Abstract
Background: Access to healthcare contributes to the attainment of health and is a fundamental human right. People with disabilities are believed to experience widespread poor access to healthcare services, due to inaccessible environments and discriminatory belief systems and attitudes. Qualitative data on these barriers has not previously been systematically reviewed. A meta-synthesis was undertaken of qualitative studies exploring the barriers to primary healthcare services experienced by people with disabilities in low- and middle-income countries.
Methods
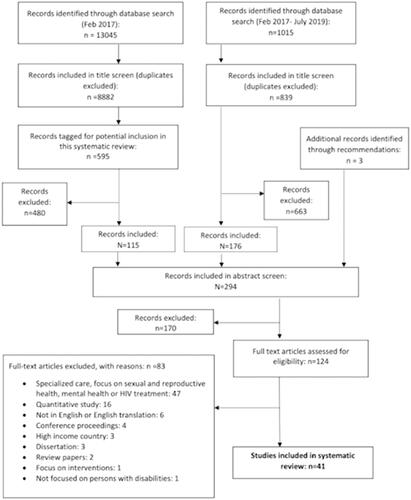
Six electronic databases were searched for relevant studies from 2000 to 2019. Forty-one eligible studies were identified.
Results
Findings suggest that the people with disabilities’ choice to seek healthcare services or not, as well as the quality of intervention provided by primary healthcare providers, are influenced by three types of barriers: cultural beliefs or attitudinal barriers, informational barriers, and practical or logistical barriers.
Conclusion
In order to achieve full health coverage at acceptable quality for people with disabilities, it is necessary not only to consider the different barriers, but also their combined effect on people with disabilities and their households. It is only then that more nuanced and effective interventions to improve access to primary healthcare, systematically addressing barriers, can be designed and implemented.
People with disabilities in both high income and low- and middle-income country settings are more likely to experience poorer general health than people without disabilities.
Barriers to accessing primary healthcare services for people with disabilities result from a complex and dynamic interacting system between attitudinal and belief system barriers, informational barriers, and practical and logistical barriers.
Given primary healthcare is often the initial point of contact for referral to specialty care and rehabilitation services, it is crucial for people with disabilities to access primary healthcare services in order to get appropriate referrals for such services, specifically rehabilitation as appropriate.
To achieve full health coverage at acceptable quality for people with disabilities, starting with primary healthcare, it is necessary for healthcare stakeholders, including rehabilitation professionals, to consider the combined and cumulative effects of the various barriers to healthcare on people with disabilities and their families and develop an understanding of how healthcare decisions are made by people with disabilities at the personal and the household level.
IMPLICATIONS FOR REHABILITATION
Introduction
Health is defined as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [Citation1]. Achievement of good health is inherently important, but also contributes to the attainment of other goals, such as inclusion in education and freedom from poverty. Everyone, regardless of their age, health conditions or related impairments, needs general health services, with only some requiring specialist or impairment-related care. The general health services are often provided at the primary healthcare level, where around 80–90% of people’s healthcare needs across their lifetime can be provided [Citation2]. Primary healthcare has therefore been recognised as an essential component for achieving health for all since the Alma- Ata Declaration in 1978, and is often the first point of contact within national health systems for individuals, families, and communities [Citation3]. Unfortunately, however, according to the World Health Organization (WHO) approximately 400 million people worldwide lack access to healthcare services, with a disproportionate percentage of this population belonging to particularly vulnerable or marginalised groups, such as people with disabilities [Citation4]. The United Nations’ Convention on the Rights of Persons with Disability defines disability as an “evolving concept….disability results from the interaction between people with impairments, attitudinal, and environmental barriers that hinder their full and effective participation in society on an equal basis with others” [Citation5]. It is estimated that about one billion people worldwide live with a disability with approximately 80% living in LMIC [Citation4]. Given these statistics, it is important to understand the barriers to primary healthcare access that are experienced by people with disabilities so that they can be overcome, and the right to healthcare for all can be realised.
The relationship between disability, health, and healthcare access is complex. Research has shown that people with disabilities in both high income and low and middle-income countries (LMIC) are more likely to experience poorer general health than people without disabilities [Citation4]. While the presence of a health condition is the original cause of an impairment, there are additional reasons why people with disabilities may experience worse health than others. Social and economic causes of poor health are well recognised [Citation6] and the interaction between such factors is complex and for people with disabilities this disadvantage is often magnified. For example, people with disabilities are on average older and poorer [Citation7], and often excluded from opportunities for productive living such as accessing education and employment [Citation4]. These disadvantages can lead to worsening of mental and physical health [Citation6,Citation8]. People with disabilities may also experience secondary health conditions as a result of their impairment (e.g., pressure sores) and are on average more likely to exhibit unhealthy behaviours related to the consequences of intersectionalties, and limited access and opportunities for programs that allow for healthier life choices, contributing to poorer health [Citation9].
People with disabilities consequently may have additional needs for general healthcare, because of their greater vulnerability to poor health. They may also require specialist care and rehabilitation to address ongoing aspects of their impairments, which may be accessed through referral from primary health services [Citation4]. Yet, at the same time, people with disabilities often experience greater barriers to their healthcare access, despite their greater need [Citation10–18], due to inaccessible environments and discriminatory belief systems and negative attitudes. Evidence from high income contexts suggests that, in comparison to non-disabled people, people with disabilities attend fewer routine health examinations [Citation19], and are less likely to receive preventive care [Citation14,Citation20–22]. This impact on healthcare access has also been reflected in data from LMICs [Citation23]. While limited, evidence also suggests that when people with disabilities do seek healthcare, they receive poorer quality services [Citation16,Citation24–27] and incur greater expenses [Citation4,Citation26].
Given the importance of access to healthcare services for all, different researchers have focused on how healthcare “access” can be conceptualized. One conceptual framework of access to health care is proposed by Levesque et al. [Citation28]. In this framework, the authors focus on identifying barriers to access along the healthcare-seeking journey from identification of a healthcare need, seeking healthcare services, reaching healthcare resources, obtaining or using healthcare services and actually being offered services appropriate to their care needs [Citation28]. The framework identifies five dimensions of accessibility of services (supply side determinants) and five corresponding dimensions which describe the abilities of consumers to access healthcare services (demand side determinants). This framework is one of the only ones that explicitly takes into consideration consumers’ capacities and as a result may be particularly relevant when considering access to healthcare for people with disabilities ().
