Abstract
Purpose
To examine whether nurse-led stroke aftercare is beneficial for long-term psychosocial outcome of community-dwelling persons with stroke.
Materials and methods
Comparative effectiveness research design in which a prospective stroke aftercare cohort (n = 87) was compared to care-as-usual (n = 363) at six- and 12-months post stroke. Changes over time in cognitive and emotional problems experienced in daily life, fatigue and stroke impact on daily life were examined for stroke aftercare only. Multilevel modelling was used to compare stroke aftercare to care-as-usual concerning anxiety and depression symptoms, social participation and quality of life, over time.
Results
Sample characteristics did not differ between cohorts except for stroke type and on average, more severe stroke in the stroke aftercare cohort (p < 0.05). Following stroke aftercare, anxiety and emotional problems decreased significantly (p < 0.05), whereas care-as-usual remained stable over time in terms of anxiety. No significant changes over time were observed on the other outcome domains.
Conclusions
Nurse-led stroke aftercare showed to be beneficial for emotional well-being in comparison to care-as-usual. Providing psychoeducation and emotional support seem effective elements but adding other therapeutic elements such as self-management strategies might increase the effectiveness of nurse-led stroke aftercare.
Routine stroke follow-up care should pay attention to psychosocial and emotional outcome in a systematic manner, in addition to secondary prevention.
Healthcare professionals such as (specialized) nurses are needed to appropriately address the hidden cognitive and emotional consequences of stroke.
Providing psychoeducation and emotional support in stroke aftercare diminish insecurities and worries in community-dwelling persons with stroke, leading to better outcomes.
Implications for rehabilitation
Introduction
Stroke is one of the most disabling chronic conditions worldwide [Citation1] as it can cause people to suffer from long-lasting physical problems [Citation2], cognitive impairment [Citation3], emotional difficulties [Citation4] and fatigue [Citation5]. Moreover, these long-lasting consequences affect participation in the community and quality of life [Citation6,Citation7].
The majority of stroke patients are discharged home from the hospital or inpatient rehabilitation services [Citation6,Citation8]. At home, the real confrontation with the lasting consequences of stroke starts [Citation9]. Moreover, problems with cognition or emotional functioning are not directly visible to the eye and therefore considered to be “hidden.” When “hidden” problems remain unrecognized this can lead to social distress [Citation10]. Feelings of uncertainty disrupt the transition to home and persons with stroke continue to need information and individualized support from healthcare professionals [Citation11].
Current routine follow-up care is mostly focused on secondary prevention or on neurological symptoms in the first weeks post stroke [Citation12]. Consequently, the long-lasting psychosocial problems are insufficiently addressed by current routine follow-up care [Citation13]. Research has shown that additional efforts are needed to improve healthcare services for persons with stroke. Next to being aware of psychosocial problems, suggested improvements include timely and relevant provision of psychoeducation, and continuity of support by improving active follow-up in primary healthcare [Citation14].
Effective follow-up care addressing emotional and psychosocial outcome at home after stroke are scarce [Citation15] and when effective, mostly involve extensive follow-up models such as home-based rehabilitation [Citation16]. However, the majority of the stroke population experiences mild problems which need less extensive interventions, as described by the stepped-care model [Citation17]. Moulaert et al. [Citation18] showed clinically relevant psychosocial improvement in early stages after cardiac arrest after one or two face-to-face consultations. In their intervention, specialized nurses provided cognitive and emotional screening, psychoeducation, promoted self-management strategies and referred to specialist care when needed [Citation18]. Moreover, nurses have been shown to provide the same, or better, quality of care in primary care settings than physicians, leading to an increase in patients’ satisfaction [Citation19]; all at the level of affordable care [Citation20].
This study examined whether nurse-led stroke aftercare at six months after hospital admission, is beneficial for the long-term psychosocial outcome of community-dwelling persons who suffered from stroke or transient ischemic attack. We compared the outcomes after stroke aftercare to care-as-usual [Citation21], which enabled us to discuss whether stroke aftercare showed to be a valuable addition to routine follow-up care. Based on the results of the study of Moulaert et al. [Citation18], we hypothesized that this nurse-led stroke aftercare is beneficial for the psychosocial outcome of community-dwelling persons with stroke.
