Abstract
Purpose
To analyse the number of, timing of, and reasons for early termination of interdisciplinary pain rehabilitation (IPR).
Methods
A multicentre study in two Dutch rehabilitation centres with a mixed method design. Quantitative part: retrospective patient file review of all IPR patients. Qualitative part: 20 semi-structured patient interviews with early IPR terminators.
Results
One hundred and thirty-seven of 428 participants (31.3%) had terminated IPR early, of which almost 30% had a positive reason. Of a planned treatment duration of 12 weeks, the median (interquartile range (IQR)) reduction was 5.3 week (3.0; 8.0). Over 80% of the early terminators with negative reasons stopped in the first half of IPR, whereas approximately 55% of the early terminators with positive reasons stopped in the final quarter of IPR. A discrepancy between patient expectations of the aim and content and the actual IPR was mentioned as a negative reason for early termination. Many of the positive early terminators were able to self-manage.
Conclusions
Previously reported figures on early termination were confirmed. Early termination of IPR should not be considered negative per se, because a substantial proportion of early terminations have a positive reason. Negative early terminators tend to stop earlier during IPR, compared to positive terminators.
Substantial rates of patients (31%) terminate interdisciplinary pain rehabilitation (IPR) earlier than planned.
Early IPR termination should not be considered negative per se, because a substantial proportion of early terminations have a positive reason (i.e. goals achieved early).
Although patients receive extensive personalised information about aim and content of IPR before starting, early terminators with a negative reason often have different expectations about the aim and content of treatment.
Clinicians and researchers should be focused on how to explain IPR to the patient and check whether the patient has understood it well and is convinced of its credibility.
Implications for rehabilitation
Introduction
Between 9% and 42% of patients terminate interdisciplinary pain rehabilitation (IPR) earlier than planned [Citation1–6]. The majority of the early terminators of IPR stopped during the diagnostic phase or in the first 8 weeks of treatment [Citation2,Citation5]. Poor bio-psychosocial functioning predicts higher pain severity [Citation7], and high pain severity before rehabilitation is associated with higher rates of early termination [Citation6]. In a recent systematic review, 18 predictors of early termination were identified in four domains: socio-demographic, patient, disease, and treatment [Citation8]. For example, the review showed that ethnicity, duration of work disability and somatisation are predictors for early termination. Also, the treatment location appears important; higher rates of early terminators have been described in rehabilitation centres compared with rehabilitation treatment in a hospital. No differences were found in sex and age between early terminators and completers, nor in predictors such as inpatient and outpatient programs, diagnosis or country [Citation4].
There is a wide diversity in duration of IPR [Citation9,Citation10]. A gold standard treatment duration is not available. A mean and median IPR treatment duration of around 12 weeks is described, but often the actual treatment duration was not equal to the initially planned treatment duration [Citation5,Citation11].
Single predictors for treatment adherence in chronically ill patients showed conflicting results [Citation12]. Research of physical and perceptual barriers to adherence, and patients’ beliefs and concerns regarding treatment could provide more insight into causes of non-adherence, which may be also important in patients with chronic pain. Reasons for not maintaining exercise in patients with low back pain are beliefs that exercise does not help or aggravates pain, disliking exercise or other medical problems that prevent exercise [Citation13]. Predictors of early IPR termination are, among other things, pre-contemplation and low self-efficacy [Citation8]. In mental health care also practical barriers, such as transportation problems or difficulties arranging childcare, have been associated with early termination [Citation14].
In two Dutch studies of IPR patients of non-Dutch origin (i.e., Turkish and Moroccan), the most frequently mentioned reason for early termination is a discrepancy between the expected content of the treatment and the actual treatment, for example, expecting a specific medical diagnosis or pain relief as a result of IPR [Citation15,Citation16]. Interpretation of earlier information and experiences influences patients’ beliefs about their illness and therefore effects their behaviour [Citation17]. These pre-existing beliefs about illness and treatment may affect adherence to and outcomes of treatment [Citation18]. However, several meta-analyses have shown a very weak relationship between individual illness beliefs and treatment adherence in patients with chronic diseases [Citation19,Citation20].
