Abstract
Purpose: There is lack of knowledge, evidence, and guidelines for rehabilitation interventions for persons with neuralgic amyotrophy (NA) or brachial plexus pathology. A first pilot study, evaluating the effect of an integrated rehabilitation programme, showed improvements in activity and participation levels.
Aim: To gain insight, from the perspective of patients and therapists, into the critical ingredients of the programme, that contributed to improvements in activity and participation.
Materials and methods: A qualitative study using semi-structured interviews with eight patients and five therapists (three occupational therapists and two physical therapists). Participants were asked to identify and describe factors regarding the rehabilitation that they perceived as positive and aspects of the programme that could be improved. Data were analysed using a constant comparative approach.
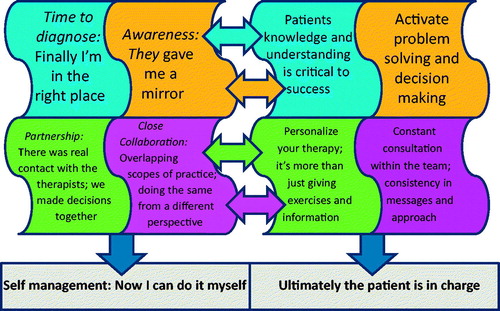
Results: Patients reported (1) Time to diagnose: “Finally I’m in the right place;” (2) Awareness: “They gave me a mirror;” (3) Partnership: “There was real contact with the therapists; we made decisions together;” (4) Close collaboration: “Overlapping scopes of practice; doing the same from a different perspective;” and finally (5) Self-management: “Now I can do it myself.” Therapists reported (1) “Patients knowledge and understanding is critical to success;” (2) “Activate problem solving and decision making;” (3) “Personalize your therapy; it’s more than just giving exercises and information;” (4) “Constant consultation within the team; consistency in messages and approach;” and (5)” Ultimately the patient is in charge.”
Conclusions: The critical ingredients, correspond well with each other and include a person-centred approach, education, support in problem solving and decision making and an integrated team approach. These ingredients provided the patients with confidence to take responsibility to manage their everyday lives, the ultimate goal of the programme.
Both patients and therapists believe that the ability to self-manage and take control should be the outcome of high quality integrated rehabilitation programmes for patients with neuralgic amyotrophy and/or other brachial plexus injuries.
A person-centred, collaborative, and integrated team approach, among all members of the team, are critical components of care delivery in personalised interventions.
Critical programme ingredients are knowledge and education of both the patient and therapists; partnership between patient–therapist and within the team; patient activation and self-reflection; and personalised care.
Patients recommend more options for personalisation of the intensity and duration of rehabilitation, the possibility to consult a psychologist and peer support within a group setting.
Implications for rehabilitation
Introduction
Persons with neuralgic amyotrophy (NA) experience severe pain, fatigue, and problems in performing movements of the upper extremity [Citation1]. NA limits forward reaching, lifting the arms above shoulder height, maintaining static arm positions, and repetitive movements. The combination of limited movement, pain, and fatigue compromise the performance of many activities and roles in daily life, making NA a very debilitating condition.
NA is a peripheral nerve disorder characterised by episodes of severe neuropathic pain at onset, followed by multifocal paresis and atrophy of the upper extremity muscles [Citation2,Citation3]. It can result in impaired humero-scapulothoracic coordination and scapula alata (winging of the shoulder blade) and increased fatigability of the muscles, leading to compensatory movements, and limitations in everyday life [Citation4,Citation5]. Recovery is mostly slow and often incomplete [Citation2,Citation3]. Previously, NA was known as a rare disease (incidence of 2–3 per 100,000 per year [Citation6]), however, recently it has been shown that NA is quite common with an incidence of 1 in 1000 [Citation7]. Still, NA is not well recognised by physicians and therapists and, as a result, treatment provided is often nonspecific and sub-optimal. Lack of or incorrect diagnosis, inconsistent or wrong advice, and absence of a clear intervention plan contribute to patients’ anxiety that often further aggravates symptoms.
There is limited evidence to guide treatment of NA [Citation3]. While the use of prednisolone treatment in the acute phase [Citation8] is showing promising results, evidence and protocols during the sub-acute phase are limited. Therefore, people with NA often receive the message that they “have to live with it” with no support to manage life with pain and paresis that limits function at work, during sports, leisure, and/or self-care activities.
