Abstract
Purpose
Physical activity (PA) post-myocardial infarction (MI) can reduce risk of reoccurrence and mortality. Yet uptake of PA through cardiac rehabilitation (CR) is poor, and little is known about the long-term PA behaviour of cardiac patients. This study aimed to explore the lived experiences of patients’ engagement with PA post-MI, together with the experiences of their family.
Methods
Longitudinal interviews with six family-dyads were conducted which drew on interpretative phenomenology to understand the lived experiences of PA for post-MI patients and family members.
Results
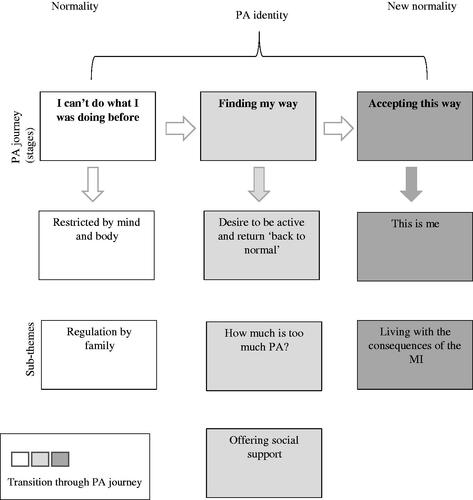
Participants described a journey that involved leaving “normality” (doing what PA they wanted and when) and transitioning to a new “normality” (being active within post-MI parameters). This journey was expressed through feelings of “I can’t do what I was doing before,” “finding my way,” and “accepting this way”.
Conclusion
The role of family within the patient’s journey was complex, with PA identity, beliefs, and fear of MI re-occurrence influencing PA support both positively and negatively. PA engagement post-MI is a dynamic and interactive process within which the family can have an important influence.
The process of (re-)engaging in physical activity post-myocardial infarction involves a complex journey towards acceptance of a new “normality”.
Family play an important role in regulating and supporting patients’ physical activity during the rehabilitation process.
Promoting positive health beliefs and helping families understand what, how and when patients should be physically active may optimise the rehabilitation journey for post-myocardial infarction patients.
IMPLICATIONS FOR REHABILITATION
Introduction
Coronary heart disease (CHD) is a leading cause of mortality worldwide [Citation1]. Myocardial infarction (MI) is an acute manifestation of CHD resulting from intracoronary plaque rupture or erosion, and subsequent thrombus formation in one of the heart’s coronary arteries. The resulting transient or permanent vessel occlusion causes myocardial ischaemia or infarction [Citation2]. A diagnosis of a coronary condition heightens the risk of further cardiac events [Citation3] therefore, understanding ways of improving secondary prevention and managing CHD is imperative.
Globally, cardiac rehabilitation (CR) is recognised as a multi-faceted intervention which aims to limit the physiological and psychological effects of cardiac illness [Citation4]. Physical activity (PA), referred to “as any bodily movement produced by the skeletal muscles that requires energy expenditure” [Citation5,p.126], post-MI is a core component of recovery [Citation6], which is included globally in CR as structured exercise. Although no formal PA guidance exists post-MI, patients are encouraged to work towards achieving 150 min of moderate intensity PA weekly [Citation7].
PA post-MI has been shown to reduce cardiac morbidity and mortality, yet, to accrue such benefits, PA should be sustained into the longer term (24 months post cardiac event) [Citation8]. However, evidence suggests PA maintenance post-CR is poor [Citation9], and may be due to a number of barriers including fatigue, low mood (feeling teary and emotional), a lack of motivation and a fear of being active (scared to do themselves harm) [Citation10] barriers which have been found to affect an MI population specifically. A commonly cited facilitator for PA engagement is social support [Citation11–13]. There are varied theoretical explanations for the mechanisms through which social support influences PA behaviour. The Theory of Planned Behaviour (TPB) [Citation14] posits that subjective norms, referring to an individual’s perceived social pressure to engage in a particular behaviour, may influence individuals’ PA behaviour [Citation15], whereas social cognitive theory (SCT) [Citation16] suggests individuals’ PA engagement may be enhanced when they observe someone they identify with perform a task (vicarious learning) and receive positive feedback from others (verbal/social persuasion). Further, Self-Determination Theory (SDT) [Citation17] suggests individuals are more likely to feel autonomously motivated to engage in PA when they feel connected and respected by others [Citation18]. Family have been identified as positive support providers given their ability to facilitate and encourage engagement in healthy behaviours [Citation19–21]. Within a CHD context, patients have been shown to experience better outcomes if their families offer encouragement to make positive health choices, listen to patient concerns, and take a practical interest in patients’ health and well-being (e.g., PA engagement) [Citation22–23]. Whereas overprotective, neglectful, critical, demanding or withdrawn behaviours (even if originating from a point of care), can negatively impact upon patients’ ability to make lifestyle changes [Citation21]. Explanations for variation in support provision are numerous and include families’ own PA identity, beliefs surrounding patients’ recovery [Citation23] and their own emotional wellbeing (e.g., feelings of depression/anxiety) [Citation24].
As discussed, it appears evident that within a CHD population, family support can impact health outcomes [Citation21–23], however, little is known of how patients and families make sense of, and experience PA-post-MI, whilst also exploring temporal change. Therefore, the aim of the current study was to explore the lived experiences of patients’ engagement with PA post-MI, together with the experiences of their family. Data was collected over the course of nine months (during the first year post-MI), with the aim of understanding how perceptions of PA may change over time.
