Abstract
Purpose: Classical galactosaemia is an inborn error of galactose metabolism which may lead to impairments in body functions and accordingly, need for additional care. The primary aim of this study was to establish the type and intensity of this additional care.
Materials and methods: Patients with classical galactosaemia aged ≥2 years were evaluated with the Capacity Profile, a standardised method to classify additional care needs according to type and intensity. Based on a semi-structured interview, current impairments in five domains of body functions were determined. The intensity of additional care was assessed (from 0, usual care, to 5, total dependence).
Results: Forty-four patients with classical galactosaemia, 18 males and 26 females (median age 15 years, range 2–49 years), were included. There was a wide spectrum of impairments in mental functions. Motor function impairments were present in four patients, and mild speech impairments in eight patients. Additional care for sensory functions was uncommon. All patients needed a diet, which care is scored in the physical health domain.
Conclusions: Apart from the diet all patients need, classical galactosaemia leads to the need for additional care mainly in the domains of mental functions and speech and voice functions.
The Capacity Profile is a useful tool to demonstrate additional care needs in classical galactosaemia.
In classical galactosaemia additional care is mostly indicated by mental impairments and speech and voice functions.
One-fifth of patients have impairment of speech and voice functions at time of the study, and half of all patients had received speech therapy in childhood.
Over 70% of patients need additional care/help due to impairment of mental functions, ranging from coaching due to social vulnerability to full day care.
Implications for rehabilitation
Introduction
Classical galactosaemia (OMIM 230400) is an inborn error of galactose metabolism, caused by a severe deficiency of the enzyme galactose-1-phosphate uridyltransferase (EC 2.7.7.12). Affected newborn infants who are fed galactose-containing milk, develop a life-threatening illness (liver failure, kidney failure, sepsis-like symptoms, and Escherichia coli sepsis) that quickly resolves after the start of treatment: a life-long galactose-restricted diet [Citation1]. Despite early diagnosis and treatment, patients are at risk for long-term complications, including decreased cognitive abilities, neurological complications (movement disorders), speech (verbal dyspraxia), and language problems, and bilateral cataracts presenting in the neonatal period [Citation2]. Though there is a high frequency of these different complications, the consequences of these impairments in body functions for daily life and participation have not been studied. These impairments may limit the capacities of the affected person, leading to the need for ongoing additional care. Recognition of impairments is important for planning of individual care, and for the implementation of adequate and timely medical interventions. For parents, information about the future need for care is important to help them to set realistic goals, and to make adequate arrangements for the child’s future requirements. The Capacity Profile is a standardised method for classifying additional care needs in permanent conditions, indicated by current impairments in five domains of body functions: physical health, motor (neuromusculoskeletal and movement-related), sensory, mental, and voice and speech functions. The intensity of care in each domain is defined from 0 (no need for additional care) to 5 (needs help with every activity), and indicates the Capacity Profile for the individual patient [Citation3]. By scoring the dependency on additional care in each separate domain irrespective of the need for care in the other domains, and not combining the five scores into one single Capacity Profile score, insight is obtained about the contribution of the additional care to the various domains. In the development of the Capacity Profile the International Classification of Functioning, Disability and Health was the frame of reference.
The aim of this study was to assess the current impairments in body functions in patients with classical galactosaemia, and the subsequent need for additional care, using the Capacity Profile as a test instrument.
Materials and methods
Research design
We performed a cross-sectional study, in which Capacity Profile scores for the five domains of body function were determined in a single semi-structured interview with patients and/or parents. Additional questions were asked concerning: time of start of dietary treatment and dietary compliance, current and past interventions (speech and language therapy, physiotherapy, and mental health care), educational attainment, work, living situation, and relationships. Residual galactose-1-phosphate uridyltransferase enzyme activity, and genetic analysis were retrospectively collected from the patients’ medical charts.
Participants
Eligibility criteria
In the Netherlands, all patients aged ≥2 years, with a residual galactose-1-phosphate uridyltransferase enzyme activity of <15% (compared to healthy controls) and/or two known pathogenic variations in the gene encoding galactose-1-phosphate uridyltransferase, are treated as if they are classical galactosaemia patients, and were eligible for inclusion in the study. This is in line with the international guideline [Citation4] which defines classical galactosaemia as a profound impairment of galactose-1-phosphate uridyltransferase enzyme activity (absent or barely detectable), but acknowledges that newborn screening detects patients with low but not profoundly deficient galactose-1-phosphate uridyltransferase enzyme activities up to 15%. If the diagnosis of classical galactosaemia was not confirmed, patients were excluded from the analysis.
Sample size
Sample size of this study was based on feasibility.