In 2009, the department of rehabilitation and neurology at Radboud University Medical Center began seeing outpatients at a specialised, multidisciplinary clinic for patients with disorders of the brachial plexus, the so called “Plexus Clinic.” People with NA form the largest group attending this clinic. Consisting of a neurologist, rehabilitation physician, physical and occupational therapist, the multidisciplinary team has assessed three to four new patients every week for the past seven years. The assessment includes making the diagnosis and providing the patient with a personalised intervention plan. Most patients are then referred to their own region for implementation of this plan; however, patients living in the Nijmegen region are treated by our own multidisciplinary team. Intervention includes physical and occupational therapy and, if necessary, medication and/or orthosis/aids provided by the rehabilitation physician.
As the first integrated rehabilitation programme for NA, the limited available scientific evidence was combined with the practice-based expertise of the multidisciplinary team to develop a standardised integrated rehabilitation programme [Citation9]. The aim of this programme is to support patients to gain control over their symptoms in order to manage their life with NA. The focus of physical therapy is to regain scapular muscular balance [Citation10]. Using an individualised adaptation of a fatigue management group intervention [Citation11], occupational therapy supports life balance and self-management strategies known to reduce fatigue and improve quality of life [Citation11,Citation12]. Both physical and occupational therapist assist patients to identify and adapt activities that provoke pain. The programme consisted of a 16-week treatment period during which patients were treated weekly in week 1–4, once every two weeks in week 5–8 and monthly in week 9–16. Each treatment session involved one-hour occupational therapy and one-hour physical therapy.
In 2013, a pilot study (n = 8) was conducted to evaluate the effectiveness of the multidisciplinary rehabilitation intervention for persons with NA [Citation9]. Results showed significant and clinically important differences on participation (performance and satisfaction) scores on the Canadian Occupational Performance Measure [Citation13] as well as significant improvement in self-reported shoulder function, pain, and activities of daily living performance. However, patients did not report improvements in strength or decrease in fatigue [Citation9]. These results are encouraging and support the need for further studies, with more robust methodology and larger samples. As our ability to diagnose the disorder in a timely and adequate manner improves, the number of patients requiring treatment is increasing as is the need for new multidisciplinary teams to provide care. Understanding the critical ingredients of the programme’s effectiveness will facilitate replication at other centres.
The aim of this study was, therefore, to gain insight, from the perspective of both patients and therapists, into the aspects of the integrated rehabilitation programme that positively contribute to the improvements in activity and participation. The research question was “what are patient and therapist reflections on the rehabilitation programme; how do they identify and value the programme ingredients and understand their contribution to their outcomes?”
Materials and methods
Design of the study
This qualitative study employed interpretative epistemology and hermeneutic methodology [Citation14] whereby patients’ and therapists’ reflections were used to interpret and give meaning to the different ingredients of the rehabilitation programme. The study was conducted in 2012 and 2013, using semi-structured interviews.
Participants and context
After receiving ethical approval from the Medical Ethics Committee of Radboud University Medical Center (registration number 2012/510), participants were recruited. All patients and therapists, who participated in the pilot study to evaluate the effect of our integrated rehabilitation programme [Citation9], were approached. All eight patients met the inclusion criteria: (1) diagnosed with NA; (2) uni- or bi-lateral complaints with pain scores on the numeric rating scale [Citation15] of more than 5; (3) at least 6 months after onset; (4) aged 18 years or over; and (5) able to understand written and spoken Dutch. Each received a telephone call inviting their participation and requesting permission to send information about the study. All gave their permission. Five of the six therapists who delivered the programme (two physical and three occupational therapists) also agreed to participate. One physical therapist was unavailable because of maternity leave. All potential participants (patients and health providers) received a letter describing the study. Patients received a follow-up phone call by a research assistant one week later. Willingness to participate was re-confirmed with all providing informed consent. To preserve anonymity, demographic variables of participants (patients and therapists) are band into categories (see and ). Patient participants varied in age, sex, affected arm and time between onset of NA and start of the treatment. Six males and two females ranging in age from 34 to 62 years participated. Time between onset of NA and start of the treatment varied from 7 to 156 months; five patients had NA of the dominant arm/shoulder. Therapists also varied; four were females, and years of experience with NA ranged from three to nine years.