Methods
Philosophical approach
Using qualitative methods within a rehabilitation context has the potential to help improve practice [Citation25]. Therefore, we adopted a qualitative longitudinal approach to capture patients and family members’ experiences of PA post-MI and understand how perceptions of PA may change over time, given experiences are often time specific [Citation26] and reflected on differently as individuals’ social worlds evolve. We drew on Interpretative Phenomenological Analysis (IPA) [Citation27] for its grounding in understanding how participants make sense of, and attribute meaning to, their personal and social world following a significant life experience [Citation28]. In IPA, the prerequisite for accessing knowledge about individuals’ lived experience is a process of interaction [Citation29], achieved through entering a hermeneutic cycle of in-depth interpretation between individual(s) and researcher. This ongoing process of interaction spanned a period of nine months, during which we conducted semi-structured interviews at three time-points with each family dyad (approximately 1, 4- and 9-months post-MI).
Within IPA it is important to acknowledge the inherent biases that may arise from the research team’s prior knowledge and experience [Citation27], which in this case was drawn from the domains of PA and health, psychology and cardiac nursing. As a means of reflecting and accepting biases as they occurred, and therefore ensuring an authentic and honest representation of participant accounts, [SB] engaged in a process of bracketing throughout the study, which involved keeping a reflective log and having regular conversations with the research team.
Study setting and participant recruitment
Participant recruitment began in May 2017 and ended in December 2017, with patients recruited from a CR service located within the North West of England. The CR service comprised of 4 phases, and patients were encouraged to attend by practitioners in their care team. However, as families’ interactions with the CR service of study occurred incidentally, much of the CR information was provided to patients. Phase 1 took place in a hospital setting following patients MI diagnoses and involved a discussion with a member of the patient’s cardiac team regarding the patient’s condition. Phase 2 involved a home visit by a cardiac nurse (CN) within 5 days of patients’ hospital discharge, where they discussed lifestyle behaviours and explained the process of phases 3 and 4 of CR. Phase 3 began approximately 3 weeks post-MI (dependent on patients’ health status) and took place within an outpatient hospital setting with other cardiac patients. It involved 6 weeks of supervised and individualised exercise sessions with a physiotherapist, coupled with 6 weeks of stress management led by an occupational therapist (OT). Phase 4 began approximately 9 weeks post-MI (dependent on patients’ health status) and took place within a community setting (i.e., leisure centre facilities) with other cardiac patients and involved 12 weeks of supervised and individualised exercise with an activity referral scheme officer. Additionally, all phases were supplemented with ongoing education as recommended by the BACPR [Citation6].
For patients, eligibility for study inclusion included being ≥18 years of age, an MI diagnosis within the previous month, a fluent English speaker and present in the study region for the study duration. Patients were excluded if the MI had resulted in coronary artery bypass graft or were unable to engage in PA due to another co-morbidity, injury or ongoing investigation. Patients were asked to recruit at least one family member they deemed influential in their health and wellbeing. Patients were identified by two CNs on their routine home visit to patients within 5 days of their hospital discharge. During this visit, all patients deemed eligible by the CNs were approached and provided with written details of the study (n = 121 patients). The CNs gained verbal consent from interested patients to share their details with the researcher [SB], who then contacted patients to discuss the study further and arrange the first interview (if applicable).
Final sample
In total, 6 family dyads consented to take part in the research (). Each dyad comprised one post-MI patient and one family member (5 spouses, 1 son). Three male and three female patients took part. All were retired with a median age of 68 years (range 60–79 years). In regard to MI incidence and type, four patients had suffered their first MI, and 2 had suffered multiple MIs (their second and third respectively). Two patients had been diagnosed with having a ST segment elevation MI ((STEMI) – ST segment elevation on an electrocardiogram with a rise in cardiac biomarkers greater than the 99th percentile [Citation30]), and 4 others as non-ST segment elevation MI ((Non-STEMI) – absence of ST segment elevation on an electrocardiogram with respective rise in cardiac biomarkers [Citation30]).
Table 1. Post-myocardial infarction patient demographic overview.
Data collection
[SB] interviewed each family dyad in their own home on three occasions between August 2017 and September 2018, with each interview lasting between 30 and 120 min. Interviews took place approximately 1, 4- and 9-months post-MI in an attempt to capture each patient’s PA journey through and after CR. However, due to participant availability, interviewing at these timepoints was not possible for all dyads, and the time between MI and first interviewed ranged from 1 to 3 months, although the time between interviews remained consistent. Our initial intention was to interview patient and family members separately, so participants felt comfortable discussing their feelings and experiences, however as the study progressed, most dyads expressed a preference to be interviewed together. Consequently, from the 2nd interview onwards the majority of interviews were conducted with both patient and family member together (5 dyads). Refer to for information detailing whether dyads interviewed together and separately. This approach provided an in-depth understanding of the family dynamic revealing a collaborative family reality, whilst also demonstrating how each family member negotiated their own experience [Citation31]. Written consent was obtained from all participants before the start of the 1st interview and indicated their consent to be involved in the subsequent two interviews. All dyads completed all three interviews.
We used a semi-structured interview guide to allow participants to speak openly about their PA experiences post-MI [Citation28]. As the initial plan was to interview patients and family members separately, separate interview guides were developed for patients and family members for each timepoint. Interview topics included PA attitudes, past and current experiences, future intentions, facilitators and barriers as well as family support. However, to capture participants’ unique experiences, some questions and prompts were tailored to reflect the emerging discussion and therefore not pre-determined in the interview guide. Supplementary Material 1 presents the interview guides. Questions were asked one at a time allowing each participant to think about their responses. For participants who were interviewed together, [SB] posed questions separately to allow each member of the dyad time to respond. However, as some of the topics on the guide were similar, participants often interjected one another with their thoughts and experiences. In these situations, to ensure participant responses were captured fully, [SB] made sure to go back to the question and ask if participants had anything further to add.
