Abstract
Introduction
The main idea underlying this paper is that impairments such as deafness are particularly relevant to the extent that they lead to deprivation of capability. Likewise, the impact of healthcare services such as cochlear implants and subsequent rehabilitation can best be inferred from the extent that they protect or restore capability of those affected.
Methods
To explore children’s post-implant capabilities, we tested two newly developed digital, adaptive child self-report and parent-report questionnaires in 19 deaf children (aged 8–12 years) and their parents during rehabilitation, as well as in 23 age peers with normal hearing.
Results
Despite the impressive speech-language results that were recorded with cochlear implants, the post-implant capabilities of the deaf children we evaluated differed from those of their hearing peers, with the cochlear implant group appearing particularly disadvantaged in areas such as accessing information, communication, social participation, and participation in school.
Conclusion
Deaf children with cochlear implants who are performing well on linguistic and auditory tests can still experience serious limitations in desired functioning. Our findings suggest that a capability approach may reveal aspects of what is being achieved through rehabilitation that might otherwise remain unnoticed, and that could help to further improve the well-being of our patients.
Overall, children with cochlear implants appeared disadvantaged in certain capability areas, like accessing information, communication, social participation, and participation in school.
It may be worthwhile to also ascertain capabilities in these children, representing a domain not covered by clinical measures, tapping directly into areas that are valuable to the patient.
IMPLICATIONS FOR REHABILITATION
Introduction
Rehabilitation is about helping (former) patients to find or regain a mode and level of functioning that enables them to lead a gratifying and satisfying life. This normative concept implies that the patient’s aspirations are defined, taking into account his or her personal context, potential, motivation, and interests. A host of instruments, questionnaires, and scales have been developed to assess functioning and changes therein during rehabilitation [Citation1]. In the study presented here, we will be exploring capability as a potentially useful concept to assist caregivers and deaf children in defining individual goals and in determining the associated achievements after cochlear implantation.
The concept of capability was developed by Nobel Prize laureate Amartya Sen as an alternative to utility for the measurement of human well-being [Citation2–4]. According to Sen, an individual’s well-being should be primarily gleaned from the real opportunities an individual has for being and doing the things he has reason to value [Citation5,Citation6]. Hence, capability extends beyond an individual’s actual functioning by asking what range of valued activities and modes of being are available to him. The idea of capability then differs from other available models and instruments in the sense that it aims to establish the degree of freedom a patient enjoys or lacks in choosing his or her own way of life. In other words, to what extent does a patient’s life reflect own choices and to what extent is it determined by factors inherent to the individual patient and his/her social and physical environment? Accordingly, capability is conceived as a function of the resources that are available to an individual and his or her ability to convert those resources into something that represents value to him. Among such conversion factors are an individual’s social and physical conditions, as well as his own physical, mental, and social competencies [Citation7].
Although the concept has attracted extensive interest from a wide range of disciplines globally, its operationalisation is still considered a challenge [Citation7,Citation8]. Key issues here include (1) the delineation of what constitute, in a particular context, valuable activities and modes of being, (2) the lack of methods to establish whether someone might be capable of being or doing something, especially if that person has, for one reason or another, refrained from entering in certain activities or modes of being so far, and (3): the identification of the resources and conversion factors that are critical to the enactment of such activities or attainment of the desired mode of being.
In this paper, we will present the first results obtained with a child- and parent-report questionnaire that was specifically developed to explore the capability of deaf children wearing a cochlear implant. In the Western world, the majority of the prelingually deaf children (i.e., those with an onset of deafness before the age of (4) receive such an implant [Citation9]. In terms of their post-implant performance on hearing and speech tests, these children can generally achieve levels that are close to those of their normal-hearing peers [Citation10–15]. Also in terms of self-reported quality of life, their scores tend not to differ from those obtained in their peers [Citation16–19]. However, performance scores on standardised hearing and speech tests may merely predict poor performance in day-to-day conditions (e.g., at school, in public spaces, at home), while self-reported quality of life measures may be confounded by the response shift phenomenon, i.e., the respondents’ adaptation to their (new) living conditions [Citation2,Citation3,Citation20]. The assessment of capability could then reveal whether, in spite of the cochlear implant and subsequent rehabilitation, children still experience constraints in pursuing their aspirations in terms of achievements and modes of being. If this proves to be the case, possible underlying causes can be explored, differentiating between the lack of requisite resources and factors impeding their conversion, potentially offering ways to remediate the situation.
