Abstract
Purpose: To compare family and functional outcome in infants at very high risk of cerebral palsy, after receiving the family centred programme “Coping with and Caring for infants with special needs (COPCA)” or typical infant physiotherapy.
Materials and methods: Forty-three infants at very high risk were included before 9 months corrected age and randomly assigned to one year COPCA (n = 23) or typical infant physiotherapy (n = 20). Family and infant outcome were assessed before and during the intervention. Physiotherapy intervention sessions were analysed quantitatively for process analysis. Outcome was evaluated with non-parametric tests and linear mixed-effect models.
Results: Between-group comparisons revealed no differences in family and infant outcomes. Within-group analysis showed that family’s quality of life improved over time in the COPCA-group. Family empowerment was positively associated with intervention elements, including “caregiver coaching.”
Conclusions: One year of COPCA or typical infant physiotherapy resulted in similar family and functional outcomes. Yet, specific intervention elements, e.g., coaching, may increase empowerment of families of very high risk infants and may influence quality of life, which emphasizes the importance of family centred services.
One year of the family centred programme “Coping with and a Caring for infants with special needs” compared with typical infant physiotherapy resulted in similar family outcome and similar functional outcome for the infants at very high risk for cerebral palsy.
Specific contents of intervention, such as caregiver coaching, are associated with more family empowerment and increased quality of life.
Emphasis on family needs is important in early intervention for infants at very high risk for cerebral palsy.
Implications for rehabilitation
Introduction
Prenatal, perinatal, or postnatal complications in early infant life inducing cerebral lesions are major risk factors of cerebral palsy (CP) [Citation1]. For families, the knowledge of the presence of such risk factors suddenly alters the expectations on their child’s development. As limited knowledge is available on the exact nature of early developmental trajectories, the presence of the “at risk” status implies that caregivers have to deal with uncertainty about future expectations.
CP induces impairments in body functions and structures, such as dysregulation of muscle tone, causing limitations in activities and participation restrictions [Citation2,Citation3]. In infancy, most activities and participation occur in the context of the home environment. The family environment is a constant factor, with continuous interactions between the infant and his or her family. The physical, cognitive, and behavioral constrains of infants at risk of or with a developmental disorder usually induce challenging caregiving demands [Citation4,Citation5]. Caregivers of children with CP perceive in general more stress, a lower quality of life, increased time constraints, and financial and psychological burdens [Citation6,Citation7]. Less is known about caregivers of infants at risk of CP, i.e., before a diagnosis has been made. The uncertain future of the child adds to the stress [Citation8]. A large burden of care and significant stress may influence caregivers’ health condition and interaction with the child. For instance, caregivers of children with CP are at risk of a depressed mood [Citation9]. Therefore, not only the infant’s developmental problems, but also the mental health of caregivers may increase the infant’s risk for social, cognitive, and behavioral problems and later psychopathology [Citation10,Citation11]. Notwithstanding the accumulation of risk factors, many caregivers of children with developmental problems cope well with their family situation and adjust their expectations and daily life [Citation12]. Little is known about the coping of families with an infant at very high risk of developmental problems, but it is conceivable that similar mechanisms play a role.
Originally, paediatric physiotherapy was largely involved with normalizing and optimizing body functions and structures. Over the years, focus shifted from body functions and structures towards activities, participation and the environment, including the family [Citation13]. Family centred services have been introduced, with more involvement of families, aiming for equal partnership between families and professionals [Citation14,Citation15]. Early intervention programmes for preterm infants which included parent–child interaction have been shown to be more effective than interventions which focus either alone on the infant or on the caregivers [Citation16].
We recently performed the LEARN2MOVE 0-2 study [Citation17], a randomized controlled trial on early intervention in infants at very high risk of CP. The COPCA-intervention (COPing with and CAring for infants with special needs – a family centred programme) was compared with regular infant physiotherapy. COPCA was developed in beginning of the 21st century; it has two components: (1) a family component, with autonomy of the family and a coaching role of the physiotherapist to empower families to make their own decisions; and (2) a neurodevelopmental component, based on the Neuronal Group Selection Theory, with a hands-off approach to challenge the infant to find its own adaptive motor strategy in various circumstances. The physiotherapist coaches caregivers to implement interventional elements into daily life activities [Citation18,Citation19]. The control group received the standard physiotherapy as provided in the Netherlands (typical infant physiotherapy). Typical infant physiotherapy was originally based on NeuroDevelopmental Treatment principles, but nowadays a more functional approach and more involvement of the family has been implemented [Citation13,Citation18,Citation20]. In our accompanying paper, we reported that infant neuromotor, cognitive, and behavioral function was similar in the two intervention groups [Citation21].