Prior to data collection, [SB] conducted four pilot interviews with post-MI patients and family members not eligible for participation in the current study. Participants fed back on the appropriateness and tone of the questions, but also on topics absent from the guide they felt would be beneficial to explore. Modifications to the guides were made based on participant feedback and included refining questions to have a clearer focus.
Data analysis
Interviews were audio recorded, transcribed verbatim and analysed following IPA principles [Citation27] which involved reading and re-reading (transcripts), taking initial notes, developing emergent themes, searching for connections across emergent themes, moving to the next case and looking for patterns across cases. We also explored how themes manifested within and across cases over time. This combination of cross-case and longitudinal analysis portrayed temporal change of how participants experienced PA post-MI providing insight into how experiences unfolded and were made sense of over time. Analysis was undertaken by [SB] with [IJ, RM, IG, PM] acting as “critical friends” [Citation32] throughout the process. All authors reviewed a sample of transcripts and engaged in regular meetings to discuss and debate themes and ensure authentic representation of participant experiences.
Longitudinal analysis of family experiences
To capture experiences within the context of each family’s journey, we analysed transcripts from each dyad (i.e., patient and family member interviews at times 1, 2 and 3) as a whole. After several readings of each transcript, [SB] added initial notes manually to margins to highlight utterances pertaining to the research questions (an effort was made to link notes closely with participants’ spoken words to ensure their experiences were captured accurately). [SB] then explored initial notes for meaning and developed themes that were represented as small phrases grounded in the essence of what was found within the text, but also reflected her subjective interpretation. These themes were noted down on paper allowing [SB] to search for connections between themes, including associations, contradictions and changing meanings over time. Themes were then collapsed to form subthemes and super-ordinate themes, and names applied to capture the spirit of each theme. Theme development involved reviewing, removing, adding and changing codes, ensuring they fitted the data rather than forcing data into themes. This process was repeated for each dyad.
Cross-case analysis
Following the process of theme development, themes developed from each dyad during the longitudinal analysis were manually noted on paper and supported with verbatim quotes from the transcripts (see Supplementary Material 2 for a visual representation of themes by family). [SB] then transferred each theme to a post-it note and mapped these onto a pin board to search for patterns (e.g., convergence and divergence) across accounts. From this, a new pin board was created representing themes across dyads and created an overall synthesis of participant experiences. Themes were then written up and presented in narrative form (see Supplementary Material 3 for the thought processes underpinning the narrative). This process allowed themes to be expanded and further refined and developed so the longitudinal narrative could be explored and accurately represented, which involved multiple written drafts until the themes were deemed to be an authentic representation of participants’ subjective experience.
Ethical approval
Ethical approval for this study was granted in May 2017 by [West of Scotland] NHS Research Ethics Committee, reference number: [reference number: 17/WS/0053].
Results
Findings suggested post-MI, patients experienced a journey of PA rediscovery, and family experienced this journey with patients, but also shaped the way it was experienced by them. The journey portrayed a transition from ‘normality’ (i.e., patients being able to do what PA they wanted when they wanted to do it) to a ‘new normality’ (i.e., living life as an MI patient) and was characterised over three sequential but overlapping stages, ‘I can’t do what I was doing before’, ‘finding my way’ and ‘accepting this way’, with subthemes within each (refer to for overview of themes and subthemes). The stages identified were not bound by interview time-point, instead, all families experienced the stages but not at the same pace or the same way, and the subthemes within stages transcended across time.
How dyads viewed themselves in relation to PA appeared to influence their PA journey. Out of the dyads interviewed, five perceived themselves as active (“active dyads”) and one perceived themselves as inactive (“inactive dyad”). Pseudonyms are used throughout to protect participant anonymity.
Active dyads (Alex and Joanne, Doris and Anthony, Julia and George, Alice and David, Robert and Sarah)
For dyads who considered themselves as active, PA aligned to their personal values and interests. They understood PA was important and beneficial for health and consequently being active formed a regular part of the patients’ pre-MI routine. Although “active dyads” viewed PA as a holistic phenomenon, some PA examples they provided during the interviews were structured and fitness orientated (and would be defined as exercise according to Caspersen, Powell and Christenson’s (1985) definition [Citation5]). For these dyads, patients’ MI came as a shock (due to perceived healthy lifestyle), leaving patients experiencing feelings of disbelief as they did not associate their identity with what they believed to be typical of “MI patients”.
Inactive dyad (Thomas and Mary)
For the dyad who perceived themselves to be inactive, they spoke about both exercise and PA during their interviews, although neither aligned with their values or interests, and consequently there was no intention to engage in PA or purposeful exercise post-MI. Whilst both patient and family member appeared to engage in incidental PA, this was not considered active nor the same as purposeful exercise. They did not buy-in to the benefits of PA for health and due to the patient’s perceived unhealthy behaviours (i.e., sedentary lifestyle), the MI did not come as a surprise.
I can’t do what I was doing before
Restricted by mind and body
In the immediate aftermath following the MI, patients experienced a loss of autonomy over what their bodies could achieve post-MI, which left many feeling frustrated. Active patients reported how the MI had shaped and controlled their PA experiences as their bodies and mind restricted them from being able to engage in ‘life as it were’. The impact of the MI shifted active patients’ physical identity from fit and healthy to slow, frail, and breathless, characteristics they disassociated with themselves. Patients were aware of this shift and the interruptions it caused to their activities of daily living (e.g., unable to wash their car, go shopping, cut grass, walk dogs). This situation led patients to feel a sense of hopelessness, loss and decreased confidence, questioning whether to engage in physical tasks in case they caused harm (something that pre-MI did not cross their minds), highlighting patients’ vulnerability to their condition and loss of freedom:
I’ve always been fit and able to do anything…it’s like I would’ve never have done a bungee jump but now I definitely wouldn’t do one… it’s things like that where I’m thinking “is that putting me at risk?” which is something I didn’t concentrate on before (Julia, 1st interview).
