Abstract
Purpose
The study aimed to explore the self-perceived cognitive status and cognitive challenges associated with lifestyle changes in cardiac rehabilitation among elderly myocardial infarction (MI) patients (≥65 years). Further, the study explored coping strategies developed to manage these challenges in the everyday life.
Methods
Nine patients were included in the study. Data were collected by telephone or in person, between 6 and 12 weeks post MI, using semi-structured interviews. Data were analysed inductively, using thematic analysis.
Results
Four major themes were identified, highlighting elderly MI patients’ experiences of their cognitive status and cardiac rehabilitation management: (1) A change in cognition over time, (2) Situating the MI within a challenging and changing life context, (3) Navigating the hurdles of cardiac rehabilitation, and (4) Being seen within the healthcare system.
Conclusion
Elderly MI patients are situated in a complex life context, dealing with a transition to retirement, multiple health issues and age-related cognitive decline. In this context, the MI experience is marginalised, and cognitive decline normalized. By adopting individually tailored interventions and improving healthcare provider continuity and accessibility, cognitive challenges associated with cardiac rehabilitation could be easier to overcome.
Self-perceived cognitive impairment, in particular regarding memory, seems fairly common among elderly MI patients and should likely be identified prior to hospital discharge in order to optimize the prospects of self-care.
There seems to exist an unmet need to implement the practice of individually adapted education and information further, in accordance with current recommendations for elderly cardiac patients.
The overall health and cognitive status, social network and the objective living conditions (e.g., distance from service and housing) should be taken into account when planning the patient’s cardiac rehabilitation management.
Healthcare providers likely need to strengthen the continuity of care and increase its accessibility for elderly MI patients, in particular following the transfer from hospital care to local health centres.
IMPLICATIONS FOR REHABILITATION
Introduction
Ischaemic heart disease (IHD) is one of the leading causes of morbidity and premature death globally [Citation1]. However, trends in mortality have been decreasing during the last decades [Citation2], and the onset of disease increasingly occur in old age [Citation3]. The average age of first onset of myocardial infarction (MI), one of the clinical manifestations of IHD, is >70 years in high-income countries [Citation3]. It is well established that elderly patients have an elevated risk of adverse outcomes following an MI, which may contribute to prolonged hospitalization and a consecutive deterioration of the patients’ health status and independence. In addition, elderly patients are more likely to have additional comorbidities prior to the onset of cardiovascular disease [Citation4,Citation5].
Mild cognitive impairment (MCI) is one of the most common comorbidities, estimated to affect approximately one-fifth of the elderly population (≥71 years) [Citation6]. MCI is commonly referred to as a transitional stage between normal cognitive function and dementia (e.g., Alzheimer’s disease) [Citation7]. The decline in cognition is often gradual, associated with ageing [Citation8], and may affect one or several cognitive domains, including memory, executive function, and attention [Citation9]. To meet the general criteria for MCI, a patient should have an abnormal cognitive function but not fulfil the diagnostic criteria for dementia; a self-perceived cognitive decline combined with deficits on objective cognitive tasks; and largely preserved functional capacities [Citation7]. Various possible aetiologies for MCI have been identified, including degenerative, psychiatric, and cardiovascular causes [Citation10]. In fact, coronary heart disease has been associated with an increased risk of cognitive impairment [Citation11], with an estimated prevalence of up to around 50% among cardiac patients [Citation12,Citation13].
An MI may significantly impact a person’s daily life due to subsequent morbidity, functional limitations, and psychological distress [Citation14,Citation15]. In addition, secondary prevention measures, aiming to decrease the risk of recurring cardiac events and increase the quality of life [Citation16], may introduce additional demands in the form of lifestyle changes and adherence to new medical regimens. International consensus guidelines for cardiac rehabilitation in older patients highlight behavioural interventions, including the promotion of physical activity, exercise training, nutritional counselling, weight management, and smoking cessation [Citation17], on top of evidence-based medication. However, despite counselling and support, changing lifestyle following an acute coronary syndrome has been proven challenging [Citation18–20], and probably even more so for patients suffering from simultaneous MCI. In fact, maintenance of disease-related knowledge and treatment adherence have both been associated with patients’ cognitive performance and functioning [Citation21,Citation22]. Furthermore, MCI has been found to negatively affect self-care management in chronic diseases, including heart failure and obstructive pulmonary disease [Citation23–25]. The current knowledge concerning self-perceived cognitive challenges among elderly MI patients is, however, limited.