Recruitment strategies
Patients were invited for this study via multiple routes. First, all members (n = 131) of the Dutch Galactosemia Patient Society were invited through e-mail in March 2016. This invitation was linked to an invitation for a family weekend of the society. Before this invitation, all treating physicians in the Netherlands were informed about this research.
Second, all patients who were not recruited after this invitation, who attended the outpatient clinics of the Academic Medical Center (Amsterdam, The Netherlands) (n = 20) or Radboud University Medical Center (Nijmegen, the Netherlands) (n = 20) were invited. These patients were invited between March and September 2016. By inviting all patients of two large centres, in addition to the invitation via the patient society, risk of sampling bias was minimalised.
Ethical approval and consent procedure
The Ethical Committee of the Academic Medical Center, Amsterdam, The Netherlands, confirmed that the Medical Research Involving Human Subjects Act does not apply to this research and that an official approval of this study by the Ethical Committee was not required. All patients and/or parents provided written informed consent.
Measurement
The intensity of care in each domain of the Capacity Profile is defined from 0 (no need for additional care) to 5 (needs help with every activity). A score of 1 or higher means there is impairment to an extent that adaptations in the daily programme or additional care are needed. See for a detailed description of the definitions of the intensity of additional care in each of the domains. The Capacity Profile aims to provide insight into the need for additional care, and it does not aim to compare patients to the general population, and therefore no control group is necessary. The Capacity Profile has been validated in preschool children and adolescents with variable non-progressive neurodevelopmental disorders, such cerebral palsy [Citation5,Citation6]. The Capacity Profile has not been validated for adults, and has not been separately validated for classical galactosaemia.
Table 1. Definitions of the intensity of additional care in each of the domains of the Capacity Profile.
Procedure
Patients and/or their parents were interviewed once in a quiet and private environment. If the patient was <18 years, or if the patient was a non-capacitated adult, at least one of the parents was present during the interview. All interviews were performed by the same investigator (LW) who was trained in the use of the Capacity Profile.
Statistical analysis
All results were presented in a descriptive manner. We used SPSS version 22 (SPSS, Chicago, IL) to perform the descriptive statistics. Because of a non-normal distribution, age is presented as median range.
Results
Participants
Participation rate
After the invitation through the Dutch Galactosemia Society, 32/131 invited individuals were recruited. In addition, 14 patients who had not responded after this invitation, were recruited after invitation through their treating physicians at the Academic Medical Center (12 of 20 individuals invited) and the Radboud University Medical Center (2 of 20 individuals invited). A total of 46 patients were thus interviewed, and 44 patients were included in our study; two patients were excluded afterwards because classical galactosaemia had not been confirmed with enzyme measurement or genetic analysis. All participants were interviewed between March and September 2016.
Characteristics of the respondents
Of the 44 patients included, 18 were male and 26 were female, with a median age of 15 years (range 2–49 years). This sample included 23 children and adolescents (2–17 years), and 21 adults (range 18–49 years). All patients had either a galactose-1-phosphate uridyltransferase enzyme deficiency (range 0–7.1% of healthy controls), and/or two known pathogenic variations in the in the gene encoding galactose-1-phosphate uridyltransferase.
Capacity profile scores
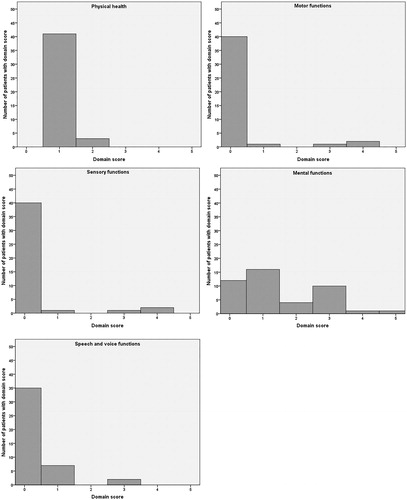
Frequency of domain scores is presented separately for each of the five domains in .
Physical health
At time of the study, all patients adhered to a galactose-restricted diet, and therefore all participants scored at least 1 at this scale (see ). Three of 44 patients needed more care (all had a score of 2); in two adults this was due to further adaptation of their daily programme because of tiredness during the day, and in one adult patient due to epilepsy that was not fully controlled with anti-epileptic medication (this patient suffered from severe motor retardation and cognitive impairment).
Motor functions
Four of 44 patients (aged 11–19 years) suffered from impairment of motor functions, scoring 1–4 on the Capacity Profile scale. These patients suffered from mild to severe tremors in their extremities, necessitating adaptations in their daily programme or extra personal help in all. All four demonstrated moderate to severe cognitive impairment with scores of three or higher on the mental functions scale. Two of these four patients additionally were wheelchair bound because of motor impairments. Of the complete group, many patients/parents reported abnormalities in fine and gross motor skills which did not lead to additional care. Reported abnormalities were: difficulties with handwriting (and other fine motor skills), stiff/clumsy gross motor skills, difficulties in learning new (sets of) movements (such as a new swim stroke or dancing moves) until automated, struggles with games and activities using a ball.
