Abstract
Introduction
Following distal radius fractures in young non-osteoporotic patients, clinical relevancy of outcome has been scarcely reported. Outcome can be put in perspective by using measurement errors of radiological measurements and Minimal Important Change when reporting on clinician and patient reported outcome. Aim of this study was to assess the clinical relevance of radiological measurements, clinician and patient reported outcomes following distal radius fractures in young non-osteoporotic patients.
Methods
Retrospective cohort study. Non-osteoporotic patients following a distal radius fracture were selected. Radiographs of both wrists were obtained at baseline, 6 weeks and at follow-up. Active range of motion and grip strength measurements were obtained at the follow-up visit and 4 questionnaires were answered to assess pain, upper extremity functioning, and health status.
Results
Seventy-three patients (32 women, 41 men) with a mean age of 33.5 (SD 9.2) years at the time of injury were included. Median follow up was 62 months (IQR 53.0–84.5). Several radiological measurements evolved statistically significantly over time, however none exceeded measurement errors. Flexion/extension difference of injured compared to uninjured wrist (mean difference 11.2°, t = −7.5, df = 72, p < 0.001), exceeded Minimal Important Change, while grip strength differences did not. When comparing patients with DRFs to healthy controls, only the differences on Patient Reported Wrist Evaluation subscales “pain”, “function” and total scores exceeded minimal important change (8, 10 and 13 points, respectively). Multivariable regression analysis revealed statistically significant relationships between residual step-off and respectively diminished flexion/extension (B = −36.8, 95% CI −62; −11.1, p = 0.006), diminished radial/ulnar deviation (B = −17.9, 95% CI −32.0; −3.9, p = 0.013) and worse ShortForm-36 “mental component score” (B = −15.4, 95% CI −26.6; −4.2, p < 0.001).
Conclusion
Radiological measurements following distal radius fractures seem to evolve over time, but differences were small and were probably not clinically relevant. Range of motion, in particular flexion/extension, was impaired to such extend that it was noticeable for a patient, whereas grip strength was not impaired. The Patient Reported Wrist Evaluation was clinically relevantly diminished. Residual articular incongruency seems to influence range of motion.
Reporting Minimal Important Change regarding clinician and patient reported outcome following distal radius fractures is of more clinical value than reporting on statistical significance.
Following distal radius fractures, the changes in radiological measurements do not seem to reflect a clinical relevant change.
Range of motion, in particular flexion/extension, should be measured following distal radius fractures, as this might be impaired in a clinically relevant way.
Measuring grip strength is of less importance following distal radius fractures, because grip strength does not seem to be affected.
Residual articular incongruency seems to influence range of motion and therefore should be reduced to a minimum when treating non-osteoporotic patients.
Implications for rehabilitation
Introduction
Associations of radiological measurements with outcomes in young non-osteoporotic patients who sustained a distal radius fracture (DRF) have been described in a limited number of studies [Citation1–3]. Radiological measurements that have mostly been used to describe the anatomy of the distal radius following a fracture are ulnar variance, radial length, radial inclination and dorsal angulation [Citation4–9]. Normal ranges for radiological measurements have previously been described [Citation4–9]. Recent literature puts these measurements in perspective by reporting on questionable intra- and interrater reliability and considerable error magnitudes of radiological measurements following DRFs [Citation10]. In addition, it has been described that DRFs in young non-osteoporotic patients often have intra-articular involvement, since they are more involved in high-energy trauma than older people, who mostly sustain DRFs after low or medium energy trauma [Citation11]. This can result in residual articular incongruence, which is usually described in step-offs and gaps [Citation12–17]. Error magnitudes of residual gaps and/or steps have been reported to be within 1–2 mm [Citation10]. As intra- and interobserver reliability of measuring residual gap and step were reported to be moderate to poor, it has been questioned if these radiographic measurements should be used as criteria for guiding treatment to be conservative or surgical [Citation10,Citation18]. Intercarpal ligamentous injuries, radiologically reflected in the distance between scaphoid and lunate (SL distance) and distal radio-ulnar joint (DRUJ) instability are also associated with DRFs and might influence outcome [Citation11,Citation19,Citation20].
To interpret change scores of Clinician Reported Outcomes (CROs: range of motion or grip strength), and Patient Reported Outcomes (PROs: questionnaires) two benchmarks are required: the smallest detectable change (SDC) and the minimal important change (MIC), which the Consensus-based Standards for the development of Measurement Instruments (COSMIN) group defines as respectively “the smallest change that can be detected by the instrument, beyond measurement error” and ‘the smallest change in construct to be measured which patients perceive as important [Citation21–23]. Most literature reports on SDC when reporting on outcomes following DRFs. This is a statistical measurement and does not take into account change as experienced by patients. Clinically more relevant is the MIC, which is the smallest change in an outcome measurement that a patient would perceive as important [Citation21–24]. If the value of the MIC is less than that of the SDC, the MIC is within the limit of measurement errors or change [Citation25,Citation26]. Therefore, the MIC represents true clinical change when the value of the MIC is more than that of the SDC. The MIC threshold is very important in daily practice, where clinicians can compare at a patients’ individual level, the current and previous values of outcome measures of interest. MICs regarding outcomes following DRFs have been reported scarcely on CROs [Citation27,Citation28] and PROs [Citation29–31].
The association between radiological measurements and CROs, such as active range of motion (aROM) and grip strength measurements, remains unclear [Citation1,Citation8,Citation13,Citation32–39]. The association between radiological parameters and PROs presents conflicting results regarding patients of osteoporotic ages [Citation13,Citation33,Citation34,Citation40]. However, in young patients malalignment and ligamentous injury following DRFs is significantly more often associated with poorer CROs and PROs than in patients over 60 years of age [Citation2,Citation3]. We hypothesize that non-osteoporotic patients have higher demands of their wrist, because of an active working life and therefore might experience more impact of diminished function in daily life.
