Abstract
Purpose
Sedentary behaviour is any waking behaviour in sitting, lying or reclining postures with low energy expenditure. High sedentary behaviour levels, common after stroke, are associated with poor health and higher levels of mobility disability. The aim of this study was to undertake a behavioural diagnosis of sedentary behaviour in the early phase after stroke to inform interventions that may reduce sedentary behaviour and associated disability.
Methods and materials
Independently mobile stroke survivors were interviewed three months after stroke. The topic guide was informed by the central layer of the Behaviour Change Wheel to explore three components: capability, opportunity and motivation. This model recognises that behaviour is the consequence of an interacting system of these components. Interviews were transcribed verbatim and analysed using The Framework Method.
Results
Thirty one people were interviewed (66.7 years; 16 male). The perception of diminished capability to reduce sedentary behaviour due to physical tiredness/fatigue, and pain/discomfort acting as both a motivator and inhibitor to movement, were discussed. Environmental barriers and the importance of social interaction were highlighted. Perceived motivation to reduce sedentary behaviour was influenced by enjoyment of sedentary behaviours, fear of falling and habitual nature of sedentary behaviours.
Conclusions
This information will inform evidence-based sedentary behaviour interventions after stroke.
Higher levels of sedentary behaviours are associated with poor health and stroke survivors are highly sedentary.
Stroke survivors have complex reasons for spending time in sedentary behaviours including fatigue, pain, fear of falling and environmental barriers.
Future interventions should educate stroke survivors on the health consequences of sedentary behaviours and encourage an increased awareness of time spent sedentary.
Supporting stroke survivors to identify enjoyable and achievable activities that involve standing and movement, and ideally social interaction, is recommended.
Implications for rehabilitation
Introduction
Sedentary behaviours (SB) are any waking behaviours characterised by low energy expenditure (≤1.5 metabolic equivalents) while in a sitting, reclining or lying posture [Citation1]. Stroke survivors are highly sedentary, with independently ambulatory individuals spending three quarters of their waking hours in SBs within 1 month of completion of inpatient rehabilitation [Citation2]. This volume of SB is likely to be detrimental to health, increasing the risk of cardiovascular disease incidence and mortality [Citation3], disability, including reduced physical function [Citation4], frailty [Citation5] and poor mental health [Citation6]. Breaking SB with frequent, short bouts of light intensity activity has been shown to decrease systolic blood pressure in stroke survivors, potentially reducing the risk of recurrent stroke [Citation7]. The American Heart Association/American Stroke Association recommend the reduction of SB for secondary stroke prevention [Citation8], but evidence is limited on how to do this. In 2017, Ezeugwu et al. [Citation9] reported qualitative findings from 13 stroke survivors on their SB up to 12 years after stroke, and highlighted that experiences in the early post-stroke period may lead to increased SB. The perception was that as stroke survivors left hospital their mindset was to go home to rest and recuperate. Ezeugwu et al. [Citation9] identified the early phase after discharge from stroke services as important for intervention to ensure any gains made during rehabilitation support were not lost due to participants spending excessive time engaging in SBs at home. The importance of this early post-stroke phase is further reinforced by evidence that objectively-assessed SB patterns in the early post stroke phase (1 month after stroke) are retained up to 1 year later, even in individuals who were living at home and reported high levels of functional independence [Citation10]. Determining how to reduce SB in ways that are meaningful to stroke survivors in their everyday lives, and that link to the ongoing achievement of their rehabilitation outcomes is therefore vitally important.
Behaviour change interventions, based on knowledge and theories from health psychology are increasingly being used to provide motivational support for active practice within stroke rehabilitation [Citation11], and to support behaviour change in relation to uptake and maintenance of physical activity and reduction of SB after rehabilitation [Citation12]. Applying this approach to development of an environmentally appropriate, person-centred intervention, to reduce SB after rehabilitation is therefore timely and appropriate.
Good practice in designing behaviour change interventions for application in a range of contexts, is to align with the Medical Research Council framework for complex intervention development and evaluation, using the best available evidence and appropriate behavioural theory [Citation13]. However, there exists a myriad of theories and it is difficult to identify the most appropriate. Michie et al. [Citation14] judged that none of the existing frameworks were comprehensive and few were linked to a behaviour change model. Some existing frameworks were based on the assumption that behaviour was primarily driven by beliefs and perceptions, while others placed a greater emphasis on unconscious bias or the social environment. Michie et al. [Citation14] judged that all these elements were important and needed to be brought together in a comprehensive and coherent manner. Consequently, Michie et al. [Citation15] proposed the Behaviour Change Wheel (BCW) to assist with the application of theory to intervention development. The BCW was developed from 19 existing behaviour change frameworks.
Michie et al. [Citation15] argued that in order to change behaviour it is important to first understand the nature of behaviour. Following a review of existing theories a simplified, yet comprehensive, model was proposed. At the core of the BCW is a model of behaviour known as COM-B [Citation15]. COM-B recognises that behaviour is the consequence of an interacting system involving three components (Capability, Opportunity and Motivation) [Citation15]. Capability relates to an individual’s psychological and physical capability to do the behaviour (e.g., the person must have the necessary physical strength, knowledge, skills or stamina). Opportunity relates to both the physical and social environment (e.g., physical accessibility, affordability, social acceptability and time). The final aspect relates to motivation, and includes both automatic and reflective motivational processes that may influence engagement in the behaviour, or not. These COM components interact as shown in , such that for example, enhanced capability or opportunity could increase motivation [Citation14], and together influence the behavioural outcome.
Figure 1. The COM-B system: a framework for understanding behaviour (Reproduced with permission from Michie et al. [Citation15]).
![Figure 1. The COM-B system: a framework for understanding behaviour (Reproduced with permission from Michie et al. [Citation15]).](/cms/asset/210b934d-c078-4934-a44a-f21b6c0f7c4f/idre_a_1768304_f0001_c.jpg)
According to the BCW, changing behaviour will involve changing one or more component(s) of the COM-B model. A strength of the BCW framework is that it guides the intervention design process by identifying appropriate intervention functions relating to the different aspects of the BCW. Each of these intervention functions is then linked to specific behaviour change techniques [Citation16], which form the intervention “active ingredients” of behaviour change. The BCW also aligns the intervention functions and associated behaviour change techniques with seven policy categories ().
Figure 2. The Behaviour Change Wheel (Reproduced with permission from Michie et al. [Citation15]).
![Figure 2. The Behaviour Change Wheel (Reproduced with permission from Michie et al. [Citation15]).](/cms/asset/12f845c9-1953-4805-8fbb-9dd7a4b3aeda/idre_a_1768304_f0002_c.jpg)
There has been a growth in research using the COM-B to undertake a behavioural analysis in a range of behaviours [Citation17–20]. Fewer studies have undertaken the full BCW process to design and test an intervention. An exception is Munir et al. [Citation22] who designed an intervention to reduce SB in the workplace [Citation21], showing both short and long-term effectiveness. The BCW offers an effective approach to intervention design; however to date, no study has used this comprehensive approach to develop and test a person-centred SB intervention after stroke.
