Abstract
Purpose: To understand children and parents’ views of the effectiveness and acceptability of intensive dysarthria therapy.
Materials and Methods: Twenty-two children with cerebral palsy and dysarthria joined a pilot RCT comparing intensive therapy and usual care. Children (n = 11) allocated to dysarthria therapy comprising three 40-minute sessions per week for six weeks and their parents (n = 11) were interviewed two weeks before and six weeks after therapy. Interviews were transcribed verbatim and analysed thematically.
Results: Analysis revealed five themes: Motivations, My new voice; The new me; I can do more; Success rooted in therapy design. Children had received little therapy for speech and were keen to improve intelligibility. Overall, therapy was viewed as effective. Participants described changes in children’s speech production, which they associated with increased speech intelligibility. Children were described as more confident following the therapy, to have more successful conversations, with a wider range of partners in more environments, thereby increasing their social participation. The programme was viewed as acceptable, despite its intensity, due to the short term commitment and wider benefits for the child. Parents valued the organised structure and individualisation of the programme and inclusion in the therapy process.
Conclusion: Families found the intervention acceptable and effective. A definitive trial of its clinical effectiveness is warranted.
Children with cerebral palsy who have dysarthria and their parents reported that intensive speech therapy focussing on creating a stronger voice and a steady speech rate increased the clarity of children’s voice and the intelligibility of their speech.
Therapy may have additional benefits for children’s self-confidence and social participation.
The programme of therapy comprising three sessions per week for six weeks was seen as manageable by families in view of the results achieved.
Implications for rehabilitation
Introduction
Approximately 20% of children with cerebral palsy have speech difficulties arising from their motor disorders [Citation1–3]. Their voice may sound weak, breathy, lacking in inflection or interrupted by pitch breaks and unexpected changes in loudness. They may also use a restricted range of speech sounds [Citation4–6]. These impairments limit children’s intelligibility and create a barrier to social participation [Citation7]. Therapy to help children control their breath support to create a stronger speech signal, in which speech sounds are more clearly differentiated, and to speak at a steady rate, so that they have time to articulate sounds and create emphasis more clearly, has recently been tested [Citation8]. Increases in children’s intelligibility [Citation9–11] and engagement in social and educational activities [Citation11] have been observed in early phase group trials, demonstrating the approach’s potential efficacy. The interventions are underpinned by motor learning principles of frequent practice for acquisition of new speech behaviours, knowledge of results, fading of feedback for retention of new skills [Citation12,Citation13]. They also use behaviour change techniques including goal-directed, graded tasks, and provision of encouragement and social support to empower children in their verbal communication and sustain motivation across the programme [Citation14,Citation15].
Two therapy programmes have been reported most widely– Lee Silverman Voice Therapy (LSVT) Loud® [Citation9] in the US and the Speech Systems Approach [Citation16] in the UK. Both programmes work on breath support by targeting speech loudness; the Speech Systems Approach also targets rate. In both approaches, therapy is delivered in three to four individual sessions per week for four to six weeks. Children are taught to produce a strong voice, first in open vowels and then in words and phrases, with practice in speech tasks that involve increasing cognitive challenge, both within and outside the clinical environment. Sessions follow a predictable format of exercises; for example, warm up, practice of individualised phrases used in daily life, practice of a particular level of speech in the complexity hierarchy, and random practice. Full details of the therapy can be found elsewhere [Citation9,Citation16].
The National Institute of Health and Clinical Excellence now recommends that this type of therapy should be offered to children with cerebral palsy in the UK who have dysarthria but use speech as their primary means of communication and who can engage with the intervention [Citation17]. However, its implementation as specified in the therapy protocols will entail a change in service provision; children with cerebral palsy in UK generally receive far less intensive intervention than the programmes demand [Citation18]. Positive results from fully powered trials of the intervention delivered in usual clinical conditions are needed to establish its clinical effectiveness. A pilot trial has recently demonstrated the feasibility of conducting a definitive trial in the NHS [Citation19], but before embarking on such a large scale study, qualitative studies of the acceptability of the intervention are required to demonstrate that the trial and any consequent offers of therapy are likely to be taken up by families. Although most of the children who took part in the studies reported to date have completed the intervention and their parents have reported perceptual changes in children’s speech patterns and use of speech to engage positively in social activities [Citation8], little is known about families’ opinions on the therapy. The aim of this study was to understand the views of children with cerebral palsy and their parents on the acceptability and effectiveness of intensive dysarthria therapy.
Methods and procedures
This study adopted a qualitative design to ascertain the views of children and parents on an intensive dysarthria therapy following the Speech Systems Approach. It was undertaken alongside a pilot randomised trial of the intervention designed to test the methods for a fully powered controlled trial of the programme [Citation19]. The UK Health Research Authority Yorkshire and The Humber – Leeds East Research Ethics Committee provided ethical approval for the study (14/YH/0058).
Participants
Participants were eligible for the study if they were aged 6-18 years old; had a diagnosis of cerebral palsy; were judged by their local speech and language therapist to have moderate to severe dysarthria; were able to understand grammatically simple instructions (no other restriction was placed on intellectual functioning); had vision correctable with spectacles; hearing loss <50 dB; attended mainstream or special school in the North of England; and had not received this type of intervention before. Participants were identified by NHS SLTs and via newsletters in parent support groups, schools and voluntary organisations supporting families of children with neurodisability (e.g. Contact, Cerebra).
