Abstract
Purpose
A major amputation affects the patients’ independence, well-being and HRQoL. However, prosthesis use and the impact on the patient’s HRQoL are scarcely described. The aim was to compare HRQoL between walker and non-walker amputees. Secondary aim was to evaluate prosthesis use and habits.
Method
Ninety-eight patients with a major amputation due to peripheral arterial disease were included during 2014–2018. They were interviewed using EQ-5D-3L (HRQoL), Stanmore Harold Wood mobility grade (prosthesis use) and Houghton scale (prosthesis habits).
Results
Seventy-three patients completed the one-year follow-up, out of them 56 got a prosthesis. Twenty-three used it to walk both inside and outside. EQ-5D-3L at follow-up was increased in all patients in comparison to baseline (0.16 versus 0.59, p < 0.001). Patients walking with prosthesis had the largest improvement (0.12 versus 0.78, p < 0.001). A sub-analysis aiming to study the importance of independent movement showed an improved HRQoL at follow-up among those classified as prosthesis-user (p<0.001) and walker (p<0.001), but not among non-prosthesis users (p = 0.245).
Conclusion
Learning how to use, not exclusively to walk with, a prosthesis after an amputation is important for the patients’ HRQoL. At follow-up, patients using their prosthesis to walk or to move to a wheelchair, showed an improved HRQoL compared to baseline.
Walking ability with a prosthesis is important for the patient’s perceived HRQoL after an amputation.
Rehabilitation of amputees should focus on independence and movability and not only on walking ability.
Wider use of prescribing prostheses after an amputation also to those predicted as non-walkers, may increase the number of patients with independence and improved HRQoL.
When using their prosthesis for independent movement, patients who were otherwise unable to walk due to their amputation were able to achieve HRQoL comparable to walking amputees.
IMPLICATIONS FOR REHABILITATION
Introduction
In Europe, 90% of the major lower limb amputations are performed in patients with the peripheral arterial disease (PAD) [Citation1]. PAD is divided into three stages: asymptomatic disease, intermittent claudication, and critical limb ischemia. Critical limb ischemia, defined as chronic ischemic rest pain or non-healing ulceration or gangrene, is the most severe form, and most of the patients who underwent an amputation have this stage [Citation2]. Patients with critical limb ischemia is a patient group with multiple chronic co-morbidities, especially diabetes and cardiovascular disease [Citation3]. The mortality is 16–35% in the first year after being diagnosed with critical limb ischemia, and it seems to continue at the same level [Citation4,Citation5]. PAD is a disease with a large impact on the patient’s Health-Related Quality of Life (HRQoL) as it is associated with a high risk of lower extremity amputation, morbidity, and death [Citation6–8]. It is a disease associated with a lower HRQoL in comparison with the general population, and revascularization may improve the patient’s perceived health status [Citation9–10]. Primary amputation is a treatment alternative, often decided when no other treatment is possible, and many times associated with intense anxiety. However, amputation may bring about a better outcome in perceived HRQoL than repeated revascularization attempts with little likelihood of wound healing [Citation11,Citation12].
Mobility is one of the most important factors for good HRQoL after an amputation. Limited functional status decreases the patient’s possibility to return to an independent life [Citation13,Citation14]. The association between mobility, use of a prosthesis, and perceived HRQoL among those amputated due to peripheral arterial disease is largely unknown. Previous studies on amputees often consist of patients referred to a rehabilitation ward, resulting in a selection of healthier patients, more likely to be prosthesis users [Citation15]. Additionally, to receive a prosthetic limb is not necessarily the same as using it, thus patients with a prosthesis show a large variation in usage time [Citation16].
HRQoL has become an important patient-related outcome measure particularly in chronic diseases affecting the patient’s independence and well-being. The concept has been defined in different ways but the most common is based on the person’s ability to be self-determined and independent with control of the disease processes. The concept also measures the individual’s own perception of satisfaction with life and a sense of psychological, physical, and social well-being [Citation17].
The aim of the study was to compare the HRQoL between walker and non-walker amputees after a major amputation due to peripheral arterial disease. The secondary aim was to evaluate prosthesis use and habits after major amputation.