In designing an intervention for use as an adjunct to stroke rehabilitation and recovery, it is critical to consider how the COM-B aligns conceptually with the dominant model of rehabilitation. Considering congruence at this stage will ensure that a developed intervention will match with rehabilitation practice, thus assuring uptake and delivery by relevant professionals. For this purpose, we employed the International Classification of Functioning, Disability and Health (ICF). The ICF is a conceptual framework that describes the consequences of disease with respect to the concepts of body functions and structure (functioning at the level of the body), activity (functioning at the level of the individual) and participation (functioning of a person as a member of society), and posits that those are influenced by contextual factors: environmental and personal factors (physical, social and attitudinal environments in which people conduct their lives) [Citation23]. The ICF also categorises activity and participation into different domains, and we will refer to those domains throughout, for categorisation purposes and clarity about what the activities are.
The ICF provides a scientific basis for understanding and studying health and health-related states, outcomes, determinants, and changes in health status and functioning, and is widely used to guide rehabilitation and measurement of rehabilitation outcomes [Citation23]. Its strong alignment to concepts within the COM-B and the wider BCW mean that it serves to link behaviour change to concepts of rehabilitation. Exploring environmental and personal factors, characterised within the COM-B as motivation and capability, will facilitate development of an intervention that promotes participation in person-centred meaningful activities relevant to individuals’ unique identities as they receive rehabilitation and recover from stroke [Citation24]. Considering both models will determine how a behavioural intervention can be developed to influence reduction in SB in the context of stroke rehabilitation and recovery.
The aim of this study was to undertake the first step in the intervention design process by undertaking a behavioural diagnosis of SB in the early post stroke phase, guided by COM-B and more broadly informed by the ICF. This information can then be used alongside the wider BCW to design an intervention with appropriate intervention functions, policy categories and behaviour change techniques to reduce and break up SB in individuals post-stroke.
Materials and methods
The study followed the Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist for reporting qualitative research [Citation25] and was registered with the National Health Service Research Scotland Stroke Research Network. The study was funded by the Chief Scientist Office of the Scottish Government (CZH/4/1091) and ethical approval was obtained from Wales Research Ethics Committee 6 on 11/06/2015 (15/WA/0224).
Participants
Independently mobile stroke survivors were purposively sampled on the basis of gender and recruited from Royal Infirmary, Edinburgh (16/09/2015-05/07/2016). Stroke survivors were included even if they were able to walk only very short distances, as these individuals could potentially reduce SB. The use of a walking aid was permitted. The recruitment target was 30 stroke survivors, (15 female, 15 male). National survey data suggest gender may influence total volume of sedentary time (contrary to physical activity (PA)), men are more sedentary than women) [Citation26]. Exclusion criteria included subarachnoid haemorrhage (unless secondary to intraparenchymal haemorrhage); dysphasia or cognitive impairments severe enough to preclude informed consent; medically unstable and/or considered too unwell by the clinical team to participate; or discharge to a nursing home. Upon recruitment, descriptive information (gender, age, Scottish Index of Multiple Deprivation (SIMD), side and effect of stroke, functional status pre/post stroke and walking aid) was collected.
Interviews
Six weeks after stroke, the research assistant (SN) checked each participant was well and an interview appointment was arranged. One week prior to the interview, participants were posted a questionnaire booklet which included the Hospital Anxiety and Depression scale [Citation27]; the Fatigue Assessment Scale (FAS) [Citation28]; the Physical Activity Scale for the Elderly (PASE) [Citation29]; Barthel Index of Activities of Daily Living [Citation30]; the Simplified Modified Rankin Scale [Citation31] and a Visual Analogue Scale to determine the percentage of the day spent sedentary.
Semi-structured interviews were conducted, at three months post stroke, in participant’s own homes, audio-recorded on a digital device and transcribed verbatim. The interview topic guide (Supplementary File S1) was informed by COM-B [Citation15]. Participants were asked questions about their daily sitting behaviour, questions targeting factors that influence their sitting behaviour with reference to capability, opportunity and motivation and their thoughts on how to reduce sitting. The interview topic guide was piloted with the first three study participants and no changes were made.
Analysis
Anonymised transcripts were analysed using the Framework Method [Citation32], which is a matrix based seven stage method providing a systematic, comprehensive and transparent approach to analysing qualitative data [Citation32]. The seven stages are: transcription, familiarisation with the interview, coding, developing a working analytical framework, applying the analytical framework, charting data into the framework matrix and interpreting the data. After transcription, three researchers (SN, CF and AN) familiarised themselves with three interview transcripts and conducted line by line coding (familiarisation with the interview). The researchers met to discuss their interpretations of each interview, and reach agreement on how to consistently code (coding). Individual codes were inductively grouped together into themes, which were subsequently clustered into the pre-existing overarching themes in line with the COM-B (developing working analytical framework). The analytical framework was developed, and applied to a further three transcripts, to further confirm consistency of interpretation of the coding framework. The framework was applied to one transcript by a fourth member of the research team (JM) to ensure correct application of the framework (applying analytical framework). The remaining transcripts were coded in line with the analytical framework by SN with CF double coding a further four transcripts to continue to discuss and confirm interpretations (charting data into framework). Gale et al. [Citation32] discussed it is helpful in multi-disciplinary teams to compare and contrast styles of summarizing in the early stages of the analysis process to ensure consistency within the team. Data were managed using NVivo 10. Once all transcripts were coded, framework matrices were developed to facilitate interpretation of the data. To condense the findings, a 1-2 page memo summarising each theme was written, including key findings. If present, any gender or age differences were noted.
Enhancing rigour
In order to enhance rigour in the method, several strategies were incorporated. Self-reflection is an essential part of qualitative research whatever the chosen qualitative methodology. The researcher must take into consideration any “pre-understanding,” both in the planning and analysis process, to help reduce researcher bias [Citation33]. In this study, it is acknowledged that the COM-B component of the BCW was identified by the researchers as a useful framework to address the research question, and as such informed both the data collection and analysis. Nevertheless, the identification of sub-themes in the analysis was an inductive process, and the content of these sub-themes was not pre-defined. During this process, rigour was enhanced by including several members of the research team, agreeing upon coding rules prior to the analysis, and regularly discussing, debating, and reflecting on coding, theme development, and finally the content of the overarching framework. Member checking was also included in order to verify with the participants the researcher’s interpretation of the interviews [Citation34]. The Consolidated Criteria for Reporting Qualitative Research recognises member checking as a method of rigour: “ensuring that the participants’ own meanings and perspectives are represented and not curtailed by the researchers’ own agenda and knowledge” [Citation25]. The research assistant read through each transcript and made a 1-2 page summary of the key points. These summaries were posted to each study participant. Participants were asked to review the summary of their interview to check that they felt our interpretation of the discussion was appropriate.
