Abstract
Purpose: The purpose of this scoping review was to explore the literature on experiences and perspectives of patients with hip fractures and their caregivers during transitions in care.
Methods: Seven databases were searched for studies published between 1 January 2000 and 3 July 2018. Grey literature was also searched.
Results: Eleven articles met the inclusion criteria. The scoping review found that patients and caregivers encounter several challenges during care transitions including the following: lack of information sharing, role confusion and disorganized discharge planning. Common suggestions reported in the literature for improving care transitions were: increasing written communication, offering a patient representative role, using technology for knowledge dissemination and increasing geriatrician involvement.
Conclusions: The results of this scoping review provide a useful foundation from which to build strategies to address challenges such as lack of information sharing, role confusion and disorganized discharge planning experienced by patients and caregivers during care transitions. Further research needs to explore the development of strategies to promote patient-centered care especially during discharge from an acute care facility.
Encourage health care providers to collaborate with patients with hip fracture and caregivers on decision-making about rehabilitation and recovery goals, discharge planning and safe patient transfer.
Assess the needs of patients with hip fracture and caregivers before, during and after a care transition to deliver patient and family-centered care across multiple care settings.
Provide patients with hip fracture and caregivers standardized information-exchange tools to increase timely, accurate exchange of information during care transitions.
Encourage formal discussions about roles and responsibilities in the transitions in care process among patients with hip fracture, caregivers and health care providers.
Implications for rehabilitation
Introduction
Hip fractures are one of the most common causes of fall-related hospitalizations in adults over the age of 65 [Citation1–3]. Patients with hip fracture are likely to experience functional decline, multi-morbidity and institutionalization after their injury [Citation4]. Approximately 13.5% of patients die within 6 months of sustaining a hip fracture and amongst those that survive, only 50% of patients are able to regain pre-fracture mobility [Citation5,Citation6]. Patients with hip fracture require treatment from a diverse range of health care providers across settings including hospitals, in-patient rehabilitation units, outpatient clinics, home care, assisted living facilities and long-term care homes [Citation7–10]. They are estimated to undergo 3.5 relocations or transfers within six months of incurring the injury [Citation11]. Care transitions are a vulnerable time for patients as poorly managed transitions can result in medication errors, hospital readmissions, poor patient outcomes and compromised patient satisfaction [Citation4,Citation12].
During transitions in care, caregivers (i.e., unpaid family members or friends) are often the only constant factor in a patient’s life [Citation12]. Caregivers and patients can provide insight into the quality of care transitions and their involvement in care planning can improve patient outcomes [Citation13]. A randomized controlled trial (n = 1,393) performed by Coleman et al. [Citation13] found that elderly patients had lower hospital readmission rates when caregivers and patients were given tools to communicate with providers, encouraged to take an active role in care planning and received guidance from a transition coach. Unfortunately, despite the importance of caregivers in care planning, there is often a lack of caregiver involvement during transitions in care [Citation8,Citation14]. Jeffs et al. [Citation14] found that caregivers of orthopedic patients were not actively engaged by health care providers during care planning and did not receive adequate support from the health care team after discharge.
Moreover, there is a growing need to integrate the perspectives of patients and caregivers in care planning to ensure that a patient and family-centered care approach is adopted to attain optimal patient outcomes [Citation12]. Understanding the experiences of patients with hip fracture and their caregivers as they navigate the health care system during care transitions will help policy-makers, health care providers and researchers design, develop and implement interventions to improve transitions of care in older patients with hip fracture. The purpose of this scoping review was to determine what is known about the perspectives of patients and caregivers on care transitions for adults recovering from a hip fracture. In addition to determining the extent and nature of evidence available, suggestions are made to identify future directions for research.
Methods
This scoping review was conducted to map the literature on the experiences of patients with hip fracture and caregivers during transitions in care. According to Arksey and O’Malley [Citation15], a scoping review is used to summarize and disseminate the key research findings in a field of study, identify gaps where there is a lack of research and to map the sources and types of research evidence available on a topic. This review was performed following Arksey and O’Malley’s [Citation15] methodological framework with updates by Levac et al. [Citation16]: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) charting the data; (5) collating, summarizing and reporting results; and (6) consultation. This scoping review was performed in accordance with the reporting guidelines presented in Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews [Citation17].
