?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background and purpose: The increase in use of everyday information and communication technologies can lead to the need for health professionals to incorporate technology use competencies in practice. Information and communication technologies has the potential to improve participation in daily life among people with disability. The aim was to review and describe evidence of the use of information and communication technology, including mobile technology, for improving participation in everyday life. A secondary aim was to describe how study outcomes were related to participation.
Materials and methods: A scoping review methodology was used to identify studies through databases as MEDLINE, CINAHL, Cochrane Library. Thereafter, the studies were screened and assessed for inclusion.
Results: Eleven studies were included. The most commonly used technology were videoconferencing and the telephone. Ten of the 11 studies reported a change in participation in everyday life. Participation was mainly described as involvement in a life situation or related to activities of daily living.
Conclusion: Delivering an intervention to improve participation through information and communication technology can be a valid option in rehabilitation. There is a need to measure and describe the intervention and its outcomes in relation to a definition of participation in future studies.
The use of an information and communication technology application seems to be as good as the face-to-face intervention.
There is a need for defining the concept of participation related to outcome measures in future studies.
IMPLICATIONS FOR REHABILITATION
Introduction
Since 2005, the World Health Organization has urged member states, “to develop the infrastructure for information and communication technologies (ICT) for health as deemed appropriate to promote equitable, affordable, and universal access to their benefits, and to continue to work with information and telecommunication agencies and other partners in order to reduce costs and make eHealth successful” [Citation1, p. 109]. The use of ICT can have great potential to support rehabilitation and it is consequently of interest to explore evidence as well as benefits and implications for clinical practice. There are many terms used to describe the use of ICT to support healthcare. These terms are often used interchangeably, which can contribute to misunderstanding or misconceptions. Terms include: eHealth, mHealth, telehealth, telerehabilitation and telemedicine. For instance, the World Health Organization (WHO) uses the term eHealth to describe the use of ICT to support population health and in healthcare areas [Citation1]. Within rehabilitation sciences, telerehabilitation is emerging [Citation2–4], defined by the delivery of rehabilitation services via ICT [Citation2] to include a wide range of services such as: assessment, intervention, supervision, education, consultation and counseling [Citation5,Citation6]. To prevent confusion, ICT will be used in this study as a term to describe technologies used to support and deliver healthcare services.
The use of ICT, specifically smartphones and tablets is rapidly growing [Citation7]. It is estimated that the amount of smartphone subscriptions in Europe will reach 880 million by 2021 [Citation8], and mobile app markets will expand even more, with currently over 160,000 mobile health apps available for download [Citation9]. The use of ICT in healthcare has shown great potential in improving the quality of life among senior citizens [Citation10], by facilitating support in independent living for persons with conditions such as stroke and Alzheimer’s disease [Citation11,Citation12]. Moreover, ICT has demonstrated potential in improving communication between patients and healthcare providers [Citation13]. Although it is still unclear how telerehabilitation services can most appropriately be rendered, it has been suggested that ICT can add value to current stroke rehabilitation [Citation14,Citation15]. For instance, White et al. [Citation16] described how, among persons with stroke, the use of a tablet was experienced as contributing to motivation, socialization, and was non-burdensome. This is also in line with earlier research showing that people after a stroke were using smartphones and tablets in their everyday life [Citation17,Citation18]. Moreover, smartphones and tablets have been widely integrated in the performance of everyday activities [Citation19,Citation20]. Yet many of the mobile applications available today lack expert involvement from health professionals or researchers, and do not adhere to relevant medical evidence [Citation21]. It can be argued that research to support evidence for the use of technologies in clinical practice is needed [Citation15,Citation22,Citation23].
