Abstract
Background
Treatment of temporomandibular disorder (TMD) currently consists of a combination of noninvasive therapies and may be supported by e-Health. It is, however, unclear if physical therapists and patients are positive towards the use of e-Health.
Purpose
To assess the needs, facilitators and barriers of the use of an e-Health application from the perspective of both orofacial physical therapists and patients with TMD.
Methods
A descriptive qualitative study was performed. Eleven physical therapists and nine patients with TMD were interviewed using a topic guide. Thematic analysis was applied, and findings were ordered according to four themes: acceptance of e-Health, expected utility, usability and convenience.
Results
Physical therapists identified the need for e-Health as a supporting application to send questionnaires, animated exercises and evaluation tools. Key facilitators for both physical therapists and patients for implementing e-Health included the increase in self-efficacy, support of data collection and personalization of the application. Key barriers are the increase of screen time, the loss of personal contact, not up-to-date information and poor design of the application.
Conclusions
Physical therapists and patients with TMD are positive towards the use of e-Health, in a blended form with the usual rehabilitation care process for TMD complaints.
The rehabilitation process of temporomandibular complaints may be supported by the use of e-Health applications.
Physical therapists and patients with temporomandibular disorders are positive towards the use of e-Health as an addition to the usual care.
Especially during the treatment process, there is a need for clear animated videos and reminders for the patients.
Implications for rehabilitation
Introduction
Up to 15% of the adult population reports pain in the temporomandibular region [Citation1,Citation2]. The cause of TMD is a combination of musculoskeletal and biopsychosocial factors [Citation3–5]. Known risk factors for TMD pain are parafunctional habits, trauma, emotional distress, joint laxity, comorbidity of rheumatic and musculoskeletal disorders, and a poor general health and unhealthy lifestyle [Citation6,Citation7]. TMD can have an extensive impact on quality of life and can lead to work impairment [Citation7,Citation8].
Currently, TMD treatment consists of a combination of noninvasive therapies including physical therapy and splint therapy [Citation2,Citation9]. The American Association for Dental Research (AADR) recommends additional home-based care programs to TMD treatment to educate patients about their illness and how to manage their complaints [Citation10]. Such home-based programs can be delivered through e-Health, which may facilitate the diagnostic process, intervention and follow-up evaluations [Citation11]. E-Health can be described as the application of information and communication technologies across the wide range of activities that are performed in healthcare [Citation11]. Other common terms for e-Health are “telehealth,” “telemedicine” or “mobile health” [Citation12]. E-Health can be used as a way to monitor health, communication between patient and healthcare provider and collection of health data [Citation13]. E-Health interventions can substitute or complement traditional face-to-face healthcare delivery [Citation14]. Hence, the potential of e-Health for TMD management is considerable. However, a major issue in e-Health is adherence; just half of the patients fully adhere to e-Health (i.e., observed usage of e-Health compared to the intended usage) [Citation15], which reduces treatment effectiveness. The design of e-Health applications is important for better adherence [Citation15,Citation16]. Furthermore, a lack of acceptance of e-Health by healthcare providers such as physical therapists is a barrier in the implementation of e-Health [Citation17]. For new e-Health initiatives to be successful, it is important to investigate the opportunities and challenges in TMD management.
TMD management is often multidisciplinary, in which a specialized physical therapist plays an important role next to a specialized physician or dentist who determines the medical diagnosis [Citation18]. In the field of oral and maxillofacial surgery, e-Health has already been welcomed to decrease waiting time to see specialists and to provide information and education before and after surgery [Citation19]. From this field, promising results are presented with regard to patients receiving the correct treatment and cost reduction [Citation19,Citation20]. However, it is unknown whether this type of e-Health is effective for patients with TMD who are seen by orofacial physical therapists (OPTs). Additionally, it is unknown whether OPTs would even recommend e-Health to this population.
Therefore, the aim of this study was to assess the needs, facilitators and barriers of an e-Health application included in the healthcare process of patients with TMD, from the perspective of both OPTs and patients with TMD.
Methods
This study has been performed and written according to the Standards for Reporting Qualitative Research (SRQR) [Citation21]. The funders played no role in the design, conduct, or reporting of this study.
Qualitative approach and research paradigm
A descriptive qualitative study design was applied, using open interviews to obtain an in-depth understanding of the perception on the needs, facilitators and barriers with regard to e-Health in the healthcare process of patients with TMD [Citation22].
