Abstract
Purpose
To examine current practices of occupational health professionals in assessing significant others’ cognitions and behavioral responses that may influence work outcomes of workers with a chronic disease.
Methods
A survey study among occupational health professionals, focusing on the assessment of illness perceptions, work-related beliefs and expectations, and behavioral responses of significant others of workers with a chronic disease. We performed linear regression analyses to investigate which factors are related to occupational health professionals’ assessment practices. We used thematic analysis to analyze qualitative data on occupational health professionals’ reasons to assess or overlook significant others’ cognitions and behavioral responses.
Results
Our study sample included 192 occupational health professionals. Most seldom asked about significant others’ cognitions and behavioral responses. Organizational norms and occupational health professionals’ self-efficacy were related to reported assessment practices. Reasons to assess significant others’ cognitions and behavioral responses included recognizing their influence on work participation, and occurrence of stagnation. However, occupational health professionals indicated some doubt whether such assessment would always contribute to better care.
Conclusions
It is not common practice for occupational health professionals to assess significant others’ cognitions and behavioral responses, although they recognize the influence of these factors on work outcomes. More research is needed as to how occupational health professionals can best address the role of significant others, and apply these new insights in their daily practice.
Most occupational health professionals do not commonly ask about significant others’ cognitions and behavioral responses despite the possible influence of these factors on work outcomes.
Occupational health professionals may be able to better support workers with a chronic disease by paying more attention to the influence of significant others.
Aside from asking about practical support, occupational health professionals should consider asking about significant others’ illness perceptions, work-related beliefs and expectations, and other behavioral responses.
Implications for rehabilitation
Introduction
Significant others (SOs), like partners, family members or friends, can play an important role in work and health outcomes of individuals with a chronic disease [Citation1–4]. SOs can be an important resource to help individuals cope effectively with a chronic disease and to manage their working life [Citation1,Citation4–6], and may therefore be important facilitators of work participation. However, they can also be an important barrier, for example, when SOs believe that return to work will worsen the condition and they pressure the worker to refrain from work [Citation7,Citation8].
Various models have been used to explain how an individual’s coping can be influenced by a SO. For example, both the developmental–contextual model and the Systemic Transactional Model are based on the assumption that stressors, such as a chronic illness of one partner, affect both the patient and the partner and that there is interdependence between their stress and coping processes [Citation9]. Both models highlight the importance of appraisals about the stressor and the behavior of both members of the couple under stress to understand individual and dyadic coping processes. This is in line with prior research that indicates that SOs’ cognitions (e.g., illness perceptions, beliefs, and attitudes) and behavioral responses (e.g., social support and negative or solicitous responses) can influence how workers cope with chronic disease [Citation10–15]. More specifically, in a recent systematic review, we found that SOs’ positive and encouraging attitudes regarding work participation, encouragement and motivating behavior and open communication with workers can facilitate work participation [Citation4]. On the other hand, SO’s positive attitudes towards sickness absence and advise, encouragement or pressure to refrain from work can hinder work participation of workers with a chronic disease. As there is evidence that clinical health care interventions in which SOs are involved are more effective than care in which SOs are not involved [Citation16–19], this may also be beneficial in occupational health care.
The recent shift from a predominantly medical to a biopsychosocial approach indicates that occupational health professionals (OHPs) need to be aware of environmental factors as well as medical and personal factors, as the interaction between these factors has been found to influence functioning and disability [Citation20–23]. Moreover, various multidisciplinary and clinical guidelines advise health professionals to address environmental factors and to involve SOs such as family members in treatment and care [Citation16,Citation17,Citation24–28]. For example, the Scottish guideline “Management of chronic pain” recommends that health professionals assess the influence of family on pain behavior [Citation25], and the Dutch multidisciplinary occupational health guideline “Chronically ill and work” enjoins OHPs to take into account the influence of social support and overprotection by SOs [Citation24].
Until now, the extent to which such guideline recommendations are implemented in daily practice is unclear. In particular, little is known about how often OHPs assess the cognitions and behavioral responses of SOs of workers with a chronic disease, whether they assess particular cognitions or behavioral responses more frequently than others, and what motivates them to assess or overlook these cognitions and behavioral responses. Gaining insight into current practices could provide an empirical basis to improve involvement of SOs in occupational health care and to develop effective interventions to deal with SOs’ influences on workers with chronic illnesses.
The first aim of this study was thus to examine to what extent OHPs assess cognitions and behavioral responses of SOs of workers with a chronic disease in their daily practice, and whether they assess certain cognitions or behavioral responses more frequently than others. Secondly, we aimed to determine which factors are related to the assessment of SOs’ cognitions and behavioral responses. Third, we aimed to explore why OHPs’ either assess or overlook these cognitions and behavioral responses.