In the present paper, we study the effects of the two interventions on family function and infants’ activities and participation. We address the following questions: (1) do families receiving COPCA or typical infant physiotherapy differ in outcome, regarding empowerment, stress, coping, and quality of life?; (2) do infants at very high risk of CP receiving COPCA or typical infant physiotherapy differ in functional outcome and quality of life?; (3) are specific interventional elements related to family and infant outcome; and (4) does the severity of the infant’s physical impairment affect family outcome? We expected a more positive family outcome in the COPCA-group, because COPCA is based on a family centred approach. We hypothesized that infants who received COPCA would have less limitations in activities and participation restrictions than infants who received typical infant physiotherapy, as COPCA aims to challenge the infants to find their own motor solutions. The implementation of these strategies into daily life activities is part of the COPCA-programme. Based on our previous studies [Citation22,Citation23], we expected that especially the interventional elements “caregiver coaching” and “challenging the infant to self-produced motor behavior” would be associated with better infant and family outcomes. Finally, we expected that the severity of physical impairment has a relatively small influence on family function, as often the infant’s motor impairment is only one of the many factors that affect family function [Citation5,Citation24].
Materials and methods
Participants
Infants at very high risk of CP were included in the study between 0 and 9 months corrected age (CA). Inclusion criteria were: (1) cystic periventricular leukomalacia (cPVL); or (2) parenchymal lesions as a result of infarction or haemorrhage; or (3) severe asphyxia with brain lesions on magnetic resonance imaging (MRI); or (4) clinical dysfunction suspect for development of CP. Exclusion criteria were (1) insufficient understanding of the Dutch language; or (2) severe congenital anomalies. The inclusion period was between November 2008 and November 2013, during which 43 infants from 12 different hospitals in the Northern region of The Netherlands were included. Caregivers gave informed consent. Infants were randomly assigned to either COPCA (n = 23) or typical infant physiotherapy (n = 20) by one of the authors (T.D.) with random sequence generating and concealment of the groups, using stratified blocks based on the inclusion criteria. The study was approved by the Medical Ethical Committee of the University Medical Center of Groningen and registered in the Dutch trial register under NTR1428.
Interventions
After inclusion, one year intervention of either COPCA or typical infant physiotherapy started, provided by paediatric physiotherapists. Paediatric physiotherapists in the COPCA-group received a COPCA-training. COPCA was provided at the infant’s home (n = 23), typical infant physiotherapy usually at home (n = 17) and sometimes in an outpatient setting (n = 3). Frequency of intervention was somewhat lower than the intended once a week (median (range): frequency per month: COPCA 3.0 (1.8–4.0); typical infant physiotherapy 2.5 (1.3–4.3), p = 0.009), due to holidays, illness and logistic factors.
Measurements
Primary outcome of the LEARN2MOVE 0-2 study is the Infant Motor Profile [Citation25], and power calculation was also based on the Infant Motor Profile, described in our accompanying paper [Citation21]. The current paper addresses family and infant outcomes measured by questionnaires and structured interviews. They were assessed at the infant’s home at baseline (T0), halfway the intervention (after 6 months, T2) and at the end of the intervention (after one year, T3). At the age of 21 months CA (T4), absence or presence of CP was based on fulfilling the criteria for a neurological syndrome (abnormalities in posture and movement, muscle tone and reflexes) according to the Touwen Infant Neurological Examination [Citation26,Citation27]. In case of CP, the severity was classified with the Gross Motor Function Classification System (GMFCS) [Citation28]. The latter two assessments are reliable and valid instruments [Citation27,Citation28].
Assessors were blinded for type of intervention, caregivers were asked not to inform them. Therapists and caregivers were not blinded for the type of intervention.
Family outcome
Main family outcome was the Family Empowerment Scale (FES) [Citation29], a questionnaire measuring empowerment in families with children with developmental problems. The original questionnaire consists of three subscales: (1) empowerment in the family system, (2) empowerment in the service system, and (3) parents’ involvement in the community. The first two subscales were translated into Dutch for the LEARN2MOVE 0-2 study [Citation30] and together with their total score, they were used as measures of family empowerment. The psychometric properties of the original FES are adequate [Citation29], for the Dutch version they have only been evaluated partially [Citation30].
Caregivers’ stress was measured by the Nijmeegse Ouderlijke Stress Index questionnaire, short version (NOSI-K) [Citation31], based on the Parenting Stress Index [Citation32]. Originally, the NOSI was designed for parents of children between 2 and 13 years, with good psychometric properties [Citation31]. Application of the NOSI-K at younger ages indicated proper function (Cronbach’s alpha 0.92) [Citation33,Citation34].
Coping strategies of caregivers were measured by the reliable and valid Utrechtse Coping List [Citation35,Citation36]. This questionnaire asks about general coping mechanisms and strategies. It results in scores on seven different scales of coping: active coping, palliative coping, avoiding, social support seeking, depressive coping, expression of negative emotion, or comforting ideas.