Better insight in numbers, timing, and reasons for early termination is needed, because early termination from IPR is associated with poor treatment outcomes [Citation21–23]. Numbers and better understanding of early termination may help to inform strategies to decrease unneeded early termination. However, an accurate number of early termination is unknown in Dutch IPR. In addition, very few studies have reported on the timing of early termination [Citation2,Citation5]. Timing refers to the stage of IPR and the amount of IPR that is lost due to early termination. Research on early IPR termination had been mainly focused on differences in characteristics between completers and early terminators [Citation8], but not patient-reported reasons. The aims of this study were to calculate the rate of early terminations in two Dutch outpatient IPR centres, to analyse the timing of early termination, and to explore the reasons for early termination.
Materials and methods
Design
This study used a mixed method design conducted on the outpatient clinic in two rehabilitation centres (UMCG and Revalidatie Friesland) and one rehabilitation department of a hospital (Revalidatie Friesland). In the quantitative part, numbers, timing, and reasons for early termination were retrieved from patient files. In the qualitative part, reasons for early termination were further explored in semi-structured interviews with early IPR terminators. It is non-medical research with only mentally competent adults. All participants received care as usual, so there were no additional safety concerns for the participants. Participation of the interviews was voluntarily after informed consent. The research took little time of the participants. Therefore, the Medical Ethical Review Committee of the UMCG (METc 2016/276) confirmed that the Medical Research Involving Human Subjects Act (WMO) did not apply for our research and that official approval of this research by the Medical Ethical Review Committee was not required (Research Register 201600420).
Participants
In the quantitative part, all patient files of adult patients with chronic musculoskeletal pain who had followed IPR in 2015 were studied in two outpatient centres for IPR in the North of the Netherlands: UMCG Center for Rehabilitation, and Rehabilitation Friesland (two locations). There were no exclusion criteria for participation in the study. Based on historical data, we estimated that 400–500 files would be available. With a mean rate of early termination of approximately 25% [Citation1–6], a rate of 100–125 early terminators was expected. In the qualitative part, all adult early terminators of IPR during that time (2017–2018) at the same centres were recruited. Also for this part there were no exclusion criteria.
There are several definitions of early termination in literature. One definition is: “patients with chronic pain, who were referred to a chronic pain management program, who initiated (participated in the baseline assessments), but discontinued prior to completion of the entire program” [Citation3]. Based on earlier literature [Citation5] and expert opinion, we accepted a range of ±1 week between the planned treatment duration and actual treatment duration. Therefore, in this study, early terminators were operationally defined as participants who stopped IPR at least more than 1 week before the planned duration. Positive early terminators were defined as early terminators who had achieved their goals early. Participants with all other reasons for early termination were regarded as negative early terminators.
Intervention
Patients were referred by their general practitioner or medical specialist for outpatient pain rehabilitation treatment. The rehabilitation team of IPR consists of rehabilitation physicians, physiotherapists, occupational therapists, psychologists, and social workers and in Revalidatie Friesland also of psycho-motor therapists and music therapists. During the consultation with the rehabilitation physician, the medical history is taken and a physical examination is conducted. At the end of the consultation, the patient receives extensive verbal personalised information about chronic pain and the content and aim of IPR. Most of the time they also receive information about one or more educational websites and/or written information. In a shared decision-making process, it is decided whether the patient is admitted to IPR. Patients of the UMCG have a one-day screening and patients of Revalidatie Friesland eventually a screening by a psychologist before starting the IPR. After this screening, it is decided whether the patient continues the treatment and the total IPR duration is planned (generally 12 weeks). IPR consists of physical therapy as well as occupational therapy, two to four times a week, and an appointment with the psychologist or social worker, one time a week. In individual cases also psycho-motoric therapy or music therapy is added to IPR. If possible, the frequency of physiotherapy and occupational therapy was decreased to one time per week in the second half of IPR. The overall aim of IPR was to decrease pain-related disability.