Materials and methods
Design
The current study used a comparative effectiveness research design in which stroke aftercare was compared to care-as-usual.
Participants
Stroke aftercare
The stroke aftercare study took place between November 2016 and December 2017 during which persons with stroke (≥18 y) were prospectively included. Persons were invited to visit stroke aftercare if they suffered from either ischemic or hemorrhagic stroke, or suffered from a transient ischemic attack and were hospitalized. All were discharged home or to rehabilitation care after visiting the emergency department or hospitalization. Persons were not invited to stroke aftercare if they: (1) were discharged to a nursing home or (2) were discharged to a region outside Maastricht-Heuvelland. Additional exclusion criteria for participating in this stroke aftercare study were: (1) insufficient command of the Dutch language to complete questionnaires or (2) no legal competency.
Care-as-usual
The care-as-usual cohort was part of the multicenter, longitudinal, prospective Restore4stroke cohort in which persons with stroke were recruited and followed for up to two years post stroke [Citation21]. Recruitment took place between March 2011 and March 2013. Persons with stroke were included if they had a clinically confirmed diagnosis of either ischemic or hemorrhagic stroke as confirmed by the neurologist within the past seven days. Exclusion criteria were: (1) comorbid condition which was anticipated to interfere with study outcomes such as neuromuscular diseases, (2) a premorbid Barthel Index (BI) score lower than 18 which is indicative of premorbid dependency in activities of daily life, (3) insufficient command of the Dutch language to understand and complete the questionnaires as judged by the clinician and (4) a premorbid cognitive decline as indicated by a score ≥ 1 on the hetero-anamnesis list cognition [Citation22]. Persons were only included for analyses in this study if they were living at home during the full study period.
Interventions
Stroke aftercare
Stroke aftercare is current practice and part of the stroke care pathway in the region of Maastricht, the Netherlands. As part of regular care, all patients receive an invitation to a consultation at the outpatient clinic of neurology at six to eight weeks after discharge and were enrolled in regular follow-up secondary prevention purposes. Additionally, at discharge from the hospital, persons with stroke and their caregivers receive an invitation for stroke aftercare at approximately six months post stroke. The aim of stroke aftercare is threefold: (1) to signal potential problems experienced in daily life concerning physical, cognitive and emotional symptoms, (2) to provide support and psychoeducation to the person with stroke and caregiver, and (3) to refer the person to further specialized healthcare professionals such as neuropsychologists and physiotherapist, when needed.
The stroke aftercare is situated in a Primary Care Plus (PC+) center in Maastricht, the Netherlands. PC + aims to reduce healthcare costs by offering specialist knowledge in the primary care setting, with the general practitioner in a gatekeeping and coordination role [Citation23]. The stroke aftercare consultation is led by a registered nurse (four years of education) specialized in neurology and takes place at the PC + center. Two weeks prior to the consultation, the persons with stroke and their caregivers receive questionnaires which are used as a source of information in the consultation. The consultation lasts a maximum of 45 min. A follow-up consultation at the stroke aftercare can be planned when the nurse judges this is necessary.
Care-as-usual
The care-as-usual cohort as described in the Restore4stroke study did not implement a specific intervention and therefore concerned regular care, consisting of a consultation at the outpatient clinic of neurology at six to eight weeks after discharge, and regular follow-up for secondary prevention purposes, comparable to the stroke aftercare group. No further systematical follow-up took place afterwards in the Restore4stroke cohort. The study of van Eeden et al. provides an overview of the received healthcare services as part of care-as-usual [Citation24].