Figure 1. Conceptual framework of access to healthcare by Levesque et al. [Citation28].
![Figure 1. Conceptual framework of access to healthcare by Levesque et al. [Citation28].](/cms/asset/f97e608a-fa2b-4e7a-b057-168c900a1a08/idre_a_1817984_f0001_c.jpg)
The process of accessing healthcare services for people with disabilities can be exceptionally complex depending on the type and severity of their impairment, the personal characteristics of the user (e.g., age, gender, socio-economic status, education) and their particular social context. Examples of barriers faced can range from people with physical disabilities having difficulty accessing sexual and reproductive services, due to misconceptions that they are asexual, to a person with hearing impairment awaiting his or her turn in a busy clinic where names or numbers are only called out verbally with no visual cues, and so they miss their slot. Clearly then, depending on how access or barriers to accessing healthcare are measured, some of the barriers experienced by people with disabilities may be subtle, hidden, and interlinked, and as a result are best described and explored qualitatively. There has been a significant increase in the number of studies, both quantitative [Citation23] and qualitative, published on access to healthcare for people with disabilities over the past 10 years. This increase may be partially due to the increased visibility of disability as an issue, promoted by World Report on Disability and the release of WHO Global Disability Action Plan 2014–2021: Better Health for All People with Disabilities [Citation29]. However, efforts to synthesise findings across qualitative studies have been lacking, aside from a recent literature review focusing on barriers to reproductive health services for women with disabilities in LMIC [Citation30]. To date, there have been no published meta-synthesis of this qualitative research focusing on barriers to accessing primary healthcare services for people with disabilities in LMIC countries.
This paper aims to describe the barriers to primary healthcare services experienced by adults with disabilities in LMICs, through a meta-synthesis of qualitative studies. We believe that the focus on the qualitative literature will allow the identification of a network of more complex and nuanced barriers that may be commonly missed by existing quantitative metrics and meta-analysis.
Methods
Six databases (EMBASE, CINAHL, Web of Science, MEDLINE, Global Health and PSYCHINFO) were used to search for peer reviewed studies published between January 2000 and July 2019. The search was done in two stages. First, the literature published between 2000 and February 2017 were searched by one of the authors, TB. Articles were screened into two groups. One group was qualitative papers focusing on access to primary healthcare by people with disabilities in LMIC for this current review, while the second was for a quantitative systematic review focusing on access and uptake of general healthcare services in LMIC by people with disabilities completed by TB and HK [Citation23]. In July 2019, the same database search strategy was applied again by TB for the period of 2017–2019, to update the qualitative literature review, with the inclusion of additional terms to limit the findings to qualitative studies only.
The literature search strategy for both reviews included keywords for the three common concepts shared between the two reviews: LMICs, people with disabilities, access/barriers to health services. The key words used in the searches were developed using MeSH (Medical Subject Headings used by the National Library of Medicine to index articles) or equivalent headings, as well as from other reviews on similar topics. Boolean, truncation, and proximity operators were used to construct and combine searches for the key concepts as required for individual databases [Citation23]. An example of the search terminology is provided in Supplementary File S1.
Two of the authors (GH and HK) screened all titles, abstracts and full texts from both searches independently, to identify potentially eligible qualitative studies based on the inclusion and exclusion criteria. The inclusion criteria were:
Used at least one qualitative data collection method (e.g., interviews, focus groups, action research, or observations – including textual or visual analysis).
Published in English language on or after the year 2000. This cut off year was chosen as it was the year of the Millennium Summit that led to the development of the Millennium Development Goals, designed to address some of the global challenges faced at the time, including meeting the needs of the most vulnerable and to enhance equality [Citation31].
Investigated access to general or primary healthcare services by adults with disabilities, either from the perspective of people with disabilities, their caregivers, and healthcare stakeholders.
Conducted in LMICs as defined by the World Bank country classifications [Citation32].
The exclusion criteria included:
Conducted in a country that is not considered a LMIC, according to the World Bank country classification [Citation32].
Quantitative nature of data collection.
Investigated access to HIV/AIDS specific services, sexual and reproductive health, mental health and/or specialized healthcare services as these services are often received after referral from a primary healthcare provider.
Focus only on access to primary healthcare services for children with disabilities.
Any disagreements in the selection of the full text for inclusion were resolved through discussion. If multiple reports based on the results of the same study were identified, the paper which included more detailed results of the qualitative data focusing on access to primary healthcare was included.
While no papers were excluded on the basis of the quality of the research or reporting, one of the authors (GH) assessed all the selected studies using the consolidated criteria for reporting qualitative research (COREQ) checklist [Citation33]. The COREQ checklist provides a comprehensive analysis of the components that should be included in qualitative studies, consisting of the research team, study design, data analysis, and reporting [Citation33].
The meta synthesis was performed taking into consideration both the ENTREQ (Enhancing Transparency in Reporting the Synthesis of Qualitative Research), and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) statements [Citation34,Citation35]. Both the PRISMA and ENTERQ checklists are provided in the Supplementary Files S2 and S3 respectively.
Data extraction and analysis
All selected papers were analysed using a thematic synthesis approach used by Thomas and Harden [Citation36]. Thematic synthesis is a strategy that was developed for analysis and integration of findings in systematic reviews of qualitative literature [Citation36]. The approach has been recommended as it goes beyond content analysis of the original studies and involves further synthesis of the themes [Citation36]. The process consists of three stages: line by line coding of the “findings” or “results” of the primary studies, developing descriptive themes, and developing analytical themes in order to identify overarching patterns occurring across the included studies. Nvivo 12 software was used to manage the qualitative data analysis process.
The first two stages of the process involved coding text and developing descriptive themes, as outlined by the thematic synthesis approach above. Both inductive and deductive coding strategies, based on prior knowledge of the topic, were applied. The number of codes was dynamic, in that at times it was realized that a code needed to be divided into two, or two codes could be combined into one. The coding process was completed by GH for all the studies, with independent and random checking of 20% of the studies by MW, which resulted in discussions and further merging or separation of codes. The final stage, analytical theme generation, involved discussions between authors GH and MW on various potential angles and approaches to how the codes could be categorized into descriptive and analytical themes which best accounted for the findings arising across the entire combined dataset.
Results
The first database search conducted in February 2017 identified 8882 titles (after duplicates were removed) and the second database search conducted in July 2019 identified an additional 839 titles. Title, abstract, and full article screening of papers resulted in 41 eligible studies that were reviewed. The details of the screening process involved in identification of the articles in the review are presented in .
