Abstract
Purpose
Total knee arthroplasty is increasingly performed on working-age individuals, but little is known about their recovery process. Therefore this study examined recovery courses of physical and mental impairments, activity limitations and participation restrictions among working-age total knee arthroplasty recipients. Associated sociodemographic and health-related factors were also evaluated.
Materials and methods
A prospective study among working total knee arthroplasty patients (aged <65 years) (n = 146). Surveys were completed preoperatively and 6 weeks and 3, 6, 12, and 24 months postoperatively. Outcomes represented domains of the International Classification of Functioning, that is, physical impairments (pain, stiffness, vitality), mental impairments (mental health, depressive symptoms), activity limitations (physical functioning), and participation restrictions (social-, work functioning, working hours). Covariates included age, gender, education, home situation, body mass index, and comorbidity.
Results
Largest improvements in physical and mental impairments and activity limitations were observed until 3 months postoperatively. Participation in social roles improved early after surgery, and improvements in work participation occurred from 6 to 12 months. Older age, being male and fewer comorbidities were associated with better recovery courses.
Conclusion
Working-age total knee arthroplasty patients recover soon from physical and mental impairments, activity limitations, and participation in social roles, but participation at work occurs later. Younger patients, females, and those with musculoskeletal comorbidities appear at risk for suboptimal recovery after total knee arthroplasty.
An increasing number of working-age patients are asking for total knee arthroplasty and have high expectations of total knee arthroplasty, in particular, to participate in the workforce again;
Recovery after total knee arthroplasty (TKA) does not occur in the short term and is not limited to clinical improvements for working-age TKA recipients only, as an important part of recovery, that is, participation occurs in the long term (>6 months);
Closer collaboration between occupational physicians and orthopedic surgeons might result in increased and earlier ability to work full contractual hours;
Rehabilitation after TKA should focus on patients with multiple comorbidities, whereby musculoskeletal diseases may even need additional preoperative treatment to optimize outcomes and prevent work disability.
Implications for rehabilitation
Introduction
The number of working-age patients undergoing total knee arthroplasty (TKA) is rapidly increasing in Western societies [Citation1–3]. This is mainly due to increased prosthetic survivorship and the fact that particularly the severity of osteoarthritis (OA), instead of age, has become a major criterion in the decision-making process to undergo TKA [Citation4,Citation5]. In the Netherlands, the number of working-age TKA patients (aged <65) tripled between 1995 and 2005, which is a higher increase than that observed among elderly patients. The number of TKA procedures is expected to rise further and the proportion of the working-age group will be even greater due to higher retirement ages [Citation1]. For the USA it is estimated that in 2030 up to 62% of TKAs will be performed on patients of working age, compared to ∼40% in 2010 [Citation2,Citation6].
Due to these dramatic increases in primary TKA rates, it is important to pursue a more detailed understanding of working-age patients’ recovery following surgery. So far, prospective studies among working-age patients have focused mainly on knee-specific outcomes like pain and joint function [Citation7–9], yet these outcomes only partially explain the recovery process after TKA [Citation10,Citation11]. Knee-specific pain and function, for example, do not address whether TKA allows people to engage in activities of daily living and/or participate in society and work. In addition, studies mainly focused on outcomes at one or two follow-up moments and did not examine the course of improvement over time. To obtain a more holistic approach to recovery there is growing recognition for examining a broad spectrum of outcome measures that capture physical and mental impairments, activity limitations, and participation restrictions as represented in the International Classification of Functioning (ICF) model at multiple follow-up moments [Citation11,Citation12].
Participation is a particularly important outcome for working-age TKA patients, who are concerned about their return to participation in social roles and work [Citation13]. Participation at home and in the community has been investigated in a subsample of patients aged <65 [Citation14]. These patients reported improvements in taking care of daily responsibilities and social activities postoperatively. Females, depressive symptoms, and severe pain in either knee were associated with decreased participation [Citation14]. Regarding work, previous studies mainly evaluated return-to-work outcomes and showed that ∼34 to 67% of patients return to work within 3 months of surgery [Citation7,Citation15–18]. However, after returning to work TKA patients can still experience difficulties at the workplace due to physical impairments and activity limitations. This may result in sick leave or limited work functioning. Two years postoperatively, sick leave, [Citation19] and substantial at-work productivity loss exists [Citation20], but recovery of participation at work in terms of work functioning is unknown.