Sensory functions
Three of 44 patients (all adults) reported abnormal sensory functions (vision, hearing, and tactile sense). One patient suffered from glares in his vision due to cataract. The other two patients suffered from hearing impairment, unrelated to the galactosaemia, which indicated adaptations in their daily life (score of 1).
Mental functions
Scores on the mental functions scale ranged from 0 to 5, with a median of 1.
Of the adults, 6/21 patients had a score of 0, and were thus not in need of any additional help or coaching, and received normal primary and secondary education.
Nine of 21 adult patients had a score of 1, mainly due to the fact that they were socially vulnerable and needed some coaching in their daily life. Most of these patients had difficulties with social interaction, such as making contact with others and maintaining friendships. Of these patients, four received special education in primary school, of which one also received special education in secondary school. Three patients had a score of two, due to learning problems and need of frequent coaching and support from others. One of three patients received special primary education, but all received normal secondary education. Two patients had a score of three, because they had severe learning problems and/or were in need of daily support from others. One of these two received special primary and secondary education, the other patient received normal education but suffered from autism. One patient had a score of four (severely impairment intellectual disability), and was fully dependent on the care.
Of all adults, 18/21 were living independently (all had a score of 0, 1, or 2 on the mental functions domain) or would be able to live independently in the near future, as four patients were aged <22 years and lived with their parents. The three patients who were not able to live independently had domain scores ranging from 2, 3, and 4, respectively, on the mental functions domain.
Of the children, 6/23 patients had a score of 0, and thus received normal education (two patients were not in school yet). Seven of 23 patients had a score of 1, mainly because they were socially vulnerable and parents reported these children to behave young for their age. One patient was not in school yet, two were in primary school and received normal education. The five others were in secondary school, of whom one received special education. One of 23 patients had a score of 2, and this patient was in kindergarten at the age of six and not ready yet to receive primary education. Eight of 23 patients had a score of three, because of severe learning problems and/or need of daily support from others. Three patients were in primary school and received special education, and five were in secondary school and all received special education. Zero patients had a score of four, and one patient had a score of five (severely impairment intellectual disability), and was fully dependent on care.
Many patients who received normal education, or had received normal education in childhood/adolescence, reported extra help in school specifically for math, reading, and languages, both in primary and secondary education.
Speech and voice functions
Out of 44 patients, nine (of whom five children and four adults) suffered from impairment on the speech and voice functions scale. Reported problems differed in severity and included articulation errors, speech sound errors (phonemes), disturbed voice quality, and speech difficult to understand (mainly mumbled speech). The majority had a score of one, meaning that listeners had to concentrate more, and understanding in telephone conversation was difficult. Many parents of children reported difficulties with phonemes, but these difficulties did not always result in clear impairment of speech function, therefore not leading to a score above zero on the scale. Out of 44 patients, 22 were received speech and language therapy in the past, and four received speech and language therapy at time of the study.
Discussion
The aim of this study was to assess the type and intensity of the need for additional care in patients with classical galactosaemia using the Capacity Profile. The importance of identifying such impairments lies in achieving early recognition and timely initiation of appropriate extra help, care or treatment, to facilitate participation. Moreover, defining the severity of disorders in this way, provides insight in the efforts that parents, other caregivers, and society, should make. Ranging from 0 to 5, a CAP score of 1 or higher indicates the need for adaptations in the daily programme or need for additional care. The most frequent impairment besides the dietary adaptations, with also the widest spectrum, was found in the domain of mental functions, which is in line with the spectrum of cognitive abilities found in patients with classical galactosaemia, which ranges from severely decreased to above average. The mental function’s domain also includes social elements. Remarkably, there is are large group of patients with a score of 1 (16 of 45 patients), with (low) normal cognitive abilities, and usually normal education, but in need of additional care/help in the form of coaching due to social vulnerability and difficulties in social interaction. Because the Capacity Profile is not designed to specify the type and severity of problems in social functioning, future research is warranted to further explore social functioning in patients with classical galactosaemia.
Also in line with previously published results about childhood apraxia of speech and other speech and language defects in classical galactosaemia, 9 of 45 patients had some impairment of speech. Half of all patients received speech and language therapy in childhood.