Summarizing existing literature, there seems to be a need for better understanding of changes in radiological measurements, their relation with outcomes and clinical relevancy of both radiological measurements and outcomes in young non-osteoporotic patients who sustained a DRF.
Aim
The aim of this study was to assess the clinical relevance of radiological, CROs, PROs following DRFs. The objective of this study was threefold; (1) to report on the clinical relevance of changes in radiological measurements, (2) to report on the clinical relevance of CROs and PROs and (3) to analyze associations between radiological measurements and CROs and PROs following DRFs in young non-osteoporotic patients.
Methods
This retrospective cohort study was approved by the Medical Ethics Committee (NL41587.099.13) and registered at the Dutch Trial Registration (TC 4002). Before entering the study, participants signed an informed consent form. All patients with a DRF who presented at a level II trauma center between January 2005 and January 2011 and who were considered to be in a non-osteoporotic age range (men 18–50 years, women 18–40 years at the time of the injury) were retrieved from the local trauma registry database. The age criteria were chosen to minimize the chance of including patients with pre-existent osteoporosis [Citation41–43]. Medical histories regarding risk factors for osteoporosis and the radiographs were analyzed as well for signs of osteoporosis and patients were excluded if osteoporosis was present. Additional exclusion criteria were fractures treated after the 7th day following injury, open fractures, pre-existing osteoarthritis or risk factors for early osteoporosis (steroid use, alcohol abuse or early menopause), because outcomes in patients with these risk factors might not be representative for non-osteoporotic patients.
Patients were invited to pay a single visit to the hospital for functional measurements and radiographs of both wrists. Radiographs were retrieved before treatment, immediately after intervention (closed reduction or surgical treatment), at 6 weeks following injury and at the participants’ visit at follow up. For this study, baseline radiographs were defined as the accepted position of the DRF (either not needing reduction or following intervention) within 7 days following injury. At the time of the participants’ visit, lateral (Lundy) and posteroanterior (PA) wrist radiographs were made of both wrists. According to the international commission on radiological protection the estimated risk for the radiological procedure (4 x-rays per participant) is categorized as a very low level of risk of radiogenic cancer, >0.2 and <2 mSv [Citation44]. All radiographs (baseline, 6 weeks and at follow up) were evaluated by a single radiologist specialized in musculoskeletal disorders with a special interest in hand and wrist anatomy.
Radiological parameters were measured according to the technique described by Kreder et al.; ulnar variance, radial length, radial inclination and dorsal angulation and step-off and gap () [Citation18,Citation45]. In addition, the SL distance [Citation46,Citation47] and the DRUJ space were measured [Citation48,Citation49] (). Normal ranges and error magnitudes for radiological factors have previously been described and are depicted in .
Figure 1. (A) Posteroanterior measurement guidelines: (1) The center of the radial shaft is determined at 3 cm and 5 cm below the mid-region of the proximal lunate articular surface. This line represents the central axis of the radius. (2) A line perpendicular to the central long axis of the radius is drawn at the level of the most distal aspect of the radial articular surface. (3) A line perpendicular to the central long axis of the radius is drawn at the level of the ulnar margin of the distal radial articular surface. (4) The radial and ulnar margins of the distal radial articular surface are connected. (5) A line perpendicular to the central long axis of the radius is drawn at the level of the distal ulnar articular surface. (B) Lateral measurement guidelines: (1) The center of the radial shaft is determined at 3 cm and 5 cm below the mid-region of the proximal lunate articular surface. This line represents the central long axis of the radius. (2) A line perpendicular to the central long axis of the radius is drawn at a convenient level. (3) The dorsal and anterior margins of the distal radial articular surface are connected. (C) Step-off and gap measurement. (1) Step-off at the articular surface of the distal radius was measured parallel to the central long axis of the radius by drawing perpendicular lines from the most distal margin of each side of the articular incongruence. (2) Gap deformity was measured along a perpendicular line to the central long axis of the radius. UV: ulnar variation; RL: radial length; RI: radial inclination; DT: dorsal tilt; SL: scapholunate ligament; DRUJ: distal radioulnar joint.
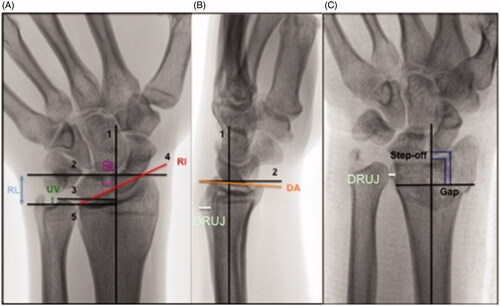
Table 1. Reference values, error magnitudes for radiological measurements and SDCs and MICs for CROs and PROs.
To correct for anatomical variation between patients, radiographs of the uninjured wrist were obtained at follow up and used as a reference to interpret measurements of the injured wrist at baseline, at 6 weeks and at follow up.
At the visit to the hospital at follow up, a single hand therapist recorded all CROs: active range of motion (aROM) and strength measurements. The participants were positioned sitting at a table, with hips and knees flexed in 90 degrees. Elbows were positioned on the table and flexed in 90 degrees with wrists in neutral position. The aROM of flexion/extension, ulnar/radial deviation and supination/pronation was measured using a digital protractor of Biometrics LTD and computed using E-Link® software and was presented in degrees. Grip strength, sustained grip strength and key pinch strength were measured using a digital Jamar dynamometer using Biometrics LTD and E-Link® software and presented in kilograms and as percentage of the uninjured hand. Grip strength and key pinch strength were presented in kilograms, and were derived from the maximum peak strength sustained during at least 2 s. The mean of three performances was calculated. For assessing sustained grip strength, patients were asked to grip as hard as they could using the dynamometer during a 30 s period. Sustained grip strength is the average grip strength in kilograms, computed over the last 18 s of this 30-s period. For people with right sided dominance it is known that the right hand has 10% more grip strength in comparison to the left hand [Citation51]. This is not the case when people are left sided dominant or ambidexter; grip strength in both hands is similar. Therefore, correction for dominance with the 10% rule was performed for grip strength measurements in individuals with right sided dominancy. First, all aROM measurements were recorded and subsequently grip strength measurements were assessed. Measurements were performed for both wrists. In addition, reference values for CROs in a healthy population (n = 22, median age 48.5 years, IQR 39.5; 64.3) were derived from a previous published paper by our research group () [Citation50]. The SDCs en MICs as reported in literature for flexion/extension and grip strength are reported in [Citation27,Citation28].