The purpose of this study was therefore to provide a more holistic approach of working-age patients’ recovery following surgery, including physical and mental impairments, activity limitations, and especially participation restrictions in working life. By identifying these outcomes at multiple follow-up moments for a 2-year period, courses of recovery could be described. These courses are useful for showing the development of recovery over a longer period of time and subsequently to detect distinct courses of recovery after TKA. Together with associated sociodemographic and health-related factors of these courses, this can increase our understanding of how and when recovery after TKA surgery can be optimized. The aim of the present study was therefore to (1) investigate courses of physical and mental impairments, activity limitations, and participation restrictions in working-age patients undergoing TKA surgery preoperatively up to 2 years postoperatively and (2) examine the associations between sociodemographic and health-related factors with these courses.
Methods
Study design and participants
This prospective cohort study entitled “Work participation In Patients with Osteoarthritis” consecutively included patients with knee OA scheduled for TKA between March 2012 and July 2014 in the northern part of the Netherlands. Preoperative (T0) and postoperative data at 6 weeks (T1) and 3 (T2), 6 (T3), 12 (T4), and 24 (T5) months were gathered. Inclusion criteria were primary or secondary knee OA and undergoing TKA, preoperative employment, and age between 18 and 63 years. The age of 63 was chosen in order to complete the 2-year follow-up before the (former) Dutch retirement age of 65 years. Exclusion criteria were insufficient knowledge of the Dutch language and having undergone joint arthroplasty in the previous 6 months. Four hospitals participated: University Medical Center Groningen (UMCG) (tertiary university hospital), Medical Center Leeuwarden (MCL) (large teaching hospital), Martini Hospital Groningen (MHG) (large teaching hospital) and Röpcke-Zweers Hospital Hardenberg (general hospital). The study was approved by the Medical Ethical Committee of University Medical Center Groningen (METc 2012.153) and in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was considered as obtained if the patient granted our request to participate in the study by returning a set of completed questionnaires. Patients who did not want to participate in the study were requested to return a blank questionnaire. Patients were informed of this consent method by mail, in an information letter that also communicated the voluntary nature of the study and the anonymous nature of all the data to be processed. Patients who did not respond after initial informed consent were invited/contacted by phone no more than twice to resume participation. The Medical Ethical Committee approved this consent procedure.
Measures
The outcome measures in the cohort were grouped following the World Health Organization framework of the ICF model, considering physical and mental impairments, activity limitations, and participation restrictions [Citation12]. The selection of outcome measures and classification in the ICF model was guided by a previous study that examined the discriminant validity of commonly used TKA outcome measures with ICF constructs [Citation21].
Physical and mental impairments
Impairments were divided into physical and mental impairments. Physical impairments included general and knee-specific pain, vitality, and stiffness. General pain and vitality were measured with the equivalently named subscales of the Dutch version of the RAND 36-item Health Survey, which measures health-related quality of life [Citation22]. General pain includes two questions on the severity of pain, and vitality includes four questions about energy level and fatigue. Subscores range from 0 to 100 and higher scores reflect less pain and better vitality. The RAND-36 is a reliable and valid instrument [Citation22]. Knee-specific pain (5 items) and stiffness (2 items) were measured with the Dutch version of the Western Ontario and McMaster Osteoarthritis Index (WOMAC) [Citation23], and these subscales were transformed into a 0–100 scale. A higher score represents less pain or stiffness. The WOMAC has proven to be valid and reliable [Citation24].
Mental impairments included mental health and depressive symptoms. Mental health was captured by the subscale of the RAND-36 and asks five questions about depressive symptoms and anxiety [Citation22]. Subscores range from 0–100 and higher scores reflect better mental health. Depressive symptoms were measured with the PHQ-9 questionnaire. The PHQ-9 is the depression module from the PRIME-MD instrument for common mental disorders, which scores each of the nine DSM IV criteria from 0 (“not at all”) to 3 (“nearly every day”). Participants were asked how often they experienced each of the depressive symptoms over the last 2 weeks. The PHQ-9 is a valid and reliable instrument [Citation25]. The scale was recoded to a 0–100 scale, where higher scores represent fewer depressive symptoms.