After detailing our study populations, we will briefly describe the development of our post-implantation capability questionnaires, after which we will compare their outcomes to the performance results obtained with standardised hearing and speech tests.
Materials and methods
Participants
We invited 19 deaf children with cochlear implants (consecutive sampling) in the ages between 8 and 12 years attending grades 3–6 of a local mainstream primary school or a regional primary school for the deaf) and their parent(s)/caregiver(s) to participate in the study during their annual follow-up at the out-patient clinic of our academic hospital. We recruited 23 age-matched normal-hearing children from local mainstream primary schools. lists the demographic and clinical characteristics for the two study groups.
Table 1. Demographic characteristics of the children with cochlear implants and the age-matched normal-hearing controls.
Assessments
Capability
For our study we developed two digital, adaptive child and parent self-report questionnaires. “Types of doings and beings”, or functionings, that children in our particular age group living in developed countries might value were derived from the relevant literature [Citation15,Citation21–24], from conversations with parents of children with cochlear implants conducted at our clinic, and input from members of the cochlear implant team of our hospital. This resulted in nine domains: School participation, Information access, Relationship with parents, Social participation, Social skills, Communication, Assertiveness, Independence, and Psychological well-being. We initially formulated 40 items asking about functionings within each domain; this list was reduced to 22 by combining overlapping concepts. All 22 items are scored on a 3-point Likert scale, ranging from positive to negative. For each domain, the questionnaire starts by inquiring about the perceived state of affairs through a statement (e.g., “I participate in sports activities”). Depending on the answer, different questions are presented: in case of “true,” a question appears asking about any difficulties relating to performances with the topic. To distinguish between non-performance due to inability or different interests, the respondent is asked why performance is not possible, or why it is difficult. The parents independently complete the same questionnaire, giving their estimation of their child’s capability, where the phrasing of items is adapted to match the parental perspective. Note that it was only the parents of the children with a cochlear implant that completed this questionnaire since we were primarily interested to learn whether the ratings of the children with impaired hearing differed from their parents’ ratings. Concordance in the responses of the parent-child pairs was calculated using Cohen’s Kappa coefficients.
The children with cochlear implants and their parents completed the questionnaire separately during their annual appointment at the outpatient clinic or at home, while the normal-hearing children did so at school.
Depending on the responses, three capability levels were distinguished for each of the 22 domains: optimal capability (level A) in case of performance with little or no difficulty, moderate capability (level B) in case of difficulties in performing, to minimal/absent capability (level C) in case of non-performance and perceived inability to perform. shows the breakdown of the capability levels.
Table 2. Capability levels as defined based on response combinations.
Speech perception in noise
Speech-perception abilities in noise were assessed with the Bosman Dutch open-set identification test, containing consonant – vowel – consonant words (Bosman & Smoorenburg, 1995). Stimuli were presented via loudspeakers to prevent lip-reading in a sound-treated booth at a presentation intensity of 65 dB SPL with a 65 dB SPL noise level, resulting in a 0'db speech/noise ratio. Response consisted of the oral repetition of the presented word. Speech perception was quantified as the percentage of phonemes that was correctly repeated. The clinical norm score of 59% was used as the cut-off point [Citation25].
Word comprehension
Word comprehension was assessed with the Peabody Picture Vocabulary Test-III-NL (PPVT) [Citation26]. Stimuli consisted of words presented live by the experimenter with lip-reading being possible. The children were asked to identify the stimulus word from four pictures presented to them. Outcomes were expressed as correct words identified, where a minimum quotient score of 85 (one SD below average) was used as the cut-off threshold [Citation26].
Analyses
The capability levels (A – C) were determined per domain for each child. The differences in domain scores between the cochlear implant and the control group were tested for statistical significance using non-parametric Mann-Whitney U tests. We used chi-square tests to differentiate between the two conditions in terms of optimal (A) capability items. Correlations between capability levels and speech and hearing performance outcomes were assessed using non-parametric Spearman correlation tests. Internal consistency analysis was applied to test the coherence of the nine domains using SPSS, version 22. A p-level of 0.05 (two-sided) was considered statistically significant.