Participants and sampling
OPTs were recruited through the registry of the Dutch Society for Orofacial Physical Therapy (NVOF) and individually interviewed in their clinical practice. Interviews were administered between March 2016 and May 2016. Inclusion criteria were: 1) having over three years of working experience as an OPT with minimal a MSc graduation and 2) seeing at least eight patients with TMD per week.
The participating OPTs recruited patients with TMD for the study. When there was no referral from a doctor or dentist, the OPTs screened for the presence of a possible TMD based on the history and physical examination of the patient. Pain in the masticatory system which was aggravated by function or palpation was an indication for a painful TMD, whereas clicking or locking of the joint during function was an indication for a functional TMD. The diagnoses were not confirmed by a dentist or other physician. The individual interviews with the patients were administered between December 2018 and February 2019. Inclusion criteria for patients were: 1) receiving or have received treatment for their TMD (at least three sessions) and 2) being over 18 years of age.
Participants were recruited until saturation was achieved, which was when no new information would be identified from the last two interviews and expected to occur between six and twelve interviews [Citation23,Citation24]. The study was approved by the ethics committee of the University Medical Center Utrecht (OPTs: 15-728/C; patients: 18-703/C). All participants signed informed consent form before the interview.
Interviews
Open face-to-face interviews were conducted with OPTs and patients using pre-defined topic guides (Supplementary Appendix 1). These topic guides were open to changes when interviews identified new information. All participants were asked about the current situation of TMD management and their experiences, followed by questions about possibilities of using e-Health. The needs, facilitators and barriers were identified through questions like “If e-Health was available, what would make you want to use it and why?” and “What would you need of such an e-Health application?”.
Four members of the research team (TvB, HvdM, LdP and CMS) were actively involved in collecting and processing data. The interviews with OPTs were conducted by TvB, a master’s student of clinical health sciences and a graduated physical therapist. The interviews with the patients were conducted by LdP, a master’s student of musculoskeletal physical therapy and a graduated physical therapist. Both were trained by HvdM, a PhD-student and OPT who received training on qualitative research methods. The topic guide for the OPT interviews was created by TvB and HvdM, the topic guide for the patients by LdP and HvdM (Supplementary Appendix 1), both were validated by CMS who is a senior researcher and OPT. Patients were interviewed at a location of their choice. There were no prior relationships between the researchers and participants.
Data analysis
Interviews lasted between 30 and 45 min and were recorded. The audio files were transcribed verbatim. Anonymized transcripts were imported in the computer program Atlas.ti version 8 for windows (ATLAS.ti Scientific Software Development GmbH) [Citation25].
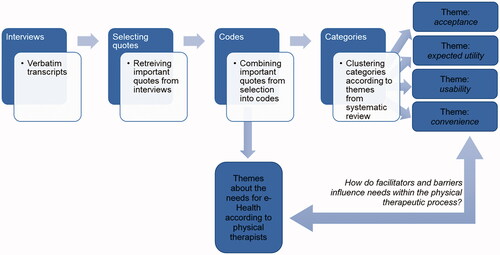
Data analysis was performed by two researchers independently (TvB and HvdM for the OPTs, LdP and HvdM for patients) and compared after the third and last interview. Data were analysed with a thematic analysis approach [Citation22]. The transcribed interviews were read closely to identify important quotes, to label codes to the data and to generate themes [Citation22]. The identified themes related to needs for e-Health were structured according to the physiotherapeutic care process: diagnostic process, treatment and evaluation. For the facilitators and barriers, categories were identified from codes, which were then structured into themes according to a recent systematic review: 1) acceptance of e-Health, 2) expected utility, 3) usability and 4) convenience [Citation26]. The flow of data analysis is depicted in . Quotes from the interviews were used to support the themes. All quotes provided in the article were translated into English by HvdM. Quotes by OPTs are marked with OPTnumber and quotes by patients are marked as Ptnumber. For every OPT it was indicated if their work experience in the field of TMD was higher than average (+ sign behind the OPTnumber) or lower than average (− sign), as described in . For every patient, the signs indicated if their age was above (+) or below (−) average as described in .
Table 1. Characteristics of the Orofacial Physical therapists (N = 11).