Infant outcome: activities and participation
To measure infant functional outcome we interviewed parents with the structured Dutch version of the Pediatric Evaluation of Disability Index (PEDI) [Citation37,Citation38]. The PEDI results in a total score and three subscores: self-care, mobility, and social function. It can be applied in children with CP from 6 months until 7 years [Citation38]. The PEDI-interview was combined with the Vineland Adaptive Behavior Scales (VABS), Dutch version, an interview about the functional status of communication, daily living skills and socialization [Citation39,Citation40] . The VABS can be used for children under 18 years. Both the PEDI a VABS have sufficient reliability and validity in children with CP [Citation39–41].
Quality of life
Quality of life was measured with the Infant and Toddler Quality of Life Questionnaire (ITQOL), a by proxy instrument to assess health-related quality of life in young children [Citation42,Citation43]. The ITQOL consists of child and parental concepts. Child concepts are: physical abilities, growth and development, bodily pain/discomfort, temperament and moods, general health perceptions; and if the infant is older than one year also: behavior, getting along with others, and change in health. Parent concepts are: impact emotional, impact time and family cohesion. The ITQOL has a good reliability and validity [Citation42,Citation43].
Caregivers quality of life was measured by a short questionnaire (CBS-list Quality of Life), consisting of two questions about how happy and satisfied caregivers were in the last month (on a 7-point Likert scale) and a visual analogue scale to assess quality of life. The questionnaire is based on a questionnaire used in the Netherlands by the central office of national statistics, with sufficient psychometric properties (Centraal Bureau voor de Statistiek (Statistics Netherlands), http://statline.cbs.nl/StatWeb) [Citation44,Citation45].
Process analysis of physical therapy intervention sessions
Contents of physiotherapy sessions after 1 and 6 months of intervention were video-recorded and analysed, according to the Groningen Observation Protocol 2.0 [Citation15]. Percentages of time spent on specific actions were scored within five main categories: neuromotor actions, educational actions, communication, position, and situation. We reduced the resulting data by performing a factor analysis (principal axis factoring with an Oblimin rotation). The factor analysis resulted in three factors: (1) NeuroDevelopmental Treatment versus COPCA-factor, a dimension reflecting the diametrically opposed core elements of NeuroDevelopmental Treatment (hands-on techniques and training) and COPCA (coaching and challenging self-produced motor activities); (2) non-directive communication and self-produced motor behavior; and (3) directive communication and training. Details of the process and factor analysis are described in our accompanying paper [Citation21].
Data analyses
Statistical univariate analyses were performed with SPSS Statistics for Windows, version 21 (Armonk NY: IBM Corp. released 2012 ) [Citation46]. We compared family and infant outcomes in the COPCA and typical infant physiotherapy groups at baseline, and after 6 and 12 months of intervention with non-parametric Mann Whitney U-tests, because of the non-normal distributions. We also compared outcome before the start and at the end of intervention (after 12 months), with Wilcoxon-signed-rank tests for dependent variables. We considered p values below 0.01 as statistically significant. For statistically significant results, Hodges Lehman estimates of the differences of the median (HL) with 95% confidence intervals (95%-CI) were calculated.
To study associations between contents of physiotherapy and the main family and infant outcomes (FES and PEDI) over time, longitudinal multilevel analyses were performed with linear and non-linear mixed-effect models (nlme) library in R version 3.3.1 [Citation47]. Potential longitudinal differential effects of COPCA and typical infant physiotherapy on the FES and PEDI were studied, taking into account the age (in corrected months) and possibly confounding factors (gestational age, level of parental education, and presence of cystic PVL (a major predictor of CP)) [Citation1], as these factors are known to influence outcome [Citation1,Citation16,Citation48]. Subject-specific time profiles per infant were described with linear mixed-effects models, taking into account correlation between observations from the same infant. We first tested possible effects over time of intervention (COPCA versus typical infant physiotherapy), taking into account possible interaction effects of intervention with age. In these analyses we did not use measurement moment as indicator of time but CA in months (and its square), to get the best model fit and avoid introducing error by neglecting the unstructured nature of the data. We repeated these analyses for each of the outcome variables in a similar way for the three factors describing physiotherapy (1= NeuroDevelopmental Treatment versus COPCA; 2 = non-directive communication; 3 = directive communication), using similar models for each outcome and again, a priori adjusted for the selected covariates.
To study relationships between physical impairment and family outcome, we compared family outcome for infants who developed CP with those who did not, using Mann Whitney U-tests. Moreover, we studied the influence of severity of motor impairment on family outcome, by correlating ordinal GMFCS-levels with outcome, by using Spearman rank correlation.