Participation is generally part of rehabilitation goals [Citation24], and in some policy documents, participation is seen as the ultimate goal [Citation25]. But the concept of participation takes on different meanings in the context of health and welfare services. Participation was recently described in the literature “as engagement in daily life and ‘everyday life’” [Citation24]. While International Classification of Functioning, Disability and Health define participation as “involvement in a life situation” [Citation26] which can be interpreted as task performance in a person’s current environment [Citation26]. This definition has been criticized for lacking a perspective of the individuals’ subjective experience of involvement in their choices [Citation24]. Since participation is a multidimensional concept with different uses and meanings, it is being used imprecisely, leaving it up to the reader to infer how the concept is used [Citation27]. In a systematic review by Pinto-Bruno et al. investigating the use of ICT to increase participation [Citation28] there was no evidence for the use of ICT to increase participation among persons with dementia. Other systematic reviews found evidence for the use of ICT in people with stroke [Citation14] and Multiple Sclerosis [Citation29], but did not investigate the increase in participation as an outcome. In order to understand the potential of ICT in rehabilitation there is a need to create an overview of the available evidence, particularly focusing on the effect of ICT interventions on participation, independent of diagnosis.
There is still a knowledge gap between clinical practice and the use of ICT applications to improve rehabilitation and participation outcomes, which needs to be filled. Therefore, the aim of this article is to review and describe evidence of the use of ICT, including mobile technology, for improving participation in everyday life. A secondary aim was to describe how study outcomes were related to measuring participation.
Method
A scoping review design was used to disseminate the field of enquiry and supported the process to identify the knowledge gaps within the existing evidence [Citation30]. This scoping review followed the five stages as described by the methodological framework of Arksey and O’Malley [Citation30]; as a complement, the recommendations by Levac et al. [Citation31] on the Arksey and O’Malley framework have been used.
Stage 1: identifying the research question
The research question guiding the scoping review was, “what evidence is available for the use of ICT, including mobile technology, for improving participation in everyday life?”
Stage 2: identifying relevant studies
For inclusion in the review the following criteria were applied: a) contains use of an ICT based intervention, b) focuses on improving participation (i.e., according to the International Classification of Functioning, Disability and Health [Citation26]) or increasing independence in activities of daily living (ADL) as an outcome measure, c) could be of any design, d) participants over 18 years old, and e) published in English.
Three electronic databases were used: MEDLINE, CINAHL, and the Cochrane Library. This search was conducted between December 2017 and February 2018, without any restriction to publication date. A combination of the following search terms was used: ICT, information and communications technology, mHealth, m-Health, eHealth, e-Health, health informatics, telehealth, telerehabilitation, mobile technology, participat*, activities of daily living, intervention and prevention. Based on the high relevance of the journals scope all of the published issues (started 2009) of The International Journal of Telerehabilitation were hand-searched.
Systematic reviews that were found during the search were excluded, but the reference lists were hand-searched for relevant studies, as were the reference lists of the articles included in this study. (Further details of the search strategy are available upon request).
Stage 3: study selection
First, all titles were screened for relevance by MZ, and non-relevant titles were removed. Two of the authors (MZ and SG) reviewed the abstracts identified from the database searches independently. Abstracts were assessed on meeting the inclusion criteria. Disagreements on inclusion or exclusion of an abstract were resolved by reaching a consensus or by consulting a third reviewer (AHP). The full text of the included abstracts were obtained to be read independently by the authors (MZ and SG) to determine studies to be included in the review. In the case of a disagreement the third reviewer (AHP) was consulted.
Stage 4: charting the data
A data extraction form was developed in Microsoft Excel, based on the research question. Data were collected on: a) the article’s authors; b) year of publication; c) aims of the study; d) study design; e) study location; f) intervention used; g) technology used; h) participants’ characteristics; i) methods used to administer outcomes or the order of measurements; j) outcome measures; and k) key findings of relevance.
Stage 5: collating, summarizing and reporting the results
The studies were summarized descriptively and compared for similarities and differences [Citation30]. More specifically, in the studies, the use of the concept of participation (including opportunities to participate in everyday activities such as work, leisure and self-care [Citation24]) was investigated and described.
