Abstract
Purpose: Rebuilding one’s life after stroke is a key priority persistently identified by patients yet professionally led interventions have little impact. This co-design study constructs and tests a novel peer-led coaching intervention to improve post-stroke leisure and general social participation.
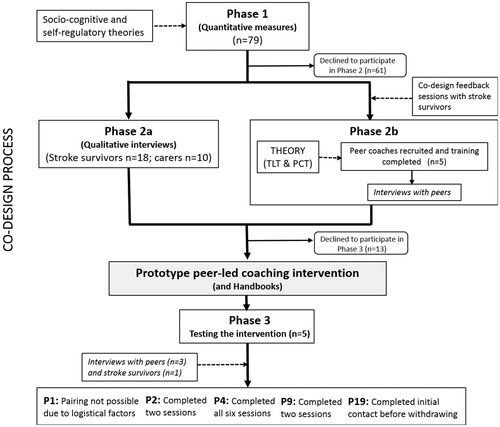
Methods: This study followed the principles of co-design by actively engaging and harnessing the knowledge of stroke survivors in order to develop and test a peer-lead coaching intervention. Phase 1 assessed function, mood, and involvement in leisure and social activities 6 months following stroke (n = 79). Phase 2 involved semi-structured, in-depth interviews with 18 stroke survivors, and 10 family carers to explore experiences related to social and leisure participation. Phase 3 tested the co-designed peer-led coaching intervention. Data collected also included co-design feedback sessions and a training workshop with selected peer coaches and in addition, interviews with stroke survivors and their peer coaches at two time-points: following the training program (n = 5) and delivery of the intervention (n = 2).
Results: A peer-coaching intervention was successfully co-designed and tested combining the use of lay knowledge sociocognitive and self-regulatory theories with principles of transformational leadership theory. Both peers and stroke survivors reported having benefited at a personal level.
Conclusions: This study reports on an innovative community-based and peer-led intervention and its results have generated new evidence on how stroke survivors engage with and respond to peer coaching support. It further provides a theoretical platform for designing and implementing peer interventions. Hence, these results have the potential to inform the development of future peer coaching intervention not only for stroke rehabilitation but also for a wide range of chronic conditions.
The results of this co-design study, if replicated and extended, provide a theoretical framework to guide rehabilitation professionals about the optimal timing of peer-coaching interventions and contextual factors that need to be taken into account.
Applying transformational leadership theory principles to the training of peers may prove useful at the time of the implementation of a coaching intervention.
Peer-led coaching interventions, which are community-based and tailored to stroke survivors at the time of discharge, may help support re-engagement in social and leisure activities.
Implications for rehabilitation
Introduction
Stroke is the third most common cause of disability in the UK, and represents a significant financial burden to society [Citation1]. The consequences of stroke for survivors and their families are complex, impacting on social as well as physical aspects of life [Citation2–4]. Indeed, one of the top ten research priorities for Life After Stroke identified by the James Lind Alliance was: “What are the best ways to improve confidence and behavioural activity after stroke, including stroke clubs or groups, offering support, one-to-one input, and re-skilling?” [Citation5]. The impact of stroke can be devastating and can involve a prolonged period of recovery [Citation4].
There is consensus that people after stroke benefit from engaging in physical activity [Citation6] and social and leisure activities [Citation7]. Despite this, a particular challenge after a stroke is that people can find it difficult to maintain adequate long-term engagement in these activities or start new ones. This is important, as research shows that those people who do not engage in social and leisure activities are more likely to become depressed and have reduced quality of life [Citation7–9]. Finding new ways of helping people engage in social participation is consistently identified as a service development priority by people affected by stroke [Citation10], however the evidence-base to inform how and what support should be provided is limited. Trials of occupational therapy interventions to promote social and leisure engagement have had non-significant results [Citation11,Citation12]. The effects of leisure-oriented interventions have been mixed, perhaps reflecting a limited theoretical base, which has focused on awareness raising and education [Citation13]. There is some evidence from a trial of a community-focused rehabilitation program where, although disability levels of participants did not show a significant reduction, participation in leisure activity and satisfaction with life increased [Citation14].
This paper presents the outcomes of a co-design study that sought to address these issues by devising, implementing and testing a peer-led coaching intervention with stroke survivors for stroke survivors, focused on reengaging in social and leisure activities. Currently, peer-led interventions are proving to be effective as a way of coping with stressful life experiences [Citation15,Citation16] and the devastating consequences of conditions such as stroke [Citation6,Citation17], spinal cord injury [Citation18], Alzheimer’s disease [Citation19], and multiple sclerosis [Citation20]. For example, a recent study assessing an intervention that consisted of a short visit to hospital to stroke survivors by peers prior to discharge and follow up telephone calls [Citation17] revealed important benefits for stroke survivors, carers, and peers by providing encouragement, motivation and by reducing the feeling of isolation. In their study [Citation17], the aim of the initial hospital visit was to provide hope, support, and information on available resources in the community. A report by Nesta [Citation21] has summarized the diverse forms of peer coaching initiatives and their respective costs and benefits. This report has highlighted the utility of peer work but also has identified the challenge of how best to integrate peer coaching into “mainstream services”.
A number of studies have shown the potential benefits of peer support initiatives for stroke survivors. However, researchers and health professionals agree that there is still the strong need for further research to determine preferred formats and timings (i.e. acute hospital versus rehab hospital versus home) in order to maximize any impact [Citation22–24].
Rationale and theoretical underpinnings
This study involved the development of an intervention co-designed and delivered by trained peers who had experienced a stroke, rather than by health professionals. In line with published co-design work [Citation25], the authors believed that a co-designed peer-led intervention would become a more effective agent for change. The scope of the intervention extended beyond awareness raising and education, by engaging stroke survivors to set and achieve social and leisure related goals using face-to-face contact with a trained peer within the community 6 months after stroke.
