Abstract
Purpose
To explore the preferable way of use and design of a work ability prognosis support tool for insurance physicians (IPs) and labour experts (LEs), based on a prediction model for future changes in work ability among individuals applying for a work disability benefit.
Methods
We conducted three focus groups with professionals of the Dutch Social Security Institute (17 IPs and 7 LEs). Data were audio recorded and qualitatively analysed according to the main principles of thematic analysis.
Results
Clarity and ease of use were mentioned as important features of the tool. Most professionals preferred to make their own judgement during the work disability assessment interview with the claimant and afterwards verify their evaluation with the tool. Concerning preferences on the design of the tool, dividing work disability claimants into categories based on the outcome of the prediction model was experienced as the most straightforward and clear way of presenting the results. Professionals expected that this encourages them to use the tool and act accordingly.
Conclusions
The tool should be easy to access and interpret, to increase the chance that professionals will use it. This way it can optimally help professionals making accurate prognoses of future changes in work ability.
A work ability prognosis support tool based on a prediction model for changes in work ability at one-year follow-up can help occupational health professionals in making accurate prognosis of individuals applying for a work disability benefit.
To be used in occupational health practice, these tools should have a simple and easy-to-use design.
Graphical risk presentation can be used to provide intuitive meaning to numerical information and support users’ understanding.
Taking professionals’ preferences into account when developing these tools encourages professionals to use the tools and act accordingly.
Implications for rehabilitation
Background
Individuals who are unable to work due to a disease or disorder can apply for a work disability benefit. In most European countries, this covers both financial support to compensate loss of income, and interventions to support return to work [Citation1]. Insurance physicians (IPs) and labour experts (LEs) in the Netherlands conduct assessments of disorders and functional abilities to determine whether a work disability benefit should be granted.
In many countries, prognosis of future changes in work ability is an important task of medical doctors during the medical disability assessment because, once a work disability benefit has been granted, changes in health may alter continuing eligibility [Citation1,Citation2]. Medical re-assessments are conducted to determine whether an individual’s health has improved or deteriorated to such an extent that adjustment of the benefit or support to return to work is required. In the Netherlands, IPs need to determine during a medical disability assessment if and when a re-assessment should be planned. To ensure that these medical re-assessment are planned at the time an assessment interview with an IP or LE has most added value, accurate prognosis of work ability is important. In general, claim duration for work disability benefits is long lasting for many claimants [Citation3,Citation4]. Because long-term occupational inactivity is bad for an individual’s health, and returning to work is generally associated with a positive effect on the future course of the disease and work ability, accurate prognosis of future changes in work disability may also enable effective return to work support [Citation5,Citation6].
However, making a prognosis of the future course of work ability is not that easy, because it requires rather complex predictions, in which a broad range of factors play a role. These include common sociodemographic and health-related characteristics such as age, educational level and diagnoses, but also more subjective measures such as coping strategies, health experience and social support from relatives [Citation7]. We developed a statistical model predicting future changes in work ability based on a broad range of factors, selected by a literature search of potential prognostic variables [Citation8]. The outcome of the prediction model is for each individual claimant the likelihood of the change in work ability one year later.
The aim of the prediction model is to help professionals in making an accurate prognosis of work ability for individual claimants during the work disability assessment. In order to make the results of the prediction model easily accessible and interpretable for professionals it needs to be supported by a suitable interface, in medicine often called clinical decision support tools. These are developed to support decision-making, in which the characteristics of individual patients are matched with a clinical knowledge base or decision rule [Citation9]. The tools present patient-specific assessments or recommendations to clinicians at the time they have to make the decisions. Clinical decision-support tools are designed to aid decision-making; they can introduce efficiencies into the tool, optimize the time with the client, and improve the overall quality of services and return to work interventions [Citation10,Citation11]. In medical practice, clinical decision support tools can increase health care quality and efficiency [Citation10,Citation12]. To be effective, not only the evidence base underlying these tools needs to be relevant and of high quality, but also the tool itself should be easily accessible and interpretable. Anticipating professionals’ needs on the preferred way of use and design are key components when developing effective and implementable decision support tools [Citation11].