Table 1. Demographic data of patients.
Table 2. Demographic data of therapists.
Data collection procedures
Two semi-structured interview guides (one each for patients and therapists) were developed. Both used nondirective, open-ended questions. Interviews with patients were held in their chosen environment (typically their home), so they would feel at ease [Citation16,Citation17]. Two patients preferred an interview at Radboud University Medical Center, for practical reasons. Interviews with all therapists were held at Radboud University Medical Center. Duration of the interviews was approximately 1 hour and interviews were performed by four research assistants. Each interview was conducted by two research assistants; one led the conversation and the other made notes, observed and assisted in the use of the recorder. Research assistants are occupational therapy students from the HAN University of Applied Sciences, who received training in conducting qualitative research.
At the beginning of every interview, the aim of the research, procedure of the interview and privacy policy was explained. There was also an opportunity to ask questions and informed, signed consent was obtained. Patients were invited to talk about their experience with the integrated intervention programme and specifically about their experience with occupational therapy and physical therapy. They were asked to identify and describe aspects of the programme that helped them the most and aspects of the programme they would like to change. Therapists were also invited to talk about their experiences with the integrated rehabilitation programme. Specific topics were perceived effectiveness of the treatment and changes in patients’ level of activity and participation during the programme. Therapists were also asked to report on factors they perceived contributed to the success of the programme and aspects of the programme they would like to improve.
Data analysis
Interviews were audiotaped and transcribed. For data-analysis, transcripts were imported into Atlas.Ti 7.1.5 software (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany). The constant comparative method was used for the analysis [Citation14,Citation17]. Analysis of the transcripts were performed by the first and last author.
Analysis consisted of four steps. (1) Familiarisation with the interviews was achieved by reading the transcripts several times. (2) This was followed by open coding of each transcript. To improve credibility, two interviews were first coded separately by the first and last author. Codes were then compared and discussed until consensus was reached. The high level of similarity in coding meant that other interviews could be coded by only the first author. (3) After the open coding of all interviews, coded text was grouped into categories with patient and therapist text analysed separately. (4) Finally, comparison and grouping of the categories led to final themes. The created themes were discussed with two other co-authors (with external perspective) and refined as described by the first author [Citation18].
Trustworthiness
To enhance the trustworthiness of the study [Citation19,Citation20] coding was performed by two researchers, the first and last author. Categories and themes were discussed in meetings with two other co-authors (with external perspective). Triangulation occurred by inclusion of two perspectives; perspective of patients as well as the perspective of therapists.
The research assistants were unfamiliar with the patients they interviewed. They did know one occupational therapist, since she held dual roles of researcher (first author) and participant therapist. Two co-authors provided an “outsider perspective” as they were not familiar with the programme and/or organisation, while the first and last author, both familiar with the content and organisation of the programme, provided an “insider perspective.” During the analysis, this enhanced the dialogue about the similarities within and differences between the categories, adding additional credibility [Citation19]. The other authors were members of the Plexus Clinic (physical therapist, neurologist, and rehabilitation physician) and also contributed to the data, interpretation and review of the manuscript. The physical therapist was also a participant in the interviews from therapists’ perspective, as well as co-author.
Results
Analysis led to five “patient themes” and five “therapist themes.” These themes represented aspects or ingredients of the rehabilitation programme that, from the different perspectives, contributed to the improvements in activity and participation (). Participants placed equal value on all themes, seeing all as required for successful outcomes. Patients and therapists shared the strong view that the overall result of the programme finds the patient being in charge and able to self-manage (see final theme for both patients and therapists in ). Each theme will be described, supported by quotes of the participants. Patients and therapists are given a number to ensure anonymity, see tables 1 and 2 . Following the quotes, the number of participant is put in brackets to show that the quotes are from different participants.
Figure 1. Findings from patients’ perspective (pieces with themes on the left side) and from the perspective of therapists (pieces with themes of the right side).
Patients’ themes
Time to diagnose: “Finally I’m in the right place”
Nearly all patients talked about the onset of the disease and how long it took for them to receive the right diagnosis. The unfamiliarity with the disease among physicians and therapists elsewhere was often reported, together with the uncertainty and frustration this created. Only a few patients had met physicians and therapists who knew what to do and how to treat their problems. Nearly all described the importance of finally being in the right place when they talked about the Plexus Clinic (i.e., a place where health professionals knew their condition and their problems), which gave them confidence and a sense of being understood.
