.
Identifying the research question
The research question for this review was: which factors in the physical environment play a role in communication between people who are communication vulnerable and health-care professionals, during conversations in health-care settings?
Identifying relevant studies
Published scientific literature was searched via electronic scientific databases (PubMed, PsycINFO, CINAHL and the Cochrane Library) and reference lists in order to obtain a comprehensive set of literature on this topic.
The research team developed a list of search terms and filtering options based on orientation searches, which led to search outcomes that best fitted the research question. A library expert was consulted for advice on search strategies in the electronic databases. A strategy for searching PubMed was used as the main protocol, and modified for other databases. The keywords were applied to titles and abstracts.
Three main keywords were combined using the Boolean term “AND”. The first main terms were “adult” AND “communication disorders” in combination with neurological disorders that may affect communication: OR aphasia, OR dementia, OR Parkinson’s disease, OR dysarthria, OR amyotrophic lateral sclerosis, OR multiple sclerosis, OR brain injuries, OR stroke. We chose to do a broad search on communication disorders and used some specific diagnoses (using “OR”) to search for more literature about diagnoses which are often linked to communication difficulties due to neurological conditions in the literature. Our first objective was to search only “communication disorders”, however, we found during several orientation searches that adding some neurological search terms that are often linked to communication difficulties gave more relevant search outcomes. We therefore used the Boolean term ‘OR’, so as not to exclude any other neurological diagnosis.
The second main keyword “environment” was used including the following related terms: OR environment design, OR health facility environment, OR hospital design, OR construction. Finally, the third main keyword, “communication”, was used with the following related terms: OR health communication, OR communication barriers, OR communication aids for disabled OR interpersonal relations. The keyword “conversations” was specifically not used because in Medical Subject Headings (MESH) this is linked to interviews, and pilot searches revealed that this led to irrelevant search outcomes. The MESH term “dialogue” was not used because it led to outcomes related to drama. The MESH term “discussion” was also not used because it led to outcomes related to ethics, focus groups and motivational interviewing. The keywords “computer communication networks” and “social environment” were excluded using the Boolean term “NOT”, since these produced irrelevant output, with no focus on the physical environment. No publication date restriction was used in the search. The following general inclusion criteria were used to filter the search: published in English, Dutch or German languages, adults and research about health-care settings.
Study selection
In the study selection phase, the relevance of the literature was assessed in three steps: title level, abstract level and full text level. In the first selection step, three researchers (SS, RD, HS) assessed the titles independently, using a three-point scale (0 = irrelevant; 1 = possibly relevant; 2 = relevant). These scores were totalled and articles with scores of 2 or more were included in the sample. Consequently, any uncertainties or discrepancies at this early stage in the review did not eliminate publications for assessment at the abstract level. Predefined inclusion criteria at the title level were: (a) people who are communication vulnerable and health-care professionals as the target groups, (b) communication as a main theme or subtheme, and (c) physical environment as a main theme or subtheme.
During the second selection step, at the abstract level, two researchers (SS, HS) assessed the included publications for relevance by reading the abstracts, using the same scoring procedure as in step one. These scores were summed and articles with scores of 1 or more were included in the sample. The predefined additional inclusion criteria for this level were: (a) the study had to reflect a natural (not laboratory) environment; (b) the participants in the study were communication vulnerable due to neurological disorders; (c) focus on conversations with professionals.
Exclusion criteria were: (a) studies focusing only on the environment in non-health surroundings and settings (e.g. public spaces) (studies about conversations between health-care professionals and people in the home environment were included), (b) studies focusing only on communication between professionals or between people who are communication vulnerable, (c) studies about “snoezelen” (Dutch for controlled multisensory stimulation environment), or (d) studies merely about “wayfinding”.