Activity limitations
Activity limitations captured general and knee-specific physical functioning, measured with subscales of both the RAND-36 and the WOMAC, respectively. The physical functioning of the RAND-36 asks about limitations in performing 10 daily activities due to health problems, such as climbing stairs, doing laundry, and doing chores around the house. The range is 0-100 and higher scores reflect better physical functioning [Citation22]. Knee-specific physical functioning was measured with the WOMAC and covers limitations in physical functioning because of knee complaints during 17 daily activities, like getting out of bed and going to the toilet [Citation26]. A higher score (range 0–100) indicates better knee-specific physical functioning.
Participation restrictions
Participation restrictions included social- and work-functioning and the number of working hours. Social functioning was measured with the RAND-36 subscale social functioning and asks about restrictions due to health problems in social activities such as visiting friends. Subscores range from 0 to 100 and higher scores reflect better social functioning. Work functioning was measured by the Work Role Functioning Questionnaire 2.0 (WRFQ). The WRFQ measures self-reported difficulties in meeting 27 work demands, given workers’ physical health and emotional problems. The total score was used (range 0–100), with higher scores indicating better work functioning. The WRFQ was not assessed at 6 weeks postoperatively due to the high possibility that many patients would not be at work. The WRFQ 2.0 has good internal consistency, moderate test–retest reliability, and responsiveness in the general working population [Citation26]. The number of working hours was calculated from the proportion of the actual number of working hours compared to the contractual number of hours.
Covariates
The sociodemographic factors included age, gender, educational level – categorized into low (i.e., primary school and lower vocational education), medium (i.e., secondary vocational education) and high (higher vocational education and university) – and home situation categorized into living alone, living with a partner and living with partner and children. Health-related covariates were body mass index (BMI) and comorbidity. BMI was derived from self-reported body height and body weight, and categorized into normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obese (>30.0 kg/m2). Comorbidity was measured by using a 28-item chronic conditions questionnaire [Citation27]. The number of comorbidities was categorized into having no, one, or two or more comorbidities.
Statistical analyses
All analyses were conducted using SPSS version 23. First, patients’ baseline characteristics were analyzed using descriptive statistics (mean, median, or percentage). To obtain the first aim, courses of physical and mental impairments, activity limitations, and participation restrictions were analyzed. Linear mixed models (LMM) were used to calculate the estimated means with corresponding 95% confidence intervals (CIs) for normally distributed measures. Differences between baseline and each follow-up moment were tested with pairwise comparisons. Additionally, change percentages between follow-up moments were calculated. Results were tabulated and graphed over time. To obtain the second aim, associations of sociodemographic and health-related factors with each separate outcome (except the percentage of working hours) were tested. A total of three models were fitted using LMM: (1) an unconditional growth model, which included the outcome measure and a categorical time variable; (2) sociodemographic factors (age, gender, educational level, and home situation) were added to the first model; and (3) sociodemographic factors with a statistical significance of p < 0.20 were added to the third model, subsequently adding health-related factors (BMI and comorbidity) to this third model. Finally, an attrition bias analysis was conducted comparing age, gender, BMI, comorbidity, educational level, and home situation of non-responders at 24 months with responders. This analysis revealed no significant differences. Statistical significance was set at p ≤ 0.05.
Results
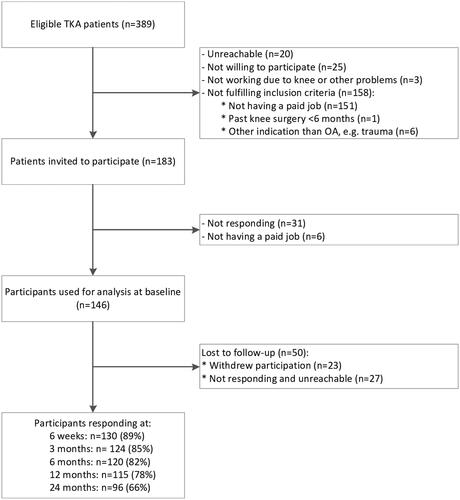
A total of n = 389 TKA patients were eligible to participate. is a flow chart showing the total number of patients recruited into the study at baseline and the drop-outs to follow-up. At baseline, n = 146 returned the questionnaire and that data was used for analysis. At 6 weeks postoperatively, n = 130 (89%) of the participants returned the questionnaire, at 3 months, n = 124 (85%); at 6 months, n = 120 (82%); at 12 months, n = 115 (78%); at 24 months, n = 96 (66%). The mean age was 55 years (range: 38–62) and 56% was female. Participants had generally completed secondary vocational education (47%) or higher education (18%), and most were living together with a partner (58%) and/or children (8%). A substantial proportion had overweight (43%) or obese (40%), and had two or more comorbidities (70%). provides a more detailed description of the baseline characteristics.