You are in the right place, where people know what it is, recognize it and do something about it. They can help you to manage, so you have the least burden (patient 8)
Knowledge of the team was also reported to be an important aspect of being in the right place. Patients felt taken seriously and reported a sense of trust that therapists had the expertise to support them in the management of their disease.
There was so much experience, I only had to say something and it was put back to my situation. Nine out of 10 times I was reassured and therefore helped (patient 7)
Awareness: “They gave me a mirror”
During the interviews patients expressed in different ways how the programme helped them to become aware of the relationship between their complaints and the performance of their activities. They gained insight into how their own actions and behaviours could trigger or exacerbate their symptoms. They also learned how to make the changes needed to reduce the pain and fatigue and improve their movements.
Becoming aware is very difficult. I'm not a disabled person. I can still work, but I realize now that I have limitations (patient 5)
“They gave me a mirror and taught me to pick up the thread” (patient 8)
Many patients described learning to change their routines. One patient reported that she could “not go on” in the same way she had been doing. She realised her complaints were not going to go away by ignoring them, nor by massaging or strengthening the muscles. Patients became aware of their movement patterns, what they were doing during the day and how they did it; how to lift the groceries, how to sit in the car or how to brush their teeth. Knowing how the performance of tasks could affect their pain was new. They also said that this awareness was exhausting and difficult, but necessary.
Some said that they missed the support of a psychologist during this difficult process.
An improvement would be to engage a psychologist, because in my case I had to ‘flip a switch’. I thought I was in control of my body, but no, the body is in control of you (Patient 8)
For all patients, it was important to learn what to do and what to avoid. The programme required patients to adapt many aspects of life, such as changing the performance of their activities and the way they organise their day. One patient said that the information and explanation of the disease in relation to his functioning was enough motivation to change the way he was coping with his problems.
“They explained why it was the way it was, that was enough motivation for me” (patient 6)
Patients also expressed how they had become more conscious about the need to listen to their body, take breaks, analyse, adapt, and prioritise their activities and roles. Patients also mentioned “learning to do things in another way.” To implement the physiotherapy exercises into daily life, they had to continuously focus on “what am I doing? And how am I doing this?”
Taking breaks, doing things in a different way. Being much more conscious of managing your body and listen carefully [to the body] (patient 1)
Partnership: “There was real contact with the therapists”
Patients talked about “having real contact with the therapist.” They valued the attention and interest that the therapists showed in them as a person. One patient described how he was not just a number for the therapists, but a real person. Patients said that the therapists gave them the right perspective and made them think about the important and meaningful aspects of life.
I have started to think about what is really important …. This happened to me and it made me realize what is most important in my life. Is it important to ride my bike in the evening or do I want to be there for my family? (patient 8)
Patients also felt they were part of the programme that was tailored to their individual needs. There was interaction with the therapists about their aims and priorities and what the therapist thought to be important. Decisions were made together.
We discussed what she thought was important and what I thought was important, there was clear agreement (patient 4)
Close collaboration: “Overlapping scopes of practice; doing the same from a different perspective”
One of the aspects that almost every patient talked about was the collaboration within the team. They described the programme as a “complete package.” Therapists complemented each other and worked across the boundaries of their professions, which was appreciated by the patients. One patient described the importance of getting the same information from different perspectives which helped in applying tips and advice in everyday life.
The physical therapist and occupational therapist work across the boundaries of their field of expertise; hearing the same from different perspectives has added value (patient 6)
Several patients expressed that they had experienced how both therapists (physical and occupational) had their specific expertise but worked together towards the patients’ goals. They valued the evaluations and the constant dialogue between both therapists during the treatment.
The talks to transfer the findings in between [consultations] and share this with each other, joint decision making, that is the perfect mix (patient 6)
The disease-specific aspects of therapy were also addressed by the patients; the value of the specific exercises they learned and applied in daily activities, ergonomic advice, the implementation of mini-breaks and the importance of pacing activities during the day and week. This was described as a process of learning to integrate advice and exercises into daily routines. They valued that both the occupational and physical therapist coached them from their own specific expertise. Patients said that this process was difficult but important to reducing their pain and fatigue.