Procedure
Eligible persons who visited the stroke aftercare were invited to participate in the stroke aftercare study for which specific informed consent was needed. The nurse provided basic study information at consultation, and if a person was interested, contact details were forwarded to the researcher. The researcher provided more information by telephone. Those willing to participate were sent a written information letter, informed consent and questionnaires concerning quality of life and stroke impact on daily life. The questionnaires administered as part of stroke aftercare, concerning anxiety, depression, experienced cognitive and emotional problems in daily life, fatigue and social participation, were collected from the persons’ hospital file after consent was obtained. Demographic and medical information were collected as well at that point. Persons who visited stroke aftercare but did not participate in the stroke aftercare study were considered non-responders. The questionnaires completed at the time of the stroke aftercare consultation were considered baseline measurements (T0). Subsequent questionnaires were sent six months after T0 at approximately 12 months post stroke (T1). The six (T0) and 12 months (T1) assessments from the care-as-usual Restore4stroke study were used for comparability. For further details on the procedures of Restore4stroke we refer to the study of van Mierlo et al. [Citation21].
Ethics
The medical ethics committee of the MUMC+ (16-4-180) approved the stroke aftercare study. The care-as-usual Restore4stroke cohort was approved by the Committee on Research involving Human Subjects of the St. Antonius Hospital in Nieuwegein (the Netherlands) and by the medical committees of all participating hospitals. Both studies were performed according to the Declaration of Helsinki’s principles. Written informed consent was obtained of all participants. Data of non-responders was used anonymously as all patients entering into care of MUMC+, including stroke aftercare, were informed that individual data might be used anonymously in retrospective studies.
Measures
Demographic and medical information
The demographic parameters age, sex and educational level were collected from T0 questionnaires. Medical information concerning stroke type, hemisphere, location and severity was collected from the persons’ hospital files. Stroke severity was assessed with the National Institutes of Health Stroke Scale (NIHSS) in which higher scores are indicative of more severe stroke symptoms (range 0–30) [Citation25].
Anxiety and depression
The Hospital Anxiety and Depression Scale (HADS) [Citation26] consists of 14 items where higher scores are indicative of more severe symptoms, for either subscale anxiety or depression (range 0–21). A score of ≥ 8 is indicative of clinically relevant symptoms on the given domain.
Fatigue
The Fatigue Severity Scale (FSS) [Citation27] consists of nine items where higher scores (range 1–7; averages) are indicative of more severe fatigue symptoms. An average score ≥ 4 indicates moderate to severe fatigue.
Cognitive and emotional problems experienced in daily life
The Checklist for Cognitive and Emotional Consequences of Stroke (CLCE-24) consists of 24 items where higher scores are indicative of more experienced problems in daily life, for either subscale cognition or emotion (score absent/present, range 0–22) [Citation28]. The two open ended items of this questionnaire were not used.
Social participation
The restrictions domain of the Utrecht Scale for Evaluation of Rehabilitation-Participation (USER-P) [Citation29] consists of 11 questions of which higher scores (range 0-100) are indicative of less experienced restrictions with social participation.
Stroke impact on daily life
The Stroke-Adapted Sickness Impact Profile (SA-SIP30) [Citation30] consists of 30 items of which higher scores (range 0-100) are indicative of a higher impact of stroke on activities of daily life.
Quality of life
Quality of life was measured with the EuroQol-5D-3L (EQ-5D-3L) and the EuroQol-5D-5L (EQ-5D-5L) [Citation31]. The EQ-5D-3L was included for comparability with the Restore4stroke cohort and the EQ-5D-5L, because of observed ceiling effects for the three-level questionnaire [Citation24]. Dutch tariffs were used. The utility score ranges from −0.330 or −0.446 (EQ-5D-3L and EQ-5D-5L respectively; worse than dead) to 1 (full health) [Citation31,Citation32].
Analyses
The first step of the statistical analyses concerned dichotomizing educational level into lower-educated (up to completed secondary education) and higher-educated (completed professional education or university and higher). Missing data was imputed at an 80% level, using individual mean imputation for all outcome measures except for the USER-P (unable due to non-applicable answer options).
Potential selection bias was assessed by comparing the participants of the stroke aftercare study to non-responders on demographic and stroke-related information, as well as on the questionnaires part of the stroke aftercare (HADS, CLCE-24, USER-P and FSS). The stroke aftercare cohort was compared to the care-as-usual cohort on demographic and stroke-related information. Independent-samples t-tests and Pearson chi-square tests were used for the comparisons between cohorts.