Results
Participants
Of the 43 included infants (n = 23 COPCA, n = 20 typical infant physiotherapy), four infants were lost to follow-up, all from the typical infant physiotherapy group (), due to study burden (n = 3) or maternal illness (n = 1). We collected interviews of the remaining participants from all of them except one (1 VABS at T3, due to family’s time constraints). Questionnaires were not filled in by all caregivers, resulting in lower numbers of collected questionnaires than interviews (). Reasons were additional study burden in families already involved in a large burden of care and time constraints.
Figure 1. Flow diagram. CBS-list QoL: Centraal Bureau voor de Statistiek list Quality of Life; COCPA: Coping with and caring for infants with special needs: a family centred programme; FES: Family Empowerment Scale; ITQOL: Infant & Toddler Quality of Life Questionnaire; NOSI-K: Nijmeegse Ouderlijke Stress Index, shortened version; PEDI: Pediatric Evaluation of Disability Index; TIP: Typical Infant Physiotherapy; UCL: Utrechtse Coping List; VABS: Vineland Adaptive Behavior Scales.
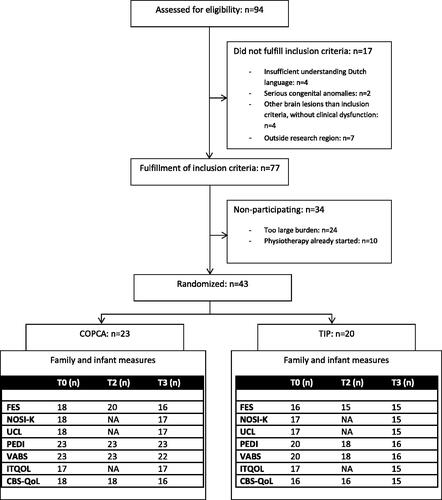
Baseline characteristics of caregivers and infants in both interventions were comparable. At the end of the study, about half (54%) of the infants was diagnosed with CP, a proportion that was similar in the two intervention groups ().
Table 1. Baseline characteristics and outcome cerebral palsy.
Family outcome – empowerment, stress, and coping
Between-group comparisons indicated that FES, coping mechanisms (Utrechtse Coping List), and parental stress (NOSI-K) scores in the two intervention groups were similar throughout the intervention period (). Also, the multilevel analyses showed that the effect of COPCA and typical infant physiotherapy on the main family outcome (FES) was similar (). We repeated the multilevel analyses with the three factors describing the interventional details of the physiotherapy actions (). Factor 1 was associated with the total FES score, indicating that less time spent with the NeuroDevelopmental Treatment-approach and more time spent with the COPCA-approach was associated with better FES scores ().
Table 2. Family outcome: empowerment, stress, coping, and quality of life.
Table 3. Longitudinal analyses, using linear mixed-effect models.
Table 4. Longitudinal analyses, using linear mixed-effect models.
and show the results of the linear mixed-effects models with random intercept (all models). In , effects of intervention on outcome are shown. In , effects of interventional elements, measured by factors 1, 2, and 3, are shown. Besides the effects of intervention (3) and interventional elements (4) on outcome, covariates statistically significant contributing to outcome are shown. No significant effects of caregivers’ educational level, gestational age or interaction effects for intervention with both age and cystic periventricular leukomalacia were found (data not shown in the tables).
Infant’s activities and participation
At all measurement moments functional outcome, measured by the PEDI and the VABS, was similar in the infants who had received COPCA or typical infant physiotherapy (). In both intervention groups, the PEDI- and VABS-scores increased significantly over time. Longitudinal multilevel analyses showed a similar effect of COPCA and typical infant physiotherapy on our main functional outcome, the PEDI, and no associations between interventional elements and the PEDI. Also these analyses indicated that PEDI-scores increased with age; moreover they revealed that cystic periventricular leukomalacia was negatively associated with PEDI-scores ( and ).
Table 5. Infant outcome: activities, participation, and quality of life.
Infant’s and family’s quality of life
Quality of life scores, measured by the ITQOL at baseline and after 12 months, were similar in the two intervention groups. However, within the COPCA-group some ITQOL domain scores changed significantly over time: scores on the child concept “General Health Perceptions” (i.e., perceptions of current, past, and future health) increased (T0: 59 (32–82); T3:77 (48–98); p = 0.003; HL: 15.9 (95%CI: 4.5–27.3)) (). This increase indicates that caregivers were more satisfied about the general health of their infants at the end of the intervention than before the intervention had started. In the parent concepts of the ITQOL, two other significant changes over time were present in the COPCA-group: the scores on “Impact emotional” (amount of worry experienced by parent due to child’s eating/sleeping habits, physical and emotional well-being, learning abilities, temperament, behavior, and ability to interact with others in an age-appropriate manner) and “Impact time” (amount of time limitations experienced by parent (time for his/her own needs) due to child's eating/sleeping habits, physical and emotional well-being, learning abilities, temperament, behavior, and ability to interact with others in an age-appropriate manner) increased significantly (Impact emotional: T0: 88 (39–100); T3: 96 (79–100); p = 0.005; HL 8.3 (95%CI 3.6–12.5); Impact time: T0: 88 (44–100); T3: 100 (71–100); p = 0.005; HL 9.5 (95%CI 4.8–19.7)) (). These increases imply that caregivers felt less emotionally worried and less restricted in time at the end of the intervention period than before the intervention had started. In contrast, in the families who had received typical infant physiotherapy, the ITQOL-scores were stable over time, both for child and parent concepts ( and ).