The COREQ checklist analysis, , revealed considerable variability in quality amongst the 41 qualitative research studies. While none of the studies met all of the checklist requirements, the majority of the studies included reporting on the key components of the domains of study design and analysis and findings. All studies used focus group discussions and/or interviews to gather qualitative data. In addition, two studies also used observation and one used photovoice to collect additional data. All but one study provided quotations to illustrate the themes or findings from their study, and all demonstrated consistency between their data and findings and the major themes discussed in their respective papers.
Table 1. Comprehensiveness of reporting using the COREQ checklist.
The 41 included papers represented a total of 1,638 participants from 18 countries: 10 African, 6 Asian, and 2 South American (). Thirty-one of the studies included the perspectives of people with disabilities, 12 included perspectives of caregivers and 21 perspective of other stakeholders ranging from policy makers, healthcare providers, non-governmental organizations and disabled people organizations. Ten studies did not include perspectives of people with disabilities, and only included non-disabled stakeholders, such as health care professionals or caregivers. Five of the studies included participants under the age of 18 years of age in addition to adult participants. While six of the studies did not specify the types of impairments and disabilities experienced by their participants, the ones that did, covered a range of impairments including: physical, sensory (hearing or vision loss), intellectual, psychological and multiple impairments. In terms of publication dates, 29 of the 41 studies (71%) were published between 2015 to 2019, with 12 studies published between 2005 to 2014, and none prior to 2005.
Table 2. Description of eligible studies.
Codes and analytical themes
A total of 58 codes were generated, however only the codes that focused on or were explicitly related to potential barriers to accessing primary healthcare services were included in the thematic analysis to minimize deviation from the main focus of review. The thematic synthesis process generated three broad overarching analytical themes: Cultural beliefs or attitudinal barriers, informational barriers, and practical or logistical barriers. provides an outline of the themes, coding groups, and their descriptions.
Table 3. Themes and codes identified.
Cultural beliefs and attitudinal barriers:
Belief systems are often shaped by social, cultural, and community attitudes [Citation37]. They can both influence people’s perception of self and others, and how one chooses to respond to such beliefs. Cultural belief and attitudinal barriers identified in the review included both direct and indirect experiences of discrimination and stigma while seeking healthcare.
One belief system that appeared to discourage people with disabilities and their caregivers from seeking any healthcare services, including primary healthcare, was the belief that disability is related to or caused by higher powers outside of the person, such as religion or witchcraft [Citation38–42]. This belief was often interpreted as the disability or any other symptoms experienced by an individual with a disability being inflicted by an external power, resulting in feelings that there was no point in seeking healthcare intervention and so treatments were only sought from traditional healers who might free the person of the condition [Citation38–42]. While this belief was mostly expressed by people with disabilities and their caregivers in the studies, it is possible that it may have also been the driving force in many of the negative interactions experienced by people with disabilities and their caregivers from community members and healthcare stakeholders, who may have shared these beliefs. This would then result in decisions to limit community presence, including accessing primary healthcare services. For example, in one of the studies a man with an intellectual impairment in Uganda described how he believed people with disabilities are perceived by healthcare providers during a focus group as:
To them (meaning healthcare providers) we are not human beings. Targeting us is a waste of time for them. I think they do not like us. They think intellectually challenged people are mad and therefore useless. [Citation43]
In another study, the caregiver of a person with disability from Peru explained how the experience of acquiring a disability identification (ID) card can be extremely negative due to the use of discriminatory language by the doctors. The experience makes the person with a disability or their caregivers less likely to go through the process of acquiring an ID card and thus effecting use of health services. He stated:
you have to go to a public hospital, which entails showing up and hoping a doctor is there, hoping they treat you well. Even the terminology they use, they might say, ‘oh, your son is mentally disabled, right?’ or ‘your son is Down, right?’… They [doctors] are, excuse the expression, beasts. [Citation44]
Such interactions can result in people with disabilities and their caregivers, while recognizing the need for primary healthcare services, deciding not to seek the services, as they don’t feel it is worth the effort in confronting the attitudinal and social stigma involved in getting the healthcare [Citation41,Citation42,Citation45,Citation46].
While cultural belief and stigma were often described by family members, friends, or healthcare staff in relation to people with disabilities when seeking services, this can also be manifested as self-marginalization, also referred to as internalized oppression. This process occurs when the person him/herself believes the oppressing and stigmatizing view that others have of them, their impairments, illness, and disability. Internalized oppression can limit the capacity or willingness to seek healthcare and is related to the feelings of shame or embarrassment about speaking up regarding concerns and complaints. This view was expressed by a woman with mobility impairments from Kenya who felt that healthcare workers would not take her or other women with disabilities’ complaints regarding quality of care seriously:
I feel that the healthcare worker is mistreating me because I am disabled, so overall, we [women with disabilities] don’t like speaking up. [Citation46]
A healthcare provider from Iran also discussed how people with disabilities’ sense of shame and disempowerment may result in lack of identification, request for provision, or referral to appropriate services from primary healthcare services:
They (people with disabilities) don’t say their issues to the doctor, maybe because they feel ashamed to talk about certain issues with the doctor and this will later lead to other problems which cannot be solved easily……….There were even some people here who suffered from cervical cancer just because they didn’t tell their problem to anyone before this and they even had to get divorced. [Citation47]
The above quotes also reveal how intersectionalities, such as between marginalized identities of gender and disability, can further reinforce the experience of internalized oppression, though this varies greatly, depending on the cultural context.
The attitudes and stigma resulting from cultural belief systems can also result in over-protection and dependency, or conversely under-protection and neglect, by friends and family members of people with disabilities when accessing healthcare services. The real and perceived level of dependence can have both positive and negative impact on both people with disabilities and their caregivers, and may further influence their decision making and prioritization for seeking healthcare services. For instance, a number of the studies indicated that people with disabilities feel less valued by their family members and that they are left to fend for themselves in finding the resources to access services, including health [Citation41,Citation44,Citation48–51]. This concern is described in the following quote by a person with visual impairment in Cameroon:
When I tell my people that I’m sick, no one is willing to give me money to go to the hospital. I struggle before strangers give me something to support myself. I need assistance from my family but they behave as if I’m not human. [Citation41]
Another man with visual impairment from Brazil explained how family perceptions impact on awareness of health promotion activities by people with disabilities in the community:
If there is an open meeting on HIV… or reproductive health, blind people may not come if the family is not interested. He or she cannot decide him- or herself to go, even if she/he will be interested to participate. [Citation52]
The above example illustrates how both family members and other community members’ attitudes and behaviour is shaped by larger societal stereotypes and stigma, and results in lack of prioritization, or support for access to health education and information related to the healthcare needs of people with disabilities.