Change in scores over time within the stroke aftercare cohort on the FSS, CLCE-24, SA-SIP30 and EQ-5D-5L were examined using paired-samples t-tests. These questionnaires were not administered in the care-as-usual cohort.
Using multilevel model analyses, the change over time in the HADS, USER-P, and the EQ-5D-3L were examined across cohorts. Variables were entered into the model as covariate based on their association with the independent (i.e., cohort) as well as the dependent variable. Likelihood ratio tests were used to assess model fit. Covariance structures were specified according to best fit. The best fitting model was used for comparing the cohorts. Interaction effects were examined to assess whether the cohorts differed in outcome over time.
An alpha of 5% (two-sided) was used for significance testing. IBM SPSS Statistics for Macintosh, version 24.0, was used for the statistical analyses.
Results
displays the flowchart of persons with stroke from hospital admission to participation in the stroke aftercare study. In total, 87 persons were included in the stroke aftercare cohort and 206 in the non-responder cohort, who were not informed or not interested in participation in this study but completed the questionnaires part of stroke aftercare. The stroke aftercare cohort was significantly younger (p < 0.05) and less often referred to geriatric rehabilitation (p < 0.05) than the non-responders (). Furthermore, the stroke aftercare cohort had significantly lower levels on HADS depression (p < 0.05), the FSS (p < 0.001) and CLCE-24 cognition (p < 0.05), and higher levels on the USER-P (p < 0.001) than the non-responders cohort.
Figure 1. Flowchart of stroke and transient ischemic attack patients’ admission to the hospital in the period of 1st April 2016 to 15th May 2017, to participation in the stroke aftercare study. The local university hospital admits nearly 700 stroke and transient ischemic attack cases annually.
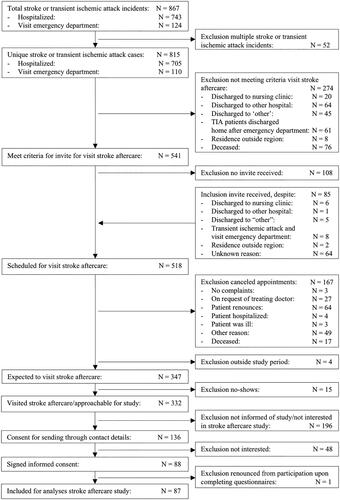
Table 1. Characteristics of persons who participated in the stroke aftercare cohort versus non-responders.
A total of 363 persons with stroke were included in the care-as-usual cohort for analyses as 32 (8.1%) were excluded because of not living at home at T0 and T1. The care-as-usual cohort differed significantly from the stroke aftercare in stroke severity (p < 0.05) and proportions of stroke type (p < 0.001), i.e., more persons suffered an ischemic stroke (adj. residual = 4.90) and none from transient ischemic attack (adj. residual = −7.50) ().
Table 2. Characteristics of the stroke aftercare cohort versus care-as-usual cohort.
shows the change over time in emotional and psychosocial outcome for the stroke aftercare cohort. A significant decrease in the score on the CLCE emotional domain was observed between T0 and T1 (p < 0.05). No significant differences between T0 and T1 were observed for the CLCE cognition domain, FSS, SASIP-30 and EQ-5D-5L.
Table 3. Change over time in emotional and psychosocial outcome for the stroke aftercare cohort.
In , we show the rate of change in emotional and psychosocial outcomes of the stroke aftercare cohort in comparison to the care-as-usual cohorts using multilevel models (time x cohort). Stroke type differed significantly between cohorts but was not significantly associated with any outcome measure (HADS, EQ-5D-3L and USER-P) (p > 0.05) and therefore not entered as a covariate in the multilevel models. Stroke severity differed significantly between cohorts and was significantly associated with the USER-P (r = −0.134, p ≤ 0.001) and was therefore entered as a covariate in the USER-P multilevel model.