Table 2. Characteristics of the patient population (N = 9).
Results
Study population characteristics
A total of 11 OPTs participated in the study. The mean age of OPTs was 43.1 years and the majority was female (). Ten OPTs worked, full or in part, in a primary care setting. Mean work experience among participants was 21.6 years and mean work experience specifically for TMD was 13.2 years. For patient participants (), saturation was reached after 9 interviews. The mean age of the patients was 48 years and the majority was female. Five patients had completed their therapy and the majority (78%) went to the OPT because of TMD pain.
Needs and opportunities of e-Health in the current TMD-treatment
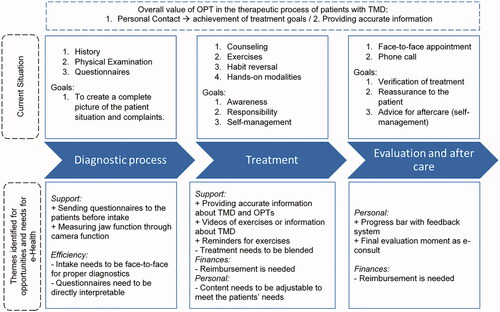
OPTs were asked to describe the current situation of care for TMD patients and what they believe the value of an OPT is in this care process (). The themes support, efficiency, personal aspects and finances () described the needs for e-Health and are ordered in each step of the care process.
Diagnostic process
The diagnostic process is seen as important to understand which factors play a role in origination and preservation of complaints and which factors can be influenced by the OPT. During the diagnostic process, in-depth conversations with the patient are perceived as the basis for formulation of patient-tailored goals. “A patient tells you their diagnosis” (OPT09 −). To support the care process, questionnaires could be sent before the intake assessment, though for efficiency it is important these questionnaires are directly interpretable.
TMD-treatment
The treatment process is based on the diagnosis, complaints and patient preferences (personal aspects). Counseling is therefore perceived as a crucial aspect of treatment and is applied throughout the entire treatment process. Additionally, exercises, habit reversal and hands-on therapies are applied. All therapies aim at creating awareness of the patient, increase self-efficacy and responsibility of the patient in their own recovery and apply self-management strategies. Vis a vis counseling is seen as essential: “But I do think that if you do not explain things, you do miss a part of the treatment” (OPT02 −). E-Health could support the treatment process through extra information, exercise videos and reminders for exercise but not displace personal contact.
Evaluation
It was emphasized that evaluations are important within the therapeutic process to see how patients do, if they understood the exercises and information that they were given and to reassure them. If the patient is doing well, the final evaluation is often done by phone. “Well, what I often do with regard to home exercises is to verify that another time to see if it is all going well and eventually, I do see evaluations as treatment as well” (OPT05 −). There is an opportunity for e-Health to support this feature, but this would need to get recognized as treatment and be reimbursed as such (finance).
Overall value of the OPT
The overall value of an OPT within the care process for patients with TMD lies in personal contact. Personal contact between OPT and patient is regarded needed to achieve treatment goals of awareness, responsibility and self-management. Using both physical touch and conversing with patients is seen as important for success. Information can be put in the right context for patients and OPTs can get more in-depth information when they see patients face-to-face. “I do think that, that is where the strength of the OPT lies, especially in the synchronization between touching and talking” (OPT06 −).
Facilitators and barriers for e-Health: Perspective of OPTs
The facilitators and barriers are described according to the structure of the interviews around these themes: 1) acceptance of e-Health: this includes participants’ opinion of and experience with e-Health in general; 2) expected utility: which summarizes the participants’ expectations of rewards and costs; 3) usability: a widespread term, including description of content of e-Health that participants find useable; and 4) convenience: which focusses on direct interaction with technology [Citation26]. The categories and themes are depicted in .
Table 3. Model of the main themes including the key facilitators and barriers according to orofacial physical therapists and patients for the use of e-Health.