Material and methods
This is a single centre prospective cohort study of patients undergoing a major amputation due to PAD during 2014 − 2018 in a catchment area covering half of the population of Stockholm county (a region with a total population of 2.2 million). The primary outcome was prosthesis use and its impact on the patient’s HRQoL. The Regional Ethics Committee of Stockholm, Sweden approved the study (No. 2014-801-31/1). The study was registered in Clinical Trials.gov ID NCT03570788.
Sample and setting
All patients planned for amputation at Södersjukhuset, Stockholm, Sweden from 12 September 2014 to 31 May 2018 were prospectively reviewed when scheduled for surgery. Inclusion criteria were patients undergoing a primary major amputation on the tibial, knee, or femoral level due to peripheral arterial disease, where revascularization was not possible or had failed. Patients not able to provide informed consent, verbally express their experience of the amputation or not Swedish speaking were excluded.
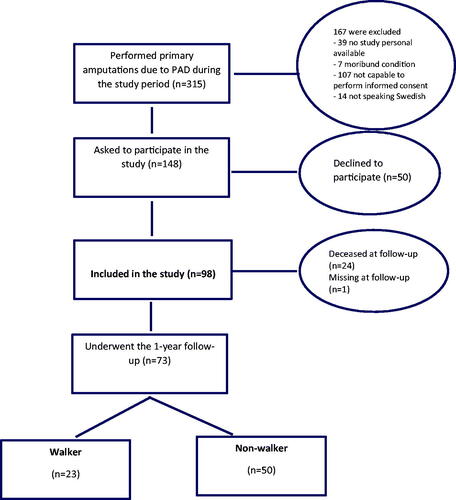
During the study period, 315 patients underwent a primary major amputation due to peripheral arterial disease. Two hundred and seventeen patients were excluded, so in total 98 were included in the study. Out of them, 73 patients completed the one-year follow-up (). Follow-up data for the last included patient were collected on 20th May 2019.
Data collection
Baseline data were collected via in-person interviews (ET) at the hospital ward in connection with the amputation and included measures of perceived HRQoL and the functional level the week before the amputation. Data on co-morbidity and perioperative characteristics of the patients who completed the one-year follow-up were retrieved by a chart review (). All baseline data of EQ-5D-3L started with the following sentence “In the following questions, I am asking you about the week before the amputation.”
Table 1. Baseline characteristics of patients that completed follow-up (n = 73).
Follow-up at 12 months after amputation was performed via phone interviews by the same researcher (ET). HRQoL was measured using the EQ-5D-3L. All patients who had received a prosthesis were asked questions regarding their walking ability and prosthetic wearing habits according to the Stanmore mobility grade [Citation18] and the Houghton scale [Citation19]. In addition, all patients were asked questions regarding their opinion on the importance of walking ability. Follow-up was performed via proxy in two patients, where a caregiver involved in the patient’s daily care answered the questions [Citation20].
Major amputation was defined as a primary amputation above the ankle.
Outcome measures and endpoints
The primary outcome was HRQoL according to the EQ-5D-3L questionnaire [Citation21] 12 months after amputation. The secondary outcome was prosthesis use and habits 12 months after amputation. A patient was regarded as a walker if they used their prosthesis to walk both inside and outside (>4 on Stanmore Harold Wood Mobility grade).
The questionnaires
The questionnaire used in the study was the EQ-5D-3L [Citation21]. The semi-structured interview of prosthesis-use and wearing habits was based on the Stanmore Harold Wood mobility grade [Citation18] and the Houghton scale [Citation19].
EQ-5D-3L
EQ-5D-3L is a widely used generic instrument with five health dimensions: mobility, self-care, usual activity, pain/discomfort, and anxiety/depression. Each dimension is measured on a three-point Likert-scale (1 = no problems, 2 = some problems or 3 = extreme problems). The five dimensions can be converted into a summary index (EQ-5D-3L index), to describe a health status profile. The index-score ranges from 1 (no problems with any of the dimensions) to −0.594 (extreme problems with all five dimensions) [Citation21] and is derived from a representative sample of the general population in the United Kingdom [Citation22]. The EQ-5D-3L instrument is validated for the Swedish language and Swedish context [Citation23].