Results
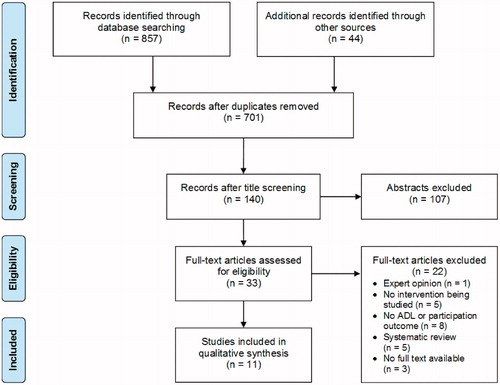
The search resulted in 701 records (without duplicates) of which 140 records were considered relevant and selected for their abstracts. Of those 140 abstracts, 33 full-text articles were assessed for eligibility, which resulted in 11 articles with consensus by the authors (MZ, SG and A-H P), for inclusion in the qualitative synthesis. The results of the identification process and selection phases of the study were described in detail based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) [Citation32] see .
Key characteristics of the included studies are presented in . Most of the studies were conducted in the USA (n = 7) and the use of a randomized controlled trial (RCT) design was most common (n = 7). Three pilot studies were included (n = 3) of which one had a RCT design and two were case studies. Most of the studies were published after 2012 (n = 8) and focused on stroke (n = 7). Multiple types of ICT were reported where video and telephone communications were the most commonly used ICT (both n = 5) and the use of email was reported in only one study. A combination of two ICT applications occurred in four of the studies.
Table 1. Main characteristics and outcomes of the included studies.
Participation was explicitly measured in three of the studies. In the remaining studies participation was a component to measure participation in everyday activities such as work, leisure and self-care [Citation26]. Six studies showed significant improvements in participation. The following results describe how ICT was used to improve participation and how participation was related to the outcomes.
ICT for improving participation in everyday life
Ten of the 11 included studies reported a change in participation, of which six studies showed a significant improvement between pre- and post-measurement. The main outcomes and the key findings of the studies are presented in . First the six significantly improved studies will be described, then the four non-significant but slightly improved studies and at last the study which found no improvement is described.
Pilutti et al. [Citation33] performed a RCT in which a behavioral intervention for people with Multiple Sclerosis combined videoconferencing with information from a website about becoming more physically active. The participants in the intervention group increased significantly in their self-reported physical activity in daily activities compared to the control group. Jones et al. [Citation34] with a single group design used a mobile phone in combination with emails to deliver the self-management program called myMoves. The participants improved significantly directly after the intervention, but the improvement did not remain significant at follow-up. It is noteworthy that the study by Jones et al. [Citation34] is the only study that asked the participants what their preference of contact was, email or telephone in order to ensure that the participants were contacted to their satisfaction. Ng et al. [Citation35] studied multiple cases who used the existing Cognitive Orientation to daily Occupational Performance (CO-OP) approach and delivered it over a videoconference. Two of three participants improved significantly after the intervention, the third participant improved, although not enough to be statistically significant. Hermann et al. [Citation36] conducted a case study in which the participant was supervised in using an electrical muscle activity stimulating device via videoconferencing. This resulted in significant improvement on the Canadian Occupational Performance Measure measuring participation in relation to daily activities. A pilot study by Forducey et al. [Citation37] also used videoconference to deliver a combination of physiotherapy and occupational therapy interventions for older people who had a stroke where the control group received standard home care without videoconferencing. A total of nine participants completed pre- and post-measurements and both groups showed significant improvements but no significance was found between the groups. Linder et al. [Citation38] used a combination of a telephone with a website in a RCT design investigating a robot-assisted therapy with a home exercise program. Both of the groups improved significantly, but showed no significant difference between the two groups.
In four of the 11 studies non-significant improvements between pre- and post-measurement were found. One of these studies was the pilot case study by Boehm et al. [Citation39], where a telephone was used to deliver the Managing Fatigue course but showed non-significant improvements for the participants. Chumbler et al. [Citation40] used a combination of videoconferences and telephone calls within a stroke telerehabilitation intervention. Improvements were found in the intervention group (N = 25), but between-group improvements were non-significant. Nguyen et al. [Citation41] compared the efficacy of the internet-based dyspnea self-management program with a face-to-face dyspnea self-management program in a study for people with COPD. Both groups showed improvements, though non-significant but they sustained these improvements at 6 months. Mayo et al. [Citation42] showed no significant effects in relation to surveillance, information and education, and psycho-social support using a RCT design where case managers kept in touch over the telephone compared to the usual care. A small improvement was measured by the Reintegration to Normal Living Index in both groups, but there was no significance within or between the groups. The conclusion was that the interventions used by the case managers were not sufficiently potent to alter the perceived health status.