Materials and methods
Context
Internationally, various types of OHPs are involved in occupational health care to assess work ability, prevent sickness absence, and promote work participation. In the Netherlands, two main types of OHPs play an important role in occupational health care: occupational physicians and insurance physicians [Citation18]. Occupational physicians are generally involved in the first two years of sick leave, during which they provide support and guidance to help employees retain or return to work. When employees have been on sick leave for over two years, they can claim a disability benefit at the Dutch Social Security Institute: the Institute for Employee Benefits Scheme (UWV). For this claim, insurance physicians assess the functional limitations of the employee due to illness or disability. Self-employed workers cannot claim a disability benefit at the Dutch Social Security Institute, but can choose to insure themselves against occupational disability risks at private insurance companies. For these workers, insurance physicians working in the private sector (medical advisors) assess the functional limitations due to illness or disability, assess disability claims, and provide medical advice regarding injury or illness in relation to work.
Design and procedure
We conducted a mixed-method cross-sectional survey study among OHPs in the Netherlands, involving a sample of occupational and insurance physicians. In total, 1,719 occupational physicians and 964 insurance physicians were registered on 31 December 2017 by the Registration Committee Medical Specialists of the Royal Dutch Society for the Advancement of Medicine (KNMG) [Citation19]. For distribution of the survey, we cooperated with the Dutch Association of Occupational Medicine (NVAB), the Dutch Association for Insurance Medicine (NVVG), and the Dutch Association of Medical Advisers in Private Insurance (GAV). An invitation letter to participate in this study was distributed by email to all occupational physicians who were members of the NVAB (1,350 occupational physicians) and insurance physicians who were member of the NVVG (668 insurance physicians) and the GAV (231 insurance physicians). The letter included information on the study aim and time needed to complete the survey, as well as privacy, confidentiality, and anonymous processing of the data. It also included a link to the online survey. Approximately three weeks later a reminder was sent. Participants were offered no compensation or reward. The first invitation offered a two-month response time, after which the survey was closed.
Informed consent was obtained at the start of the survey. Inclusion criteria for study participation were as follows: (1) being an occupational or insurance physician, and (2) being involved in return to work or work disability procedures of workers with a chronic disease. Physicians who failed to give informed consent or were not eligible to participate were automatically excluded from further participation. Moreover, participants who indicated working in more than one profession were asked to select one profession, for which they would answer the remaining survey questions. This was because assessment of SOs’ cognitions and behavioral responses might differ between professions, for example, due to a different task (i.e., supporting workers to retain or return to work versus assessment of functional limitations due to illness or disability) or phase in the return to work process in which they were involved. The survey included both multiple choice and open questions and took approximately 20–30 min to complete.
The Medical Ethics Review Committee of the University Medical Center Groningen confirmed that because the Medical Research Involving Human Subjects Act (WMO) did not apply to this study official approval by this committee was not required (METc 2017/486, M17.218841).
Measures
As we were interested in assessment practices of OHPs concerning SOs of workers, we specified SOs as a partner, family members, or friends at the start of the survey. To measure OHPs’ current assessment practices, we used three constructs, derived from our recently published systematic review [Citation4], namely assessment of SOs’ (i) illness perceptions, (ii) work-related beliefs and expectations, and (iii) supportive and unsupportive behavioral responses. For all three constructs, items were derived from existing questionnaires and adapted to the purpose of this survey. To reduce the length of the survey, we selected only those items corresponding to SOs’ cognitions or behavioral responses which had previously been reported to be related to work participation of workers with a chronic disease [Citation4]. In some cases, we combined multiple items into one. The items for each of the constructs are included in Online Resource 1. Moreover, to measure all items of the constructs we used a 5-point Likert scale (never, rarely, sometimes, often, or always).
We measured OHPs’ assessment of SOs’ illness perceptions using four items on a 5-point Likert scale. We included items regarding perceptions about the subscales “cause” and “control” of the Dutch version of the Brief Illness Perceptions Questionnaire [Citation29] and the subscales “perseverance” and “avoidance” of the Extended Illness Cognition Questionnaire [Citation30]. The internal consistency of the construct was high, with a Cronbach's alpha of .90.
We measured OHPs’ assessment of SOs’ work-related beliefs and expectations, using four items on a 5-point Likert scale. Three items were based on items from the Return-To-Work Self-Efficacy questionnaire (RTWSE-19) [Citation31] and one item was derived from the Work-Related Recovery Expectations Questionnaire [Citation32]. The internal consistency of the construct was high, with a Cronbach's alpha of .90.
We measured OHPs’ assessment of SOs’ supportive and unsupportive behavioral responses towards the worker, using eight items on a 5-point Likert scale. We derived the questions from items of the Sources of Social Support Scale [Citation33] and the Spouse Response Inventory (SRI). The internal consistency of the construct was high, with a Cronbach's alpha of .88.