Our review of the literature revealed that there is often a poor differentiation between the different types of peer interventions, leading to the development of a heuristic typology of peer coaching interventions (Supplementary File 1). This highlighted that peer coaching interventions could be differentiated along two dimensions. The first dimension is based on the degree of reliance on the knowledge being utilized to underpin initiatives, where, for instance, knowledge can be drawn from the professional evidence-base and represent a rather “top down” approach, through to a situation where knowledge is drawn from the experience of stroke survivors, i.e. takes a “bottom-up” approach. The second dimension is based on initiatives situated within professional services or framed as predominantly lay in orientation and control.
In the hospital-based Inpatient Support Program In REcovery from Stroke (INSPIRES) program [Citation26], which is significantly informed by the transfer of experiential knowledge, people in the early stages of stroke are able to access informational, practical and emotional support from one of 12 peers. Peer volunteers are provided with a mix of training and on-going support, including a “Living with Stroke” class, program-specific educational sessions, and buddy visits to stroke services. Peers typically support up to 50 patients per month. This program has been very positively received by patients and family members and has identified the importance of preparing peer volunteers in order to enabled them to lead its implementation. The prototype intervention codesigned and tested in our study is based on the transfer of experiential knowledge but less embedded in formal rehabilitation services and is underpinned by sociocognitive models of behavior and behavior change [Citation27,Citation28], self-regulatory theories of illness self-management [Citation29], and principles of transformational leadership theory (TLT) [Citation30] and personal construct theory (PCT) [Citation31]. Previous psychosocial studies have demonstrated that attitudes towards recovery, perceived control, or self-efficacy, illness perceptions, and perceived and received social support, are commonly associated with functional and emotional outcomes in chronic disease including stroke [Citation32,Citation33]. This study investigated individual beliefs to identify those associated with stroke survivors’ willingness to and engagement in social and leisure activities.
Aims and objectives
The overall aim of this study was to co-design and test a novel peer-led coaching intervention that enabled stroke survivors to rebuild meaningful social and leisure activities after stroke. The specific objectives were to:
Investigate factors perceived as impacting on stroke survivors’ ability to resume leisure and general social participation 6 months after stroke.
Explore the relationship among stroke survivors’ beliefs, intentions and experiences of rebuilding their leisure and social activities in their lives post stroke.
Co-design and test a prototype peer-led coaching intervention.
Identify requirements for the preparation, support, and supervision of peer coaches.
Methods
This study followed the principles of co-design [Citation25,Citation34] by actively engaging stroke survivors in order to develop a peer-lead coaching intervention. The following three phases were carried out:
Phase 1: investigation of stroke survivors 6 months post stroke
The study population comprised all patients who had been admitted to hospital with a diagnosis of stroke within the prior 6 months and had been discharged and were residing in community settings (rather than care homes, where the context of leisure and social participation is different). Three sites were recruited into this study.
The aim of this phase was to assess function, mood, and involvement in leisure and social activities of stroke survivors 6 months post stroke. It was underpinned by socio-cognitive and self-regulatory theories of illness self-management. This phase of the study tested the hypothesis that those stroke survivors who perceive more control over their treatment and their stroke symptoms, and have higher understanding of stroke, higher recovery expectations, and a positive attitude will be the ones more likely to engage in leisure and social participation. A research nurse with stroke research experience, scanned the stroke register, and posted a Study Information Pack to all eligible stroke survivors. Of those participants that consented to take part, health records were accessed to obtain demographic (age, gender, and living arrangements) and stroke data (1) stroke type—Oxford Stroke Classification; (2) stroke severity—Modified Rankin [Citation35] on admission to acute stroke service; (3) length of stay; (4) functional dependence—Barthel Index [Citation36] on first transfer of care to community setting; (5) mood (General Health Questionnaire v12 [Citation37]) on first transfer of care to community setting). Research nurses visited all stroke survivors recruited for phase 1 to complete a number of measures ().
Table 1. Measures completed by stroke survivors recruited for phase 1.
Phase 2a: exploration of stroke survivors’ experiences of leisure and social participation
The purpose of this phase was to provide exemplary, rather than generalizable information in regards to stroke survivors’ intentions and experiences of rebuilding social and leisure participation. In-depth semi-structured interviews were carried out 6 months post stroke. The interviews explored the following issues: personal meanings attached to social and leisure activities, the type and effects of stroke in the level of engagement, the role of environmental factors (e.g. the availability and access to opportunities), personal factors such as motivations and beliefs, expectations, and experiences of support from others and professional help. Carers were also invited to be interviewed separately to explore factors that may promote or inhibit patient engagement. All participants recruited to phase 1 were offered the opportunity to take part in phase 2 and were given an information pack and consent form to sign. Interviews were carried out by the main author (PMA) who arranged to meet the participants at their home at a day and time that was convenient for them. Family members and carers were able to attend the interview to support patient/stroke survivor communication if desired. Subject to consent, interviews were digitally recorded and fully transcribed.
Phase 2b: peer training and co-design of peer-led coaching intervention
Peers were recruited via advertising the study in local stroke groups and in the local newspaper. Those recruited would be in charge of delivering the intervention. In order to prepare them to be able to do so and to contribute to the design of the intervention, a training workshop was organized. The workshop was designed by the main author who has an occupational therapy and research background. As a research activity, written informed consent to take part in the training was obtained from all participants. The training was based at Bangor University and consisted of four days of in-class sessions which took place over a period of 2 weeks. After consultation with those recruited as peers, each training day was around 3 h long. The training was delivered in a flexible way that promoted open discussions and allowed participants to co-design the peer intervention as well as engage in shaping the training content (). Accordingly, the content and means of delivery of the training were modified as the training progressed, with the use of brief presentations, open discussions, individual and group work. Each session started with an opportunity for participants to reflect on the previous training day and discuss any issues which they wished to revisit.
Table 2. Peer training content.
