Abstract
Purpose: The aim was to investigate the feasibility of introducing a novel transdiagnostic occupational rehabilitation program delivered in groups mixing participants with chronic pain, chronic fatigue and common mental disorders.
Materials and methods: Observational data on group climate and individual participation were triangulated with qualitative data from focus group interviews on the participants’ experiences with transdiagnostic groups.
Results: The study included 222 participants receiving a temporary work disability benefit. Self-reported chronic pain (75%), chronic fatigue (79%), and mental distress (62%) were prevalent and the majority reported overlapping conditions (78%). Program completion among participants was high (96%). Those completing participated actively (95%) in the program. Overall group climate was stable with moderately high engagement. Participants with clinically confirmed mental disorders (22%) showed similar outcomes. Self-reported problems with “working in a group” prior to rehabilitation were not associated with how participants experienced group climate. Qualitative data supported the findings of positive participant experiences with transdiagnostic group settings.
Conclusions: Transdiagnostic groups showed high participation rates, moderately high group engagement across symptom profiles and positive participant experiences. Implementing transdiagnostic occupational rehabilitation in groups mixing participants with chronic pain, chronic fatigue and common mental disorders was feasible and acceptable to participants.
Most research has been done on disorder-specific occupational rehabilitation programs, but emerging evidence supports a more generic approach.
Transdiagnostic therapies, such as Acceptance and Commitment Therapy (ACT), have shown promising results for both somatic and mental disorders.
The feasibility of implementing transdiagnostic rehabilitation groups, their acceptability to participants and the demand for such groups has not been established.
This study indicates that it is feasible to introduce a novel transdiagnostic group-based occupational rehabilitation program for mixed groups of sick-listed participants with chronic pain, chronic fatigue and/or common mental disorders.
Implications for rehabilitation
Introduction
Work disability comes at a high cost for both the individual and society [Citation1,Citation2]. In an effort to prevent work disability, a multitude of different occupational rehabilitation programs have been introduced within various settings and in different cultures. A common feature of these programs is that they target specific disorders, e.g., musculoskeletal disorders [Citation3] or mental disorders [Citation4–6], or even more narrow diagnostic entities such as low back pain [Citation7,Citation8]. Crossover between programs for mental and somatic disorders has been discussed [Citation9], and it has been pointed out that interventions may be applicable across different diagnoses [Citation10].
Feasibility studies in real world settings are lacking for the implementation of transdiagnostic programs within occupational rehabilitation that bridge somatic and psychiatric care. This feasibility study follows real time implementation of a novel occupational rehabilitation program that targets a population with mental and/or somatic disorders while delivering the program in a transdiagnostic group-format. The construct feasibility is approached as recommended by Bowen [Citation11]. The main focus is on the implementation of transdiagnostic groups, their acceptability to participants, and the demand for such groups.
A multifactorial rationale supports introducing transdiagnostic group-based programs: Individuals on long-term sick leave often have combinations of health complaints. For example, 98% of patients with chronic low back pain had other health complaints [Citation12], a third of patients with low back pain also had a mental disorder [Citation13], and painful physical symptoms are common among depressed persons [Citation14,Citation15]. Multiple symptom disorders and medically unexplained physical symptoms (MUPS) are commonplace and it is argued that similarities in clinical expression and underlying mechanisms outweigh differences between conditions [Citation16,Citation17]. The considerable overlap of complaints and disorders makes it challenging, if not irrelevant, for general practitioners to provide one single diagnosis to accurately describe the patient’s health problems. Substantial variability is seen between general practitioners when diagnosing patients presenting exactly the same symptoms [Citation18]. Furthermore, independent of health issues, many non-medical factors (e.g., social, and workplace-, healthcare-, and compensation system) strongly influence return to work (RTW) [Citation19]. Many authors argue that the complex causes of sick leave require a broad assessment of bio-psychosocial factors [Citation20,Citation21] and functioning [Citation22] with due attention to workplace and system factors [Citation23].
In psychotherapy transdiagnostic approaches have many advocates and citations, and studies of transdiagnostic models have shown both promise and utility [Citation24,Citation25]. Acceptance and Commitment Therapy (ACT), is based on the transdiagnostic concept that addresses both psychological and somatic distress in the form of psychological inflexibility and experiential avoidance [Citation26,Citation27]. Utilizing a transdiagnostic model as ACT opens for including participants with both mental and somatic diagnoses into the same groups. Group treatment is often the method of choice in rehabilitation settings as it is cost-effective and increases treatment capacity. Participants receiving cognitive therapy in groups report emotional benefits (e.g., self-acceptance and positive relationships with others), while effects on treatment outcome are generally equally satisfactory or better when group treatment is compared to individual treatment [Citation27–29]. Furthermore, transdiagnostic groups may contribute towards neutralizing the cleft between psyche and soma that is still deeply ingrained in modern health care, a division that is often regarded counterproductive [Citation14] and stigmatizing [Citation30] for the individuals these programs are meant to help.
Occupational rehabilitation is a highly relevant area for transdiagnostic therapy since the aim is not primarily to reduce symptoms or cure a specific disease but rather to improve work ability, a goal that carries commonality across diagnoses. Crossover between occupational rehabilitation programs for mental and somatic disorders has not been adequately operationalized and investigated in a systematic manner. Treatment strategies that take into account comorbidity are advised [Citation14,Citation31] and transdiagnostic programs are already emerging within occupational rehabilitation [Citation32] Still, some stakeholders voice anxiety about departing from more familiar diagnose-specific rehabilitation. Decision makers need knowledge on the feasibility of implementing transdiagnostic rehabilitation programs and their acceptability to participants. This paper explores key uncertainties in the design of transdiagnostic group-based occupational rehabilitation while adhering to the call for practice-based evidence [Citation33], research on heterogeneous populations [Citation34], early phase evaluation of complex interventions [Citation35–37] and exploring feasibility through mixed methods [Citation11].