No effect was observed in one study by Makai et al. [Citation43] who developed a web-based online health community to facilitate multidisciplinary communication for frail elderly. The online health community was only used actively by 26.2% of the participants and did not improve any of the outcomes.
Measurement of participation
In the included studies participation was measured in different ways and only three studies had participation as a primary outcome [Citation34,Citation35,Citation42]. Jones et al. [Citation34] reported that they used the modified Reintegration to Normal Living Index to measure participation, which assesses how well people return to normal living patterns related to participation in daily activities, recreational activities, social activities, family roles, and relationships. Although the participants improved in their participation during intervention but the effect was not sustained at the follow-up. The Reintegration to Normal Living Index (the non-modified version) was also used in a study by Mayo et al. [Citation42], though it was used without further explanation and with only a non-significant improvement that was not further discussed. Ng et al. [Citation35] described how they used Participation Index and indirectly the Canadian Occupational Performance Measure as their primary outcome and as a secondary outcome the Mayo-Portland Adaptability Inventory-4 to measure participation.
Three studies have measured participation as a satisfaction of performance in self-chosen activities by using the Canadian Occupational Performance Measure [Citation35,Citation36,Citation39]. In four studies [Citation37,Citation38,Citation41,Citation43] participation was used as an outcome for ADL in the intervention. These studies used ADL measurements such as the Functional Independence Measure, the Stroke Impact Scale, Katz-ADL and the Chronic Respiratory Questionnaire dyspnea subscale.
Two studies have also used physical activity in the frame of participation as an outcome measure [Citation33,Citation40]. First Chumbler et al. [Citation40] connected physical activity to ADL, measured by the Late-Life Function and Disability Instrument. Secondly, a broader connection was made by Pilutti et al. [Citation33], who defined physical activity as leisure, occupational or household activities that are planned or unplanned as a part of everyday life and showed significant effects with a behavioral intervention on physical activity.
Discussion
The primary aim of this scoping review was to review and describe the evidence of the use of ICT, including mobile technology, for improving participation in everyday life. A total of 11 studies were found on targeting participation as an outcome of an ICT based intervention. The participants in the majority of studies had had a stroke (64%). Ten of 11 studies found a change in participation in daily life, of which six showed a significant improvement. While many aspects of the results can be discussed, we will focus on three main findings: 1) the potential improvement’s in participation through using ICT, 2) the approach used in ICT-based interventions and challenges in conducting research pertaining to a rapidly changing technology landscape, and 3) the possible gaps between how participation was used as an outcome and addressed in projects.
Firstly, the studies included in this scoping review show that there is potential in using ICT-based interventions to improve participation however the design of a study has different impact on the level of evidence provided. Traditionally RCT designs are viewed as having a higher impact than for example case studies [Citation44]. Case study design were used in three studies and a single group pre-post design in one study. RCT design was used in seven of the included studies, only one showed significant improvements in favor of the ICT-based intervention group compared to the control group [Citation33], two studies found a non-significant improvement in favor of the intervention group [Citation40,Citation42], and one found no improvement [Citation43]. The remaining three RCT’s found improvements in participation in both the intervention and the control groups, with a non-significant difference between groups. Forducey et al. [Citation37], compared the effects of home-based ICT versus standard home care services. Even though both groups improved significantly, the amount of visits were significantly lower in the ICT group, which suggests it could be more cost-effective compared to the standard face-to-face home care services. The study by Nguyen et al. [Citation41] aimed to develop an intervention that would be (equally) effective whether delivered via ICT or face-to-face, in order to reach a larger number of patients with COPD. Both treatment groups had improved results, rendering the study a success. Of these three studies only the study by Linder et al. [Citation38] hypothesized that the ICT intervention group, who received the home exercise program together with the Hand Mentor Pro robotic device, would be significantly better than the control group receiving only the home exercise program. These studies show the potential of using ICT to deliver interventions as being equally efficient as face-to-face interventions and at the same time beneficial for healthcare at distance and for cost-effectiveness. Being able to provide healthcare services in the patient’s own environment increases the chances of improving the persons participation because of the contextual relevance the home environment creates [Citation45]. If there is an ICT option available, or more suitable for a patient, it seems to be a viable option. The results indicate that there is still a need for studies with sufficient power to investigating the effectiveness of ICT-based interventions.