In the third selection step, two researchers (SS, HS) assessed the remaining full texts. To define the inclusion criteria for this level, a small subset of studies (15) was used. The final inclusion criteria were: (a) the study had to present information relevant to conversations between people who are communication vulnerable and health-care professionals, (b) the study had to present a direct association between the physical environment and conversations with professionals. The inclusion of information was not limited by the methodological quality of the research [Citation23–25]. Each article was discussed by the two researchers to decide upon inclusion or exclusion. Inconsistencies or uncertainties were discussed with a third researcher (RD) who also checked the article for the selection criteria. The reference lists of the publications included in this third step were checked for additional relevant publications.
Charting the data
After the final full text inclusion, a data extraction form was developed based on a small set of full texts and a research team consultation. This data extraction form consisted of descriptive elements (author, year, location and aim of the study, study design, study population, and setting). Two researchers (SS, HS) independently charted the data and subsequently discussed inconsistencies.
Collating, summarizing and reporting the results
A summary was made of the main characteristics of the literature, using the descriptive elements of the data extraction form. Thereafter, the researchers conducted a thematic analysis of the information in the publications. In the first phase of the thematic analysis, two researchers (SS, HS) read the publications independently and highlighted text fragments related to the scoping review research question. In the second phase, these text fragments were independently placed in an Excel file and, based on discussion, a final Excel file including all relevant information was developed. In the third phase, labels were added to the text fragments independently by the two researchers (SS, HS) and the text fragments were ordered according to these labels. Three researchers discussed the formulated labels, and developed factors and sub-factors.
Results
Based on the initial 5048 hits in the databases, 16 publications were included in this review (), published between 1989 and 2015. Two publications were included in the final selection based upon the reference list search. Of the 152 excluded publications in the full text phase, 115 publications were excluded because they were not about conversations between people who are communication vulnerable due to a neurological condition and health-care professionals. The other 37 publications were excluded because no direct association was made between communication and physical environment. The included publications comprised book chapters, discussion reports and articles about empirical research.
Figure 1. This Figure illustrates the number of publications included during each phase of this review.
Descriptive summary of the articles
The characteristics of the publications are presented in , in which the author, year and country, aim of the study, study design, study population and the setting of the studies are described. A total of 16 publications were included, consisting of two qualitative studies, seven quantitative studies, one mixed method research, one discussion report and four literature reviews. One book chapter was included. The research articles embraced a wide range of settings and target groups. These settings were: long-term care settings, hospitals, dementia facilities, acute stroke units, ALS clinics, speech and language therapy practices, and professionals visiting the home environment. Various target groups within the scope of “people who are communication vulnerable” were included in the publications: for example people with dysarthria, aphasia, dementia, Parkinson’s disease, or ALS.
Table 1. Descriptive summary of studies included in the scoping review (in alphabetical order).
Thematic summary of the articles
A thematic analysis of the articles revealed factors in the physical environment that influence the conversations between people who are communication vulnerable and health-care professionals. These factors were: (1) lighting (3 articles); (2) acoustic environment (11 articles); (3) humidity and temperature (3 articles); (4) setting and furniture placement (8 articles); (5) written information (5 articles); and (6) availability of augmentative and alternative communication (11 articles). Some articles describe more than one factor. The factors are further described using sub-factors in which barriers and strategies were identified (). First, the factors with regard to human-made changes to the environment are described, followed by the factors related to products and technology (written information and AAC) [Citation15]. Since the results are a thematic summary, the order of the factors does not give an indication of their relevance or priority.
Figure 2. Factors in the physical environment which play a role in conversations between people who are communication vulnerable and healthcare professionals.