It involves all those little things, but those are the things giving you the most trouble; for example, cooking is still a burden, however, a lot less than in the beginning (patient 2)
Exercises are implemented into the daily movements. If I wash my hair, I'll keep that in mind. You learn a completely different movement pattern (patient 1)
Self-management: “Now I can do it myself”
Patients described how the therapists provided them with tools to manage themselves in daily life. They reflected how important it was to know the aim of the exercises and to learn to feel whether their movement patterns were correct or incorrect. It was important to link this to learning to pacing and planning.
You learn to feel when you move incorrectly or when your body needs a break (patient 1)
One patient said that although she was provided with the right tools to improve functioning, there were still moments when it went wrong. She felt that the tools then helped her to regain control.
There are still times when it goes wrong, but now you know what you can do to make it better (patient 2)
A few patients said that they had other expectations of physiotherapy at the start of the treatment. They thought it would be more massage and a physical training programme. Some of them expressed the desire to have more massage in the programme.
This last theme from the patients’ perspective also included their reflections of the importance of being able to live and manage their life with NA. Nearly all patients described how their own role and responsibility in the treatment had gradually increased.
They teach you to pick up the thread bit by bit, that’s why there is gradually more time between the appointments, in order to see how long you can manage yourself (patient 1)
Now (when therapy is finished) I need to do it myself (patient 5)
Patients also expressed difficulties with this responsibility. Some patients said that this way of therapy “needs to fit you in order to be effective,” because it is demanding and not everybody is able to take on this responsibility.
Both (occupational and physical therapist) expect an ‘iron discipline’ of the patient, that has to fit you (patient 6)
A few patients mentioned that they would have appreciated peer support to learn from others and share experiences how to manage themselves.
Therapists’ themes
Patients knowledge and understanding is critical to success
Most therapists stressed the importance of patients understanding their disease process and its consequences. They said that the effectiveness of the therapy is greater when patients understand why they continue to experience limitations, even when the period of inflammation and neuropathic pain is over. According to the therapists, patients need toPatients knowledge and understanding is critical to success understand which factors contribute to the persistence of the symptoms and what they can do to influence these factors. The therapists feel that this is essential in regaining control over the symptoms and the limitations patients’ experience.
The effect has to do with whether people understand it; the pain is no longer due to the acute NA, but due to the overload that follows. When people do not understand their contribution to their symptoms, the treatment is less effective (Therapist 2)
Most therapists believe that knowledge and understanding support patients’ motivation to change their behaviour.
People make their own choices, that’s why it is very important that they understand why certain things are the way they are; then the motivation to change behavior is completely different (Therapist 2)
Activate problem solving and decision making
This theme focused on activating patients; informing them, allowing trial and error and letting them experience where things go wrong and where there is scope for improvement. Therapists reported how they coach their patients to find their own solutions to the problems they experience. This was felt to be the best way to change behavior. Nearly all therapists addressed the value of shared decision making. They reported how they had seen the positive effects when the patient is made a partner in decisions regarding treatment goals and interventions.
When someone finds his own solution, it will fit best with his strategies (Therapist 1)
Motivational interviewing techniques were reported to be very helpful in this process.
Let people decide for themselves what they want to work on; make the patient your partner in the treatment, that is the largest advantage of motivational interviewing (Therapist 5)
Personalize your therapy; it’s more than just giving exercises and information
Therapists stated that all patients are taught similar exercises and strategies, but these are personalised to their specific complaints, daily tasks and life roles.
The treatment itself is not unique, but it is adapted to the patient. Everyone gets broadly the same, but not exactly the same (Therapist 5)
They said that even though all patients are educated on exercises, ergonomics and finding a balance between activity and rest, there is no “one size fits all.” Patients are not just given exercises and information, but it is always tailored to the personal situation.
Most successful is continuously linking [treatment] to someone’s specific situation. Not only providing training and giving information (Therapist 2)
Constant consultation within the team; consistency in messages and approach
All therapists addressed the value of the multidisciplinary team. Working together towards the same goals, from each professional perspective is seen as a key to success. Therapists said that it is important for the patients to receive the same messages several times. They think that “hearing a similar message, from a different point of view” increases the success of the therapy.