Identifying the research question
The following research question guided this scoping review: What is reported in the literature on the perspectives of patients and caregivers on care transitions for adults recovering from a hip fracture?
Through this scoping review we identified: (1) types of research studies on the topic; (2) characteristics of adults with hip fracture included in studies (e.g., age, gender, geographic area, etc.); (3) attitudes, perspectives and experiences of patients with hip fracture and caregivers during care transitions; and (4) factors impacting patients with hip fracture and caregiver experiences with care transitions.
Identifying relevant studies
A search strategy was developed with the input of an Education and Liaison Librarian at the University of Toronto. The following electronic databases were searched for literature published between January 1, 2000 and July 3, 2018: MEDLINE, EMBASE, PsycINFO, Allied and Complementary Medicine, Cumulative Index to Nursing and Allied Health Literature, Applied Social Sciences Index and Abstracts and Cochrane Database of Systematic Reviews. Grey literature was searched on TSpace, Health Quality Ontario, Bone and Joint Canada, Canadian Institute for Health Information and the World Health Organization websites. The reference lists of included studies and relevant review articles were manually searched to identify studies for inclusion; however, no additional articles were identified.
The literature search was performed using appropriate command line search syntax and indexing for each database. Broad keywords were combined using Boolean operators, truncators and wild card and proximity operators to account for permutations of the terms. Search terms included: hip fracture, transitional care, care continuum, patient transfer, care transitions (Supplemental Material A).
Study selection
Studies retrieved from the literature search were managed using EndNoteX8 software and Microsoft Excel. Deduplication of the initial search results was performed using Bramer et al.’s [Citation18] three stage method, which involved cross-referencing the study citations obtained from the six databases using custom export filters. Studies were included in the scoping review if they met the following criteria: (1) included a study sample of patients with hip fracture over the age of 18; (2) primarily focused on patient and caregiver experiences; (3) addressed the topic of transitions in care; (4) were peer-reviewed or in the grey literature; and (5) published between January 1, 2000 to July 3, 2018. In order to meet criteria three (addressed the topic of transitions in care), the study had to explicitly discuss the movement of patients between settings (e.g., transfer of patient from an acute care facility to a nursing home, or rehabilitation to home). In studies with a mixed sample of patients and caregivers, the results were not stratified by population and were frequently reported together.
Studies were excluded if they met any of the exclusion criteria: (1) books, book chapters, opinion pieces, editorials, study protocols, case laws, trial papers; (2) studies performed on non-humans; and (3) conference and poster abstracts without a full-text article.
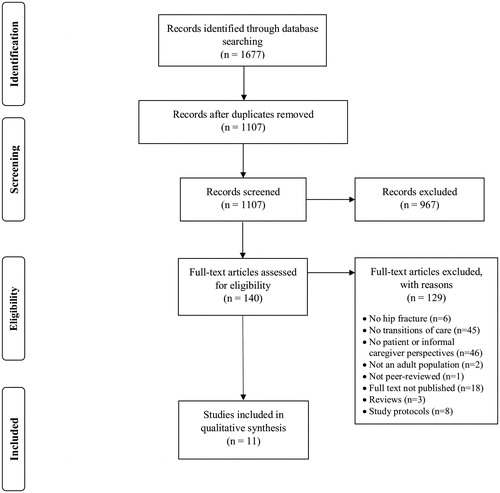
Two reviewers (MA and LC) independently screened the titles and abstracts of the first 100 articles procured from the search. Articles that did not meet the inclusion criteria were excluded. The overall kappa agreement of the researchers was 0.97, suggesting there was high inter-rater agreement [Citation19]. Discrepancies were discussed in-person between reviewers and resolved by consensus. The remaining articles were independently screened by a single reviewer (MA). After the initial title and abstract screening, 140 articles remained for full-text review. Two reviewers (MA and LC) independently screened 14 full-text articles and with a kappa agreement of 1.00, the remaining full-text articles were reviewed by a single reviewer (MA). After full-text review, 11 articles were included for data extraction.