Secondly, the approach in eight of the 11 studies showed that ICT was used as a tool for delivering an intervention. The intervention could either have been recently developed or be a currently existing intervention. An example is Hermann et al. [Citation36], they guided a patient using videoconferencing in the use of a previously developed electrical muscle stimulating hand orthosis. The results suggested that it was the orthosis that caused most of the improvement, and not as much the therapy received over videoconferencing since the therapist mainly had a counseling and supervising role. Three of the 11 studies have instead developed an intervention to be based on ICT as an integrated platform for the rehabilitation process; a web-based application [Citation41], a website [Citation33] and an online health community [Citation43]. These three studies used the potential of ICT as a form of rehabilitation intervention, rather than the other eight studies that used ICT as a tool for delivering an intervention that also could have been face-to-face. The majority of the included studies used existing interventions, which can be explained from a cost-effectiveness point of view, but also from the perspective of ICT interventions being a young research area. One challenge in integrating new technologies is short utility period. The time from development to implementation needs to be rapid in order to be competitive in relation to how fast the development of ICT products is happening. Nearly as soon as a new product is launched, there is a need for of a new version or an update. Surprisingly no studies were found on using smartphones targeting participation in everyday life, even though the aim of this study included the use of mobile technology and the fact that there is already such a large amount of mobile applications available [Citation9]. However, four of the 11 studies used a website or web-based application to connect participants with each other and the professionals [Citation41,Citation43], to track progress [Citation38,Citation41], or to communicate with participants [Citation33,Citation41]. The websites that have been used might be convertible to a mobile application in the future. The current growth rate in technology [Citation46,Citation47] can be one reason for why there are few studies available with the latest smart phone technology.
At last a relevant finding was the analysis of how participation was described, measured, and used as an outcome in the included studies. Interestingly, participation was mainly used as an outcome for involvement in a life situation as measured by using assessment tools such as the Reintegration to Normal Living Index, or as related to ADL. Only three studies included the outcome of participation as a choice, by using the Canadian Occupational Performance Measure as an outcome [Citation35,Citation36,Citation39]. Participation demonstrated improvement as an outcome in three of the studies [Citation34,Citation35,Citation42], even though participation was not described as a direct intervention target in any of the included studies nor as a primary aim. Instead participation was indirectly targeted by improved ADL or physical activity. This suggests that there is a potential in the design of ICT-based interventions to also target participation as an outcome measure in future studies. However, in most of the studies the concept of participation was not defined. A definition of participation would add to the generalisability of the studies and would make it more accessible to implement in other locations [Citation24]. By describing how participation was measured in the included studies, this scoping review illuminates the potential of improving participation with the use of ICT-based interventions. As improving participation is a relevant goal for rehabilitation and healthcare [Citation24,Citation25], there is also a need to measure and describe the intervention and its outcomes in relation to a definition of participation.
Although the results from the current scoping review suggest that ICT-based intervention could improve participation in relation to engagement in daily life and ‘everyday life” [Citation26] and “involvement in a life situation” [Citation27], there is still a need for more studies focusing on healthcare supported applications of ICT in improving participation in everyday life.
Methodological considerations
To our knowledge this is the first scoping review conducted with a focus on ICT and participation. There is a knowledge gap regarding how ICT is used in rehabilitation, therefore this scoping review was performed in order to disseminate the evidence for improving participation in everyday life using ICT. However, in this study only studies written in English were included; this might have limited the results, since the ICT interventions could be given in other languages and those results could’ve been published in the same language. This can be seen in the results where only one of the 11 included studies is from a non-English speaking country. The all-encompassing term ICT was used to combine different terms within the review, the search however was conducted with many terms that were found combined with a Boolean operator. In this search, some more unknown terms could have been missed.