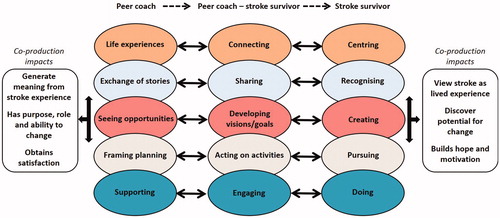
The training package was informed by principles of TLT [Citation30] and PCT [Citation31]. TLT is a behavioral approach to leadership that delineates leader behaviors that are proposed to have a positive influence on followers. These behaviors typically include elements of caring, support, and positive role modeling behaviors. PCT is underpinned by the premise the people try to make sense of the world by developing personal theories. These personal theories can then be used to help individuals anticipate future events and revise their personal theories based on their experiences of these events. In this study, both TLT and PCT focused on enabling peers to use their experiential and biographical resources to think about goal setting and activity analysis (). This theoretical underpinning enabled the potential replication of the training package in differing contexts with a range of peers. During the training, peers had access to products that provided a “scaffold” for peer coaching. These products were initially co-designed for the study, through detailed work with two peers who regularly met with the research team in order to define what the peer coaching intervention would consist of. They were subsequently modified by the remaining peers during the training workshop. These consisted of: a Peer Handbook which (Supplementary File 2) provided material collated to reinforce the training, with tools and scripts to facilitate coaching interventions and a Stroke Survivor Handbook (Supplementary File 3) which included information about the project and a brief summary of proposed aims and content of each of the peer-led sessions. By the end of the training, one of the authors (SW) carried out interviews with all peers. With the input of the peers, the prototype peer coaching intervention and supporting tools were designed and finalized.
Phase 3: testing the prototype peer-led coaching intervention
All stroke survivors who completed phase 2 were asked about their willingness to be part of phase 3. Those participants who expressed an interest were asked to complete the consent form and once this was received arrangements were made to pair them with a suitable coach. The pairing was done by the main author and was based on characteristics of openness and positivity together with post-stroke symptoms of both the peer and the stroke survivor. Geographical separation was also taken into account as distance could undermine the successful delivery of the coaching intervention.
Once the coaching sessions were over one of the authors (SW) interviewed both the peers and stroke survivors in order to explore their experiences of peer coaching. Subject to consent, interviews were digitally recorded and fully transcribed.
Data analysis
Numerical data was analyzed using SPSS v22. Relevant descriptive statistics summarized central tendency and variation for all variables (clinical, social, or psychological predictors of social participation, engagement in, and satisfaction with leisure activities). In order to help identify the factors that impact on stroke survivors’ use of spare time, correlation analyses were also carried out between the measures and the concurrent engagement with leisure activities. Furthermore, the assessment of the influence of role of age and gender upon outcome measures was carried out in order to inform whether the design and/or delivery of the peer intervention required any tailoring.
All qualitative data analysis followed a constructivist grounded theory (CGT) approach [Citation38], which centered on understanding the social process and the experience of “being a peer” and “engaging with peer support” by generating categories. Firstly, the main author analyzed a subsample of interviews (three) and this led to an initial coding framework being formulated to support the development of identified categories. All the remaining transcripts were then analyzed using constant comparative analysis, supported by the developing coding framework. New codes were added until data saturation was reached [Citation38] and emergent categories were sufficiently delineated. All the final codes and the higher level categories were grounded with their relevant data extracts. The data analysis procedures were subject to crosschecking by the coauthors across all the transcribed data, in order to ensure rigor in the application of analytic procedures and check for clarity and consistency of the emergent codes and categories. Data management included the use of Atlas-Ti software.
Ethical approval for this study was obtained from Wales REC 4 Ethics Committee on the 8th of August 2014 (REC 4 14/WA/1092) as well as the Healthcare and Medical Sciences Academic Ethics Committee (Bangor University, July 2014).
Results
A prototype peer coaching intervention was co-designed and tested following the process described in .
Initial co-design work
In total, n = 79 stroke survivors (49 males, 30 females; mean age 69.66 (SD 11.81), range 40–96 years) completed phase 1 (). The length of stay in hospital measured in days ranged from 1 to 96 with a mean stay of 17.02 days (SD 22.22). The highest populated class was posterior circulation syndrome (POCS) with 10 participants followed by lacunar syndrome (LACS) with 6 participants and partial anterior circulation syndrome (PACS) with five participants. Results from descriptive statistics are summarized in . As seen in , on recruitment to the study, the sample exhibited high levels of independence (mean Barthel score 90.67 SD 18.71), low levels of distress (mean GHQ12 of 14.14 SD 6.68), moderate-high stroke impact (mean score 29.98 SD 7.18) and moderate-high self-efficacy (GSES 30.17 SD 6.97).
Table 3. Descriptive statistics of sample of 79 stroke survivors.
In terms of what environmental factors were considered to impact on their ability to complete their chosen activity participants’ answers showed a wide spread (). The most prevalent barrier was ‘not feeling comfortable’ in the location where the chosen activity took place (n = 13). Most of the participants (n = 69) did not think that cost, a suitable location (n = 70) or carer support (n = 63) had a negative impact on them being able to complete the activity. Thirty-one “other” reasons were recorded which included bad weather (n = 4), family difficulties (n = 2), and medication issues (n = 3) amongst others.
Figure 2. Environmental barriers to the completion of the activity (X being an important social or leisure activity that the stroke survivor used to do regularly before having their stroke).
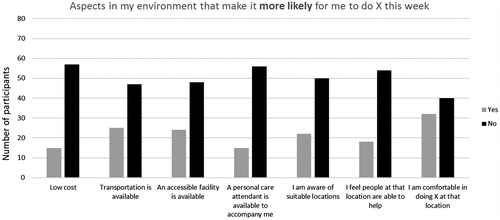
Age (using Pearson’s correlation) and gender (using t-test) were also assessed in relation to all the measures. There was no evidence of an association between age and any of the measures. There was no evidence of a difference between genders for any of the measures.