Twenty-two children took part in the study. Newcastle Clinical Trials Unit randomly allocated participants a one-to-one basis to either individual intensive dysarthria therapy following the Speech Systems Approach or treatment as usual.
Children allocated to the intensive dysarthria group included five boys and six girls whose ages ranged from 6 to 13 years (mean age 8.8 years, SD 2.10). Children lived at home with their parent(s). Five children attended special schools, others were in mainstream education. Six had predominantly spastic-type motor disorder and five had dyskinetic type. All children used speech as their main means of communication; two also used voice output communication aids to supplement their speech when conversing with people outside their immediate family. Children’s average length of phrases in connected speech (e.g. speaking in conversation, describing pictures etc) ranged from 1.8 to 7.9 words (mean 5.2; SD 1.9 words). Unfamiliar listeners correctly understood a mean of 37.2% of children’s connected speech without contextual cues when measured from audio recordings taken before the therapy (SD 33.8%; range 1.8–98.1%). Scores on the Test of Reception of Grammar [Citation20] suggested that some children had typically developing language comprehension and others severe delays in this domain (mean standard score 87.3; SD 22.5; age equivalent range 4–12 years). All but one child was receiving some input from SLT services at school, although the amount of therapy and goals differed. None was receiving therapy to improve their speech.
Procedure
Children allocated to intensive dysarthria therapy received three 40 minute therapy sessions per week for six weeks, from research speech and language therapists via Skype. Three research speech and language therapists worked on the study and were trained in the therapy protocol by the corresponding author. The therapists worked on different days of the week, and all children received therapy from two therapists. Intervention followed the Speech Systems Approach described in Pennington et al [Citation10,Citation11] and Parker, Kelly and Pennington [Citation16]. At the start of the programme, the speech and language therapist briefly explained to the child how speaking louder and at a steady rate can make speech clearer and easier to understand, and that loudness is achieved with ‘more breath’. The therapist modelled clear speech at a slightly louder than conversational level and provided individualised prompts and feedback to help children sustain a loud, clear voice and to speak at a steady rate. Each child named their target voice (e.g. my ‘strong’ voice) and this cue was used to prompt children to use their target speech pattern in a hierarchical set of speech exercises from articulatory simple single words (e.g. ‘no’), through increasingly more complex words (e.g. ‘splat’, ‘butterfly’) and phrases, and in activities with increasing cognitive load (repetition, picture description, question-answer, conversation, verbal memory tasks). Children allocated to treatment as usual received their regular services from their NHS speech and language therapist. None of the children were in receipt of independent therapy provision at the time of the trial.
All children allocated to intensive dysarthria therapy and their parents (nine mothers, two fathers) were interviewed two weeks before therapy started and six weeks after its completion. Interviews asked about participants’ experiences relating to the design of the trial, acceptability of the intervention, its effects and its delivery via Skype. Interviews were semi-structured and followed a topic guide (Supplementary Material 1 shows the post therapy topic guide). Here we report participants’ expectations of therapy programme design and views of the acceptability and effectiveness of the intensive dysarthria therapy programme. Findings regarding trial design and internet (Skype) delivery of the programme are reported elsewhere [Citation19].
Pre-therapy interviews were conducted in participants’ homes. Post therapy interviews took place at home, school or over the telephone or Skype, at participants’ convenience. Interviews were audio-recorded and took 35 minutes (range 15–45 minutes) for children and 45–50 minutes for parents. Parents provided written consent, children gave written or verbal assent. All interviews were conducted by a researcher who was not involved in the development or delivery of therapy.
Analysis
Interviews were transcribed verbatim and checked for errors against audio tapes by the interviewer. Participants were assigned codes to indicate whether they were a child or mother/father and a number to indicate the family pairing (C1, 6 YRS; MLU = 5, M1, F1). Interview data were analysed using thematic analysis methods [Citation21]. Two researchers repeatedly read and compared interview transcripts to ensure familiarity with the data and made notes of any initial ideas, interesting points or patterns. Codes were developed inductively through analysis of the data and compared across transcripts [Citation22]. Data extracts relevant to each code were collated and visual representations were developed to explore relationships between codes and to group codes into over-arching themes and sub-themes. Main themes and sub-themes were reviewed to ensure the data cohered meaningfully whilst maintaining identifiable distinctions between themes. Themes were then finalised by defining and naming them ensuring the “essence” of each was captured. The development of themes, codes and application of codes to text was verified with KB and LP through discussion of code examples and potential themes that emerged. The team included speech and language therapists and social scientists. Individual researchers’ experience and knowledge was acknowledged in the discussion of themes, codes and text to improve reflexivity [Citation23]. Disagreements were resolved through further review of the dataset and explanation of thinking behind particular coding or themes.
Results
Five themes were developed from the interviews. One theme related to the reasons that families decided to take part in the study, the remaining four related to the perceived effects and acceptability of the therapy programme. Each theme is presented below with quotes from participants. The age of the child and their mean length of utterance in whole words are provided to aid contextualisation.