Prognosis of work ability is an important task of IPs and LEs, and an evidence-based prediction model for future changes of work ability can help them making accurate prognosis. Although such tools are more common in clinical practice, they are currently lacking in work disability assessments. In order to develop a useful and relevant work ability prognosis support tool via which the outcome of the prediction model can be provided to IPs and LEs, it is important to know how and where in the decision making process these professionals will use the tool and how they like the results to be presented. Therefore, the aim of this study was to obtain information on the preferences of IPs and LEs regarding the way of use and design of a work ability prognosis support tool regarding the prognosis of work ability of disability benefit claimants’, based on a prediction model.
Methods
This study employs a qualitative focus group approach to explore the preferable way of use and design of a work ability prognosis support tool based on a prediction model for future changes in work ability. Unlike individual interviews, focus groups allow for interaction among group members. This enhances creativity, and makes it a useful approach for generating ideas, attitudes and opinions about a topic. Conducting focus groups helps individual participants to become aware of the range of design and use options and possible ways in which the work ability prognosis support tool can be applied.
We conducted three focus groups with IPs and LEs working at the Dutch Social Security Institute (SSI). IPs are medical doctors who conduct disability assessments, based on diagnoses and functional abilities. Subsequently, LEs, who often have a background in social work, conduct an assessment of corresponding job opportunities. According to Dutch law (WMO), no ethical approval was necessary for this study, because no patients were included in the study and the physicians were not exposed to any intervention.
Work ability prognosis support tool
The goal of the focus groups was to examine the usability of a work ability prognosis support tool, based on an evidence-based prediction model that identifies claimants with a high probability of experiencing an improvement in Work Ability Score (WAS) at one-year follow-up [Citation13]. The prediction model was based on a longitudinal cohort of 944 individuals, who were granted a work disability benefit by the SSI. Statistical variable selection was used to select the prognostic factors that were included in the final model. These were several physical and mental functioning factors, work status, wage loss, and work ability at baseline. The outcome of the prediction model is, for each individual claimant, the expected change in work ability at one-year follow-up. This outcome can be used by IPs and LEs as an additional source of information when they need to make decisions about the prognosis of claimants applying for a work disability benefit. For more information on the prediction model we refer to Louwerse et al. [Citation8]. The participants of the focus groups did not have any knowledge in advance about the prediction model, but a short presentation about the development and prognostic factors was given at the start of the focus group meetings.
Participants
The SSI has 27 offices, divided over 12 regions. In total, about 900 IPs and LEs were working at the SSI in 2018. Each focus group consisted of both IPs and LEs, who were working in the same region but possibly at different offices. This was done to reduce travel time, thereby making it easier to participate, and because there are very small differences in work procedures between regions. Convenience sampling was used to recruit participants. To start with, three regions were selected based on their willingness to participate and geographical distribution; one in the west, one in the middle, and one in the east of the Netherlands. Depending on the level of data saturation, i.e., whether new themes did emerge when analysing the third focus group, more focus groups could be organized. IPs and LEs were recruited via their supervisors. A prerequisite was that all participants currently need to perform medical disability assessment interviews. In order to capture a wide range of perspectives on the preferable way of use and design of the work ability prognosis support tool, we informed the supervisors that we aimed at a range of demographic characteristics (gender, age) and years of working experience when recruiting the participants. However, recruitment of participants was voluntary and all IPs and LEs who showed interest were accepted. Participants received no compensation for their participation in the focus groups.
Both IPs and LEs are involved in prognosis of future changes of work ability. However, while for IPs it is one of their main tasks during the medical disability assessment, LEs in the Netherlands mainly focus on current limitations and corresponding job opportunities. As IPs will be the main users of the work ability prognosis support tool, we aimed for at least two thirds of the participants being IPs.