Associations between each of the outcomes and Leisure Profile use of spare time score (a measure of engagement with leisure activities) were calculated (Pearson’s correlation coefficients). All measures were correlated in the direction expected and for the majority significantly so (). Many of the sociocognitive variables derived from the Theory of Planned Behaviour were not significantly correlated with engagement in leisure activity, but critically perceived behavioral control was, and a trend is seen with motivation to comply. Those high in perceived behavioral control and motivation to comply were more engaged in leisure activity. Consistent with hypotheses, all of the illness perception components were significantly associated with engagement in leisure activity.
Table 4. Summary of correlations between engagement in leisure activities and the outcome measures.
In summary, correlation results showed that those stroke survivors who have a positive attitude to their recovery, who feel more in control over their treatment and recovery and who believe in their ability to manage symptoms and remain motivated were the ones who showed higher engagement in leisure and social participation. The two stroke survivors who attended the co-design feedback sessions () agreed with these results and identified the peer coaching intervention as focused on the dynamic between a stroke survivor and a peer coach (a person affected by stroke) who helped the participant review illness perceptions and self-efficacy beliefs. According to the stroke survivor, the peer supported the stroke survivor in (1) Establishing a meaningful social and leisure goal, (2) Developing a shared vision for that goal that reflected mutual experiences, capacity and resources, (3) Translating this goal into achievable steps and finally, (4) Providing support and challenge through role modeling to encourage achievement. This was illustrated via an initial framework that schematically depicts a dynamic and iterative-reflexive process whereby the stroke survivor and the peer move through a number of phases as part of peer-led work (). The framework illustrates the anticipated impacts from these interactions for both peers and stroke survivors representing distinct but separate outcomes for both parties.
Mapping experiences of stroke and social and leisure activities
A total of n = 18 stroke survivors and n = 10 carers consented to be interviewed at their homes for phase 2 (). This produced in-depth descriptions of beliefs, experiences, and (dis)engagement with social and leisure activities. Following the method described above six higher order categories emerged from the data ().
Figure 4. Relationship amongst lower and higher level categories (ADL – activities of daily living).
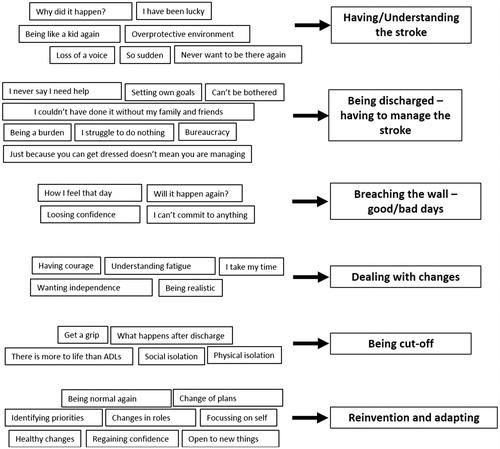
Table 5. Summary information of participants who took part in Phase 2.
Having the stroke participants described having the stroke as a life event that impacted in all aspects of their lives, although it was initially poorly understood by participants in its early stages. During the interviews, participants often stated “I didn’t know what was wrong” (P19). Most participants could recall feeling that something was not right and slowly going through the motions. As one participant expressed: “I was a disconnected valley individual” (P4). Participants described their stroke as sudden and unpredictable: as a female stroke survivor put it: “It all happened too quickly really, and no idea why, I was very fit before” (P2).
Overall participants and their carers were content with the treatment they received in hospital, however, most of them recalled feeling trapped and disheartened in hospital by not having their own space and feeling overprotected:
I’d never, ever want to go back to that place again, although they were fantastic. It’s just a horrible place to be when you’re … when you’re not used to it. You know. I’m used to doing what I want to do, when I want to do it, and all of a sudden everyone is protecting me and I’m not allowed to move from here without saying to somebody ‘Can I go?’ (P15)
Although they described their experience of stroke as very difficult, participants explained that whilst in hospital they often felt they had been lucky. As one participant explained “I could have had it worse, I was surrounded by people that were completely out of it” (P6).
Managing the stroke interview data showed how all participants were aware of the important role that carers and family support had played in their recovery once they were discharged home: “I’m very lucky, I know I’m lucky. I had a very good family and circle of friends prior to this happening … you know. It would be very different for people that haven’t got that” (P13). In line with phase 1 quantitative results, those participants with more control over their recovery and a strong support network (family members and friends willing to help nearby) explained that they would not have been able to resume their everyday activities without it. Yet participants expressed difficulty in asking for help as, in their minds, this could lead to them becoming a burden to their families: “I don’t like asking for help because in my mind then, I am being a burden; although they say I’m not” (P7).
Two participants explained how OT input after discharge had made a difference to them and had built up their confidence (associated with self-efficacy) as to what they could do by themselves. On the other hand, when discussing recovery goals participants explained “They check that you can feed yourself and wash yourself and dress yourself but then that is it. And there is much more to it than that” (P9). Participants felt they needed to be in charge of their recovery and establish their priorities and goals, in other words, decide what they wanted to start doing again. One participant, who was a radio presenter, reported: “the speech is what I wanted to get back, more than anything because I enjoyed doing the radio” (P13). As reflected in the quantitative data, those participants who had set goals for themselves reported greater confidence in getting back to doing the things they enjoyed and engaging in social and leisure activities.
Good/bad days: all participants explained how one of the hardest things they have had to learn how to manage is the daily changes in mood and stamina. The good/bad day changes have an impact on their ability to resume normal life and resume social and leisure activities, as reported by one participant “I can’t commit to anything because I don’t know how I am going to feel on that day” (P19). As quantitative data reflected, participants taking part in interviews identified how these uncertainties had impacted on their confidence levels and ability to engage in social and leisure activities, especially when they have pushed themselves ‘too hard’ and suffered the consequences. As one participant discussed in regards to going back to work “The minute I started back at work, and tried my best, then failed, instantly my confidence left. And I’m not sure what kind of life is ahead of me now” (P2).
