Abstract
Purpose
To explore multi-professional teamwork in relation to the physical environment in three newly built or renovated stroke units.
Materials and methods
An observational study was undertaken. The participants were all staff members of a multi-professional team working in the reviewed stroke units. The data were collected using behavioural mapping and semi-structured observations, and they were analysed by content analysis and descriptive statistics.
Results
Out of all the observations in the behavioural mapping, very few were of two or more members from the team together with a patient. None of the included stroke units had a co-location for all the members of the multi-professional team. Three main categories emerged from the analysis of the interviews: (i) the hub of the unit; (ii) the division of places; and (iii) power imbalance. All the categories reflected the teamwork in relation to parts of the physical environment.
Conclusion
The design of the physical environment is important for multi-professional teamwork. Emphasis must be placed on better understanding the impact of the physical environment and on incorporating the evidence related to multi-professional teamwork during the design of stroke units.
Understanding the link between the physical environment and effective teamwork can lead to more tailored and supportive design solutions.
The design of the physical environment should be considered as a vital part of effective teamwork in stroke units.
The physical environment should include shared workstations, allowing team members to meet and communicate face to face.
IMPLICATIONS FOR REHABILITATION
Introduction
Fifteen million people experience a stroke around the world each year, and strokes are the second leading cause of disability [Citation1]. According to the current evidence and international guidelines, care in a stroke unit should be the first choice for people who are experiencing the acute phase of a stroke. Care at stroke units reduces the risk of complications, disability and death [Citation2]. A stroke unit is defined as an identifiable geographic area in hospitals that is devoted to people who have a stroke, and it is staffed by a multi-professional team with specialist knowledge of stroke care [Citation3]. Multi-professional teamwork means that professionals from different disciplines benefit from each other’s skills and work towards common patient goals [Citation4]. Teamwork has been shown to improve satisfaction with care [Citation5] and the quality of care for persons with complex needs, such as the period after a stroke [Citation6]. Regarding stroke care, several studies have described the benefits of multi-professional teams as a factor that contributes to the beneficial effects of care in a stroke unit, e.g. a reduced risk of complications and disability [Citation3,Citation6,Citation7]. On an ideal stroke team, there is coordination and effective collaboration between various professions, such as nurses, physicians, physiotherapists, and occupational therapists. The team should perform activities towards common goals and respect the shared responsibility of group efforts [Citation8,Citation9]. Teamwork was defined by Gharaveis, Hamilton and Patis [Citation4, p.120], “as a behavioural process, wherein team members collectively accomplish specified goals efficiently and effectively in the context of one or more patient care objectives”. This way of working requires regular team meetings as well as assessments of the patient’s health status to create a coordinated care plan [Citation3,Citation10]. Given this background, it is understood that the multi-professional team is of significant importance for a high standard in healthcare. However, teamwork in stroke care is complex, demanding and highly varied in format, leadership style and team climate [Citation11].
Earlier studies showed an association between the well-being of patients and staff at healthcare facilities and the design of the physical environment [Citation12–15]. In stroke units, the physical environment has been described as essential for patient activities and care [Citation16–18]. Changes in the physical environment have been found to influence patient activity and social interactions [Citation16]. In a recent study, patients were found to have higher levels of activity in a stroke unit that had a combination of single and multi-bed room designs compared to a stroke unit with only a single-room design [Citation18]. However, the interplay between the physical environment of stroke units and multi-professional teamwork has rarely been investigated.
Generally, efforts to make the environment supportive of patient needs must also consider the needs of the staff. For instance, the physical environment could include spaces designed to allow team members to work together, face to face, and to accommodate supplies nearby, such as rooms for medical products and storage facilities [Citation4]. Ulrich et al. [Citation13] found that the physical environment can contribute to staff stress, fatigue and ineffectiveness in delivering care, which may influence patient safety, health outcomes, and the overall quality of the healthcare. Recently, a systematic review [Citation4] of the impact of a well-functioning physical environment on teamwork and communication demonstrated that both layout and spatial arrangement influenced all aspects of communication in healthcare facilities.