Objectives
The aim of this study was to investigate the feasibility of introducing a novel occupational rehabilitation program using Acceptance and Commitment Therapy as a transdiagnostic approach delivered in groups that mixed sick-listed participants with chronic pain, chronic fatigue and common mental disorders. Key areas of focus are the implementation of transdiagnostic groups, demand for such groups and their acceptability to participants. Inference on these selected areas of feasibility is based on triangulating quantitative and qualitative data. To approach the aim, we attempt to answer three basic research questions: How did the participants in mixed groups report on group climate? What were the rates of program completion and active participation? How did the participants describe their experiences of the transdiagnostic group setting?
Materials and methods
Study design
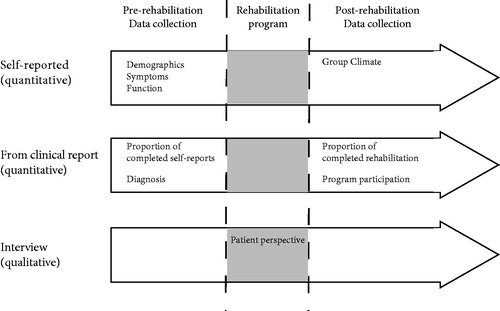
This mixed methods study included quantitative observational data and qualitative data from focus group interviews. Participants and clinicians reported observational data prior to rehabilitation and at the end of the program. Self-reported group climate as well as rates of program completion and active participation were investigated. The participants’ response rate to internet-based self-reporting from home was registered. The timeline and data sources are shown in .
Participants
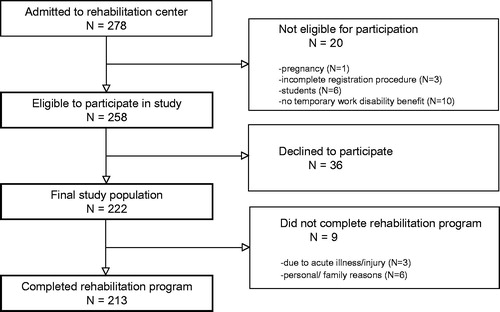
Participants were enrolled over an 18-month period from January 2012 to June 2013. They were referred for occupational rehabilitation by general practitioners or other medical specialists and were clinically screened at outpatient facilities before admission to the rehabilitation center. The clinical program and the study had the same inclusion and exclusion criteria. Inclusion criteria were: age 18–59 years, receiving a temporary work disability benefit (sick-listed >8 weeks duration, partial or full-time). The Norwegian Social Security System has two different temporary work disability benefits: sickness benefit and work assessment allowance. Both benefits require that the individual has been sick-listed by a sickness certifier (usually a general practitioner). Participants receiving either of the benefits were eligible for inclusion in the study and should have one or more of the following conditions: a musculoskeletal/other pain disorder, fatigue or a common mental disorder. Participants should have self-defined goals of increasing work participation and prior to admission be adequately assessed and treated for any specific health problems demanding critical care. Patients were expected to be able to communicate in Norwegian and to maintain basic daily care for themselves during a stay at the rehabilitation center. The exclusion criteria were: severe mental illness (ongoing mania, psychosis or suicidal orientation), active substance abuse and addiction, pregnancy or having a goal of entering/returning to studies rather than competitive work. Participants who were admitted to rehabilitation and eligible according to the above criteria were consecutively invited to participate in the study. A flow-chart of participant inclusion is given in .
Study setting
This study was nested in the clinical routine of an occupational rehabilitation program with three distinct phases: internet-based reporting from home, pre-admission clinical assessment and the occupational rehabilitation program.
Internet-based reporting from home
Before inclusion and before the first clinical assessment, the participants were asked to complete a comprehensive 376-item internet-based questionnaire from their home. A project coordinator sent the participants written information about the log-on procedure, while a unique password was sent separately to their cell phone. Before the log-on code was administered, appointment times for clinical screening were sent to the participants to ensure them that possible failure to complete the self-report questionnaire would not influence negatively on access to clinical assessment. Self-reported data was shared between clinical practitioners and researchers according to a recommended single-source [Citation38] approach to prevent repetitive collection of the same information from participants. For example, pain, fatigue and mental distress scores were of interest to the interdisciplinary clinical team as well as to researchers. Only pre-defined and clinically relevant data were accessible to clinicians in the form of self-reports in the electronic patient journal. The electronic patient journal was not accessible to researchers, who received data though separate files from the third party database.
Pre-admission clinical assessment
An outpatient multidisciplinary team at St. University Hospital, consisting of a physician, a psychologist, and a physiotherapist, assessed potential participants. This team evaluated whether the referred participants met the inclusion criteria for the study. Self-report data was used to aid clinical assessment.
On-site occupational rehabilitation program
The setting for the occupational rehabilitation program was Hysnes Occupational Rehabilitation Center, a rural division of St. University Hospital, Norway. The program included both individual and group-based sessions. Participants lived on-site and participated in 6.5-h workdays at the rehabilitation center over a consecutive period of 3.5 weeks. RTW coordinators were involved in coordinating and executing the program. Each coordinator was responsible for mentoring up to four participants during the rehabilitation program. The coordinators’ backgrounds were diverse (physical therapy, psychology, sociology, exercise physiology, nursing or other).