Data collection
The focus groups were held in May and June 2018, at an office in the region where the IPs and LEs were based. One moderator (IL) and one observer (MHA and HJvR), all working as researchers in the field of occupational health, facilitated the focus groups. JO was present at all focus groups to take notes. For IL, it was the first time as a moderator. However, all other researchers (MHA, HJvR, JO, AvdB and JRA) had previous experience with conducting focus group meetings. Moreover, the procedures and topics of the focus groups were discussed in detail in the research team beforehand. There were no established relationships between the moderator and the participants prior to the study.
All three focus groups lasted for about 1.5 h, with a short break halfway through the focus group. The focus groups started with an explanation of the goal of the study, and the role of the moderator and the observer(s). Then, all participants introduced themselves and the topics were discussed. Two topics were discussed: 1) the preferred way of use of the work ability prognosis support tool, and 2) the preferable design of the work ability prognosis support tool. A more detailed overview of the topics is provided in . The topic guide for the focus groups was developed based on extensive discussions during several meetings of the research team.
Table 1. Overview of focus group topics.
Two weeks before the focus group meeting, participants were sent an information letter stating the goal and procedures of the focus groups, and the data management process. Participants were informed that everything discussed during the focus group would be handled confidentially, and all quotes would be anonymized. If participants agreed, they were asked to sign the informed consent form that was enclosed. During the meeting, data were recorded with an audio-recording device. Besides, the observer took notes of the topics discussed. Before the start of the focus group, participants were asked to fill in a short questionnaire, regarding demographics and working experience. Each participant was then given a number, linked to the questionnaires, and their names were not used in the analysis. Within one week after the meeting, participants received a summary of the content of the focus group, which they were asked to check. They were asked to contact the researchers if they found any errors or omissions. In the results, we used quotes originating from the interviews to illustrate our findings. Cited professionals were described by the job title of their profession, gender and age. Quotes were translated by one researcher (IL) and checked by all other researchers.
Analysis
Data were analysed using a thematic analysis approach [Citation14]. The COREQ checklist for reporting qualitative studies was used [Citation15]. All data were transcribed verbatim in Dutch. The data collection continued until saturation of information was established, i.e., the transcripts of the meetings provided no new information. The focus groups were analysed according to the main principles of thematic analysis, i.e., through a systematic classification process of coding and identifying themes or patterns in order to describe the preferable way of use and design of the work ability prognosis support tool [Citation16,Citation17]. All transcribed text and the notes of the focus groups were used in the analysis. First, two researchers (IL and JO) coded two thirds of each of the focus groups transcripts independently. During this phase of open coding, transcripts were carefully read, text parts that seemed relevant were coded and relations between main and sub codes were suggested. Second, during the phase of axial coding, the researchers discussed whether the created codes were appropriate to describe the data and whether the relation between main and sub codes was appropriate. This discussion continued until consensus was reached. As the researchers were both present during all focus groups, the interaction between the participants was taken into account as well. Finally, patterns in the data were identified by looking for returning themes and by making connections between these themes. After consensus was reached, all transcripts were (again) analysed by IL, using the provisional code list. All analyses were conducted using ATLAS.ti software.
Results
Participants
After three focus groups, a satisfactory level of data saturation was reached and therefore no additional focus groups were organized. In total 24 professionals participated; 5 in the first focus group (3 IPs and 2 LEs), 8 in the second (6 IPs and 2 LEs), and 11 in the third (8 IPs and 3 LEs). The actual distribution of 17 IPs and 7 LEs in total was in line with the intended distribution of about two thirds of the participants being IP, and one third being LE. The mean age of the participants was 51 years (SD = 9 years), 9 were female and 15 were male. The average working experience was 17 years (SD = 12 years) for IPs and 14 years (SD = 6 years) for LEs.