Ethical considerations
The Radboud University Medical Centre’s Committee on Research Involving Human Subjects (CMO) approved the study protocol (reference 2016–2845). Written informed consent was obtained from the children’s parents. The children were allowed to withdraw from the study at any point without them or their parents having to provide reasons for ending their participation.
Results
The distribution of the capability levels across the various domains for our two study groups is shown in .
Figure 1. Box plots of the percentage of items per capability level for the children with cochlear implants (CI) and the normal-hearing children (NH).
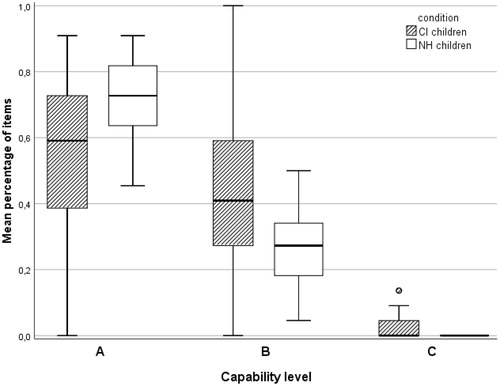
The cochlear implant group scored significantly less often within the optimal capability range (level A) than the control group (54%, SD = 25%, vs. 72%, SD = 12%, U = 121.5, p = 0.014), while the normal-hearing children were significantly less often categorised at level B (moderate capability) (27%, SD = 12%, vs. 44%, SD = 25%, U = 122.5, p = 0.015). No significant differences were observed between the ratings of the children with cochlear implants and their parents.
Of the 19 children with cochlear implants six were classified at capability level C for at least one item (vs. 3 of the 23 normal-hearing children). The internal consistency analysis revealed that the 22 items could be considered independent (Cronbach’s α <.5). Normal-hearing children reported significantly more optimal capabilities compared to children with cochlear implants in five of the 22 items, listed in .
Table 3. Results of chi-square tests and descriptive statistics for Capability Level per study group.
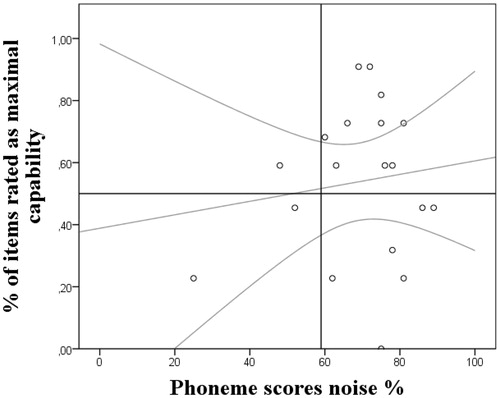
The mean percentage of phonemes the children with cochlear implants correctly repeated (speech perception in noise test) is 69% (SD = 15%). shows the relationships between these scores and the children’s optimal (level A) capabilities. The horizontal reference line divides the data into two equal parts, separating the children with less than half of their answers leading to optimal capabilities from those with more than half, where the vertical reference line separates the adequate from the poor performers based on the 59% cut-off threshold (clinical norm score) [Citation25].
Figure 2. Phoneme scores for the speech perception in noise test and the capabilities for the children with cochlear implants. The grey lines are regression lines and 95% confidence intervals; the vertical and horizontal reference lines indicate cut-off points for the two outcomes.
shows the associations between the capabilities and word comprehension results of the cochlear implant group, expressed as verbal comprehension quotients (M = 90, SD = 20). Deviating more than one standard deviation (15) from the test’s norm (100) is considered poor performance and indicated by the vertical reference line.
Figure 3. Word comprehension as expressed in the verbal comprehension quotient and the capabilities for the children with cochlear implants. The grey lines are regression lines and 95% confidence intervals; the vertical and horizontal reference lines indicate cut-off points for the two outcomes.
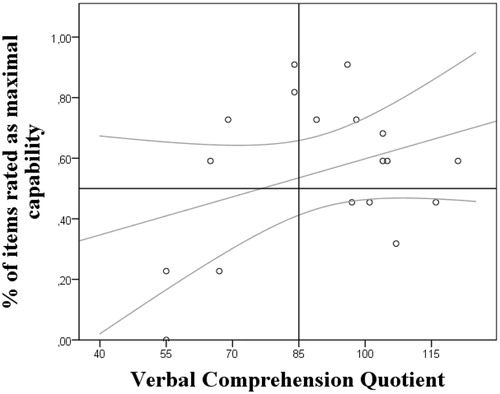
The children with good and sufficient verbal comprehension and phoneme performance (depicted in the two quadrants to the right-hand side of the vertical line) still differed widely in terms of capabilities, having the most problems with going out on their own, solving their own problems, and understanding the feelings of other children. More than half of the ratings of the four children depicted in the upper-left quadrant were classified as capability level A, specifically high degree of freedom from parents, having fun, and good relationship with their parents, while their performance on the clinical measures was insufficient.