The program integrated mental and physical training together with work-related problem solving. The majority of sessions were group-based, but individual sessions with the RTW coordinator or other clinicians were also offered in the program. The core element of both group-sessions and individual meetings was Acceptance and Commitment Therapy (ACT) [Citation39]. Other elements of the program were mindfulness training as well as psycho-education on topics as stress-regulation, chronic symptom interpretation, nutrition, and sleep. Physical activity sessions involved strength and endurance training but also focused on improving movement patterns and countering fear of movement or tension related pain. During rehabilitation, discussions on return-to-work and focused commitment on values were stressed, rather than focusing on specific symptoms. Work-related problem solving was used to identify challenges and possibilities for reentry to work, increase readiness for work and employ coping strategies. The participants themselves made plans for work reentry in cooperation with RTW coordinators and stakeholders (general practitioner, social security advisor and employer and others relevant in the rehabilitation process) who were contacted and included in the process. The program components have been described in further detail in a related study [Citation40].
Baseline
Baseline measurements were registered pre-admission. Measurements from internet-based self-reporting of interest for this study are presented. Chronic pain was measured using a single question from the Short Form 8*: “How much bodily pain have you had the last week?” The response alternatives are: none, very mild, mild, moderate, severe, and very severe [Citation41]. This scale has been validated and used as a proxy measure of chronic pain in Norwegian population studies, using a cutoff at ≥ moderate pain [Citation42]. Chronic pain was defined as duration of 6 months or more [Citation42]. Symptom duration was also confirmed through individual assessment of clinical reports.
Chronic fatigue was measured using the 13-item Chalder Fatigue Scale [Citation43]. Each item has four response categories that are bimodaly scored as 0–0-1–1 (better than usual =0, no more than usual =0, worse than usual =1, much worse than usual =1). The first 11 items reflect symptom intensity. The cutoff was set at a score of ≥4 combined with symptom duration of 6 months or more [Citation43]. This is the recommended cutoff when using the 13-item Chalder Fatigue Scale that has been validated for a Norwegian population [Citation44]. Likert scores were also calculated.
Mental distress was measured using the 14-item Hospital Anxiety and Depression Scale (HADS) [Citation45]. The HADS is made for evaluating mental distress in populations with physical symptoms. It consists of both an anxiety and a depression scale, each having seven items. Every item has four response categories from 0 to 3, giving a maximum score on each scale of 21. Mental distress is defined as present if a score ≥8 on either the anxiety and/or the depressive scales of HADS [Citation46]. The cutoff is validated for a Norwegian population [Citation47].
Self-reported disability was assessed using two items from the 39-item Norwegian Function Assessment Scale (NFAS) that target activities closely related to functioning in group activities: “working in a group” and “participating in a conversation”. Each item has five response categories (no difficulty, little difficulty, moderate difficulty, much difficulty, could not do it). The NFAS was derived from the activities/participation dimension of the International Classification of Functioning, Disability and Health (ICF). It is used to assess the need for rehabilitation, adjustment of work demands among sick-listed persons and rights to social security benefits. The has been validated for use in a Norwegian population [Citation48], and is shown to discriminate between individuals who are expected to report different levels of disability. A clinically relevant cutoff was set at 3 and higher (“moderate disability” and more). NFAS starts with the question “Have you had difficulty with doing the following activities during the last week?” [Citation49].
Clinical assessment for mental disorders was done by psychologists prior to admission as part of the interdisciplinary assessment. Self-reported results from the Psychiatric Diagnostic Screening Questionnaire (PDSQ) [Citation50] were followed up clinically with the Structured Clinical Interview for DSM-IV (SCID-I) [Citation51]. The PDSQ is a validated 126-item screening tool that screens for the 13 most common mental disorders. It has been shown to have a high sensitivity, but somewhat lower specificity [Citation50]. If the participants scored above the cutoff on the PDSQ, or if the psychologists found other indications of psychiatric disorders, the participants were interviewed according to the SCID-I. Participants were registered as having a mental disorder if the presence of a disorder was confirmed by the SCID-I interview.
Outcome
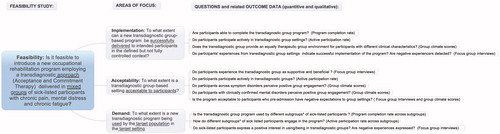
A limited set of quantitative outcome measures (Self-perceived group climate, program completion rate and active participation rate) were triangulated with data from focus group interviews. Outcome targeted key uncertainties of the program: whether transdiagnostic groups could be implemented as planned, if transdiagnostic groups settings would be acceptable to participants and whether participants would use the program (clinical demand). shows focus areas of feasibility (implementation, acceptability and demand) and how quantitative and qualitative outcome data were combined to draw inference.
Figure 3. Focus areas of feasibility (implementation, acceptability and demand) with map of how quantitative and qualitative outcome data were combined to draw inference.*Different subgroups of participants: This refers to the subgroups of participants with either different self-reported symptom (chronic pain, chronic fatigue or mental distress) or participants with/without clinically confirmed mental disorders.
Self-perceived group climate
Participants’ perception of group climate was investigated using the Group Climate Questionnaire - Short form (GCQ-S) [Citation52]. The instrument consists of 12 items rated on a 7-point Likert scale indicating extent of agreement ranging from 0 (not at all), 1 (a little bit), 2 (somewhat), 3 (moderately), 4 (quite a bit), 5 (a great deal) and 6 (extremely). These items are divided into three subscales: engagement (5 items), avoidance (3 items) and conflict (4 items). The GCQ-S assesses the individual group members perception of the climate in the group/therapeutic environment in the group [Citation52]. This instrument is not based on any particular theoretical orientation, and is thus applicable to many different group situations and formats. The GCQ-S has been widely used across different treatment populations, and its construct validity has been tested extensively [Citation53]. Internal consistency of the GCQ-S subscales has been shown to be high, with alpha coefficients ranging from 0.88 to 0.94 [Citation53]. Participants completed the GCQ-S a few days before completing rehabilitation.