Results
Thirty one stroke survivors were interviewed ().
Table 1. Participant characteristics.
Results are reported in line with COM-B, and quotations included to illustrate these findings. ICF definitions of activities are used to distinguish the types of activities participants described, that were not sitting.
Behaviour domain
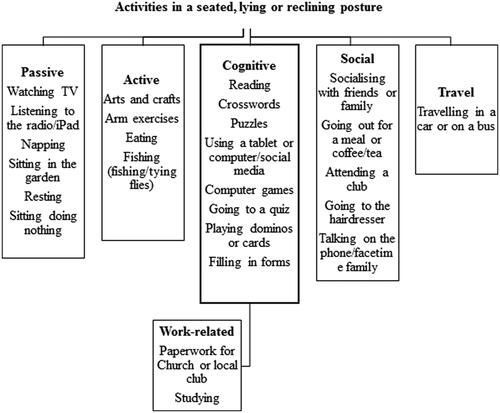
Participants discussed leisure and recreational activities they undertook while in a sitting, lying or reclining posture ().
Men tended to watch TV or read the newspaper, for example: “…bring the papers back, and I’ll sit down and have my breakfast and I’ll read the papers and it can take two hours.” (Male, 72 years, SIMD 4-5, no walking aid), while women tended to watch TV, do puzzles, crosswords or arts and crafts:
Well, in an afternoon, I like to sit down and watch the telly, about three o’clock, after my lunch. I’ll maybe, or maybe four o’clock or something, I do a bit of art. Because they say that’s for stress – stress relief things, this is a new thing for stress relief, this colouring in thing. So I do an hour, or two hours of that.
(Female, 83 years, SIMD 4-5, no walking aid)
Opinions about time spent watching the television varied. Some participants purposively watched particular programmes, as illustrated by this quote: “I watch television. I watch the news. I like to catch the ten o’clock news, so I’m watching the ten o’clock news and then I’m watching the BBC 2 type of programmes.” (Male, 72 years, SIMD 4-5, no walking aid). Conversely, the TV was also used to help consume or pass the time: “there’s very little on the telly I really enjoy, very little, but just sitting and something to do, that’s all. Passing the time, as they say.” (Male, 80 years, SIMD 4-5, 1 walking stick).
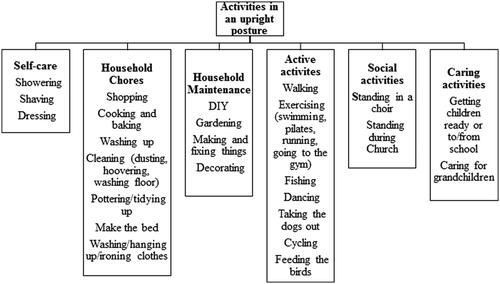
Participants also described their day-to-day activities in an upright posture and these were grouped into clusters involving self-care tasks, domestic and household chores and household maintenance, caring activities involving assisting others, and socialising ().
Both men and women frequently discussed shopping, cooking and tidying up/cleaning tasks, while household maintenance tasks were mentioned more frequently by men:
…just general DI…just dodging about the house. I’ve always got something to do.
I: What kind of things do you like doing then, round the house?
R: Anything, electrical stuff, plumbing. That’s ceiling fell down in the kitchen, so I’ve started on that the now. I’ve got my shed and always out there
(Male, 50 years, SIMD 1-3, no walking aid)
Many participants described walking as their dominant non-sitting activity. This included walking the dog or walking with friends and family. Walking was undertaken for leisure or recreation, or health benefits. Walking facilitated recreation, leisure and socialising, enabling people to get to the shops, bus stop, Church, to meet friends and take grandchildren to the park:
I walk – there is a wee shop along the road just on the way to [text removed for anonymity], so we walk along there to get the paper and then we walk back. I can walk quite well on the flat but I can’t do hills. (Female, 80 years, SIMD 4-5, 2 walking sticks)
The COM-B model was then used to explore the influences of the behaviour in relation to capability, opportunity and motivation to reduce/break up SB. The most frequently reported themes that emerged are shown in .
Table 2. Overarching themes in line with COM-B model.
Capability
Six themes were identified within this overarching theme, two related to physical capability and six to psychological capability.
Physical capability and stroke related physical health
Physical capability was influenced by the impact of stroke on body functioning, specifically movement related function, as defined by the ICF. Physical capability was defined as a participant’s ability to be active and sit less, and carry out daily self-care and household tasks. All participants reported they were physically able to mobilise independently, most without difficulty. A small number of participants mentioned dizziness on standing, difficulty getting out of a chair/climbing stairs, or not having been out of the house yet. An element of physical capability related specifically to stroke related physical health problems and included arm and leg hemiparesis, problems with balance/dizziness/co-ordination, speech, vision, bladder control, pain in knee/legs/back, fine motor control, and numbness in feet and hands. Participants discussed how they felt their physical capabilities (classified within the ICF as impairments in body function, that occurred either as result of their stroke or their general health) influenced SBs, and consequently caused limitations in different types of activity. Nine participants felt their ability to stand/move was limited due to pain or discomfort and needing to sit because of pain/discomfort in hips/back/legs or to rest swollen feet, for example: “It’s sore to be standing. When I’m trying to stand at the worktop, I just get low back pain. Awful low back pain.” (Female, 67 years, SIMD 1-3, no walking aid). In contrast, a small group of five participants felt that sitting/lying caused pain/discomfort with feelings of stiffness or pain in back/coccyx or side mentioned: “I get pains in my coccyx if I’m doing a lot of sitting, I think, you know.” (Female, 56 years, SIMD 4-5, 1 walking stick).
Twenty-two participants discussed feelings of fatigue or tiredness across both physical capability and stroke related health themes – the majority attributed fatigue/tiredness symptoms to their stroke, but a small group did not feel their stroke was the cause (cough (n = 2), work, COPD or not sure). Feelings of general fatigue or tiredness in specific parts of the body were discussed (e.g., back or legs). Some participants talked about how tiredness influenced their sitting in an “acute” or “delayed” sense after activity. These perceived impairments in body function affected activity performance, with individuals discussing doing a task or activity and urgently having to sit down – “being hit by a wall of weariness.” Examples given were having to sit down after taking a shower, sitting on the bed after going upstairs, or doing some dishes and then having to sit down and go back again, for example: “I come out the shower and like have to sit on the end of the bed; I’m absolutely knackered.” (Male, 54 years, SIMD 1-3, no walking aid). Delayed fatigue was mentioned if the previous day had involved activity: “Like if I’ve got my hospital appointments at the [text removed for anonymity], I am totally and utterly knacked the next day” (Female, 67 years, SIMD 1-3, no walking aid). More generalised fatigue was also discussed and trying to manage fatigue symptoms across the day. There was an awareness they had to sit to manage energy levels and to rest their body or a specific body part (mostly legs): “…and also because you’ve only got so much energy in the day and you do have to rest after you have a stroke.” (Female, 56 years, SIMD 4-5, 1 walking stick).