Caregivers’ quality of life, measured by the short CBS-list questionnaire, was similar in the two intervention groups throughout the intervention period (). Yet, in the COPCA-group caregivers’ quality of life increased significantly over time (T0: 8.1 (5.0–10.0); T3: 8.9 (6.8–10.0); p = 0.004; HL 0.7 (95%CI 0.0–1.3)) (). In the typical infant physiotherapy-group, quality of life scores did not change over time (T0: 8.3 (5.4–9.1); T3: 8.3 (6.1–10.0); p = 0.799; HL 0.11 (−0.7–1.0)).
Physical impairment and family outcome
Family outcome was similar in families with infants who developed CP and in families with infants who did not develop CP (data not shown). In addition, severity of motor impairment, measured by the GMFCS, was not associated with family outcome.
Discussion
The randomized controlled trial indicated that family outcome and the infant’s functional outcome (activities and participation) in the COPCA and typical infant physiotherapy groups were similar. However, a too small sample size resulted in underpowering of our study, so it is not possible to draw clear conclusions [Citation21]. After analysing contents of intervention, family empowerment was positively associated with COPCA-related interventional elements. Within-group analyses indicated that quality of life increased over time in families who had received COPCA-intervention, but not in the typical infant physiotherapy families. Family outcome was not related to the severity of the infant’s motor impairment.
The COPCA-related intervention elements that were associated with better family empowerment consisted of caregiver coaching and challenging the infant to self-produced motor behavior. Coaching is one of COPCA’s key components, aiming to empower caregivers in making their own decisions, both within their own family system and in the health care system [Citation18,Citation19]. The positive association between COPCA-related actions and family empowerment may be the result of an effect of coaching over time. This idea is supported by a previous study that suggested that coaching in early intervention is associated with long-term behavioral changes in caregiver behavior [Citation49]. Empowering caregivers aims to promote a sense of mastery over situations, which is positively related to psychological health of caregivers [Citation5] and may influence caregivers’ health and well-being on the longer term. Therefore, coaching and empowering may have been the mediators of the changes in quality of life over time, which is in accordance with the literature [Citation50]. In the families who had received COPCA overall quality of life increased, with less emotional worries and feeling less restricted in time, and more positive perceptions about growth and development of their child. Empowerment and better quality of life may positively influence parent–child interaction and therewith, in the longer term, child development [Citation9,Citation51]. While we found changes in caregivers’ quality of life during the intervention, we did not find changes in coping strategies or parental stress. It is conceivable that coping strategies are relatively stable personal characteristics (“traits”) and therefore less sensitive to change. The absence of differences in experienced stress as measured by the NOSI-K is more remarkable, as we did find that caregivers felt less emotionally worried and less restricted in time. However, the NOSI-K measures parental stress more generally, by addressing views and thoughts about the child’s growing up, expectations, child behavior, and parenting, which can all be relatively stable over time and therefore also less sensitive to change. Another explanation may be that the NOSI-K has been designed for caregivers of children above two years, although it has been used also in younger populations [Citation31,Citation32,Citation52].
Regarding infants’ activities and participation, we found – not surprisingly – that infants were more engaged in ambulatory, social, daily life, communication, and self-care activities over time. These changes most probably are related to developmental changes over age. The increase in activities and participation was similar in the two intervention groups. This is in contrast to our hypothesis that COPCA would be associated with more involvement in activities and participation than typical infant physiotherapy, because COPCA aims to encourage the infant to find adaptive motor strategies throughout daily life activities. However, also in standard physiotherapy a functional approach has been increasingly implemented [Citation13]. Moreover, the similar infant neuromotor, cognitive, and behavioral outcome in both intervention groups [Citation21] may have resulted in similar abilities to engage in activities and participation. Infants with some motor abilities may have a natural drive to use them [Citation50], to discover the world around them, independent of intervention.
Family empowerment, coping, stress, and quality of life were not associated with the diagnosis CP or the severity of motor impairment. Our findings are in line with the literature on families with older children with disabilities, which describes that other factors, such as behavioral factors, cognitive problems, and burden of care, usually contribute more to quality of life and parental well-being than the child’s physical impairment [Citation5,Citation24].