Degree of participation
Degree of participation was recorded by RTW coordinators at time of discharge through two questions: (a) Did the participant complete the rehabilitation stay? (yes/no) and (b) Did the participant participate actively in individual and group sessions? (yes/no).
Participants’ experiences
Qualitative focus group interviews were performed for a convenience sample of 23 participants who were interviewed in five focus groups the day before discharge from the program. Four of the focus groups were identical with the therapy group, while one focus group comprised two therapy groups. Interviews were based on an interview guide. The guide included questions about the participants’ experiences of the different parts of the rehabilitation program, their descriptions of what they had learnt and changed during the program, and their perspectives on and expectations to life after the program. Parts of the interview data material have been used in a previous publication [Citation54]. One of the topics in the interview guide was how the participants experienced that the group therapy was conducted in a transdiagnostic setting. Data from these specific parts of the interviews are used in the present study. The interviews were conducted during the period from November 2012 until March 2013. Two of the interviews were conducted by two researchers and the other three by one researcher. The interviews lasted between 20 and 90 min and were audiotaped and transcribed verbatim. Redundant words were omitted and local dialect was changed to written language. Quotes presented were translated from Norwegian to English by the 5th author (MBR).
Data analyses
Descriptive statistics of demography, symptoms and function, as well as program participation, were given as numbers and percentages of the sample. Caseness for substantial symptom burden was dichotomized according to validated cutoff values for chronic pain, chronic fatigue and mental distress, as defined above. Since participants were clustered within rehabilitation groups, multilevel linear regression analysis was applied to be able to separate group effects from effects of individual factors, such as self-reported symptoms, group functioning or confirmed mental disorder. A “random intercept only model” was used to explore the possible contribution of belonging to a specific group on group climate [Citation55]. All analysis was predefined and performed separately for each of the three subscales of the GCQ-S (engagement, conflict and avoidance), and interclass correlation coefficients (ICC) were calculated. The associations between GCQ-S subscales and each separate symptom (chronic fatigue, chronic pain or mental distress) were analyzed in simple models adjusted for age and gender. The full model included all symptom (chronic pain, chronic fatigue and mental distress) adjusted for age and gender. The association between GCQ-S subscales and clinically confirmed mental disorder was adjusted for age and gender, as was the association between GCQ-S subscales and self-reported group functioning. Coefficients (β) were reported with 95% confidence intervals (CI). Statistical analysis was performed using STATA version 14.1 (StataCorp. 2015, College Station, TX).
Qualitative data analysis was conducted according to a phenomenological approach [Citation56]. Analyses were conducted in a group of four persons with various backgrounds, two medical doctors and two public health researchers. In addition, a fifth researcher (a psychiatrist) took part in the initial stages of analysis. Data collection continued until saturation was reached according to a group decision. Initially, interview transcripts were read and coded by the authors separately before the code list was discussed in the whole author group. Codes were then grouped into larger thematic categories, and discussed several times until consensus. The thematic categories relating to the participants’ experiences of the group setting included: (a) the participants’ expectations towards transdiagnostic group therapy before the program, (b) their experiences with transdiagnostic group therapy in general, and (c) their self-perceived benefits with the transdiagnostic setting, compared to the prospect of being in a group where all participants had the same diagnosis. The qualitative findings presented in this study are used to elaborate on the quantitative findings. Quotes from the participants are used to illustrate the findings.
Ethics, consent, and permissions
The study was approved of by the Regional Committee for Ethics in Medical Research in Mid-Norway (Ref.no. 2010/2404). All procedures followed were in accordance with the Helsinki declaration of 1975, as revised in 2000. Informed consent was obtained from all patients included in the study.
Results
Participants
In total 278 participants were admitted to the rehabilitation program. Twenty were not eligible due to pregnancy [Citation1], incomplete study registration procedure [3], student status, i.e., goal of returning to studies rather than to work [Citation6], or not being registered as receiving a temporary medical benefit [Citation10]. Thirty-six declined participation in the study, leaving 222 participants to enter the study (see ). The preclinical self- report questionnaire was successfully completed by 220 (99%) of the included participants. In total 96% of the participants fully completed the 3.5-week rehabilitation program, while nine participants had left early due to acute illness/injury [Citation3] or other personal/family reasons [Citation6]. This left 213 participants to be analyzed for all outcome measures. Further reporting is based on this sample.
Baseline
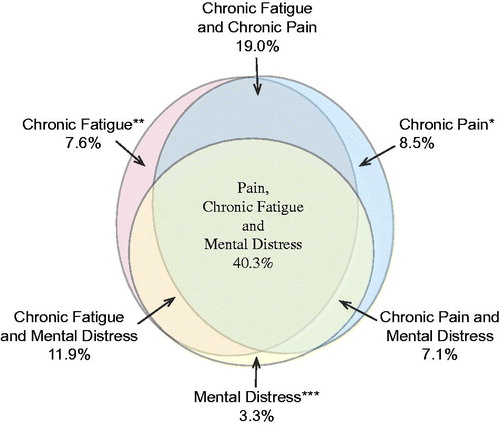
The average age of participants was 42 years (range 20–59), 80% (170/213) of participants were women, and 42% (89/213) of participants had higher education (completed college/university education). All 213 participants were receiving partial or fulltime temporary benefits due to work disability. Overall, 75% (159/212) of participants reported chronic pain (of at least moderate intensity), 79% (167/212) reported chronic fatigue, and 62% (132/212) reported symptoms of mental distress. Overlapping conditions were seen in 78% (165/211) of participants. The distribution and overlap of symptoms is illustrated in .