All patients completed 4 questionnaires involving pain scores, specific upper extremity functioning, and health status. Reference values for PROs in a healthy population were derived from the earlier mentioned 22 healthy controls () [Citation50].
The Disability of Arm, Shoulder and Hand (DASH) Questionnaire is a 30-item self-report measure assessing physical functioning and symptoms of the upper limb. DASH-scores range from 0 to 100 (higher scores indicate worse function). The DASH has a good validity, reliability and responsiveness in upper extremity disability assessment [Citation52,Citation53]. MIC of the DASH questionnaire has been described to be 10.83 points and SDC 10.81 points in 255 patients following upper limb musculoskeletal disorders with a mean age of 49 years and short follow up duration () [Citation29].
The Patient Rated Wrist Evaluation (PRWE) is a 15-item questionnaire divided into two subscales: pain (5 items) and function (10 items). The PRWE was developed to assess pain and functioning in patients with DRFs [Citation54]. The pain items were selected to represent the total spectrum of frequency and intensity. The function items were selected to represent a range of physical activities that require different ranges of motions or muscle strength capabilities. For both subscales the maximum score is 50 (most disability) and the minimum score is 0 (no disability). Although these subscales have been reported frequently in literature, it has been suggested that the PRWE measures a single dimensional trait, and a single (sum) score should be used [Citation55]. The questionnaire has a good validity for symptoms and function of the wrist [Citation56]. For the PRWE following DRFs in 102 patients with mean age of 59 years, MIC has been determined at 11.5 points, while SDC was achieved at 11.0 points () [Citation31].
The Michigan Hand Outcomes Questionnaire (MHQ) assesses hand outcomes that are of importance to patients and specifically for the impaired hand (left and right separately) and includes 6 subscales; general function, activities of general life, work, pain, esthetics and satisfaction. The subscale score is the sum of the outcome of each question and ranges from 0 to 100. A higher score on the pain subscale indicates less pain. For the other five subscales and the total score higher scores imply a better function. The MHQ compares favourably with other PROs regarding upper extremity in the area of test-retest reliability, validity and responsiveness. In addition it has high internal consistence [Citation57]. The strength of the MHQ is its multidimensional construct in measuring symptoms, function, aesthetics and satisfaction [Citation57]. It has been reported that no discriminative ability is present as captured in MIC for the MHQ following DRFs, because of the ceiling effect with high scores at 3 months follow up and only a mean change of 10 points (mean score 3 months 78, mean score 12 months 89) [Citation30].
The SF-36 is developed to survey overall health status [Citation58]. It contains 36 questions to assess limitations in (1) physical function, (2) role function, (3) social function, (4) bodily pain, (5) general mental health, (6) limitations in role function due to emotional problems, (7) vitality and (8) general health perception. Scale scores range from 0 to 100 with higher scores indicating a better health status. Scale scores can be used to calculate a physical and a mental component summary score [Citation58]. Validity of this questionnaire is sufficient for groups reporting varying extents of illness-health [Citation59]. To our knowledge, no SDC or MIC values regarding the SF36 have been published.
Statistical analysis
Continuous data were presented as means (SD) or as median (IQR) if no normal distribution of the data was present. T-tests were performed when analyzing continuous variables if a normal distribution was found and outcome was presented with t-values and degrees of freedom (df). If continuous data did not have a normal distribution, Mann Whitney U tests were applied and outcome was presented with U-values. Explanatory variables were included in the multivariable regression analysis when the p-value was ≤0.2 in the univariable regression analysis. Multivariable linear regression analysis, using backward stepwise selection (until all p values were ≤0.2 to avoid excluding important risk factors) was performed analyzing radiological measurements as explanatory variables and CROs and PROs as dependent variables. Outcome of the multivariable regression analyses were presented with B-values (regression coefficient). Level of significance was set at p ≤ 0.05. All statistical analyses were performed using IBM SPSS, version 22.
Results
A total of 433 patients fulfilled the inclusion criteria and received an invitation to participate in the study. A notification of changed home address was received from 43 participants of whom current addresses could not be retrieved. From 306 patients, no response was received. Eighty-four patients responded of which seventy-three patients (32 women, 41 men) with a mean age of 33.5 (SD 9.2) years at the time of injury, consented for participation after a median follow up of 62.0 months (IQR 53.0–84.5) ().
Table 2. Patient characteristics.
Radiological measurements
Baseline versus six weeks
DRUJ distance increased between baseline and 6 weeks post-injury (2.0 versus 2.4 mm, t = −2.3, df = 42, p = 0.024). No other statistical significant differences between the measurements at baseline and 6 weeks were present and all measurement changes were within magnitude error (). SL distance at baseline and at 6 weeks exceeded the normal range of <2.0 mm by 0.2 mm.
Table 3. Radiological measurements at baseline, 6 weeks and follow up.