Table 4. Rate of change in outcomes of the stroke aftercare cohort versus the care-as-usual cohort.
HADS anxiety was not significantly different on baseline between cohorts. No time x cohort interaction effect was observed. The stroke aftercare cohort showed significantly decreased HADS anxiety scores, whereas the care-as-usual cohort did not change from T0 to T1. At T1, HADS anxiety was not significantly different between cohorts. No significant main, or time x cohort interaction effects were observed for HADS depression, indicative of stable levels over time for both cohorts ( and ).
Figure 2. Graphs displaying outcomes over time of the stroke aftercare and care-as-usual. Note: coefficients are estimated marginal means of the multilevel model. HADS: Hospital Anxiety and Depression Scale; USER-P: Utrecht scale for Evaluation of Rehabilitation- Participation; EQ: EuroQol; QoL: Quality of Life.
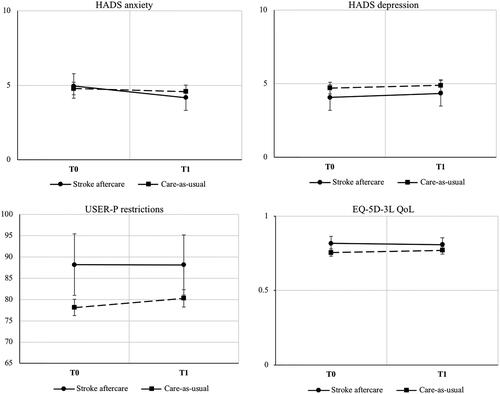
A significant higher score on the USER-P restrictions (i.e., less experienced restrictions) is observed at baseline for stroke aftercare in comparison with care-as-usual. No significant time x cohort interaction was observed. The care-as-usual cohort increased significantly on USER-P restrictions, while the stroke aftercare cohort remained on stable levels (non-significant change). The stroke aftercare cohort still had a significantly higher score on the USER-P restrictions at T1 (i.e., less experienced restrictions; and ).
EQ-5D-3L was significantly higher in the stroke aftercare cohort at baseline in comparison to care-as-usual with no significant effects over time for both cohorts. No significant time x cohort interaction was observed. At T1, EQ-5D-3L did no longer appear to be significantly different between the aftercare cohort and care-as-usual cohort ( and ).
Discussion
In this study, we examined whether nurse-led stroke aftercare at six months after hospital admission is beneficial for the long-term psychosocial outcome of community-dwelling persons with stroke. Stroke aftercare showed significant beneficial effects on emotional well-being in comparison to care-as-usual. Emotional problems experienced in daily life and the severity of anxiety symptoms decreased significantly after attending stroke aftercare, whilst care-as-usual remained on stable levels of anxiety symptoms. No significant changes over time were observed in relation to depressive symptoms, fatigue, cognitive problems experienced in daily life, fatigue, stroke impact on daily life and quality of life. Restrictions with participation decreased significantly in care-as-usual whereas the stroke aftercare cohort remained on low and stable levels of experienced restrictions with social participation.
Stroke aftercare was shown to be particularly beneficial for emotional well-being. Beneficial effects were small but considered clinically relevant. Each change directly reflects improvement in a person’s psychosocial functioning as we used patient-reported outcome measures. The beneficial effects may be attributed to the elements of active psychoeducation and emotional support through counseling with a focus on reassurance and diminishing insecurities and worries. Active psychoeducation has been shown to be beneficial to person’s mood, knowledge of stroke and satisfaction [Citation33]. It allows for clarification and consolidation of information through reinforcement in contrast to the passive form of psychoeducation which includes, for instance, sending information packages a person’s home [Citation33]. Further, beneficial effects on mood have been described through counseling for persons with stroke and caregivers [Citation34,Citation35]. Through counselling the nurse provides emotional support, which is needed for persons with stroke in order for them to cope with the drastic changes in their lives [Citation34]. Caregivers provide the needed support at home [Citation36] and therefore fulfill an important role in stroke aftercare. Further, the screening of potential problems in daily life, on all levels, enables the nurses to provide personalized care and support [Citation11,Citation37]. Altogether, the active and person-centered approach is regarded to be essential in providing stroke aftercare. Nonetheless, the beneficial effects of stroke aftercare in its current form are small and limited to emotional functioning. To increase effects, the therapeutic design could be enriched by training the nurses in self-management strategies [Citation38] or motivational interviewing [Citation39]. This way, the nurses will be better equipped to address each person’s needs and possibly increase beneficial effects of stroke aftercare.