We also collected descriptives of OHPs (age, gender, profession, employment status, years in practice, and core tasks). We measured OHPs’ self-efficacy to address SOs’ cognitions and behavioral responses in daily practice using six items on a 5-point Likert scale ranging from strongly disagree to strongly agree. Three items related to OHPs’ self-perceived knowledge, skills, and availability of tools to assess SOs’ cognitions and behavioral responses on a 5-point Likert scale ranging from strongly disagree to strongly agree. The other three items measured OHPs’ self-perceived knowledge, skills, and availability of tools to respond effectively to cognitions and behavioral responses of SOs. The internal consistency of the construct was high, with a Cronbach's alpha of .92. In addition, we measured the organizational norm for assessing SOs’ cognitions and behavioral responses by asking OHPs whether they were expected to assess (i) beliefs and expectations or (ii) responses, behaviors, and involvement of SOs according to the social norm in their organization. Only OHPs who indicated that they were in paid employment were asked to answer these items, as self-employed OHPs are not employed at an organization with colleagues working in the same profession and these items, therefore, did not apply to these OHPs.
Finally, using four open-ended questions we collected data on OHPs’ reasons to assess or not to assess SOs’ cognitions and behavioral responses. Two questions asked for participants’ reasons to assess: (i) SOs’ beliefs and expectations and (ii) SOs’ responses, behaviors, and involvement. The other two questions asked participants to state their reasons for not assessing these factors.
The survey was piloted by five OHPs (both occupational and insurance physicians). They were asked to read the invitation letter, complete the survey, and think about strategies to enhance participation in the survey study. Based on their feedback, we made some small linguistic adaptations in the invitation letter and the survey.
Data analysis
Quantitative data were analyzed using SPSS version 25 [Citation34]. Descriptive statistics (e.g., frequencies, percentages, means, standard deviations) were used to describe the study sample and to indicate how often OHPs address each of the constructs (SOs’ illness perceptions, work-related beliefs, and expectations, or behavioral responses). The Friedman test was used to determine whether OHPs assess certain constructs more frequently than others. Post-hoc analyses with Wilcoxon signed-rank tests were conducted to determine where the differences occurred. Sensitivity analyses were performed to determine whether assessment practices differed between occupational and insurance physicians.
To investigate which factors related to OHPs’ assessment of SOs’ cognitions and behavioral responses, univariate and backward multiple linear regression analyses were performed for each construct. The three constructs were entered as dependent variables. We performed preliminary analyses for each construct to ensure that there was no violation of the assumptions of normality, multicollinearity, and homoscedasticity. The independent variables entered in the models were as follows: (i) gender, (ii) profession, (iii) employment status, (iv) years in practice, (v) core task of the professional, (vi) self-efficacy, and (vii) organizational norm to assess SOs’ cognitions (for the two cognitive constructs) or behavioral responses (for the behavioral construct). Dummy variables were created for all variables, except for self-efficacy (continuous variable). To prevent interpretation difficulties, dummy variables belonging to the same variable were entered as a block. After the performance of the univariate linear regressions for each construct, we performed backward multiple linear regressions, entering only those independent variables that were significantly associated with the dependent variable in the univariate regressions (p < 0.05). We entered a block of dummy variables in the multiple regressions when at least one dummy variable in the block was significant in the univariate regressions (p < 0.05).
To analyze OHPs’ responses on the four open-ended questions regarding why they did or did not assess SOs’ cognitions and behavioral responses, we used thematic analysis, following the six recommended phases for conducting such analysis [Citation35]. In the first phase, we read and re-read transcripts to become familiar with the data (NCS, HdV). In the second phase, initial codes were generated and data were systematically collated to each code across the entire data (NCS, HdV). In the third phase, codes were collated into potential themes (NCS, HdV). In the fourth phase, the potential themes were reviewed and refined, first on the level of the coded extracts, after which the process was repeated on the level of the entire data set (NCS, HdV). The fifth phase involved generating a definition and name for each theme, and with two additional members of the research team (MH, SB) we checked the final themes. In the final phase, we selected examples of quotes for each theme and described the findings (NCS).
Results
A total of 241 OHPs agreed to participate in the study (response rate of 10.7%). OHPs who did not respond to all items of at least one of the three constructs (SOs’ illness perceptions, work-related beliefs, and expectations, or behavioral responses) were excluded from the analyses (n = 49). The final study sample consisted of 192 OHPs (79.7%). In the group of non-responders, a higher percentage of OHPs were female (53.1 vs. 39.6%) and self-employed (41.5 vs. 31.3%) than in the final study sample. In addition, in the non-response group, a higher percentage worked as insurance physicians and indicated that providing medical advice was their core task (34.7 vs. 27.1%). The majority of the final study sample were male (60.6%) and worked in paid employment (64.8%). Seventy-three percent were occupational physicians and 84 percent indicated having had at least 16 years of work experience, a percentage comparable to the general population of OHPs in the Netherlands [Citation36]. More detailed demographic information of the participants is provided in .
Table 1. Characteristics of participating occupational health professionals (N = 192).
Assessment of SOs’ cognitions and behavior
Most OHPs reported that they did not frequently ask about SOs’ (i) illness perceptions (), (ii) work-related beliefs and expectations (), and (iii) behavioral responses (). They (70.4%) reported frequently (often or always) assessing only practical support, while 8.9–36.5 percent of OHPs frequently assessed the other items. More detailed information about the response distribution within the three constructs is provided in Supplementary Table S1. Sensitivity analyses showed no significant differences between assessment practices of occupational versus insurance physicians.