Only one participant added a remark to the content of the summary provided for them to check. The participant stressed the importance of a certain issue mentioned during the focus group. The comments of this participant were taken into account in the results.
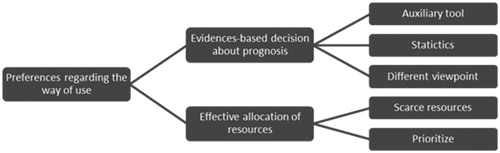
Our findings are presented per theme: the preferences regarding the way of use are set out first, followed by the preferences regarding the design of the decision support tool. Quotes were used to illustrate our findings, whereby we aimed for a distribution of profession, gender and age that represents the distribution of these characteristics among the participants. As an example of the coding tree that we developed, shows part of the coding tree for the first theme.
Preferences regarding the way of use
Evidence-based decisions about prognosis
Accurate prognosis of future work ability was considered as an important task of IPs and LEs. It aids provision of effective interventions to return to work for claimants who will benefit most from it. Assisting claimants to get back to work is stated in the vision of the SSI, and participants mentioned it as an important motivator for work.
Some participants had difficulties determining how to value the prediction model compared to their own consideration and estimation of a claimant’s prognosis. In answer to this, other participants argued that it aims to be an auxiliary tool, based on statistics of large numbers rather than physician’s knowledge and experience, which gives a different viewpoint and helps professionals to make more evidence-based prognosis.
It is helpful as an auxiliary tool: is the prognosis that I make based on literature and guidelines correct? (Insurance physician, female, 40 years)
Effective allocation of resources
Concerning reasons to use the work ability prognosis support tool, participants thought that, in case of scarce resources, the work ability prognosis support tool could guide effective allocation of resources. IPs conduct medical re-assessments to determine whether an individual’s health and work ability have improved or deteriorated to such an extent that adjustment of support to return to work is required. The participants suggested that the work ability prognosis support tool can help to select the claimants who are most likely to experience a significant improvement in work ability and hence are expected to benefit most from return to work support. According to the participants, the tool assists professionals to prioritize these claimants when they need to allocate limited resources and plan re-assessments.
It is also possible to prioritize, depending on the available capacity. We first assign resources to claimants who are most likely to benefit from it. Depending on the capacity that remains, we can assign it to claimants of whom we are less sure. (Labour expert, male, 56 years)
Verify and validate own prognosis
Opinions on when to use the tool differed. The majority of the participants stressed that they are open-minded at the start of the work disability assessment interview. They felt that using the work ability prognosis support tool at this stage would prohibit them from being so. They would first want to make their own judgement during the interview with the claimant and afterwards verify or falsify their evaluation with the work ability prognosis support tool. It will strengthen their belief that they made the right decision if the outcome of the prediction model matches their own prognoses, and it will be a reason to reconsider their prognoses if it does not match. A prerequisite in this case is that the work ability prognosis support tool should be available briefly after the work disability assessment interview, when IPs need to write a medical report.
Then I can first get my own idea and afterwards see if this coincides with the outcome of the prediction model. If you consult the work ability prognosis support tool before the interview with the claimant, then it might be in the back of my mind during interview. Although it will not completely determine my way of thinking, it might influence it anyway, and cause you to ask certain questions that you would otherwise not have asked. (Insurance physician, male, 58 years)
More thorough preparation for the interview
A few participants argued that being able to use the work ability prognosis support tool before the disability assessment interview would help in preparing the interview, and might give guidance for topics to pay additional attention to during the interview with the claimant. Moreover, it gives the possibility to discuss the prognosis and follow-up actions with the claimant during the interview.
I think it could be useful when preparing for the interview with the claimant. What information is, for instance, available about expected return to work and the motivation of the claimant. I could use this information to ask specific questions to the claimant and talk about potential barriers for return to work. (Insurance physician, male, 41 years)
No distraction from the conversation with the claimant
All participants agreed that using the work ability prognosis support tool during the disability assessment interview is not desirable as during this contact they want to focus full attention on the interview with the claimant. Using the work ability prognosis support tool and judging the outcome of the prediction model would distract them and would take too much time.