Study procedures
In the quantitative part of the study, patient files were analysed by the main researcher (DS) or co-author (AMB). Age, sex, planned treatment duration, actual treatment duration and reason for early termination were documented. In the qualitative part, semi-structured interviews with early terminators were conducted by the main researcher (DS). All early terminators were asked to participate by one of the IPR team members. The main researcher contacted the early terminators for informed consent, and an appointment for the interview was made. New interviews were held until data saturation had occurred [Citation24], indicating that all possible reasons for early termination were mentioned. Interviews were performed by the main researcher. The interviews were held face-to-face in the rehabilitation centre, at the patient’s home or, if preferred, by telephone. On average, the interviews took approximately 30 min and were recorded. Main goal of the semi-structured interviews was to identify reasons for early IPR termination based on the opinions of the early terminators. Participants were interviewed regarding their reasons for early termination, expectations of the rehabilitation treatment, earlier diagnostics and/or treatment, cause of the pain and personal information. Those topics were based on literature and expert opinion. The interviews were pilot-tested with a psychologist from the IPR team. After the first interviews, the topic list was adjusted on the acquired information. For patients who declined to be interviewed, the IPR team was asked to register age and sex.
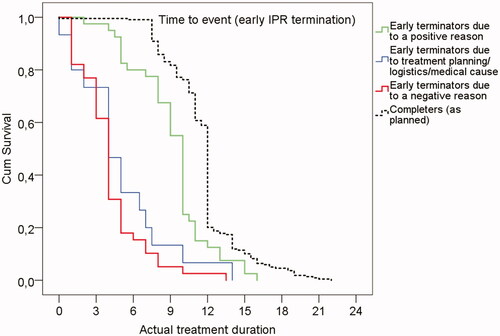
Data analyses
Quantitative part of the study: The number of early terminators and reduction in IPR duration (descriptive statistics) were calculated with the Statistical Package for Social Sciences (SPSS version 23, SPSS Inc., Chicago, IL). A survival analysis was performed to determine the timing of termination. For this survival analysis, participants were classified into four groups: (1) early terminators due to a positive reason (goals achieved earlier); (2) early terminators due to IPR planning/logistics/medical reason; (3) early terminators due to a negative reason (all other reasons than 1 and 2); and (4) completers as planned. Participants with an unknown actual treatment duration or an unknown reason for early termination were excluded for the survival analysis. A log rank test was performed to analyse differences in treatment duration between early terminators due to a positive reason, goals achieved earlier (group 1) and early terminators due to a negative reason (group 3). A post hoc power analysis was performed with PS Power and Sample Size Calculations (version 3.0, January 2009).
Qualitative part of the study: All interviews were recorded and transcribed by the main researcher, and afterwards the main researcher performed coding with AtlasTi. Recurrent and similar codes were merged and categorised into preliminary main themes by the main researcher. Those preliminary themes and corresponding quotes were discussed with all other researchers, adjustments were made, and again discussed. The main researcher was a resident physiatrist. Other researchers all possess PhD-Degree, and two of them are physical therapist and two of them are physiatrists with extensive IPR and research experience.
Results
Quantitative part
A total of 428 patient files were studied. The mean patient (standard deviation (SD)) age was 42.4 (13.3) years, and 68% were women. About 70% of the participants was treated in a rehabilitation centre and 30% at the rehabilitation department in a hospital. Overall, 137 participants (31.3%) had terminated IPR early. The mean (SD) age of the early terminators was 41.5 (14.0) years and 67% were women. The difference in age (independent t-test) or sex (Pearson’s chi-square) between early terminators and completers was not significant (p = 0.327 and p = 0.855, respectively). In the rehabilitation centres, there was an early termination percentage of 27.2% and at the rehabilitation department in the hospital there was an early termination percentage of 43.3%. Data about the initially planned and actual IPR duration were available for 82 early terminators (60%). The median (interquartile range (IQR)) planned IPR duration was 12.0 weeks (12.0; 12.0); the median reduction of the program by the early terminators was 5.3 weeks (3.0; 8.0).