To create a physical environment that supports positive health outcomes for patients and staff, decisions on design alternatives in the environment should be based on research. Evidence-based design has become the theoretical framework on which to base decisions about design to set up a physical environment that has positive health outcomes for patients and staff [Citation19]. In an evidence-based design process, decisions about the design should be based on current evidence and experiences from existing healthcare environments [Citation20]. This approach includes research about the needs of those working in the stroke units [Citation19] and how the physical environment could be a facilitator or a barrier to the multi-professional team’s ability to provide high quality care and rehabilitation.
For effective and safe stroke care, the physical environment in modern stroke units should facilitate evidence-based care in which the multi-professional team has a central role. There is sparse knowledge as to how the physical environment impacts multi-professional teamwork in stroke units, although environmental factors are generally outlined as being important in terms of how staff can work within healthcare facilities.
Aim and research questions
The overall purpose of this study was to explore multi-professional teamwork and the physical environment in three newly built stroke units. This purpose was addressed using the following questions as a guide:
To what extent are the team members working together during the day?
In what location are the team members working together to care for the patients in the stroke unit?
How does the physical environment impact the multi-professional teamwork?
Materials and method
Design
The current work is part of a larger study in which different factors in the physical environment important for patients and staff in stroke units have been explored. For this study, an observational design was used to observe the multi-professional teamwork and the physical environment in stroke units. A combination of both qualitative and quantitative methods was used in the data collection and analysis according to the basic principles from the Creswell and Plano Clark [Citation21] model of a convergent parallel mixed design. This method refers to the different independent strands employed during data collection and analysis, followed by relational comparisons of the results during the overall interpretation and discussion.
Study sites – the physical environment
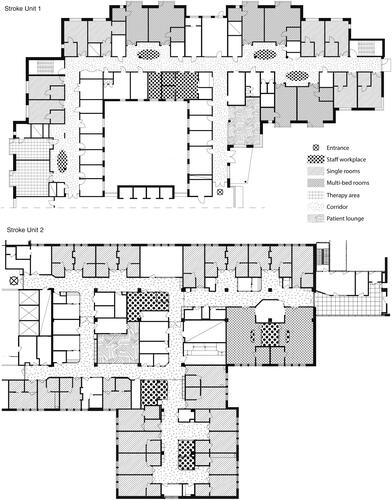
This study was conducted at one regional and two university hospitals in Sweden. One stroke unit was newly constructed [SU1] and two units were recently renovated with a new design [SU2 and SU3]. Their physical environment characteristics () and design () somewhat differed. All the units had a combination of acute care and rehabilitation, and were built after the ratification of the Swedish stroke guidelines in 2009 [Citation22], which are consistent with European stroke guidelines [Citation3].
Figure 1. Schematic of the included stroke units.
Table 1. Characteristics of the physical environment.
Participants
In this study, the definition of the multi-professional team was based on the European stroke guidelines [Citation3], i.e. a multi-professional stroke team consists of different healthcare professionals with special competence in stroke care. For this study, all the staff members of the multi-professional team in the included stroke units were eligible for inclusion. The participants were nurses, nurse assistants, occupational therapists, physicians, physiotherapists, and speech therapists. The team could work both as a team with two or more professionals together and as individuals during meetings with the patients. All patients included in the behavioural mapping were able to give informed consent, answer questions and to perform some activities (e.g. stand, walk, eat, sit in the bed or sit out of bed).
Data collection
Data were collected through behavioural mapping [Citation23] and semi-structured observations from April 2013 to December 2015. The behavioural mapping and the semi-structured observations were performed at the same week at the included stroke units, but not at the same time. To provide a rich description of the physical environment (), examples from the included stroke units based on the semi-structured observation and examples from the planning and design documents were collected by the first author.
[i] Behavioural mapping. While the patient’s activities and interactions were systematically observed and recorded using behavioural mapping [published elsewhere], the identity of the people in the multi-professional team, that were present during the observation were recorded, in addition to their location. The first and last author and two research assistants, trained and guided by a detailed manual in behavioural mapping procedures, performed all observations. For the behavioural mapping, each patient was observed over one weekday from 8 a.m. to 5 p.m. Observations were recorded every 10 min on a previously defined route in the stroke unit, which remained consistent throughout the day. At each observation point, categories of physical activity [e.g. sitting, walking], the people present [e.g. physicians, nurses, family], and the location of the activity [e.g. bathroom, patient’s room, corridor] were recorded. When observing the people present, it was possible to note more than one member of the multi-professional team.