You need time to interpret and evaluate the work ability prognosis support tool. It is difficult to do this during the interview with the claimant. (Insurance physician, male, 60 years)
Reservations about self-reported factors
Participants expressed their concern about using self-reported measures as prognostic variables for the prediction model. They mentioned that applying for a work disability benefit is an emotional process during which claimants can experience a lot of insecurities and that these emotions could influence the answers claimants give on self-reported questionnaires. Moreover, they questioned whether the work ability prognosis support tool would be for professional use only, or if and how its results can be communicated to claimants as well.
We have claimants who have negative thoughts about getting back to work, while we think that there are opportunities for return to work. If claimants own opinions greatly influence the outcome of the prediction model, it would be less reliable for me. (Labour expert, male, 53 years)
One model for all claimants
Concerning reasons for non-use, participants mentioned some factors that by themselves almost completely determine the expected prognoses and the recommended return to work interventions were mentioned. For instance older claimants often have less psychological resilience than younger claimants, and less motivation to put a lot of effort in a return to work intervention when they are close to reaching the retirement age. Other factors that were mentioned as determinants for lower expectations of future improvements of work ability and successful return to work support were claimants suffering from comorbidity, claimants with non-health related complications, such as financial or personal issues, and claimants with several and longer periods of work disability in the past.
Age plays a role. For instance when a woman older than 50 years has a long-term depression, her psychological resilience becomes less and you can take that into account during your assessment. (Insurance physician, male, 58 years)
Claimants who are already longer without a job, either because of unemployment or sickness, have a larger distance to the labour market, and are usually also less motivated. (Labour expert, female, 58 years)
However, participants agreed that they would not beforehand exclude participants from the prediction model. The work ability prognosis support tool has most added value in cases where professionals are unsure about the prognosis, for instance when the course of the disease is unclear. However, also when an insurance physician is more confident about the expected change in work ability, some of them argued that they could use the work ability prognosis support tool in these cases to verify their thoughts. Because the prediction model is based on a diverse set of variables, both SSI registration data and self-reported measures, it is a useful complement to the prognosis of the professional.
I think it always adds something, because when I think an improvement of work ability is very likely and the work ability prognosis support tool shows green, then this confirms my expectations. And otherwise, the tool shows the opposite, it would make me think I missed something, I will think about it more thoroughly. So I think it is always useful. (Insurance physician, male, 59 years)
Preferences regarding the design
Clearly present the outcome of the prediction model
Participants mentioned clarity and ease of use as important features of the tool. They argued that these features are crucial for successful use of the tool in practice. Dividing claimants into groups based on their predicted future change in work ability and assigning colours to the groups (e.g., green for claimants with a high probability of experiencing an improvement in work ability, red for claimants with a high probability of experiencing a deterioration in work ability, and orange if no relevant change in work ability is predicted) was seen as a straightforward and clear way of presenting the results of the prediction model. As users have a quick and uniform association with colours, this encourages them to take action.
By using colours in the outcome of the prediction model it is immediately clear. (Labour expert, female, 47 years)
I also think that if you represent it this way, that it encourages us to take action faster than if you would represent it in a more neutral way. (Insurance physician, male, 31 years)
Detailed information about the predicted outcome
Participants argued that more detailed information might be helpful in some cases, for instance when for a claimant the predicted value falls on the boundary of two categories. More precise presentation of the outcome of the prediction model, e.g., by dividing the claimants into more than three categories or by presenting the prediction on a continuous scale, gives more accurate information but would also be more difficult to interpret. Moreover, it would result in less uniformity as more detailed information leads to larger differences in interpretation between professionals. Moreover, some participants mentioned that they would like to have some information about the uncertainty of the predicted value (e.g., the outcome of the prediction model and the corresponding category that a claimant is assigned to), for instance by presenting the confidence interval around the predicted value on a continuous scale. However, most participants thought that it would be difficult for them to value this information and that it would work against an easy interpretation of the main outcome.