Table 1. Baseline characteristics.
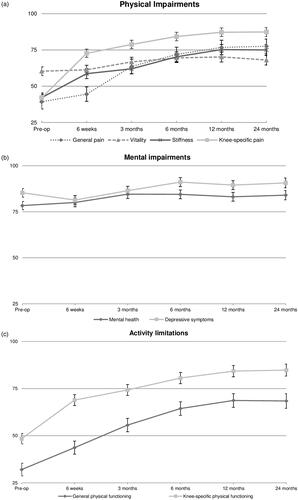
Courses of physical and mental impairments
Physical impairments improved significantly (p < 0.001) over time, with the largest changes within the first 3 months. For knee-specific pain and stiffness, the largest improvement was observed between preoperatively and 6 weeks postoperatively (72.9 and 39.1%, respectively). This was followed by major improvements in general pain and vitality between 6 weeks and 3 months (42.8 and 8.9%, respectively; ). Beyond 12 months stable courses were observed ().
Figure 2. Recovery courses of physical (a) and mental impairments (b), activity limitations (c) and participation restrictions (d) following TKA surgery (n = 146). All measures are standardized to 0–100 scores (Y-axis), where higher scores represent fewer impairments, limitations or restrictions.
Table 2. Results of linear mixed models of physical and mental impairments, activity limitations, and participation restrictions over 2 years’ time.
Mental impairments improved significantly over 2 years’ time (p < 0.001) (), though in a stable course (). Mental health improved mainly between 6 weeks and 3 months (5.6%), with minimal changes subsequently. Depressive symptoms worsened shortly after surgery (−4.6%), but improved significantly again at 6 months (5.4%), and showed minimal changes until 24 months postoperatively (, ).
Courses of activity limitations
Activity limitations improved significantly over 2 years’ time (p < 0.001). For both general and knee-specific physical functioning, the largest improvements were observed between the preoperative level and 6 weeks postoperatively (36.2 and 42.2%, respectively), followed by another major improvement in general physical functioning between 6 weeks and 3 months (27.4%). Knee-specific physical functioning improved gradually after 6 weeks. Stable courses were observed between 12 and 24 months. Knee-specific physical functioning increased by a total of 75.0% over 2 years, which is a lesser improvement compared to 113.5% for general physical functioning (, ).
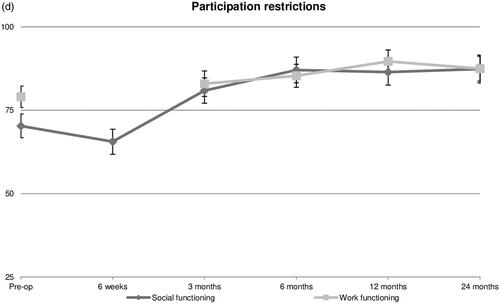
Courses of participation restrictions
Social functioning improved significantly between 6 weeks and 3 months postoperatively (23.3%), after a small setback (−6.7%) within the first 6 postoperative weeks. Work role functioning gradually improved over time and the largest improvement was observed between 6 and 12 months (5.1%). The reported work functioning level at 24 months (87.5) was significantly higher than the preoperative state (79.2) (, ).
The percentage of working hours was not normally distributed and was therefore analyzed by reporting the median and interquartile range. Preoperatively we observed a median of 100.0% (100.0–100.0; n = 129), at 6 weeks 55.0% (39.0–100.0; n = 22), at 3 months 62.5% (40.0–100.0; n = 67), at 6 months 100.0% (66.7–100.0; n = 86), and at 12 and 24 months 100.0% (100.0–100.0; n = 101 and n = 62, respectively).
Associations between sociodemographic and health-related factors with the recovery courses
In the final third model, older age was positively associated with all outcomes (see ). Being male was positively associated with the recovery courses for stiffness (B: 6.8), mental health (B: 4.2), and general physical functioning (B: 4.9). Moreover, a lower number of comorbidities was associated with less general pain (B: 6.6), better vitality (B: 7.7), better general physical functioning (B: 12.5), and better social functioning (B: 7.5). A lower educational level was only associated with better social functioning (B: 12.4). The results of all three models are presented in the Supplementary Material (Table S1).