Acceptance of e-Health
Identified facilitators were familiarity with e-Health and going with natural changes (i.e., technology is becoming more integrated in society including health care). Some OPTs either developed e-Health initiatives for professional use or tested and evaluated e-Health in their line of work. For example, the NVOF used to have a mobile application for patients to find OPTs throughout the Netherlands and to view videos of exercises which was recommended to their patients by some OPTs. The majority of the OPTs stood positive towards technology to support or improve current healthcare and believed that e-Health will become a part of healthcare. Some OPTs believed the rise of technology in healthcare is unavoidable. “The way you will work and the way you will give information to the patients and counsel people. Changes are coming, I am sure of that.” (OPT03 +)
A barrier for acceptance of e-Health the OPTs identified the technical skills needed for e-Health. For some the use of devices or online services is not natural yet: “But I have to automate myself more for digital things.” (OPT01 −) This was perceived as a barrier for efficiency, which was identified as in the health care process.
Expected utility of e-Health
Regarding expected utility of e-Health, the following facilitators were identified: prevention, self-efficacy, motivation, insight in treatment process and reliable information processing. e-Health could be helpful as prevention for re-occurring complaints and to decrease treatment frequency and needs. OPTs felt this may lead to an increase in self-efficacy and awareness in patients regarding the management of their complaints. “I think it [e-Health] can help in the actively involved role of the patient” (OPT09 −). The positive effects would then mostly be seen in the support of the treatment process.
The barriers identified were time investment of the OPT and losing personal contact during the TMD care process as major concern . “We, of course, never want to lose the essence of our business, and I think that, that is that you also have physical contact” (OPT09 −).
Usability
Key facilitators regarding usability were compatibility with TMD treatment, reminder functionality, information distribution and moment of use. OPTs mentioned that e-Health is suitable for treatment of TMD. Push notifications and reminders were seen as possibly useful. “When you can, for example, send a signal to your phone to sometimes get a stimulant of ‘oh, what am I doing?' ” (OPT11 +). A timeline or chart to see the progress and goals of the patients was seen as beneficial. Additionally, OPTs were open to a communication source with patients and preferred short messages or a video-chat.
The main barrier reported for usability was regarding the educational content. If the content of an e-Health application was not up-to-date, this could lead to misinformation of the patients.
Convenience
Facilitators for OPTs in using the e-Health application were the availability of an application or website, having a clear menu, having animated exercises and for e-Health to be adjustable and personalized to the patient. Currently most OPTs provide exercises on paper and they see great opportunities in animated videos of exercises, as long as they are of high quality. “At that way [videos] it is just to create an even better picture of the exercises” (OPT02 −). Poor design of the application or having to pay a disproportionate amount of money for the application, were identified barriers. “I think well-working websites is a must, actually. […] It is hard to get to and if you want to show your patient something, it is never easy. So that is why I have so much of my own information and things, but I would think it would be great [if the website was better designed].” (OPT06 −).
Facilitators and barriers for e-Health: Perspective of patients with TMD
The same themes were used as for the OPTs to cluster the facilitators and barriers for patients (). The needs identified by the patients were affiliated to the themes of the perspective on e-Health.
Acceptance of e-Health
The key facilitator for patients to accept e-Health was being familiar with e-Health already. Some patients already use simple apps for their health like a pedometer-app.
Key barriers were the lack of technical skills of the patient and screen time. Some patients did not think highly of their technical skills. “I am not really the one to look things up online.” (Pt01 +). Most of them were positive: “I think it [e-Health] could work, especially with the jaw, because most work is done when you are not with your physical therapist” (Pt04 −).
Expected utility
Prevention, self-efficacy, motivation, insight in the process and reliable information processing were mentioned as facilitators. Patients were positive towards the use of e-Health as they felt it could be helpful to prevent re-occurring complaints and decrease treatment frequency and needs. “I think it [e-Health] can be very cost-effective for health care, especially for jaw complaints. You can see your OPT less often because you already have your tools with you. I think it’s a very good idea” (Pt04 −). E-Health could provide motivational support, give insight in the progress of the patient, and provide reliable information to the OPT about complaints patients may have. Moreover, information about OPTs can also be provided. Barriers identified by the patients were time investment of the OPT, changes in treatment, losing personal contact and fixation on complaints. Patients were concerned about the loss of personal contact between the OPT and patient. “I like the contact, not just exercises but also the chats, just how you are and give feedback” (Pt08 +). Additionally, patients were concerned that including e-Health would change their treatment and might create too much fixation on the complaints. “[…] then you are just too preoccupied with it.” (Pt09 −).