The strength of the treatment is the collaboration; the power of repetition and approaching something from another perspective in just a different way (Therapist 1)
It is the combination of technical exercise therapy with behavioral aspects (Therapist 5)
Both therapists (occupational and physical) felt that they complemented each other. For example, when the physical therapist trains the scapula position while sitting, the occupational therapist pays attention to the appropriate seating ergonomics. The therapists described working intensely together and informing each other about the progress, successes and areas of focus so that each can continue to address these aspects from their own perspective.
I cannot imagine that you would do this separately; one and one is more than two, in this case (Therapist 2)
Ultimately the patient is in charge
In this last theme, therapists stressed the responsibility of the patients. Therapists said that they could only provide the patients with information, tools, and support. However, in the end, it is the patient who needs to implement the strategies and exercises in his/her daily life in order to regain control.
You hope that everybody can take matters into their own hands again and can go further by themselves, that they no longer need you (Therapist 2)
It was generally felt by the therapists that giving responsibility to the patients had an empowering and motivating effect on them.
Success [of the therapy] because you give the responsibility to the patient, they want to get better, we teach them the tools. That motivates (Therapist 4)
However, several therapists felt that not all patients were happy or able to take this responsibility. Some patients continue to expect that the therapist can “treat” the complaints instead of coaching them to become in charge of their own complaints.
Discussion
This study sought to understand the critical ingredients of an integrated rehabilitation programme for patients with NA in order to better understand what contributes to patient outcomes. Three important insights have emerged:
Patients and providers identified similar ingredients from separate perspectives. These ingredients align with self-management of other chronic conditions.
Patients and therapists strongly endorsed shared decision making and a partnership model of care delivery. From a patient perspective, this means focusing on their goals and priorities. From a provider perspective, it means contributing both professional and disease-specific expertise.
Patients and providers both recognise that ultimately it is the patient who must take control in order to manage everyday life with a chronic condition.
The ingredients that have been identified by patients and therapists in the themes correspond well with self-management skills as identified by Lorig and Holman [Citation21], which include problem solving, decision making, appropriate resource utilisation, forming a partnership with a healthcare provider, and taking necessary actions and self tailoring. Both the patient self-management skills and the method of care delivery are consistent with components of the chronic care model [Citation22]. This model is predicated on the belief that productive interactions between an activated patient and a prepared and proactive team, are essential for positive outcomes. Participants in this study endorsed this view and provide empirical evidence to support the model. In these productive interactions are illustrated by the arrows between the aspects identified by the patients and the aspects identified by the therapists and by the shared fifth theme. Patients valued the “proactive team” identifying how both the occupational and physical therapist contributed their specific expertise while still engaging in close collaboration so that patients received a consistent message from different perspectives. It should also be considered that other therapeutic characteristics, such as taking time with the patients, being open, listening, and being empathic, also can contribute to the perspective of the patients. Recognition by the professional of client values underlying their needs (uniqueness, comprehensiveness, continuity of life, fairness, and autonomy) and underlying the care-relationship (equality, partnership, and interdependence) has been identified as a central element within the interaction [Citation23]. Feelings of recognition with the client seem to reinforce autonomy, self-esteem, and participation. Recognition is optimally felt in a dialogue. Four professional competencies have been identified by Schoot et al. [Citation23] related to recognition: attentiveness (ongoing actions to know and understand the patient); responsiveness (active, committed, and responsible care guided by respect of patient identity); being a critical partner in care (giving and grounding professional opinion and discuss boundaries); and being a developer of client competencies (facilitating and developing client participation within care) [Citation23].
The disease-specific content of therapy (not specifically identified as a theme) was often alluded to by patients within the different themes. These included the specific exercises, the need for minibreaks, and the planning and pacing strategies they learned and applied in daily activities in order to regain control. However, the first theme strongly emphasised the importance of the expertise of the team. Patients sense of “being in the right place” spoke of their relief in finding knowledgeable and skilled clinicians that were in sharp contrast to the distress they had experienced when searching for a diagnosis, understanding, and effective interventions.