Figure 4. A Venn illustration of the percentage of participants presenting with chronic fatigue, chronic pain, or mental distress, and the overlap of these conditions. Note that 2.4% of participants did not present with either of the conditions.*Chronic pain: a score ≥ moderate to very severe pain and a duration of ≥6 months.**Chronic fatigue: a score of ≥4 on the Chalder Fatigue Scale and a duration of ≥6 months.***Mental distress: a score of ≥8 on either the anxiety and/or the depressive scales of the HADS.
After psychological assessment, 46 participants (22%) were diagnosed with a mental disorder according to DSM-V (SCID-I). This was further translated into a corresponding ICD-10 diagnosis. A total of 38% (76/201) of the participants reported moderate or more severe problems with “working in a group” and 33% (68/208) reported moderate or more severe problems with “participating in a conversation”.
Participants were divided into twenty-five groups with an average of 8.5 participants per group. Results for group composition showed that all groups were transdiagnostic in that they included both participants reporting mental distress and somatic symptom. In one of the groups all participants (n = 6) reported mental distress, thereof one as mental distress alone, two in combination with chronic pain and three in combination with both chronic pain and chronic fatigue.
Outcome
Self-perceived group climate
Group climate reports filled out by the participants themselves at the end of the rehabilitation program, showed subscale values as following: median 4 (mean 3.90) for engagement, median 0 (mean 0.45) for conflict and median 2 (mean 2.04) for avoidance on a scale ranging from 0 (not at all) to 6 (extremely). Mixed model linear regression analysis showed that belonging to a specific group accounted for 12% of the variance in GCQ-S levels for engagement and conflict, but did not influence on GCQ-S levels for avoidance (ICC < 0.01). The same percentages were found in the full model that adjusted for symptom. Increasing age was associated with reduced perceived engagement, while male gender was associated with lower perceived conflict and avoidance. Mental distress was positively associated with avoidance in the simple and full model that adjusted for age, gender, mental distress, chronic fatigue and chronic pain, indicating increased avoidance perceived by those with mental distress. There were no other statistically significant (5% level) associations with group climate in either simple (adjusted for age and gender) or full models (adjusted for age, gender and symptom) for other individual factors that were explored; chronic fatigue, chronic pain, confirmed mental disorder and preconception of group functioning. Results from the participants’ self-report on GCQ-S subscales are presented in and in which proportions of the population with and without chronic fatigue, chronic pain and mental distress are compared. GCQ-S was missing for 70 participants (33%) for the subscales engagement and conflict and 71 (33%) for avoidance. Missing data was mainly related to time-periods when participants were prevented from answering the GCQ-S due to technical system problems with online data registration.
Figure 5. Plot showing change in participant scores on the three subscales (engagement, avoidance and conflict) of the Group Climate Questionnaire – Short Form (GCQ-S). B coefficients and 95%CI from the full multilevel linear regression model are reported for caseness (versus non-caseness) of: *Chronic pain: a score ≥ moderate to very severe pain and duration of ≥6 months. **Chronic fatigue: a score of ≥4 on the Chalder Fatigue Scale and duration of ≥6 months. ***Mental distress: a score of ≥8 on either the anxiety and/or the depressive scales of the HADS.
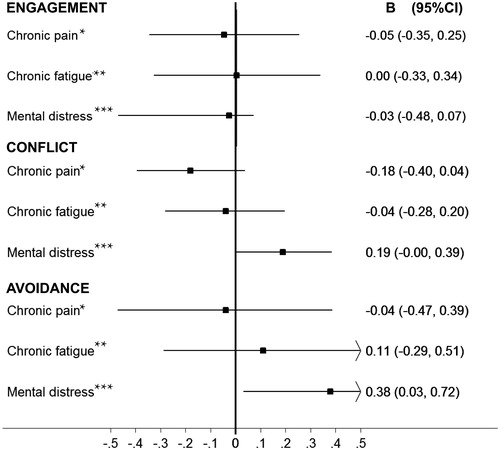
Table 1. Results from multilevel regression analysis on the association between self-reported symptoms (chronic pain, chronic fatigue or mental distress) and group climate subscales: engagement, avoidance and conflict.
Degree of participation
Clinical reports from the RTW coordinators showed that 95% (203/213) of the participants who had completed the full program were present and participated actively in the groups. Participating actively in the group could for example involve sharing experiences, taking part in discussions or supporting other group members. The remaining 5% had either missed several group sessions or if present, did not actively participate. Self-reported symptoms and clinically confirmed mental disorders were similarly present among those that participated versus those that did not.
Participants’ experiences
Findings from the qualitative interviews supported the quantitative findings that most participants felt comfortable with working in a transdiagnostic group, while a few participants stated that they generally found it hard to share personal thoughts and feelings in a group setting. One participant expressed that she never became comfortable with being in the group setting. However, she did not relate this to the group being transdiagnostic, but to her social anxiety disorder.
None of the participants expressed negative experiences with the fact that the groups included participants with different diagnoses. On the contrary, many emphasized that transdiagnostic groups allowed for a change of perspective away from focusing on the specific health problems towards focusing on how to effectively cope with the health problems, disregarding diagnoses. In addition, some participants said that they appreciated the absence of “pain-talk” and comparing of diagnoses and treatment.
Interviewer: You have quite different health problems. How has it been to work together in the same group?
Participant 2: If you have groups with just one type of health problems I think it can be a strong focus on, let’s say the shoulder, if it’s a shoulder group. We have focused very little on diseases. The only times we have focused on it is in preparing the exercise program. Besides that, it [diseases] has not been a topic.