Considering the increased risk of adverse outcomes [Citation4,Citation5], participation in cardiac rehabilitation constitutes a key secondary preventive measure for elderly patients, contributing positively to functional capacity and level of physical activity; attainment and maintenance of an independent lifestyle; as well as a decreased risk for re-infarction and mortality [Citation16,Citation26–28]. However, elderly patients, and especially patients with cognitive impairment, are less prone to participate in cardiac rehabilitation programs compared to younger patients [Citation4,Citation12,Citation27]. Several underlying reasons for the low participation rate have been suggested, including suboptimal referral, limited awareness, inconvenience, and deterrence by existing health problems [Citation12,Citation27].
Furthermore, overconfidence in the curative role of medical interventions among elderly patients, sometimes renders the belief that no additional lifestyle changes are necessary [Citation29]. These misperceptions indicate that patient information is interpreted differently than intended and potentially lowers the engagement in self-care activities.
Qualitative research has identified various coping strategies utilised by patients to manage cognitive impairment in daily life [Citation30,Citation31]. There are, however, a lack of studies exploring the perceptions and experiences of cognitive challenges associated with cardiac rehabilitation among elderly patients with MI, and how these are managed. A deeper understanding of these aspects will provide valuable knowledge in order to design tailored rehabilitation programmes, facilitate participation and improve adherence to rehabilitation among elderly MI patients.
Aim
The study aims to explore the self-perceived cognitive status as well as cognitive challenges associated with cardiac rehabilitation among elderly MI patients (aged ≥65 years). Further, the study aims to explore strategies developed among elderly MI-patients in order to cope with these challenges in the everyday life.
Research questions
How do elderly MI patients perceive their cognitive status?
What are the cognitive challenges experienced by elderly MI patients?
How do elderly MI patients cope with cognitive challenges associated with cardiac rehabilitation?
Methods
Study design
This study is a sub-study within the clinical MIMCI project (Myocardial infarction and Mild Cognitive Impairment), with the overarching aim to explore the prevalence of cognitive impairment among elderly MI patients and the impact of cognitive status on cardiac rehabilitation. By exploring the experiences, meanings, and realities of the patients [Citation32], this study will fill an important gap in the literature, providing information on the perceived self-care capability among elderly MI patients.
Setting, participants, and procedure
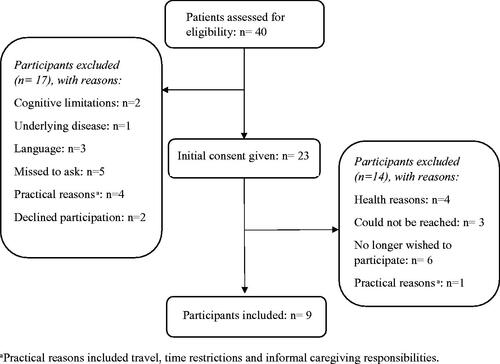
Patients were recruited between August and December 2019. A purposive sampling technique was deemed appropriate, where patients were chosen due to their age and disease-specific characteristics and experiences, which would enable a detailed exploration of the research questions at hand [Citation33]. The following criteria for inclusion were applied: (i) age ≥65 years, (ii) confirmed MI diagnosis. The following criteria for exclusion were applied: (i) confirmed dementia diagnosis, (ii) other pre-existing serious health condition(s) that could cause difficulties in participation or in the interpretation of the findings, and (iii) difficulties with written and/or spoken Swedish. Cardiac nurses, who were well informed of the aim of the study, approached eligible patients at their follow-up appointment at Uppsala University hospital scheduled 2 weeks post-MI. Patients received verbal information of the ongoing study, and if willing to participate, additional written information was distributed describing the study aim and methods further. For inclusion process details, see .
Data collection
Out of 23 approached patients, nine patients were included. For detailed demographic characteristics, see . Data collection by semi-structured interviews was performed between October 2019 and January 2020, within the range of 6–12 weeks post-MI. Interviews were conducted by TL, over the telephone or in-person depending on patient preference. Interviews were conducted in Swedish, were audio-recorded, and lasted between 30 and 60 min. In the two cases where the interviews were conducted in person, the interviewer met with the participant in a private meeting room at the interviewer’s office, in accordance with the respondents’ preferences of practicality. Data collection proceeded until saturation was reached when no new information seemed to emerge from the interviews.
Table 1. Demographic characteristics of participants.
Ethical considerations
The MIMCI project has been granted ethical approval from the Regional Ethics Review Board in Uppsala (project number 2016/261). Written informed consent was obtained at the time of recruitment, and additional verbal consent was obtained at the time of the interview and audiotaped for verification. Prior to the interview, patients received a letter with written information about the study, contact information to the research team, and a specification of time and mode of interview. At the time of the interview, patients received additional verbal information about anonymity and the voluntary basis of participation, including the right to withdraw from the study at any time without having to specify why along with the opportunity to ask questions.