The most frequently documented (30%) reason for early termination was “goals achieved early” (). A second or a third reason for early termination was documented in 39 cases and in one case, respectively. In 6%, the reason for early termination was unknown. Survival analyses of early terminators due to a positive reason (group 1, 30%) and early terminators due to a negative other than logistic or medical reasons (group 3, 44%) showed that over 80% of the early terminators with a negative reason stopped in the first half of IPR (1–6 weeks), whereas approximately 55% of the early terminators with a positive reason stopped in the final quarter of IPR (between 9 and 11 weeks; ). The median (95% confidence interval (CI)) survival time of early terminators due to a positive reason (group 1) was 10 weeks (9.5; 10.5) and of early terminators due to a negative reason (group 3) was 4 weeks (3.5; 4.5). The differences in IPR duration between early terminators due to a positive reason (group 1), and early terminators due to a negative reason (group 3) were significant (log rank test (χ2=38.6, 1 df, p < 0.001)). A post hoc power analysis showed a power of 0.994 (α was set at 0.05; number of early terminators due to a positive reason = 41; median time to termination due to a positive reason = 10 weeks; median time to termination due to a negative reason = 4 weeks; accrual time = 52 weeks; follow-up = 22 weeks; the ratio of negative terminators over positive terminators = 1.49).
Table 1. Reasons for early termination noted in patient files.
Qualitative part
During the inclusion period, at least 35 early terminators were registered by the IPR team. Of those, 11 patients did not want to participate, one patient had no data registered, and three patients did not respond by telephone and/or e-mail. After interviewing five early terminators due to positive reasons, no new themes seemed to come forward. After four more interviews with early terminators due to positive reasons, still no new themes came forward. Therefore, we decided that data saturation occurred after interviewing nine early terminators who had achieved their goals earlier than initially planned. Thereafter, only early terminators due to other reasons were included. In total, 20 semi-structured interviews were conducted. The mean age of the interviewees was 44.0 years (SD 13.9), and 10 participants were women (50%). All participants were of Dutch origin. The 11 patients who did not want to participate had a mean age of 41.0 years (SD 13.3) and four were women (36%). The themes that arose from the semi-structured interviews are reported below. The quotes were selected as being representative for these themes.
Goals achieved early
Positive early terminators told that IPR went well and they had achieved their goals early; therefore, there was no indication for further IPR. Most of the positive early terminators felt the responsibility to make further adjustments in their private and professional lives. Some participants experienced pain relief as a result of those adjustments. Better understanding and management of their pain complaints was for most positive early terminators enough, and no further counselling was necessary. For example, one of the positive early terminators (patient 3) told that becoming pain free was not a goal for her, but as a result of IPR she was not depended on her wheelchair anymore.
Patient 1 (female, age 27): The goals, which were set, were achieved. And the treatment costs a lot of time. It is a treatment that needs you to come two times a week, whereas I could come only once a week. So we decided I could continue it at home, because it went well.
Patient 19 (male, age 35): I just went well. And continuing the treatment has to be meaningful. […] The pain is still there, but it’s quite reduced. I noticed that stress highly influences my body. […] I have made a lot of decisions. That was my main goal.
Expectations on the aim and content of the treatment
Some negative early terminators had hoped for further diagnostics or pain reduction as an effect of IPR. Besides that, some of them expected a more physical approach and less focus on the psychological aspects, especially during physiotherapy and occupational therapy. For example, they expected exercises from the physiotherapist and advice about postures from the occupational therapist.
Patient 5 (male, age 53): The actual reason to stop were the negative results. I have back complaints for years and I hoped that they could find a cause for my complaints. Afterwards it turned out to be just rehabilitation. […] And then I thought, now the physician will examine me, once more looking whether there is something wrong with the vertebras or my back. And then you end up with rehabilitation. That disappointed me.
Patient 6 (female, age 68): The treatment was not helpful. I had hoped for pain reduction. Or, at least, instructions which could lead to pain reduction. Anyhow, that didn’t happen. […] And after some time, I expected the occupational therapist to say for example how to lie down, how to sit, how to stand and how to walk. And the therapist to ask: well, and how are you going to do that? I received just one instruction, nothing more.
Patient 17 (male, age 52): The reason for early termination was the fact that with this treatment a lot of psychological counselling is given, but my problem is not a psychological problem. […] Maybe I wasn’t completely aware of the quite high psychological aspect. Maybe that is one thing that could be better explained before starting.