Figure 1. Distribution of responses for assessment of significant others’ illness perceptions by occupational health professionals (Median = 2.8, IQR = 2.0–3.0).
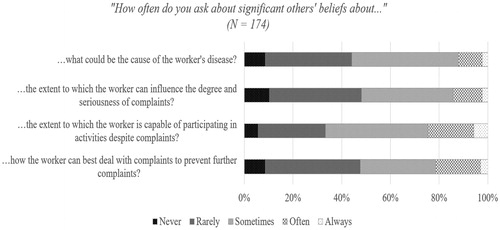
Figure 2. Distribution of responses for assessment of significant others’ work-related beliefs and expectations by occupational health professionals (Median = 2.5, IQR = 2.0–3.0).
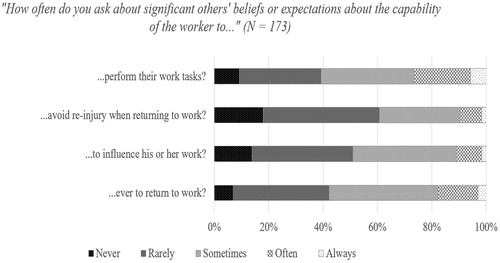
Figure 3. Distribution of responses for assessment of significant others’ behavioral responses by occupational health professionals (Median = 3.0, IQR = 2.9–3.5).
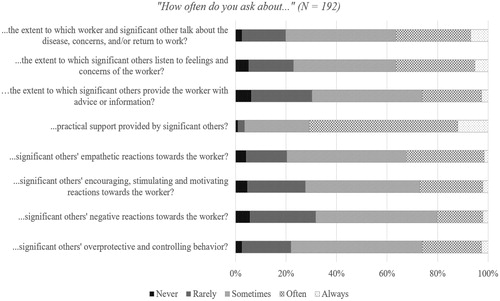
Comparison of the assessment frequencies of the three constructs indicated a statistically significant difference (χ2(2) = 99.54, p < 0.001). Post-hoc analyses showed that OHPs more frequently reported asking about SOs’ behavioral responses than about their illness perceptions (Z = −7.12, p < 0.001) and work-related beliefs and expectations (Z = −8.02, p < 0.001). Moreover, they more frequently reported asking about SOs’ illness perceptions than about their work-related beliefs and expectations (Z = −2.68, p < 0.007).
Factors associated with OHPs’ assessment practices
shows the results of the univariate and multiple linear regression analyses for OHPs’ assessment of the three constructs.
Table 2. Univariate and multiple regression analyses for variables predicting OHPs’ assessment of significant others’ illness perceptions, work-related beliefs and expectations, and behavioral responses.
With regard to the construct assessment of SOs’ illness perceptions, only the variable organizational norm remained in the final multiple regression model, explaining 17.2 percent of the variance (F(1, 116) = 24.02, R2 = 0.172, p < 0.001). OHPs who regarded it customary within their organization for someone of their profession to ask about SOs’ cognitions were more likely to do so themselves.
For the construct assessment of SOs’ work-related beliefs and expectations, the variables organizational norm, profession and self-efficacy remained in the final multiple regression model, explaining 19.3 percent of the variance (F(3, 114) = 9.07, R2 = 0.193, p < 0.001). The presence of an organizational norm to assess SOs’ cognitions was positively associated with OHPs’ reported assessment of SOs’ work-related beliefs and expectations. In addition, insurance physicians reported asking less frequently about SOs’ work-related beliefs and expectations than occupational physicians. Furthermore, OHPs’ showed a trend of a positive relation between self-efficacy to address cognitions and behavioral responses of SOs and reported assessment practices. However, this trend was not statistically significant.
With regard to the construct assessment of SOs’ behavioral responses, the variables organizational norm and years in practice remained in the final multiple regression model, explaining 29.8% of the variance (F(5, 119) = 10.09, R2 = 0.298, p < 0.001). Both variables were positively associated with OHPs’ reported assessment of SOs’ behavioral responses.
In the final multiple regression models, the presence of an organizational norm was the only variable that significantly contributed to OHPs’ assessment practices across all three constructs. However, the inclusion of the organizational norm in the regression analyses considerably reduced our study sample because participating self-employed OHPs did not complete the items on the organizational norm as these items did not apply to them (n = 60). We, therefore, conducted additional multivariate regression analyses excluding the variable organizational norm (, third column). In the additional analyses, OHPs’ self-efficacy was the only variable that significantly contributed to OHPs’ assessment practices for all three constructs. OHPs who felt more competent to ask about and effectively respond to SOs’ beliefs and expectations or behavioral responses were more likely to assess these factors. Aside from the inclusion of the variable self-efficacy instead of the organizational norm, the final multiple regression models of the additional analyses resembled those of the initial analyses with regard to those variables that remained in the final models. However, the final multiple regression models of the additional analyses explained less of the variance (8.0–15.3%) than did the final multiple regression models of the initial analyses, in which the variable organizational norm was included (17.2–29.8%).