A continuous scale is visually attractive, but if you want to evaluate it, you should attach recommendations or actions to it. Otherwise everyone will interpret it in his or her own way, and that will not result in better prognosis. (Insurance physician, female, 40 years)
Information about the prognostic variables
To create more support and confidence in the work ability prognosis support tool and the underlying prediction model, participants argued that they need more information about the prognostic variables of the prediction model. Some participants preferred a concise summary of characteristics of claimants and the prognostic variables of the prediction model, for other participants a presentation beforehand about how the prediction model is constructed and its underlying variables would be sufficient.
It is difficult for me to interpret the outcome of the prediction model if I don’t have information about what the model looks like. What are the most important factors? Some general information about the prediction model and the variables that are included would be helpful. (Labour expert, female, 47 years)
Also for the acceptance of my colleagues it is important that we have a better understanding of the prediction model. (Insurance physician, male, 47 years)
Discussion
Main findings
The goal of this study was to explore the preferences of professionals regarding the way of use and design of a work ability prognosis support tool, which can help them in making accurate prognoses of future changes in work ability. Qualitative analysis of focus groups showed that IPs and LEs of the SSI reported a large number of preferences regarding the way of use (e.g., evidence-based decisions about prognosis, effective allocation of resources, and verify and validate own prognosis) and preferences regarding the design (e.g., clearly present the outcome of the prediction model and information about the prognostic factors) of the decision support tool. Participants agreed that clarity and ease of use are important features of the tool. Dividing claimants into categories based on the outcome of the prediction model and assigning colour labels to the classes was experienced as the most straightforward and clear way of presenting the results of the prediction model. It encourages professionals to use the tool and act accordingly. Concerning preferences on when to use the tool, most professionals would prefer to first make their own judgement during the work disability assessment interview with the claimant and afterwards verify or adjust their evaluation based on the outcome of the work ability prognosis support tool.
Interpretation of findings
Ease of use was mentioned by the participants of the focus groups as key component for successful actual use of the tool. This is in agreement with previous qualitative research that concluded that a simple and easy-to-use design was a necessity for IPs to use a prediction rule aimed at supporting work disability assessment of cancer survivors [Citation18]. In this earlier study, IPs mentioned that a prediction rule should take little time to use, should have added value for the work disability assessment and should be both valid and reliable. Ensuring ease of use by using computers to generate the support is an important feature for clinicians and other health care stakeholders to use clinical support tools [Citation19]. Even if the tool is very well designed, it will be useless if the professional is not able to use prediction rule at the time of decision making [Citation20].
Another crucial component for successful use of the tool mentioned by the participants of our focus groups was clarity of the work ability prognosis support tool. This concurs with the results of studies describing the use of computer tools among physicians, stating that professionals will not be happy about using a support tool if the information that it presents does not fit on a single screen [Citation21]. Our participants indicated that even simple and relatively straightforward recommendations can be interpreted in different ways, depending on one’s perspective or experience. This is in line with results found in the general field of risk communication that people have difficulties with interpreting and providing meaning to numerical information [Citation22,Citation23]. Even across samples consisting of only highly educated individuals, participants appeared to have difficulties understanding and interpreting health statistics [Citation24,Citation25]. Instead, graphical risk presentation, such as using colours and verbal categorical labels, intends to provide intuitive meaning to numerical information. By using graphical formats it is usually easier to attract the attention of the user and to support their understanding [Citation26,Citation27]. Dividing claimants into three categories based on the prediction model and assigning colours and recommendations to these categories seems a good way to prevent differences in interpretation.