Table 3. Final models showing significant associations of sociodemographic and health-related factors with physical and mental impairments, activity limitations and participation restrictions.
Discussion
This is the first study to simultaneously examine the recovery courses of physical and mental impairments, activity limitations, and participation restrictions, as represented in the ICF model, among the rapidly growing group of working-age TKA recipients. Within the first 3 postoperative months, patients showed the largest improvements in physical impairments and activity limitations. After 12 months stable courses were observed in both ICF domains. Mental impairments improved in a stable course with minimal changes during follow-up. Participation restrictions in social roles improved in the first 3 postoperative months, followed by improvements in participation at work after 6–12 months in terms of working hours and work functioning. Persons who were older, male, and had a lower number of comorbidities showed significantly better recovery courses over 2 years’ time.
The literature on the recovery of working-age TKA recipients is scarce and therefore comparison with literature was limited. Generally, physical impairments showed a substantial total change over 24 months’ follow-up, whereby main gains were made within the first 3 months as anticipated by TKA surgery. This is in line with literature on senior TKA patients (mean age >65 years) that shows similar improvements within the first 3 postoperative months [Citation28] as well as gradual improvements between 3 and 12 months postoperatively [Citation29,Citation30]. Recovery courses have not been identified yet among working-age patients specifically, but knee-specific pain has been evaluated at one or two follow-up moments. At 2 years postoperatively, significant improvements in knee-specific pain were also observed [Citation8,Citation9]. The present study adds that between 12 and 24 months no substantial improvements were reported. This conforms with the literature on the forgotten joint score, which represents how natural the prosthesis feels. Patients generally no longer feel their knee prosthesis after the first year [Citation31], as we confirmed with the presented clinical outcomes. Improvements in mental health in the first 3 months are in line with other studies that examined mental health at 6 months postoperatively [Citation9]. The present study also identified that depressive symptoms worsened just a little bit (from 83 to 79%) in the first months after surgery. The reported score of 79% at 6 weeks may be attributed to the presence of pain or limited function as the PHQ-9 questionnaire prescribes [Citation25].
The present study showed that the greatest improvements in activity limitations already occurred within 6 weeks, even before physical impairments fully diminished. This finding is in contrast to Davis et al., who found that among patients of all ages activity limitations started decreasing only after physical impairments had improved [Citation29]. We also found that patients’ general physical functioning was worse than knee-specific physical functioning preoperatively, and recovered in a slower pattern. As anticipated by TKA surgery, knee-specific physical functioning improved strongly and early after surgery. It might be that the recovery of TKA patients is more hampered by their general physical functioning, probably due to functional limitations from body regions other than the operated knee.
The improvements in participation concerning social functioning are in line with a previous study that identified home and community participation among patients aged <65. That study also observed major improvements in home and community participation after 1 year postoperatively [Citation14]. The present study adds that improvements in social participation already occur earlier, that is, between 6 weeks and 3 months. This was followed by an improvement in participation at work. So far, studies have mainly reported on return-to-work outcomes, whereby between 34 and 67% of patients returned to work by 3 months postoperatively. We did not include the return to work as a primary outcome, but rather the number of actual working hours compared to the contractual number of hours, which was assessed solely among those who returned to work. We observed a high variety of working hours, which shows a skewed distribution. Only at 12 months, a majority of patients reported working their full contractual hours again (IQR 100.0–100.0). Additionally, participants already reported better postoperative work functioning earlier, from 3 months onwards, with the greatest increase between 6 and 12 months. This is in line with Sankar et al., who found that TKA is associated with significantly fewer limitations at work in the first year after surgery [Citation32]. Work functioning is classified as “good” from 90 points or higher, which was reported at 12 months postoperatively [Citation33,Citation34]. As patients experienced good work functioning at 12 months, a majority also worked their contractual number of hours again.