Charting the data
Data from the included studies (n = 11) was extracted by a single reviewer (MA) and organized into a Microsoft Excel spreadsheet. The extracted data included study characteristics, patient and caregiver population characteristics, information about the care journey (e.g., patient and caregiver experiences, patient and caregiver suggestions for improving care transitions), intervention characteristics and study outcomes, main themes, and findings.
Collating, summarizing and reporting results
Extracted data that addressed the aims of this scoping review was discussed in weekly meetings with the research team. These meetings identified broad themes emerging in the literature, which is essential to the scoping review charting process [Citation15]. Two broad themes were identified: challenges affecting care transitions and suggestions for improving care transitions. Following this, the extracted information was color coded by two authors (MA, LC) who independently and collaboratively sorted the informational points according to emerging subthemes in order to assist with reporting of the scoping review findings. This was an iterative process in which findings across the qualitative studies were collated to identify key themes describing patient and caregiver experiences with care transitions.
Results
The initial search identified 1,107 unique articles (). After screening the titles and abstracts, a total of 140 articles underwent full-text review, with 11 articles ultimately meeting the inclusion criteria. Two systematic reviews [Citation20,Citation21] and one literature review [Citation4] were retrieved during the initial search and were excluded during full-text review; however, the articles referenced in these reviews were assessed using the inclusion criteria.
Characteristics of the 11 studies included in this scoping review are summarized in . Most included studies used a qualitative design (n = 10), with only one quantitative study [Citation24]. The included studies were performed in Canada (n = 6), Norway (n = 1), the United States (n = 1), Denmark (n = 1), and Australia (n = 1). One study was conducted across multiple countries: Czech Republic, France, Germany, Poland, Portugal, Spain and Turkey [Citation24]. The included studies were published between 2010 and 2017, with a considerable increase in publications after 2013 (n = 7). Study sample sizes ranged from 1 to 6,536; however, most studies had less than 50 participants in their overall sample (n = 8). Only five studies reported the mean age of patients, which ranged from 76 to 87.5 years [Citation8–10,Citation24,Citation26]. The studies predominantly included female patient participants, with more female patients than male patients in six studies [Citation9,Citation10,Citation24–27]. Three studies had a study population consisting of more female caregivers than male caregivers [Citation9,Citation22,Citation26] and two studies included only female caregivers [Citation8,Citation23]. Only two studies provided data on patients’ other medical conditions or comorbidities [Citation10,Citation28].
Table 1. Characteristics of studies identified in scoping review (n = 11).
The overall characteristics of patients’ and caregivers’ experiences with care transitions are described in . Two studies reported exclusively on caregiver experiences with care transitions [Citation9,Citation26], one study on patients’ experiences with continuity of care [Citation24] and the remaining eight studies on the perspectives of different combinations of patients, caregivers and health care providers [Citation7,Citation8,Citation10,Citation22,Citation23,Citation25,Citation27,Citation28]. The majority of studies (n = 7) contained a description of the patients’ care journey [Citation7–10,Citation22,Citation26,Citation28]. Three articles featured the perspectives of individuals from more than one type of patient population (e.g., hip fracture patients and stroke patients included in the same study) [Citation22,Citation24,Citation28].
Table 2. Common themes and author recommendations identified in the included studies.
Two overarching thematic categories were identified across the studies: (1) common challenges encountered by patients and caregivers during care transitions; and (2) suggestions for improving care transitions. These thematic categories represent the most commonly discussed concepts relating to patients and caregivers’ experiences with care transitions.
Common challenges encountered by patients and caregivers
Many studies discussed challenges encountered by patients and caregivers during care transitions. From the 10 qualitative articles, three sub-themes were identified as barriers complicating hip fracture patient care transitions: (1) lack of information sharing; (2) role confusion; and (3) disorganized discharge planning.