Usability
The identified facilitators were the compatibility with the TMD treatment, reminder function, information distribution, moment of use and following progress. Patients believed that e-Health is suitable for treatment since exercises for TMD are suitable to their daily routine and can be done anywhere. “You can grab your phone anywhere, in an instant, if you’re somewhere in the waiting room and you think, how was it again, then you can just grab it! You can always do those jaw exercises on the bus or train, because almost no one ever notices” (Pt02 +). An often-mentioned feature of an e-Health application was being able to receive reminders to do exercises. Patients who had to change their parafunctional behaviour, had trouble to detect and minimize these habits, therefore there is a great need of a reminder: “And for myself, yes if I notice, I stop it [parafunctional behaviour] right away. But it is very hard to notice that” (Pt05 −). Besides reminders, another facilitator would be a timeline or chart to see the progress and goals of the patients. A chat function was mentioned, but the patients concluded a “Frequently Asked Question” section may be sufficient.
Patients identified the following usability barriers: exercise difficulty, separate treatments, and the need for information. When exercises would be deemed too easy and therefore not require support by an app or video, or exercises can be found online (for example on YouTube), patients did not see additional value in an e-Health application. Some also stated that they did not need extra information, as they receive all information they need from their OPT.
Convenience/accessibility
Facilitators for patients were the availability of the application or website, having a clear menu, having animated exercises and for the app to be adjustable and personalized to the patient. According to patients, an application should be part of treatment and needs guiding, like blended care. For example, feedback of the therapist is needed to control implementation of the exercises. Animated exercises in an application would help. “If you have an app for people who have received treatment then it might be convenient if they have their personalized exercises on it.” (Pt02 +)
Barriers were costs, advertising, social media, poor design or technology and making a complex profile. If an e-Health application would include advertising, having to create a complex profile or attaching it to a social media platform, this would be a barrier for patients to use the application. A poor design of the application or having to pay a disproportionate amount of money for the application, would prevent patients from using the e-Health application as well. “[…] because I already pay for the physio actually. Then work is taken away again through the app, then I do not think I have to pay for it. Yes, they are just service tasks, they have to organize something else for that. No, I would not pay for that.” (Pt06 +)
Discussion
The key findings of this study are that e-Health would be accepted by OPTs and TMD patients when it is used in a blended form to complement the usual TMD-treatment. The need for blended care is because the greatest value of an OPT was identified to be the personal contact between OPTs and patients. The personal contact helped the patients achieve their goals and receive the right information about their complaints. This personal contact was important throughout the entire care process, from history, diagnostics and treatment. Both OPTs and patients did see opportunities for e-Health within the current TMD care process for additional information, support for exercises, up-to-date information and reminders and feedback to realize behavioural change.
Common facilitators for people to use e-Health are clarity of information, speed of the system, compatibility with one’s existing routine, presence of reminders and receiving feedback [Citation26,Citation27]. This was comparable in the current study, where the OPTs were most focused on the clarity of information and the patients on the system and how to use it. TMD-treatment goals consist of increasing self-management and self-efficacy [Citation2], and both OPTs and patients believe e-Health can facilitate this process. This was also found in patients with chronic obstructive pulmonary disease, where an e-Health application for the management of exacerbations was studied [Citation28]. This supports the needs identified in the current study, where OPTs stated that e-Health could help with the support and efficiency of the diagnostic process as well as treatment process, when the application was person-centred and made use of the identified facilitators.
Poor design or technology of an e-Health application was not only mentioned as a barrier in the current study, but was also one of the main barriers found in a systematic review [Citation26]. Additionally, financial costs were a common barrier throughout several populations [Citation26], including the one from the current study. OPTs wanted to receive financial reimbursement (which was also identified as a need), but patients were not willing to pay for the use of an application. At this moment not all health insurance companies reimburse the use of e-Health, but this could facilitate the implementation of e-Health. The lack of personal contact was the main barrier for OPTs as well as the TMD patients. In the current study, personal contact was considered the biggest value of an OPT in the care process of TMD patients. The option of blended e-Health was perceived as the optimal solution, where e-Health can support certain factors of the TMD-care process. Blended care was also identified as an optimal solution for patients with osteoarthritis, which was just as effective as usual physical therapy [Citation29,Citation30]. In patients with headache, there are tools available for screening and monitoring complaints, which could also be used for blended care [Citation31]. None of the above mentioned studies describe the need for personal contact and how the lack of that may influence the commitment and effectiveness of an e-Health application. Therefore, this needs to be studied in patients with TMD specifically.