Psychological capability
Six key themes emerged under psychological capability related to mental health after the stroke – stroke related psychological health and mental strength, knowledge about SB, PA and stroke, and awareness of sitting.
Stroke related psychological health
Psychological consequences that participants perceived as a result of their stroke included feeling frightened/anxious, low mood/depression and variability in mood, increased feelings of aggression/less tolerant, forgetfulness or disorientated, loss of concentration, and struggling to sleep. Some participants were aware these psychological changes had influenced their activities, discussing feelings of anxiety or embarrassment when out of the house, anxiety or depression stopping them doing things, or uncertainty about whether changes in mental health were a sign to slow down, for example: “Me. Me, myself. My anxiety, my depression, that stops me. I don’t want to do anything and it’s… I know I should but I just don’t want to do it” (Male, 53 years, SIMD 1-3, no walking aid).
Mental strength
Mental strength was less specific than stroke-related psychological issues and was defined as the participant’s mental ability to sit less. Nine participants discussed how they could not be bothered to do things and feelings of apathy. These individuals were aware that mental tiredness was different to physical fatigue – they wanted to get on and do things but just could not summon themselves to do it, for example:
I mean, how can someone go from being so active to having….well virtually non activity, which is what’s happening. But I don’t feel the need. Whether it’s just because of all the stroke and this, I don’t know. (Female, 67 years, SIMD 1-3, no walking aid)
Knowledge about the potential health consequences of sitting
Some participants expressed uncertainty about effects of sitting on their health, for example “I: How do you think sitting for long periods affects your health? R: I have no idea” (Female, 34 years, SIMD 1-3, no walking aid). Others expressed specific health concerns (not good for your heart/back, could cause another stroke, body gets sore, not maximising your abilities).
Knowledge of physical activity
As well as understanding the health consequences of not sitting too much, a third of participants discussed the importance of being purposefully physically active, as illustrated by this quote: “Well, it’s important to keep yourself moving and all that, you know. And you can’t just sit all the time and vegetate or whatever like, you know” (Male, 74 years, SIMD 4-5, no walking aid). Some discussed specific benefits including helping blood pressure, the spine, the mind/coping, and keeps muscles moving. Others expressed uncertainty about how much PA they should be doing.
Knowledge of potential causes of stroke
A range of possible causes for stroke was given including age, lifestyle and stress. Some participants (6) spoke about being anxious or worried about bringing on another stroke and limiting movement to prevent stroke, while one younger participant discussed trying to change lifestyle habits by engaging more in purposeful physical activities:
I would say that, now, that I am worried, I’m sitting a lot less. Because I understand that the problem was with, like they were saying, the blood, and the flow of blood, and that. So I’m sitting a lot less, I’m trying to be more active, I try to, I don’t know, change the habits that caused my stroke. (Male, 36 years, SIMD 4-5, no walking aid)
Awareness of sitting
Awareness of sitting included an awareness (or lack) of time spent sitting. The majority of participants were not aware of how long they spent sitting, often losing track of time throughout the day. Some individuals discussed how they lost track of time due to engagement in a seated leisure or recreational task, while others commented more generally that they did not notice time passing, for example, “There are sometimes I do realise I’m sitting a long time but most of the time it just goes away. Time at the moment for me is nothing” (Male, 53 years, SIMD 1-3, no walking aid).
Opportunity
Physical environment
All participants discussed their physical environment and how it influenced their SB. Participants identified the home environment as influential, with home modifications (rails/cushions/risers), access to a garden, and stairs in the home helping to increase how much they moved around. For example, one participant highlighted “I think your environment plays a large role. I have no choice but to go up and down the stairs, you know – if I lived in a bungalow it would be different” (Female, 53 years, SIMD 1-3, no walking aid). Bad weather and darker nights increased SB and made walking for leisure less likely as illustrated by one participant:
“R: …well, in the summer we’d be out walking a bit but, I mean, in this weather you don’t want to go out.
I: Do you think the weather and the seasons, kind of, dictate how much you can….
R: That, and then of course the winter is dark and I’m frightened of the dark”
(Male, 83 years, SIMD 4-5, zimmer).
Positive aspects of the local physical environment that enhanced particpants’ walking for leisure and participation in social activities included access to nice walking spaces, access to public transport and local community classes. However, a lack of these and/or a lack of public seating were attributed to decreased outdoor walking for leisure, for example:
R: I used to take walks away up the back up that way, it used to be all fields. We used to take the dog – the dog could run about and everything and now it’s all houses – it’s the same down that way – it’s all houses now.
I: No green space to walk in?
R: No, not as much as there was. (Male, 46 years, SIMD 1-3, no walking aid)
Financial problems were a concern for some study participants. Since their stroke, a lack of money meant participants could no longer participate in recreational and leisure activities outside the home. However, access to free bus travel enabled walking for leisure outside the home and reduced SB: “because the bus from here goes right to [text removed for anonymity] and we could walk right through to [text removed for anonymity] and then get…I mean, it costs us nothing on the buses” (Male, 83 years, SIMD 4-5, zimmer).
Social environment
Social environment related to how the participant’s social environment influences opportunities to sit less by providing active opportunities for socialisation. Participants detailed active social lives, meeting friends for coffee or lunch, going to Church, caring for grandchildren, going to local clubs, the pub, or having visitors. Social participation helped to break sitting, by getting participants up and out the house or getting them up to complete self-care tasks if visitors are coming. For example, one participant said:
If I knew somebody was coming, like my speech therapist, my occupational therapist, I’d make the effort in the morning and get up and have a shower and have a shave and I’d be ready for her. Then other…if they weren’t coming I would just probably be sitting do nothing. (Male, 50 years, SIMD 1-3, no walking aid)
Some participants had more limited social circles, spending more time sitting alone. While some were happy with this, others felt wider social participation would give them purpose and opportunities to reduce SB. One individual said: “I don’t have a particularly strong social life and I think that that would actually help, you know, if you were, sort of, even if it was just going and doing something fairly low key with other people” (Female, 53 years, SIMD 4-5, no walking aid). Lack of social participation was particularly evident with participants in their 40 s and 50 s. Professional working commitments had limited social opportunities prior to stroke, teenage children may still be at home but gaining independence, and partners and friends were often out working during the day. Interacting with psychological capability, psychological changes since the stroke influenced social opportunities in some participants including a reluctance to go out on their own, a loss of confidence in busy environments, or not wanting to socialise with others.