Dealing with changes overall participants explained how their energy levels had depleted after having their stroke. Participants explained how they “feel tired all the time” or as one participant explained, “I feel like I could just lie down all day” (P10). For most participants managing fatigue and tiredness had been a learning process of trying to come to terms with it and fitting ‘resting time’ into daily routine:
It can be frustrating in terms of tiredness, but it varies. Immediately after the stroke I would last until 11 in the morning and then it would be like, switch of. Now it varies a lot more, yes, some days, middle afternoon sometimes I will be going the whole day. (P4)
Participants and family members often discussed how since their stroke they have had to be realistic and change the way they look at the future, including their ‘retirement plans’. One couple explained:
It is frustrating, there is always so much you want to do that you haven’t been able to do and you… we were hoping, you know, this would be our time to do these things, but you know, things don’t always work out. (P6)
Being cut off: overall participants felt that post-discharge support was “not the best”. One participant explained, “I feel like you are chopped out of the system” (P6). Another participant had a similar view as she stated, “then you come home to nothing, they pop in and check you are all right but they do that for a couple of weeks and then that is it” (P4). Participants often explained that they felt health professionals were expecting them to “Get a grip. Get on with it” (P17) and that this had had a negative impact in their confidence as they struggled in their everyday life, especially in those cases when the stroke survivor had little support from family and friends. For a number of participants, the stroke had affected their social life as the illness made them have to “pull out from the social circle” (P16) since they could not go out as often with friends. In many cases, this isolation had been further exacerbated by the impact of not being able to drive and “get to places” (i.e. Loss of independence).
Reinvention and adapting/acceptance: in line with results from the quantitative analyses, participants and carers reported that they were more in control of their recovery and were aware that along the recovery path they had to ‘reinvent’ themselves were more successful at re engaging in social participation. This reinvention process was not seen in all participants, with others engaging in what was described as ‘refocusing on self’ following their stroke with participants explaining that since their stroke they had made a conscious effort on slowing down and thinking about themselves more than they did before. One participant explained it in this way:
“I have taken a backwards step now. Instead of being a hare, who was always rushing ‘round and trying to do everything, I’m now … the tortoise. Who … is at the back, and, if it gets done, it gets done. It doesn’t get done … it’s not going to kill me, is it? (P11)
Adapting to life following stroke was focused on realigning priorities as noted by a participant:
“After the stroke, I’ve had to change my life. Completely, you know? No stress, and whatever stresses me out, I have to switch off, I have to with the children if they are here. If they stress me out “go away!” and I have to be like that, which is totally different for me”. (P2)
Prototype peer-led coaching intervention
A prototype peer-led coaching intervention was co-designed and tested. This included a maximum of six coaching sessions, each lasting up to 1 h and taking place in public setting of their choice (e.g. café, library, etc.). provides a summary of sessions and their goal. The peer coach was paired with a participant and asked to contact them directly (via telephone call) to arrange delivery of the coaching intervention. On completion of the six sessions, participants, if interested, were directed to on-going support from organizations within the locality (e.g. voluntary sector support services/GP/local gyms). Whilst delivering the intervention, peers were regularly in touch with the author (PMA) who was able to provide peer-debriefing and follow-on support as needed.
Table 6. Sessions framework.
Five peers (3 males and 2 females) were recruited into the study. They all completed the training. Out of the 18 stroke survivors who completed phase 2, five consented to phase 3 (P1, P2, P4, P9 and P19). The main reason that participants gave for not wanting to take part in phase 3 was the fact that they were happy with the level of help they had from family and friends and did not feel they needed any extra support. Amongst these 5, three were women and two were men, all apart from one where 60 years or under. None of them were working at the time of the study; four of them had stopped working due to their stroke and had not been able, due to ill health, to go back since. Only one (P4) completed all six sessions of the peer coaching intervention. Two participants completed two of the sessions before withdrawing from the study (P2 and P9). One participant withdrew due to family commitments and explained that she considered she had benefited from those two sessions but did not think further sessions would further benefit her. The other participant explained that complex family circumstances mean that she was unable to commit to the study. One participant consented but due to unavailability of the right peer because of large geographical distance the coaching did not take place. The final participant (P19) consented and engaged in the initial telephone conversation with the peer but on the day of the first session decided to stop her involvement and canceled the session. She briefly explained that she did not feel she was able to continue but when asked for a reason she did not wish to elaborate any further.
A number of interesting issues emerged from the interviews carried out with the participant who completed the six coaching sessions (P4) and with the three peers who carried out coaching sessions. The participant (P4) spoke about how he was able to engage in the process because initially his curiosity overrode his lack of confidence. He further explained that as the sessions progressed his confidence increased. In his words:
It’s a weird sort of combination of not having the confidence in social situations, but still having some curiosity. And what I did gain from … the series of interviews with [Peer] was my curiosity was further stimulated. And that might be the healing process, or it might be … just a … a slight increase in confidence. It … it allowed me to perhaps open the door a little bit, and perhaps … have the confidence to begin to step through it. (P4)
With regards to initial thoughts prior to the first meeting one peer explained:
A big worry of mine was dealing with somebody that I didn’t have anything in common with. I was lucky because the hobby he (the participant) had been doing was a big hobby of mine as well and he had not been able to do it because of his stroke so I saw that as a starting point. (Peer 1)
These feelings were shared by another peer who said, “I was nervous at the beginning, hoping that I was going to be of help and that I was going to say the right things” (Peer 2).