Participant 1: I think that is helpful. I think it is crucial that we are mixed and that we have not all had knee surgery. Then we would have been limping around and talked about knees and knees and knees.
Participant 2: We have hardly spoken about diseases during the program. We have not been focusing on that… not in the group either. (Focus group 6)
In all groups, some participants said that they had been worried and apprehensive about the transdiagnostic group setting before the rehabilitation program started. The participants nevertheless described that the group had become an important support factor during the program. Mainly, this included confirmation that “they were not the only one” having problems, and that others had similar experiences.
Participant: I feel that we are a good group. I have shared things in this group, which I didn’t think I would share with them… a good group. Interviewer: Does that mean that you felt safe? Did the others understand you?
Participant: I felt that the others in the group shared my experiences. It wasn’t just me who struggled with this, several of us did… It felt good.
(Focus group 1)
Discussion
A novel group based occupational rehabilitation program successfully included sick-listed participants with chronic pain, chronic fatigue, and common mental disorders in transdiagnostic groups. The results showed stable group climate across different symptom profiles, high completion of the program (96%), and high active participation rates (95%). Focus group interviews confirmed that the patients’ experiences with transdiagnostic rehabilitation in mixed groups were positive. The feasibility of delivering ACT-based occupational rehabilitation in a transdiagnostic group setting is discussed in relation to focus areas of this study: the implementation of transdiagnostic groups, their acceptability to participants and the demand for such groups.
Implementation and acceptability to participants
Engagement is a desired quality in group treatment since it has repeatedly been associated with a positive group outcome [Citation57–60]. It has been proposed that a common therapeutic task in all group treatments should be to develop a group climate where participants are active and engaged. McKenzie argues that group engagement on the GCQ-S captures many of the essential elements of group cohesion, and may be described as an indicator of the positive bonding relationship that is usually thought of as a necessary ingredient in any effective therapy [Citation52]. We suggest that group engagement be used as an indirect and early phase measure of successful implementation of a group intervention.
With the exception of higher levels of avoidance seen for participants reporting mental distress, the participants’ experiences of group climate were not significantly associated with self-reported mental distress, chronic pain or chronic fatigue, or with a clinically confirmed mental disorder. The finding of higher group avoidance for participants experiencing mental distress may be considered of less importance for outcome than if similar results had been seen on the engagement subscale. The avoidance subscale has shown the least internal consistency of the GCQ-S subscales [Citation61] and higher levels of avoidance may even predict improvement [Citation58]. Interpretations of the GCQ-S avoidance ratings should therefore be cautious and context specific with regard to the treatment modality used [Citation58]. The GCQ-S results from this study give no evidence to discourage the use of rehabilitation groups mixing participants with mental and somatic disorders. Together with high participation rates the GCQ-S findings suggest that implementation of transdiagnostic groups was successful and the qualitative data further support this.
Findings from focus group interviews showed that participants were positive to the fact that groups were mixed. Through qualitative data, the participants expressed that a transdiagnostic rehabilitation program moved focus away from the disorder/diagnosis by allowing for focusing on general coping of health problems, rather than specific health issues Although a few participants described some discomfort with group settings, they did not perceive this as being related to the group being transdiagnostic.
Outcome for group climate and participation did not significantly differ for participants who prior to rehabilitation had reported problems with working in a group or participating in conversations. Thus, a participant’s prior belief that she or he did not function well in a group was not associated with actually withdrawing from group participation or reporting negative group climate. Results suggests that persons who perceive themselves as having problems with group functioning may - when actually being exposed to a group setting - equally participate and report a positive group climate. This was confirmed by the qualitative data from interviews: Participants who prior to rehabilitation had expressed worry and apprehension about the group setting, afterwards described the group as a support factor. Overall, quantitative and qualitative data support that the transdiagnostic program was acceptable to participants.
Demand for a transdiagnostic group program
Participants were surprisingly uniform with regard to self-reported health complaints despite being heterogeneous in terms of reasons for referral. This strengthens findings from earlier studies showing that participants on sick leave have a high degree of comorbidity and multiple health complaints [Citation13,Citation62,Citation63]. High symptom overlap in the studied population supports the demand for a transdiagnostic approach to accommodate for comorbidity in the sick-listed populations. The single-disease framework is widely viewed as insufficient for participants with comorbidity and complex symptom disorders [Citation10,Citation64–66].
This study observed that participants who pre-admission were clinically diagnosed with a mental disorder (22%) completed the rehabilitation program and reported group climate in a similarly satisfactory manner as participants with only subclinical or no mental problems. Individuals who struggle with mental disorders often report that they feel ignored, stigmatized and belittled in western societies [Citation67]. Reducing stigma around mental disorders is highly relevant for avoiding disability [Citation67]. A transdiagnostic approach to work disability may be desirable from a participant perspective since loss of work capacity is equally validated regardless of cause, rather than dichotomized into somatic or mental type.
The clinical demand for a transdiagnostic approach in occupational rehabilitation is discussed though not covered comprehensively in this paper. The program was successfully used by sick-listed participants with mental and/or somatic symptoms and disorders. Our findings support the demand for and possible benefits of a transdiagnostic program, and indicate that different diagnostic groups within the sick-listed population can use it.
Limitations and strengths of the study
A narrow set of quantitative tools are used: the self-reported GCQ-S, the clinician-reported bimodal measurement for active participation and program completion rate, all selected for easy use in clinical practice. A targeted approach towards feasibility to match the needs of the situation is common [Citation11]. However, future studies may wish to refine outcome measures or expand the scope of the feasibility study to include the perspectives of those delivering the program or other stakeholders. Due to technical problems, not all participants had an opportunity to answer the GCQ-S, but we have no reason to assume that this would systematically affect the results. A strength of this study is that targeted areas of feasibility were investigated from several perspectives and it has been pointed that studies using mixed methods may yield more innovative feasibility results [Citation11].