Being Understood and Motivations to Take Part
In pre-therapy interviews, children and their parents talked about current speech patterns and described how intelligibility limitations restricted children’s social participation. Children reported that they were frequently not understood in daily conversation and continual requests for repetition caused them frustration, annoyance and ‘anger’ (C5 (7 yrs; MLU = 5)). Children described how they restricted their spoken communication to avoid conversation with unfamiliar people and individuals who had not understood them in the past. They also limited the amount they spoke in environments with higher levels of background noise, such as classrooms, playgrounds, and shops.
I just talk to the people who understand me. C1 (6 yrs; MLU = 5)
That’s the only person, them are the only person in the family who understands me because they have had me from the beginning. C9 (9 yrs; MLU = 7)
There are plenty of times I don’t understand as well, which drives us all round the bend doesn’t it, when I don’t get it or Dad doesn’t get it? M5 (7 yrs; MLU = 5)
It makes me angry. C5 (7 yrs; MLU = 5)
People ask me to repeat what I say over and over again….I get annoyed. C1 (6 yrs; MLU = 5)
If they don’t understand her they just look at me. M11 (7 yrs; MLU = 8)
Some parents attributed anxiety and self-esteem issues to intelligibility difficulties and were seeking help for their children to address both intelligibility and self-confidence.
[outcomes of therapy] To target the areas he struggles on. M10 (13 yrs; MLU = 8)
His confidence, isn’t it? ‘Confident’ is the main, key word, if you give him confidence. F10 (13 yrs; MLU = 8)
He’s very anxious in class and one of the big reasons is that when he needs help he is worried that he will not be seen or heard. M5 (7 yrs; MLU = 5)
It’s hard for her to maintain friendships sometimes because she doesn’t say a lot. I would like it to increase her confidence….I would love her not to do that anymore: to look at me to speak for her. M7 (10yrs; MLU = 6)
Most parents reported infrequent contact with their child’s speech and language therapist, as services were provided at school, and that their child had historically received little input focussing on speech. Some felt that professionals had given up on their child’s speech.
The comment was made [by previous therapist] “Well really her speech is what it is and that’s how it will remain.” Which to me, as a mum, is very much, well actually you don’t know until you give it a go. M4 (7yrs; MLU = 4)
Given the high value parents placed on intelligibility and self-confidence in communication, families were willing to ‘just make the time’ (M7 (10 yrs; MLU = 6)) for an intensive programme focussed on speech production. They recognised that to acquire and maintain new speech behaviours children would need to practice. However, some were concerned that their child would lose motivation if they did not see the benefit or the programme was not tailored to their interests.
I hope she stays motivated for the whole six weeks period M6 (11yrs; MLU = 3)
Things have to be at the right level to be motivating, don’t they? M7 (10 yrs; MLU = 6)
In summary, the factors motivating families to take part in the study were the possibilities for children to be better understood in their daily lives and to increase their self-confidence. Families recognised that to be successful, therapy would need to be designed to keep children’s interest and motivation throughout an intensive programme. In post-therapy interviews children and their parents spoke about the impacts of the therapy and their experiences of completing the programme. We developed four main overarching themes: ‘My new voice’; ‘The new me’; ‘I can do more’; ‘Success rooted in therapy design’.
My new voice
Children and their parents talked about how the child’s speech had changed following the therapy, using terms relating directly to objectives concerning loudness and rate which showed understanding of the consequences of changing their speech production.
I feel like I’ve got more breath so … I’ve got more words to say. C1 (6 yrs; MLU = 5)
I used to talk in a quiet voice but now I talk in a strong one like this. C5 (7 yrs; MLU = 5)
[friend] can hear me when I go slowly but when I go fast she can’t hear me. C1 (6 yrs; MLU = 5)
Additionally, some parents reported changes in speech function, such as articulation, that were not directly targeted in therapy but should theoretically result from increased control over breath support and steady speech rate.
Yes, he’s been doing, sort of, being able to get more, better words and better pronunciation. M8 (10 yrs; MLU = 6)
Children used their new voice often and when needed, rather than constantly, indicating their ability to self-monitor in conversation and repair conversation breakdowns, with potentially new awareness of the listener’s perceptions.
She will be in mid conversation and she will stop. She will go, “You are not getting that. I need to say it again. But I need to take my time. I need to have a breath. I need to say it.” M6 (11 yrs; MLU = 3)
When she has friends over and I hear them chatting in the car and she’s using a different voice to the one she uses at home…it’s really nice to know that she knows what to do. M7 (10 yrs; MLU = 6)
However, speech changes were not consistent across all children. One child reported little change, saying she found it ‘easier’ to talk to people but that her voice was ‘the same’ post-therapy (C6 (11 yrs; MLU = 3)). Changes were, however, apparent to her mother, who noticed that listeners were understanding her frequently and who judged that her ‘voice has improved’ (M6 (11yrs MLU = 3)). Some parents saw incremental but not large changes, and some only noticed the magnitude of change when they were pointed out by people outside the family.
I think he's benefited in the fact that he talks louder and it does become a lot clearer when he's louder. Not massively, completely changed, but I can notice he is a little bit clearer. M10 (11 yrs; MLU = 8)
A few weeks ago I had an occupational therapist in and he was chatting away to her, and I was sat there listening, and he was so clear, and you know when you think, wow. It really was clear, that’s when I really noticed the difference. M3 (8 yrs; MLU = 4)
When we went round she was like, “Wow [child].” Things like that, you don’t realize how much he has changed until someone who hasn’t seen him for a while says something. M5 (7 yrs; MLU = 5)
The new me
In addition to improved intelligibility, children’s comments that the therapy was associated with increases in self-esteem and confidence and changes in their sense of self. Post therapy, they saw themselves as more successful speakers.