We sought sociodemographic and health-related factors associated with the recovery courses. Older age was the only factor that was positively associated with all courses. We analyzed age on a continuous scale, and these findings are in line with a previous study of Townsend et al., who found that TKA patients aged 50–59 years reported worse pain, function, and stiffness scores compared to those aged 60–69 years or older [Citation35]. This might suggest that within the working-age population, specific age classes exist showing different patterns of recovery. Working-age patients are known to have high preoperative expectations to perform better on many activities of daily life, for example, work and leisure time, which may hinder satisfaction with recovery [Citation13,Citation36]. Other age-related aspects might additionally play a role, as younger patients are more likely to be taking care of children at home and might feel more pressure to earn wages, compared to older patients in their pre-retirement years. Future studies should examine whether such differences exist between specific age classes, possibly affecting the appraisal of the recovery process.
Our findings showed that among working-age TKA patients, males have better outcomes in terms of stiffness, mental health, and general physical functioning compared to females, which is in line with literature that includes TKA patients of all ages [Citation11,Citation29,Citation37]. No gender differences were found on the participation level though. As expected, comorbidity was associated with measures in all three ICF domains, that is, general pain, vitality, and general physical functioning and social functioning. In a posthoc analysis we identified that, besides the operated knee, low back pain and osteoarthritis of limbs and arms were most prevalent, followed by diabetes mellitus and hypertension. The association of other musculoskeletal disorders, such as low back pain or osteoarthritis of joints other than the operated knee, with worse recovery courses is in line with the literature and reasonable to expect [Citation38].
Strengths and limitations
An important strength of this study is the prospective design with multiple follow-up moments and outcome measures, which allowed us to examine courses of recovery over a 2-year follow-up period for a broad spectrum of outcome measures in line with the ICF model. The classification of outcome measures in the ICF model was done following the discriminant validity of the outcomes in each ICF construct. We are aware of the fact that the knee-specific pain subscale of the WOMAC represents both physical impairments and activity limitations [Citation21]. However, we decided to include knee-specific pain as physical impairment and not to leave it out, in order to be able to compare with literature and to deepen the insight into painful experiences. Another strength is the heterogeneous sample of patients and therefore the generalizability of the results. Patients were derived from primary, secondary, and tertiary hospitals. Study limitations included the relatively small sample size, whereby we could not fully fit the models – that is, the inclusion of the interaction terms of covariates with time was not possible. Moreover, the question about working hours was filled in by a lower number of patients (n = 129), while some patients answered either their actual working hours or their contractual working hours, therefore the proportion between the two amounts could not be calculated for these patients. In the present study, only self-reported outcome measures were used. Although self-report questionnaires continue to be the most frequently used instruments, allowing the collection of data from a large number of people at a low cost, accurately answering questions or questionnaires is a complex cognitive task for patients. Objective measures would have added insight into items such as knee function, but are not applicable to all other outcomes included in this study. We, therefore, chose to focus solely on self-reported outcome measures. Furthermore, we did not gather specific information on post-surgical rehabilitation protocols. However, the Dutch Orthopaedic Association and the Royal Dutch Society for Physiotherapy have recommendations that are followed nationwide [Citation39], as a result, no significant differences are expected between the hospitals.
Implications and recommendations
This study showed that among working-age TKA recipients, physical impairments, and activity limitations mainly improve in the first 3 months after surgery. These clinical improvements were followed by recovery of participation in social roles and at work, with improvements in work participation happening latest, that is between 6 and 12 months postoperatively. For clinical practice, this stresses that recovery does not occur in the short term and is not limited to clinical improvements for working-age TKA recipients only. An important part of recovery, that is, participation, occurs in the long term (>6 months). Especially participation at work is a crucial outcome from a personal and societal perspective [Citation13,Citation40,Citation41], and considering the work participation outcomes in the present study, further gains can be made in this domain. Qualitative interviews highlighted that healthcare professionals play an important role in reintegration at work among this specific patient population [Citation42]. Hence a closer collaboration between occupational physicians and orthopedic surgeons might result in increased and earlier ability to work full contractual hours. Moreover, results showed that recovery from TKA surgery is not only about knee-specific outcomes: patients are also hindered by other comorbidities such as musculoskeletal disorders and osteoarthritis in other limbs. In line with a recent scoping review [Citation43], we recommend that rehabilitation after TKA should focus on patients with multiple comorbidities, whereby musculoskeletal diseases may even need additional preoperative treatment to optimize outcomes and prevent work disability. Lastly, as discrepancies exist in studies that examined several younger age classes, further identification of vulnerable age classes (<65 years) is recommended.