[ii] Semi-structured observation. A semi-structured observation guide inspired by Spradley [Citation24] was applied. The first and last author performed all the semi-structured observations. The guide included the location where the observation was performed, the design of the location, the description of the activity, who was involved, and the utilities and structure of the room. To capture the daily work of the multi-professional teams and their collaboration in the included units, a wide range of regular team-based activities were chosen for observations: stroke team meetings, daily activities at different workstations, and rounds and care planning meetings. The focus of the observations was on the ways in which the physical environment was a facilitator of or a barrier to the multi-professional team performing their activities. The duration of the observations ranged from 0.5 to 1.5 h. The first and last authors and a research assistant performed the observations. During the observations, field notes were taken. The field notes were both a description and a reflection of the facilitators and barriers in the physical environment, and the aim was to make them as complete and detailed as possible [Citation25,Citation26].
Data analysis
To address the question (a) to what extent are the team members working together during the day, we examined behavioural mapping data and counted the number of observations when more than one team member was present together with the patient. Further, to address the question of the location of teamwork (b), we also counted each episode and summary statistics are presented. Quantitative data in the form of behavioural mapping were analysed using descriptive statistics in Microsoft Excel 2016, and they are reported as the number of observations.
To address the question (c) how the physical environment impacts the multi-professional teamwork, content analysis [Citation27,Citation28] was used to analyse the field notes from the semi-structured observations. In the analysis, the authors read through the field notes several times to obtain an overall impression and then started to select units of meaning for analysis. The next step in the analysis was an initial coding, followed by the identification of subcategories. The guiding research question for the coding was How does the physical environment impact the multi-professional team activities? The subcategories were then scrutinised by the members of the research team to identify similarities and differences, which were then organised into overarching categories (). These categories were further improved, resulting in the final three main categories. Discussions were held within the research group to reach a consensus.
Table 2. Examples of units of meaning, codes, sub-categories and categories.
Ethical consideration
A Regional Ethical Review Board approved the study. All the participants received verbal information on the study and gave informed consent prior to each observation. The data collectors were not employed by the participating units.
Results
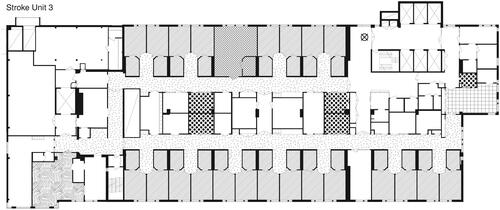
The results are presented as the numbers of observations () and as descriptions of the activities observed from the field notes (). The behavioural mapping was based on 2970 observations, and the field notes were based on 56 semi-structured observations. Three main categories appeared in the qualitative analyses: (i) the hub of the unit; (ii) division of places; and (iii) power imbalance.
Figure 2. The multi-professional team at different locations. *Team member combinations. Total number of observations, n = 2970. Physician-Nurse: a physician and at least one nurse were present. Nurses-Nurse assistants: at least one nurse and one nurse assistant were present. PT, OT and ST: at least two of the PT, OT, and ST were present. Nurse, Nurse Assistants, PT, OT and ST: a nurse or a nurse assistant plus at least one PT, OT, and ST were present. Family and Staff: a family member was observed together with at least one of the following people: doctor, nurse, nurse assistant, PT, OT, and ST. Family and PT, OT and ST: a family member was observed together with one or more of the following people: PT, OT, and ST.
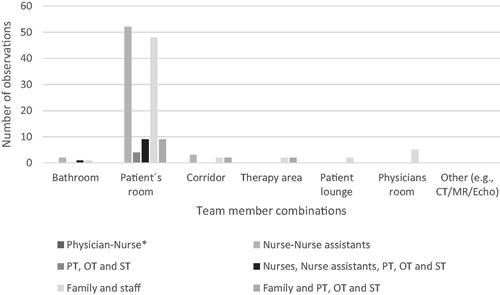
Table 3. The physical environment and teamwork outlined as sub-categories, categories and main categories.
Team members and locations of the multi-professional team in the stroke units
Observations taken when parts of the team [two or more professions] and the patient were interacting were low overall (). These meetings mostly occurred in the patients’ rooms. During the majority of the observations, the most common team constellation was a nurse and a nurse assistant collaborating in a meeting with a patient. Few other constellations were observed.