Six weeks versus follow-up
Between 6 weeks and follow-up, ulnar variance and radial inclination increased ((mean 0.4 mm versus 1.12 mm, t = −4.3, df = 49, p < 0.001 and 24.3° versus 25.2°, t = −2.3, df = 49, p = 0.028, respectively) increased (). In contrast, the step-offs and gaps diminished (step-off 0.4 versus 0.1 mm, t = 2.2, df = 31, p = 0.032, gap 1.5 versus 0.1 mm, t = 3.7, df = 33, p = 0.001) (). However, none of the measurement changes exceeded error magnitudes. SL distance at 6 weeks and follow-up exceeded the normal range of <2.0 mm with respectively 0.2 and 0.1 mm.
Injured versus uninjured wrist
When comparing the radiological measurements of the injured to the uninjured wrist at follow up, dorsal angulation was statistically significantly more pronounced in the injured wrist (−1.3° versus −5.1°, t = 5.0, df = 72, p < 0.001) (). This measurement change did not exceed the reported error magnitude of 6–8°.
Table 4. Radiological measurements of the inured and uninjured wrist at follow-up.
CROs
All aROM measurements of the injured wrist were statistically significantly lower in comparison to the uninjured wrist at follow up (respectively flexion/extension 141.3° versus 152.5°, t = −7.5, df = 72; ulnar/radial deviation 58.1° versus 649.9°, t = −5.9, df = 72; pro/supination 146.7 versus 152.0°, t = −3.4, df = 72, all p < 0.001) (). With regard to flexion/extension the difference of 11.2° exceeded the reported MIC of 5.0–7.1°.
Table 5. CROs derived from injured and uninjured wrist at follow-up.
Grip strength of the injured wrist was statistically significantly lower in comparison to the uninjured wrist at follow up (respectively 43.5 kg versus 46.1 kg, t = −3.8, df = 72, p < 0.001) (). The grip strength difference of 2.6 kg between the injured and uninjured wrist did not exceed the reported MIC of 6.5 kg.
PROs
When comparing PROs with outcomes as reported for healthy controls, the differences for PRWE subscales pain (8), function (10) and total PRWE score (13) all exceeded the reported MICs. The difference between DASH scores did not exceed the reported MIC of 10.83 ().
Table 6. PROs at follow up compared to measurements of healthy controls.
Associations between radiological measurements, CROs and PROs
The results of the univariable regression analyses are presented in and . Multivariable regression analyses revealed that step-off was statistically significantly associated with diminished flexion/extension as well as ulnar/radial deviation (respectively B = −36.8, p = 0.006 and B = −17.9, p = 0.013, respectively) (). Multivariable analyses revealed that shorter radial length was associated with diminished grip strength, sustained grip strength and key pinch strength measurements (B = 2.8, B = 2.1, and B = 0.5, all p < 0.001, respectively) ().
Table 7. Univariable regression analyses of radiological measurements and CROs.
Table 8. Univariable regression analyses for radiological measurements and PROs.
Table 9. Multivariable regression analyses of radiological measurements and CROs.
Only SF36 physical component score and mental component score were entered in the multivariable regression analyses (). SF36 mental component score was associated with step-off (B = −15.4, p = 0.008).
Table 10. Multivariable linear regression analysis for radiological measurements and PROs.
Discussion
Multiple radiological measurements changed statistically significantly over time. However, none of the measurement changes exceeded reported magnitude errors. As such, clinical relevancy could not be revealed.
All aROM measurements were statistically significantly diminished in the injured wrist compared to the uninjured wrist. Since MIC is only reported for flexion/extension, this finding appeared to be clinically relevant. Although grip strength was statistically significantly lower in the injured wrist, the difference was not clinically relevant. The differences between patients with DRFs and healthy controls for PRWE subscales pain, function and total PRWE score all exceeded the reported MICs, suggesting a clinically relevant diminished score for non-osteoporotic patients following a DRF. Associations between radiological measurements and outcomes were found for step-off and diminished flexion/extension as well as ulnar/radial deviation and SF 36 mental component score. Radial length was associated with all grip strength measurements.
The evolution of radiological measurements in perspective
Ulnar variation, radial length, radial inclination and dorsal angulation were within normal ranges as presented in literature at all follow-up moments [Citation4–9]. Neidenbach et al. stated that most changes of radiological measurements occur in the first 6 weeks following injury [Citation34]. Although this seems to be logical, our study did not show many signs of radiological changes in the first 6 weeks following initial treatment after a DRF. Although these authors stated that no changes in radiological measurements occur between 6 weeks and 1 year follow-up, our study did suggest that ulnar variance and radial inclination increased and step-off and gaps diminished during 5 years following a DRF[Citation34]. When ulnar variance and radial inclination increase, but radial length does not increase, a compression (and relative shortening) of the ulnar side of the distal radius must be present. Rikli and Regazzoni described this anatomical area in 1996 as the intermediate column [Citation60,Citation61]. It consists of the lunate facet and the sigmoid notch and is responsible for >50% of the axial compressive forces that are transmitted across the wrist during normal activity [Citation62]. Brink and Rikli acknowledge the importance of the intermediate column and describe the volar and dorsal “key corner” of the intermediate column [Citation61]. They state that control with reduction and stable fixation of this “key corner” should be the first step of the operative strategy after a DRF, because insufficient treatment may result in carpal subluxation [Citation61]. Our results suggest that the intermediate column is likely to be compressed after 6 weeks following a DRF, which may result in shortening. We agree with Brink and Rikli that care should be taken to pursue anatomical reduction and stable fixation of the intermediate column. However, when comparing the differences in measurements in our study to reported magnitude error by Watson et al., all findings were within the 95% confidence interval of expected normal ranges [Citation10]. This suggests that the evolution of these radiological measurements over time might be regarded as measurement error and might not yield a clinically relevant change.