Julia’s statement highlights how the MI caused her to question the way she interacted with the world. This sense of uncertainty/insecurity appeared restraining on her PA experiences. In contrast, Thomas, who saw himself as inactive, took comfort from the physical restrictions placed on him by the MI, as it provided a rationale for him to do what he enjoyed:
I was told to rest [post-MI] as that was the best recuperation…I didn’t argue with that [laughs], that’s what I enjoy, not exercise (1st interview).
Here, Thomas is accepting of what is expected of him during his initial recovery, informed by his own personal views of activity.
Regulation by family
All families recalled how during the early stages of recovery, they regulated patients’ PA, which was not always positive as it led to inadvertently promoting a sedentary lifestyle. As family cared for patients, they feared losing them to another MI, regulation was therefore used for preventative and protective purposes as told by Joanne (Alex’s family member):
I worry about him having another [MI] and I don’t know how I’d cope without him (1st interview).
Distinctions were evident in how family regulated patients’ behaviour and differed by PA identity. For Thomas and Mary, Mary protected Thomas through behaviours such as taking on his household chores. Conversely, for active families who felt PA would benefit patient health, regulation translated as monitoring PA frequency, intensity, time and type, allowing patients to be active but within parameters accepted by the family. If family perceived tasks to be potentially harmful (e.g., heavy lifting), or that patients had done enough (e.g., looking tired), they asked the patient to stop and rest. Many patients interpreted families’ behaviour as an act of love, although for some, these feelings co-existed with feelings of frustration at not being the ruler of their own destiny, which led to a loss of perceived autonomy:
…it’s “careful because there’s this, be careful cause there’s that”, which is frustrating sometimes because they’re [family] only thinking about you…but they [family] do watch me like a hawk (Doris, 1st interview).
Finding my way
Desire to be active and return ‘back to normal’
As time progressed, as did patients’ relationship with PA. For active patients, PA made them feel better, healthier and as though they were doing something, and it played a meaningful role in their experience of recovery. Physical activity was multi-functional, acting as a vehicle for recovery to help re-build strength lost through the MI and increasing life quality and quantity, helping them reach their goals of ‘returning to normal’, which appeared valued and important to achieve:
…being active has always helped me feel better, it has helped me recover from past injuries…I think it’ll just help me get back to normal and be active again (Alex, 1st interview).
For Alex, PA was purposeful, but his use of the phrase ‘return back to normal’ further intensified the dissonance between the reality of his current life and that of which he aspired to, which was also felt by many patients who identified as active.
It was important for patients who perceived themselves as active to have control of how they engaged in PA. Some patients opted to follow the traditional CR pathway, favoured due to the safe setting and knowledgeable staff. However, this only seemed apparent for phase 3, when asked about phase 4, many patients were not aware of its presence. Other patients opted to forgo PA within CR phases 3 and 4, deciding to do PA that fitted into their pre-existing routines, a decision based on personal assumptions of CR expectations and requirements. Given the desire to ‘return to normal’, CR for these patients did not appear a constructive use of time. Robert (whose latest MI had been his third) had attended CR twice in the past, recalling:
I know the exercises; I know the regime they do it in…so I didn’t really think it would benefit me…I’ll do the exact same exercises [in the gym] it’ll just be without the physiotherapist (2nd interview).
For Robert, his previous experience had equipped him to be more independent in his rehabilitation for his most current MI. Julia on the other hand (whose current MI was her first) viewed CR as a place for older and/or unfit MI patients, an image she dissociated with herself. Julia’s beliefs that CR was like “one flew over the cuckoo’s nest” (2nd interview) pertained to her belief she could achieve more from doing her own PA, than the perceived sedated activity prescribed during CR:
I think CR is alright for somebody whose older and isn’t very fit…and that’s not me… I’ve been told it’s easy really…so if it’s not very physical there’s no point doing it (1st interview).
In contrast, and aligned with his PA beliefs, Thomas expressed no desire to be active post-MI or ‘return back to normal’, especially given he felt the MI had no real impact on him. However, his PA behaviour differed from his spoken intentions. Although Thomas spoke about disliking activity (“…you may have guessed, we [Thomas and Mary] aren’t big believers in exercise….do you see those chairs [points to garden chairs], that’s the type of activity we like” (interview 1)), PA engagement was evident (“I’ve been preoccupied finishing my fencing, this is the activity I want, something [with] a meaningful end to it… “(interview 2)). For Thomas PA appeared to be a bi-product of doing activities that served a valued purpose and were therefore done for enjoyment rather than recovery:
I’m out in the garden and I love it, no extreme activity for the sake of it, if I die I want to die happy, not healthy (interview 3).
This may explain why Thomas did not perceive himself as physically active, activity for him was a means to an end rather than a conscious decision.
How much is too much PA?
Perceptions of patients’ PA abilities varied amongst patients and family members. These perceptions influenced the PA-related interactions between family members and patients, which were manifested through concern and advice from family members, and varying levels of acceptance on the part of patients.
Although Doris felt she could do a little more, she adhered to family advice of ‘slowing down’ (i.e., only engage in activity deemed appropriate) and appeared to do so out of an obligation to ‘do the right thing’ by family members. She was aware the MI had impacted on her family, thus taking on advice ensured no harm could come to them and disrupt family life further:
…you can’t be looked after [by your family] and then ignore what they are asking you to do, even if you think you can do different [laughs], so…I do what I’m told (3rd interview).
Doris’s feelings towards her family were evident. Her willingness to sacrifice her own PA wishes and be active within the parameters outlined by her family, demonstrated how her care for others overrode her own sense of self, providing insight into her own self-value in relation to others within her social network.