How do you feel when you are using your new talking? Interviewer
Amazing. C5 (7 yrs; MLU = 5)
I think it’s amazing what you’ve done because it’s like I’m a different person. C7 (10 yrs; MLU = 6)
My friends hadn’t used to hear me and now they can hear me. C9 (9 yrs; MLU = 7)
How did that make you feel? Interviewer
Happy. C9 (9 yrs; MLU = 7)
As expected from parents’ discussion in pre-therapy interviews, changes in children’s self-perception and confidence were highly prized.
That’s awful to think that she doesn’t [didn’t] feel confident enough to speak like that in front of class, and now that she does that’s just a great outcome, I’m really thrilled with that. M7 (10 yrs; MLU = 6)
How do you feel when you are using your new talking? Interviewer
(pauses) Happy. C4 (7 yrs; MLU = 4)
You join in more don’t you? M4 (7 yrs; MLU = 4)
Yes. C4 (7 yrs; MLU = 4)
I can do more
Children’s new voice, their altered sense of self, increased confidence in their own abilities and ability to self-regulate in conversation appeared to feed into increased willingness to get involved in interactions and the success of those interactions. Descriptions of the effects of therapy on communicative participation were prevalent in discussion.
Children and their parents spoke about talking more frequently and for longer after the therapy.
Talking more often? Interviewer
A lot more. C1 (6 yrs; MLU = 5)
At the start of the six-week study if you’d have given [child] a picture and asked her to give you some detail about it, it would have been very, very minimal detail. Whereas by the end of it she was looking at pictures and she was actively looking for more information…That’s been a massive gap for her, particularly for about the last 18 months. M4 (7 yrs; MLU = 4)
In conversations across different environments, including those that had been avoided pre-therapy, children were more likely to be perceived correctly
When I didn’t start this I was like “[sister], do you want to play at parties?” and she was like, “What? I can’t understand you”…I’m telling her [post-therapy] what I did at school and she can hear me much better.” C9 (9 yrs; MLU = 7)
[We used to say] “Ask us later.” We don’t need to do that so much now because we will actually ask because he knows there is a much better chance he is going to get it across. M5 (7yrs; MLU = 5)
If you go to a big party and it’s quite loud because there are a lot of people…There is loud music and all that. I used it [new voice] then. C1 (6 yrs; MLU = 5)
Increased intelligibility allowed children to carry out conversations without support, which they were not necessarily able to do before therapy, and which afforded them greater independence. For example, the quotation below shows how a child previously relied on parents to interpret their speech for strangers, such shop assistants.
When we have been in the shops and things and [child] has said, “Hello” or “Thank you” it hasn’t taken for us to then have to repeat after [child] “Hello”, “Thank you”. We went to [shop] and I can’t think what she bought but she wanted to pay for it and she did everything. M6 (11 yrs; MLU = 3)
She ordered her own food and the waiter was Spanish but understood everything that she’s said. And that was quite a big thing; she’s always had the confidence to do that and she’s always ordered her own things, but she hasn’t always been understood and she was this time. M7 (10 yrs; MLU = 6)
Generalisation of children’s new voice occurred in social settings, as described above, but also where children may be under more pressure to perform. Increased involvement in educational activities was highlighted.
I’ll put my hand up more than I used to.… I [used to get] get really nervous when I’m up at the front…Talking to the class, and I haven’t done that since I’ve been doing speech therapy. C7 (10 yrs; MLU = 6)
Her expression has grown with her reading [aloud] as well. I spoke to her teaching assistant this morning because I’ve got a meeting with her this afternoon and she was saying that she’s definitely noticed a difference in school…You’re [child] better at explaining things, I think. M4 (7yrs; MLU = 4)
Success Rooted in Therapy Design
Parents’ and children’s discussion about the acceptability of the programme appeared to be related to its outcomes, whether these were the reported changes in speech or the increases in children’s participation and confidence described and showcased above.
I think it’s been definitely worthwhile, I think it works on a lot of levels. F1 (6yrs; MLU = 5)
Hearing how [child]’s speech has developed and the skills she’s gained, it’s all completely worth it. M7 (10yrs; MLU = 6)
We've not had much input from speech, really since birth. I know it's one of those areas that are very short-staffed and there probably are other children out there that need it more than him, and so forth. It was always that he was just left to get on with it, really. By having this, it's really opened our eyes as to what's available. I think it's great. I think it's brilliant. M10 (13 yrs; MLU = 8)
Individual features of the therapy design also seemed to contribute to its perceived acceptability. As expected given its frequency and duration, the programme was viewed as intensive and demanding, both physically: “I’m out of breath…It was hard work” (C5 (7 yrs; MLU = 5)) and logistically. Although clinicians tried to accommodate family commitments when scheduling appointments, some families did forgo activities and move mealtimes to attend sessions. This was described as ‘short term pain’ (M7 (10yrs; MLU = 6) that was manageable for the six week therapy block.