Clinical and research implications
This feasibility study was preformed alongside a full-scale implementation of an occupational rehabilitation program. Results supported continuing the program in mixed groups. We hypothesize that transdiagnostic rehabilitation programs can be expanded to cover an even wider range of disabling symptom disorders (e.g., irritable bowel syndrome). A prerequisite may be that participants have a common goal of increasing everyday functioning and work participation. Limitations may apply if basic assessment and treatment have not yet been completed. We recommend further research on transdiagnostic occupational rehabilitation to investigate the effect on return to work and explore possible benefits or drawbacks of mixed groups.
With a response rate of 99%, the internet-based, preclinical self-report was widely available to be used as clinical tool in the early process of shifting participant focus from a specific diagnosis or complaint, to a wide range of biopsychosocial factors related to both health and return to work. Although several researchers have stressed the need to shorten surveys and questionnaires [Citation68], our data suggest that in clinical settings it is possible to achieve a high response rate on self-report questionnaires prior to clinical consultation, despite it being time-consuming for participants and demanding use of basic technical equipment (personal computer and cell phone)
Conclusions
Participants in transdiagnostic groups reported moderately high levels of group engagement, completed the program and participated actively, while those interviewed expressed being positive to the transdiagnostic group experience. Transdiagnostic groups were used by the target population and were acceptable to these participants. The results from this study support the feasibility of implementing a transdiagnostic approach in occupational rehabilitation programs for mixed groups of participants with chronic pain, chronic fatigue and common mental disorders.
Acknowledgements
The authors would like to thank the staff at both the Hysnes Outpatient Department and the Hysnes Rehabilitation Center for their assistance in data collection.
Disclosure statement
The authors Karen Walseth Hara, Petter Christian Borchgrevink, Henrik Børsting Jacobsen, Marius Steiro Fimland, Marit By Rise, Sigmund Gismervik, and Astrid Woodhouse all declare they have no competing interests, financial or non-financial.
References
- Waddell G, Burton AK. Is work good for your health and well-being?: The Stationery Office; 2006.
- OECD. Sickness, Disability and Work: Breaking the Barriers; A Synthesis of Findings Across Oecd Countries. OECD; 2010.
- Vermeulen SJ, Anema JR, Schellart AJ, et al. A participatory return-to-work intervention for temporary agency workers and unemployed workers sick-listed due to musculoskeletal disorders: results of a randomized controlled trial. J Occup Rehabil. 2011;21:313–324.
- Bond GR, Drake RE, Becker DR. An update on randomized controlled trials of evidence-based supported employment. Psychiatr Rehabil J. 2008;31:280.
- Burns T, Catty J, Becker T, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet. 2007;370:1146–1152.
- Blonk RW, Brenninkmeijer V, Lagerveld SE, et al. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress. 2006;20:129–144.
- Loisel P, Abenhaim L, Durand P, et al. A population‐based, randomized clinical trial on back pain management. Spine. 1997;22:2911–2918.
- Lambeek LC, van Mechelen W, Knol DL, et al. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:c1035.
- Briand C, Durand MJ, St-Arnaud L, et al. Work and mental health: learning from return-to-work rehabilitation programs designed for workers with musculoskeletal disorders. Int J Law Psychiatry. 2007;30:444–457.
- Vooijs M, Leensen MC, Hoving JL, et al. Interventions to enhance work participation of workers with a chronic disease: a systematic review of reviews. Occup Environ Med. 2015;72:820–826.
- Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–457.
- Hagen EM, Svensen E, Eriksen HR, et al. Comorbid subjective health complaints in low back pain. Spine. 2006;31:1491–1495.
- Reme SE, Tangen T, Moe T, et al. Prevalence of psychiatric disorders in sick listed chronic low back pain patients. Eur J Pain. 2011;15:1075–1080.
- Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–2445.
- Demyttenaere K, Bonnewyn A, Bruffaerts R, et al. Comorbid painful physical symptoms and depression: prevalence, work loss, and help seeking. J Affect Disord. 2006;92:185–193.
- Aamland A, Malterud K, Werner EL. Patients with persistent medically unexplained physical symptoms: a descriptive study from Norwegian general practice. BMC Fam Pract. 2014;15:107.
- Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354:936–939.
- Maeland S, Werner EL, Rosendal M, et al. Diagnoses of patients with severe subjective health complaints in Scandinavia: a cross sectional study. ISRN Public Health. 2012;2012:851097.
- Loisel P, Durand M-J, Berthelette D, et al. Disability prevention. Dis Manag Health Out. 2001;9:351–360.
- Shaw WS, Van der Windt DA, Main CJ, et al. Early patient screening and intervention to address individual-level occupational factors (“blue flags”) in back disability. J Occup Rehabil. 2009;19:64–80.
- Durand M-J, Loisel P, Hong QN, et al. Helping clinicians in work disability prevention: the work disability diagnosis interview. J Occup Rehabil. 2002;12:191–204.
- Heerkens Y, Engels J, Kuiper C, et al. The use of the ICF to describe work related factors influencing the health of employees. Disabil Rehabil. 2004;26:1060–1066.
- Loisel P, Buchbinder R, Hazard R, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. J Occup Rehabil. 2005;15:507–524.
- Mansell W, Harvey A, Watkins E, et al. Conceptual foundations of the transdiagnostic approach to CBT. J Cogn Psychother. 2009;23:6–19.
- Craske MG. Transdiagnostic treatment for anxiety and depression. Depress Anxiety. 2012;29:749–753.
- Hayes SC, Luoma JB, Bond FW, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44:1–25.