Lack of information sharing
Patients' and caregivers' dissatisfaction with the amount and content of information provided about the care journey was reported in seven of the ten qualitative studies [Citation7–9,Citation22,Citation23,Citation26,Citation28]. These studies illustrated that few patients and caregivers had access to adequate and timely information regarding the patients’ continuity of care. Examples of the lack of information sharing with patients and caregivers included an absence of the following: clinician-initiated conversations about treatment plans, accurate information about the recovery and information from hospital staff during discharge and admission.
Hospital policies regarding patient privacy occasionally complicated information procurement [Citation7,Citation23,Citation26]. In Glenny et al.’s study [Citation23], caregivers identified privacy policies as a barrier to obtaining important information about the patient during rehabilitation procedures and were disappointed about the lack of education on navigating hospital procedures to obtain information. In three studies, patients and caregivers identified the timing and mode of information delivery as barriers to information sharing [Citation9,Citation23,Citation26]. Caregivers and patients reported that health care providers were inflexible about when a meeting could be arranged to discuss the patient’s future care plan [Citation9,Citation23,Citation26]. This resulted in caregivers, who were often balancing multiple responsibilities, to lose the opportunity to discuss their concerns about the patient’s care transition with the health care team [Citation9,Citation23,Citation26]. In one Canadian study, Elliott et al. [Citation9] found that the rural setting made it difficult for caregivers to commute to the hospital and attend meetings with health care providers, and distant family members also experienced distress about being unable to be more involved in the patient’s treatment [Citation9].
Role confusion
Another sub-theme identified was role confusion, which highlighted the impact of unclear individual roles and responsibilities during transitions in care [Citation7,Citation8,Citation22]. The sub-theme of role confusion came up in different contexts across the three studies: confusion about the role of different health care providers [Citation7], a lack of clarity about where clinical responsibilities ended and caregiver responsibilities began [Citation8] and ambiguity about caregiving responsibilities when multiple family members were involved [Citation22]. Toscan et al. [Citation7] identified health care provider role confusion as a challenge complicating the care transition of an elderly, female patient who had undergone a hip fracture. The patient in this study reported difficulty physically distinguishing clinicians due to the similarity of their uniforms and expressed confusion about the role of each health care provider on the team [Citation7]. When multiple family members were involved in patients' circle of care, it resulted in patients feeling disengaged from the management of their condition, and caregivers feeling stressed and overwhelmed, due to a lack of clarity about their specific role [Citation8, Citation22]. In Giosa et al.'s study [Citation22], caregivers reported that health care providers rarely considered family dynamics when designing a care plan and did not assess family members’ capacity and willingness to provide care.
Disorganized discharge planning
Six studies reported that patients and caregivers experienced distress during care transitions due to disorganized discharge planning [Citation7,Citation8,Citation10,Citation23,Citation25,Citation28]. Examples of this sub-theme included the following: a focus on rapid discharge [Citation8,Citation23], absence of patient and caregiver involvement during discharge planning [Citation7,Citation10,Citation25] and a lack of standardized patient assessment during care transitions [Citation28]. A lack of patient-centered discharge planning and patient and caregiver involvement during the transition from acute or intermediate care facilities to independent community living contributed to poor care transition experiences for several participants [Citation8,Citation23]. Additionally, in Toscan et al.’s study [Citation8], participants felt that policies and procedures in a hospital setting emphasized early discharge even when services to support the patient at home were lacking. These expectations of early discharge resulted in patients feeling rushed to recover [Citation7,Citation8,Citation23]. For example, Glenny et al. [Citation23] found that caregivers felt that the fast-paced hospital setting resulted in clinicians making quick decisions about transferring the patient from the hospital and prevented providers from collaborating with patients and caregivers on the discharge planning process.
Suggestions for improving care transitions
Common suggestions identified in the studies to improve care transitions for hip fracture patients and caregivers were: (1) increasing written communication; (2) offering a patient representative role; (3) using technology for knowledge dissemination; and (4) increasing geriatrician involvement.