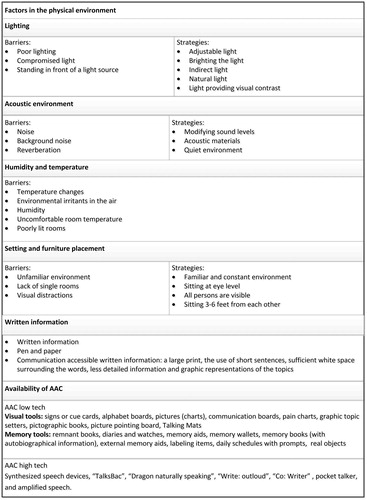
Lighting
In studies about conversations with people with dementia [Citation26] or a stroke [Citation27], lighting was described as having an influence on communication. Both the type of light and the position of lighting were considered important. Barriers mentioned were poor lighting, compromised light and standing in front of a light source [Citation27]. Day and colleagues explain that light particularly affects people with dementia because they often suffer from visual deficits, such as difficulties with colour discrimination, depth perception and sensitivity to contrast.[Citation28]
Strategies mentioned to overcome light as a barrier to communication were using adjustable light, brightening the light, using indirect lighting sources, using natural light, and using light providing visual contrast.[Citation26,Citation29] Direct light can also be filtered through sheer draperies and shades, and professionals can observe whether the faces of people speaking are in good light.[Citation26]
Acoustic environment
Sound in an environment, such as (excessive) noise and background noise, was often described as disturbing to conversations between people who are communication vulnerable and health-care professionals.
Several studies mentioned that noise is a barrier to communicating for people with aphasia,[Citation30] cognitive communication barriers,[Citation20,Citation27] spasmodic dysphonia,[Citation29] stroke,[Citation20,Citation27] dementia,[Citation26,Citation28] ALS,[Citation29,Citation31] and hospitalized elderly people.[Citation32,Citation33] In the studies of Park and Song [Citation33] and Ruan and Lambert,[Citation32] noisy environments were rated as one of the most important environmental barriers to communication by patients and nurses. O’Halloran and colleagues describe examples such as oxygen being delivered through a facemask, which can create between 75 and 90 dB of background noise at the level of the person’s ears, and radiology equipment which also creates significant background noise.[Citation20] Hull and Griffin [Citation34] described how the acoustic characteristics of environments were often not suitable for communication; hard surfaces and square or rectangular spaces create an unusual amount of reverberation and, therefore, distortion of the sound (and speech) in that environment.[Citation34]
Strategies to change the acoustic environment, such as modifying sound levels (shutting doors and windows), using better acoustic materials, or moving to a quiet environment, were often mentioned as strategies to facilitate conversations between people who are communication vulnerable and professionals.[Citation26,Citation31,Citation35] Carpeting, softer furniture and drapes could be helpful to absorb sound and reduce reverberation.[Citation34] According to Bruce and colleagues changes in the auditory environment led to more focused and less stressful interactions for the target group of people who suffered from dementia.[Citation26] Light and sound level meters were also reported as useful for monitoring environmental barriers and for making appropriate adjustments.[Citation26] Howe [Citation29] noted, however, that noise can also be a facilitator for people with Parkinson’s disease, as they spoke more loudly when background noise was present.
Humidity and temperature
Humidity and temperature were identified in three articles as important factors during conversations. Howe [Citation29] reported in her review that temperature changes, environmental irritants in the air and humidity can be barriers for people who are communication vulnerable. In the studies of Park and Song [Citation33] and Ruan and Lambert,[Citation32] uncomfortable room temperature and poorly lit rooms were identified by elderly patients and professionals as possible communication barriers in conversations.
Setting and furniture placement
The characteristics of the setting and furniture placement were also identified in the literature as having an impact on conversations. For example, unfamiliar (hospital) environments could hinder conversations between people who are communication vulnerable and professionals.[Citation32,Citation33,Citation35] Weitzel and colleagues [Citation35] explained that people who suffer from dementia in particular can be impaired by an unfamiliar environment, since it limits their ability to understand explanations, follow directions, report symptoms, ask for help, and maintain relationships with professionals. Excessive stimuli (e.g. visual or acoustic distractions) in the immediate environment can hinder people who are communication vulnerable from focusing on a conversation,[Citation29,Citation30] especially people who suffer from dementia.[Citation20] The lack of single rooms in a health-care facility can limit the opportunity to have conversations about difficult topics requiring privacy and/or fewer distractions.[Citation30]
Strategies put forward to overcome barriers in rooms and furniture include using a familiar and constant environment, rearranging furniture in the room to make sure that people sit at eye level, and that all people are completely visible and sitting at a distance between 3–6 feet from each other.[Citation26,Citation29,Citation34,Citation35] Park and Song advise providing a detailed admission orientation in which necessary adjustments are discussed,[Citation33] as the factors may contradict each other. For example rearranging the furniture may make the environment of the person who is communication vulnerable less familiar.