- de Ornelas Maia AC, Nardi AE, Cardoso A. The utilization of unified protocols in behavioral cognitive therapy in transdiagnostic group subjects: A clinical trial. J Affect Disord. 2014;172:179–183.
- Yalom ID, Leszcz M. The theory and practice of group psychotherapy. 5th ed. New York (NY): Basic Books; 2005.
- Kroenke K, Swindle R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psychother Psychosom. 2000;69:205–215.
- Arboleda-Florez J, Stuart H. From sin to science: fighting the stigmatization of mental illnesses. Can J Psychiatry. 2012;57:457–463.
- Dudley R, Kuyken W, Padesky CA. Disorder specific and trans-diagnostic case conceptualisation. Clin Psychol Rev. 2011;31:213–224.
- Oyeflaten I, Hysing M, Eriksen HR. Prognostic factors associated with return to work following multidisciplinary vocational rehabilitation. J Rehabil Med. 2008;40:548–554.
- Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research: issues in external validation and translation methodology. Eval Health Prof. 2006;29:126–153.
- Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–1632.
- Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–696.
- Hardeman W, Sutton S, Griffin S, et al. A causal modelling approach to the development of theory-based behaviour change programmes for trial evaluation. Health Educ Res. 2005;20:676–687.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50:587–592.
- Fritz F, Ständer S, Breil B, et al. CIS-based registration of quality of life in a single source approach. BMC Med Inform Decis Mak. 2011;11:26.
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: the process and practice of mindful change. New York (NY): Guilford Press; 2011.
- Fimland MS, Vasseljen O, Gismervik S, et al. Occupational rehabilitation programs for musculoskeletal pain and common mental health disorders: study protocol of a randomized controlled trial. BMC Public Health. 2014;14:368.
- Ware J, Kosinski M, Dewey J, et al. A manual for users of the SF-8 Health Survey. Lincoln, RI: Quality Metric Incorporated; 2001.p. 4–19.
- Landmark T, Romundstad P, Dale O, et al. Estimating the prevalence of chronic pain: validation of recall against longitudinal reporting (the HUNT pain study). Pain. 2012;153:1368–1373.
- Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res. 1993;37:147–153.
- Loge JH, Ekeberg Ø, Kaasa S. Fatigue in the general Norwegian population: normative data and associations. J Psychosom Res. 1998;45:53–65.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77.
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosom Med. 2004;66:845–851.
- Brage S, Konráðsdóttir ÁD, Lindenger G. Work Disability Evaluation. In: Escorpizo R, Brage S, Homa D, et al., editors. Handbook of Vocational Rehabilitation and Disability Evaluation. New York (NY): Springer; 2015. p. 107–139.
- Osteras N, Gulbrandsen P, Garratt A, et al. A randomised comparison of a four- and a five-point scale version of the Norwegian Function Assessment Scale. Health Qual Life Outcomes. 2008;6:14.
- Zimmerman M, Mattia JI. The psychiatric diagnostic screening questionnaire: development, reliability and validity. Compr Psychiatry. 2001;42:175–189.
- First MB, Spitzer RL, Gibbon M, et al. User's guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. Arlington (VA): American Psychiatric Pub; 1997.
- MacKenzie K. Measurement of group climate. Int J Group Psychother. 1981;31:287–295.
- Kivlighan DM, Jr, Goldfine DC. Endorsement of therapeutic factors as a function of stage of group development and participant interpersonal attitudes. J Couns Psychol. 1991;38:150.
- Rise MB, Gismervik SO, Johnsen R, et al. Sick-listed persons' experiences with taking part in an in-patient occupational rehabilitation program based on Acceptance and Commitment Therapy: a qualitative focus group interview study. BMC Health Serv Res. 2015;15:526.
- Twisk J. Applied multilevel analysis: a practical guide Cambridge, United Kingdom: Cambridge University Press; 2006.
- D L. Phenomenological research methods. Research Methods and data analysis in psychology. New York (NY): Pearson Education Limited; 2004. p. 274–292.
- Ogrodniczuk JS, Piper WE. The effect of group climate on outcome in two forms of short-term group therapy. Group Dyn. 2003;7:64.
- Ryum T, Hagen R, Nordahl HM, et al. Perceived group climate as a predictor of long-term outcome in a randomized controlled trial of cognitive-behavioural group therapy for patients with comorbid psychiatric disorders. Behav Cogn Psychother. 2009;37:497–510.
- Kivlighan DM, Jr, Lilly RL. Developmental changes in group climate as they relate to therapeutic gain. Group Dyn. 1997;1:208.
- Braaten LJ. Predicting positive goal attainment and symptom reduction from early group climate dimensions. Int J Group Psychother. 1989;39:377–387.
- Johnson JE, Pulsipher D, Ferrin SL, et al. Measuring group processes: a comparison of the GCQ and CCI. Group Dyn. 2006;10:136–145.
- Snekkevik H, Eriksen HR, Tangen T, et al. Fatigue and depression in sick-listed chronic low back pain patients. Pain Med. 2014;15:1163–1170.
- Loisel P, Anema JR. Handbook of work disability. Prevention and management. New York (NY): Springer; 2013.
- Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
- Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22:391–395.
- Britt HC, Harrison CM, Miller GC, et al. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189:72–77.
- Ilic M, Reinecke J, Bohner G, et al. Belittled, avoided, ignored, denied: assessing forms and consequences of stigma experiences of people with mental illness. Basic Appl Soc Psych. 2013;35:31–40.
- Sahlqvist S, Song Y, Bull F, et al. Effect of questionnaire length, personalisation and reminder type on response rate to a complex postal survey: randomised controlled trial. BMC Med Res Methodol. 2011;11:62.