Reasons (not) to ask about SOs’ cognitions or behavioral responses
We defined six themes regarding OHPs’ reasons to ask about SOs’ cognitions and behavioral responses, and ten themes regarding OHPs’ reasons not to ask about this. provides an overview of the themes, including theme descriptions and illustrative quotes.
Table 3. Description of qualitative data on occupational health professionals’ reasons whether or not to ask about significant others’ cognitions and behavioral responses.
A frequently reported reason to ask about SOs’ cognitions or behavioral responses was to understand the worker’s social context and how SOs support or influence him/her because these OHPs already presume that these persons can influence the worker, the recovery, and/or the re-integration process (theme 1). For example, an occupational physician indicated:
It can be an important supportive factor, but it can also play a role in negative cognitions or stagnation of recovery, for example when a significant other is fearful or has many concerns
OHPs also reported asking about SOs’ cognitions or behavioral responses to get additional information, for instance about the worker’s complaints, functioning and coping (theme 2). OHPs reported being able to use this information as hetero anamneses or as a starting point for more in-depth discussion during consultations, for example, to mobilize the support of SOs or intervene if SOs showed overprotective behavior. For instance, an insurance physician answered:
If the client himself cannot sufficiently put it into words
OHPs further reported asking about significant others’ views and reactions in cases of stagnation of some kind (theme 3). To illustrate, an occupational physician stated:
If there is inadequate behavior, recurrent setbacks, and clients are not able or afraid to change their behavior
Moreover, the presence of mental health problems, severe complaints, or coping issues (theme 4) and the presence of an SO during the consultation (theme 5) could lead OHPs to ask about the SO’s cognitions and behavioral responses. For example, an insurance physician answered:
In the presence of mental complaints or obvious mourning because of changed life perspective due to the illness
Finally, OHPs reported asking more in depth about the views and reactions of SOs if the topic was raised in the natural course of the conversation or mentioned by the worker himself (theme 6). To illustrate, an occupational physician reported:
When I get the impression from the conversation (for example after asking about social support or when people indicate something about this themselves) that something is going on here
One reason for OHPs not to ask about SOs’ views and reactions was that they do not always consider these relevant or likely to improve care (theme 7). For example, when a worker seems to be coping adequately and re-integration is proceeding as expected, OHPs are less inclined to ask about SOs’ cognitions and behavioral responses. For example, an occupational physician wrote:
If there is no reason to do so or if the clinical picture is clear and reintegration is proceeding well
OHPs also reported not asking about this due to lack of time (theme 8) or because of giving priority to the worker’s perspective instead of that of SOs (theme 9). For instance, an insurance physician stated:
I primarily want to know about the experience of the person concerned
Some OHPs also indicated feeling that an SO would be a disruptive factor in the conversation (theme 10), and that it would be a breach of the worker’s privacy to ask about SOs’ views and reactions and, moreover, a difficult or sensitive topic to discuss (theme 11). For example, an insurance physician wrote:
When it is expected that the significant other wants to take over the conversation from the person concerned
Furthermore, OHPs reported not asking about the views and reactions of SOs if the latter were not present during the consultation (theme 12). To illustrate, an occupational physician indicated:
In my opinion, you can only ask that to the significant other him- or herself, not to the person concerned. Therefore, in my opinion this is only possible if the significant other is present, and this is more often not the case
In addition, OHPs reported not always needing to ask specific questions because certain topics were sometimes raised naturally (theme 13). Others reported not asking unless the topic was brought up during the consultation (theme 14). Finally, OHPs reported not always thinking of asking about SOs’ views and reactions (theme 15), and not always having a specific or conscious reason not to ask about these factors (theme 16). For example, an insurance physician answered:
Never a conscious reason not to do it, actually
Discussion
In this mixed method survey study, we aimed to examine current practices of OHPs in the assessment of SOs’ cognitions and behavioral responses that could influence work outcomes of workers with a chronic disease. Our findings indicate that most OHPs do not commonly ask about SOs’ illness perceptions, work-related beliefs, and expectations, and behavioral responses, despite the possible influence of these factors on work outcomes, as well as guideline recommendations to address social factors in occupational health care. Although OHPs did report to frequently assess practical support by SOs, this was not the case for other behavioral responses and cognitions of significant others. These reported assessment practices were related to both organizational norms and OHPs’ self-efficacy to address these factors. Furthermore, OHPs reported multiple reasons for asking or not asking about these issues; their answers to the open-ended questions indicate that they do not always find it necessary to ask, either because recovery and re-integration are going well or because they see no indication that SOs have a strong influence. However, in the presence of mental health problems, severe complaints, coping issues and stagnation of the re-integration process, OHPs do seem more inclined to inquire about SOs’ cognitions and behavioral responses.
There are several possible explanations for most OHPs’ low assessment frequency of SOs’ cognitions and behavioral responses. First, OHPs may often feel that asking about this would not contribute to better care, and indeed our results indicate that OHPs feel that this is beneficial only under certain circumstances. Studies in other fields have also suggested that the effectiveness of involving SOs in interventions may depend on circumstances or conditions such as gender, illness severity, and whether or not the significant other is unsupportive prior to intervention [Citation37–39]. This could also be the case for occupational health care. However, more research on this is needed.