Stanmore Harold Wood mobility grade
We used the Stanmore Harold Wood mobility grade [Citation18] to quantify prosthesis use. The self-reported questionnaire is designed for patients with lower limb amputations and containing one question; “How is the grade of your mobility?” with six grades of mobility (Supplementary S1). We defined walking ability as Stanmore Harold Wood mobility grade four (walks indoors and outdoors) or higher, and prosthesis use as grade two or three. The reason to use this definition was that we had a presumption that being able to walk outdoors, and not only in their home, was an important factor for their HRQoL.
The motivation to use the Stanmore Harold Wood mobility grade was that we believe that it is necessary to use an instrument with few questions as this is a fragile patient group. The scale is suited for telephone interviews and is frequently used, even though it is not validated.
Houghton scale
The Houghton scale is a self-reported validated questionnaire capturing prosthetic wearing habits among patients with lower limb amputation [Citation19,Citation24]. The questions are “How much time are you using your prosthesis,” “When do you use the prosthesis,” and “Do you use walking aids or similar tool?”, with four response categories ranging from 0–3 (Supplementary S2). The fourth question in the instrument was excluded in this study in accordance with results from a validation study [Citation24]. The scale was used to describe the wearing habits among those who had a prescribed prosthesis and were using it at the 12 months follow-up (n = 53, ).
Table 2. Characteristics wearing habits of the prosthesis, according to Houghton scale, n = 53.
Statistical analysis
Baseline differences in categorical variables were evaluated with Pearson’s Chi-square test. Continuous variables with normal distribution were presented with mean and standard deviation (SD), and non-normal distribution with median and interquartile range (IQR). The Mann–Whitney U test was used to compare differences in EQ-5D-3L domains and health status between walker and non-walker amputees (with eta-square as effect size measure) choosing this statistical method since data were on the ordinal level. Bonferroni’s post-hoc test for multiple comparisons was used (p = 0.008) [Citation25]. A two-way analysis of variance (ANOVA) was performed to explore differences between HRQoL and the outcome walker versus non-walker.
The analysis of baseline characteristics and HRQoL was performed on the subsample of patients completing the 12 months follow-up. The analysis of prosthesis use was performed on the cohort that had a prosthesis prescribed. A two-tailed p-value < 0.05 was considered significant. Analyses were performed with IBM SPSS statistics version 25 (IBM Inc., Chicago, IL) and in R statistical analyses, version 3.4.3 (Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org).
Result
Perioperative characteristics
In total, 98 of 315 patients were included in the study (). Most of the patients were men and had severe comorbidities (ASA class 3 or 4 [Citation26]). Half of the patients had undergone a vascular intervention prior to the amputation. A majority of the patients had a transtibial amputation, 13 patients had a contralateral amputation prior to the study (Supplementary S3).
Male sex and lower age were more common among those who walked with a prosthesis at follow-up. Ambulatory status prior to amputation was strongly associated with prosthesis use. Almost all of those who walked independently prior to amputation were classified as walkers at follow-up. A quarter of those that where wheelchair-bound prior to amputation also learned to use the prosthesis for independent movement for example to a wheelchair ().
Prosthesis use and habits
Of the 73 patients who completed the follow-up, 56 had a prosthesis, and 53 patients used it at follow-up. Nearly half of those who wore their prosthesis at follow-up were able to walk both indoors and outdoors and were thereby categorized as walkers (Stanmore four to six). Among patients categorized as prosthesis users (Stanmore two or three), nine were wheelchair-bound and eight used walking aids indoors. There was a large difference in wearing habits between the patients, half of them (n = 27) used their prosthesis less than 3 h a day, while a third (n = 16) used it more than 12 h a day. Nearly all of the patients that used their prosthesis to walk had an assistive device, where two crutches or a walker were most common ().
Outcome of HRQoL
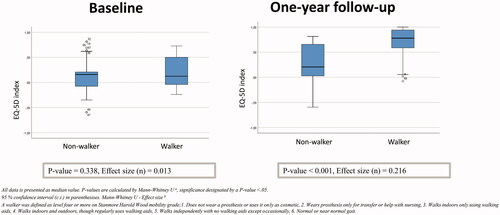
Most patients estimated their overall health status as better at follow-up compared to the week before their amputation. The median value in the EQ-5D-3L index for all patients (n = 98) at baseline was 0.16 (IQR: −0.46 to 0.54). The patients who completed the 12 months follow-up (n = 73) had a median value of 0.59 (IQR: 0.07 to 0.73).