The physical environment and teamwork
Main category 1: the hub of the unit
The observations showed that centrally located workplaces were visible hubs in the middle of the corridors close to the patients’ rooms. They could differ in design, were all small and were often marked with different colours on the walls, pillars, and floors. Workplaces were either open desks where staff kept their documents or cubicles with space for 2–3 staff members. The staff members who worked at these workplaces were mostly nurses and nurse assistants. These workplaces signalled openness (i.e. staff availability) yet provided privacy. The open desks were accessible and clearly defined by different colours in the corridor. In contrast, the physically open desks made it difficult for staff to maintain confidentiality. During the observations, patients often sat or walked around the workplaces. At one unit (SU1), there was full transparency into the workstation, in which all the documents on the tables and on the computer screens were visible to patients and relatives. The staff had to remember to log out of the computers and to avoid leaving any documents at the desk. During the observations, it was also noted that everything the staff talked about was audible in the corridor and in nearby patient rooms. Sometimes, the physicians and therapists [physiotherapists and occupational therapists] passed by to report on patient’s health status. During the observations, there were few signs of ongoing teamwork in which the professionals were meeting and discussed the care in the stroke units.
Another type of workplace was the secluded workplace, with glass walls facing the corridor and with doors that could be closed (SU2 and SU3). Sometimes these workplaces had frosted glass, sometimes not. These workplaces enabled visibility, but the staff could choose to close the door, thus providing confidentiality. To facilitate planning and patient overviews [for all the professionals in the team], there were visible patient overview notice boards on the walls. At all the observed workplaces, these notice boards were visible to unauthorised persons [patients, relatives and other temporary visitors]. These secluded workplaces were used as rooms for the daily rounds but also for larger team conferences with all the professionals in the team present. During their use for the entire team's meetings/conferences, these rooms seemed too small. It was difficult for all the team members to take part in the information exchange and the conversation. The air quickly became bad, and then the doors were opened, which in turn allowed people passing in the corridor to overhear the conversation, causing an unintended lack of confidentiality.
Main category 2: division of places
All the stroke units had a division of places, which meant that different professions had separate rooms. None of the stroke units had any places that were designed so that the entire multi-professional team could be together during their daily tasks. Instead, different workplaces were spread throughout the entire stroke units. In all the included units, a nurse station was located at one end of the corridor, and in the opposite end, there were rooms for the physiotherapists or the physicians. There were various spaces named as workplaces such as team stations, open work desks, nurse stations, physician rooms, and meeting and conference rooms. Even though a room was named a team station, it was often a workplace for nurses and nurse assistants for their documentation and administration work.
Nurses, physicians, physiotherapists and occupational therapists all had individual rooms for their professions. In these rooms, work such as documentation, other types of administration and care planning were performed. It was only during the special team meetings that the entire multi-professional team met and planned the care for the patients. In two of the included stroke units (SU1 and SU3), these team rounds were held in special seminar rooms with a table in the centre of the room. In one stroke unit (SU2), all the team meetings were held in one of the workplaces in the corridor.
Main category 3: power imbalance
The observations showed that the design of the room could create a power imbalance between members in the team and between the team and the patient. Thus, the design appeared to impact the multi-professional team and their cooperation during team meetings and patient reviews. It appeared that the design was significant when it came to how work was conducted and how power was distributed. Meetings in small rooms (SU1) were headed by the member of staff whose room it was, and it was that person who determined what would be discussed, who could talk and how long the meeting would run. Since the small rooms were not intended for meetings, there were certain interruptions, such as extra chairs having to be brought in. Furthermore, the setting appeared to prevent the participation of all team members: for example, physicians spoke with their backs towards team members while accessing medical records, which was not conducive to face-to-face discussions.
Some of the team meetings took place in specially designed conference or seminar rooms (SU1 and SU3), which allowed all members of the multi-professional team to gather around an oval or rectangular table and have face-to-face communication. In addition, rooms that were dedicated for team meetings made confidentiality possible. The seminar rooms in SU1 and SU3 were brightly coloured and had good lighting and ventilation: these seemed to be conducive to discussion. Designating a room for meetings enabled multi-professional teams to work without interruption, and the lack of visibility from the corridors was conducive to teamwork.