Conclusion
This scoping review provides an overview of studies investigating an intervention delivered by, or based on, ICT to improve participation in everyday life. Ten of 11 included studies found a change when reported measuring participation, of which six showed a significant improvement. Delivering an existing intervention via ICT could be a valid option and shows significant improvement just as the face-to-face interventions. In future studies, there is a need to measure, and describe the intervention and its outcomes in relation to a definition of participation.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- World Health Assembly. Fifty-Eighth World Health Assembly. World Health Organ; 2005.
- Brennan D, Mawson S, Brownsell S. Telerehabilitation: enabling the remote delivery of healthcare, rehabilitation, and self management. Stud Health Technol Inform. 2009;145:231–248.
- Rogante M, Grigioni M, Cordella D, et al. Ten years of telerehabilitation: a literature overview of technologies and clinical applications. NeuroRehabilitation. 2010;27(4):287–304.
- Rogante M, Kairy D, Giacomozzi C, et al. A quality assessment of systematic reviews on telerehabilitation: what does the evidence tell us? Ann Ist Super Sanità. 2015;51(1):11–18.
- Brennan D, Tindall L, Theodoros D, et al. A blueprint for telerehabilitation guidelines. Int J Telerehabil. 2010;2(2):31–34.
- Russell TG. Telerehabilitation: a coming of age. Aust J Physiother. 2009;55(1):5–6.
- Lella A. comScore Reports February 2016 U.S. Smartphone Subscriber Market Share 2016. Available from: https://www.comscore.com/Insights/Rankings/comScore-Reports-February-2016-US-Smartphone-Subscriber-Market-Share
- Ericsson. Europe Ericsson Mobility Report. 2015 (November) accessed February 22, 2018.
- IMS Institute for Healthcare Informatics. Patient adoption of mHealth. USA: IMS Institute for Healthcare Informatics; 2015.
- Demiris G, Skubic M, Rantz MJ, et al. Facilitating interdisciplinary design specification of "smart" homes for aging in place. Stud Health Technol Inform. 2006;124:45–50.
- Lindqvist E, Borell L. Computer-based assistive technology and changes in daily living after stroke. Disabil Rehabil. 2012;7(5):364–371.
- Pilotto A, D'Onofrio G, Benelli E, et al. Information and communication technology systems to improve quality of life and safety of Alzheimer's disease patients: a multicenter international survey. J Alzheimers Dis. 2011;23(1):131–141.
- Crotty M, Killington M, van den Berg M, et al. Telerehabilitation for older people using off-the-shelf applications: acceptability and feasibility. J Telemed Telecare. 2014;20(7):370–376.
- Laver KE, Schoene D, Crotty M, et al. Telerehabilitation services for stroke. Cochrane Database Syst Rev. 2013;2013(12):1–46.
- Dinesen B, Nonnecke B, Lindeman D, et al. Personalized telehealth in the future: a global research agenda. J Med Internet Res. 2016;18(3):e53.
- White J, Janssen H, Jordan L, et al. Tablet technology during stroke recovery: a survivor’s perspective. Disabil Rehabil. 2015;37(13):1186–1192.
- Gustavsson M, Ytterberg C, Nabsen Marwaa M, et al. Experiences of using information and communication technology within the first year after stroke - a grounded theory study. Disabil Rehabil. 2018;40 (5):561–568.
- Kamwesiga JT, Tham K, Guidetti S. Experiences of using mobile phones in everyday life among persons with stroke and their families in Uganda - a qualitative study. Disabil Rehabil. 2017;39(5):438–449.
- Engström A-LL, Lexell J, Lund ML. Difficulties in using everyday technology after acquired brain injury: a qualitative analysis. Scand J Occup Ther. 2010;17(3):233–243.
- Rosenberg L, Nygård L, Kottorp A. Everyday technology use questionnaire: psychometric evaluation of a new assessment of competence in technology use. OTJR: Occup Part Heal. 2009;29(2):52–62.