When participants and peers were asked to give an opinion regarding the way in which the first telephone conversation and first encounter took place (which had been agreed by peers during the training workshop), feedback was positive. However, one peer was less convinced about this option having been through the process:
If the person that interviewed the participant (researcher) was to introduce them to the peer in the first meeting maybe they would be less wary about meeting a stranger in a strange place. (Peer 1)
Sharing a purpose was a vital part of the process as peers expressed. One of the peers who completed two sessions with a participant explained how he had felt a bit disheartened. He explained:
I think partly it was like a day out for her, breaking the monotony, but once her family came back she had something to fill the day. When I had my stroke and was looking for help, anything I was offered I would go for it. For me I was looking for solutions to problems, I was meeting with her to work on solving problems. Her problem was loneliness, so I was the solution. (Peer 2)
One participant further explained how he was taken out of his comfort zone and was encouraged to identify an initial goal and work towards it by breaking it down into necessary steps. Although challenging, the participant could see the need for this. In his words:
So, I think [Peer] was … more goal-orientated than me. I think for me, it was useful to have that structure […] so … it was useful that he was having those. (P4)
The participant and peer agreed on a goal which involved the participant being able to take a digital photograph and follow the necessary steps to save it, download it, edit it and finally print it. The participant expressed how he could see the change as the coaching progressed:
But as I engaged and went on through the weeks … I know that I was able to …, I could absorb the information and … be able to apply it. (P4)
By Session 6 the participant was able to complete the photographic process and he expressed this had a positive impact on his confidence.
One of the peers identified the need for progression in order to ensure engagement and motivation throughout the six sessions. In his words:
The process needs to be rewarding, you need to aim for something that is likely to be achievable. Nobody works for nothing. It is important to see a progression; each meeting goes a little bit further than before, so they can see a progression. (Peer 1)
The participant considered that having a peer coach that had experienced stroke himself was, as he expressed “more of a level playing field”, however when asked to elaborate the participant said:
If it was somebody who was … hadn’t had a stroke, I think … I think I could have adapted reasonably okay … to that too. Yeah. It would have been different, not negative or positive … it would have been different. (P4)
When asked about the number of sessions the participant and the peers agreed on the fact that having a set number of sessions was beneficial because it helped plan and outline what the process was going to be like. Planning and keeping to the plan, not wanted to go too fast, was an important part of the process, as shared by the peer:
You have laid out the plan at the start and they know what the end product is going to be but sometimes they try to get there before covering the bits in between and the bits in between are what make it all work. (Peer 2)
The peers identified that although they had not experienced this difficulty, they could see how there was the potential for the stroke survivor to become attached to the peer:
It’s hard to meet somebody one to one. To meet them at a personal level and then suddenly, that is it, you are never going to see them again. This could be a problem because if you get the wrong sort of people, the ones that cling on all the time they would be phoning you all the time just for a bit of company. (Peer 1)
Peers were provided with a handbook (Additional file 2) and supported not only during the training but throughout the process via supervision and regular contact with the research team. On this, one peer said:
It was very confidence building in myself to know that there were things to turn back to, a pack of information and the fact that help is only a phone call away. In my mind, to have somebody there behind you that you can get to on the phone and say ‘look, this has happened, what can we do about it? (Peer 1)
The peer who completed the six sessions reflected that there was a dynamic process of change based on the relational aspect of peer work and the structured approach adopted in the study:
I couldn’t believe how well it had gone. The participant was really interested in what he was doing. After the first meeting, I got more confident because I got a positive response. As it was going on I was gaining more confidence and not only the participant could see an improvement in his confidence, I could see it as well. (Peer 1)
Indeed, ‘being a peer’ was viewed as a rewarding experience and included positive gains for the peer as a stroke survivor themselves:
It all came right, and it gives you that much confidence and of course, you get pleasure from it because it’s a satisfaction because you can see what you are doing is working, you know. So, it is an achievement for me in my own way that I am actually doing something that I never envisaged I would do and I am helping somebody that is appreciating the help (Peer 1).
Discussion
Overall, the results of this study have highlighted the challenges facing stroke survivors engaging with social and leisure activities post-stroke and the complexity of developing an effective peer-led coaching intervention that they will engage with. This co-design study has advanced evidence on how peer coaching can be best delivered to provide a tailored source of support for stroke survivors. The findings here reported, although contextually different, are in line with what other studies have shown. The aim of the peer support intervention proposed by Kessler et al. [Citation17] which consisted of a short visit to hospital at the time of discharge and follow up telephone conversations was to provide hope, support, and information on available resources in the community. Their results show that stroke survivors, carers, and peers reported feeling less isolated and more confident and motivated. Peer coaches also reported benefits relating to an increase in confidence and feelings of making a positive difference.
Kouwenhoven et al. [Citation39] highlighted the value of dialog in facilitating adjustment to the psychosocial challenges following stroke, including a structured guide to facilitate discussion; this example focused on training health professionals. Other programs have previously addressed the topic of lay peer work, such as the INSPIRES program [Citation26]. The lay peer-led coaching model we propose was underpinned by the notion that there is an ‘exchange’ between the stroke peer and recipient stroke survivor, which provides motivation for engagement by the stroke peer. Our results show that the relationship between the stroke peer coach and stroke survivor involves a reciprocal exchange in mutual benefits, with the peer providing coaching and hope for the stroke survivor, but also receiving satisfaction, a sense of meaning and role from having experienced the consequences of stroke. In this study, the role of the peer coach was as a facilitator and it was time-limited, although the process was centered on ensuring sustainability once the intervention was over by enabling the stroke survivor to subsequently rehearse the same step-by-step process and seek support from relevant sources should this be needed.
Our co-design study has provided further evidence on the beneficial impact that peer coaching can have on the stroke survivors’ rehabilitation journey. Although limited by a small sample our results are in line with previous studies [Citation6,Citation40] that explored the opinions and perspectives of stroke survivors, carers and peers attending hospital-based peer coaching groups. These studies revealed that the value of peers relies in the possibility of connecting and sharing that it provides and in how it promotes a sense of belonging, empowerment and improved resilience. However, the results here reported highlight a number of key messages about peer coaching interventions. This study focused on a community-based case, which utilized high levels of experiential lay knowledge and was not embedded within services. These findings echo an early study into peer coaching for carers that indicated the importance of particular experiential phases for carers of stroke survivors and the crucial aspect of “timing it right” [Citation41]. Indeed Goldfinger et al. [Citation42] reported that the overwhelming experience of hospitalization and the discharge process for stroke survivors creates barriers to recruitment for any peer intervention. Our results provide further evidence on the need to link peer support services with a community-based peer intervention that will target stroke survivors in their recovery journey post-discharge, at the time when they are dealing with changes and reinventing themselves.