Child-parent correlations
The overall agreement on child- and parent-reported capabilities (cochlear implant group only) was relatively low, with only seven of the 19 child-parent dyads showing significant agreement on all 22 items, with Cohen’s Kappa coefficients ranging from poor (κ = .16, p = 0.04) to fair agreement (κ = .63, p < 0.001).
Open questions
The children with cochlear implants reported significantly lower capability levels on five of the 22 items than their normal-hearing peers. presents a summary of their answers on the open questions (e.g., “Why is it difficult for you to achieve …”) of these five items. No significant differences were found on the remaining 17 items.
Table 4. Examples of capability constraints reported by children with cochlear implants.
Mention is made of difficulties hearing teachers or keeping up with the signs when sign language is used, with other factors including lack of vocabulary, difficulties speaking clearly and typing on a keyboard. Also, some environmental issues are mentioned, such as noise in the classroom and living far away from school and friends. Social problems that are reported include feeling ashamed when they need to ask for help, being bullied, or being nervous of other people’s reactions.
Discussion
A key question, in any rehabilitation context, is in what way and to what extent illnesses (acute or chronic) interfere with the daily lives of those directly affected, and how rehabilitation succeeds in remediating this. There are various approaches to assess disease-related impact and changes following interventions and rehabilitation, each with their own strengths and weaknesses. In the case of deaf children who have received a cochlear implant, speech perception (in noise) and verbal word comprehension are considered important parameters. However, using a child and parent version of an adaptive self-report questionnaire we explored the effects of cochlear implants on a wider range of capabilities of these children and our findings provide preliminary evidence that mentioned hearing-related measures are relatively poor proxies of the true impact of cochlear implants. Although we by no means wish to suggest that these conventional tests are not useful to monitor hearing-related changes, we do suggest that exploring other post-implant capabilities may provide valuable insights into the wider effects of the treatment and rehabilitation given that, even with significantly improved speech-language functions, we found the post-implant capabilities of the deaf children we assessed to still differ from those of their normal-hearing peers, with the cochlear implant group particularly lagging behind in domains such as accessing information, communication, social and in-school participation.
This is in contrast with results from studies on self-reported quality of life, suggesting that deaf children with cochlear implants are usually on a par with their normal hearing peers [Citation16–19,Citation27]. The difference might be explained by a differential impact of response shift, the general phenomenon of adjustments of humans to adverse conditions (including chronic illness or disability) over time [Citation28]. We would hypothesize that this phenomenon is manifest in particular when questionnaires are being used that query respondents about their experienced quality of life, such as the KIDSCREEN, KINDL and CHIP-CE [Citation29–31]. In contrast, in the present study, the questionnaire queries respondents about their assessment of their capability to perform valued tasks. We intend to explore this issue further, using methods that have been described in the literature for assessing response shift such as card sorting, the then-test, or idiographic assessment of personal goals [Citation32].
Our capability questionnaire helps members of the cochlear implant team and the children and their parents to identify problem areas that may still exist in spite of the child’s adequate performance on conventional measures, where the additional outcomes may prompt them to find causes and solutions for the child’s constrained capabilities. Conversely, it may be highly informative to explore the mechanisms underlying apparently adequate capabilities in spite of relatively poor hearing-related performance. Of course, the causes and remedy of (certain) discrepancies in assessment outcomes may be beyond the realm of clinical or ambulatory care, but in the interest of the child and the need to optimise care services, it seems sensible to include other than clinical factors that also warrant attention, even if this involves referrals to other remedial or (health)care services. The questionnaire that we have presented in this paper could support cochlear implant teams in their evaluations and shared decisions.