Written information
The availability of written information was described as a facilitator in conversations with people who are communication vulnerable, to help them understand information from professionals.[Citation27,Citation30] Research shows that people who had a stroke or with cognitive communication impairments benefited from written information. O’Halloran and colleagues found that clients with cognitive communication impairments did not receive any written information to help them recall the detailed information given to them verbally during discharge.[Citation30] When providing written information it is essential that the written information is communicatively accessible for the different target groups.[Citation17,Citation20] Suggested strategies to enhance the communication accessibility of written information are: large print, the use of short sentences, sufficient white space surrounding the words, less detailed information, and graphic representations of the topics.[Citation17,Citation27,Citation29,Citation30] The use of pen and paper can also be beneficial in conversations between these target groups and professionals.[Citation17] Pen and paper can be used as a strategy to write keywords, use drawings or prompt clients to write.[Citation36] Dialog notebooks can be used in which patients or professionals write their notes during conversations.[Citation36] O’Halloran and colleagues noted that is it important that pen and paper are directly available during conversations, to help clients to express themselves.[Citation20]
Augmentative and alternative communication
Several articles noted the availability of augmentative and alternative communication tools (AAC) as communication-facilitating objects in the physical environment.[Citation17,Citation20,Citation26,Citation27,Citation30] According to the literature, the availability of AAC can facilitate and support communication between people who are communication vulnerable and professionals.[Citation17,Citation20,Citation26] AAC should be tailored to the needs of the person concerned.[Citation17,Citation27,Citation30] Both low tech AAC (non-electronic) and high tech AAC (electronic) were mentioned in the included publications.
Low tech AAC
The literature explains that people who are communication vulnerable can benefit from non-electronic visual tools or information during conversations,[Citation20] such as signs or cue cards,[Citation26] alphabet boards,[Citation17,Citation20,Citation30] pictures (charts),[Citation30,Citation36] communication boards,[Citation30] pain charts,[Citation30] graphic topic setters,[Citation17,Citation37] pictographic books,[Citation38] picture pointing boards,[Citation36] translated picture resources,[Citation36] and tools such as Talking Mats [Citation17,Citation29]. Visual cues were used to increase communication effectiveness (e.g. for people who suffer from dementia), or to help with following instructions (e.g. for people with communication disabilities).[Citation27,Citation30]
Weitzel and colleagues [Citation35] and Bruce and colleagues [Citation26] described that augmentative aids which focus on compensating memory have also proved to be valuable in improving conversations. Examples of these aids are: remnant books, diaries and watches, memory aids, memory wallets, memory books (with autobiographical information), external memory aids, labelling items, daily schedules with prompts and the use of real objects to aid communication.[Citation26,Citation35]
High tech AAC
High tech electronic AAC were mentioned to support conversations, mostly facilitating verbal expression. Examples are synthesized speech devices,[Citation29] “TalksBac”,[Citation17,Citation29] “Dragon naturally speaking”,[Citation17] “Write: outloud”,[Citation17] “Co: Writer”,[Citation17] and amplified speech.[Citation27] Howe and colleagues reported in two publications [Citation17,Citation29] that electronic AAC systems such as synthesized speech devices serve as facilitators to support conversations for people with aphasia and dysarthria. Another AAC that appeared to be helpful in supporting communication for people who suffer from severe aphasia, was the program “TalksBac”.[Citation17,Citation29,Citation39] Waller and colleagues,[Citation39] found that the use of TalksBac led to an increase in the communication-vulnerable person’s control of the conversation, and an increase in the communication partner’s understanding of the person who is communication vulnerable. Amplified speech of good sound quality can also support conversations with professionals for people who, for example, suffer from a communicative impairment.[Citation27]
Discussion
This scoping review aimed to provide an overview of factors in the physical environment that contribute to communication in conversations between people who are communication vulnerable and health-care professionals. In total, 16 publications were included, containing various types of publications (book chapters, discussion papers, and research articles) and different types of research (literature reviews, qualitative and quantitative designs). The findings revealed six factors that can have an influence on conversations: (1) lighting, (2) acoustic environment, (3) humidity and temperature, (4) setting and furniture placement, (5) written information, and (6) the availability of AAC.