Increasing written communication
Authors of the included articles discussed that a written summary about the hip fracture injury, recovery plan and caregiver responsibilities could be provided to patients and caregivers at discharge to promote mutual understanding between clinicians, caregivers and patients [Citation9,Citation22,Citation25–27]. In one Canadian study, Schiller et al. [Citation27] conducted semi-structured interviews with 19 participants including patients with hip fracture and their caregivers. Study participants described feeling ill-informed about the recovery process and suggested that a clearly illustrated timeline of recovery and benchmarks would be useful [Citation27]. It was recommended across several studies that a written informational guide about rehabilitation techniques and procedures, recovery goals and caregiver-responsibilities in the home would help prepare patients and caregivers for what to expect after the patients’ injury [Citation9,Citation22,Citation25]. Giosa et al. [Citation22] also suggested that a formal contract outlining the caregivers’ responsibilities, clinicians’ contact information and details about the patient’s injury and ongoing care plan would help caregivers build a relationship of trust with clinicians.
Offering a patient representative role
Three articles suggested that the integration of a patient navigator role in the health care delivery system would improve patient and caregiver experiences with transitions of care [Citation7,Citation8,Citation27]. In all three studies, it was identified that this individual would advocate for the patient, coordinate and manage care for the patient across settings and organize communications between individuals in the patient’s circle of care. Two studies referred to this individual as a “system navigator” [Citation7,Citation8] and one study referred to this individual as a “patient care advocate” [Citation27]. The literature did not specify who should take on this role; however, patients and caregivers in Schiller et al.’s study [Citation24] wanted an intermediary to ask health care providers questions on their behalf during transitions of care. These caregivers and patients felt that having a “patient care advocate” would facilitate their navigation of the health care system [Citation24].Similarly, Toscan et al. [Citation7] suggested that a “system navigator” should be a single point of contact for the patient, who could help caregivers understand their roles after patient discharge, give supportive advice about their new caregiving responsibilities and advocate for the patient’s health.
Using technology for facilitating communication
Three studies proposed that face-to-face communication should be supplemented with online communication tools and information-technology [Citation9,Citation23,Citation26]. The authors of all three studies focused on the use of technology to improve communication primarily between caregivers and health care providers and to provide caregivers with access to resources about caregiving responsibilities. Two studies suggested that the integration and development of an online resource center with information about the recovery process could improve communications and care transitions [Citation23,Citation26]. Nahm et al. [Citation26] proposed that an online resource center should include interactive educational resources and communication features to facilitate discussions between clinicians and caregivers [Citation26]. The studies found that technology should be used to address time and geographical barriers, which limit communication between patients, caregivers and health care providers [Citation9,Citation23]. Similarly, Elliott et al. [Citation9] noted that the incorporation of telecommunications technology (e.g., Skype) in rural health care settings as being especially valuable to engage distant caregivers.
Increasing geriatrician involvement
Two articles identified that geriatrician involvement during care transitions could improve patient outcomes, especially for patients with multiple comorbidities and polypharmacy [Citation10,Citation28]. Killington et al. [Citation10] conducted a study exploring the efficacy of a hospital outreach rehabilitation program for patients (n = 28) returning to a nursing home following a hip fracture. The authors found that nursing home residents who had a geriatrician, out-patient support and physiotherapy encountered fewer problems with pain management during care transitions, experienced improved patient outcomes and also had improved outlooks on life compared to the patients without these resources [Citation10]. Additionally, Storm et al. [Citation28] recommended that elderly patients with complex clinical needs should have geriatricians perform comprehensive assessments during admission and discharge to avoid functional decline upon their return home [Citation28].
Discussion
To our knowledge, this is the first scoping review on transitions in care experiences of patients with hip fracture and their caregivers. In the 11 studies identified, the most common challenges encountered by patients and caregivers were the lack of information-sharing, role confusion and disorganized discharge planning. This scoping review also described commonly reported suggestions to improve care transitions, which included: increasing written communication, offering a patient representative role, using technology for knowledge dissemination and increasing geriatrician involvement.