There were at least three recommendations to improve the quality of the programme. Some patients missed the potential support that a psychologist might offer during the exhausting and difficult process of becoming aware that they needed to change their behavior. Self-management is often described as medical, role and emotional management [Citation21]. This programme appears to explicitly support the first two with less explicit emphasis on emotional management an aspect that patients highlighted as important. Future consideration should be given to enhancing the programme through additional aspects of emotional support.
The second aspect was the fact that, for some patients, this programme’s focus on self-management, did not appear to fit their needs. Patients expressed that this approach warranted an iron discipline and several therapists felt that not all patients were able to take this responsibility. Ways to support patients, perhaps with more time or coaching to become ready to change, may need to be considered.
Finally, a few patients would have appreciated peer support, for which a group intervention could be recommended. A large advantage of a group intervention would be that participants would see people similar to themselves manage task demands successfully, which contribute to people’s belief in self-efficacy. This is also referred to as vicarious experiences provided by social models and is one of the four main sources of self-efficacy [Citation24]. The other sources include mastery experiences, social persuasion that one has the capabilities to succeed and inferences from somatic and emotional states indicative of personal strengths and vulnerabilities. The final theme from the perspective of both patients and therapists is the ability to manage and be in charge which can be referred to as achieving self-efficacy. To achieve this, people go through a process in which the therapists support them to gain mastery experience. This is achieved by experiences in overcoming obstacles through perseverant effort. As Bandura [Citation24] states, “setbacks and difficulties in pursuits serve a useful experience that success usually requires sustained effort. After people become convinced they have what it takes to succeed, they persevere in the face of adversity and quickly rebound from setbacks.” In the current programme, people go through this process by themselves, whereas a group programme would add an additional source of efficacy with peer experiences.
Although, the programme was individualised in the sense that attention was paid to the personal situation and goals from the patients, the intensity of the programme (number of sessions and duration of intervention period) was more or less “one size fits all.” This aspect needs more consideration in the future. Audulv [Citation25] has found that self-management does not develop as one uniform pattern. Instead, different self-management behaviours are enacted in different patterns, which can be distinguished as consistent, episodic, on demand, and transitional. It is likely that self-management activities require support strategies tailored to each behaviour’s developmental pattern.
Strength of this study was that all patients from the pilot study [Citation9] participated in this study. Apart from one physical therapist, who was unavailable, all therapists on the team also participated. Collecting the perspective of patients and professionals (physical and occupational therapists) has been done in other studies [Citation26] and allowed strong triangulation [Citation27] of the data and findings. In the future, it would be interesting to add the perspective of the neurologist and rehabilitation physician who is also part of the integrated team. Because partners and close family members are also affected, their inclusion would also add a valuable perspective.
We limited our sample to patients involved in the original pilot study, creating a limited sample to draw from. Fortunately, all eight patients and five out of six therapists were available for this study. During the analysis, we found repeating patterns of the same experiences suggesting that saturation had been reached [Citation27], despite the limited sample.
The fact that the primary researcher was also a member of the Plexus Clinic and integrated rehabilitation programme has both strengths and limitations. As part of the team, this might have introduced a positive bias into the research process. On the other hand, intimate knowledge of the programme brings inside knowledge to the analysis and interpretation of both patient and therapist data. To mitigate potential bias, all interviews were conducted by independent research students trained in interviewing who were at arm’s length from the team. In addition, the research team was strengthened with two experienced researchers who participated in the analysis and interpretation of the findings from an outside perspective.
Conclusion
This study investigated the critical ingredients of an integrated rehabilitation programme for patients with NA from the perspective of patients and professionals. The expertise and close collaboration of the team members was an important aspect which contributed to the trust, confidence, understanding, awareness, and ability of patients to actively regain control of their everyday activities and participation. Working in partnership coupled with shared decision making led to a personalised approach that was valued by patients and emphasised by therapists as essential to successful outcomes. The critical ingredients can be summarised as a combination of supporting patient self-management skills coupled with disease and profession specific expertise delivered in a collaborative partnership approach. Some patients would have liked more emotional support and some might have needed a more flexible and tailored approach regarding the intensity of the interventions provided. These qualitative results further inform the results of the original pilot study. It appears from both patient and provider perspectives, that the integration of the named ingredients provides the patients with confidence to take responsibility to manage their condition in their everyday lives. For application of the interventions in other healthcare settings, these ingredients are important to consider.