This co-design study charted the complexity of not only setting up but also conducting community-based peer coaching for stroke survivors. Its innovative and theory informed approach has helped to understand and represent the complexity of stroke survivors’ experiences and the task of peer coaching. Indeed, our results describe stroke survivors’ experiences of recovery (e.g. having good/bad days, facing changes, being cutoff) which depict a dynamic and challenging area for peer intervention. This provides a platform to design and implement tailored peer coaching interventions in future trials and clinical interventions. Our findings highlight the need for further research effort focused on identifying implementation challenges and ways in which the reach and impact of these peer interventions could be maximized and sustained. Previous studies have identified [Citation17,Citation24], the peer role as challenging and time-consuming. Peers in our study provided support to a small number of stroke survivors and did not define their role in this way. However, the authors are aware that if recruitment had been higher peers could have possibly found the role more challenging and may have withdrawn from their supporting role. Hence, it is vital that future studies address the question of how these peer support programs are sustained over time.
Importantly, the co-design of the peer training and coaching intervention within this study was heavily informed by TLT and backed up by the results of the first two phases which confirmed the strong correlation between “treatment control beliefs”, “expectations”, and “personals beliefs” and engagement in social and leisure participation. Although this is the first study to do so in the context of stroke rehabilitation, previous peer mentoring studies such as Beauchamp et al. [Citation18] examined the nature of effective peer mentoring of adults with spinal cord injury drawing from TLT. They found that when peers displayed transformational leadership behaviors participants increased their motivation and confidence and overall well-being. Our results provide preliminary evidence of the successful application of TLT initially during the training of peers and subsequently during the delivery of the stroke rehabilitation peer coaching intervention. However, the use of TLT may require adaptation depending on the type of peer intervention and specific experiential phases.
Limitations
Although target recruitment numbers were reached for phase 1 and phase 2, recruitment for phase 3 was low and a number of possible reasons were identified. During the first months of recruitment for phase 1, it was clear from fieldwork to follow up those declining the intervention that the term social and leisure activities were highly problematic. This term had little meaning for lay communities and stroke survivors and was regarded as ambiguous. In order to address this issue, the research team organized a morning workshop to discuss alternative wording with recruiting staff who were in charge of carrying out the initial telephone calls. Recruitment for phase 1 improved after that and target numbers were reached. Secondly, the study identified challenges regarding the timing of the intervention. In this study, 6 months post-stroke was chosen as it coincided with a review clinic appointment that patients should receive as usual care. This decision was further informed by discussions with recruited peers who confirmed that this could potentially be the “optimum time” for stroke survivors to start reengaging in leisure and social activities. However, results show that for many participants 6 months was still early days in their recovery and for others it came too late as they had already adapted and resumed their normal daily routine to fit their new post-stroke needs. Future research should carefully address this issue and attempt as much as realistically possible to have a pragmatic tailored approach. Similarly more work needs to be done in order to identify what is the optimal time and what factors influence the shift from being a stroke survivor to becoming a peer. Finally, the way in which the initial contact between the peer coach and the stroke survivor took place appeared to be ‘daunting’ for a number of participants who, as they explained, would have liked the researcher to be present. This issue was discussed with peers during the design and peer training stages. Peers did not see the way the initial contact (telephone conversation) was arranged as a limitation but as a possible strength linked to its lay and informal set up. Further studies will need to re-think how they organize the initial contact in terms of logistics and persons present. Doing this can maximize not only the interest of stroke survivors in the offer of peer support but also the recruitment of those interested in becoming a peer.
Conclusions
This co-design study developed and delivered an innovative community-based and peer-led coaching intervention for stroke survivors. Its results have generated new evidence on how stroke survivors engage with and respond to peer coaching support. The theoretically informed prototype intervention was co-designed with peers as a “bottom-up” initiative and demonstrated a promising model of community-led peer coaching, based on co-produced theoretical frameworks, which identified key processes and mechanisms for action in implementing peer coaching in practice. Additionally, this study has identified the importance of developing a sound theoretical framework and tools to underpin and guide peer-led coaching interventions sensitive to the context of the intervention, located in the community or hospital and whether embedded within a therapeutic team setting or lay-focused. In this way, it mapped the challenges and opportunities of peer-led coaching interventions in stroke and consequently identified the need for clarity of purpose, structures, processes and support in guiding the intervention. These results have the potential to inform the development of future peer coaching interventions for stroke rehabilitation and have wider application to other conditions.
In this study, the aim was to co-design and test a community peer-led coaching intervention for stroke survivors. Further research investigating where to best embed this type of intervention and addressing recruitment barriers, and optimal timing needs to be carried out building on the theoretical advances generated from this work in order to develop a sustainable model for community-based peer coaching for stroke survivors.
Supplemental_File_3.pdf
Download PDF (1.4 MB)Supplemental_File_2.pdf
Download PDF (7 MB)Supplemental_File_1.pdf
Download PDF (227.6 KB)Acknowledgements
The authors would like to thank all peers and all stroke survivors who took part in the study for their time and important contribution.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- National Audit Office (UK). Progress in improving stroke care. 2010. Her Majesty’s Stationery Office P002346666 02/10 77240.
- World Health Organization (WHO). WHO STEPS Stroke Manual: The WHO STEPwise Approach to Stroke Surveillance. Geneva: World Health Organization; 2006.
- Daniel K, Charles DA, Wolfe MD. What are the social consequences of stroke for working-aged adults? A systematic review. Stroke. 2009;40:e431–e440.
- Lo Buono V, Corallo F, Bramanti P, et al. Coping strategies and health-related quality of life after stroke. J Health Psychol. 2017;22:16–28.