This review highlights the importance of communication and information-sharing between -patients, caregivers and health care providers [Citation7–9,Citation22,Citation23,Citation26,Citation28]. The results illustrate that there is a lack of systematic, timely information sharing between patients with hip fracture, caregivers and clinicians during transitions in care. The findings also show that communication within the patients’ care circle was exacerbated by geographical distance, timing issues and lack of physician-initiated dialog [Citation8,Citation9,Citation22,Citation23,Citation26,Citation28]. The use of individualized written communication was a common suggestion made by patients, caregivers and health care providers to improve information-sharing during care transitions [Citation9,Citation22,Citation25–27].
Addressing this issue of information sharing, Coleman et al. [Citation29] explored the effectiveness of a written communication tool to improve care transitions in patients with complex care needs. The authors examined the effectiveness of a care transitions intervention, which was characterized by the use of the Personal Health Record and a transition coach, in chronically ill older patients (N = 750) undergoing care transitions [Citation29]. When used in conjunction with a transition coach, the personal health record reduced rehospitalizations, increased patient confidence after the transition and improved patients’ medication management skills [Citation29].
Another key finding from this review involves the contribution of unclear roles and responsibilities of clinicians and caregivers to role confusion and poor patient and caregiver experiences during transitions in care [Citation7,Citation8,Citation22]. When a patient with a hip fracture injury transitions through multiple care settings, the number of providers involved in delivering care to the patient increases [Citation7,Citation8,Citation22], which was shown to dilute personal responsibilities and impede delivery of care for patients with hip fracture [Citation8]. However, the addition of a transitions coach in previous research has been shown to improve care transitions with lowered rehospitalization rates and increased patient satisfaction during transitions [Citation30].
Caregivers’ and patients’ need for unambiguous accountability from health care providers is well documented in the literature [Citation14,Citation30,Citation31]. The patients and caregivers interviewed in a study performed by Mitchell et al. [Citation30] described valuing a clear channel of responsibility with specific individuals being accountable for overseeing their care transition plan and feeling abandoned when they were unable to identify or trust their primary care physician. These findings accentuate the need for educating patients, caregivers and health care providers about their role in arranging and coordinating care services for patients and caregivers during transitions of care.
The findings from this scoping review indicate that patients and their caregivers felt that patients were moved between settings haphazardly, without formal assessment or warning [Citation7,Citation8,Citation10,Citation23,Citation25,Citation28]. Although they are few in number, some studies have tried to develop operating protocols to standardize patient handoff procedures during discharge. Friesen et al. [Citation32] developed a standard operating protocol, which required health care providers to consistently follow a seven step procedure. Another standardized tool was implemented in a study performed by Weingart et al. [Citation33] to guide patient handoff between pediatric services, resulting in increased provider and caregiver satisfaction with the patient handoff process.
Important research gaps have been identified in this scoping review. First, this review found that research exploring the lived experiences of patients with hip fracture and caregivers during transitions is limited. More specifically, this review highlighted a gap in the literature examining the care transitions of male patients with a hip fracture injury. The studies included in this review did not report the experiences of men and women separately. Longitudinal research on gender differences in patients with hip fracture shows that men suffer higher mortality than women in the year after discharge [Citation34,Citation35]. Men are also more likely to suffer post-operative complications after discharge, which can significantly increase the likelihood for rehospitalization and morbidity [Citation35]. Thus, males with hip fracture may have had different experiences than women and future research should report the experiences of men and women separately.
The second gap is in the types of studies conducted to date: experiences of patients with hip fracture and their caregivers should be explored both quantitatively and qualitatively. In this scoping review, only one empirical study assessed patient experiences using quantitative measures, and the remaining studies were qualitative. For example, there were no quantitative studies identified in this review that evaluated interventions designed to improve patient experiences with care transitions. Patient and caregiver experiences are complex and difficult to evaluate; however, using standardized quantitative evaluation and measurement approaches (e.g., patient reported experience measures and patient-reported outcomes) in conjunction with qualitative data can provide a more multi-faceted description of patient and caregivers’ satisfaction, perceptions, engagement and preferences during care transitions.