Strengths of our study are in the first place the broad evaluation of both family and infant. It furnished opportunities to relate infant and family outcome to each other and investigate mediating factors. However, such a large battery of measurement instruments has also its reverse: study burden increases, and questionnaires which had to be filled in by the caregivers, were not always completed (). Therefore, the numbers of collected questionnaires were lower than for the infant neuromotor measures or caregiver interviews. This may have resulted in a selection bias, i.e., that only caregivers who had enough time and energy filled in the questionnaires; this may have influenced the results in a positive way, which may be shown by the relatively high overall score on quality of life (median above 8). However, both in COPCA and in typical infant physiotherapy we missed questionnaires and therefore, this bias may have occurred in both groups. A second strength of our study is the longitudinal study design, allowing for longitudinal multilevel analyses, which are less sensitive to missing data. Another strength is the combined approach of the randomized controlled trial design with a detailed process analysis of the contents of intervention, to overcome the heterogeneous character of physiotherapy and detect working elements within interventions. A certain limitation of our study is the small sample size, which led to underpowering, due to selective attrition in the typical infant physiotherapy group [Citation21]. It raises the question about what is acceptable to ask from families for research purposes. What is acceptable for parents seems to be related to what parents perceive as added value, together with how overloaded families already are. It is important to realize as a researcher what will be asked from already busy families and to choose measures carefully, to minimize study participation burden and the risk of drop out. Another limitation is that not all measurements are appropriate for such a young age group. The NOSI-K for example is originally meant to be used in children over two years of age, the ITQOL contains elements that can be used only after one year of age and the PEDI is designed to be used from six months of age onwards. However, at the onset of the study no better alternatives were available.
In conclusion, the present study showed that COPCA and typical infant physiotherapy intervention in infants at very high risk of CP have a similar effect on family and the child’s functional outcome. However, when we focussed more on the details, we found that COPCA’s coaching approach was associated with a better family empowerment. The results of the study underscore the importance of family involvement and empowerment in paediatric physiotherapy. Quality of life increased over time in the COPCA-families, which may have been mediated by more empowered families. It is conceivable that a better quality of life may positively influence caregivers’ health, parent–child interaction, and eventually child outcome at the long term. Fortunately, family-centred services have received increasing attention in the last decades and professionals have an open attitude to change [Citation14,Citation52]. However, we are not yet at the stage that it is obvious that professionals and caregivers create equal partnerships [Citation15]. Therefore, we have to be aware of potential differences between willing to change and real change in practice [Citation52] and also of the fact that it takes time to implement changes. In future research, we have to increase knowledge about working elements within early intervention to be able to combine them to create a mix of active ingredients, which possibly should be tailored to the needs of infant and family. A mix of active ingredients paves the way for an effective, evidence based, comprehensive type of early intervention, to achieve optimal infant and family function.
Acknowledgments
We are grateful to the infants and their families for participation in the LEARN2MOVE 0–2 years study. The L2M0–2 study is part of the Dutch national LEARN2MOVE research programme. The following members of the *L2M0–2 study group contributed to this study, in the form of including infants for the study or collecting data:
University of Groningen, Department of Special Needs Education and Child Care, Groningen: C. Vlaskamp; University Medical Center Groningen, Department of Pediatrics, division neonatology: M. Boeve, A.F. Bos, H.J. ter Horst, C.V. Hulzebos, E.W.M. Kooi, E.F. Stremmelaar; University Medical Center Groningen, Department of Neurology, division of Child Neurology: M. Boon, O.F. Brouwer, J.M. Fock, R.J. Lunsing, D. Sival; Martini Ziekenhuis Groningen: H.A. van Dijk, W.B. Geven, H.J. Waalkens, M.J. Wiersma-Zweens; Ziekenhuis Nij Smellinghe Drachten/Revalidatie Friesland: W.A. van Asselt, C. Peer, M. Wilsterman; Gelre Ziekenhuis Zutphen: F.P.J. Dikken; Vrije Universiteit Medisch Centrum Amsterdam: J.G. Becher, S.R.D. van der Schoor, R.J. Vermeulen (MUMC + Maastricht), I.A. Zonnenberg; Isala Zwolle: J. Bekhof, C. Bunkers, J. Cornelissen, L.J.M. Groot-Jebbink, E. d’Haens, M.A.C. Hemels, R. van der Lee, R.A. van Lingen, S.M. Mulder-de Tollenaer, O.F. Norbruis, J.M.E. Quack, M. de Rooij, H.L.M. van Straaten, D.C. Vijlbrief; Medisch Spectrum Twente Enschede: A.G. Kaspers; Ziekenhuisgroep Twente Almelo/Hengelo: D.S.J. van Bommel-Slee, R.S. Rijlaarsdam, G. Shabo, M.L.J. Torringa; Isala Diaconessenhuis Meppel: E. Maza; Spaarne Ziekenhuis Hoofddorp: A. Baauw, J. Christenhuis, H. Kiezenbrink, P. de Winter; Medisch Centrum Leeuwarden: R. Boontje, N.S.K. de Vries, T. de Vries; De Tjongerschans Heerenveen: S.M. van Dorth, W.F. Heikens, A.I. Kistemaker, T. Wiersma; physical therapists: I.K. de Boer, J. Geltink, M. Hijlkema; researchers, students and interns: L.C. van Balen, M.J. Coenraads, L.J. Dijkstra, I. Ebbers-Dekkers, S.J. Hooijsma, K.S.J. Post, R.F. Toonen. The Netherlands.