The present study revealed that most SSI professionals would like to use the work ability prognosis support tool to verify their own prognosis directly after the work disability assessment interview. A minority of the participants mentioned that they would prefer to have the possibility to use the tool before the disability assessment interview as well, as this would help them in preparing the interview with the claimant. In general, automatic provision of decision support at the time and location of decision making is a key element for successful actual use [Citation28]. It would be possible to give SSI professionals the opportunity to use the tool at other moments as well, but it should be investigated whether professionals would do so, as previous research showed that clinical support tools were less successful if clinicians had to initiate the use of it themselves [Citation19].
Strengths and limitations
A first strength of the present study is that the focus groups were held within three different regions of the SSI, each located in a different part of the Netherlands, and the participants were selected out of all potential users of the work ability prognosis support tool. This enabled us to gather different perspectives, design a tool that satisfies as much as possible the demands, and create a high level of support for the users. Secondly, we carefully followed the guidelines for qualitative research by having two researchers who independently analysed and coded the data, by discussing the study design and results within the research team, and by performing member checks. This contributes to the credibility and confirmability of the study. The dependability of the study was taken into account by continuing data collection until a satisfactory level of data saturation was reached, and by applying a flexible research design.
Another strength of this study is that, when considering the way of use and design of the work ability prognosis support tool, we focused on its actual use in the Dutch social security system and the procedures at the SSI. Hence, the setting in which the work ability prognosis support tool will be used is emphasized during the focus groups. However, the obvious limitation related to this is that generalizability of our findings was limited. Translation of our findings to other settings can only be done with care as work disability evaluation processes and legislation largely differ across European countries in terms of steps involved, use of professional assessors and time consumption [Citation1]. However, by giving a description of social security context in which this study was performed, and by comparing our findings with existing literature we aimed at enhancing the transferability. Other limitations of this study are that we conducted convenience sampling, which means that the participants might have provided only limited different perspectives because they were not sampled by purposeful sampling. A final limitation is that we did only focus on the preferable way of use and design of the work ability prognosis support tool and that there was no time to discuss other barriers or facilitators for use that could be faced in practice. Therefore, it is important to conduct a process evaluation alongside an effectiveness study to identify other barriers or facilitators for use.
Implications for practice and research
A work ability prognosis support tool based on a prediction model for changes in work ability at one-year follow-up can help IPs and LEs making accurate prognosis. Being supported by a suitable work ability prognosis support tool, which is easy to access and interpret, is a prerequisite to increase the chance that professionals will use the tool. The present study showed that IPs and LEs agree on the preferred way of use and design of the work ability prognosis support tool. This provides a good starting point for developing a tool that is user-friendly and aligned to the preferences of IPs and LEs and that can be tested in a trial. Based on the results of this focus group study, we will develop a work ability prognosis support tool. Next, an effectiveness study will be performed to determine if the actual use of the tool contributes to more accurate prognoses. Furthermore, a process evaluation should show whether IPs actually use the tool and how they evaluate it.
Although the development of clinical support tools has rapidly increased over the past decade, it still remains to be seen whether these tools will be part of everyday practice and to what extent they can contribute to effective occupational health provision. As clinical support tools do not guarantee a correct solution for every single case, it is important to emphasize that they should not be automatically followed. Rather, these tools should be complementary to occupational health professionals’ judgements, which should be prioritized at all times. Therefore, professionals should be informed about proper use and the scientific evidence of such tools.
Acknowledgments
The authors are grateful to all participating social insurance physicians and labour experts for their contribution.
Disclosure statement
IL and HJvR are employed at the Dutch Social Security Institute. AJvdB and JRA are shareholders of Amsterdam University Medical Center’s spin-off company Evalua Nederland BV. JRA holds a chair in Insurance Medicine on behalf of the Dutch Institute for Employee Benefit Schemes.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- De Boer WEL, Besseling JJM, Willems JHBM. Organisation of disability evaluation in 15 countries. Prat Organ Soins. 2007;3(38):205–217.