Applying the conceptual framework of access to healthcare by Levesque (2013), the examples discussed in this theme are likely to impact on the ability to perceive and ability to seek healthcare as part of the demand side determinants and the approachability and the appropriateness (interpersonal) dimensions of provision of healthcare from the supply side.
Informational barriers
Informational barriers focus on and include lack of insight, awareness, and understanding of issues related to health and wellness, including those related to impairment and the experience of disability. Informational barriers can occur on both the supply and demand side of healthcare services. From the supply side, this may mean lack of general knowledge by the healthcare providers about different impairments, the types of difficulties experienced by individuals with various impairments, or disability issues more broadly. These knowledge gaps can result in lack of comfort or confidence with providing care or adapting services to include people with disabilities, due to actual or perceived lack of expertise, even if the condition that brings the person to the service is not directly linked to their impairment (e.g., fever). This gap is recognized by both healthcare providers themselves and people with disabilities. For example, a doctor from Peru, described:
During those 7 years [becoming a doctor], you don’t receive any information regarding how to treat a person with disabilities. [Citation44]
Another healthcare stakeholder in South Africa admitted that the prejudice against people with disabilities limits healthcare provider’s openness to disability training, stating:
It’s still a difficult process and it’s still something that people are still afraid of people with disabilities. They just, and I do have to say not all persons are comfortable with even learning or becoming sensitized with people with disabilities. [Citation42]
The lack of insight on how to treat or interact with people with disabilities from healthcare providers often results in people with disabilities feeling the need to be accompanied by family members or friends when seeking care. A woman with hearing impairment from Indonesia who could directly communicate with healthcare providers only by writing information reported:
They should give us information in writing, but they don’t use that one. I cannot hear so they should communicate with me in writing … I need my husband to accompany me as they (doctors) speak with him directly. [Citation50]
Communication barriers often arise from lack of knowledge about different styles and alternative modes of communication (e.g., verbal, written, picture, or sign). In addition, use of complex technical health-related terminology can lead to difficulties in comprehension, particularly for people with cognitive difficulties. Aside from potentially creating anxiety, lack of effort in ensuring good communication can result in a person with a disability misunderstanding or questioning the accuracy and reliability of the information provided by the health professionals, and a mistrust of the quality of the services received [Citation53,Citation54].
Lack of insight about impairments and how they can limit one’s functional ability can also cause further mistreatment of people with disabilities. For instance, a woman with mobility impairments from Ghana recalled that providers often refused to help her climb onto beds that are not accessible to her:
When I get there I always struggle and climb the bed …. When I asked for help some of the nurses will start shouting on me about why I didn't bring any carer to look after me. [Citation55]
For people with disabilities, informational barriers may include lack of knowledge about their impairment, in addition to the lack of basic information and understanding of health and wellbeing, both general and specific to their underlying condition. This knowledge gap can cause the false assumption that they do not need to seek health services when they experience various symptoms. Similar to examples used in belief system barriers, such assumptions may lead to avoidably more complicated health conditions, subsequently requiring more specialized services, as demonstrated by the following quote by a man with visual impairments with a diagnosis of tuberculosis in Malawi:
They tell us when someone is infected with HIV, TB comes out because TB is a disease for those with AIDS. In my case I never suffered from AIDS and they said I don't need to go for TB testing. [Citation56]
Another similar example is from a woman with visual impairments in India who delayed seeking health services for her poor vision for five years because
my village people told me that, because my mother and mother-in-law died, I cried a lot, and that is the reason there was more water in my eyes. [Citation40]
The same phenomenon also applies to caregivers. For example, the results from Kiling et al. [Citation38] and Lamech et al. [Citation57] both revealed how the lack of information for caregivers can result in neglect, and ultimately more complicated health conditions or even death, for the person with a disability.
The lack of information related to disability both shapes and is shaped by cultural beliefs and attitudes of the communities and those in power, resulting in disability being viewed as separate or unrelated to general healthcare and not a priority. This view is expressed by a woman with disability in South Africa:
I would say because of society’s understanding of disability, because disability is not fully incorporated into our healthcare services. It’s sometimes a ‘stand alone,’ it should actually be part of all healthcare services and you know? And interventions. It shouldn’t be seen as a stand-alone. [Citation42]
In fact, as illustrated by a number of the studies, people with different types of impairments described how they were excluded from health education campaigns or opportunities due to the initiatives only targeting the mainstream, or inclusion of disability being an afterthought [Citation42,Citation43,Citation46,Citation47,Citation49,Citation58]. Common examples included people with visual impairments not being able to see posters, billboards, or read informational pamphlets with health education messages, or people with hearing impairments not being able to hear messages broadcasted via radio or television programs [Citation42,Citation45,Citation48,Citation56]. Other instances involved people with mobility impairments not being invited or told about local meetings, as assisting them to get there would take too much time or effort [Citation46].
Applying the conceptual framework of access to healthcare by Levesque et al. [Citation28], the lack of information acts across most points on the health seeking path: approachability, acceptability, availability and accommodation, and appropriateness dimensions of the supply side determinants and ability to perceive, ability to reach, ability to pay, and ability to engage from the demand side determinants.