It does get towards the end a bit hard but you know that you’re coming to the end of this, that teatime will get back to how it should be…but it was a short term thing, so you know that the end is in sight. M3 (8 yrs; MLU = 4)
However, these demands were offset by features that were viewed favourably by families, such as the planned, programmatic nature of the therapy which was being ‘tried and tested’.
Very organised…everything was ready…so there was the consistency…I think they’ve maybe spent a lot of time thinking and planning. M3 (8yrs; MLU = 4)
Parents also described how the therapy incorporated individualised, incremental challenges for their child and saw this as a key element in maintaining drive, tapping into children’s internal motivations, such as an internal desire to perform and succeed. The graded speech tasks, which were accompanied by feedback on results and praise from therapists, seemed to remain enjoyable for children, leading to a sense of achievement within sessions.
You liked all the competitions with yourself didn’t you? To try and get nine out of ten or ten out of ten. M5 (7 yrs; MLU = 5)
Yes. C5 (7 yrs; MLU = 5)
That was his thing, he wants 10 out of 10, so they did work towards that…So yes, it’s a lot of fun doing it. M3 (8yrs; MLU = 4)
[Therapist said] “Fantastic. Fantastic.” Which to me is what kids need to hear. M6 (11 yrs; MLU = 3)
Parents also reported that the supportive, collaborative working between children and therapists to set goals and individualise exercises to feature children’s areas of interest (e.g. including pictures of a child’s favourite pastimes in picture naming tasks) contributed to children feeling enjoyment rather than anxiety in challenging tasks. Therapists’ understanding of the child, their personality, and individualised efforts to increase their compliance, enjoyment and motivation for therapy was especially valued.
You always enjoyed it and you always worked hard. I think they tried to make it fun for you, didn’t they? M3 (8yrs; MLU = 4)
They were fun weren't they? They made it really good fun. M4 (7 yrs; MLU = 4)
He enjoyed doing it so it wasn't a chore or anything. M8 (10 yrs; MLU = 6)
In addition to describing features that promoted their child’s engagement in therapy, parents also discussed their own involvement. Because therapy took place at home, parents were able to observe sessions, to see the techniques therapists used and children’s responses. This helped them to understand how techniques might work, to learn how to prompt their child to use their new voice and to foster the generalisation of the new voice outside the therapy sessions.
I think if the parents don’t see it I don’t think it can be nearly as effective in the home with the family, definitely not. If you haven’t seen it happen I don’t see how you can apply it and help them (children) apply it. M5 (7yrs; MLU = 5)
It’s been really interesting and I think because she’s been doing it at home and I could hear what’s been going on whereas when it was at school it was just when it was at school it was just a few notes written in her diary and it’s not the same…so I kind of know what I need to be saying to [child’s name] to prompt her. M7 (10 yrs; MLU = 6)
Parents also commented that the therapy aim of equipping their children with strategies to use to control their speech, rather trying to ‘change’ underlying impairment (M7 (10 yrs; MLU = 6)) was a key to effectiveness, which had not necessarily been tried in previous interventions.
It’s made me realize a massive thing that I hadn’t realized, that perhaps we’re focusing on the wrong things with [child]’s speech that nobody’s ever picked up or mentioned before, so it’s been massively worth it…Nobody’s ever said about just slowing her speech down…and it made her so much clearer and we used it at home…It has made such a difference and it’s just like a Eureka moment. M11 (7yrs; MLU = 8)
In the post-therapy interview parents were asked for recommendations for change to the intervention or its delivery to improve its acceptability or effectiveness. Some parents suggested that families may be apprehensive about investing time and emotion into an intensive intervention that may not have any effect and that the opportunity to discuss the process and potential outcomes of the programme could potentially allay such concerns.
I think that if I’d have spoken to a family that had already reaped the rewards that we’ve already reaped then I think I would have felt easier about going into it. M4 (7yrs; MLU = 4)
Parents also suggested that having some sessions at school could help staff to encourage children to use their new voice parents and that small amounts of continued support post-therapy may facilitate children’s retention of their new skills.
Maybe out of three sessions, have one at school and two at home…so that school get an insight as well. M10 (13 yrs; MLU = 8)
It would have been nice to maybe have a couple of weeks of once a week therapy [after the block] and then maybe after another couple of weeks maybe after another couple of weeks maybe touching base with [research therapist]. M4 (7yrs; MLU = 4)
Discussion
This study has five main findings: intelligible speech was highly prized by children and parents, but not currently prioritised by professionals; families viewed the therapy as effective in helping children to produce clearer speech, which was more understandable in daily conversations; children became more confident and viewed themselves as more successful speakers; children took part in more conversations with more people in a wider range of social contexts; and although the therapy was intensive and sometimes difficult to schedule and tiring for children it was viewed as worth the investment.
The current lack of input focussing on speech that families described in this study is not unexpected. Until recently there was no evidence for speech interventions for children with dysarthria [Citation8], and evidence-based therapy focussing on individual speech sounds (articulation and phonology), may not be appropriate for children with motor disorders [Citation8]. A recent survey of UK speech and language therapy practice indicated that about 60% of SLTs do provide intervention for speech, but intervention may not be frequent, does not follow a structured programme and may be carried out by other members of staff (e.g. teaching assistants) as part of a consultative model of speech and language therapy provision [Citation18]. Given the nature of the therapy provision, it is possible that some of the children were receiving some intervention for speech, but perhaps not in a structured programme valued by their parents.