Conclusions
This study reported a holistic approach to recovery in the first 2 years, including physical and mental impairments, activity limitations, and participation restrictions in social and working life among working-age TKA patients, in line with the ICF model. Physical impairments and activity limitations showed major improvements within the first 3 postoperative months, followed by improvements in participation restrictions in social roles. Recovery of participation at work, in terms of work functioning and working all contractual hours, occurred last and needed up to 1 year postoperatively. Younger patients, females, and patients with musculoskeletal comorbidities or osteoarthritis in joints other than the operated knee might be at particular risk for suboptimal recovery after surgery and could need targeted guidance during rehabilitation.
Author contributions
Contributions of the authors are as follows: conception and design: TH, MS, PK, SB; analysis and interpretation of the data: TH, RS, MS, PK, SB; drafting of the article: TH, MS, SKB, PK, SB; critical revision of the article for important intellectual content: MS, RS, JvB, PR, RB, SKB, PK, SB; provision of patients: JvB, PR, RB, MS, SKB; statistical expertise: RS, SB.
Supplemental Material
Download MS Word (40.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Otten R, van Roermund PM, Picavet HS. [Trends in the number of knee and hip arthroplasties: considerably more knee and hip prostheses due to osteoarthritis in 2030]. Ned.Tijdschr.Geneeskd. 2010;154:A1534. Dutch.
- Kurtz SM, Lau E, Ong K, et al. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–2612.
- Culliford DJ, Maskell J, Beard DJ, et al. Temporal trends in hip and knee replacement in the United Kingdom: 1991 to 2006. J Bone Joint Surg Br. 2010;92-B(1):130–135.
- Long WJ, Bryce CD, Hollenbeak CS, et al. Total knee replacement in young, active patients: long-term follow-up and functional outcome: a concise follow-up of a previous report. J Bone Joint Surg Am. 2014;96(18):e159.
- Riddle DL, Kong X, Jiranek WA. Two-year incidence and predictors of future knee arthroplasty in persons with symptomatic knee osteoarthritis: preliminary analysis of longitudinal data from the osteoarthritis initiative. Knee. 2009;16(6):494–500.
- Healthcare Cost and Utilization Project [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; [cited 2018 Apr 10]. Available from: For more information about HCUP data see http://www.hcup-us.ahrq.gov/
- Scott CEH, Turnbull GS, MacDonald D, et al. Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J. 2017;99-B(8):1037–1046.
- Niemelainen M, Moilanen T, Huhtala H, et al. Outcome of knee arthroplasty in patients aged 65 years or less: a prospective study of 232 patients with 2-year follow-up. Scand J Surg. 2018;108(4):313–320.
- Goh GS, Liow MHL, Bin Abd Razak HR, et al. Patient-reported outcomes, quality of life, and satisfaction rates in young patients aged 50 years or younger after total knee arthroplasty. J Arthroplasty. 2017;32(2):419–425.
- Alviar MJ, Olver J, Brand C, et al. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011;43(5):374–381.
- Ethgen O, Bruyere O, Richy F, et al. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86(5):963–974.
- World Health Organization [Internet]. Geneva (Switzerland): WHO; International classification of functioning, disability and health: ICF; 2001 [cited 2019 Aug 11]. Available from: http://www.who.int/iris/handle/10665/42407
- Witjes S, van Geenen RCI, Koenraadt KLM, et al. Expectations of younger patients concerning activities after knee arthroplasty: are we asking the right questions? Qual Life Res. 2017;26(2):403–417.
- Maxwell JL, Keysor JJ, Niu J, et al. Participation following knee replacement: the MOST cohort study. Phys Ther. 2013;93(11):1467–1474.
- Hoorntje A, Leichtenberg CS, Koenraadt KLM, et al. Not physical activity, but patient beliefs and expectations are associated with return to work after total knee arthroplasty. J Arthroplasty. 2018;33(4):1094–1100.
- Kievit AJ, van Geenen RC, Kuijer PP, et al. Total knee arthroplasty and the unforeseen impact on return to work: a cross-sectional multicenter survey. J Arthroplasty. 2014;29(6):1163–1168.
- Kuijer PP, Kievit AJ, Pahlplatz TM, et al. Which patients do not return to work after total knee arthroplasty? Rheumatol Int. 2016;36(9):1249–1254.
- Leichtenberg CS, Tilbury C, Kuijer P, et al. Determinants of return to work 12 months after total hip and knee arthroplasty. Annals. 2016;98(6):387–395.