Practical and logistical barriers
Practical and logistical barriers relate to the need for planning and organizing the process of accessing primary healthcare services. For anyone, particularly a person with disabilities, this step involves ensuring appropriate resources or supports are in place, when and where needed so that the process of receiving or providing care can occur effectively. In developing this theme, four main codes were identified: (1) availability of resources from the supply side, (2) financial factors, (3) physical environment, and (4) transportation (see ). Some of these barriers are disability specific, depending on the type of impairments experienced. An example here is the absence of ramps for those with certain physical impairments resulting in difficulties entering the building, or lack of sign language interpreters for people with hearing impairment [Citation38,Citation41,Citation45,Citation48,Citation49,Citation54,Citation56–58]. This barrier is illustrated by an example of a person with visual impairment from Kenya, discussing the shortage or lack of sign language interpreters and guidance at the health facility:
Those who don’t talk, those with hearing impairment, you will find that the sign language interpreter maybe is not in the center or he/she is there, but they are alone and maybe they are held up somewhere else. So, there are those who have been complaining that they go to the hospital and they are not treated because maybe the sign language interpreter was not there that day…… Sometimes you will get stranded even before you get to the doctor, you don’t know where you are and you don’t know where to start because you don’t have someone to guide you. So, there should be someone to guide you so that you can get to the doctor. [Citation46]
Some barriers and failures of the system apply to everyone, such as lack of medicines, long wait times, direct and indirect costs. However, these concerns may be more palpable for people with disabilities, due to their impairments and disabled status, and likely overall greater healthcare needs and higher levels of poverty and exclusion. For example, while the lack of resources, such as limited staff, doctors and nurses, can be a general barrier resulting in long wait times, it can further discourage people with disabilities from accessing primary healthcare services, for instance, due to decreased endurance related to their impairment, reliance on special transportation or family support being available only for short periods of time or poor accessibility at the site [Citation39].
The need for help to get to the primary healthcare facility is demonstrated by this quote from a man who is a community stakeholder in South Africa:
Well transport’s number one, and that’s the biggest barrier that we have…Often people aren’t able to make the trip themselves so someone will have to stay out of work to take them. Sometimes children stay out of school to help their, accompany their parents, and parents don’t want to do that. They’d rather their kids go to school so they just don’t go to hospital. [Citation42]
Another woman with visual impairment from Malawi describes:
On my own I cannot walk to the health facility because I cannot see and I have rheumatism. My children cannot carry me on a bicycle because I have dizziness whenever I am put on the bicycle, so this makes me not access formal health care services. [Citation39]
People with disabilities can also face additional costs of transport for the person on either public or private transport [Citation49]. For instance, public transport drivers may charge extra or fail to stop for people with disabilities as they are believed to be too slow or require assistance [Citation46,Citation51]. A person with mobility impairments from Kenya explains:
It’s difficult to use public means of transport because they don’t like putting the wheelchair in the vehicle….it wastes their time carrying it from the ground and putting it on top of the vehicle and then they will have to remove it, it’s difficult, sometimes they are in a hurry to go and transport people. They only agree if we are going long distances…if we are going to a place that costs KES 100 and above or KES 200 that’s when they allow us to board but if it’s a short distance they can’t agree. [Citation46]
Physical barriers, while commonly understood and may appear resolved, can still present as a practical barrier to people with disabilities. For example, even when a healthcare facility has a ramp to enter, access may be limited to various part of the building, requiring planning ahead by people with disabilities. A person with mobility impairment from Kenya describes how she needs to plan how much liquid she consumes to avoid going to the bathroom when accessing healthcare facilities:
If I know am going to the hospital, I don’t drink anything that can make me want to go to the toilet because if I go to the toilet, I will have to leave my wheelchair at the door…the toilet doors are narrow…I don’t use the toilet until I get back home…the small wheelchairs they use in the hospital for patients can fit but I use a tricycle it’s a bit wide it can’t fit through the toilet door….we need toilets with a wide door, also when you enter the toilet seats shouldn’t be low, they should have high toilet seats so that if you enter the toilet you just sit on it and when you are through you go back to the wheelchair. [Citation46]
Another example is when accessible features, such as ramps that are installed are blocked due to misunderstanding or lack of awareness of disability. As one representative from a disabled person organization in Indonesia explained
Because of lack of understanding about the function of the infrastructure for people with disabilities, the misuse happened. For instance, the ramp was covered by motorbikes or the flower pots. [Citation50]
The examples above are only a small sample of practical and logistical barriers faced by people with disabilities when accessing primary healthcare services. These barriers tend to cluster in the middle of the conceptual framework of access to healthcare by Levesque et al., focusing on availability and accommodation, affordability, and appropriateness from the supply side determinants and ability to reach and ability to pay from the demand side determinants [Citation28]. Finally, it is important to note again that many of the barriers in this theme, especially those specific to people with disabilities, originate from either cultural beliefs and attitudinal barriers and information barriers, or both.
Discussion
This meta-synthesis of 41 primary-research qualitative studies, resulted in the identification of three key themes that influence access or act as barriers to primary healthcare services for people with disabilities: Attitudinal and belief system barriers, informational barriers, and practical and logistical barriers. While all the themes are identified as barriers, it is important to note that not all participants in all studies reported barriers related to the above themes. In fact, primary data from some of the studies included reports or examples of positive or enabling experiences [Citation53,Citation56,Citation59–63]. For example in Grut et al’s study in Malawi [Citation56], some participants did not appear to find the attitudes of the healthcare providers a barrier and felt they were given priority when needed.
As demonstrated by the examples and discussed throughout the results, the themes are inter-related and impact one another in a dynamic and complex system of connections, even if the health seeking process, starting with the identification of a healthcare need to completion of the process, may appear linear. The conceptual framework of access to healthcare by Levesque et al. [Citation28] tries to demonstrate this complexity by identifying the various dimensions of accessibility and abilities and their points of intersection with the health seeking process. While insightful, the framework appears to be missing the more dynamic variables related to how these dimensions are influenced by individual aspects and combined consequences of attitudinal and belief system, informational, and practical and logistical variables throughout the entire process.
Like everyone else, people with disabilities’ experiences of and decisions about accessing healthcare start from home where the person or the household needs to make various healthcare choices. According to Levesque et al. [Citation28] the process starts with a health need but whether or not the need is recognized and there is a desire for care is influenced by the ability of the consumers to perceive this need, their decision making autonomy, and the approachability of the providers. These dimensions are shaped by attitudinal and belief system, and informational resources. What this review reveals are that the dimensions of accessibility and capacity, not only in the first step, but throughout the entire process are influenced, though to varying degrees, by the three themes; attitudinal and belief system barriers, informational barriers, and practical and logistical barriers. Intersections between people’s socio-economic status, level of education and gender often further reinforcing some of these barriers.
There are also additional intricacies to consider. For instance, it is difficult to distinguish whether attitudinal and belief system barriers or informational barriers come first. Informational barriers can be particularly challenging for people with disabilities, as they are more likely to be illiterate, due to exclusion from formal education, with links to their type of impairment, gender, poverty, or a combination of factors [Citation4,Citation26]. Unfortunately, even when a person with a disability is educated, many healthcare stakeholders lack the training, skills and knowledge to communicate effectively with them, in particular, with people who have impairments of hearing, understanding, speech or interaction [Citation43,Citation62,Citation64–66].