The findings of the studies in the current review did not always explain why the factors in the physical environment had a positive or negative influence on conversations. For example, in the studies by Park and Song [Citation33] and Ruan and Lambert,[Citation32] a questionnaire was used to explore the communication barriers perceived by older patients and nurses. The results of this questionnaire included, for example, the factors “uncomfortable room temperature” and “poorly lit room”. Due to the nature of the data collection method, there was no further insight about how and why room temperature and poorly lit rooms influenced communication.
The results in the included studies were based upon observations from the perspective of the researcher,[Citation27,Citation30,Citation37–39] the views of health-care professionals,[Citation26,Citation30,Citation32,Citation33] the existing literature or the knowledge of the authors themselves.[Citation20,Citation28,Citation29,Citation34,Citation35] It was striking that in most of the included studies the perspective of people who are communication vulnerable themselves is lacking; although their point of view should be leading. Only four studies included the views of people who were communication vulnerable in their research,[Citation30–33] leading to an insufficient insight into the experienced facilitators and barriers of people who are communication vulnerable.
Since this study did not examine the quality of the studies reviewed, readers should not perceive the results as proven effects, but (according to the aim of this scoping review) as factors that are important to consider during conversations between people who are communication vulnerable and health-care professionals. The methodologies and designs in the articles were not always described in detail; for example in the Howe study [Citation29] the method was described as a “review”, but it did not specify what kind of review.
In this review the well-established Arksey and O’Malley framework [Citation23] was used to systematically conduct a scoping review from scientific databases.
The use of the ICF as a theoretical foundation to describe the physical environment contributed to a widespread acknowledged interdisciplinary definition of the studied area. In this review, reports written in English, Dutch as well as German were considered, however it is possible that studies written in other languages could also have met the inclusion criteria.
Several challenges relating to the search strategy will be further discussed. Searching for literature about the physical environment was a challenge since the term is not commonly used in research, and it is not a MESH term, although the term “physical environment” is an acknowledged term in the ICF. We used multiple synonyms to ensure that all relevant publications about the physical environment were included. Furthermore, in the search process we used the keyword “communication disorders” to include studies about people with communication disorders. We added neurological diagnoses that are often linked to communication difficulties with the Boolean operator “OR” to further expand our literature search. We did not include all neurological search terms, since this would lead to an enormous number of terms and therefore also publications. If a publication was found about another neurological diagnosis which was not included as a MESH term, but was related to the communication difficulties of the client, it was included during the study selection phase. Despite the rigorous search process, some studies could have been missed.
Although AAC are part of the physical environment as “objects”, we did not specifically include AAC in our search strategy since we did not focus on AAC as dedicated devices for individuals, but as objects that could be present in the physical environment to support conversations. The research on AAC is extensive, and focusing on specific AAC would blur the emphasis on the physical environment.
The current scoping review excluded studies about children, because their communication difficulties often relate to their development and require different, specific adjustments. Conversations with children also have a different process, as parents most often play an important role in their health-care process and decisions.
In this review, we specifically searched for information about the role of the physical environment in health-care settings, since effective communication is essential in these settings for client-centred care and shared decision making.[Citation1,Citation4] The first setting to provide communication friendly environments should be the health-care setting, since these settings are fundamentally aimed at supporting people with an impairment. Health-care environments could set an example for other environments, such as public spaces.