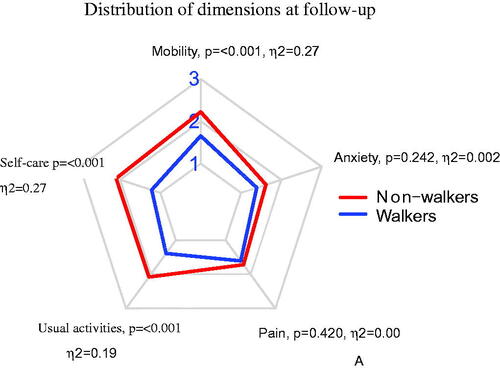
At baseline, “mobility” and “pain/discomfort,” were the dimensions where most patients reported health problems (94% and 89%, respectively). At follow-up, most patients still reported problems for the dimension “mobility” (89%), while there were fewer patients who reported problems with pain (50%). In comparison to those classified as walkers at follow-up, the non-walkers reported lower estimates on mobility (p < 0.001), role activity (p < 0.001), and self care (p < 0.001). There was no difference between the groups in the pain (p = 0.420), and anxiety (p = 0.242) domains ( and ).
Figure 2. Dimensions of EQ-5D-3L at baseline between walker and non-walker amputees. Median values with p-values based on Mann–Whitney U test with eta square as effect size (η2). Higher value indicates more severe problem.
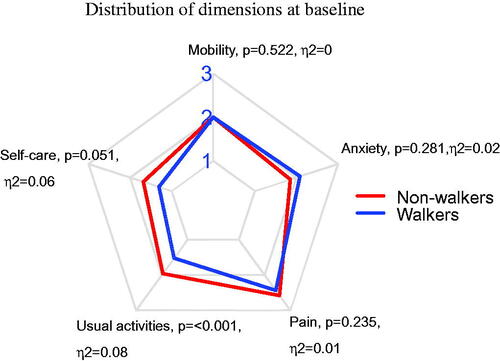
Figure 3. Dimensions of EQ-5D-3L at follow-up between walker and non-walker amputees. Median values with p-values based on Mann–Whitney U test with eta square as effect size (η2). Higher value indicates more severe problem.
The majority of those who reported extreme problems with anxiety/depression at baseline also reported problems with severe pain/discomfort (80%). At follow-up, we could not see that association.
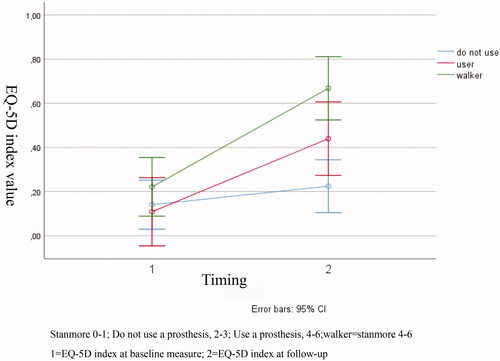
At baseline, there were no differences in EQ-5D-3L index-score between those classified as walkers 0.12 (IQR: −0.04 to 0.55) compared to non-walkers 0.16 (IQR: −0.08 to 0.22), (p = 0.338). Both groups had an increased EQ-5D-3L index-score at follow-up (p < 0.05) compared to their baseline measure (). Those who used their prosthesis to walk had an increased improvement of HRQoL during the study period when compared to non-walkers (F(0.611, 71.000) = 7.985, p = 0.006, partial η2 = 0.101).
To study if the ability to use a prosthesis had an impact on the HRQoL, we performed a prespecified sub-analysis between those classified as a non-user (Stanmore Harold Wood 0–1), a prosthesis-user (Stanmore Harold Wood 2–3) or a walker (Stanmore Harold Wood 4–6). We found no differences in the perceived HRQoL between the groups at baseline (p = 0.139). At follow-up, HRQoL was improved among those classified as a prosthesis-user (p < 0.001) and walker (p < 0.001), while in the group with non-prosthesis user there was no difference in HRQoL between baseline and follow up (p = 0.245). The difference in improvement between the three groups was not statistically significant ().