Data analysis
Audio files were transcribed verbatim and cross-checked with the corresponding audio files for accuracy. The text files were then imported into the qualitative data analysis software NVivo 12 Pro (QRS International Pty Ltd., Australia). Data were analysed inductively, using thematic analysis following the six phases described by Braun and Clarke [Citation32]. In order to minimize the risk of bias, the initial coding and development of categories were performed separately by the first and last authors (TL and EO). See for a sample of data extracts and their corresponding codes.
Table 2. Data extract, with codes.
When initial categories had been formulated the first, second, and last authors (TL, SJP, and EO) met to discuss and compare the emerging findings, to obtain consensus, and to develop overarching and interpretative themes. When differences in opinion occurred in regards to the interpretation or implications of the data, these were discussed until consensus was reached. Once the initial themes were developed, all authors discussed the structure of the themes as well as the hierarchy and relationship within and between the themes. For coding tree extract, see .
Table 3. Coding tree extract: Theme 3
Reflexivity and rigour
The interviewer, TL, has a professional background in nursing and clinical experience in performing and evaluating rehabilitation activities as well as caring for elderly patients and their family members. EO, is a licenced psychologist and associate professor at Uppsala University, he has vast experience in behavioural cardiology research focusing on psychosocial risk factors for, and psychological interventions following, cardiovascular disease. Several steps were taken to ensure the relevance and validity of the study, as well as to limit the risk of bias due to analyst preconceptions [Citation34,Citation35]. The additional research team consisted of members with various backgrounds and expertise; including qualitative research methodology (SJP); cardiology, including healthcare management of MI patients (CH); and psychology, including cognitive assessment of geriatric patients (JW). To ensure the accuracy and relevance of the interview guide, (i.e., measurement validity) [Citation36], feedbacks were given by the co-authors during its development. In addition, two pilot interviews were conducted in September 2019 with patient representatives from the Swedish Heart and Lung Association; representing opportunities to evaluate and receive feedback on the interview-guide and review its content accordingly. Triangulation through multiple analysis was performed in order to ensure the internal validity of the study [Citation36], including regular meetings within the research team and co-author peer-review of article manuscript. Moreover, field notes, combined with continuous memoing, were performed in order to sustain an audit trail [Citation37] and keep a record of emerging analytic ideas. The authors have strived to provide a detailed description of the study design, data collection, and analysis as a measure to ensure external validity and to facilitate the judgement of the finding’s transferability to similar settings [Citation35].
Results
Four major themes were identified in the analysis: (1) A change in cognition over time, (2) Situating the MI within a challenging and changing life context, (3) Navigating the hurdles of cardiac rehabilitation, and (4) Being seen within the healthcare system. Translated quotations are provided to support the findings.
Theme 1: a change in cognition over time
The first theme illustrates patients’ experiences of cognitive decline as a downhill slope with changes in cognition over a long period of time. Even though cognitive impairments are evident, these were generally perceived to be minor with a small impact on everyday life.
Among patients, cognitive decline is often described as a slow process with symptoms present during a period of between 3 and 20 years. Hence, cognitive decline is not perceived to be associated with the MI itself:
[…] it isn’t something that has appeared in connection to this heart attack, it is rather something that has been sneaking up on me for maybe 20 years, I should think, or I shouldn’t say 20 years but it is at least a longer time span than since the heart attack (Male, 77 years)
Memory difficulties, was the cognitive issue most clearly articulated by the patients, commonly manifesting as issues remembering instructions or written text. Moreover, patients frequently describe difficulties retrieving common words or names in conversations with others. Attention and planning abilities are commonly perceived to be less affected by cognitive decline. However, some patients experience concentration difficulties as well as impaired planning abilities over time, with a lack of engagement and impaired initiative:
And in that sense you can say that the planning ability, it’s still there but it it takes a little bit longer between the point when you decide something until you actually do it. Time spans that have been stretched out a bit… (Male, 78 years)
While a majority of the patients perceive the most important cognitive functions to be intact, and consequently, a limited impact on their everyday lives, some experience their cognitive decline as challenging. At times, limitations in the capability to perform daily tasks cause emotional distress and a negative impact on the self-image. Whether this lack of initiative is stemming from cognitive decline in executive functioning, or underlying emotional distress or a combination thereof is, however, at times difficult to distinguish.