Current research about communication between clients and professionals often focuses on the attitudinal and social environment; for example verbal communication strategies are studied, such as types of questions, double checking, listening etc.[Citation40,Citation41] This scoping review reveals that factors in the physical environment also have an important impact on conversations. These factors might also be supportive for conversations with clients who are not necessarily communication vulnerable. We can wonder why we provide wheelchair access ramps, but are often unaware that we can also provide communication access ramps.[Citation42,Citation43]
The literature described strategies that can be used to implement changes to the physical environment: the awareness of health-care professionals, and the use of toolkits or questionnaires. An overall awareness by health-care professionals of the potential influence of environmental elements on conversations is recommended. O’Halloran and colleagues [Citation30] argued, therefore, that professionals should receive knowledge about interventions related to adjusting the physical environment to improve conversations. Howe [Citation29] focused on speech and language pathologists, who should address both personal and environmental factors when providing interventions for people who are communication vulnerable. Bruce and colleagues [Citation26] developed a toolkit, the Environment and Communication Assessment Toolkit (ECAT) which provides an assessment of the physical environment, information about the impact of the environment on communication, and resources to make recommendations and implement interventions. This toolkit includes, for example, a tool that helps to identify the appropriate text size for a person with dementia.[Citation26] The results of their study showed that the ECAT increased the awareness of environmental modifications, influenced the practice of recommending environmental modifications, and was beneficial in diverse elements of clinical practice. The current review revealed no other assessments that examine the physical environment. Such assessments do exist; however, these probably did not emerge in this search because they often contain only a small number of questions about the environment in relation to communication. Examples are: the Craig Handicap Assessment and Reporting Technique (CHART),[Citation44] Measure of the Quality of the Environment (MQE),[Citation45] Measure of the Stroke Environment (MOSE),[Citation46] and the Stroke and Aphasia Quality of Life Scale-39 (SAQOL-39).[Citation47] Furthermore, assessments often focus on one diagnosis, such as the Profile of the Communication Environment of the Adult Aphasic.[Citation48] A systematic review looking at all measures which include questions about communication friendly environments might be valuable.
Clinical implications and future research
Health-care professionals need to have a broader view of the impact of the environment and the broad range of supportive adjustments in the physical environment when communicating with people who are communication vulnerable. However, professionals often have to work in inappropriate environments [Citation49] and do not have the ability to change this environment. Professionals need the support of institutional governance and health-care systems to make the physical environments of institutions communication accessible.[Citation19] On the other hand, as the results of this review reveals, small adjustments can contribute to a communication friendly environment for conversations.
The findings of this review reveal the need for greater awareness in health-care professionals with regard to factors in the physical environment. Educational training should pay attention to the importance of the six factors, an awareness of the impact of the physical environment on conversations, and skills to adjust the environment.
Most articles in this review described observational research, and research studying the needs of people who are communication vulnerable from their own perspective, is lacking. More research is needed to address these gaps, in order to better understand the impact of the physical environment for people who are communication vulnerable, and to provide professionals with relevant tools and strategies to improve their conversations. Qualitative methods could be used in future research to better understand how people who are communication vulnerable and health-care professionals perceive the influence of the physical environment during conversations. Quantitative methods could be used to study the effect which the factors identified in this research have on conversations. Tools such as the ECAT [Citation26] could be combined for use as quantitative measurements of the physical environment.
Conclusions
Our review found that relatively small and simple strategies to adjust the environment (e.g. improving lighting, reducing noise, using pen and paper, and using AAC such as talking mats) can support communication in conversations. Adjusting the physical environment can enable people who are communication vulnerable to express themselves better, understand others better, and be involved in decisions affecting their care and daily life. It is recommended that health-care professionals have an overall awareness of the potential influence of environmental factors on conversations. To date, as this scoping review confirms, little attention has been paid to how and why these factors influence conversations, and how people who are communication vulnerable perceive them.
Disclosure statement
The authors have no conflict of interest to declare.
References
- McGilton KS, Sorin-Peters R, Sidani S, et al. Patient-centred communication intervention study to evaluate nurse-patient interactions in complex continuing care. BMC Geriatr. 2012;12:61.
- Bartlett G, Blais R, Tamblyn R, et al. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Cmaj. 2008;178:1555–1562.