The changes in sound of children’s speech that families described, of louder speech, more perceptible speech sounds, and longer utterances, are those expected from interventions targeting breath support and speech rate [Citation24,Citation25]. Louder speech is created by increasing the pressure of exhaled air passing through the vibrating vocal folds, creating greater aero-acoustic energy. This increased energy also leads to firmer closure of contacts further up the vocal tract, for example generating hard contact between the tongue tip and hard palate to achieve plosive sounds ‘t’ and ‘d’ [Citation26]. Thus, sounds that are articulated but not heard in quiet speech become perceptible in louder speech. Speaking at a steady rate should allow children to move from one articulatory placement to another, increasing precision [Citation26]. Together, these actions should lead to clearer, more intelligible speech. As louder speech is generated from increased breath support, the greater air volumes could also support longer utterances. The changes reported here are the perceptual correlates of the change in acoustic measures found in previous studies [Citation9,Citation27–29]. The reports of children generalizing their new speech patterns to conversation outside the therapy environment and their articulation of strategies also suggest that motor learning has taken place and new behaviours can be produced when needed [Citation13].
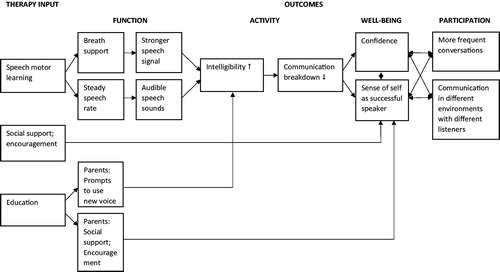
Louder, clearer speech should be easier for listeners to perceive and the reports of increased intelligibility described by families support previous objective measures of intelligibility [Citation10,Citation11]. Children’s more frequent and successful conversations at home, school and social settings may also suggest that intelligibility facilitates communicative participation. However, not all families reported this chain of effects. Some children, for example C6 (11 yrs; MLU = 3), felt that their speech had not changed or had changed little. Nevertheless, C6’s parents described increases in her intelligibility in real life exchanges and greater communicative participation. Increases in intelligibility and participation without change in speech function have been observed in previous studies [Citation11,Citation27]. This lack of coupling between speech impairment and intelligibility suggests that the mechanism of change is more complex than an increase in speech function engendering increased intelligibility prompting increased participation, and that some other mechanism is at work. Parents in the current study talked about children’s increased confidence following the intervention. Children also seemed to view themselves as more successful speakers. Having changed their beliefs about their capabilities they may have been more willing to speak to a wider range of listeners in a wider range of environments. Perhaps for some children, encouragement and social support from the therapists, who they had come to trust, and/or the focus on speech in therapy, with the expectation that it will improve, empowered them to take part in conversations and increase their social participation [Citation14,Citation30,Citation31]. It is also possible that children were better understood in conversation because they were more confident to speak for longer and to use nonverbal cues, giving more information to help get their messages across. This would represent a change in comprehensibility (extent to which messages are understood in context using all cues available), rather than intelligibility which is defined as the ability to convey information using the speech signal alone (See ) [Citation32].
Further research is needed to test the mechanisms of change for individuals in this complex intervention; to ascertain the magnitude of change in speech impairment, intelligibility, communicative participation and mental well-being at an individual level; and to determine the size of change that is deemed clinically significant in each of these domains [Citation33]. We would argue, however, that even if speech impairment changed little, but comprehensibility, well-being and participation significantly improved, the intervention should be viewed as effective. The views expressed by children and parents support previous research showing the severe detrimental impact of communication difficulties on mental well-being and participation and long term outcomes and quality of life [Citation7,Citation34–38]. Conversely, improvements in function, without increases successful communicative participation, would be insufficient outcomes for undertaking such an intensive therapy.
In addition to examining the perceived effects of the therapy, we also aimed to determine its acceptability. Since the interviews were undertaken, Sekhon and colleagues have proposed that acceptability of healthcare interventions is a multi-factorial construct [Citation39]. In Sekhon’s model, three these factors refer to prospective or anticipated acceptability. They cover how participants feel about the intervention (affective attitude), the extent to which the intervention accords with the participant’s personal values (ethicality) and the burden the intervention will place on the participant. Our pretherapy interviews indicated that all parents were keen to address their child’s difficulties in intelligibility and communicative participation and some were also troubled by children’s lack of confidence in their communication. As the intervention aimed to address each of these areas, families in this study probably started with a positive disposition to the intervention. However, intensive nature of the therapy was seen as a substantial commitment (burden) [Citation39]. Some families also expressed concerns about their children being able to maintain motivation throughout the therapy and suggested that discussions with other parents could have made the decision about whether to participate more easily. Thus, although the programme may fit with families’ views of what therapy should address, anticipated burden and concerns about lack of fit with children’s needs may present risks to prospective acceptability.