Disclosure statement
No Potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Hielkema T, Hadders-Algra M. Motor and cognitive outcome after specific early lesions of the brain – a systematic review. Dev Med Child Neurol. 2016;58:46–52.
- World Health Organization. International classification of functioning, disability, and health: children & youth version. ICF-CY. Geneva: World Health Organization; 2007.
- Beckung E, Hagberg G. Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Dev Med Child Neurol. 2002;44:309–316.
- Larson E. Identifying indicators of well-being for caregivers of children with disabilities. Occup Ther Int. 2010;17:29–39.
- Raina P, O'Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115:e626–e636.
- Majnemer A, Shevell M, Law M, et al. Indicators of distress in families of children with cerebral palsy. Disabil Rehabil. 2012;34:1202–1207.
- Brehaut JC, Kohen DE, Raina P, et al. The health of primary caregivers of children with cerebral palsy: how does it compare with that of other Canadian caregivers? Pediatrics. 2004;114:e182–e191.
- Greco V, Roger D. Uncertainty, stress, and health. Pers Individ Dif. 2003;34:1057–1068.
- Guillamón N, Nieto R, Pousada M, et al. Quality of life and mental health among parents of children with cerebral palsy: the influence of self-efficacy and coping strategies. J Clin Nurs. 2013;22:1579–1590.
- Beardslee WR, Gladstone TR, Wright EJ, et al. A family-based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112:e119–e131.
- Barlow JH, Ellard DR. The psychosocial well-being of children with chronic disease, their parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2006;32:19–31.
- Kandel I, Merrick J. The child with a disability: parental acceptance, management and coping. ScientificWorldJournal. 2007;7:1799–1809.
- Law M, Darrah J. Emerging therapy approaches: an emphasis on function. J Child Neurol. 2014;29:1101–1107.
- Palisano RJ, Snider LM, Orlin MN. Recent advances in physical and occupational therapy for children with cerebral palsy. Semin Pediatr Neurol. 2004;11:66–77.
- Hielkema T, Toonen RF, Hooijsma SJ, et al. Changes in the content of pediatric physical therapy for infants: a quantitative, observational study. Phys Occup Ther Pediatr. 2017;21:1–32. Epub ahead of print.
- Spittle A, Orton J, Anderson PJ, et al. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. 2015;12:CD005495.
- Hielkema T, Hamer EG, Reinders-Messelink HA, et al. LEARN 2 MOVE 0-2 years: effects of a new intervention program in infants at very high risk for cerebral palsy: a randomized controlled trial. BMC Pediatr. 2010;10:76.
- Dirks T, Blauw-Hospers CH, Hulshof LJ, et al. Differences between the family-centered "COPCA" program and traditional infant physical therapy based on neurodevelopmental treatment principles. Phys Ther. 2011;91:1303–1322.
- Akhbari Ziegler S, Dirks T, Hadders-Algra M. Coaching in early physical therapy intervention: the COPCA program as an example of translation of theory into practice. Disabil Rehabil. 2018;16:19.
- Howle JM. Neuro-developmental treatment approach: theoretical foundations and principles of clinical practice. Laguna Beach: NeuroDevelopmental Treatment Association; 2002.
- Hielkema T, Hamer EG, Boxum AG, et al. LEARN2MOVE0-2 years, an early intervention trial for infants at very high risk of cerebral palsy: neuromotor, cognitive and behavioral outcome. Accompanying paper, submitted to Disability and Rehabilitation.
- Blauw-Hospers CH, Dirks T, Hulshof LJ, et al. Pediatric physical therapy in infancy: from nightmare to dream? A two-arm randomized trial. Phys Ther. 2011;91:1323–1338.
- Hielkema T, Blauw-Hospers CH, Dirks T, et al. Does physiotherapeutic intervention affect motor outcome in high-risk infants? An approach combining a randomized controlled trial and process evaluation. Dev Med Child Neurol. 2011;53:e8–15.
- Parkes J, Caravale B, Marcelli M, et al. Parenting stress and children with cerebral palsy: a European cross-sectional survey. Dev Med Child Neurol. 2011;53:815–821.
- Heineman KR, Bos AF, Hadders-Algra M. The Infant Motor Profile: a standardized and qualitative method to assess motor behaviour in infancy. Dev Med Child Neurol. 2008;50:275–282.