Acknowledgements
We are grateful to the people who were willing to share their experience with the integrated rehabilitation programme during the interviews. We also thank the research assistants, Chantal Dijkstra, Jessica Groen, Marijke van Leeuwen and Moniek Meijerman, who successfully organised and performed the interviews during this study.
Disclosure statement
The authors report no conflicts of interest.
References
- Cup EH, Ijspeert J, Janssen RJ, et al. Residual complaints after neuralgic amyotrophy. Arch Phys Med Rehabil. 2013;94:67–73.
- Van Eijk JJ, Groothuis JT, Van Alfen N. Neuralgic amyotrophy: an update on diagnosis, pathophysiology, and treatment. Muscle Nerve. 2016;53:337–350.
- van Alfen N, van Engelen BG, Hughes RA. Treatment for idiopathic and hereditary neuralgic amyotrophy (brachial neuritis). Cochrane Database Syst Rev. 2009;Cd006976.
- Beghi E, Kurland LT, Mulder DW, et al. Brachial plexus neuropathy in the population of Rochester, Minnesota, 1970–1981. Ann Neurol. 1985;18:320–323.
- Geertzen JH, Groothoff JW, Nicolai JP, et al. Brachial plexus neuropathy. A long-term outcome study. J Hand Surg Br. 2000;25:461–464.
- MacDonald BK, Cockerell OC, Sander JW, et al. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain. 2000;123:665–676.
- van Alfen N, van Eijk JJ, Ennik T, et al. Incidence of neuralgic amyotrophy (Parsonage Turner syndrome) in a primary care setting–a prospective cohort study. PLoS One. 2015;10:e0128361.
- van Eijk JJ, van Alfen N, Berrevoets M, et al. Evaluation of prednisolone treatment in the acute phase of neuralgic amyotrophy: an observational study. J Neurol Neurosurg Psychiatry. 2009;80:1120–1124.
- Ijspeert J, Janssen RM, Murgia A, et al. Efficacy of a combined physical and occupational therapy intervention in patients with subacute neuralgic amyotrophy: a pilot study. NeuroRehabilitation. 2013;33:657–665.
- Cools AM, Dewitte V, Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35:1744–1751.
- Packer TL, Brink N, Sauriol A. Managing fatigue: a six-week course for energy conservation. Tucson (AZ): Therapy Skill Builders; 1995.
- Matuska K, Mathiowetz V, Finlayson M. Use and perceived effectiveness of energy conservation strategies for managing multiple sclerosis fatigue. Am J Occup Ther. 2007;61:62–69.
- Law M, McColl MA, Paterson M, et al. Canadian occupational performance measure. Can J Occup Ther. 2000;67:22–30.
- Carter ST, Little M. Justifying knowledge, justifying method, taking action: epistemologies, methodologies, and methods in qualitative research. Qual Health Res. 2007;17:1316–1328.
- Jensen MP, McFarland CA. Increasing the reliability and validity of pain intensity measurement in chronic pain patients. Pain. 1993;55:195–203.
- Matthews SH. Crafting qualitative research articles on marriages and families. J Marriage Fam. 2005;67:799–808.
- Bogdan RC, Knopp Biklen S. Qualitative research for education: an introduction to theories and methods. Boston (MA): Pearson Education Group, Inc.; 2003.
- Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant 2002;36:391–409.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- Golafshani N. Understanding reliability and validity in qualitative research. Qual Rep. 2003;8:597–606.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
- Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20:64–78.
- Schoot T, Proot I, ter Meulen R, et al. Recognition of client values as a basis for tailored care: the view of Dutch expert patients and family caregivers. Scand J Caring Sci. 2005;19:169–176.
- Bandura A. Self-efficacy. In: Ramachaudran VS. editor. Encyclopedia of Human Behavior. New York (NY): Academic Press; 1994. p. 71–81.
- Audulv A. The over time development of chronic illness self-management patterns: a longitudinal qualitative study. BMC Public Health. 2013;13:452.
- Doig E, Fleming J, Cornwell P, et al. Comparing the experience of outpatient therapy in home and day hospital settings after traumatic brain injury: patient, significant other and therapist perspectives. Disabil Rehabil. 2011;33:1203–1214.
- Sandelowski M. Sample size in qualitative research. Res Nurs Health. 1995;18:179–183.