Four of the constructs suggested by Sekhon et al refer to retrospective acceptability [Citation39]. These comprise how well participants understand the components of the intervention and how it works (coherence), the degree to which valued and enjoyed activities must be given up to undertake the intervention (opportunity costs), the degree to which the intervention meet its goal (perceived effectiveness), and participants’ confidence in being able to comply with the intervention tasks (self efficacy). Each of these constructs was evident in our data and discussion with parents and children following intervention completion suggested high levels of retrospective acceptability. Similar to parents whose children attended LSVT in the USA [Citation28], the opportunity costs of reorganising family activities and forgoing some social activities during the six weeks of intervention were seen as manageable because of the defined, short term nature of the programme. Perceived effectiveness was high, as seen in participants’ talk of changes to intelligibility, confidence and participation. Parents had clearly monitored the intervention’s benefits, sometimes using responses of others outside the family to make these evaluations [Citation40]. Similarly, self efficacy was evident in description of how children used the techniques taught in therapy in their daily lives and in parents’ discussion of how they were able to prompt their children to use techniques if they were not understood. Parents also spoke favourably about being involved in therapy and seemed to view themselves as effective in their role in helping to generalise speech behaviours, showing their buy-in to the techniques and the potential of the therapy to empower parents to support their children’s communication development [Citation31,Citation39,Citation41,Citation42].
Substantial discussion focussed on the face validity/coherence of the therapy programme [Citation39,Citation40]. Parents talked about its difference from other therapies, which were not always seen as effective; were able to articulate the aims and objectives of the therapy techniques (e.g. breath support enabling audible production of speech sounds) and what they needed to do to use the techniques (e.g. speak slowly); and understood the potential benefits of the techniques. Similar to a recent review of parents’ views of allied health interventions, parents in our study gave credence to the planned, programmatic nature of the intervention [Citation43]. They also valued its individualisation and grading of tasks, provision of feedback with knowledge of results, use of praise and encouragement, and social support. They attributed these features to treatment success, particularly in motivating their child to stick with the programme to master new behaviours and in empowering their children to become more successful communicators. Motivation and empowerment are key features of successful therapy interventions [Citation31], and our results here provide support for the motor learning and behaviour change theories that underpin the Speech Systems Approach [Citation12–14,Citation30].
Overall, it seemed that the therapists, parents and children had worked together successfully to implement the therapy and its techniques and that families viewed the intervention as acceptable. As the families who participated in the current study might represent a very motivated group, further research is needed to investigate its acceptability to the wider population of families of children with dysarthria. Implementation of the programme should pay attention to the prospective acceptability of the programme, offer families the opportunity to discuss the programme with previous participants and be clear about the burden the therapy entails.
A strength of this study is that both children and their parents were interviewed before and after the intervention, ensuring we heard from the people who received the therapy – the children – and those supporting them. The study also included two fathers, whose voices are rarely heard in childhood disability research. Families were recruited from across the north of England and received speech and language therapy services from different providers, so the findings are not attributable or restricted to a single environment. However, we recruited a small number of families who may be particularly motivated to work on speech. Other families, with different circumstances and who place less priority on speech, may have different views of the intervention. Families were interviewed six weeks post-therapy; it is unknown if views on acceptability and effectiveness may change with greater distance from the therapy.
Conclusions
Intensive dysarthria therapy following a Speech Systems Approach was viewed as effective and acceptable by the group of highly motivated families who took part in this study. The benefits to communicative participation that families described may be achieved through a number of mechanisms. A fully powered randomised controlled trial is now required to test if the intervention can improve the communicative participation and well-being of this group of young people, who are at particular risk of poor health and social outcomes, when it is delivered by local services.
DR_Supplementary_material_Acceptability_paper.docx
Download MS Word (19.5 KB)Acknowledgements
We thank the families for taking part in the study and sharing their views.
Disclosure statement
The authors report no conflicts of interest. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Additional information
Funding
References
- Nordberg A, Miniscalco C, Lohmander A, et al. Speech problems affect more than one in two children with cerebral palsy: Swedish population-based study. Acta Paediatrica, Int J Paediatr. 2013;102(2):161–166.
- Parkes J, Hill N, Platt MJ, et al. Oromotor dysfunction and communication impairments in children with cerebral palsy: a register study. Dev Med Child Neurol. 2010;52(12):1113–1119.
- Australian Cerebral Palsy Register Group. Report of the Australian Cerebral Palsy Register 2016. Birth years 1993–2009. Sydney, Australia: Cerebral Palsy Alliance and CP Register; 2016.
- Ansel BM, Kent RD. Acoustic-phonetic contrasts and intelligibility in the dysarthria associated with mixed cerebral palsy. J Speech Hear Res. 1992;35(2):296–308.
- Workinger MS, Kent RD. Perceptual analysis of the dysarthrias in children with athetoid and spastic cerebral palsy. In: Moore CA, Yorkston KM, Beukelman DR, editors. Dysarthria and apraxia of speech: perspectives on management. Baltimore: Paul Brookes; 1991. p. 109–126.
- Love RJ. Childhood motor speech disability. 2nd ed. Boston: Allyn & Bacon; 2000.
- Fauconnier J, Dickinson HO, Beckung E, et al. Participation in life situations of 8–12 year old children with cerebral palsy: cross sectional European study. BMJ. 2009;338:1458–1471.
- Pennington L, Parker NK, Kelly H, et al. Speech therapy for children with dysarthria acquired before three years of age. Cochrane Database Syst Rev. 2016;(7):CD006937.