- Anner J, Kunz R, de Boer W. Reporting about disability evaluation in European countries. Disabil Rehabil. 2014;36(10):848–854.
- Louwerse I, Huysmans MA, van Rijssen HJ, et al. Characteristics of individuals receiving disability benefits in the Netherlands and predictors of leaving the disability benefit scheme: a retrospective cohort study with five-year follow-up. BMC Public Health. 2018;18(1):157.
- Wise DA. Social security programs and retirement around the world: Historical trends in mortality and health, employment, and disability insurance participation and reforms. Chicago: University of Chicago Press; 2012.
- OECD. Sickness, disability and work: breaking the barriers: a synthesis of findings across OECD countries. Paris: OECD Publishing; 2010.
- Waddell G, Burton AK. Is work good for your health and well-being? London: The Stationery Office; 2006.
- Kok R, Verbeek JAHM, Faber B, et al. A search strategy to identify studies on the prognosis of work disability: a diagnostic test framework. BMJ Open. 2015;5(5):e006315.
- Louwerse I, Huysmans MA, van Rijssen JH, et al. Predicting future changes in work ability of individuals receiving a work disability benefit: weighted analysis of longitudinal data. Scand J Work Environ Health. 2019. DOI:10.5271/sjweh.3834
- Sim I, Gorman P, Greenes RA, et al. Clinical decision support systems for the practice of evidence-based medicine. J Am Med Inform Assoc. 2001;8(6):527–534.
- Roshanov PS, Fernandes N, Wilczynski JM, et al. Features of effective computerised clinical decision support systems: meta-regression of 162 randomised trials. BMJ. 2013;346(feb14 1):f657.
- Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10(6):523–530.
- Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8(4):299–308.
- Ahlstrom L, Grimby-Ekman A, Hagberg M, et al. The work ability index and single-item question: associations with sick leave, symptoms, and health – a prospective study of women on long-term sick leave. Scand J Work Environ Health. 2010;36(5):404–412.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
- Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Boeije H. Analysis in qualitative research. London: Sage publications; 2009.
- van Muijen P, Duijts SFA, Kornet-van der Aa DA, et al. Work disability assessment of cancer survivors: insurance physicians’ perspectives. OCCMED. 2015;65(7):558–563.
- Kawamoto K, Houlihan CA, Balas EA, et al. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330(7494):765.
- Lee F, Teich JM, Spurr CD, et al. Implementation of physician order entry: user satisfaction and self-reported usage patterns. J Am Med Inform Assoc. 1996;3(1):42–55.
- Shojania KG, Yokoe D, Platt R, et al. Reducing vancomycin use utilizing a computer guideline: results of a randomized controlled trial. J Am Med Inform Assoc. 1998;5(6):554–562.
- Reyna VF, Brainerd CJ. The importance of mathematics in health and human judgment: numeracy, risk communication, and medical decision making. Learn Individ Differ. 2007;17(2):147–159.
- Maviglia SM, Zielstorff RD, Paterno M, et al. Automating complex guidelines for chronic disease: lessons learned. J Am Med Inform Assoc. 2003;10(2):154–165.
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21(1):37–44.
- Gigerenzer G, Gaissmaier W, Kurz-Milcke E, et al. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest. 2007;8(2):53–96.
- Waters EA, McQueen A, Cameron LD. Perceived risk and health risk communication. In: Heidi E. Hamilton, Wen-ying Sylvia Chou, editors. The Routledge handbook of language and health communication. New York; London: Routledge; 2014. p. 47–60.
- Trevena LJ, Zikmund-Fisher BJ, Edwards A, et al. Presenting quantitative information about decision outcomes: a risk communication primer for patient decision aid developers. BMC Med Inform Decis Mak. 2013;13(S2):S7.
- Garg AX, Adhikari NKJ, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293(10):1223–1238.