- Pollock A, St George B, Fenton M, et al. Top ten research priorities relating to life after stroke. Lancet Neurol. 2012;11:209.
- Morris R, Morris P. Participants’ experiences of hospital-based peer coaching groups for stroke patients and carers. Disabil Rehabil. 2012;34:347–354.
- Sveen U, Thommessen B, Bautz-Holter E, et al. Well-being and instrumental activities of daily living after stroke. Clin Rehabil. 2004;18:267–274.
- Hartman-Maeir A, Soroker N, Ring H, et al. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil. 2007;29:559–566.
- Carlsson GE, Moller A, Blomstrand C. Managing an everyday life of uncertainty-a qualitative study of coping in persons with mild stroke. Disabil Rehabil. 2009;31:773–782.
- Jones S, Auton M, Burton C, et al. Engaging service users in the development of stroke services: an action research study. J Clin Nurs. 2008;17:1270–1279.
- Parker CJ, Gladman JRF, Drummond AER, et al. A multicentre randomized controlled trial of leisure therapy and conventional occupational therapy after stroke. Clin Rehabil. 2001;15:42–52.
- Logan PA, Gladman JRF, Drummond AER, et al. A study of interventions and related outcomes in a randomized controlled trial of occupational therapy and leisure therapy for community stroke patients. Clin Rehabil. 2003;17:249–255.
- Desrosiers J, Noreau L, Rochette A, et al. Effect of a home leisure education program after stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1095–2000.
- Hartman-Maeir A, Eliad Y, Kizoni R, et al. Evaluation of a long-term community based rehabilitation program for adult stroke survivors. Neurorehabil. 2007;22:295–301.
- Reupert A, Maybery D. A snapshot of Australian programs to support children and adolescents whose parents have a mental illness. Psychiatr Rehabil J. 2009;33:125–132.
- Foster K, Lewis P, McCloughen A. Experiences of peer support for children and adolescents whose parents and siblings have mental health illness. J Child Adolesc Psychiatr Nurs. 2014;27:61–67.
- Kessler D, Egan M, Kubina LA. Peer support for stroke survivors: a case study. BMC Health Serv Res. 2014;14:256–265.
- Beauchamp MR, Scarlett LJ, Ruissen GR, et al. Peer mentoring of adults with spinal cord injury: a transformational leadership perspective. Disabil Rehabil. 2016;38:1884–1892.
- Greenwood N, Habibi R, Mackenzie A, et al. Peer support for carers: a qualitative investigation of the experiences of carers and peer volunteers. Am J Alzheimers Dis Other Demen. 2013;28:617–626.
- Ng L, Amatya B, Khan F. Outcomes of a peer support program in multiple sclerosis in an Australian community cohort: a prospective study. J Neurodegener Dis. 2013;2013:429171.
- Nesta (UK). Peer Support: What is it and does it work? National voices. People shaping health and social care. 2015.
- Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud. 2003;40:321–332.
- Ch'ng AM, French D, McLean N. Coping with the challenges of recovery from stroke: long term perspectives of stroke support group members. J Health Psychol. 2008;13:1136–1146.
- Hancock E. Health Recovery Social Networks: Exploring the experiences of participants in stroke recovery peer support groups. Ottawa, Canada: Stroke Recovery Canada®; 2009. http://www.marchofdimes.ca/EN/programs/src/Documents/Strokepeersupport.pdf]
- Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25:509–517.
- Beaver LG, Litowsky L, Suddes M, et al. I.N.S.P.I.R.E.S. - in-patient support program in recovery from stroke- “the voice(s) of experience”. Stroke. 2012;43:e115–e162.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211.
- Bandura A. Self-efficacy. New York: Freeman; 1997.
- Leventhal H, Diefenbach MA, Leventhal EA. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cogn Ther Res. 1992;16:143–163.
- Bass MB. Leadership and performance beyond expectations. 4th ed. New York: Free Press; 1985.
- Kelly GA. The psychology of personal constructs. 2nd ed. New York: Norton; 1955.
- Johnston M, Pollard B, Morrison V, et al. Functional limitations and survival following stroke:psychological and clinincal predictors of 3-year outcome. Int J Behav Med. 2004;11:187–196.
- Morrison V, Pollard B, Johnston M, et al. Depression and anxiety following stroke: Demographic, clinical, psychological predictors of 3-year outcome. J Psychosom Res. 2005;59:209–213.
- Clarke D, Jones F, Harris R, et al. What outcomes are associated with developing and implementing co-produced interventions in acute care settings? A rapid evidence synthesis. BMJ Open. 2017;7:e014650.
- Van Swieten J, Koudstaal P, Visser M, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–607.
- Quinn T, Langhorne P, Stott D. Barthel index for stroke trials: development, properties, and application. Stroke 2011;42:1146–1151.
- Goldberg D, Williams P. A User’s Guide to the General health Questionnaire. Windsor: NFER-Nelson; 1988.
- Charmaz K. Grounded theory: Objectivist and constructivist methods. In: Denzin N.K. & Lincoln T.S. eds. Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 2002.
- Kouwenhoven SE, Kirkevold M, Engedal K, et al. Depression in acute stroke: prevalence, dominant symptoms and associated factors. A systematic literature review. Disabil Rehabil. 2011;33:539–556.
- Simoni A, Shanks A, Balasooriya-Smeekens C. Stroke survivors and their families receive information and support on an individual basis from an online forum: descriptive analysis of a population of 2348 patients and qualitative study of a sample of participants. BMJ Open. 2016;6:e010501.
- Cameron JI, Gignac MA. “Timing It Right”: a conceptual framework for addressing the support needs of family caregivers to stroke survivors from the hospital to the home. Patient Educ Couns. 2008;70:305–314.
- Goldfinger JZ, Kronish IM, Fei K, et al. Peer education for secondary stroke prevention in inner-city minorities: design and methods of the prevent recurrence of all inner-city Strokes through Education randomized controlled trial. Contemp Clin Trials. 2012;33:1065–1073.