Social support
The majority of participants had received support with domestic tasks from family and friends. In some instances this encouraged activity, for example if a family member or a neighbour offered to take them shopping, while in other instances family members or friends completed tasks for the individual, for example cooking a meal or bringing in wood for the fire. Support initially given after the stroke was reducing as participants re-established their independence – “It’s just other people have got things to do that you can’t expect them to keep coming round and doing things with me. Everybody’s got their own lives and their own activities and what have you” (Female, 78 years, SIMD 4-5, 1 walking stick).
Around half of participants perceived their family/friends would be supportive of them sitting less, especially if it aided recovery. Some participants felt however, their friends and family would be unsure about them sitting less. These participants reported friends/family felt they currently did enough, expressed a fear of them being out of the house or doing certain tasks. One individual explained how her friend encouraged her to sit down and relax:
My friend actually bought me one of those, you know, adult colouring books and she said, oh this will be really good and this will help you sit down and relax and it will help your cognitive, you know, skills as well, you know.
She is always saying, ah you are still running around too much, you should take it easy, you know, your body is trying to tell you to, you know, it’s still repairing itself (Female, 53 years, SIMD 1-3, no walking aid)
Professional support
Professional support included support given (or not) from health professionals and other services within the community. Advice to sit less would not conflict with any advice participants had received from health professionals, but participants mentioned the importance of a consistent message from health professionals, with one individual saying they would not want anything to conflict with advice given by their general practitioner. Timing of information provision was also highlighted, as illustrated by this quote: “Because although you’ve been given the information in hospital, a lot of it doesn’t sink in because….well I don’t know about everybody else, but I was frightened” (Male, 60 years, SIMD 1-3, no walking aid). The majority of participants would agree with advice from a health professional to try and sit less, although some individuals wanted further information on why it would be important and how to go about it, for example:
“R: Well, if they gave me a good reason for it I would take it on board.
I: How do you think you would go about doing that then?
R: Well, I’d want to understand the logic, or rationale behind what they’re telling me to do” (Male, 72 years, SIMD 4-5, no walking aid).
Three months after their stroke, one-third of the sample spoke about still being in receipt of rehabilitation services (physiotherapy, occupational or speech therapy, counselling). Three people mentioned waiting either to be sent for physiotherapy or for a place in a stroke exercise class. Others perceived a general lack of professional input following discharge, discussing what they felt was relatively minimal support, for example
“From the health professional side, the professional side of it I think once, if like myself you are still mobile, you are left – that’s it”
(Male, 46 years, SIMD 1-3, no walking aid).
Opportunity to sit less
Over half of participants felt they had opportunities to sit less, whilst others reported they were already doing all they could. Some participants were unsure how to sit less, suggesting, in line with rehabilitation delivery, that they would need Health Professionals to give alternatives to sitting, while others offered suggestions on how to reduce sitting including walking, doing housework such as cleaning, changing position by standing and moving more, and socialising. Reasons for breaking sitting were varied. Women discussed household tasks to break their sitting, whereas men discussed walking to break sitting. Techniques in the home included household tasks, tidying and cleaning, going to the toilet, making tea or coffee, or cooking a meal, as illustrated by this quote: “I mean I’ll stand up when I’m preparing food I’m standing up, you know. I do cook from scratch; I don’t do instant meals and things, so I’m standing up with food preparation” (Female, 56 years, SIMD 4-5, 1 walking stick). Assisting others by letting pets out and by caring for a family member (children and elderly partners) were other ways to break sitting. Some participants used cues to break sitting, including TV adverts, monitoring time, reminders on a computer or phone, or getting up to answer the phone.
Motivation
Reflective motivation
In relation to reflective motivation, three themes were identified under intention – whether participants intended to be more physically active/move more/sit less; lacked intention to sit less/move more or be more physically active; or intended to sit. Returning to previously enjoyed leisure and recreational activities/physical activities/previous functioning in domestic and social life or having a goal of returning to work encouraged less sitting and an increase in purposeful PA, as did relieving boredom, wanting to play with grandchildren and feeling “lucky” in comparison to others. For example, one individual said:
And it makes me…when I’m sitting talking to these and seeing where they are now, what they can and cannot do and how long the….ago their stroke and everything else, it makes me realise how lucky I was. But also makes me a little bit more determined to get out and do that walk and do that bit of exercise
(Male, 60 years, SIMD 1-3, no walking aid)
Some participants intended to be more physically active, but discussed limitations and setbacks they were facing, for example: “I wish I could walk more, you know. But unfortunately I can’t really walk far at all” (Female, 87 years, SIMD 1-3, 1 walking stick). Participants also detailed times across the day when they intentionally sat, such as to enjoy and concentrate on valued leisure or recreational activities, as illustrated by this quote: “…but if there’s something I’m looking at particularly you’ve got to sit down, haven’t you. You can’t walk about the house and concentrate” (Male, 72 years, SIMD 4-5, no walking aid). However, some participants talked about how they actively forced themselves to sit across the day – ”No, I really force myself to sit. I’m tired, I’m still a bit fatigued and my minds saying do that, do this and I just stop…” (Male, 50 years, SIMD 1-3, no walking aid). A sense of entitlement to sit was evident in some individuals, either due to perception of high PA earlier in their life or a feeling of accomplishment if they had done a lot that day with one participant saying:
“I do sit quite a bit now, but I think I’m entitled, after four children, within six years. So I feel that I deserve it, sitting down, if you don’t mind!”
(Female, 83 years, SIMD 4-5, no walking aid).
A lack of intention to move was evident in some participants including negative perceptions of sitting and lack of movement – shear laziness, cannot be bothered, getting a bit lazy, boredom. There was a sense of frustration as to why intention was lacking and an awareness that intention could vary daily. Some participants felt they needed help to become motivated with one individual saying: “I wouldn’t go out but I would try and I would go, well sometimes you’d try, sometimes you’d have your funny days and these kind of days nobody could motivate you” (Male, 50 years, SIMD 1-3, no walking aid). There was also a reluctance in some participants to adopt different behaviours when carrying out tasks normally performed when sitting (e.g., standing to read or talk on the phone), as illustrated by this quote: “I wouldn’t dream of standing and reading a paper like, you know, when I’ve got half a dozen chairs here, eh, so” (Male, 74 years, SIMD 4-5, no walking aid).
Beliefs about capability
Confidence to engage in social, leisure, recreational or physical activities that were not sedentary was reduced for many, especially early after stroke. A loss of independence was illustrated by reluctance to go out alone, use public transport, drive, walk the dog, or travel to meet friends, and that had increased SBs. Uncertainty around the distance they could safely walk and fear of falling were key issues, especially for women. Physically participants were aware of a need to pace themselves and plan regular breaks, with one individual saying: “I do everything in stages because of my fatigue. But now I can do it and I just need to stop ‘cause I’m not wanting to tire myself out or damage myself” (Male, 50 years, SIMD 1-3, no walking aid).