SL distance in our study exceeded the normal value of <2.0 mm with only 0.1–0.2 mm and was not statistically significantly different in comparison to measurements of the uninjured wrist [Citation47]. In addition to proper physical examination, it has been reported that diagnosing concomitant ligamentous injury on static radiographs is challenging, as only Geissler type IV lesions are represented by a distance between scaphoid and lunate >2 mm due to a complete SL tear [Citation19,Citation47,Citation63–65]. Prevalences up to 98% of associated ligamentous injury with DRFs, mostly SL ligament injuries, have been described [Citation65,Citation66]. Fortunately, most often these injuries do not need surgical repair when treating DRFs, because very rarely the SL injury significantly affects carpal stability and outcome [Citation19,Citation63]. Measurements regarding SL distance in our study were small and most likely do not represent ligamentous injury with significant impact on outcome.
DRUJ distance increased statistically significantly from 2.0 to 2.4 mm between baseline and 6 weeks, but this distance did not differ significantly from the uninjured wrist. In literature it has been described that DRUJ instability is suspected when a difference is present between DRUJ distance on PA radiographs of the injured compared to the uninjured wrist. In addition, when on a lateral radiographs a distance is measured exceeding 4–5 mm between the dorsal cortexes of the distal radius and ulna, this is also a suggestion for DRUJ instability [Citation49]. We therefore conclude that in our study DRUJ instability was most likely not present.
Residual articular incongruence in perspective
Surprisingly, our results showed that step-off and gap diminished significantly between 6 weeks and follow-up, although these differences were within earlier mentioned magnitude error [Citation10]. Conflicting results regarding reliability of measuring gaps and step-offs following distal radius fractures have been reported. It has been reported that observers, independent of skill level, may measure step-off and gaps accurately to 0.62 ± 53 mm (95% CI 0.59–0.65) [Citation67]. Intraclass correlation coefficient scores showed “substantial” (0.78) to “almost perfect” (0.81) inter- and intraobserver agreement [Citation67]. In contrast, other studies reported low intra- and inter-reliability ICC values [Citation10,Citation18]. Watson et al. showed that measurement error lies within 1–2 mm, indicating that clinicians cannot measure differences ≤1 mm [Citation10]. They therefore questioned the reliability of using these radiographic measurements to guide treatment decisions regarding conservative or operative management. To our knowledge, no literature on the decrease of articular incongruence over time in adult patients is available. Bone healing is a complex event that involves coordination of two complex forces: anabolism or tissue formation and catabolism or remodelling under influence of axial, translational and rotational forces [Citation68,Citation69]. Possibly remodelling processes have diminished the articular incongruence.
Outcomes in perspective
Flexion/extension seems to be a clinically relevant measurement in non-osteoporotic patients following DRFs, because our findings seemed to exceed MIC references [Citation27]. As reported by our research group and others, it is well known that fractures healed with a step-off ≥ 2 mm are associated with development of PA, which may affect CROs and PROs [Citation12–14,Citation16,Citation17,Citation32,Citation70]. Multiple studies report on better CROs following plate fixation with better anatomical realignment of articular congruence in comparison to conservative treatment or external fixators [Citation71–73]. Unfortunately, no MICs for ulnar/radial deviation and pro/supination are reported in literature. Therefore, further research is mandatory to determine MIC references to evaluate the clinical relevance of CROs. We conclude that patients with a DRF should be informed that lasting limitations in flexion/extension might be expected.
Although in our study a statistically significant difference in grip strength between the injured and uninjured wrist was found, this result did not exceed the reported MIC [Citation28]. This suggests that no clinically relevant impact on grip strength is expected following DRFs. As such, grip strength seems to be merely a reflection of overall strength and the physical condition of a chain of muscles in the upper limb [Citation74].
In our study, the MIC of the DASH was not exceeded, but MICs of PRWE subscales pain, function and total score were [Citation29,Citation31]. For the MHQ, no discriminative ability is present as captured in MIC following DRFs, because of the ceiling effect of the MHQ with high scores at 3 months follow up [Citation30]. To our knowledge, no literature reported on MICs of the SF36 following DRFs so far. However, seemingly substantial differences between patients with DRFs and healthy controls on subscales MHQ general function, work, pain, satisfaction as total MHQ were found. In addition, for the SF36 subscales vitality and pain this seemed also to be true. More knowledge on reference MICs regarding PROs is mandatory to put these differences in clinical perspective. It is known that outcomes as measured with PROs and assessed using MICs can differ significantly between certain injuries or disorders and can therefore not be extrapolated [Citation57]. In addition, slight variation exists in the psychometric properties of PROs measuring outcomes of different injuries or disorders, which can hamper comparability [Citation55,Citation75,Citation76]. Waljee et al. and Goldhahn et al. have proposed a core set of parameters including aROM, grip strength, the PROs PRWE, DASH, MHQ, and the Patient Reported Outcome Measurement Information System (PROMIS®) upper extremity item banks to be included when reporting in literature on DRFs to improve comparability [Citation77,Citation78]. We believe that reporting on aROM, grip strength and PROs with adequate MICs would improve interpretability of the clinical relevance of outcomes following DRFs in non-osteoporotic patients immensely.
Associations between radiological measurements and outcome in perspective
Step-offs were significantly associated with diminished flexion/extension and ulnar/radial deviation. Several authors reported on the association between articular incongruency following DRFs and the association with development of posttraumatic arthritis (PA) at longer follow up duration [Citation13,Citation15,Citation79–81]. The development of PA is related to several causes, such as increased stress on the articular surface following overcorrection of radial length, radiocarpal instability caused by ligamentous injuries or articular incongruency [Citation12,Citation82,Citation83].
Radial length seems to be important to correct surgically, because radial shortening may result in diminished grip strength. However, this decreased grip strength may not be clinically noticeable for a patient, because measurements did not exceed reported MICs [Citation28]. Note that several reports have associated radial shortening with diminished ROM and diminished grip strength measurements [Citation32,Citation38,Citation84–86]. In contrast, a few others did not find such associations [Citation34,Citation35]. Radial shortening may cause an increased pressure in the DRUJ and a shift in the centre of pressure within the sigmoid notch and can cause diminished ROM and grip strength [Citation87–89].