Another complexity is that people with disabilities may need to make difficult decisions about where to use their limited resources, including when to seek healthcare services, given their often-disadvantaged position in society and related poverty. For example, as demonstrated by the quotes presented, a person with a disability may say that cost or transportation are the main barrier, when in fact underlying this it may be that not enough priority within the family is given to or by the person with disability, to support investment in their health. The combination of scarcity of resources such as money and time, the anticipated stress of dealing with various logistical factors, such as inaccessible public transport system and the excessive costs involved in arranging alternative transportation to seek primary healthcare services may not be deemed worthwhile.
Strengths and limitations of the review
This review has important strengths, in addition to being the first meta-analysis looking at qualitative research focusing on barriers to primary healthcare for persons with disabilities in LMIC. Participants in included studies provided data from three perspectives, those of people with disabilities, their caregivers, and healthcare providers. While the majority of the participants were people with disabilities, the inclusion of the different perspectives from both the demand and supply side did allow for some level of triangulation and validation of results from each perspective, ensuring minimization of gaps in the findings. Furthermore, the inclusion of 41 papers allowed patterns to be drawn across a large set of literature sources, and more insights gained than is possible through single studies. In addition, the studies provided examples from people with a range of impairments living in different regions and contexts globally. However, it is still important to be cautious and limit extrapolation, especially in relation to Latin American countries where data appear to be lacking.
The inclusion criteria were restricted to those articles published in English, and so studies from regions such as Francophone Africa and Spanish/Portuguese Latin America in particular may have been excluded. We also did not have access to the primary data from each study and relied on the reports from the authors in the included studies, which demonstrated considerable variability in their reporting according to their COREQ checklist.
Conclusion
Identification of disability-specific barriers, and the dynamic and cumulative nature of barriers to accessing healthcare services, is important when considering intervention strategies and their potential effectiveness in improving access to primary healthcare services for people with disabilities. Further studies on the decision-making process around accessing primary healthcare and where priorities are placed by consumers can further facilitate the development of interventions to overcome access barriers. Similarly, a more in-depth identification and analysis of the factors that can support healthcare providers’ in better serving the needs of people with disabilities is important, taking into account their day-to-day experiences and demands, and often limited resources.
The results of this review indicate a complex and dynamic interacting system between cultural beliefs and attitudes, informational, and practical and logistical barriers faced by both healthcare providers (supply side) and people with disabilities (demand side) as consumers of primary healthcare services. In order to achieve full health coverage at acceptable quality for people with disabilities, starting with primary healthcare, it is necessary not only to consider the different barriers but also their combined effect on people with disabilities and their families. It is only then that more nuanced, appropriately adapted and effective interventions to improve access to primary healthcare can be designed and implemented.
The experience of the global pandemic with Covid 19 has further highlighted the urgency to develop interventions to improve access to primary healthcare and inclusive services by revealing the challenges faced across various countries in managing the specific healthcare needs of people with disabilities [Citation67].
Supplementary_File_S3.docx
Download MS Word (17.3 KB)Supplementary_File_S2.docx
Download MS Word (19.3 KB)Suplementary_File_S1.docx
Download MS Word (20.7 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- WHO. CONSTITUTION OF THE WORLD HEALTH ORGANIZATION [Internet]. Geneva: World Health Organization; 1984. [cited 2019 Dec 13]. Available from: http://apps.who.int/gb/bd/PDF/bd47/EN/constitution-en.pdf
- Lancet T. The Astana Declaration: the future of primary health care? The Lancet. 2018;392(10156):1369.
- WHO | WHO Congress on Traditional Medicine, 7–9 November 2008, Beijing, China [Internet]. WHO. [cited 2018 Oct 23]. Available from: http://www.who.int/traditional-complementary-integrative-medicine/about/beijing-congress/en/.
- WHO and World Bank. World disability report. Geneva: WHO; 2011.
- United Nations. Convention on the Rights of Persons with Disabilities- Preamble [Internet]. United Nations; 2006. [cited 2019 Aug 20]. Available from: https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities/preamble.html
- Marmot michael. Fair Society Healthy Lives (The Marmot Review) [Internet]. England: Institute of Health Equity; 2010. Available from: http://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review
- Banks M, Polack S. The economic costs of exclusion and gains of inclusion of people with disabilities [Internet]. Cbm, International Center for Evidence in Disability, London School of Hygiene and Tropical Medicine; 2014. p. 83. Available from: http://disabilitycentre.lshtm.ac.uk/files/2014/07/Costs-of-Exclusion-and-Gains-of-Inclusion-Report.pdf.
- Emerson E, Madden R, Graham H, et al. The health of disabled people and the social determinants of health. Public Health. 2011;125(3):145–147.
- Hashemi G, Kuper H, Wickenden M. SDGs, Inclusive Health and the path to Universal Health Coverage. Disabil Global South. 2017;4:1088–1111.
- Froehlich-Grobe K, Jones D, Businelle MS, et al. Impact of disability and chronic conditions on health. Disabil Health J. 2016;9(4):600–608.
- Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health. 2004;94(3):443–445.
- Wilber N, Mitra M, Walker DK, et al. Disability as a public health issue: findings and reflections from the Massachusetts survey of secondary conditions. Milbank Q. 2002;80(2):393–421.
- Australian institute of health and Welfare. Health of Australians with disability: health status and risk factors [Internet]. Canberra: AIHW; 2010. Report No.: 83. Available from: https://www.aihw.gov.au/getmedia/070c288b-8603-4438-86a3-bac43f1845c3/11608.pdf.aspx?inline=true
- Reichard A, Stransky M, Phillips K, et al. Prevalence and reasons for delaying and foregoing necessary care by the presence and type of disability among working-age adults. Disabil Health J. 2017;10(1):39–47.
- Kuper H, Dok AM, Wing K, et al. The impact of disability on the lives of children; cross-sectional data including 8,900 children with disabilities and 898,834 children without disabilities across 30 countries. PLoS One. 2014;9(9):e107300.
- Rotarou ES, Sakellariou D. Inequalities in access to health care for people with disabilities in Chile: the limits of universal health coverage. Critical Public Health. 2017;27(5):604–616.
- National Health Interview Survey (U.S.), National Center for Health Statistics (U.S.), editors. Disability and health in the United States, 2001–2005. Hyattsville (MD): Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2008. 80 p. (DHHS publication).