When parts of the multi-professional team met patients during care planning, these meetings were also held in different conference rooms/meeting rooms (SU1, SU2 and SU3), with a proper table and chairs. During the care planning meetings, the patient was acting as the chairperson. In these situations, everyone was able to have eye contact with the patient.
Discussion
This study showed that the design of the physical environment could have an impact on the multi-professional teamwork in a stroke unit. The physical environment was not always designed based on existing evidence about factors considered to facilitate teamwork, e.g. a design that facilitates face-to-face communication and appropriate spaces to allow the members to work together [Citation4]. This observations of the physical environment and the multi-professional teamwork should lead to careful consideration, since the importance of multi-professional team-based care and rehabilitation has been emphasised repeatedly in stroke guidelines [Citation3,Citation10,Citation22] and acts as unequivocal evidence of improved outcomes [Citation2,Citation3,Citation29]. Stroke teams are larger than many other healthcare teams and include a wide range of professionals, such as physicians, nurses, nurse assistants, and physio-occupational and speech therapists, so coordination and effective collaboration are important; however, this collaboration is reportedly difficult to accomplish [Citation29]. Therefore, it is important to continue careful study of what it is in the environment that can contribute to teamwork facilitation.
In the present study, despite the large number of observations, situations in which two or more members of the multi-professional team working together with the patient present were rarely observed. This result is worrying, because it is difficult to achieve a coordinated care plan for the patient if the team does not make a coherent assessment at the same time during the meeting with the patient [Citation3]. Ultimately, the involvement of patients in their own care can be jeopardised if all team members do not attend the meeting. The relationship between professionals and patients requires communication structures that encourage patients to express their expectations, goals and preferences. At every patient meeting, patients must be regarded as partners in the team and be involved in the decision-making process about their care [Citation30–32]. A recent systematic review of the benefit of single versus multi-bedroom design for persons with neurological disorders such as stroke did not find strong evidence to support or to refute single room design [Citation33]. Based on the findings of our study it may be the case that when the multi-professional team works together with the patients, the single bedroom could be the best physical environment to enhance patient participation since it allows for a high level of confidentiality.
Most commonly, a nurse and nurse assistant were observed together, and mostly in the patient’s room. This result is not surprising because nurses and nurse assistants have traditionally worked together bedside in care activities; they are also the largest professional groups and they participate in patient care 24 h a day [Citation10]. Another explanation might be an undefined meaning of what teamwork should be in the units. Other research [Citation11] has shown that teamwork can suffer if there is a lack of clarity in terms of work relationships and team interactions, especially if the physical environment is not designed for team interaction.
This study shows the importance of the physical environment when it comes to face-to-face communication. Often, team members had to sit with their backs towards one another. In some cases, the rooms were small, and their primary function seemed to be as a workplace designed for 2–3 people. In a newly published review [Citation4], visual connectivity and the size of a space, such as the presence of large rooms with space for all team members, was shown to strengthen communication between the team members.
We also found that centrally placed visible workplaces acted as the hub of the unit. These hubs were placed in the middle of the corridors and were designed for communication and for short meetings with staff from the multi-professional team. The spatial relationship of a centrally placed workstation near the patient rooms has been shown to foster strong interactions and collaborative communication within the team [Citation34]. Even if the hubs at the observed units seemed to be good places for communication, they were not appropriate for activities that required confidentiality. Open and visible workplaces can be important for facilitating communication and interactions, but it is simultaneously essential to secure confidentiality when sharing information about the patients.
The results also showed that none of the included stroke units had any space for members of the multi-professional team to meet and work together as a team in a room that could be closed with a door. We could also observe that the various professionals had their own workplaces, i.e. there was a clear division between those different workplaces that appeared not to fully, support multi-professional team activities. Earlier research [Citation9] showed that shared locations and professional proximity are necessary factors for successful teamwork, and co-location can render repeated engagement in sharing patient information and in exploring different perspectives [Citation9]. Furthermore, a physical environment that is divided into different rooms for different professions can make team communication poor and incomplete. This finding is of particular importance since good communication is fundamental for safe care [Citation35] and thus central for increasing patient safety [Citation3]. For better communication, therefore, the physical environment should be designed to support communication, i.e. meeting rooms, e.g. being equipped with supporting technology and common workplaces.