More physical complaints due to IPR
Some participants told that it was impossible to continue with the program due to an increase of physical complaints after therapy.
Patient 12 (male, age 66): The treatment was physically too heavy. The exercises were too heavy due to the pain. There were some days that I couldn’t walk anymore. And the physiotherapist didn’t listen very well. He made me do things that I couldn’t do. And afterwards I came home with much more pain.
Timing of the IPR
Sometimes the IPR timing was not right. One patient received the outcome of his request for a disability pension during the IPR and another patient’s child became ill.
Patient 9 (male, age 47): The reason why I stopped the treatment was because at the same time my sick leave period terminated. Then I received a disability pension for 72% and I appealed against that decision. […] And that decision was at the same time of the observational period. It all became too much.
Patient 18 (female, age 32): The second time I terminated was because my child had a seizure 4 or 5 months ago. And afterwards he had a lot of seizures and is diagnosed with epilepsy. So it was too hectic. […] When you have to come two or three times a week combined with a sick child, it is very busy.
Multiple participants mentioned a second or third reason for early termination, suggesting that early termination is often multifactorial. Reasons were the feeling of not being taken seriously and points of concern about treatment planning and logistics. These were overall themes, and most of the time not the main reason for early termination; however, in some cases, the reason contributed to the early termination.
Feeling of not being taken seriously
The participants’ feeling that the physician or therapist is taking the symptoms seriously is important for having confidence in the treatment. A physical examination or (explaining earlier) diagnostics (e.g., radiograph or MRI) can be helpful. When a patient does not accept the explanation for the symptoms, it can result in a negative reason for early termination.
Patient 3 (female, age 24) (goals achieved early): In the rehabilitation centre, I was examined another time. They also studied the MRI another time, and explained it to me. And then I thought, this is a second opinion, but they also showed the MRI to me on the screen. And at that point I thought, yes, I’m being taken seriously.
Patient 11 (female, age 42) (other expectations on the content of the program): They always told me that the complaints were related to stress. Every time it was repeated: stress, stress, stress. And it started to irritate me. I know that stress can cause physical complaints, but I also have real back complaints. And that’s not stress. So, when you have real back complaints, they say, ‘That could be right, because you have a really busy job.’ Then I think, ‘Here we go again.’
Points of concern about treatment planning and logistics
In multiple interviews, the short duration of the physiotherapy and disturbances, such as phone calls, during IPR were mentioned. Besides that, not being able to fit much therapy into the short appointment time and discontinuity of therapists were frequently mentioned.
Patient 11 (female, age 42): Therapy takes only half an hour. At first, the therapist has to search for a room. Then, the therapist has to type something on the computer. And, when you are treated by different physiotherapists all the time, you constantly need to explain your problem again. And, sometimes, in the middle of therapy, the therapist will pick up the phone. It’s not professional and it all detracts from my time.
Discussion
This study showed that almost one-third of the participants terminated early from IPR, with a median reduction of 5.3 weeks. In contrast to others [Citation2], this study showed a higher percentage of early terminators in the hospital compared to the rehabilitation centres. The most frequently mentioned reason for early termination was “goals achieved early”. Approximately, 55% of the early terminators with positive reasons stopped in the final quarter of IPR, whereas over 80% of the early terminators with negative reasons stopped in the first half of IPR. Many negative early terminators mentioned, a discrepancy between expectations of the aim and content of the actual IPR, as the reason for early termination. Participants had hoped for pain reduction and/or expected a more physical approach. Otherwise, many of the positive early terminators were able to self-management. Besides “goals achieved early” and “other expectations on the aim and content of the programme”, other reasons for early termination were also identified by the semi-structured interviews. Participants experienced more physical complaints as a result of the treatment, the timing was not right due to personal factors, the feeling of not being taken seriously, or due to problems concerning treatment planning and/or logistics.