Differences between men and women
Male sex was associated with a higher chance of being a walker, (43% for men versus 14% for women, p = 0.008). There were no differences between men and women in age (p = 0.961), ASA class (p = 0.145), mortality (p = 0.402), preoperative ambulatory status (p = 0.962), or having had a contralateral amputation prior to inclusion in the study (p = 0.140). Having a transtibial amputation was more common among men (86 versus 76%, p = 0.014). There were no differences at baseline in EQ-5D-3L index-score, 0.39 for men versus 0.34 for women (p = 0.363). However, at follow-up men rated a higher index value than women, 0.42 versus 0.32 (p = 0.020, η2 = 0.075). At baseline, mobility was the only dimension where men and women reported differences (p = 0.01). Almost all men, 98%, reported that they had some problems with mobility, while 14% of the women reported no problem, 76% reported some problems and 10% reported extreme problems. We could not find any differences between men and women at follow-up.
Discussion
This study of patients amputated due to PAD showed that it is important for the patient’s perceived HRQoL to learn to use a prosthesis. One interesting finding was that we saw an improvement in HRQoL even for those who only used their prosthesis to move, for example to a wheelchair. To be independent and not need to rely on others is important for the patient’s experienced HRQoL [Citation13].
Most patients reported problems at baseline in the dimension “mobility” and “pain/discomfort,” Mobility was still a problem at follow-up, while fewer patients perceived problems from pain/discomfort. We found a difference at follow-up between those classified as a walker versus non-walker, in the domain’s ability to move, self-care, and role activity. These findings are probably an explanation of the differences in perceived HRQoL between the groups as those dimensions contribute to a feeling of independence.
Being able to walk with a prosthesis explained 20% of the total difference in index-score at follow-up. An earlier study of the minimally important clinical difference in EQ-5D-3L in patients with chronic pain suggested that differences at 10% or more had a clinical benefit [Citation27]. As most of the patients undergoing an amputation due to PAD are affected with severe pain, we believe that the results from patients’ experiencing chronic pain are transferable. Additionally, when taking the confidence interval into account, the patients classified as a walker had an increased index-score of more than 10% when compared to the non-walkers, indicating that prosthesis use has a clinical effect.
Two-thirds of the patients in our study who completed the one-year follow-up have prescribed a prosthesis. Of these, only half of the patients used it to walk other than at the prosthetic centre or to move to their wheelchair, however, we saw an improvement in HRQoL at follow-up even for those who only used their prosthesis to move, for example to a wheelchair. This supports the idea that it is important for the patients’ independence to be able to use the prosthesis to stand. Earlier studies have also pointed out that wheelchair mobility has an important role in the rehabilitation programme for amputees [Citation16,Citation28]. Based on these results, we recommend that the patient’s ability to learn independent movement, and not only their ability to learn to walk, should be considered when deciding which patients will be prescribed a prosthesis. A generous prescription of prostheses and rehabilitation after amputation will give the patient a chance to learn to use the prosthesis and thereby improve his/her HRQoL.
Amputation below the knee has been found to optimize the patient’s likelihood of learning to walk, as walking with a BKA requires less energy in comparison to an AKA [Citation29]. However, we could not find any significant differences in prosthesis use among those having had a BKA compared to an AKA (p = 0.470). This may be explained by the fact that our cohort consisted of 80% having had a BKA, which is higher than in previous studies [Citation30]. Another explanation may be that most of the performed studies consist of patients referred to a rehabilitation ward, while we included our patients in connection with their amputation, giving a non-selected population [Citation31].
To measure prosthesis use in an elderly population has difficulties. A walking test that measures the distance may be preferable as it is an objective method [Citation32], however, it does not measure the patient’s ability to walk over time. One week a patient uses walking aids and next week they must use a wheelchair as their physical conditions have changed or due to problems with their prosthesis or amputation stump [Citation33]. Another disadvantage with a walking test is that it demands a visit to a clinic which could lead to problems with drop out from the study.