Beliefs about consequences of activity
This theme linked to participants’ “knowledge” about PA and included beliefs about being active for long periods. The majority discussed beliefs about the consequences of being physically, socially or recreationally active, for example – ”I think everybody needs to do something. I think when you’ve got nothing to do that’s worse, worse than anything for a stroke patient, really. I think if you can get up and do it’s so much better” (Female, 72 years, SIMD 4-5, no walking aid). Finding a balance though in the amount and type of physical activity was necessary to avoid pain, fatigue, bringing on another stroke or increasing blood pressure, falling, or having knock-on effects to the next day. One individual talked about this in relation to her blood pressure: “so I’m quite anxious about getting the balance between trying to get back to normal and being fit and healthy and the risks of spiking my blood pressure and causing further problems” (Female, 53 years, SIMD 4-5, no walking aid).
Beliefs about consequences of sitting
Positive beliefs about time spent sitting clustered around mental health benefits, sitting to rest and facilitating valued seated activities. Negative beliefs clustered around physical health, including stiffness and discomfort. Participants perceived sitting slows the body down, becoming more dependent on sitting in the future. Sitting could also cause boredom, depression, low mood and a lack of purpose, which all would further increase SB. There was a sense of frustration and guilt in a number of participants due to not getting household tasks done and increasing the burden of others.
Automatic motivation
Habit and explanation of daily routine
A small group of participants described their sitting as a habit. Participants reported it was a natural thing to sit, especially if they had nothing to do, for example: “Basically if I’m not doing anything – I mean I’ve been out and I’ve done everything, then the most natural thing is just to sit” (Female, 53 years, SIMD 1-3, no walking aid). Other explanations given for habitual sitting included boredom, lack of conscious tracking of sitting (or standing), a routine you fall into and sitting when all chores were completed. There was a perception that watching TV was a bad habit (“I tend to watch the TV which is a bad habit, I know” (Male, 72 years, SIMD 4-5, no walking aid)), however some participants reported it gave them something to do. Participants were aware time of day influenced their sitting patterns. Social norms around sitting in the evening were discussed, as well as clustering household tasks in the morning, followed by increased sitting in the afternoon and evening – “In the evenings, that would be the time…you’re just slumping a bit, as most people do I suppose” (Female, 56 years, SIMD 4-5, 1 walking stick).
Discussion
This is the first qualitative study on SB in the early post stroke phase (3 months after stroke) in a large sample of stroke survivors (31 participants). Our qualitative findings provide an essential point of reference for the development of robust SB interventions in the early phase after a stroke, that will inevitably complement the broad goals of rehabilitation during that phase, by also encouraging participation and skill development in a wide range of physical, domestic and leisure activities. The most salient factors that future SB interventions should consider related to the influence of physical tiredness and fatigue on SB; pain/discomfort acting as both a motivator and inhibitor to these activities; environmental barriers to participation in physical, domestic and leisure activities; the importance of social interaction; fear of falling; enjoyment of SB/lack of intention to move; the importance of valued physical, domestic and leisure activities; and the habitual nature of SB.
At three months after stroke, TV viewing emerged as a dominant SB, and non-SB activities could typically be categorised as household tasks, such as shopping, cooking and household tidying/cleaning, or walking. Although evidence exists regarding levels of SB post-stroke (English, 2014), the findings of this study provide context relating to SB, which is important for tailoring interventions. In relation to physical capability to reduce SB, physical tiredness and fatigue emerged as strong determinants. Fatigue after stroke is a common complaint – at 3 months post stroke fatigue prevalence in a Norwegian sample was 31% [Citation35]. Previous studies with stroke survivors [Citation9], older women [Citation36] and care home residents [Citation37] have noted the influence of fatigue on SB and daily activity levels. We are not aware however, of any previous qualitative studies that have distinguished between the effects of acute tiredness and chronic fatigue symptoms on SB after stroke. Acute task-related tiredness may be a result of reduced cardiorespiratory fitness in this group, either as a result of premorbid activity, the effects of the stroke, or low levels of activity after the stroke [Citation38]. Focusing on regular short breaks in SB may be more realistic in these individuals than a longer, continuous session of more physically demanding leisure activities or exercise. Interrupting prolonged sitting with light-intensity walking breaks has been shown to lower self-reported fatigue in obese adults aged 45-75 years, and may therefore present a promising therapeutic intervention after stroke [Citation39].
Pain and discomfort were viewed as both motivators and inhibitors to movement. This has previously been noted in older women [Citation36] and older men and women [Citation40]. While more time spent in SBs has been shown to result in worse bodily pain in community-dwelling older adults [Citation41], greater engagement in daily SB has also been shown to be associated with less subsequent bodily pain in community dwelling older adults and in older adults with knee osteoarthritis [Citation42,Citation43]. The literature around pain and SB is clearly complex and highlights the need for individualised intervention components with scope for variability in pain symptoms. This may help to avoid the scenario where individuals avoid movement, leading to future deconditioning, additional muscle weakness and contributing to increased pain [Citation44].
A broad range of psychological consequences of the stroke was discussed, eliciting in some anxiety about leaving the house and uncertainty about how much physical activity to do. Feelings of mental tiredness/fatigue and apathy evidently influenced ability to move in some. This aligns with Ezeugwu et al. [Citation9] who concluded a major determinant of SB in the early post stroke phase was what they termed the “head game,” with one of their participants discussing how you come out of hospital in a mental state where you just want to sit. Causes of post-stroke fatigue are complex and multifactorial [Citation45]. Mental fatigue has been associated with cognitive impairment, specifically impairments in memory, executive functioning and attention [Citation46,Citation47]; and with depression [Citation48]. It is therefore likely that SB occurs in part as a consequence of the experience of mental fatigue that results from some or all of these factors. In development and implementation of an intervention to reduce SB, consideration of fatigue and associated cognitive deficits and mood, as well as of physical functioning, should be undertaken. This will require multi-disciplinary input from physiotherapists and occupational therapists as practice specialists.
Interestingly however, at three months after their stroke, some of the participants discussed a lack of professional rehabilitation support since discharge, which they felt would have been beneficial. This perceived lack of professional support may reflect the diversity of stroke survivors with those who may not seem to have been badly affected/made a reasonable recovery, unable to access rehabilitation services.
Knowledge about potential health consequences of SB was varied. Ezeugwu et al. [Citation9] noted a limited awareness of the health risks of SB among stroke survivors. Concise and user-friendly information is needed on the health consequences of SBs after stroke, ideally incorporating evidence-based guidance on the frequency and duration of upright behaviours needed to reduce future stroke risk. This should help to allay fears that not sitting and moving more may result in another stroke. The majority of participants were unaware of how long they spent sitting across the day. Future research should explore the use of technologies using computer, mobile and or wearable devices that can make stroke survivors aware of their SB and facilitate self-monitoring [Citation49].