- Touwen BCL. Neurological development in infancy. Clinics in developmental medicine No. 58. London: Heinemann Medical Publications; 1976.
- Hadders-Algra M, Heineman KR, Bos AF, et al. The assessment of minor neurological dysfunction in infancy using the Touwen Infant Neurological Examination: strengths and limitations. Dev Med Child Neurol. 2010;52:87–92.
- Palisano R, Rosenbaum P, Bartlett D, et al. GMFCS—E &R. Hamilton. Canada: CanChild Centre for Childhood Disability Research, McMaster University; 2007.
- Koren PE, DeChillo N, Friesen BJ. Measuring empowerment in families whose children have emotional disabilities. A brief questionnaire. Rehab Psychol. 1992;37:305–321.
- Kruijsen-Terpstra AJ, Ketelaar M, Verschuren O, et al. Efficacy of three therapy approaches in preschool children with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2016;58:758–766.
- De Brock A, Vermulst AA, Gerris JRM, et al. NOSI-K: Nijmeegse ouderlijke stress index. Lisse: Zwets & Zeitlinger; 1992.
- Abidin RR. Parenting Stress Index (PSI). Charlottesville (VA): Pediatric Psychology Press; 1990.
- Pal SM, Maguire CM, Bruil J, et al. Very pre‐term infants' behaviour at 1 and 2 years of age and parental stress following basic developmental care. Br J Dev Psychol. 2008;26:103–115.
- Van der Veek SM, Kraaij V, Garnefski N. Cognitive coping strategies and stress in parents of children with Down syndrome: a prospective study. Intellect Dev Disabil. 2009;47:295–306.
- Schreurs PJG, Van de Willige G, Tellegen B, et al. De Utrechtse Coping Lijst: UCL-handleiding. Lisse: Swets & Zeitlinger; 1988.
- Sanderman R, Ormel J. De Utrechtse Coping Lijst (UCL). validiteit en betrouwbaarheid. Gedrag Gezondheid. 1992;20:32–37.
- Haley S, Coster W, Ludlow L, et al. Pediatric Evaluation of Disability Inventory (PEDI). Development, standardization and administration: manual. Boston (MA): Boston University; 1992.
- Custers JW, Wassenberg-Severijnen JE, Van der Net J, et al. Dutch adaptation and content validity of the 'Pediatric Evaluation Of Disability Inventory (PEDI)'. Disabil Rehabil. 2002;24:250–258.
- Wassenberg-Severijnen JE, Custers JW, Hox JJ, et al. Reliability of the Dutch pediatric evaluation of disability inventory (PEDI). Clin Rehabil. 2003;17:457–462.
- Sparrow SS, Balla DA, Cicchetti DV. The Vineland adaptive behavior scales. Circle Pines (MN): American Guidance Service Inc.; 1984.
- van Berckelaer-Onnes IA, Buysse WH, Dijkxhoorn YM, et al. Dutch translation of the Vineland adaptive behavior scales. Leiden: University of Leiden; 1997.
- Landgraf JM. The Infant and Toddler Child Health Questionnaire: conceptual framework, logic content, and preliminary psychometric results. Boston (MA): Health Act; 1994.
- Raat H, Landgraf JM, Oostenbrink R, et al. Reliability and validity of the Infant and Toddler Quality of Life Questionnaire (ITQOL) in a general population and respiratory disease sample. Qual Life Res. 2007;16:445–460.
- Van Beuningen J, Van der Houwen K, Moonen L. Measuring well-being. An analysis of different response scales. Discussion Paper. Den Haag/Heerlen: CBS; 2014.
- IBM Corp. SPSS statistics for windows, Version 21.0. Armonk, NY: IBM Corp; 2012.
- R Development Core Team R. A language and environment for statistical computing. R Vienna, Austria: Foundation for Statistical Computing; 2008. ISBN 3-900051-07-0. Available from http://www.R-project.org
- Himpens E, Oostra A, Franki I, et al. Predictability of cerebral palsy in a high-risk NICU population. Early Hum Dev. 2010;86:413–417.
- Hamer EG, Hielkema T, Bos AF, et al. Effect of early intervention on functional outcome at school age: follow-up and process evaluation of a randomised controlled trial in infants at risk. Early Hum Dev. 2017;106-107:67–74.
- Graves KN, Shelton TL. Family empowerment as a mediator between family-centered systems of care and changes in child functioning: identifying an important mechanism of change. J Child Fam Stud. 2007;16:556–566.
- Nachshen JS, Minnes P. Empowerment in parents of school-aged children with and without developmental disabilities. J Intellect Disabil Res. 2005;49:889–904.
- Mayes LC, Zigler E. An observational study of the affective concomitants of mastery in infants. J Child Psychol Psychiatry. 1992;33:659–667.
- Jette DU, Bacon K, Batty C, et al. Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003;83:786–805.