Challenges in PA behaviour arose for multiple reasons. In the months following patients’ MI, concerns over how much PA was too much PA was still felt by family members and consequently family continued to place restrictions on patients’ PA (e.g., questioning activities, telling patients to stop, asking patients to slow down or take frequent breaks). Patients challenged this belief because they felt only they knew their body’s ability and PA capacity, as stated by Sarah (Robert’s family member):
I sometimes think when [Robert] is trying to do something he’s pushing himself too hard and I have to try and say “that’s a bit too much for you” I guess at the moment it is always at the back of my mind is he going to have another one [MI] (Sarah, 2nd interview).
However, Robert felt otherwise:
It’s like when people tell me “don’t do too much”, what is too much?!…I feel like you’ve gotta push your body to understand what your limitations are (2nd interview).
Despite family concerns, decisions over their PA behaviour was important to patients and provided autonomy over their condition. These patients began experimenting with PA to help establish their own parameters, going through a process of trial and error (e.g., lowering PA expectations and intensity, slowing down, taking regular breaks and experimenting with new activities) to understand their body’s capabilities. For some, trial and error appeared a product of reduced PA ability, which for “active” patients caused feelings of frustrations and sadness at their body’s inability to work at the same capacity as pre-MI. In Julia’s account, comparisons between ‘now’ and ‘then’ were used to help her make sense of her PA ability, but also served as a reminder of being unable to meet her self-imposed PA expectations, which ignited feelings of frustration:
…it’s depressing to get up every day and not feel good as I thought I would…I thought I would feel like superwomen by now but I just don’t… I’m back walking the dogs but not like I used to…I’ve had to slow down (2nd interview).
Offering social support
As time progressed, family members within active dyads, came to understand the important role PA played in patients’ recovery and began supporting patients’ PA. Support included verbal encouragement, being active together, taking an interest, praising patients for PA, providing positive reinforcement (e.g., ‘you can do it’) and assisting patients with travelling to PA sessions. Many patients appeared to appreciate PA support from family, as it acted as additional encouragement, especially helpful to overcome feelings of demotivation or fatigue. Instrumental support (e.g., being active with patients), allowed family to observe patients’ PA and helped inform family of patients’ PA ability. The following statement details Robert’s experience of support from his family member, Sarah:
[Sarah] encourages me, sometimes I don’t want to do anything, but [Sarah] will suggest going for a walk or to the gym…and [as we’ve been going to the gym together] she’s more comfortable with what I do…she can see I’m not doing much more than her (2nd and 3rd interview).
Robert’s account displays how social support plays a dual purpose, not only shaping PA experiences but also how involvement may work to put families’ mind at ease.
Although support in many cases was offered as a direct means to encourage patients to be active, this was not the case for all families. For Thomas, who engaged in PA for the purpose of achieving a meaningful outcome, his family member (Mary) helped him complete these tasks, and therefore support was for the final outcome, rather than for the purpose of encouraging PA.
Accepting this way
This is me
Over time, patients started to accept the MI as part of their identity, however, the premise on which acceptance occurred differed amongst patients. Some patients experienced feelings of disappointment at coming to accept their PA ability may never be back to what it was:
I’m not as fit as I was 12 months ago…it’s depressing, but you’ve just gotta think…” the physical side isn’t as good as it was but that’s the way it has to be and that’s the way it will be” (Alice, 3rd interview).
Here Alice is accepting of her new PA ability, although indicates the challenges she faced during this process. Namely, the loss of her ‘old physical self’, to which her current self does not fulfil, causing feelings of ‘depression’.
Conversely, patients who had additional health concerns during their recovery appeared more willing of the acceptance process. Doris, who had experienced multiple falls during her recovery noted:
…do what you can with a happy heart…be strong enough to say ‘I’ve done enough now and I’m happy with that (3rd interview).
For Doris doing PA post-MI was about appreciating what her body could do as opposed to being disappointed in what it could not, and this sense of acceptance allowed her to have positive appreciation of her body’s ability.
Living with the consequences of the MI
Although physically the MI had happened to patients, it left a lasting impact on the family also. For Thomas and Mary, the MI had led to the long-term change of family relationships. For Thomas, whose daughter had forbidden him from engaging in any type of activity post-MI, there was inconsistency between his actual behaviour and what he was telling his daughter. Internal conflicts were apparent with him not wanting to upset his daughter, but also wanting to do as he wished. To have autonomy, but also adhere to his daughter’s wishes, dishonesty was used as a means to manage the disagreements and was evident into the longer term:
…my daughter’s theory is I should do nothing, you’ve had a heart attack…we [Mary and I] go along with it because we don’t want to upset our daughter…so we keep quiet about the things we do (2nd interview).
Immediately following patients’ MIs, family members feared another, however for active dyads, time reduced worry, with families witnessing patients engaging in PA with no negative consequences, as displayed by George (Julia’s family member):
…I’m not as worried as I was about [Julia engaging in PA] she’s [Julia] been walking the dogs and nothing ‘bad’ has happened to her (2nd interview).
Here, patients’ physical responses to PA gave indication of their physical wellness, and therefore dictated how family should feel about them engaging in PA. Although worry decreased, it never totally dissipated. As the MI had come unexpectedly for many, family worried that it could occur again. Worrying about something that ultimately was beyond families’ control was fruitless, and it appeared more important to enjoy every day rather than worrying about ‘what ifs’, as told by Joanne (Alex’s family member):
… because [Alex] had [MI] and we didn’t see any of warning signs…what will be will be…you can’t put your life on hold and say “we can’t do this” we just have to get on with things (3rd interview).
For Joanne and Alex, (referred through use of ‘we’) their positive outlook and attitude towards life influenced how they saw and managed worry. Living life for them outweighed living safely but living in fear.