Strengths and limitations
A major strength in the current study is having the perspective of both OPTs and patients, which helps to paint the full picture of when an e-Health application would or would not be used in the TMD care process.
There are some limitations of the current study that need to be considered. Firstly, as saturation was reached after 9 interviews in patients and 11 interviews in OPTs, this may suggest that the interviews did not go in-depth enough in the perspectives of the OPTs and patients. However, sample sizes of this size are common in qualitative research [Citation24,Citation28] and the findings of the current study were comparable to findings of a large systematic review [Citation26]. A second limitation is the fact that the OPTs recruited patients to participate in the study, which may have introduced selection bias. Another limitation could be that the interviews were executed by different people, which may have led to some differences in the way of interviewing. By using a pre-set topic guide (Supplementary Appendix 1), the main topics were covered and the analysis phase confirmed this. Lastly, due to the qualitative research design there are no objectively verifiable results available that can be generalised [Citation32]. Even though quantifying the perspective on something that has not happened yet cannot easily be done, when addressing the experience of an e-Health application in use quantitative data should be collected to increase transparency and external validity.
We concluded that an e-Health application would have added value if barriers and facilitators are taken into account. As there already are e-Health initiatives available, these can be used as starting point to suit the needs of the TMD care process, for instance by adding videos of specific TMD exercises [Citation33]. At least one study described the use of telemedicine for TMD patients. This system shortened waiting time supported diagnostics [Citation20], however, this system did not have all needed elements as the participants from the current study have described in order to use the e-Health application. Therefore, future research needs to focus on developing an e-Health application for TMD patients that fulfils all facilitating criteria for optimal use. When such an e-Health application is available, the effectiveness should be studied while taking patient satisfaction into consideration. Additionally, as TMD management is preferred to be multidisciplinary [Citation18], future studies should consider the perspective of the specialized dentist or physician towards e-Health in this population as well. Perhaps an integrated e-Health application to not only improve communication with the patient, but also interdisciplinary communication could be benefit [Citation34,Citation35].
Another factor to consider before implementing e-Health in the physical therapeutic TMD care, is the experience of the physical therapist. In the current study, patients have had minimally three sessions of physical therapy and all included therapists are well trained in the field of orofacial complaints including TMD [Citation36]. It is uncertain, however, if the perspectives found in the current study are similar to patients who have not received minimally three sessions, or to physical therapists with a lesser extent of training. Therefore, this design should be replicated in other countries to ensure the validity of the findings.
In conclusion, OPTs and TMD patients are positive towards the use of blended e-Health in the health care process of the TMD complaints, complementary to the usual care. An e-Health application should be easy to use, accessible and contain information about the TMD complaints and animated exercises. Because there is a strong need for personal contact for both OPTs and patients, e-Health should be part of a blended care system rather than replacing physical therapy.
Appendix_1.docx
Download MS Word (12.9 KB)Acknowledgements
The authors thank all the Orofacial Physical Therapists and patients who participated in this study. The authors also thank the Dutch Society for Orofacial Therapy (NVOF) for assistance during the recruitment process.
Disclosure statement
There is no conflict of interest within this study.
Additional information
Funding
References
- LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997;8:291–305.
- List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. 2017;37:692–704.
- Michalsen A, Grossman P, Acil A, et al. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2005;11:CR555–C561.
- de Leeuw R, Klasser GD. American Academy of Orofacial Pain guidelines for assessment, diagnosis, and management. 5th ed. Chicago (IL): Quintessence Publishing; 2013.
- Speciali JG, Dach F. Temporomandibular dysfunction and headache disorder. Headache J Head Face Pain. 2015;55:72–83.
- Durham J. Temporomandibular disorders (TMD): an overview. Oral Surg. 2008;1:60–68.
- Durham J, Newton-John TRO, Zakrzewska JM. Temporomandibular disorders. BMJ. 2015;350:h1154.
- Almoznino G, Zini A, Zakuto A, et al. Oral health-related quality of life in patients with temporomandibular disorders. J Oral Facial Pain Headache. 2015;29:231–241.
- Wieckiewicz M, Boening K, Wiland P, et al. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J Headache Pain. 2015;16:106.