Nurse-led stroke aftercare could be considered a valuable addition to routine follow-up stroke care as current services do not systematically address psychosocial outcomes but which is recommended by the international stroke guidelines [Citation40]. Moreover, stroke aftercare in its current form suits a primary healthcare setting as it is elementary in its therapeutic design by particularly providing psychoeducation and emotional support. Moreover, 92% of the visitors received information folders and only a minority needed follow-up contact (16%) or referral to specialist healthcare (11%). This information seems to align with the stepped-care model [Citation17], stating that the majority of persons with stroke experience mild problems which need attention from the simplest form of interventions. In this respect, less could be considered more. However, a process evaluation should be performed in future research to gain more insight into stroke aftercare and its role in the stroke care pathway.
Moreover, stroke aftercare can only be considered a high-quality healthcare improvement when it complies with the “triple aim” theoretical framework of Berwick et al. [Citation41]. Sustainability is secured when a new form of healthcare (1) improves health of the population, (2) improves the individual’s experience of care and (3) reduces per capita costs of healthcare. Stroke aftercare has shown some health improvement regarding emotional well-being. Future research should examine the second and third aim but it could be expected that stroke aftercare achieves increased satisfaction and decreased costs, as it is designed to meet a person’s expectations of healthcare [Citation14] and to substitute expensive outpatient hospital care in low-cost primary care setting [Citation19]. Follow-up costs after, or because of stroke aftercare, should also be considered in future research.
Strengths and limitations
This study was able to give a detailed insight into stroke aftercare by describing the process from stroke admission to outcome at approximately 12 months post stroke and comparing to care-as-usual. Further, the psychosocial outcome was extensively studied by including multiple measures. Hereby, we ensured the best use of data and adequate assessment of the possible beneficial effects of stroke aftercare [Citation42]. Lastly, comparative effectiveness research designs incorporating observational studies allow for the complexity of the daily clinical practice, as opposed to randomized controlled trials which attempt to standardize interventions [Citation43,Citation44]. Comparative effectiveness research designs are, therefore, particularly known to result in improvements of healthcare services [Citation43,Citation44].
This study had some limitations as well. The observational studies included, and being bound to the daily clinical practice, resulted in a relatively large variation in follow-up time and possibly influenced the comparison to care-as-usual. Comparability between cohorts was also limited by the different data collection periods. However, the Restore4stroke study describes care-as-usual as it is performed to date. Moreover, it could be argued that the inclusion of transient ischemic attack cases in the stroke aftercare cohort influenced the results, as a transient ischemic attack is neurologically distinct from stroke. Nevertheless, psychosocial outcome after transient ischemic attack has been reported to be similar to minor stroke [Citation45]. The clinical practice variation also led to a small sample size and strong selection bias, in favor of persons with stroke experiencing only mild problems at six months. However, we still observed some beneficial effects which are expected to be greater in persons with stroke experiencing moderate to severe problems in daily life. Additionally, the high-functioning stroke aftercare cohort still experienced problems in daily life which might be indicative of an overestimation of their functioning in society [Citation46].
Conclusions
This study showed that nurse-led stroke aftercare was primarily beneficial for long-term emotional well-being after stroke. It did not show to be beneficial for psychosocial outcome and depressive symptoms. Stroke aftercare is unique as it systematically addresses psychosocial outcome, by active identification of problems through screening, provision of psychoeducation and emotional support and specialized follow-up when needed. While it is regarded as a valuable addition to current routine stroke follow-up care, person’s satisfaction and cost-effectiveness should be examined before stroke aftercare can be considered a high-quality healthcare improvement. Finally, the therapeutic character of stroke aftercare could be enhanced to increase effects which might be achieved by adding self-management strategies and motivational interviewing.