Limitations
Although a thorough search of the databases and gray literature was performed, it is possible that this scoping review omitted relevant articles and did not cover the extent of the research available on this topic. Specifically, transitions in care is a relatively broad concept, lacking a universal definition, resulting in a lack of standardized terminology in the current literature databases. In order to minimize the possibility of missed articles, our search strategy was adapted for a variety of databases and included all key words and Mesh headings relating to transitions in care and hip fracture patient and caregiver experiences. Additionally, the reference lists of the included articles were manually searched for relevant articles. Another limitation is that this review included studies in which hip fracture was pooled with other diseases. However, this was done in order to capture a wide breadth of research available on the topic. Lastly, a critical appraisal of the sources of evidence was not undertaken. This is consistent with published guidelines for the scoping review method as scoping reviews are undertaken to provide an overview of the evidence in the literature regardless of methodological quality or bias [Citation15,Citation17]. This scoping review focused on providing a descriptive review of the information provided within the studies, which can be used to provide a framework to guide future research efforts.
Next steps for future research
Future research efforts should focus on designing and evaluating interventions that provide each member of the patients’ care circle with information about the roles and unique responsibilities of caregivers and health care providers. Furthermore, most individuals that undergo a hip fracture also have comorbidities like respiratory disease, dementia, or circulatory disease [Citation36]. Thus, future studies should investigate the effectiveness of communication tools for patients with such comorbidities. Due to the lack of studies exploring male patient perspectives during care transitions, future research should seek to examine how gender influences transition experiences and overall health and well-being post-discharge. In order to strengthen the process of information-sharing during care transitions, studies should also investigate how patient and caregiver perspectives can be incorporated into the development of strategies and health information systems to create patient-centered tools that can aid in the management of a patient’s health post-discharge.
Conclusions
This scoping review provides an overview of the experiences and perspectives of patients with hip fracture and their caregivers during transitions in care. The results from this review highlight the need for improvement of care transition experiences due to lack of information-sharing, role confusion and disorganized discharge processes. This scoping review provides a useful foundation from which to build strategies to address challenges experienced by patients and caregivers during care transitions. Further research needs to explore the development of strategies to promote patient-centered care especially during discharge from an acute care facility. The information obtained from this review signals the need to reflect on current policies regarding effective transitions in care, utilization of services to improve patient and caregiver experiences, and highlights the need for timely and accurate information-sharing, physician-initiated conversations about caregiver responsibilities and systematic patient assessment at discharge.
Supplemental_Material_A.docx
Download MS Word (21.9 KB)Acknowledgements
The authors would like to thank the University of Toronto librarians for sharing their knowledge and expertise in literature syntheses, as well as Stephanie Cimino for help with data extraction from the articles.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Injury Prevention. 2002;8:280–283.
- DeGrauw X, Annest JL, Stevens JA, et al. Unintentional injuries treated in hospital emergency departments among persons aged 65 years and older, United States, 2006–2011. J Safety Res. 2016;56:105–109.
- Scott VP, Pearce M, Pengelly C. Technical report: injury resulting from falls among Canadians age 65 and over. Report on seniors’ falls in Canada 2005. Canada: Public Health Agency of Canada; 2005.
- Hung WW, Egol KA, Zuckerman JD, et al. Hip fracture management: tailoring care for the older patient. JAMA. 2012;307:2185–2194.
- Vochteloo AJH, Moerman S, Tuinebreijer WE, et al. More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int. 2013;13:334–341.
- Hannan EL, Magaziner J, Wang JJ, et al. Mortality and locomotion 6 months after hospitalization for hip fracture risk factors and risk-adjusted hospital outcomes. J Am Med Assoc. 2001;285:2736–2742.
- Toscan J, Manderson B, Santi SM, et al. "Just another fish in the pond": the transitional care experience of a hip fracture patient. Int J Integr Care. 2013;13:e023.
- Toscan J, Mairs K, Hinton S, et al. Integrated transitional care: patient, informal caregiver and health care provider perspectives on care transitions for older persons with hip fracture. Int J Integr Care. 2012;12:e13.