Discussion
The purpose of this study was to explore the lived experiences of patients’ engagement with PA post-MI, together with the experiences of their family over time. We found that post-MI, patients go on a journey of PA re-discovery that is shared and influenced by the family. Patients appeared to leave pre-MI “normality,” characterised as being able to do what they wanted and when, and journeyed to a “new normality,” where patients were active but within parameters of their experiences of suffering the MI.
How patients viewed themselves in relation to PA appeared to influence how they experienced their journey of PA post-MI. Patients who identified as “active” appeared to experience feelings of anger, loss and frustration in relation to their perceived PA (in)abilities post-MI. The experiences of those active pre-MI support the premise of Kübler-Ross’s (1969) [Citation33] five stages of grief (denial, anger, bargaining, depression and acceptance) following forms of personal loss. In this study, patients’ loss appeared to centre on their pre-MI life and how they were restricted by their bodies during recovery. Post-MI, active families experienced disbelief, unable to understand how the MI had happened given the patient’s active lifestyle. This was followed with feelings of frustration, anger and annoyance as patients began to realise the reality of the situation and the impact on their lives. Bargaining was shown through patients’ desire to ‘return back to normal’, living with a lowered PA ability, hopeful it would help them return to their pre-MI life in the longer-term. The desire to ‘return back to normal’ has been reported elsewhere [Citation20], linking with a desire to readjust, a process allowing patients to move from an unfamiliar to familiar self. This transition was evident by some patients within the current study, but within a specific PA context. Some patients recognised they were unable to engage in PA in the same way as pre-MI which led to accompanying negative moods (e.g., depression), despondent at their PA inability. Over time, however, patients came to accept their body’s limitations, understanding they may never attain the same level of PA as pre-MI, and learning to live with a new PA identity. The process of grief and loss amongst chronically ill patients has been documented elsewhere [Citation20,Citation34]. Evidence suggests trauma can be interpreted as an attack on the self, which can lead individuals to lose a sense of their personal identity [Citation35]. Within the current study, patients who saw themselves as active questioned their identity, as the MI undermined how they perceived themselves, and how they were perceived by others (as healthy and active).
Evidence suggests PA identity is predictive of PA intention and behaviour [Citation36], and evident within the current study, where a noticeable discrepancy between the “active” and “inactive” families’ was observed in their approach to PA during patients’ recovery. Patients who identified as active pre-MI displayed motivation and intent to engage in PA during the course of their recovery, and over time, their behaviour mirrored their intent. However, both Thomas and his wife displayed a lack of intent to engage in PA and as such, did not perceive themselves as being physically active. Evidence suggests identity acts as a self-regulating mechanism of motivation [Citation37], which can act as a prompt to be active when people feel a disparity between their PA identity and PA behaviour. Many patients within the active dyads reported feeling a misalignment between their PA identity and PA behaviour post-MI that was evident through their desire to “return back to normal”. Post-MI, evidence suggests patients “re-orientate towards the active self” [Citation38] attempting to live life as they had pre-MI. However, this is thwarted by illness restrictions, ultimately leading patients to moderate/adapt their activities to regain a sense of their self. This proposed model of behaviour was displayed amongst patients in the current study, but they also experienced family as well as illness restrictions on their PA engagement. However, the model of readjustment as proposed by Brink and colleagues [Citation38], only reflected patients’ readjustment five months post-MI. The findings from this current study propose an extension to this model, suggesting an acceptance phase following the moderation/adaptation of PA behaviour, with patients going on to accept a lowered PA ability. Also interesting was how families’ health beliefs fed into their identity formation (e.g., active families believed that PA was good for health and were shown to be physically active). Our research with health practitioners working with MI patients [Citation39] suggests that familial health beliefs play a valuable role in underpinning how both patients and their family members respond to PA post-MI. It is therefore reasonable to assume that such beliefs may have influenced participant responses in the current study. Whilst the wider influences on PA identity (outside of a family context) were not discussed by participants, it is worthwhile to acknowledge that wider social (e.g., peer networks), cultural (e.g., religious beliefs) and environmental (e.g., accessibility to health information) factors inform our health beliefs and as such, provides a context for how we interpret and respond to illness [Citation40]. Therefore, whilst acknowledging patients and their families’ PA identity is important, taking time to understand factors that underpin their identity (e.g., health beliefs), and how these are influenced by wider societal influences, may be worthwhile to help ensure patients achieve optimum health outcomes.
Thomas (who did not see himself as active) displayed a lack of intention to engage in PA, although his identity and intention did not always match. Evidence suggests older adults are more likely to engage in incidental PA (i.e., for leisure), which they may not perceive as activity [Citation13,Citation41]. For Thomas and Mary, this was evident through the garden fence and pond built during the course of Thomas’ recovery, this was primarily for the enjoyment gained from the task itself, rather than from the PA which came secondary. Consequently, it is perhaps sensical that these activities were not perceived as PA, however, does highlight the importance of education around what constitutes PA following MI.
Overprotection is considered a support style within the context of heart disease [Citation42], with one form involving restricting patients in performing certain activities [Citation43]. Within this study, family members expressed concerns over how much, and what activities patients should do, which led them to regulate patients’ PA behaviour in fear of a reoccurring MI. As with other studies exploring relationship dynamics in cardiac illness [Citation43], overprotective behaviour could be explained as a coping mechanism for families to avoid the emotional turmoil of observing the patient experience another MI. It is also possible this overprotection behaviour was influenced by the historic perception that “bedrest is best” post-MI. This was evident in Thomas’s perception that he was advised to “rest” and in his daughter’s “forbidding” of any PA. It is now well established that PA post-MI has numerous benefits including reduced cardiac mortality [Citation4], so it is important these messages are portrayed to the family, and their concerns addressed so they feel able to support patients to become physically active.