Clearly, the nature of the capability concept requires a different approach from cochlear implant team members as well as an instrument with relevant, explicitly phrased and adaptive questions. Firstly, agreement should be sought among cochlear implant team members, the children, their parents, and other stakeholders regarding the nature of the “doings and beings” that may be considered of value in age categories and individual contexts. Secondly, the focus should then be on whether the child would be able to achieve these given its personal circumstances. We opted to first inquire about the actual, self-perceived state of affairs and whether the child or parent saw any problems in the area at hand. Our reasoning, here, was that in case of engagement or experiences, capability is implied. In case no involvement or achievement was reported, we sought to determine whether this was due to the child having different interests or whether the child did take an interest but considered him/herself incapable of achieving the activity or state, which, evidently, would reflect a different type of constrained capability. In the former case, where the child shows little interest in an activity or state that is generally considered of value, the lack of capability will be of little significance to the child, while in the latter case, where it did aspire to the activity or state but reported failure to achieve it, remedial intervention may be considered.
At the group level, the deficits in capability involved the domains of accessing information, participating socially, and feeling independent as described by the children reporting non-participation/no experience in the topic that they did aspire to, while foreseeing difficulties should they try and engage in it. This information can help identify the daily-life problems after cochlear implantation and rehabilitation and inspire changes in the latter process. At the patient level, the proposed capability approach could help to explore opportunities to further a child’s capabilities in problem areas.
Limitations and future directions
Our findings are a first step towards the development of a child- and parent-report instrument that can help cochlear implant teams monitor how the capabilities of post-implant children develop during their rehabilitation. The differences in capability between the children with cochlear implants and normal-hearing peers it revealed, appear to support its discriminant validity as one could expect these groups to differ on these themes. Application of the questionnaire in a larger sample of cochlear implant patients is needed to test other hypotheses and uncover potential adaptations before we can confirm the scale’s reliability and (external) validity [Citation33].
Our inter-respondent reliability analysis showed poor agreement in the child and parental judgments, but this was to be expected since parents and children are known to vary in their perceptions of the quality of life of children learning to live with cochlear implants [Citation18,Citation19,Citation27]. Taking validity as a test of hypotheses [Citation33], we should base the premises on how we expect deaf children with cochlear implantss or any post-treatment patient from different socioecological backgrounds to score on such a capability instrument on the relevant literature and new empirical findings. We feel that the described approach as such is applicable in other rehabilitation contexts, where our questionnaire can help the various stakeholders to reflect on the types of capabilities (“doings and beings”) that could be relevant to assess in their specific settings. Additional data might also be derived from participatory observations, for instance, and from empirically surveying prerequisites for capability.
Conclusion
Capability testing provides a different lens through which to look at patients after they have received a health intervention and to gauge the benefits and problems they experience during their rehabilitation process. Basically, it allows us to see whether and how they succeed in finding new degrees of freedom to shape a life of their own choosing. This requires that we, beyond conventional clinical indices, also explicitly consider the kind of activities and states that they aspire to and reflect on whether and how these can become attainable for any specific group or individual patient to further improve their well-being.
Acknowledgements
The authors thank the parents and children for their participation in this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Karimi M, Brazier J, Basarir H. The capability approach: a critical review of its application in health economics. Value Health. 2016;19(6):795–799.
- Bellanca N, Biggeri M, Marchetta F. An extension of the capability approach: towards a theory of dis-capability. ALTER - European Journal of Disability Research/Revue Européenne de Recherche sur le. Handicap. 2011;5(3):158–176.
- Morris C. Measuring participation in childhood disability: how does the capability approach improve our understanding? Dev Med Child Neurol. 2009;51(2):92–94.
- Trani JF, Browne J, Kett M, et al. Access to health care, reproductive health and disability: a large scale survey in Sierra Leone. Soc Sci Med. 2011;73(10):1477–1489.
- Sen A. Equality of What? Cambridge (UK): Cambridge University Press; 1980.
- Sen A. Economics and health. Lancet. 1999;354:20–20.
- Robeyns I. Sen's capability approach and gender inequality: Selecting relevant capabilities. Fem Econ. 2003;9(2–3):61–92.
- Robeyns I. The Capability Approach: a theoretical survey. J Hum Dev. 2005;6(1):93–117.
- Petersen NK, Jorgensen AW, Ovesen T. Prevalence of various etiologies of hearing loss among cochlear implant recipients: Systematic review and meta-analysis. Int J Audiol. 2015;54(12):924–932.