A range of environmental facilitators and barriers to movement emerged. Providing clear information on local facilities, their cost and transport opportunities may help change perceptions in relation to accessing activities outside the home. Specifically focusing on strategies to reduce SBs in the home during the wintertime when dark evenings/poor weather may limit outdoor activities is worthy of consideration [Citation50]. Social networks helped to break sitting, by getting participants up and out the house, or to complete self-care tasks. This finding is consistent with previous research showing a perception that social isolation increases time spent sitting in older men and women [Citation40]. Opinion was divided with our participants as to whether family/friends would be supportive of them reducing SB. The protective influence of relatives around activity levels has previously been observed in care home residents [Citation37]. Going forward, interventions should involve family members and friends, reassuring them that breaking up SB will be of benefit and strategies they could employ to support the stroke survivor. Similar to family members and caregivers, training and educational materials are needed for health professionals to ensure consistent messaging. Intervention materials could seek to incorporate the strategies and cues participants in this study were aware they used to break up their sitting (e.g., prompted by advert breaks on television).
In relation to motivation to sit less, participants discussed a range of factors which encouraged movement, including relieving boredom or being keen to get back to their “old life.” Recognising sitting though as a positive, valued behaviour emerged from our interviews with participants acknowledging they enjoyed sitting or found it beneficial (pain management, relaxation). Sitting for relaxation or comfort emerged as the main reason participants sat in the Ezeugwu et al. [Citation9] study, while enjoyment of sitting and sedentary activities has previously been noted as a barrier to reducing SB in older adults [Citation51]. A lack of intention to move was evident in some, aligning with psychological fatigue [Citation52], with some participants feeling they needed help to become more motivated. Some participants spoke of needing interesting, valued activities to be more active. Taking a person-centred approach to reducing SB is therefore vital. Person-centredness in rehabilitation means taking a biopsychosocial perspective of the person in their context, empowering them in shared decision making, and creating a therapeutic alliance in which recipients of rehabilitation are partners [Citation24]. Future interventions delivered as part of, or as an adjunct to, rehabilitation should therefore support participants to identify positive, personally valued and enjoyed activities that involve standing and/or moving. Matei et al. [Citation50] highlighted the importance of providing a clear justification of any intervention strategies – for example standing and moving during breaks in a TV show may help manage stiffness and discomfort. When participants discussed beliefs about their capability to reduce their SB a fear of falling emerged, especially in women. Mobility problems and fear of falling have previously been documented in care home residents as barriers to engaging in movement/activity [Citation37]. Intervention materials should seek to incrementally build a person-centred plan to break sitting and encourage walking and moving more that aligns with individual ability and builds confidence, while also drawing on the literature on the influence of habitual PA on reducing falls and improving bone health [Citation53,Citation54]. Overall, it is important to recognise that stroke is a very complex condition and affects individuals not only physically and cognitively but also socially. Individuals who have similar aetiology of strokes may present differently and therefore individualised approaches to reducing SB are required.
Some participants discussed their SB as a habit with sitting perceived as a natural thing to do. Social norms around sitting in the evening were discussed, as well as clustering household tasks in the morning. Time-lapse camera data has shown that many older adults tend to sit more in the afternoon and evening [Citation55]. Interventions could aim to reduce the automaticity of sitting by increasing awareness of the behaviour and encouraging development of new non-SB habits.
Strengths and limitations
The qualitative nature of this study and open-ended questioning throughout the interviews have allowed rich, descriptive data on SB after stroke to be elicited from a large number of participants. A limitation of our approach is that we focused on SBs from the perspective of the individual stroke survivor at a single time point. Interviewing stroke survivors at other time points, as well as interviewing staff or family/friends would enable a broader synthesis. Michie et al. [Citation14] recommend utilising a range of approaches to data collection (interviews, focus groups, observation, review of key documents) to enhance confidence in the findings. Nevertheless, the views of the intended recipients of any future intervention are, arguably, the most important, and thus justify the focus on these participants. The structured approach used during analysis, aligning the qualitative data with the COM-B constructs, could be perceived as a limitation. However, the use of an inductive approach using the Framework Method, prior to aligning themes to COM-B ensured a systematic and robust approach to the data analysis. The use of the COM-B framework in the context of the ICF is a strength of this work as the theoretical underpinning of the work allows the qualitative data to be developed into a theory driven behaviour change intervention that fits with concepts within rehabilitation. A further limitation of the study was that we did not collect data on ethnicity and therefore do not have any specific cultural related findings to report.
This study presents a behavioural diagnosis of SB in the early post stroke phase, guided by COM-B. This information will be used alongside the wider BCW and the ICF to design an intervention with appropriate intervention functions, policy categories and behaviour change techniques to reduce and break up SB in individuals post-stroke.
Supplementary_material.pdf
Download PDF (417.8 KB)Acknowledgements
The authors thank the NHS Research Scotland Stroke Research Network for their assistance with recruitment.
Disclosure statement
Two members of the research team (GM & CF) are co-investigators on a National Institute for Health Research Programme Grant for Applied Research [RECREATE: Development and evaluation of strategies to reduce sedentary behaviour in patients after stroke and improve outcomes; 2017-2024; RP-PG-0615-20019].
Data availability statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Additional information
Funding
References
- Tremblay MS, Aubert S, Barnes JD, et al.; SBRN Terminology Consensus Project Participants. Sedentary Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75.
- Ezeugwu VE, Manns PJ. Sleep duration, sedentary behavior, physical activity, and quality of life after inpatient stroke rehabilitation. J Stroke Cerebrovasc Dis. 2017;26:2004–2012.
- Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162:123–132.
- Gennuso K, Gangnon R, Matthews CE, et al. Sedentary Behavior, Physical Activity, and Markers of Health in Older Adults. Med Sci Sports Exercise. 2013;45:1493–1500.
- del Pozo-Cruz B, Mañas A, Martín-García M, et al. Frailty is associated with objectively assessed sedentary behaviour patterns in older adults: evidence from the Toledo Study for Healthy Aging (TSHA). PLoS ONE. 2017;12:e0183911
- Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. 2015;15:513
- English C, Janssen H, Crowfoot G, et al. Frequent, short bouts of light-intensity exercises while standing decreases systolic blood pressure: Breaking Up Sitting Time after Stroke (BUST-Stroke) trial. Int J Stroke. 2018;13:932–940.
- Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2532–2553.
- Ezeugwu VE, Garga N, Manns PJ. Reducing sedentary behaviour after stroke: perspectives of ambulatory individuals with stroke. Disabil Rehabil. 2017;39:2551–2558.
- Tieges Z, Mead G, Allerhand M, et al. Sedentary behavior in the first year after stroke: a longitudinal cohort study with objective measures. Arch Phys Med Rehabil. 2015;96:15–23.
- Stewart C, Power E, McCluskey A, et al. Development of a participatory, tailored behaviour change intervention to increase active practice during inpatient stroke rehabilitation. Disabil Rehabil. 2019.