As patients’ recovery progressed, family members in this study demonstrated support for patients’ PA behaviour that can be aligned to Uchino’s [Citation44] definitions of emotional support (e.g., providing a rationale for being active, encouragement without making demands, praise for being active and being active together), tangible support (e.g., taking patients to CR PA classes) and belonging support (e.g., being active together). These activities were in turn shown to have a positive impact upon patients’ PA engagement, and further support the premise of planned behaviour, social cognitive and self-determination theories, whereby social support from others can positively influence PA engagement, when delivered in a constructive, nurturing and supportive manner [Citation19,Citation21]. As might be expected, it was family members whose own beliefs aligned with PA that were most supportive of patients’ PA engagement. Pertaining to familial theories that partners’ health behaviours can co-occur through mutual interest [Citation45–46], it is possible that social support came from understanding the value of PA to help enhance health and cardiovascular risk factors. Given the potential influence of patients’ immediate social environment on PA, promoting the involvement of family within CR may help promote patient PA engagement. However, given that the provision of support may depend on how family view themselves in relation to PA, it may also be worthwhile exploring ways to work with families to promote positive health beliefs.
Post-MI, CR is actively encouraged to not only enhance patients’ health outcomes through the engagement and promoting of positive health behaviours, but to also help reduce cardiac reoccurrence [Citation6]. Interestingly, only three of the patients interviewed attended the exercise component of phase 3 CR, whilst no patients reported attending phase 4. Although patients did not discuss their rationale for not attending phase 4, they did for phase 3. Thomas discussed his lack of desire for activity, Robert felt the knowledge he had gained from his previous attendance put him in a position where he could do the exercises but not in a CR setting, whilst Julia’s self-perception of fitness influenced her decision, perceiving herself to be fitter than other cardiac patients. Interestingly, social comparisons with those they perceive to take part in CR, and the impact this has on CR attendance has been previously documented [Citation47–48]. So, whilst evidence suggests that CR can be of huge benefit to those following a cardiac event [Citation4], poor attendance rates can mean that they often fail to serve all those who are in need. Given that our findings suggest factors occurring outside of patients’ family units also influence patients’ PA engagement, further work is needed to explore these barriers and how they might be overcome to encourage CR attendance.
Strengths and limitations
This study is the first longitudinal study to interview both post-MI patients and family to explore the PA experiences of patients post-MI and how PA may change over the course of patients’ recovery. Conducting interviews with both post-MI patients and family members provided a novel dual-perspective insight into family roles in shaping patients’ PA experiences. It must however be noted that all participants in this study were over the age of 50 years, of White British descent, and 5/6 families perceived themselves as being active. Consideration must therefore be taken when applying the findings to other populations.
Conclusion
This study provided a longitudinal insight into patients’ lived experiences of PA post-MI, together with the experiences of their family. We found that following MI, patients went on a journey of PA rediscovery, and family accompanied patients on this journey and influenced how it was experienced. However, how the family were involved within patients’ PA journey was complex, varying based on factors such as their PA identity, beliefs and MI reoccurrence, which impacted upon the support they provided which was both positive and negative in nature. Physical activity post-MI is a dynamic and interactive process, where the family can be instrumental. To help ensure the support families provide to patients encourages engagement in PA it may be worthwhile involving family in patient conversations around PA, including what PA is appropriate and how this may relate to their pre-MI PA, and how this may change over time. Building on positive supportive behaviours such as verbal encouragement and being active together may also be worthwhile, as well as working with families to reduce temptation to (over)regulate patients’ PA.
Supplementary Material 3
Download MS Word (277.6 KB)Supplementary Material 2
Download MS Word (41.3 KB)Supplementary Material 1
Download MS Word (56.7 KB)Acknowledgements
The authors would like to extend their thanks to Liverpool John Moores University who funded the research through a University scholarship awarded to [SB]. Further, the authors express their thanks to all of the participants who took their time to take part in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so support data is not available.
References
- World Health Organisation. The top 10 causes of death. 2018 [cited 2019 Jun]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
- Ashley EA, Niebauer J. Cardiology explained. London: Remedica; 2004.
- Brieger DB, Chew DPB, Redfern J, et al. Survival after an acute coronary syndrome: 18-month outcomes from the Australian and New Zealand SNAPSHOT ACS study. Med J Aust. 2015;203(9):368–368.
- Dalal H, Doherty P, Taylor R. Cardiac rehabilitation. BMJ. 2015;351:h5000.
- Casperson CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131.
- British Association for Cardiac Rehabilitation and Prevention. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation. 2017 [cited 2019 Jun]. Available from: http://www.bacpr.com/resources/AC6_BACPRStandards&CoreComponents 2017.pdf
- Bäck M, Hansen TB, Frederix I. Cardiac rehabilitation and exercise training recommendations. Cardiac rehabilitation: rationale, indications and core components. 2017 [cited 2020 Nov]. Available from: https://www. escardio.org/Education/ESC-Prevention-of-CVD-Programme/Rehabilitation
- Clark AM, Hartling L, Vandermeer B, et al. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–672.
- Karmali KN, Davies P, Taylor F, et al. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database of Syst Rev. 2014;(25):CD007131.
- Rogerson MC, Murphy BM, Bird S, et al. “I don’t have a heart”: a qualitative study of barriers to and facilitators of physical activity for people with coronary heart disease and depressive symptoms. Int J Behav Nutr Phys Act. 2012;9:140.
- Treiber FA, Baranowski T, Braden DS, et al. Social support for exercise: relationship to physical activity in young adults. Prev Med. 1991;20(6):737–750.