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We would like to thank all the participants of this study and the stroke aftercare nurses for their efforts in recruiting persons with stroke for this study.
Disclosure statement
The authors report no conflicts of interest.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439–458.
- van de Port IG, Kwakkel G, van Wijk I, et al. Susceptibility to deterioration of mobility long-term after stroke: a prospective cohort study. Stroke. 2006;37(1):167–171.
- Leśniak M, Bak T, Czepiel W, et al. Frequency and prognostic value of cognitive disorders in stroke patients. Dement Geriatr Cogn Disord. 2008;26(4):356–363.
- Bergersen H, Froslie KF, Stibrant Sunnerhagen K, et al. Anxiety, depression, and psychological well-being 2 to 5 years poststroke. J Stroke Cerebrovasc Dis. 2010;19(5):364–369.
- Snaphaan L, van der Werf S, de Leeuw FE. Time course and risk factors of post-stroke fatigue: a prospective cohort study. Eur J Neurol. 2011;18(4):611–617.
- van Mierlo ML, van Heugten CM, Post MW, et al. Quality of life during the first two years post stroke: The Restore4Stroke Cohort Study. Cerebrovasc Dis. 2016;41(1-2):19–26.
- Hartman-Maeir A, Soroker N, Ring H, et al. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil. 2007;29(7):559–566.
- Tooth L, McKenna K, Goh K, et al. Length of stay, discharge destination, and functional improvement: utility of the Australian National Subacute and Nonacute Patient Casemix Classification. Stroke. 2005;36(7):1519–1525.
- Olofsson A, Andersson SO, Carlberg B. 'If only I manage to get home I'll get better'-interviews with stroke patients after emergency stay in hospital on their experiences and needs. Clin Rehabil. 2005;19(4):433–440.
- Carlsson G, Möller A, Blomstrand C. A qualitative study of the consequences of 'hidden dysfunctions' one year after a mild stroke in persons < 75 years. Disabil Rehabil. 2004;26(23):1373–1380.
- Connolly T, Mahoney E. Stroke survivors' experiences transitioning from hospital to home. J Clin Nurs. 2018;27(21–22):3979–3987.
- van Schaik SM, de Vries BS, Weinstein HC, et al. Practice variation in long-term secondary stroke prevention in the Netherlands. J Stroke Cerebrovasc Dis. 2015;24(3):566–572.
- Harrison M, Ryan T, Gardiner C, et al. Psychological and emotional needs, assessment, and support post-stroke: a multi-perspective qualitative study. Top Stroke Rehabil. 2017;24(2):119–125.
- Pindus DM, Mullis R, Lim L, et al. Stroke survivors' and informal caregivers' experiences of primary care and community healthcare services – a systematic review and meta-ethnography. PLoS One. 2018;13(2):e0192533.
- Allison R, Shelling L, Dennett R, et al. The effectiveness of various models of primary care-based follow-up after stroke: a systematic review. Prim Health Care Res Dev. 2011;12(3):214–222.
- Fens M, Vluggen TP, van Haastregt JC, et al. Multidisciplinary care for stroke patients living in the community: a systematic review. J Rehabil Med. 2013;45(4):321–330.
- Kneebone II. Stepped psychological care after stroke. Disabil Rehabil. 2016;38(18):1836–1843.
- Moulaert VR, van Heugten CM, Winkens B, et al. Early neurologically-focused follow-up after cardiac arrest improves quality of life at one year: a randomised controlled trial. Int J Cardiol. 2015;193:8–16.
- Martínez-González NA, Djalali S, Tandjung R, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14(1):214.
- Martínez-González NA, Tandjung R, Djalali S, et al. The impact of physician-nurse task shifting in primary care on the course of disease: a systematic review. Hum Resour Health. 2015;13(1):55.