- Greene CS. Managing the care of patients with temporomandibular disorders: a new guideline for care. J Am Dent Assoc. 2010;141:1086–1088.
- Vukovic V, Favaretti C, Ricciardi W, et al. Health technology assessment evidence on e-Health/m-Health technologies: evaluating the transparency and thoroughness. Int J Technol Assess Health Care. 2018;34:87–96.
- Fatehi F, Wootton R. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J Telemed Telecare. 2012;18:460–464.
- Shaw T, McGregor D, Brunner M, et al. What is eHealth (6)? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19:e324.
- Elbert NJ, van Os-Medendorp H, van Renselaar W, et al. Effectiveness and cost-effectiveness of ehealth interventions in somatic diseases: a systematic review of systematic reviews and meta-analyses. J Med Internet Res. 2014;16:e110.
- Kelders SM, Kok RN, Ossebaard HC, et al. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14:e152.
- Donkin L, Christensen H, Naismith SL, et al. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;13:e52.
- Brewster L, Mountain G, Wessels B, et al. Factors affecting front line staff acceptance of telehealth technologies: a mixed-method systematic review. J Adv Nurs. 2014;70:21–33.
- Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, et al. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. 2018;11:571–587.
- van den Bosch SC, van de Voort NEM, Xi T, et al. Oral & Maxillofacial surgery is ready for patient-centred eHealth interventions - the outcomes of a scoping review. Int J Oral Maxillofac Surg. 2019;48:830–840.
- Salazar-Fernandez CI, Herce J, Garcia-Palma A, et al. Telemedicine as an effective tool for the management of temporomandibular joint disorders. J Oral Maxillofac Surg. 2012;70:295–301.
- O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89:1245–1251.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
- Creswell JW. Qualitative inquiry and research design. 2nd ed. Thousand Oaks (CA): SAGE Publications; 2007.
- Guest G, Bunce A, Johnson L. How many interviews are enough? Field Methods. 2006;18:59–82.
- ATLAS.ti: the qualitative data analysis and research software. Available from: https://atlasti.com/
- Simblett S, Matcham F, Siddi S, et al.; RADAR-CNS Consortium. Barriers to and facilitators of engagement with mHealth technology for remote measurement and management of depression: qualitative analysis. JMIR Mhealth Uhealth. 2019;7:e11325.
- Simblett S, Greer B, Matcham F, et al. Barriers to and facilitators of engagement with remote measurement technology for managing health: systematic review and content analysis of findings. J Med Internet Res. 2018;20:e10480.
- Korpershoek YJG, Vervoort S, Trappenburg JCA, et al. Perceptions of patients with chronic obstructive pulmonary disease and their health care providers towards using mHealth for self-management of exacerbations: a qualitative study. BMC Health Serv Res. 2018;18:757.
- Bossen D, Kloek C, Snippe HW, et al. A blended intervention for patients with knee and hip osteoarthritis in the physical therapy practice: development and a pilot study. JMIR Res Protoc. 2016;5:e32.
- Kloek CJJ, Bossen D, Spreeuwenberg PM, et al. Effectiveness of a blended physical therapist intervention in people with hip osteoarthritis, knee osteoarthritis, or both: a cluster-randomized controlled trial. Phys Ther. 2018;98:560–570.
- Mosadeghi-Nik M, Askari MS, Fatehi F. Mobile health (mHealth) for headache disorders: a review of the evidence base. J Telemed Telecare. 2016;22:472–477.
- Choy LT. The strengths and weaknesses of research methodology: comparison and complimentary between qualitative and quantitative approaches. IOSRJHSS. 2014;19:99–104.
- Lindfors E, Arima T, Baad-Hansen L, et al. Jaw Exercises in the Treatment of Temporomandibular Disorders-An International Modified Delphi study. J Oral Facial Pain Headache. 2019;39:389–398.
- Janssen A, Brunner M, Keep M, et al. Interdisciplinary eHealth practice in cancer care: a review of the literature. IJERPH. 2017;14:1289.
- Hines M, Brunner M, Poon S, et al. Tribes and tribulations: interdisciplinary eHealth in providing services for people with a traumatic brain injury (TBI). BMC Health Serv Res. 2017;17:757.
- Dekker-Bakker L, van Maanen C, Wilbrink W, et al. Beroepscompetentieprofiel orofaciale fysiotherapie. NVOF; 2008.