- Kringle EA, Barone Gibbs B, Campbell G, et al. Influence of interventions on daily physical activity and sedentary behavior after stroke: a systematic review. PM&R. 2020;12:186–201.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
- Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. London: Silverback Publishing; 2014.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
- Michie S, Richardson M, Johnston M, et al. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann Behav Med. 2013;46:81–95.
- McCutchan G, Wood F, Smits S, et al. Barriers to cancer symptom presentation among people from low socioeconomic groups: a qualitative study. BMC Public Health. 2016;16:1052.
- Handley MA, Harleman E, Gonzalez-Mendez E, et al. Applying the COM-B model to creation of an IT-enabled health coaching and resource linkage program for low-income Latina moms with recent gestational diabetes: the STAR MAMA program. Implement Sci. 2016;11:73.
- MacDonald B, Fitzsimons C, Niven A. Using the COM-B model of behaviour to understand sitting behaviour in U.K. office workers. Sport Exerc Psychol Rev. 2018;14:23–32.
- Phillips R, Copeland L, Grant A, et al. Development of a novel motivational interviewing (MI) informed peer-support intervention to support mothers to breastfeed for longer. BMC Pregnancy Childbirth. 2018;18:90.
- Munir F, Biddle SJH, Davies MJ, et al. Stand More AT Work (SMArT Work): using the behaviour change wheel to develop an intervention to reduce sitting time in the workplace. BMC Public Health. 2018;18:319.
- Edwardson CL, Yates T, Biddle SJH, et al. Effectiveness of the Stand More AT (SMArT) Work intervention: cluster randomised controlled trial. BMJ. 2018;363:k3870.
- World Health Organisation. Towards a common language for functioning, disability and health: the International Classification of Functioning, Disability and Health. Geneva: ICF; 2001.
- Sarah GD, Richard J, Siegert , Taylor WJ. Interprofessional rehabilitation: a person-centred approach. Chichester: Wiley-Blackwell; 2012.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357.
- Scottish Government. Scottish Health Survey 2012 Main Report. 2013.
- Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Mead G, Lynch J, Greig C, et al. Evaluation of fatigue scales in stroke patients. Stroke. 2007;38:2090–2095.
- Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61–65.
- Bruno A, Akinwuntan AE, Lin C, et al. Simplified Modified Rankin Scale Questionnaire. Stroke. 2011;42:2276–2279.
- Gale N, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
- Bengtsson M. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14.
- Krefting L. Rigor in qualitative research: the assessment of trustworthiness. Am J Occup Ther. 1991;45:214–222.
- Egerton T, Hokstad A, Askim T, et al. Prevalence of fatigue in patients 3 months after stroke and association with early motor activity: a prospective study comparing stroke patients with a matched general population cohort. BMC Neurol. 2015;15:181.
- Chastin SF, Fitzpatrick N, Andrews M, et al. Determinants of sedentary behavior, motivation, barriers and strategies to reduce sitting time in older women: a qualitative investigation. Int J Environ Res Public Health. 2014;11:773–791.
- Giné-Garriga M, Sandlund M, Dall PM, et al. A Novel Approach to Reduce Sedentary Behaviour in Care Home Residents: The GET READY Study Utilising Service-Learning and Co-Creation. IJERPH. 2019;16:418.
- Billinger SA, Coughenour E, Mackay-Lyons MJ, et al. Reduced cardiorespiratory fitness after stroke: biological consequences and exercise-induced adaptations. Stroke Res Treat. 2012;2012:959120.
- Wennberg P, Boraxbekk CJ, Wheeler M, et al. Acute effects of breaking up prolonged sitting on fatigue and cognition: a pilot study. BMJ Open. 2016;6:e009630.
- Palmer VJ, Gray CM, Fitzsimons CF, et al. What do older people do when sitting and why? Implications for decreasing sedentary behavior. Gerontologist. 2019;59:686–697.
- Balboa-Castillo T, León-Muñoz LM, Graciani A, et al. Longitudinal association of physical activity and sedentary behavior during leisure time with health-related quality of life in community-dwelling older adults. Health Qual Life Outcomes. 2011;9:47.
- Park S, Veldhuijzen van Zanten J, Thøgersen-Ntoumani C, et al. The role of physical activity and sedentary behavior in predicting daily pain and fatigue in older adults: a diary study. Ann Behav Med. 2018;52:19–28.
- Zhaoyang R, Martire LM. Daily sedentary behavior predicts pain and affect in knee arthritis. Ann Behav Med. 2019;53:642–651.
- Macera CA, Cavanaugh A, Bellettiere J. State of the art review: physical activity and older adults. Am J Lifestyle Med. 2017;11:42–57.
- Hinkle JL, Becker KJ, Kim JS, et al.; American Heart Association Council on Cardiovascular and Stroke Nursing and Stroke Council. Poststroke fatigue: emerging evidence and approaches to management: a scientific statement for healthcare professionals from the American Heart Association. Stroke. 2017;48:e159–e170.
- Graber M, Garnier L, Duloquin G, et al. Association between fatigue and cognitive impairment at 6 months in patients with ischemic stroke treated with acute revascularization therapy. Front Neurol. 2019;10:931.
- Moran GM, Fletcher B, Calvert M, et al. A systematic review investigating fatigue, psychological and cognitive impairment following TIA and minor stroke: protocol paper. Syst Rev. 2013;2:72.
- Snaphaan L, van der Werf S, de Leeuw FE. Time course and risk factors of post-stroke fatigue: a prospective cohort study. Eur J Neurol. 2011;18:611–617.
- Stephenson A, McDonough SM, Murphy MH, et al. Using computer, mobile and wearable technology enhanced interventions to reduce sedentary behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14:105.
- Matei R, Thuné-Boyle I, Hamer M, et al. Acceptability of a theory-based sedentary behaviour reduction intervention for older adults (‘On Your Feet to Earn Your Seat’). BMC Public Health. 2015;15:606.
- Greenwood-Hickman MA, Renz A, Rosenberg DE. Motivators and barriers to reducing sedentary behavior among overweight and obese older adults. Gerontologist. 2016;56:660–668.
- Staub F, Bogousslavsky J. Post-stroke depression or fatigue? Eur Neurol. 2001;45:3–5.
- Daly RM, Ahlborg HG, Ringsberg K, et al. Association between changes in habitual physical activity and changes in bone density, muscle strength, and functional performance in elderly men and women. J Am Geriatr Soc. 2008;56:2252–2260.
- Thibaud M, Bloch F, Tournoux-Facon C, et al. Impact of physical activity and sedentary behaviour on fall risks in older people: a systematic review and meta-analysis of observational studies. Eur Rev Aging Phys Act. 2012;9:5–15.
- Leask CF, Harvey JA, Skelton DA, et al. Exploring the context of sedentary behaviour in older adults (what, where, why, when and with whom). Eur Rev Aging Phys Act. 2015;12:4.