- Mulumba M, Nantaba J, Brolan CE, et al. Perceptions and experiences of access to public healthcare by people with disabilities and older people in Uganda. Int J Equity Health. 201413(1):76.
- Chun SM, Hwang B, Park J-H, et al. Implications of sociodemographic factors and health examination rate for people with disabilities. Arch Phys Med Rehabil. 2012;93(7):1161–1166.
- Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Arch Phys Med Rehabil. 2004;85(5):749–757.
- Iezzoni LI, McCarthy EP, Davis RB, et al. Mobility impairments and use of screening and preventive services. Am J Public Health. 2000;90(6):955–961.
- Taegtmeyer M, Hightower A, Opiyo W, et al. A peer-led HIV counselling and testing programme for the deaf in Kenya. Disabil Rehabil. 2009;31(6):508–514.
- Bright T, Kuper H. A systematic review of access to general healthcare services for people with disabilities in low and middle income countries. IJERPH. 2018;15(9):1879.
- McColl MA, Jarzynowska A, Shortt SED. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010;25(2):205–218.
- CBM. Inclusion counts - the economic case for disability-inclusive development [Internet]. Bensheim (Germany): CBM; 2016. p. 125. Disability Inclusive Development. Available from: https://www.cbm.org/article/downloads/54741/DID_series_2_-_Inclusion_Counts__coming_soon_.pdf
- Grech S. Disability and poverty in the global south [Internet]. London: Palgrave Macmillan UK; 2015. [cited 2018 Oct 30]. Available from: https://doi.org/https://doi.org/10.1057/9781137307989
- Smith E, Murray S, Yousafzai A, et al. Barriers to accessing safe motherhood and reproductive health services: the situation of women with disabilities in Lusaka, Zambia. Disabil Rehabil. 2004;26(2):121–127.
- Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12(1):18.
- WHO global disability action plan 2014–2021. Better health for all people with disability. [Internet]. WHO; 2015. [cited 2020 Apr 28]. Available from: https://www.who.int/disabilities/actionplan/en/
- Casebolt MT. Barriers to reproductive health services for women with disability in low- and middle-income countries: a review of the literature. Sex Reprod Healthc. 2020;24:100485.
- United Nations Millennium Development Goals [Internet]. [cited 2019 Feb 3]. Available from: http://www.un.org/millenniumgoals/
- World Bank Country and Lending Groups – World Bank Data Help Desk [Internet]. [cited 2018 Nov 8]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(1):45.
- Ingstad B, Whyte SR, editors. Disability in Local and Global Worlds. 1 ed. Berkeley: University of California Press; 2007. 334. p.
- Kiling I, Due C, Li D, et al. Perceptions of disability, environmental risk factors and available services among local leaders and parents of young children with disabilities in West Timor, Indonesia. Disabil Rehabil. 2019;41(20):2421–2432.
- Munthali AC, Swartz L, Mannan H, et al. “This one will delay us”: barriers to accessing health care services among persons with disabilities in Malawi. Disabil Rehabil. 2019;41(6):683–690.
- Zuurmond M, Mactaggart I, Kannuri N, et al. Barriers and facilitators to accessing health services: a qualitative study amongst people with disabilities in Cameroon and India. IJERPH. 2019;16(7):1126.
- Opoku MP, Mprah WK, Mckenzie J, et al. Lives of persons with disabilities in Cameroon after CRPD: voices of persons with disabilities in the Buea Municipality in Cameroon. Int J Disabil Human Dev. 2017;16(1):67–75.
- Hussey M, MacLachlan M, Mji G. Barriers to the implementation of the health and rehabilitation articles of the United Nations Convention on the Rights of Persons with Disabilities in South Africa. Int J Health Policy Manag. 2017;6(4):207–218.
- Chireshe R, Rutondoki EN, Ojwang P. Perceptions of the availability and effectiveness of HIV/AIDS awareness and intervention programmes by people with disabilities in Uganda. Sahara J. 2010;7(4):17–23.
- Aguerre IM, Riley-Powell AR, Weldon CT, et al. “Knocking on doors that don’t open”: experiences of caregivers of children living with disabilities in Iquitos and Lima, Peru. Disabil Rehabil. 2019;41(21):2538–2547.
- Lamptey D-L. Health beliefs and behaviours of families towards the health needs of children with intellectual and developmental disabilities (IDD) in Accra, Ghana. J Intellect Disabil Res. 2019;63(1):12–20.
- Kabia E, Mbau R, Muraya KW, et al. How do gender and disability influence the ability of the poor to benefit from pro-poor health financing policies in Kenya? An intersectional analysis. Int J Equity Health. 2018;17(1):149.
- Soltani S, Takian A, Akbari Sari A, et al. Cultural barriers in access to healthcare services for people with disability in Iran: a qualitative study. Med J Islam Repub Iran. 2017;31:51.
- Mji G, Braathen SH, Vergunst R, et al. Exploring the interaction of activity limitations with context, systems, community and personal factors in accessing public health care services: a presentation of South African case studies. Afr J Prim Health Care Fam Med. 2017;9:1. Available from: https://phcfm.org/index.php/phcfm/article/view/1166
- Chintende GN, Sitali D, Michelo C, et al. Situational analysis of communication of HIV and AIDS information to persons with visual impairment: a case of Kang’onga Production Centre in Ndola, Zambia. BMC Res Notes. 2017;10(1):150.
- Marella M, Smith F, Hilfi L, et al. Factors influencing disability inclusion in general eye health services in Bandung, Indonesia: a qualitative study. IJERPH. 2018;16(1):23.
- Järnhammer A, Andersson B, Wagle PR, et al. Living as a person using a lower-limb prosthesis in Nepal. Disabil Rehabil. 2018;40(12):1426–1433.
- Saulo B, Walakira E, Darj E. Access to healthcare for disabled persons. How are blind people reached by HIV services? Sex Reprod Healthc. 2012;3(1):49–53.
- Kritzinger J, Schneider M, Swartz L, et al. “I just answer ‘yes’ to everything they say”: access to health care for deaf people in Worcester, South Africa and the politics of exclusion. Patient Educ Couns. 2014;94(3):379–383.
- Mprah WK. Perceptions about barriers to sexual and reproductive health information and services among deaf people in Ghana. DCID. 2013;24(3):21.