Theme 2: situating the MI within a challenging and changing life context
The second theme illustrates contextual factors that influence patients’ perceptions of their MI and their cognitive status. The age-specific context in which the patients are situated is at times experienced as challenging, and underlying diseases and concurrent life events, such as the transmission into retirement, tend to overshadow the MI in perceived severity and impact.
Patients describe being struck by the MI at a time in life when other health conditions are prevalent (see ). For some, underlying physical and psychological conditions have a significant impact on the health and well-being, causing limited mobility, pain, and depressive mood. Consequently, these conditions tend to overshadow the perceived impact of the MI itself, as highlighted by one participant talking about his cancer diagnosis:
[…] yes I have another disease that I perceive as worse, that is that have affected me more, and that is that I have prostate cancer (Male, 77 years)
At times, patients speculate whether simultaneous health conditions could be underlying causes of cognitive change. However, a decline in cognitive abilities is frequently looked upon as a normal change, associated with ageing. This view of normality is at times reinforced in the comments from family members and in comparisons with others at the same age. For some, cognitive challenges, in particular memory difficulties, become a part of the persona and a source of humour and inside jokes together with family members or friends experiencing the same challenges.
Furthermore, the transition from working life to retirement entails a readjustment to new normality with altered cognitive demands. While working, the patients were subjected to intellectual stimulation, which was argued to uphold and maintain cognitive abilities. Whereas retired life contributes with less of this cognitive stimulation:
[…] when you’re still working, then you’re using the brain or in a completely different way. You were busy then and there, there was like a break then when you stopped working. […]. With the mental exercise if I say so. And that that isn’t good I think, I think that it makes you unwell (Male, 77 years)
Theme 3: navigating the hurdles of cardiac rehabilitation
Patients are engaged in self-care activities to a large degree, adapting activities to their own capabilities and preferences. Some highlight cardiac rehabilitation programmes as the starting point of change for the better. However, performing lifestyle changes is not always easy and patients describe several strategies utilised in order to cope with challenges associated with their cardiac rehabilitation.
Following their MI, a majority of patients describe having participated in organized physical activities and received advice from healthcare professionals in regards to their self-care management. Reflecting on their experiences from the cardiac rehabilitation programs, views are positive and patients describe how advice received is put into practice in their daily lives. Overall, the patients have a positive perception of their self-care capability following the MI. Even so, cognitive challenges associated with cardiac rehabilitation are experienced to a varying degree. For some, these challenges become evident while trying to follow the instructions provided by healthcare staff. In particular, the introduction of new medicines can cause difficulties remembering their names, dosages, and administration times. Furthermore, understanding and remembering information received by healthcare professionals, in general, can constitute an additional cognitive challenge.
Some patients narrate how motivation and interest in a specific task improve cognitive functions, including memory and concentration abilities. However, a lack of motivation for rehabilitative activities, paired with physical challenges including adverse effects of medications, constitute common barriers to initiate and participate in cardiac rehabilitation and self-care activities. The negative impact of these barriers are largely perceived to exceed that of additional cognitive challenges, as described by one participant experiencing fatigue due to respiratory issues:
There is an element of impaired memory and planning as I mentioned but… I don’t think that’s the primary thing. The primary thing for me is… It is respiration […] And especially respiration during the night time […] And that is difficult really, it is (Male, 72 years)
In order to succeed with their cardiac rehabilitation, despite existing challenges, patients utilize several coping strategies. Individual strategies to handle cognitive limitations have often evolved over time, and following MI these strategies are applied to issues related to cardiac rehabilitation management. In order to support declining memory capacities patients utilise digital reminders and note taking as facilitating means, setting phone alarms at medication times and taking notes of medication names and doctors’ appointments. Furthermore, one participant describes practising note-taking at meetings with healthcare staff in order to remember instructions. Following clear routines is also mentioned as a measure to manage cognitive limitations. Routines include self-care activities such as exercise and management of medications, which often are administrated in the same manner every day.
Furthermore, patients frequently describe the importance of social support in the context of cardiac rehabilitation. This includes practical and emotional support from friends, fellow patients, and family members. Foremost, patients highlight the importance of support from the partner/spouse, in regards to practicalities, life-style changes, and emotional support:
Yes, we’re talking about these kind of things. I’m not keeping dreams from her and she’s not keeping dreams from me. Those conversations are incredibly important, naturally. So it’s not just that she’s there for me but we’re… trying to help each other to make sense of things (Male, 78 years)
Theme 4: being seen within the healthcare system
In addition to the individual challenges described in the previous theme, patients highlight several challenges associated with the healthcare provided following their MI. These include structural challenges within the healthcare system as well as interpersonal challenges in the contact with healthcare staff. This theme explores these challenges and highlight actions and interventions with the potential to facilitate cardiac rehabilitation management and adherence among elderly MI patients.