- Boliek C, Fox C. Therapeutic effects of intensive voice treatment (LSVT LOUD®) for children with spastic cerebral palsy and dysarthria: a phase I treatment validation study. Int J Speech-Language Pathol. 2017;19(6):601–615.
- Pennington L, Miller N, Robson S, et al. Intensive speech and language therapy for older children with cerebral palsy: a systems approach. Dev Med Child Neurol. 2010;52(4):337–344.
- Pennington L, Roelant E, Thompson V, et al. Intensive dysarthria therapy for younger children with cerebral palsy. Dev Med Child Neurol. 2013;55:464–471.
- Maas E, Robin DA, H A, et al. Principles of motor learning in treatment of motor speech disorders. Am J Speech Lang Pathol. 2008;17:277–298.
- Schmidt RA, Lee TD. Motor control and learning: a behavioral emphasis. 4th ed. Leeds: Human Kinetics Europe Ltd; 2005.
- Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Quality Safety Health Care. 2005;14:26–33.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
- Parker N, Kelly H, Pennington L. Speech systems approach for dysarthria in cerebral palsy. In: Dodd B and Morgan A, editors. Intervention case studies of child speech impairment. Guildford, UK: J & R Press; 2017. p. 95–114.
- NICE. Cerebral palsy in under 25s: assessment and management. NICE guideline [NG62]. London: National Institute of Health and Care Excellence; 2017.
- Watson RM, Pennington L. Assessment and management of the communication difficulties of children with cerebral palsy: a UK survey of SLT practice. Int J Lang Commun Disord. 2015;50:241–259.
- Pennington L, Stamp E, Smith J, et al. Internet delivery of intensive speech and language therapy for children with cerebral palsy: a feasibility randomised controlled trial. BMJ Open. 2018; http://dx.doi.org/10.1136/bmjopen-2018-024233.
- Bishop DV. Test of reception of grammar 2. Oxford: Pearson Assessment; 2003.
- Braun V, Clark V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
- Tuckett AG. Applying thematic analysis theory to practice: a researcher's experience. Contemp Nurse. 2005;19:75–87.
- Koch T, Harrington A. Reconceptualizing rigour: the case for reflexivity. J Adv Nurs. 1998;28:882–890.
- Fant G. Acoustic theory of speech production. The Hague, Netherlands: Mouton; 1960.
- Kent RD, Read C. The acoustic analysis of speech. San Diego, CA: Singular Publishing Group; 1992.
- Yorkston KM, Hakel M, Beukelman DR, et al. Evidence for effectiveness of treatment of loudness, rate or prosody in dysarthria: a systematic review. J Med Speech-Lang Pathol. 2007;15:11–36.
- Pennington L, Lombardo E, Steen N, et al. Acoustic changes in the speech of children with cerebral palsy following an intensive program of dysarthria therapy. Int J Lang Commun Disord. 2018;53:182–195.
- Fox C, Boliek C. Intensive voice treatment (LSVT LOUD) for children with spastic cerebral palsy and dysarthria. J Speech Lang Hear Res. 2012;55:930–945.
- Boliek C, Fox C. Individual and environmental contributions to treatment outcomes following a neuroplasticity-principled speech treatment (LSVT LOUD) in children with dysarthria secondary to cerebral palsy: a case study review. Int J Speech-Lang Pathol. 2014;16:372–385.
- Michie S, Johnston MV, Francis J, et al. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57:660–680.
- Lord C, Rapley T, Marcroft C, et al. Determinants of parent-delivered therapy interventions in children with cerebral palsy: a qualitative synthesis and checklist. Child: Care Health Dev. 2018;44:659–669.
- Hustad KC. The relationship between listener comprehension and intelligibility scores for speakers with dysarthria. J Speech Lang Hear Res. 2008;51:562–573.
- Craig P, Dieppe P, MacIntyre S, et al. Developing and evaluating complex interventions: new guidance. London: Medical Research Council; 2008.
- Majnemer A, Shevell M, M L, et al. Participation and enjoyment of leisure activities in school-aged children with cerebral palsy. Dev Med Child Neurol. 2008;50:751–758.
- Geisthardt CL, Brotherson MJ, Cook CC. Friendships of children with disabilities in the home environment. Educ Train Mental Retard Dev Disabil. 2002;37:235–252.
- Mei C, Reilly S, Reddihough D, et al. Activities and participation of children with cerebral palsy: parent perspectives. Disabil Rehabil. 2015;37:2164–2173.
- Lindsay S. Child and youth experiences and perspectives of cerebral palsy: a qualitative systematic review. Child: Care Health Dev. 2016;42:153–175.
- Michelsen S, Uldall P, Kejs AMT, et al. Education and employment prospects in cerebral palsy. Dev Med Child Neurol. 2005;47:511–517.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17:88.
- Murray E, Treweek S, Pope C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med. 2010;8:63.
- Dirks T, Hadders-Algra M. The role of the family in intervention of infants at high risk of cerebral palsy: a systematic analysis. Dev Med Child Neurol. 2017;53:62–67.
- Zimmerman MA, Israel BA, Schulz A, et al. Further explorations in empowerment theory: an empirical analysis of empowerment theory. Am J Community Psychol. 1992;20:707–727.
- Beresford B, Clarke S, Maddison J. Therapy interventions for children with neurodisabilities: a qualitative scoping study. Health Technol Assess. 2018;22:1.