- Dalemans RJ, De Witte LP, Beurskens AJ, et al. An investigation into the social participation of stroke survivors with aphasia. Disabil Rehabil. 2010;32:1678–1685.
- Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Br J Gen Pract. 1999;49:477–482.
- Sheldon LK, Barrett R, Ellington L. Difficult communication in nursing. J Nurs Scholarsh. 2006;38:141–147.
- Hemsley B, Balandin S, Worrall L. Nursing the patient with complex communication needs: time as a barrier and a facilitator to successful communication in hospital. J Adv Nurs. 2012;68:116–126.
- Blackstone SW. Augmentative communication news. Augment Commun. 2009;21:1–5.
- Costello JM, Patak L, Pritchard J. Communication vulnerable patients in the pediatric ICU: Enhancing care through augmentative and alternative communication. J Pediatr Rehabil Med. 2010;3:289–301.
- Stans SE, Dalemans R, de Witte L, et al. Challenges in the communication between 'communication vulnerable' people and their social environment: An exploratory qualitative study. Patient Educ Couns. 2013;92:302–312.
- WHO. 2015 What are neurological disorders? 2015; [cited 30-11-2015]. Available from: http://www.who.int/features/qa/55/en/
- World Health Organization. Geneva: World Health Organization; 2001; [cited 2015 Dec 15]. Available from: http://www.who.int/classifications/icf/icfbeginnersguide.pdf?ua=1
- Silverman J, Kurtz S, Draper J. Vaardig communiceren in de gezondheidszorg. Den Haag: Boom Lemma uitgevers; 2014.
- Mazzi MA, Rimondini M, Deveugele M, et al. What do people appreciate in physicians' communication? An international study with focus groups using videotaped medical consultations. Health Expect. 2013;18:1215–1226.
- Uitterhoeve RJ, Bensing JM, Grol RP, et al. The effect of communication skills training on patient outcomes in cancer care: a systematic review of the literature. Eur J Cancer Care (Engl). 2010;19:442–457.
- WorldHealthOrganization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization; 2001. [cited 2015 Nov 30]. Available from: http://www.who.int/classifications/icf/en/.
- Kielhofner G. Model of human occupation. Baltimore: Lippincott Williams & Wilkins; 2008.
- Howe TJ, Worrall LE, Hickson LMH. What is an aphasia-friendly environment? Aphasiology 2004;18:1015–1037.
- Bricout JC, Gray DB. Community receptivity: the ecology of disabled persons' participation in the physical, political and social environments. Sjdr. 2006;0:1–21.
- Hammel J, Jones R, Smith J, et al. Environmental barriers and supports to the health, function, and participation of people with developmental and intellectual disabilities: report from the State of the Science in Aging with Developmental Disabilities Conference. Disabil Health J. 2008;1:143–149.
- O'Halloran R, Hickson L, Worrall L. Environmental factors that influence communication between people with communication disability and their healthcare providers in hospital: a review of the literature within the International Classification of Functioning, Disability and Health (ICF) framework. Int J Lang Commun Disord. 2008;43:601–632.
- Soril LJ, Leggett LE, Lorenzetti DL, et al. Effective use of the built environment to manage behavioural and psychological symptoms of dementia: a systematic review. PLoS One 2014;9:e115425.
- Wylie K, McAllister L, Davidson B, et al. Changing practice: implications of the World Report on Disability for responding to communication disability in under-served populations. Int J Speech. Lang Pathol. 2013;15:1–13.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
- Halas G, Schultz AS, Rothney J, et al. A scoping review protocol to map the research foci trends in tobacco control over the last decade. BMJ Open 2015;5:e006643.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
- Bruce C, Brush JA, Sanford JA, et al. Development and evaluation of the environment and communication assessment toolkit with speech-language pathologists. Semin Speech Lang. 2013;34:42–51.
- O'Halloran R, Worrall L, Hickson L. Environmental factors that influence communication between patients and their healthcare providers in acute hospital stroke units: an observational study. Int J Lang Commun Disord. 2011;46:30–47.