Articular incongruence of ≥1 mm may lead to lower SF36 scores [Citation15] as is supported by our study in which the SF36 mental component score was significantly associated with residual step-off. Unfortunately no MICs are reported for the SF36 and no sound conclusion can be drawn. It does illustrate the need for more knowledge on MICs following DRFs when reporting on outcome using PROs.
Strength and weaknesses
By reporting on a young non-osteoporotic population who sustained a DRF 4-11 years ago, we contribute to the knowledge on radiological measurements after a DRF and their associations with CROs and PROs. All measurements regarding CROs have been performed by one hand therapist for consistency. To eliminate interobserver bias, all measurements on radiographs were assessed by one specialized radiologist. It has to be acknowledged that, although all radiographs have been taken according to protocol, measurement accuracy can be influenced by the quality of the radiographs. Our response rate was low, presumably because our population was young and moved for study or work purposes and therefore many current addresses could not be retrieved. The included number of 73 patients might be insufficient to draw firm conclusions. However, in most studies describing populations after DRFs, the included number of patients did not exceed our cohort [Citation11,Citation72,Citation90]. To our knowledge, no MIC values regarding the PROs MHQ and SF36 have been reported yet. Therefore we have compared the results of our cohort to a healthy young non-osteoporotic cohort of 22 participants. Care should be taken when drawing conclusions regarding comparisons with this healthy cohort, because the sample size is minimal. In addition, lack of consensus regarding the best methodology to determine the MIC exists. There are two main approaches; anchor-based methods in which an external criterion is used to define an important change (often patient-based judgement) and distribution-based methods, which use statistical measures as a value for MIC [Citation76]. This could result in large variations in MIC values for CROs and PROs reported in literature [Citation76]. Care should be taken to interpret MIC values and consensus should be reached on the preferred MIC methodology.
Conclusions
Radiological measurements following DRFs seem to evolve over time, but differences were small and are probably not clinically relevant. Range of motion, in particular flexion/extension, was clinically relevantly diminished in non-osteoporotic patients following a DRF, while grip strength was not. Residual articular incongruency seems to influence range of motion, where shortening of the radius might influence grip strength. The association between residual articular incongruency and patient reported outcomes needs further attention. Further research on MIC is mandatory, to enhance interpretation of clinically relevant outcomes after a DRF.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Beumer A, Adlercreutz C, Lindau TR. Early prognostic factors in distal radius fractures in a younger than osteoporotic age group: a multivariate analysis of trauma radiographs. BMC Musculoskelet Disord. 2013;14(1):170.
- Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg Am. 2007;32(7):962–970.
- Kumar S, Penematsa S, Sadri M, et al. Can radiological results be surrogate markers of functional outcome in distal radial extra-articular fractures? International Orthopaedics (Sico). 2008;32(4):505–509.
- Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg Am. 1982;7(4):376–379.
- Schuind FA, Linscheid RL, An KN, et al. A normal data base of posteroanterior roentgenographic measurements of the wrist. J Bone Joint Surg Am. 1992;74(9):1418–1429.
- Solgaard S. Angle of inclination of the articular surface of the distal radius. Radiologe. 1984;24(7):346–348.
- Friberg S, Lundstrom B. Radiographic measurements of the radio-carpal joint in normal adults. Acta Radiol Diagn (Stockh). 1976;17(2):249–256.
- Altissimi M, Antenucci R, Fiacca C, et al. Long-term results of conservative treatment of fractures of the distal radius. Clin Orthop Relat Res. 1986;206:202–210.
- Metz VM, Gilula LA. Imaging techniques for distal radius fractures and related injuries. Orthop. Clin. North Am. 1993;24(2):217–228.
- Watson NJ, Asadollahi S, Parrish F, et al. Reliability of radiographic measurements for acute distal radius fractures. BMC Med Imaging. 2016;16(1):44.
- Lindau T, Hagberg L, Adlercreutz C, et al. Distal radioulnar instability is an independent worsening factor in distal radial fractures. Clin Orthop Relat Res. 2000;Jul(376):229–235.
- Lutz M, Arora R, Krappinger D, et al. Arthritis predicting factors in distal intraarticular radius fractures. Arch Orthop Trauma Surg. 2011;131(8):1121–1126.
- Catalano LW, Cole RJ, Gelberman RH, et al. Displaced intra-articular fractures of the distal aspect of the radius. Long-term results in young adults after open reduction and internal fixation. J Bone Joint Surg Am. 1997;79(9):1290–1302.
- Doi K, Hattori Y, Otsuka KEN, et al. Intra-articular fractures of the distal aspect of the radius: Arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Jt Surg Ser A. 1999;81(8):1093–1110.
- Fernandez DL. Should anatomic reduction be pursued in distal radial fractures? J Hand Surg Br. 2000;25(6):523–527.
- Fitoussi F, Ip WY, Chow SP. Treatment of displaced intra-articular fractures of the distal end of the radius with plates. J Bone JT Surg Ser A. 1997;79(9):1303–1312.
- Strange-Vognsen H. Intraarticular fractures of the distal end of the radius in young adults: a 16 (2–26) year follow-up of 42 patients. Acta Orthop Scand. 1991;62(6):527–530.
- Kreder HJ, Hanel DP, McKee M, et al. X-ray film measurements for healed distal radius fractures. J Hand Surg Am. 1996;21(1):31–39.
- Forward DP, Lindau TR, Melsom DS. Intercarpal ligament injuries associated with fractures of the distal part of the radius. J Bone Joint Surg Am. 2007;89(11):2334–2340.