The use of a subjective self-reported scale such as the Stanmore Harold Wood mobility grade [Citation18], may be affected by the patient’s subjective experience of prosthetic use. One patient may have an experience that they walk independently and can perform what they wish, yet another patient with the same clinical status may experience impaired walking ability which affects his/her everyday life. On the other hand, the definition of HRQoL that we used refers to the patient’s appraisal and satisfaction with their current level of functioning and we believe this is an important measure [Citation34].
We found that there were differences between prosthetic use and men and women. That is in line with an earlier study of the impact of gender on prosthetic fit rates that showed a higher amount of prosthesis use among men compared to women (p = 0.001) [Citation35]. Similar to our result, they found that having a transtibial amputation was more common in men which may contribute to the higher number of walkers in this group. However, as the main focus of our study was not differences between men and women, we do not have sufficient data to draw any conclusions, and there is a risk of selection bias as there were more men than women who participated in the study. We, therefore, recommend further studies with this aim.
An earlier study of patients amputated due to PAD found that patients who had undergone an amputation had a decreased HRQoL when compared to the general population norm in the United Kingdom [Citation36]. However, a more relevant measure maybe if the patient perceives an improvement from the time before the amputation, as has been shown in this study.
Instruments used when measuring HRQoL can be either generic with a broader perspective on health targeting a non-specific patent group or disease/condition specifically developed and relevant only for a specific disease or condition. The recommendation within HRQoL research is to use a combination of both for a more complete and nuanced description of the patient’s situation [Citation37]. The EQ-5D-3L questionnaire was considered suitable as it includes the domains mobility, pain, and mental health concerns which have been identified as important factors with an impact on the HRQoL in patients amputated due to peripheral arterial disease [Citation13]. The use of a generic instrument to measure the perceived HRQoL entails the result to be compared with other populations, but there is a risk that it does not identify factors specific for patients who have been amputated. Unfortunately, there is no validated condition-specific HRQoL-instrument for amputees including both wheelchair-bound and those who walk with a prosthesis. Therefore, we recommend further research aiming to develop such an instrument, aiming to increase the specificity and sensitivity [Citation38–39].
Limitations
Research within this frail population is a challenge. Except for 24 patients who died before follow-up, only one patient was missing, resulting in a very high response rate (74%) compared to other studies of cohorts including patients amputated due to PAD (43–66%) [Citation35,Citation40,Citation41]. The generalizability of the study must be discussed as only 52% of the patients who were eligible for the study were included. However, there were no differences in baseline characteristics between the groups, except for a higher number of men among those included in the study. The wide inclusion criteria may also affect the generalizability as a patient with a transtibial amputation has different mobility potential than one with a transfemoral amputation. However, one of the intentions of the study was to provide data on a non-selected population, giving a broader knowledge of the outcome after an amputation. Sub analyses for different confounding factors would provide better information, however, it would take a very long time to get enough patients for sufficient power for the analysis.
Increasing age and cognitive impairment in a population are factors that contribute to missing data and may have an impact on the reliability of the study [Citation42]. To reduce this possible source of error, all questionnaires were filled in during the interviews, in order to clarify any difficulties with the questions asked.
As this is an observational study with a long follow-up, there may be confounding factors that affect the results. However, we believe that a long follow-up is important to be able to see differences in HRQoL, as this is a patient group that often needs re-operations and has a long rehabilitation period. In addition, all patients in the study were offered the same kind of rehabilitation and support.
At the time for planning and designing the study, the Swedish version of EQ-5D-5L was not widely used and therefore the 3L-version was chosen. It is possible that the 5L version would have given further information as it is developed with the aim to be more sensitive and to reduce ceiling effects, as compared to the EQ-5D-3L.
The Stanmore Harold Wood mobility grade is not a validated instrument which is a limitation [Citation33]. However, as it can be used among those who have a prosthesis but do not use it to walk every day, it suited our aim. To increase validity, we used the Houghton scale to describe the patient’s prosthetic-wearing habits [Citation19].