Moreover, our results indicate a relationship between OHPs’ assessment practices and their self-efficacy to assess and effectively respond to SOs’ cognitions and behavioral responses. Although family interventions and education and training programs on the involvement of SOs are available for mental health care professionals [Citation40,Citation41], this is not the case for OHPs. Moreover, no tools or instruments are currently available for OHPs to assess and intervene on SOs’ illness perceptions, work-related beliefs and expectations, and behavioral responses. This lack of available education, interventions, tools, and clear guidelines may thus partly explain OHPs’ lack of attention to these factors.
Barriers within OHPs’ organizations may also partially explain why OHPs do not frequently assess SOs’ cognitions and behavioral responses. Several OHPs reported lack of time and the absence of a significant other during the consultation as reasons not to ask about this. Moreover, the organizational norm appears to play an important role, which is in line with other studies that indicate that perceived social norms can influence intentions, decision making, and behaviors of health professionals [Citation42–45]. Organizations could facilitate the involvement of SOs by making it common practice to invite them to attend one or more consultations and by providing OHPs with more time and resources. It is thus important for organizations to recognize the importance of involving SOs in occupational health care.
Barriers in the occupational health care system may be another explanation for the low assessment frequencies. For example, although multiple Dutch occupational health guidelines recommend that OHPs address factors in the social environment [Citation24,Citation17,Citation46,Citation47], each guideline specifies only a few relevant factors (e.g., overprotection, social support, irrational fears or beliefs that hinder recovery). This might be due to the lack of quantitative evidence on the influence of specific cognitions and behavioral responses of SOs on work outcomes, as most research available on this topic is qualitative. Therefore, a higher level of evidence requires more quantitative research [Citation4].
Strengths and limitations
A strength of this study is our use of a mixed-method design to collect both quantitative and qualitative data in a representative population of OHPs. The invitation letter and link to the survey were distributed through the three largest professional associations for occupational and insurance physicians in the Netherlands, potentially reaching more than 80 percent of Dutch OHPs [Citation36,Citation48]. Although the estimated response rate of this study was low (10.7%), our sample appears to be a good reflection of the total population of Dutch OHPs registered as of 1 January 2016, with regard to age, gender, and proportion of occupational versus insurance physicians [Citation36]. Moreover, we derived the items of our survey from validated questionnaires, and all constructs had high internal consistencies.
As this study took place within the Dutch occupational health care system and was explorative in nature, the generalizability of our results is limited. To the best of our knowledge, similar studies have not been conducted in other countries; as a result, the extent to which OHPs in other countries pay attention to SOs’ cognitions and behavioral responses remains unknown. Our results can therefore not be compared to other findings.
Furthermore, as OHPs’ self-reported practices may not accurately represent their actual practices, a social desirability bias must also be considered. Although our results indicate that OHPs seldom assess SOs’ cognitions and behavioral responses, an even smaller frequency may be possible. However, our survey focused on specific illness perceptions, work-related beliefs and expectations, and behavioral responses of SOs that could influence work participation; while many OHPs may not ask about these specific factors, they may address social factors in other ways, for example, by asking more in general about a worker’s social context.
Implications and recommendations for future research and occupational health practice
This study provided insight into OHPs’ practices and their perspectives as to the involvement of SOs in occupational health care, including a number of implications for occupational health practice. In addition, we have several recommendations for future research.
First, it is important to better understand the perspectives of different stakeholders on involving SOs in occupational health care and methods to implement SO involvement in daily practice. Such insight can provide an empirical basis for recommendations on how to involve SOs in occupational health care. Such information could also be used in the development of training programs and tools for this purpose. Future research should, therefore, focus on gaining more insight into this topic from the perspective of OHPs, as well as that of workers with a chronic disease and their SOs.
Our findings furthermore suggest that the benefits of assessing SOs’ cognitions and behavioral responses may depend on various contextual and case-specific factors (e.g., re-integration versus claim assessment, complexity of the case, and re-integration progress). These findings are in line with prior research in other fields which has also pointed to possible other factors influencing the effectiveness of involving SOs in interventions: factors like gender, illness severity, and lack of support [Citation37–39]. However, more research on this question is needed. Moreover, because of important implications for practice, such future research should focus on exploring which factors determine the relevance of involving SOs.
Conclusions
Our study shows that OHPs do not commonly assess SOs’ cognitions and behavioral responses, despite recognizing that these factors can influence work outcomes. Both the organizational norm and OHPs’ self-efficacy appear to play a role in their descisions. Qualitative data showed that one important reason for OHPs not to ask about SOs’ cognitions and behavioral responses is that recovery and re-integration are going well. Nevertheless, OHPs are more inclined to ask about this when perceiving mental health problems, severe complaints, coping issues and/or stagnation of the re-integration process. Our findings indicate that OHPs may be able to better support workers with a chronic disease in their self-management and ability to work by paying more attention to the influence of SOs. However, more research is needed on how to address SOs’ cognitions and behavioral responses and to determine which circumstances influence the effectiveness of involving others in occupational health care.