- van Mierlo ML, van Heugten CM, Post MW, et al. A longitudinal cohort study on quality of life in stroke patients and their partners: Restore4Stroke Cohort. Int J Stroke. 2014;9(1):148–154.
- Meijer R, van Limbeek J, de Haan R. Development of the Stroke-unit Discharge Guideline: choice of assessment instruments for prediction in the subacute phase post-stroke. Int J Rehabil Res. 2006;29(1):1–8.
- van Hoof S, Kroese M, Spreeuwenberg M, et al. Substitution of hospital care with primary care: defining the conditions of Primary Care Plus. Int J Integrated Care. 2016;16(1):12.
- Van Eeden M, van Heugten C, van Mastrigt G, et al. The burden of stroke in the Netherlands: estimating quality of life and costs for 1 year poststroke. BMJ Open. 2015;5(11):e008220.
- Brott T, Adams HP, Jr., Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989;20(7):864–870.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46(10):1121–1123.
- van Heugten C, Rasquin S, Winkens I, et al. Checklist for cognitive and emotional consequences following stroke (CLCE-24): development, usability and quality of the self-report version. Clin Neurol Neurosurg. 2007;109(3):257–262. Apr
- Post MW, van der Zee CH, Hennink J, et al. Validity of the utrecht scale for evaluation of rehabilitation-participation. Disabil Rehabil. 2012;34(6):478–485.
- van Straten A, de Haan RJ, Limburg M, et al. A stroke-adapted 30-item version of the Sickness Impact Profile to assess quality of life (SA-SIP30). Stroke. 1997;28(11):2155–2161.
- Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72.
- Selivanova A, Buskens E, Krabbe PF. Head-to-Head Comparison of EQ-5D-3L and EQ-5D-5L Health Values. Pharmacoeconomics. 2018;36(6):715–725.
- Forster A, Brown L, Smith J, et al. Information provision for stroke patients and their caregivers. Cochrane Database Syst Rev. 2012;(11):CD001919.
- Oikarinen A, Kääriäinen M, Kyngäs H. A framework of counseling for patients with stroke in nursing: a narrative literature review. J Neurosci Nurs. 2014;46(5):E3–E14.
- Visser-Meily A, van Heugten C, Post M, et al. Intervention studies for caregivers of stroke survivors: a critical review. Patient Educ Couns. 2005;56(3):257–267.
- Boger EJ, Demain SH, Latter SM. Stroke self-management: a focus group study to identify the factors influencing self-management following stroke. Int J Nurs Stud. 2015;52(1):175–187.
- Edwards DF, Hahn MG, Baum CM, et al. Screening patients with stroke for rehabilitation needs: validation of the post-stroke rehabilitation guidelines. Neurorehabil Neural Repair. 2006;20(1):42–48.
- Fryer CE, Luker JA, McDonnell MN, et al. Self management programmes for quality of life in people with stroke. Cochrane Database Syst Rev. 2016;(8):CD010442.
- Cheng D, Qu Z, Huang J, et al. Motivational interviewing for improving recovery after stroke. Cochrane Database Syst Rev. 2015;(6):CD011398.
- Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018–2030. Eur Stroke J. 2018;3(4):309–336.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–592.
- Maas AI, Menon DK, Lingsma HF, et al. Re-orientation of clinical research in traumatic brain injury: report of an international workshop on comparative effectiveness research. J Neurotrauma. 2012;29(1):32–46.
- Maas AI, Murray GD, Roozenbeek B, International Mission on Prognosis Analysis of Clinical Trials in Traumatic Brain Injury (IMPACT) Study Group, et al. Advancing care for traumatic brain injury: findings from the IMPACT studies and perspectives on future research. Lancet Neurol. 2013;12(12):1200–1210.
- Fens M, van Heugten CM, Beusmans GH, et al. Not as transient: patients with transient ischaemic attack or minor stroke experience cognitive and communication problems; an exploratory study. Eur J Gen Pract. 2013;19(1):11–16.
- Swift TL, Wilson SL. Misconceptions about brain injury among the general public and non-expert health professionals: an exploratory study. Brain Inj. 2001;15(2):149–165.