With almost one-third of participants terminating IPR early, it is important to identify the reasons for early termination. While the prevailing assumption is directed toward negative reasons only, this study is the first to shed a different light on early termination from IPR. “Goals achieved early” was most frequently mentioned reason for early termination, suggesting that the current duration of IPR may be too long for a subgroup. On the other hand, almost half of the early terminators had a negative reason for early termination. Negative early termination can be regarded as an undesirable outcome because it will contribute to disappointment of patients and clinicians, and unnecessary medical costs. Due to the outcomes of our semi-structured interviews, this study provides more insight into the patients perspectives of reasons for IPR termination.
Studies about the dose–effect relation of vocational rehabilitation show that patients with a poor prognosis for returning to work benefit most from extensive treatment, whereas patients with a good prognosis benefit from both extensive as from less extensive treatment [Citation25]. These findings suggest that an individual IPR dose should be determined based on characteristics such as prognosis. Prognosis and adherence to IPR are difficult to predict. A validated tool to assist in the personalised decisions for IPR content and dosage, however, is unavailable.
Although patients receive extensive personalised information about the aim and content of IPR before starting, this study showed that Dutch early terminators with a negative reason have often different expectations on the aim and content of the treatment. Two other Dutch studies of patients of non-Dutch origin showed also a discrepancy between the expected content of the treatment and the actual treatment as the main reason for early IPR termination [Citation15,Citation16]. Although early termination due to a discrepancy between the expected content of the treatment and the actual treatment occurred significantly more frequently in patients of non-Dutch origin, substantial rates of Dutch early terminators had also different expectations (82% in patients of non-Dutch origin versus 62% in Dutch patients) [Citation16]. Furthermore, in the same study [Citation16], early termination due to unknown reasons (refusal to participate and no show) occurred more often in Dutch patients (38% in Dutch patients versus 15% in non-native patients). We postulate that those different expectations may not be determined by ethnicity, but because the initial information is not sufficiently adjusted to the specific needs of the individual patient. Low health literacy combined with inadequately tailored communication of the health care practitioner may explain patients’ different expectations on the aim and content of IPR. Health literacy entails patients’ knowledge, understanding, appraisal and apply of health information in order to make judgments and take decisions concerning health care [Citation26]. Nearly half of the Europeans have inadequate health literacy skills, and migrants have more often limited health literacy skills [Citation27]. These limited skills can explain the higher rate of early termination due to different expectations among patients of non-Dutch origin compared to Dutch patients. Otherwise, little is known about the influence of health literacy on patients’ beliefs about their condition [Citation28]. IPR should aim to increase patients’ health literacy through therapeutic patient education [Citation29]. There is limited evidence that pain neurophysiology education (PNE) significantly increases knowledge about pain [Citation30]. The use of universal health literacy precautions to provide understandable and accessible information for all patients is recommended [Citation28]. In addition, printed information and visual aids can enhance patient understanding. In the future, health care professionals and research studies should be less focused on the amount of information, and more focused on the way to explain it to the patient and check whether the patient has understood it well and is convinced of its credibility. For example, it may be useful for more patients than now already done to schedule a new appointment after approximately 2 weeks to discuss the provided information, checking whether the patient has understood it and is still motivated for IPR. In addition, to increase physical activity, time contingent principles are used instead of pain contingent principles. In the beginning, this might temporarily aggravate the musculoskeletal pain as a result of inactivity and deconditioning. Explaining this concept and possible reactions to IPR before participation is therefore important, stressing and educating that a temporary symptom increase does not equal unsafety. Participants were informed that when in doubt, they could contact the physiatrist for explanation and maybe recurrent or additional medical examination. No formal complaints were issued by the participants. Thus, we have no reason to believe that IPR has inflicted serious adverse events in any of the participants.
Besides providing understandable and accessible information to patients, exploring patients’ illness beliefs seems also to be important. Those beliefs are based on interpretation of earlier information and experiences and influence their behaviour and also may affect their adherence to and outcomes of treatment [Citation17,Citation18]. As the aim of IPR is that patients with chronic pain are able to cope with their pain complaints, therefore patients have to change their explanatory model [Citation31] away from finding the solution to their pain complaints, in order to be able to make behaviour adjustments. In a study with rehabilitation physicians of patients of non-Dutch origin, early terminator was reported that some patients kept searching for a medical explanation for their complaints due to a need for identification of their complaints regarding their social environment [Citation15]. Sometimes, patients were given the benefit of the doubt regarding their possibilities to adjust their way of coping, but not all patients were able to make the shift to the pain being explained by a multifactorial cause rather than solely a medical cause. Then they lost confidence and terminated early. It is not clear if the results of those interviews can be generalised to all early terminators. With our research we shed a light on the view of early terminators. But more insight in the perspectives of IPR team members about early termination could be interesting. Qualitative interviews with IPR team members of Dutch early terminators about early termination is an implication for further research.