- Elliott J, Forbes D, Chesworth BM, et al. Information sharing with rural family caregivers during care transitions of hip fracture patients. Int J Integr Care. 2014;14:e018.
- Killington M, Walker R, Crotty M. The chaotic journey: Recovering from hip fracture in a nursing home. Arch Gerontol Geriatr. 2016;67:106–112.
- Boockvar KS, Litke A, Penrod JD, et al. Patient relocation in the 6 months after hip fracture: risk factors for fragmented care. J Am Geriatr Soc. 2004;52:1826–1831.
- Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc. 2003;51:549–555.
- Coleman EA, Smith JD, Frank JC, et al. Preparing patients and caregivers to participate in care delivered across settings: the Care Transitions Intervention. J Am Geriatr Soc. 2004;52:1817–1825.
- Jeffs L, Saragosa M, Law MP, et al. The role of caregivers in interfacility care transitions: a qualitative study. Patient Prefer Adherence. 2017;11:1443–1450.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69.
- Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467.
- Bramer WM, Giustini D, De Jong GB, et al. De-duplication of database search results for systematic reviews in endnote. J Med Libr Assoc. 2016;104:240–243.
- Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Syn Methods. 2014;5:371–385.
- Allen J, Koziak A, Buddingh S, et al. Rehabilitation in patients with dementia following hip fracture: a systematic review. Physiotherapy Canada. 2012;64:190–201.
- Leigheb F, Vanhaecht K, Sermeus W, et al. The effect of care pathways for hip fractures: a systematic review. Calcif Tissue Int. 2012;91:1–14.
- Giosa JL, Stolee P, Dupuis SL, et al. An examination of family caregiver experiences during care transitions of older adults. Can J Aging. 2014;33:137–153.
- Glenny C, Stolee P, Sheiban L, et al. Communicating during care transitions for older hip fracture patients: family caregiver and health care provider's perspectives. Int J Integr Care. 2013;13:1–13.
- Groene O, Arah OA, Klazinga NS, et al. Patient experience shows little relationship with hospital quality management strategies. PloS One. 2015;10:e0131805.
- Jensen CM, Smith AC, Overgaard S, et al. "If only had I known": a qualitative study investigating a treatment of patients with a hip fracture with short time stay in hospital. Int J Qual Stud Health Well-Being. 2017;12:1–9.
- Nahm E, Resnick B, Orwig D, et al. Exploration of informal caregiving following hip fracture. Geriatr Nurs. 2010;31:254–262.
- Schiller C, Franke T, Belle J, et al. Words of wisdom - Patient perspectives to guide recovery for older adults after hip fracture: a qualitative study. Patient Prefer Adherence. 2015;9:57–64.
- Storm M, Siemsen IMD, Laugaland K, et al. Quality in transitional care of the elderly: key challenges and relevant improvement measures. Int J Integr Care. 2014;14:e013.
- Coleman EA, Parry C, Chalmers S, et al. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828.
- Mitchell SE, Laurens V, Weigel GM, et al. Care transitions from patient and caregiver perspectives. Ann Fam Med. 2018;16:225–231.
- Bragstad LK, Kirkevold M, Foss C. The indispensable intermediaries: a qualitative study of informal caregivers' struggle to achieve influence at and after hospital discharge. BMC Health Serv Res. 2014;14:331–342.
- Friesen MA, Herbst A, Turner JW, et al. Developing a patient-centered ISHAPED handoff with patient/family and parent advisory councils. J Nurs Care Qual. 2013;28:208–216.
- Weingart C, Herstich T, Baker P, et al. Making good better: implementing a standardized handoff in pediatric transport. Air Med J. 2013;32:40–46.
- Hawkes WG, Wehren L, Orwig D, et al. Gender differences in functioning after hip fracture. J Gerontol A Biol Sci Med Sci. 2006;61:495–499.
- Sharma H, Vashishtha P, Sharma R. Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma. 2005;19:365–366.
- Panula J, Pihlajamäki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older - A population-based study. BMC Musculoskelet Disord. 2011;12:105–110.