When we designed the study, we had a presumption that being able to walk outside would be the most important factor for perceived HRQoL. Our result shows that it might have been better to also include those that used their prosthesis to walk inside into the walking group, as the independent movement was an important factor for the patient’s HRQoL. However, when performing a subanalysis that included walking inside with a prosthesis into the walker group, the results were identical. Therefore, the original definition is kept.
At follow-up, the patients used different kinds of assistive devices, which may affect their ability to learn to walk. However, in Sweden, all devices are provided for free and are equal in quality and functionality. So, as it was the patients who decided which assistive device they thought worked best for them, we believe that this has not been a major contributor to the result.
Conclusion
Patients who walked or were able to use their prosthesis for independent movement to for example a wheelchair had an improved level of HRQoL one year after their amputation. Our findings indicate that it is important that rehabilitation centres also support non-walking mobility in order to improve the patient’s independence. A generous prescription of prostheses and rehabilitation after amputation will increase the patient’s possibilities to learn to use the prosthesis and thereby increase his/her HRQoL.
Supplementary_Material.docx
Download MS Word (17.3 KB)Acknowledgements
We thank Mikael Andersson Franko for his help with the statistics. We also want to thank all the patients who have participated in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Unwin N. Epidemiology of lower extremity amputation in centres in Europe, North America and East Asia. Br J Surg. 2000;87(3):328–337.
- Elsayed S, Clavijo LC. Critical limb ischemia. Cardiol Clin. 2015;33(1):37–47.
- Abu Dabrh AM, Steffen MW, Undavalli C, et al. The natural history of untreated severe or critical limb ischemia. J Vasc Surg. 2015;62(6):1642–1651.
- Fridh EB, Andersson M, Thuresson M, et al. Amputation rates, mortality, and pre-operative comorbidities in patients revascularised for intermittent claudication or critical limb ischaemia: a population based study. Eur J Vasc Endovasc Surg. 2017;54(4):480–486.
- Reinecke H, Unrath M, Freisinger E, et al. Peripheral arterial disease and critical limb ischaemia: still poor outcomes and lack of guideline adherence. Euro Heart J. 2015;36(15):932–938.
- Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015;116(9):1509–1526.
- Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with Peripheral arterial disease. N Engl J Med. 1992;326(6):381–386.
- Engelhardt M, Bruijnen H, Scharmer C, et al. Prospective 2-years follow-up quality of life study after infrageniculate bypass surgery for limb salvage: lasting improvements only in non-diabetic patients. Euro J Vasc Endovasc Surg. 2008;36(1):63–70.
- Forbes JF, Adam DJ, Bell J, BASIL trial Participants, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: health-related quality of life outcomes, resource utilization, and cost-effectiveness analysis. J Vasc Surg. 2010;51(5):43S–51S.
- Wu AZ, Coresh J, Selvin E, et al. Lower extremity peripheral artery disease and quality of life among older individuals in the community. JAHA. 2017;6(1):1–8.
- Nehler MR, Peyton BD. Is revascularization and limb salvage always the treatment for critical limb ischemia? J Cardiovasc Surg. 2004;45(3):177–184.
- Conte MS, Bradbury AW, Kolh P, GVG Writing Group for the Joint Guidelines of the Society for Vascular Surgery (SVS), European Society for Vascular Surgery (ESVS), and World Federation of Vascular Societies (WFVS), et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur J Vasc Endovasc Surg. 2019;58(1S):S1–S109.
- Suckow BD, Goodney PP, Nolan BW, et al. Domains that determine quality of life in vascular amputees. Ann Vasc Surg. 2015;29(4):722–730.
- Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthet Orthot Int. 2011;35(1):90–96.
- Fortington LV, Rommers GM, Geertzen JH, et al. Mobility in elderly people with a lower limb amputation: a systematic review. J Am Med Dir Assoc. 2012;13(4):319–325.
- Davies B, Datta D. Mobility outcome following unilateral lower limb amputation. Prosthet Orthot Int. 2003;27(3):186–190.
- Theofilou P. Quality of life: definitions and measurement. EJOP. 2013;9(1):150–162.
- Hanspal RS, Fisher K. Prediction of achieved mobility in prosthetic rehabilitation of the elderly using cognitive and psychomotor assessment. Int J Rehabil Res. 1997;20(3):315–318.