- Lindau T, Runnquist K, Aspenberg P. Patients with laxity of the distal radioulnar joint after distal radial fractures have impaired function, but no loss of strength. Acta Orthop Scand. 2002;73(2):151–156.
- Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745.
- Mokkink LB, Prinsen CA, Bouter LM, et al. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz J Phys Ther. 2016;20(2):105–113.
- de Vet HCW, Knol DL, Terwee CB, et al. Measurement in medicine. Cambridge: Cambridge University Press; 2011.
- Stratford PW, Binkley JM, Riddle DL. Health status measures: strategies and analytic methods for assessing change scores. Phys Ther. 1996;76(10):1109–1123.
- Terwee CB, Terluin B, Knol DL, et al. Combining clinical relevance and statistical significance for evaluating quality of life changes in the individual patient. J Clin Epidemiol. 2011;64(12):1465–1467.
- de Vet HC, Terwee CB. The minimal detectable change should not replace the minimal important difference. J Clin Epidemiol. 2010;63(7):804–805.
- Karagiannopoulos C, Sitler M, Michlovitz S, et al. Responsiveness of the active wrist joint position sense test after distal radius fracture intervention. J Hand Ther. 2016;29(4):474–482.
- Kim JK, Park MG, Shin SJ. What is the minimum clinically important difference in grip strength?. Clin Orthop Relat Res. 2014;472(8):2536–2541.
- Franchignoni F, Vercelli S, Giordano A, et al. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30–39.
- Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan hand outcomes questionnaire. J Hand Surg Am. 2009;34(3):509–514.
- Walenkamp MM, de Muinck Keizer RJ, Goslings JC, et al. The Minimum Clinically Important Difference of the Patient-rated Wrist Evaluation Score for Patients With Distal Radius Fractures. Clin Orthop Relat Res. 2015;473(10):3235–3241.
- Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(5):647–659.
- Dario P, Matteo G, Carolina C, et al. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014;45(6):S21–S6.
- Neidenbach P, Audige L, Wilhelmi-Mock M, et al. The efficacy of closed reduction in displaced distal radius fractures. Injury. 2010;41(6):592–598.
- Tsukazaki T, Takagi K, Iwasaki K. Poor correlation between functional results and radiographic findings in Colles’ fracture. J Hand Surg Br. 1993;18(5):588–591.
- Porter M, Stockley I. Fractures of the distal radius. Intermediate and end results in relation to radiologic parameters. Clin Orthop Relat Res. 1987;220:241–252.
- McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70-B(4):649–651.
- Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19(2):325–340.
- Rubinovich RM, Rennie WR. Colles’ fracture: end results in relation to radiologic parameters. Can J Surg. 1983;26(4):361–363.
- Larouche J, Pike J, Slobogean GP, et al. Determinants of functional outcome in distal radius fractures in high-functioning patients older than 55 years. J Orthop Trauma. 2016;30(8):445–449.
- Cauley JA. Public health impact of osteoporosis. J Gerontol A Biol Sci Med Sci. 2013;68(10):1243–1251.
- Dawson-Hughes B, Looker AC, Tosteson AN, et al. The potential impact of new National Osteoporosis Foundation guidance on treatment patterns. Osteoporos Int. 2010;21(1):41–52.
- Harvey N, Dennison E, Cooper C. Osteoporosis: impact on health and economics. Nat Rev Rheumatol. 2010;6(2):99–105.
- Morgan WF. International Commission on Radiological Protection Committee 1: current status and future directions. Ann ICRP. 2015;44(1_suppl):8–14.
- van der Linden W, Ericson R. Colles’ fracture. How should its displacement be measured and how should it be immobilized? J Bone Joint Surg Am. 1981;63(8):1285–1288.
- Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg Am. 1984;9(3):350–357.
- Said J, Baker K, Fernandez L, et al. The optimal location to measure scapholunate diastasis on screening radiographs. Hand (New York, N,Y). 2018;13(6):671–677.
- Nakamura R, Horii E, Imaeda T, et al. Distal radioulnar joint subluxation and dislocation diagnosed by standard roentgenography. Skeletal Radiol. 1995;24(2):91–94.
- Wijffels M, Brink P, Schipper I. Clinical and non-clinical aspects of distal radioulnar joint instability. TOORTHJ. 2012;6(1):204–210.
- Lameijer CM, Niezen CK, El Moumni M, et al. Pain, impaired functioning, poor satisfaction and diminished health status eight years following perilunate (fracture) dislocations. Disabil Rehabil. 2018;19:1–8.
- Petersen P, Petrick M, Connor H, et al. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43(7):444–447.
- Baltzer H, Novak CB, McCabe SJ. A scoping review of disabilities of the arm, shoulder, and hand scores for hand and wrist conditions. J Hand Surg Am. 2014;39(12):2472–2480.
- Beaton DE, Katz JN, Fossel AH, et al. Measuring the whole or the parts? Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–146.
- MacDermid JC, Turgeon T, Richards RS, et al. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586.
- El Moumni M, Van Eck ME, Wendt KW, et al. Structural validity of the Dutch version of the patient-rated wrist evaluation (PRWE-NL) in patients with hand and wrist injuries. Phys Ther. 2016;96(6):908–916.
- MacDermid JC, Tottenham V. Responsiveness of the disability of the arm, shoulder, and hand (DASH) and patient-rated wrist/hand evaluation (PRWHE) in evaluating change after hand therapy. J Hand Ther. 2004;17(1):18–23.
- Shauver MJ, Chung KC. The Michigan hand outcomes questionnaire after 15 years of field trial. Plast Reconstr Surg. 2013;131(5):779e–787e.
- Ware JE, Kosinski M. Interpreting SF-36 summary health measures: a response. Qual Life Res. 2001;10(5):405–413.
- Jenkinson C, Coulter A, Wright L. Short form 36 (SF36) health survey questionnaire: normative data for adults of working age. BMJ. 1993;306(6890):1437–1440.