Ethical approval
This study is exempted from ethical approval by the Medical Ethics Review Committee of the University Medical Center Groningen (METc 2017/486, M17.218841). Informed consent was obtained from all individual participants included in the study.
Supplementary_Table_S1.docx
Download MS Word (19.8 KB)Acknowledgements
We would like to thank Marion Bloemendal, Arjen Ras, Jan Timmer, Cora Westland and Jan Zwagemakers for their contribution to the development of the survey. We would also like to thank Daniël Bossen, the Dutch Association of Occupational Medicine (NVAB), the Dutch Association for Insurance Medicine (NVVG), and the Dutch Association of Medical Advisers in Private Insurance (GAV) for their contribution to the distribution of the survey.
Disclosure statement
Drs. Snippen, Dr. de Vries, and Prof. Brouwer received grants from Instituut Gak to conduct the study; Drs. de Wit, Dr. van der Burg-Vermeulen and Prof. Hagedoorn have nothing to disclose.
Data availability
The dataset generated during this study is available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133(6):920–954.
- Cano A, Leong L. Significant others in the chronicity of pain and disability. In: Hasenbring M, Rusu A, Turk D, editors. From acute to chronic back pain: risk factors, mechanisms, and clinical implications. Oxford, England: Oxford University Press; 2012. p. 339–354.
- White C, Green RA, Ferguson S, et al. The influence of social support and social integration factors on return to work outcomes for individuals with work-related injuries: a systematic review. J Occup Rehabil. 2019;29:636–659.
- Snippen NC, de Vries H, van der Burg-Vermeulen S, et al. Influence of significant others on work participation of individuals with chronic diseases: a systematic review. BMJ Open. 2019;9(1):e021742.
- Helgeson VS, Zajdel M. Adjusting to chronic health conditions. Annu Rev Psychol. 2017;68:545571.
- Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003;30:170–195.
- Frederiksen P, Karsten MMV, Indahl A, et al. What challenges manual workers’ ability to cope with back pain at work, and what influences their decision to call in sick? J Occup Rehabil. 2015;25(4):707–716.
- Dorland HF, Abma FI, Roelen CAM, et al. Factors influencing work functioning after cancer diagnosis: a focus group study with cancer survivors and occupational health professionals. Support Care Cancer. 2016;24(1):261–266.
- Bodenmann G, Randall AK, Falconier MK. Coping in couples: the Systemic Transactional Model (STM). In: Couples coping with stress: a cross-cultural perspective. New York: Routledge; 2016. p. 31–48.
- Brooks J, McCluskey S, King N, et al. Illness perceptions in the context of differing work participation outcomes: exploring the influence of significant others in persistent back pain. BMC Musculoskelet Disord. 2013;14(1):48.
- McCluskey S, de Vries H, Reneman M, et al. I think positivity breeds positivity’: a qualitative exploration of the role of family members in supporting those with chronic musculoskeletal pain to stay at work. BMC Fam Pract. 2015;16(1):85.
- Gagnon A, Lin J, Stergiou-Kita M. Family members facilitating community re-integration and return to productivity following traumatic brain injury – motivations, roles and challenges. Disabil Rehabil. 2016;38(5):433–441.
- Tamminga SJ, de Boer A, Verbeek J, et al. Breast cancer survivors’ views of factors that influence the return-to-work process–a qualitative study. Scand J Work Environ Health. 2012;38(2):144–154.
- Kong W, Tang D, Luo X, et al. Prediction of return to work outcomes under an injured worker case management program. J Occup Rehabil. 2012;22(2):230–240.
- Sandstrom J, Esbjornsson E. Return to work after rehabilitation. The significance of the patient’s own prediction. Scand J Rehabil Med. 1986;18:29–33.
- Centre for Clinical Practice at NICE (UK). Rehabilitation after critical illness. London: National Institute for Health and Clinical Excellence; 2009. p. 83.
- van Dijk JL, Bekedam MA, Brouwer W, et al. Richtlijn Ischemische Hartziekten [Guideline Ischemic Heart Disease]. Utrecht: 2007 [cited 2019 Feb 21]. Available from: www.nvab-online.nl.
- Vooijs IM. Supporting work participation of people with a chronic disease. 2018.
- De Koninklijke Nederlandsche Maatschappij tot bevordering der Geneeskunst (KNMG). KNMG RGS Overzicht aantal geregistreerde specialisten/profielartsen 2008–2018 [Royal Dutch Society for the Advancement of Medicine, Registration Committee for Medical Specialists. Overview number of registered specialists/profile doctors 2008–2018]. 20-02-2018. 2018 [cited 2018 Oct 30]. Available from: https://www.knmg.nl/opleiding-herregistratie-carriere/rgs/registers/aantal-registraties-specialistenaois.htm.
- McDougall J, Wright V, Rosenbaum P. The ICF model of functioning and disability: Incorporating quality of life and human development. Dev Neurorehabil. 2010;13(3):204–211.
- World Health Organization. ICF: international classification of functioning, disability and health. Geneva: World Health Organization; 2001.