- Houghton AD, Taylor PR, Thurlow S, et al. Success rates for rehabilitation of vascular amputees: implications for preoperative assessment and amputation level. Br J Surg. 1992;79(8):753–755.
- Davis JC, Hsiung GY, Bryan S, et al. Agreement between patient and proxy assessments of quality of life among older adults with vascular cognitive impairment using the EQ-5D-3L and ICECAP-O. PLoS One. 2016;11(4):e0153878.
- Williams A. EUROQOL – a new facility for the measurement of health-realted quality-of life. Health Policy. 1990;16(3):199–208.
- Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095–1108.
- Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res. 2001;10:621–635.
- Devlin M, Pauley T, Head K, et al. Houghton Scale of prosthetic use in people with lower-extremity amputations: reliability, validity, and responsiveness to change. Arch Phys Med Rehabil. 2004;85(8):1339–1344.
- Dunn OJ. Multiple comparisons among means. J Am Stat Assoc. 1961;56(293):52–64.
- Doyle DJ, Garmon EH. American Society of Anesthesiologists Classification (ASA Class). Treasure Island (FL): StatPearls Publishing LLC.; 2019.
- Coretti S, Ruggeri M, McNamee P. The minimum clinically important difference for EQ-5D index: a critical review. Expert Rev Pharmacoecon Outcomes Res. 2014;14(2):221–233.
- Larsson B, Johannesson A, Andersson IH, et al. The Locomotor Capabilities Index; validity and reliability of the Swedish version in adults with lower limb amputation. Health Qual Life Outcomes. 2009;7(1):44.
- Sansam K, O’Connor RJ, Neumann V, et al. Clinicians’ perspectives on decision making in lower limb amputee rehabilitation. J Rehabil Med. 2014;46(5):447–453.
- Johannesson A, Larsson GU, Ramstrand N, et al. Incidence of lower-limb amputation in the diabetic and nondiabetic general population: a 10-year population-based cohort study of initial unilateral and contralateral amputations and reamputations. Diabetes Care. 2009;32(2):275–280.
- Taylor SM, Kalbaugh CA, Blackhurst DW, et al. Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg. 2005;42(2):227–235.
- Condie E, Scott H, Treweek S. Lower limb prosthetic outcome measures: a review of the literature 1995 to 2005. Proc Am Acad Orthot Prosthet. 2006;18(6):P13–P45.
- Rommers GM, Vos LD, Groothoff JW, et al. Mobility of people with lower limb amputations: scales and questionnaires: a review. Clin Rehabil. 2001;15(1):92–102.
- Cella DF, Cherin EA. Quality of life during and after cancer treatment. Compr Ther. 1988;14(5):69–75.
- Davie-Smith F, Paul L, Nicholls N, et al. The impact of gender, level of amputation and diabetes on prosthetic fit rates following major lower extremity amputation. Prosthet Orthot Int. 2017;41(1):19–25.
- Davie-Smith F, Paul L, Stuart W, et al. The influence of socio-economic deprivation on mobility, participation, and quality of life following major lower extremity amputation in the west of Scotland. Eur J Vasc Endovasc Surg. 2019;57(4):554–560.
- Patrick DL, Deyo RA. Generic and disease-specific measures in assessing health status and quality of life. Med Care. 1989;27(3):217–232.
- Davie-Smith F, Coulter E, Kennon B, et al. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: a systematic review of the literature. Prosthet Orthot Int. 2017;41(6):537–547.
- Chen TH, Li L, Kochen MM. A systematic review: how to choose appropriate health-related quality of life (HRQOL) measures in routine general practice? J Zhejiang Univ Sci B. 2005;6(9):936–940.
- Madsen UR, Baath C, Berthelsen CB, et al. Age and health-related quality of life, general self-efficacy, and functional level 12 months following dysvascular major lower limb amputation: a prospective longitudinal study. Disabil Rehabil. 2019;41(24):2900–2910.
- Fortington LV, Dijkstra PU, Bosmans JC, et al. Change in health-related quality of life in the first 18 months after lower limb amputation: a prospective, longitudinal study. J Rehabil Med. 2013;45(6):587–594.
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol. 2005;58(1):13–19.