- Kouvonen A, De Vogli R, Stafford M, et al. Social support and the likelihood of maintaining and improving levels of physical activity: the Whitehall II Study. Eur J Public Health. 2012;22(4):514–518.
- Smith LG, Banting L, Eime R, et al. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14(1):56.
- Ajzen I. From intentions to actions: a theory of planned behaviour. In Kuhl J, Beckmann J, editors. Action control. Berlin: Springer; 1985.
- Kim J, Dunn E, Rellinger K, et al. Social norms and physical activity in American and Canadian contexts: a scoping review. Int Rev Sport Exerc Psychol. 2019;12(1):26–48.
- Bandura A. A social cognitive theory of personality. In: Pervin L, John O, editors. Handbook of personality. 2nd ed. New York: Guilford Publications; 1999.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development and wellbeing. Am Psychol. 2000;55(1):68–78.
- Teixeira PJ, Carraça EV, Markland D, et al. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:78.
- Rosland AM, Heisler M, Piette JD. The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review. J Behav Med. 2012;35(2):221–239.
- Astin F, Horrocks J, Closs SJ. Managing lifestyle change to reduce coronary risk: a synthesis of qualitative research on peoples’ experiences. BMC Cardiovasc Disord. 2014;14:96.
- Kärner AM, Dahlgren MA, Bergdahl B. Rehabilitation after coronary heart disease: spouses’ views of support. J Adv Nurs. 2004;46(2):204–211.
- Franks MM, Stephens MAP, Rook KS, et al. Spouses’ provision of health-related support and control to patients participating in cardiac rehabilitation. J Fam Psychol. 2006;20(2):311–318.
- Astin F, Atkin K, Darr A. Family support and cardiac rehabilitation: a comparative study of the experiences of South Asian and White-European patients and their carer’s living in the United Kingdom. Eur J Cardiovasc Nurs. 2008;7(1):43–51.
- Reid J, Ski CF, Thompson DR. Psychological interventions for patients with coronary heart disease and their partners: a systematic review. PLoS One. 2013;8(9):e73459.
- VanderKaay S, Moll SE, Gewurtz RE, et al. Qualitative research in rehabilitation science: opportunities, challenges, and future directions. Disabil Rehabil. 2018;40(6):705–713.
- Charmaz K. Premises, principles, and practices in qualitative research: revisiting the foundations. Qual Health Res. 2004;14(7):976–993.
- Smith JA, Flowers P, Larkin M. Interpretative phenomenological analysis: theory, methods and research. London: Sage; 2009.
- Smith JA, Osborn M. Interpretative phenomenological analysis. In: Smith JA, editor. Qualitative psychology: a practical guide to research methods. 2nd ed. London: Sage; 2008.
- Røysland I, Friberg F. Unexplained chest pain and physical activity: balancing between existential uncertainty and certainty. Qual Health Res. 2016;26(2):215–226.
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237–269.
- Reczek C. Conducting a multi family member interview study . Fam Process. 2014;53(2):318–335.
- Smith B, McGannon KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol. 2018;11(1):101–121.
- Kübler-Ross E. On death and dying. New York: The Macmillan; 1969.
- Charmaz K. Loss of self: a fundamental form of suffering in the chronically ill. Sociol Health Illn. 1983;5(2):168–192.
- Thompson N, Walsh M. The existential basis of trauma. J Soc Work Prac. 2010;24(4):377–389.
- Rhodes RE, Kaushal N, Quinlan A. Is physical activity a part of who I am? A review and meta-analysis of identity, schema and physical activity. Health Psychol Rev. 2016;10(2):204–225.
- Husband CJ, Wharf-Higgins J, Rhodes RE. A feasibility randomized trial of an identity-based physical activity intervention among university students. Health Psychol Behav Med. 2019;7(1):128–146.
- Brink E, Karlson BW, Hallberg LRM. Readjustment 5 months after a first-time myocardial infarction: reorienting the active self. J Adv Nurs. 2006;53(4):403–411.
- Birtwistle SB, Jones I, Murphy R, et al. Family support for physical activity post-myocardial infarction: a qualitative study exploring the perceptions of cardiac rehabilitation practitioners. Nurs Health Sci. 2021. DOI:10.1111/nhs.12806
- Nielson-Bohlman L, Panzer AM, Kindig DA. Health literacy: a prescription to end confusion. Washington: National Academies Press; 2004.
- Adams KB, Leibbrandt S, Moon H. A critical review of the literature on social and leisure activity and wellbeing in later life. Ageing Soc. 2011;31(4):683–712.
- De Ridder DTD, Schreurs KMG, Kuijer RG. Is spousal support always helpful to patients with asthma or diabetes? A prospective study. Psychol Health. 2005;20(4):497–508.
- Dalteg T, Benzein E, Fridlund B, et al. Cardiac disease and its consequences on the partner relationship: a systematic review. Eur J Cardiovasc Nurs. 2011;10(3):140–149.
- Uchino BN. Social support and physical health: understanding the health consequences of relationships. New Haven: Yale University Press; 2004.
- Franks MM, Shields CG, Lim E, et al. I will if you will: similarity in married partners’ readiness to change health risk behaviors. Health Educ Behav. 2012;39(3):324–331.
- Cobb LK, Godino JG, Selvin E, et al. Spousal influence on physical activity in middle-aged and older adults: the ARIC study. Am J Epidemiol. 2016;183(5):444–451.
- Jones LW, Farrell JM, Jamieson J, et al. Factors influencing enrolment in a cardiac rehabilitation exercise program. Can J Cardiovasc Nurs. 2003;13(1):11–15.
- Clark AM, Barbour RS, White M, et al. Promoting participation in cardiac rehabilitation: patient choices and experiences. J Adv Nurs. 2004;47(1):5–14.