The strength of this study is that besides the patient file review, semi-structured interviews with early terminators were held. This combination of quantitative and qualitative data provides a broader and deeper understanding of early IPR termination, and the themes and quotes of the qualitative part appear to strengthen the results of the quantitative part. Besides the mixed method design, it is also a two-centre study conducted at three different locations, increasing the generalisability of this study. The limitations of the study were the relatively high rates of missing data in the patient files and non-participators in the semi-structured interviews. In only 60% of the patient files of early terminators, the initially planned duration of the treatment and/or the actual duration of the treatment was documented. Due to those missing data, the calculation about reduction in treatment duration is less precise. Also the relatively small sample size (n = 20) of the qualitative part is a limitation. In particular, because coding was only performed by the main researcher and there was no second researcher that performed coding to explore whether other/similar themes emerged. And therefore there was no second control if data saturation had really occurred. Besides the 20 semi-structured interviews that were held, there were at least 15 more early terminators during the inclusion period. Participants who were satisfied about treatment might have been more willing to participate in this study than participants who were not satisfied, leading to selection bias and resulting in a more positive effect. Another limitation of the study is not performing purposefully sampling of participants of non-Dutch origin versus Dutch participants, while Dutch literature shows that non-Dutch origin is an important factor in early IPR termination in the Netherlands [Citation8]. In the quantitative part, we did not analyse ethnic group because ethnicity was not specifically noted in the patient files. Of all early terminators of the qualitative part, there was no patient of non-native origin. We postulate that a couple of reasons are responsible for this. At first, inclusion of participants was performed at three locations, all in the northern region of the Netherlands. In this region, less people of non-native origin are domiciled compared to other parts of the Netherlands. Another explanation could be that patients of non-Dutch origin less often start with IPR, for example due to language barriers. Future research should also include this aspect.
This study presents both quantitative and qualitative information about early termination. Besides numbers and timing of early termination, reasons for early termination also were explored. The results show that most very early terminators stop due to negative reasons and late early terminators often stop due to positive reasons (goals achieved early). Patient beliefs about pain and expectations about IPR and self-management can influence the adherence of the treatment.
Acknowledgements
Many thanks are due to all rehabilitation physicians and therapist of the Pain Rehabilitation Department of the Center for Rehabilitation of the University Medical Centre Groningen and Revalidatie Friesland for including the participants of the qualitative part of the study.
Disclosure statement
The authors report no declarations of interest.
References
- Bendix AE, Bendix T, Haestrup C, et al. A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients. Eur Spine J. 1998;7(2):111–119.
- Sloots M, Scheppers EF, van de Weg FB, et al. Higher dropout rate in non-native patients than in native patients in rehabilitation in The Netherlands. Int J Rehabil Res. 2009;32(3):232–237.
- Rainville J, Ahern DK, Phalen L. Altering beliefs about pain and impairment in a functionally oriented treatment program for chronic low back pain. Clin J Pain. 1993;9(3):196–201.
- Turk DC, Rudy TE. Neglected factors in chronic pain treatment outcome studies-referral patterns, failure to enter treatment, and attrition. Pain. 1990;43(1):7–25.
- Waterschoot FPC, Dijkstra PU, Geertzen JHB, et al. Course of disability reduction during a pain rehabilitation program: a prospective clinical study. Int J Rehabil Res. 2015;38(1):34–39.
- McGeary DD, Mayer TG, Gatchel RJ. High pain ratings predict treatment failure in chronic occupational musculoskeletal disorders. J Bone Joint Surg Am. 2006;88(2):317–325.