- Rikli DA, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function. A preliminary report of 20 cases. J Bone Joint Surg Br. 1996;78-B(4):588–592.
- Brink PR, Rikli DA. Four-corner concept: CT-based assessment of fracture patterns in distal radius. Jnl Wrist Surg. 2016;05(02):147–151.
- Rikli DA, Honigmann P, Babst R, et al. Intra-articular pressure measurement in the radioulnocarpal joint using a novel sensor: in vitro and in vivo results. J Hand Surg Am. 2007;32(1):67–75.
- Ozkan S, Korteweg JJ, Bloemers FW, et al. Radiographic diagnosis of scapholunate diastasis in distal radius fractures: implications for surgical practice. Jnl Wrist Surg. 2018;07(04):312–318.
- Kuo CE, Wolfe SW. Scapholunate instability: current concepts in diagnosis and management. J Hand Surg Am. 2008;33(6):998–1013.
- Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg Br. 1997;22(5):638–643.
- Gunal I, Ozaksoy D, Altay T, et al. Scapholunate dissociation associated with distal radius fractures. Eur J Orthop Surg Traumatol. 2013;23(8):877–881.
- McCallister WV, Smith JM, Knight J, et al. A cadaver model to evaluate the accuracy and reproducibility of plain radiograph step and gap measurements for intra-articular fracture of the distal radius. J Hand Surg Am. 2004;29(5):841–847.
- Odgren PR, Witwicka H, Reyes-Gutierrez P. The cast of clasts: catabolism and vascular invasion during bone growth, repair, and disease by osteoclasts, chondroclasts, and septoclasts. Connect Tissue Res. 2016;57(3):161–174.
- Schindeler A, McDonald MM, Bokko P, et al. Bone remodeling during fracture repair: The cellular picture. Semin Cell Dev Biol. 2008;19(5):459–466.
- Fernandez JJ, Gruen GS, Herndon JH. Outcome of distal radius fractures using the short form 36 health survey. Clin Orthop Relat Res. 1997;341:36–41.
- Sharma H, Khare GN, Singh S, et al. Outcomes and complications of fractures of distal radius (AO type B and C): volar plating versus nonoperative treatment. J Orthop Sci. 2014;19(4):537–544.
- Toon DH, Premchand RA, Sim J, et al. Outcomes and financial implications of intra-articular distal radius fractures: a comparative study of open reduction internal fixation (ORIF) with volar locking plates versus nonoperative management. J Orthop Traumatol. 2017;18(3):229–234.
- Wright TW, Horodyski M, Smith DW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 2005;30(2):289–299.
- Leong DP, Teo KK, Rangarajan S, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386(9990):266–273.
- Van Eck ME, Lameijer CM, El Moumni M. Structural validity of the Dutch version of the Disability of Arm, Shoulder and Hand questionnaire (DASH-DLV) in adult patients with hand and wrist injuries. BMC Musculoskelet Disord. 2018;19(1):207.
- Terwee CB, Roorda LD, Dekker J, et al. Mind the MIC: large variation among populations and methods. J Clin Epidemiol. 2010;63(5):524–534.
- Waljee JF, Ladd A, MacDermid JC, et al. Distal radius outcomes consortium. A unified approach to outcomes assessment for distal radius fractures. J Hand Surg Am. 2016;41(4):565–573.
- Goldhahn J, Beaton D, Ladd A, Distal Radius Working Group of the International Society for Fracture Repair (ISFR), et al. Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg. 2014;134(2):197–205.
- Lameijer CM, Ten Duis HJ, Dusseldorp IV, et al. Prevalence of posttraumatic arthritis and the association with outcome measures following distal radius fractures in non-osteoporotic patients: a systematic review. Arch Orthop Trauma Surg. 2017;137(11):1499–1513.
- Forward DP, Davis TR, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008;90-B(5):629–637.
- Kopylov P, Johnell O, Redlund-Johnell I, et al. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg Br. 1993;18(1):45–49.
- Giannoudis PV, Tzioupis C, Papathanassopoulos A, et al. Articular step-off and risk of post-traumatic osteoarthritis. Evidence today. Injury. 2010;41(10):986–995.
- Lameijer CM, Ten Duis HJ, Vroling D, et al. Prevalence of posttraumatic arthritis following distal radius fractures in non-osteoporotic patients and the association with radiological measurements, clinician and patient-reported outcomes. Arch Orthop Trauma Surg. 2018;138(12):1699–1712.
- Batra S, Gupta A. The effect of fracture-related factors on the functional outcome at 1 year in distal radius fractures. Injury. 2002;33(6):499–502.
- Fernandez DL. Radial osteotomy and Bowers arthroplasty for malunited fractures of the distal end of the radius. J Bone Joint Surg Am. 1988;70(10):1538–1551.
- Geissler WB, Fernandez DL, Lamey DM. Distal radioulnar joint injuries associated with fractures of the distal radius. Clin Orthop Relat Res. 1996;327:135–146.
- Crisco JJ, Moore DC, Marai GE, et al. Effects of distal radius malunion on distal radioulnar joint mechanics–an in vivo study. J Orthop Res. 2007;25(4):547–555.
- Werner FW, Murphy DJ, Palmer AK. Pressures in the distal radioulnar joint: effect of surgical procedures used for Kienbock’s disease. J Orthop Res. 1989;7(3):445–450.
- Werner FW, Palmer AK, Fortino MD, et al. Force transmission through the distal ulna: effect of ulnar variance, lunate fossa angulation, and radial and palmar tilt of the distal radius. J Hand Surg Am. 1992;17(3):423–428.
- Wijffels MM, Krijnen P, Schipper IB. Clinical DRUJ instability does not influence the long-term functional outcome of conservatively treated distal radius fractures. Eur J Trauma Emerg Surg. 2017;43(2):227–232.