- Niparko JK, Tobey EA, Thal DJ, et al. Spoken language development in children following cochlear implantation. JAMA. 2010;303(15):1498–1506.
- Boons T, De Raeve L, Langereis M, et al. Expressive vocabulary, morphology, syntax and narrative skills in profoundly deaf children after early cochlear implantation. Res Dev Disabil. 2013;34(6):2008–2022.
- Boons T, De Raeve L, Langereis M, et al. Narrative spoken language skills in severely hearing impaired school-aged children with cochlear implants. Res Dev Disabil. 2013;34(11):3833–3846.
- De Raeve L. A longitudinal study on auditory perception and speech intelligibility in deaf children implanted younger than 18 months in comparison to those implanted at later ages. Otol Neurotol. 2010;31(8):1261–1267.
- Peterson NR, Pisoni DB, Miyamoto RT. Cochlear implants and spoken language processing abilities: review and assessment of the literature. Restor Neurol Neuros. 2010;28(2):237–250.
- Vermeulen AM, van Bon W, Schreuder R, et al. Reading comprehension of deaf children with cochlear implants. J Deaf Stud Deaf Educ. 2007;12(3):283–302.
- Loy B, Warner-Czyz AD, Tong L, et al. The children speak: an examination of the quality of life of pediatric cochlear implant users. Otolaryngol Head Neck Surg. 2010;142(2):247–253.
- Meserole RL, Carson CM, Riley AW, et al. Assessment of health-related quality of life 6 years after childhood cochlear implantation. Qual Life Res. 2014;23(2):719–731.
- Razafimahefa-Raoelina T, Farinetti A, Nicollas R, et al. Self- and parental assessment of quality of life in child cochlear implant bearers. Eur Ann Otorhinolaryngol Head Neck Dis. 2016;133(1):31–35.
- Warner-Czyz AD, Loy B, Roland PS, et al. Parent versus child assessment of quality of life in children using cochlear implants. Int J Pediatr Otorhinolaryngol. 2009;73(10):1423–1429.
- Hart CS. How do aspirations matter? J Hum Dev Capabil. 2016;17(3):324–341.
- Kouwenberg M, Rieffe C, Theunissen SC, et al. Peer victimization experienced by children and adolescents who are deaf or hard of hearing. PLoS One. 2012;7(12):e52174.
- Schorr EA, Roth FP, Fox NA. Quality of life for children with cochlear implants: perceived benefits and problems and the perception of single words and emotional sounds. J Speech Lang Hear Res. 2009;52(1):141–152.
- De Raeve L, Vermeulen A, Snik A. Verbal cognition in deaf children using cochlear implants: Effect of unilateral and bilateral stimulation. Audiol Neurotol. 2015;20(4):261–266.
- Bat-Chava Y, Martin D, Kosciw JG. Longitudinal improvements in communication and socialization of deaf children with cochlear implants and hearing aids: evidence from parental reports. J Child Psychol Psychiat. 2005;46(12):1287–1296.
- Sparreboom M, Langereis MC, Snik AF, et al. Long-term outcomes on spatial hearing, speech recognition and receptive vocabulary after sequential bilateral cochlear implantation in children. Res Dev Disabil. 2014;36:328–337.
- Dunn LMD, Leota M. Peabody Picture Vocabulary Test-III-NL, Nederlandse versie door Liesbeth Schlichting. Amsterdam (Netherlands): Harcourt Assessment B.V.; 2005.
- Huber M. Health-related quality of life of Austrian children and adolescents with cochlear implants. Int J Pediatr Otorhinolaryngol. 2005 ;69(8):1089–1101.
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48(8):977–988.
- Riley AW, Forrest CB, Rebok GW, et al. The child report form of the CHIP-Child edition. Med Care. 2004;42(3):221–231.
- Ravens-Sieberer U, Gosch A, Rajmil L, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5(3):353–364.
- Bullinger M, Brütt AL, Erhart M, et al. Psychometric properties of the KINDL-R questionnaire: results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17(S1):125–132.
- Schwartz CE, Sprangers M. Methodological approaches for assessing response shift in longitudinal health-related quality-of-life research. Soc Sci Med. 1999;48(11):1531–1548.
- Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. 2nd ed. Oxford (UK); New York (NY): Oxford University Press; 1995.