- Day K, Carreon D, Stump C. The therapeutic design of environments for people with dementia: a review of the empirical research. Gerontologist 2000;40:397–416.
- Howe TJ. The ICF Contextual Factors related to speech-language pathology. Int J Speech Lang Pathol. 2008;10:27–37.
- O'Halloran R, Grohn B, Worrall L. Environmental factors that influence communication for patients with a communication disability in acute hospital stroke units: a qualitative metasynthesis. Arch Phys Med Rehabil. 2012;93:S77–S85.
- Ball LJ, Beukelman DR, Pattee GL. Communication effectiveness of individuals with amyotrophic lateral sclerosis. J Commun Disord. 2004;37:197–215.
- Ruan J, Lambert VA. Differences in perceived communication barriers among nurses and elderly patients in China. Nurs Health Sci. 2008;10:110–116.
- Park EK, Song M. Communication barriers perceived by older patients and nurses. Int J Nurs Stud. 2005;42:159–166.
- Hull RH, Griffin KM. Environmental factors in communication with older persons. Communication disorders in aging. Thousand Oaks, CA, US: Sage Publications; 1989.
- Weitzel T, Robinson S, Barnes MR, et al. The special needs of the hospitalized patient with dementia. MEDSURG Nursing 2011;20:13–19.
- Jensen LC, Lovholt AP, Sorenson IR, et al. Implementation of supported conversation for communication between nursing staff and in-hospital patients with aphasia. Aphasiology 2015;29:57–80.
- Garrett KL, Huth C. The impact of graphic contextual information and instruction on the conversational behaviours of a person with severe aphasia. Aphasiology 2002;16:523–536.
- Ho KM, Weiss SJ, Garrett KL, et al. The effect of remnant and pictographic books on the communicative interaction of individuals with global aphasia. Aac. 2005;21:218–232.
- Waller A, Dennis F, Brodie J, et al. Evaluating the use of TalksBac, a predictive communication device for nonfluent adults with aphasia. Int J Lang Commun Disord. 1998;33:45–70.
- Jesus TS, Silva IL. Toward an evidence-based patient-provider communication in rehabilitation: Linking communication elements to better rehabilitation outcomes. Clin Rehabil. 2016;30:315–328.
- Kurtz S, Silverman J, Draper J. Teaching and learning communication skills in medicine. 2nd ed. Oxford: Radcliffe Medical Press; 2005.
- Dalemans RJP. Stroke survivors with aphasia and their social participation Maastricht: Maastricht University; 2010.
- Kagan A, Gailey GF. Functional is not enough: training conversation partners for aphasic adults. San Diego: Singular Publishing Group; 1993.
- Whiteneck GG, Charlifue SW, Gerhart KA, et al. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil. 1992;73:519–526.
- Foley KR, Girdler S, Bourke J, et al. Influence of the environment on participation in social roles for young adults with down syndrome. PLoS One 2014;9:e108413.
- Babulal GM, Tabor Connor L. The measure of stroke environment (MOSE): development and validation of the MOSE in post-stroke populations with and without aphasia. Top Stroke Rehabil. 2016;1–10.
- Hilari K, Byng S, Lamping DL, et al. Stroke and Aphasia Quality of Life Scale-39 (SAQOL-39): evaluation of acceptability, reliability, and validity. Stroke 2003;34:1944–1950.
- Lubinski R, editor. Environmental systems approach to adult aphasia: New York: Lippincott, Williams & Williams; 2001.
- Hull RH. Environmental factors in communication with older persons. In: Hull RH, Griffin KM, editors. Communication disorders in aging. Michigan: SAGE Publications; 1989. p. 153–161.
- Howe TJ. The ICF contextual related to speech-language pathology. Int J Speech Lang Pathol. 2008;10:27–37.
- Weitzel T, Robinson S, Barnes MR, et al. The special needs of the hospitalized patient with dementia. Medsurg Nurs. 2011;20:13–18. quiz 9.