One important finding was the power imbalance in the physical environment. Sometimes, this power imbalance appeared to be emphasised by the design and placement of furniture. In these cases, the physical environment did not support team activities in which all the members of the team could participate and contribute to the care and rehabilitation of the patient. Previous studies have also indicated that the context in which a team meeting is held is important for the balance of power [Citation4,Citation11]. Tyson et al. [Citation11] suggest that the physical environment and the ambient features can promote communication and a balance of power in a room, e.g. by using large seminar rooms with a table in the centre, a large space for each team member, a whiteboard on the wall and a large screen.
However, having professionals working in the same physical environment does not automatically generate a team that will cooperate [Citation36]. One factor that impacts teamwork can be hierarchies in healthcare. In a recent study by Green et al. [Citation37], factors contributing to healthcare hierarchies included a person’s position within a team, e.g. professional speciality, sex, personality [introvert or extrovert], increased responsibility, orders within and between professions, and professionalism [Citation37]. The importance of all these factors does not reduce the need to study the physical environment as an important factor in understanding how teams can work and communicate better. Rather, the physical environment can be part of the understanding of how the organisation and the environment interact to support team activities rather than hierarchies through a well-designed environment that promotes equal conversations.
Strengths and limitations
The results of this study were built on qualitative and quantitative data, with a large number of observations during full days, which strengthens the study. The research design and data collection was valuable because it provided the opportunity to address questions about complex phenomena such as the physical environment [Citation38]. Another strength was that the observations were performed using a well-established method of behavioural mapping, and for the semi-structured observations, a predefined observation guide was used. To minimise the risk of unsought preconceptions, detailed field notes allowed us to reach a deeper understanding of the context of our observations. Field notes were valuable and prompted close observations of the environment and interactions. A limitation that should be acknowledged is that for the unstructured observations, there might have been informal meeting places for the team without the patient present that were not observed. Another limitation is that the behaviour mapping only provided a picture of who was with the patient in the patient’s room. There may have been occasions when the staff did work together – for example, outside the patient’s room, either with or without the patient present.
Conclusion
The design of the physical environment can play a significant role in multi-professional teamwork. The physical environment can support the multi-professional team by reinforcing good communication and power distribution. This design may include a shared workstation, allowing team members to meet and communicate face to face. It is time to understand and incorporate existing evidence regarding multi-professional teamwork into the design of the physical environment of stroke units. Hence, the physical environment should be incorporated into stroke guidelines as an important component of stroke care.
Acknowledgments
The Doctoral School in Health Care Sciences at Karolinska Institutet, the Swedish Research Council Formas, The Swedish Stroke Association and Dalarna University’s Health and Welfare research area financially supported this research. The authors thank Asgeir Sigurjonsson for the illustrations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet Neurol. 2016;15(9):913–924.
- SUTC. Organised inpatient [stroke unit] care for stroke. Cochrane Database Syst Rev. 2013;(9):CD000197.
- Ringelstein EB, Chamorro A, Kaste M, et al. European Stroke Organisation recommendations to establish a stroke unit and stroke center. Stroke. 2013;44(3):828–840.
- Gharaveis A, Hamilton DK, Pati D. The impact of environmental design on teamwork and communication in healthcare facilities: a systematic literature review. Herd. 2018;11(1):119–137.
- Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958.
- Teasell R, Foley N, Salter K, et al. An evidence-based review of stroke rehabilitation. Top Stroke Rehabil. 2009;16(6):463–488.
- Lindsay P, Furie KL, Davis SM, et al. World Stroke Organization global stroke services guidelines and action plan. Int J Stroke. 2014;9(Suppl A100):4–13.
- McCallin A, Ba R. Factors influencing team working and strategies to facilitate successful collborative teamwork. NZ J Physiother. 2009;37(2):62.
- Clarke DJ. Achieving teamwork in stroke units: the contribution of opportunistic dialogue. J Interprof Care. 2010;24(3):285–297.
- Socialstyrelsen. Nationella riktlinjer för vård vid stroke. Swedish national guidelines for stroke care. Stockholm: Socialstyrelsen; 2018.