- Stigmar K, Dahlberg LE, Zhou C, et al. Sick leave in Sweden before and after total joint replacement in hip and knee osteoarthritis patients. Acta Orthop. 2017;88(2):152–157.
- Hylkema TH, Stevens M, Selzer F, et al. Activity impairment and work productivity loss after total knee arthroplasty: a prospective study. J Arthroplasty. 2019;34(11):2637–2645.
- Pollard B, Johnston M, Dieppe P. What do osteoarthritis health outcome instruments measure? Impairment, activity limitation, or participation restriction? J Rheumatol. 2006;33(4):757–763.
- van der Zee KI, Sanderman R. Het meten van de algemene gezondheidstoestand met de RAND-36: een handleiding. [Measuring general health with the RAND-36: a manual]. Groningen (The Netherlands): Noordelijk Centrum voor Gezondheidsvraagstukken, NCG; 1993.
- McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45(5):453–461.
- Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613.
- Abma FI, van der Klink JJL, Bültmann U. The work role functioning questionnaire 2.0 (Dutch version): examination of its reliability, validity and responsiveness in the general working population. J Occup Rehabil. 2013;23(1):135–147.
- Centraal Bureau voor de Statistiek (CBS) [Central Statistical Office]. Gezondsheidsenquete [health survey]. Voorburg/Heerlen; 1989.
- Lenguerrand E, Wylde V, Gooberman-Hill R, et al. Trajectories of pain and function after primary hip and knee arthroplasty: the ADAPT cohort study. PLoS One. 2016;11(2):e0149306.
- Davis AM, Perruccio AV, Ibrahim S, et al. The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthr Cartil. 2011;19(12):1413–1421.
- Nilsdotter AK, Toksvig-Larsen S, Roos EM. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthr Cart. 2009;17(5):601–606.
- Carlson VR, Post ZD, Orozco FR, et al. When does the knee feel normal again: a cross-sectional study assessing the forgotten joint score in patients after total knee arthroplasty. J Arthroplasty. 2018;33(3):700–703.
- Sankar A, Davis AM, Palaganas MP, Beaton DE, et al. Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthr Cartil. 2013;21(10):1485–1493.
- Abma FI, Amick BC, 3rd, van der Klink JJ, et al. Prognostic factors for successful work functioning in the general working population. J Occup.Rehabil. 2012;23:162–169.
- Amick BC, 3rd, Habeck RV, Ossmann J, et al. Predictors of successful work role functioning after carpal tunnel release surgery. J Occup Environ Med. 2004;46(5):490–500.
- Townsend LA, Roubion RC, Bourgeois DM, et al. Impact of age on patient-reported outcome measures in total knee arthroplasty. J Knee Surg. 2018;31(06):580–584.
- Scott CE, Bugler KE, Clement ND, et al. Patient expectations of arthroplasty of the hip and knee. J Bone Joint Surg Br. 2012;94-B(7):974–981.
- Edwards HB, Smith M, Herrett E, et al. The effect of age, sex, area deprivation, and living arrangements on total knee replacement outcomes: a study involving the United Kingdom National Joint Registry Dataset. JB & JS Open Access. 2018;3(2):e0042.
- Podmore B, Hutchings A, van der Meulen, et al. Impact of comorbid conditions on outcomes of hip and knee replacement surgery: a systematic review and meta-analysis. BMJ Open. 2018;8(7):e021784.
- Kampshoff CS, Peter WFH, Van Doormaal MCH, et al. Royal Dutch Society of Physical Therapy guideline in osteoarthritis of hip and knee . [cited 2019 Sep 1]. Available from: www.zorginzicht.nl
- Li X, Gignac MA, Anis AH. The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Med Care. 2006;44(4):304–310.
- Hermans J, Koopmanschap MA, Bierma-Zeinstra SM, et al. Productivity costs and medical costs among working patients with knee osteoarthritis. Arthritis Care Res. 2012;64(6):853–861.
- Bardgett M, Lally J, Malviya A, et al. Patient-reported factors influencing return to work after joint replacement. Occup Med. 2016;66(3):215–221.
- L Snell D, Hipango J, Sinnott KA, et al. Rehabilitation after total joint replacement: a scoping study. Disabil Rehabil. 2018;40(14):1718–1731.