Most patients did not have impairment of motor functions leading to adaptations in their daily life, but four patients suffered from invalidating tremors and two patients were wheelchair dependent. All suffered from intellectual disability as well, scoring 3, 3, 4, and 5, respectively, on the mental functions scale. Many other patients reported difficulties regarding fine motor skills (handwriting), learning new sets of movements, clumsiness, etc. At the time of the study, these patients did not report adaptations in daily life or need for additional care for these problems, but this seemed to have an effect on their self-esteem. In the domain of physical health, all patients had some adaptation in their daily programme because they all need to adhere to a galactose-restricted diet, but the vast majority of patients did not have further problems leading to impairment of physical health, felt healthy and had normal daily programmes. Only one patient suffered from impairment in sensory functions as a result of classical galactosaemia, as he reported glares in his vision due to residual cataract. Two other patients suffered from hearing impairment, which is not a known complication of classical galactosaemia. The difficulties in motor skills in combination with the social difficulties, suggests the possibility of developmental coordination disorder, which has not been described before in classical galactosaemia. Recognition of such problems is important because different therapeutic interventions for children with (characteristics of) developmental coordination disorder are available: task-orientated therapy (aims to improve specific tasks through practice) and process-oriented therapy (concentrating on developing sensory modalities involved in motor performance) [Citation7]. Also, therapies focusing on self-esteem have been developed. Future studies into this are warranted.
This study has several strengths and limitations. This is the first study to systematically evaluate the need for additional care resulting from impairment in body functions in these patients. The Capacity Profile has shown to be a helpful and effective tool in evaluating the need for additional care as the consequence of the current impairments in individual patients with galactosaemia. Strength of this study is the representativeness and size of the patient sample included. By not only inviting patients through the patient society, but also all patients followed by two major metabolic centres in the Netherlands, risk of sampling bias was kept as small as possible. The patient sample includes about one-fourth of all patients with classical galactosaemia known in the Netherlands.
The main limitation of this study is that the Capacity Profile is not a diagnostic tool, but a tool to classify the need for additional care. If impairments are reported by a patient or parents, additional assessment should be performed to further determine the type and extent of the impairments. In galactosaemia, the regular follow-up as advised by the international guideline, should be performed [Citation8]. To date, it is not known if initiation of additional care for the impairments, such as identified by the Capacity Profile, will lead to a better quality of life in the individual patient.
In conclusion, we demonstrated the need for additional care as the consequence of impairments in body functions in classical galactosaemia. These impairments occurred most frequently in the mental functions domain, with specific problems in social functioning, which have not been reported in such detail before. Ten percent of patients with classical galactosaemia had motor function impairment due to tremors, and some may have characteristics of developmental coordination disorder; however, not leading to impairments. Impairment of speech and voice function was common, but was usually mild. Impairment of physical health (above the need for compliance to a galactose-restricted diet) and sensory functions were uncommon.
The need for additional care, resulting from impairments in body functions, in patients with classical galactosaemia has now been clearly defined using the Capacity Profile tool. The results of this study are in line with the expected natural course of the disease under dietary treatment, and additionally demonstrate that impairments frequently lead to the need for additional care and help. This emphasises the need to monitor the appearance of the potential impairments associated with the disease, as described in the recent international guideline [Citation4], to achieve early recognition and timely initiation of appropriate extra help, care or treatment, to facilitate participation of patients with classical galactosaemia.
Supplemental Material
Download PDF (159 KB)Acknowledgements
The authors would like to thank the Dutch Galactosemia Foundation for supporting this research.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Berry GT. Classic galactosemia and clinical variant galactosemia. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews [Internet]. Seattle (WA): University of Washington; 1993–2018.
- Bosch AM. Classical galactosaemia revisited. J Inherit Metab Dis. 2006;29:516–525.
- Meester-Delver A, Beelen A, Hennekam R, et al. The Capacity Profile: a method to classify additional care needs in children with neurodevelopmental disabilities. Dev Med Child Neurol. 2007;49:355–360.
- Welling L, Bernstein LE, Berry GT, et al. International clinical guideline for the management of classical galactosemia: diagnosis, treatment, and follow-up. J Inherit Metab Dis. 2017;40:171–176.
- Meester-Delver A, Beelen A, Ketelaar M, et al. Construct validity of the Capacity Profile in preschool children with cerebral palsy. Dev Med Child Neurol. 2009;51:446–453.
- Meester-Delver A, Beelen A, Van Eck M, et al. Construct validity of the Capacity Profile in adolescents with cerebral palsy. Clin Rehabil. 2010;24:258–266.
- Gibbs J, Appleton J, Appleton R. Dyspraxia or developmental coordination disorder? Unravelling the enigma. Arch Dis Child. 2007;92:534–539.
- Berry GT, Palmieri M, Gross KC, et al. The effect of dietary fruits and vegetables on urinary galactitol excretion in galactose-1-phosphate uridyltransferase deficiency. J Inherit Metab Dis. 1993;16:91–100.