- Subhi Y, Bube SH, Rolskov Bojsen S, et al. Expert involvement and adherence to medical evidence in medical mobile phone apps: a systematic review. JMIR mHealth uHealth. 2015;3(3):e79.
- Erickson K. Evidence considerations for mobile devices in the occupational therapy process. OJOT. 2015;3(2):a7.
- Fischl C, Asaba E, Nilsson I. Exploring potential in participation mediated by digital technology among older adults. J Occup Sci. 2017;24(3):314–326.
- Eide AH, Josephsson S, Vik K. Participation in Health and Welfare Services. New York: Routledge; 2017.
- United Nations. The standard rules on the equalization of opportunities for persons with disabilities. New York: United Nations; 1994.
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization; 2001.
- Cornwall A. Unpacking ‘participation’: models, meanings and practices. Community Dev J. 2008;43(3):269–283.
- Pinto-Bruno ÁC, García-Casal JA, Csipke E, et al. ICT-based applications to improve social health and social participation in older adults with dementia. A systematic literature review. Aging Mental Health. 2017;21(1):58–65.
- Khan F, Amatya B, Kesselring J, et al. Telerehabilitation for persons with multiple sclerosis (Review). Cochrane Database Syst Rev. 2015 2015(4):1-53.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(59):1-9.
- Liberati A, Tetzlaff J, Mulrow C, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
- Pilutti LA, Dlugonski D, Sandroff BM, et al. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult Scler. 2014;20(5).
- Jones TM, Dear BF, Hush JM, et al. myMoves program: feasibility and acceptability study of a remotely delivered self-management program for increasing physical activity among adults with acquired brain injury living in the community. Phys Ther. 2016;96(12).
- Ng EMW, Polatajko HJ, Marziali E, et al. Telerehabilitation for addressing executive dysfunction after traumatic brain injury. Brain Inj. 2013;27(5):548–564.
- Hermann VH, Herzog M, Jordan R, et al. Telerehabilitation and electrical stimulation: an occupation-based, client-centered stroke intervention. Am J Occup Ther. 2010;64(1):73-81.
- Forducey PG, Glueckauf RL, Bergquist T, et al. Telehealth for persons with severe functional disabilities and their caregivers: facilitating self-care management in the home setting. Psychol Serv. 2012;9(2):18.
- Linder S, Rosenfeldt A, Bay R, et al. Improving quality of life and depression after stroke through telerehabilitation. Am J Occup Ther. 2015;69(2):1–10.
- Boehm N, Muehlberg H, Stube JE. Managing poststroke fatigue using telehealth: a case report. Am J Occup Ther. 2015;69(6):1–7.
- Chumbler NR, Quigley P, Li X, et al. Effects of telerehabilitation on physical function and disability for stroke patients: a randomized, controlled trial. Stroke. 2012;43(8):2168–2174.
- Nguyen H, Donesky-Cuenco D, Wolpin S, et al. Randomized controlled trial of an internet-based versus face-to-face dyspnea self-management program for patients with chronic obstructive pulmonary disease: pilot study. J Med Internet Res. 2008;10(2):e9.
- Mayo NE, Nadeau L, Ahmed S, et al. Bridging the gap: the effectiveness of teaming a stroke coordinator with patient's personal physician on the outcome of stroke. Age Ageing. 2008;37(7):32–38.
- Makai P, Perry M, Robben SHM, et al. Evaluation of an eHealth intervention in chronic care for frail older people: why adherence is the first target. J Med Internet Res. 2014;16(6):e156.
- Hoffmann T, Bennett S, Del Mar C. Evidence-based practice across the health professions-e-book. Chatswood: Elsevier; 2013.
- American Occupational Therapy Association. Occupational therapy practice framework: domain & process 3rd edition. Am J Occup Ther. 2014;68(1):S1–S48.
- Nagy B, Farmer JD, Bui QM, et al. Statistical basis for predicting technological progress. PLoS One. 2013;8(2):e52669.
- Nagy B, Farmer JD, Trancik JE, et al. Superexponential long-term trends in information technology. Technol Forecast Soc Change. 2011;78(8):1356–1364.