- Dassah E, Aldersey HM, McColl MA, et al. ‘When I don’t have money to buy the drugs, I just manage.’-Exploring the lived experience of persons with physical disabilities in accessing primary health care services in rural Ghana. Soc Sci Med. 2018;214:83–90.
- Grut L, Sanudi L, Braathen SH, et al. Access to tuberculosis services for individuals with disability in rural Malawi, a qualitative study. Mancinelli S, editor. PLoS One. 2015;10(4):e0122748.
- Lamech N, Raghuraman S, Vaitheswaran S, et al. The support needs of family caregivers of persons with dementia in India: Implications for health services. Dementia (London). 2019;18(6):2230–2243.
- Schenk KD, Tun W, Sheehy M, et al. “Even the fowl has feelings”: access to HIV information and services among persons with disabilities in Ghana, Uganda, and Zambia. Disabil Rehabil. 2020;42(3):335–348.
- Castro SS, Lefèvre F, Lefèvre AMC, et al. Accessibility to health services by persons with disabilities. Rev Saude Publica. 2011;45(1):99–105.
- Ganle JK, Otupiri E, Obeng B, et al. Challenges women with disability face in accessing and using maternal healthcare services in Ghana: a qualitative study. Ginsberg SD, editor. Plos One. 2016;11(6):e0158361.
- Morrison J, Basnet M, Budhathoki B, et al. Disabled women’s maternal and newborn health care in rural Nepal: a qualitative study. Midwifery. 2014;30(11):1132–1139.
- Oliviera Y. d, Celino S. d M, Franca I. d, Pagliuca MF, et al. Accessibility of the deaf person to public health services. J Nurs. 2015;9(Suppl 7):9018–9026.
- Tanabe M, Nagujjah Y, Rimal N, et al. Intersecting sexual and reproductive health and disability in humanitarian settings: risks, needs, and capacities of refugees with disabilities in Kenya, Nepal, and Uganda. Sex Disabil. 2015;33(4):411–427.
- Ahumuza SE, Matovu JK, Ddamulira JB, et al. Challenges in accessing sexual and reproductive health services by people with physical disabilities in Kampala, Uganda. Reprod Health. 2014;11(1):59. [cited 2018 Oct 20]. Available from: https://doi.org/https://doi.org/10.1186/1742-4755-11-59
- Cardoso AHA, Rodrigues KG, Bachion MM. Perception of persons with severe or profound deafness about the communication process during health care. Rev Lat Am Enfermagem. 2006;14(4):553–560.
- Pereira PCA, Fortes PdC. Communication and information barriers to health assistance for deaf patients. Am Ann Deaf. 2010;155(1):31–37.
- Voices of People with Disabilities During the COVID19 Outbreak [Internet]. International Disability Alliance. [cited 2020 Jul 9]. Available from: http://www.internationaldisabilityalliance.org/content/voices-people-disabilities-during-covid19-outbreak
- Van Hees S, Cornielje H, Wagle P, et al. Disability inclusion in primary health care in Nepal: an explorative study of perceived barriers to access governmental health services. DCID. 2015;25(4):99.
- Yousafzai AK, Edwards K, D’Allesandro C, et al. HIV/AIDS information and services: the situation experienced by adolescents with disabilities in Rwanda and Uganda. Disabil Rehabil. 2005;27(22):1357–1363.
- Nixon SA, Cameron C, Hanass-Hancock J, et al. Perceptions of HIV-related health services in Zambia for people with disabilities who are HIV-positive. J Int AIDS Soc. 2014;17(1):18806.
- Morrow M, Arunkumar M, Pearce E, et al. Fostering disability-inclusive HIV/AIDS programs in northeast India: a participatory study. BMC Public Health. 2007;7(1):125. [cited 2018 Oct 20]. Available from: https://doi.org/https://doi.org/10.1186/1471-2458-7-125
- Banks LM, Zuurmond M, Ferrand R, et al. Knowledge of HIV-related disabilities and challenges in accessing care: qualitative research from Zimbabwe. PLoS One. 2017;12(8):e0181144.
- Tun W, Okal J, Schenk K, et al. Limited accessibility to HIV services for persons with disabilities living with HIV in Ghana, Uganda and Zambia. J Int AIDS Soc. 2016;19(5 Suppl 4):20829.
- Vergunst R, Swartz L, Mji G, et al. ‘You must carry your wheelchair’-barriers to accessing healthcare in a South African rural area. Glob Health Action. 2015;8(1):29003.
- Patel P, Baier J, Baranov E, et al. Health beliefs regarding pediatric cerebral palsy among caregivers in Botswana: a qualitative study. Child Care Health Dev. 2017;43(6):861–868.
- Yoshida K, Hanass-Hancock J, Nixon S, et al. Using intersectionality to explore experiences of disability and HIV among women and men in Zambia. Disabil Rehabil. 2014;36(25):2161–2168.
- Hanass-Hancock J, Nene S, Deghaye N, et al. “These are not luxuries, it is essential for access to life”: Disability related out-of-pocket costs as a driver of economic vulnerability in South Africa. Afr j Disabil. 2017;6:1–10.
- Varghese J, Grills N, Mathias K. Barriers in health care access faced by children with intellectual disabilities living in rural Uttar Pradesh. J Soc Inclusion. 2015;6:55–70.
- Orrie S, Motsohi T. Challenges experienced by healthcare workers in managing patients with hearing impairment at a primary health care setting: a descriptive case study. South Afr Family Pract. 2018;60(6):207–211.
- Sermsuti-Anuwat N, Pongpanich S. Perspectives and experiences of Thai adults using wheelchairs regarding barriers of access to dental services: a mixed methods study. Patient Prefer Adherence. 2018;12:1461–1469.
- Soltani S, Takian A, Akbari Sari A, et al. Financial barriers to access to health services for adult people with disability in Iran: the challenges for universal health coverage. Iran J Public Health. 2019;48(3):508–515.
- Mei H, Turale S. Coping experience of health concerns and physical disability for older Chinese people: a qualitative, descriptive study. Nurs Health Sci. 2017;19(4):444–451.
- Alves VF, Cardoso AMR, Cavalcanti YW, et al. Oral health care offered to people with disabilities in the primary health care network: what do dentists say? J Public Health. 2017;25(1):11–17.
- Rooy GV, Amadhila EM, Mufune P, et al. Perceived barriers to accessing health services among people with disabilities in rural northern Namibia. Disabil Soc. 2012;27(6):761–775.