- Koenig AL, Kupper AE, Skidmore JR, et al. Biopsychosocial functioning and pain self-efficacy in chronic low back pain patients. J Rehabil Res Dev. 2014;51(8):1277–1286.
- Oosterhaven J, Wittink H, Mollema J, et al. Predictors of dropout in interdisciplinary chronic pain management programmes: a systematic review. J Rehabil Med. 2019;51(1):2–10.
- Scascighini L, Toma V, Dober-Spielmann S, et al. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670–678.
- Guzmán J, Esmail R, Karjalainen K, et al. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322(7301):1511–1516.
- Reneman MF, Waterschoot FPC, Burgerhof JGM, et al. Dosage of pain rehabilitation programmes for patients with chronic musculoskeletal pain: a non-inferiority randomised controlled trial. Disabil Rehabil. 2018;42:1–8.
- Kane SV, Robinson A. Review article: understanding adherence to medication in ulcerative colitis – innovative thinking and evolving concepts. Aliment Pharmacol Ther. 2010;32(9):1051–1058.
- Mailloux J, Finno M, Rainville J. Long-term exercise adherence in the elderly with chronic low back pain. Am J Phys Med Rehabil. 2006;85:120–126.
- Taylor S, Abramowitz JS, McKay D. Non-adherence and non-response in the treatment of anxiety disorders. J Anxiety Disord. 2012;26(5):583–589.
- Sloots M, Dekker JH, Pont M, et al. Reasons of drop-out from rehabilitation in patients of Turkish and Moroccan origin with chronic low back pain in The Netherlands: a qualitative study. J Rehabil Med. 2010;42(6):566–573.
- Sloots M, Dekker JH, Bartels EA, et al. Reasons for drop-out in rehabilitation treatment of native patients and non-native patients with chronic low back pain in the Netherlands: a medical file study. Eur J Phys Rehabil Med. 2010;46(4):505–510.
- Horne R, Chapman SC, Parham R, et al. Understanding patients' adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS One. 2013;8(12):e80633.
- Weinman J, Petrie KJ. Illness perceptions: a new paradigm for psychosomatics? J Psychosom Res. 1997;42(2):113–116.
- Aujla N, Walker M, Sprigg N, et al. Can illness beliefs, from the common-sense model, prospectively predict adherence to self-management behaviours? A systematic review and meta-analysis. Psychol Health. 2016;31(8):931–958.
- Brandes K, Mullan B. Can the common-sense model predict adherence in chronically ill patients? A meta-analysis. Health Psychol Rev. 2014;8(2):129–153.
- de Rooij AD, Roorda LD, Otten RH, et al. Predictors of multidisciplinary treatment outcome in fibromyalgia: a systematic review. Disabil Rehabil. 2013;35(6):437–449.
- Andrews NE, Strong J, Meredith PJ. Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2012;93(11):2109–2121.
- van der Hulst M, Vollenbroek-Hutten MM, IJzerman MJ. A systematic review of sociodemographic, physical, and psychological predictors of multidisciplinary rehabilitation-or, back school treatment outcome in patients with chronic low back pain. Spine. 2005;30(7):813–825.
- Rubin H, Rubin I. Qualitative Interviewing: The Art of Hearing Data. Thousand Oaks: Sage Publications; 1995.
- Haldorsen EM, Grasdal AL, Skouen JS, et al. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain. Pain. 2002;95(1–2):49–63.
- Sorensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(80):80.
- Kickbusch I, Pelikan JM, Apfel F, et al. Health literacy: the solid facts. Geneva: World Health Organization; 2013.
- Wittink H, Oosterhaven J. Patient education and health literacy. Musculoskelet Sci Pract. 2018;38:120–127.
- Ojala T, Hakkinen A, Karppinen J, et al. Chronic pain affects the whole person-a phenomenological study. Disabil Rehabil. 2015;37(4):363–371.
- Geneen LJ, Martin DJ, Adams N, et al. Effects of education to facilitate knowledge about chronic pain for adults: a systematic review with meta-analysis. Syst Rev. 2015;4(132):132.
- Kleinman A. Patients and healers in the context of culture. An exploration of the borderland between anthropology, medicine and psychiatry. Los Angeles: University of California Press; 1980.