- Tyson SF, Burton L, McGovern A. Multi-disciplinary team meetings in stroke rehabilitation: an observation study and conceptual framework. Clin Rehabil. 2014;28(12):1237–1247.
- Steinberg JP, Denham ME, Zimring C, et al. The role of the hospital environment in the prevention of healthcare-associated infections by contact transmission. Herd. 2013;7(1_suppl):46–73.
- Ulrich RS, Zimring C, Zhu X, et al. A review of the research literature on evidence-based healthcare design. Herd. 2008;1(3):61–125.
- Ulrich RS, Berry LL, Quan X, et al. A conceptual framework for the domain of evidence-based design. Herd. 2010;4(1):95–114.
- Tanja-Dijkstra K, Pieterse ME. The psychological effects of the physical healthcare environment on healthcare personnel. Cochrane Database Syst Rev. 2011;(1):Cd006210.
- Shannon MM, Elf M, Churilov L, et al. Can the physical environment itself influence neurological patient activity? Disabil Rehabil. 2019;41(10):1177–1113.
- Blennerhassett JM, Borschmann KN, Lipson-Smith RA, et al. Behavioral mapping of patient activity to explore the built environment during rehabilitation. Herd. 2018;11(3):109–123.
- Anåker A, von Koch L, Sjostrand C, et al. The physical environment and patients’ activities and care: a comparative case study at three newly built stroke units. J Adv Nurs. 2018;74(8):1919–1931.
- Hamilton DK, Watkins DH. Evidence-based design for multiple building types. Hoboken, New York: John Wiley & Sons; 2009.
- Stankos M, Schwarz B. Evidence-based design in healthcare: a theoretical dilemma. Interdiscip Des Res e-J. 2007;1(1):1–15.
- Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Los Angeles: SAGE; 2017.
- Socialstyrelsen. Nationela riktlinjer för vård vid stroke. 2009. Available from: http://socialstyrelsen.se/indikatorer/godvard.
- Bernhardt J, Dewey H, Thrift A, et al. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke. 2004;35(4):1005–1009.
- Spradley JP, Baker K. Participant observation. New York (NY): Holt, Rinehart and Winston New York; 1980.
- Phillippi J, Lauderdale J. A guide to field notes for qualitative research: context and conversation. Qual Health Res. 2018;28(3):381–388.
- Sanjek R. Fieldnotes: the makings of anthropology. Ithaca: Cornell University Press; 1990.
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115.
- Krippendorff K. Content analysis: an introduction to its methodology. Thousand Oaks (CA): SAGE; 2004.
- Clarke DJ, Forster A. Improving post-stroke recovery: the role of the multidisciplinary health care team. J Multidiscip Healthc. 2015;8:433–442.
- Epstein NE. Multidisciplinary in-hospital teams improve patient outcomes: a review. Surg Neurol Int. 2014;5(Suppl 7):S295–S303.
- McCormack B, McCance TV. Development of a framework for person-centred nursing. J Adv Nurs. 2006;56(5):472–479.
- McCormack B, McCormack B, McCance T. Person-centred nursing: theory and practice. Chichester (UK): John Wiley & Sons, Ltd.; 2010.
- Shannon MM, Lipson-Smith R, Elf M, et al. Bringing the single versus multi-patient room debate to vulnerable patient populations: a systematic review of the impact of room types on hospitalized older people and people with neurological disorders. Intell Buildings Int. 2018;1–19.
- Pati D, Harvey TE, Jr., Redden P, et al. An empirical examination of the impacts of decentralized nursing unit design. Herd. 2015;8(2):56–70.
- Omura M, Maguire J, Levett-Jones T, et al. The effectiveness of assertiveness communication training programs for healthcare professionals and students: a systematic review. Int J Nurs Stud. 2017;76:120–128.
- Hewitt G, Sims S, Greenwood N, et al. Interprofessional teamwork in stroke care: Is it visible or important to patients and carers? J Interprof Care. 2015;29(4):331–339.
- Green B, Oeppen RS, Smith DW, et al. Challenging hierarchy in healthcare teams - ways to flatten gradients to improve teamwork and patient care. Br J Oral Maxillofac Surg. 2017;55(5):449–453.
- Creswell JW, Clark Vl P. Designing and conducting mixed methods research. Los Angeles (CA): SAGE Publications; 2011.