- Kant I, Van Amelsvoort L. Applying a biopsychosocial perspective in occupational health: Easier said than done! Work. 2017;57(2):149–151.
- Boonen A. Werk en sociale zekerheid [Work and social security]. In: Bijlsma JWJ, Lems WF, Wildervanck-Dekker CMJ, editors. Reumatologie. Houten: Bohn Stafleu van Loghum; 2015. p. 361–371.
- Vooijs M, van der Heide I, Leensen MCJ, et al. Richtlijn Chronisch Zieken en Werk [Guideline ‘The chronically ill and work’]. Amsterdam: Coronel Institute of Occupational Health; 2016. Available from: https://www.psynip.nl/wp-content/uploads/2017/03/Richtlijn_chronisch_zieken_en_werk_2016.pdf
- Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic pain. Edinburgh: SIGN; 2013.
- Scottish Intercollegiate Guidelines Network (SIGN). Brain injury rehabilitation in adults. Edinburgh: SIGN; 2013. Available from: http://www.sign.ac.uk/assets/sign130.pdf
- National Institute for Health and Care Excellence. Stroke rehabilitation in adults. NICE. 2013;1:44.
- National Institute for Health and Clinical Excellence. Depression in adults: recognition and management. Clinical Guideline [CG90]. 2009.
- de Raaij EJ, Schröder C, Maissan FJ, et al. Cross-cultural adaptation and measurement properties of the Brief Illness Perception Questionnaire-Dutch language version. Man Ther. 2012;17(4):330–335.
- van Driel D, Hanssen D, Hilderink P, et al. Illness cognitions in later life: development and validation of the extended Illness Cognition Questionnaire (ICQ-Plus). Psychol Assess. 2016;28(9):1119–1127.
- Shaw WS, Reme SE, Linton SJ, et al. 3rd place, PREMUS 1 best paper competition: development of the return-to-work self-efficacy (RTWSE-19) questionnaire – psychometric properties and predictive validity. Scand J Work Environ Health. 2011;37(2):109–119.
- Gross DP, Battié MC. Work-related recovery expectations and the prognosis of chronic low back pain within a workers’ compensation setting. J Occup Environ Med. 2005;47(4):428–433.
- Kinsinger SW, Laurenceau J-P, Carver CS, et al. Perceived partner support and psychosexual adjustment to breast cancer. Psychol Health. 2011;26(12):1571–1588.
- IBM Corp. Released 2017. IBM SPSS statistics for windows, Version 25. Armonk (NY): IBM Corp; 2017.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Capaciteitsorgaan. Capaciteitsplan 2016. Deelrapport 4. Sociaal Geneeskundigen. [Capacity plan 2016. Sub-report 4. Social Medicine]. Utrecht; 2016.
- Shields CG, Finley MA, Chawla N, et al. Couple and family interventions in health problems. J Marital Fam Ther. 2012;38(1):265–280.
- Martire LM, Schulz R. Involving family in psychosocial interventions for chronic illness. Curr Dir Psychol Sci. 2007;16(2):90–94.
- Martire LM, Lustig AP, Schulz R, et al. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychol. 2004;23(6):599.
- Netwerk Kwaliteitsontwikkeling GGZ. Generieke module: Samenwerking en ondersteuning naasten van mensen met psychische problematiek [Generic module: Collaboration with and support of significant others of people with psychological problems]. 2016 [cited 2019 Feb 5]. Available from: https://www.ggzstandaarden.nl/generieke-modules/samenwerking-en-ondersteuning-naasten-van-mensen-met-psychische-problematiek/achtergronddocumenten.
- American Psychological Association. Public interest directorate report: family interventions. 2011 [cited 2019 Feb 13]. Avaiable from: https://www.apa.org/pi/about/publications/caregivers/practice-settings/intervention/family.
- Pittet D, Simon A, Hugonnet S, et al. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1–8.
- Askelson NM, Campo S, Lowe JB, et al. Factors related to physicians’ willingness to vaccinate girls against HPV: the importance of subjective norms and perceived behavioral control. Women Health. 2010;50(2):144–158.
- Kretzer EK, Larson EL. Behavioral interventions to improve infection control practices. Am J Infect Control. 1998;26(3):245–253.
- Smith M, Higgs J, Ellis E. Factors influencing clinical decision making. Clin Reason Health Prof. 2008;3:89–100.
- van Son MAC, Hulshof CTJ, Bruinvels DJ, et al. Richtlijn Kanker en Werk [Guideline Cancer and Work]. Utrecht: NVAB; 2017.
- Verschuren CM, Nauta AP, Bastiaanssen MHH, et al. Richtlijn ‘Eén lijn in de eerste lijn bij overspanning en burnout’ [Guideline ‘On one line in the first line in case of nervous exhaustion or burnout’]. Amsterdam/Utrecht: LVE, NHG, NVA; 2012.
- Fortuin F. NVAB, the Netherlands society of occupational medicine. 2014 [cited 2019 Feb 26]. Available from: https://www.nvab-online.nl/english/english.