Among patients, inadequate communication and information from healthcare staff, including limited opportunities to communicate pressing issues, and lacking information were at times perceived as troubling. In addition, cognitive difficulties in processing information, mentioned in the previous theme, could be exacerbated further by the perceived lack of appropriate explanations from physicians:
The physicians that I’ve met have taken things for granted; they say something and then you’re supposed to know what it means […] (Male, 78 years)
Furthermore, limited accessibility, with issues getting hold of the same healthcare provider again, difficulties booking telephone appointments, and a lack of service in general cause frustration. In particular, patients describe a lacking healthcare provider continuity in their post-MI care at the local health centres, commonly due to a large degree of movement of staff between different health facilities.
A perceived lack of continuity, alongside experiences of previous negative events, including symptoms not being taken seriously, not getting one’s heart examined in time, and disappointment regarding diagnosis, could serve as contributors to a lacking trust for the health care services provided. The challenges mentioned above emphasize the responsibility that is placed on the patient as a care recipient. According to some patients, there is a need to be active in the seeking of care, to be attentive, motivated, and have the ability to speak up to receive adequate care. Moreover, practical barriers associated with schedule and arranging transportation impact cardiac rehabilitation attendance for some patients.
In contrast, several patients describe positive aspects of the health care received at the time of the MI, stemming from a sense of trust and support as well as feelings of being well cared for and under close supervision. Furthermore, the importance of receiving adequate and timely information from healthcare staff was emphasized. One patient described a positive experience receiving information from a cardiac nurse, two days following the MI:
[…] it was really attentive and good that, the point in time was well-chosen. Because then you’ve had the time to think a bit and then you get a lot of information right when you have started to think. The information, if it comes right away, that might not be so good, because it’s too close. It was a suitable time span (Male, 78 years)
At times, additional healthcare support was found in the patients’ personal network, which could replace or complement the formal care received. Private health consultations could maintain a sense of continuity, provide additional information and reduce anxiety. Furthermore, patients described how partners could take on the role of informal caregivers, providing information and overseeing adherence to dietary recommendations and medications.
Increased access to physicians in order to pose questions related to the MI and self-care would facilitate cardiac rehabilitation management, according to the patients. One patient raised the suggestion to create an internet portal as a mean to increase accessibility for cardiac patients:
Because it wouldn’t be a strange thing really to build an internet portal actually where you could enter your questions really, if they do it like that for a specific physician, that you’ve had contact with perhaps six months after you’ve had this heart attack. […]. Because that would, I’m totally convinced, would give a sense of safety to all really who have been subjected to this (Male, 70 years)
Furthermore, providing easily accessible writing materials at healthcare visits and digital reminders for health care appointments, are mentioned as important facilitators with the ability to overcome challenges associated with cognitive limitations.
Discussion
The present study sought to fill a gap in the literature by exploring the self-perceived cognitive status among MI patients (≥65 years) and its impact on their cardiac rehabilitation management. Furthermore, the study has highlighted perceived challenges and facilitators for adherence to self-care recommendations. The interviews revealed that the participants experienced cognitive decline, especially related to memory abilities. This is in line with previous research [Citation38], where a high prevalence of undiagnosed cognitive impairments has been found among cardiac patients.
The risk of a negative impact on health and well-being following an MI is well documented in the literature, including a risk of depression and anxiety [Citation14,Citation15]. However, the majority of participants reported a limited emotional impact following their MI. In fact, within the participants’ age-specific, and at times complex, life context neither cognitive decline nor the MI were perceived as particularly limiting to their health or in their daily lives. Instead, participants described how other physical and psychological issues constituted larger challenges, both in regards to daily activities and in the context of cardiac rehabilitation.
Moreover, the tendency to normalise cognitive decline, and describe it as an anticipated aspect of aging, was common. These expressions are in line with the concept of biographical flow, coined by Faircloth et al. in their study on stroke recovery [Citation39], aiming to better understand illness as a part of ongoing life. Biographical flow highlights how the significance of the illness process depends on the patient’s biography, including age, other health concerns, and previous knowledge of the illness [Citation39]. Hence, the onset of chronic diseases, such as MI, does not necessarily need to cause a drastic disruption in the daily life of the patient affected. Similar tendencies to normalise the illness experience has been identified in previous research, for example among elderly patients living with multiple chronic conditions [Citation40].
Despite the overall subjective perception of well-functioning cardiac rehabilitation management, the patients’ narratives indicate that cognitive limitations at times constitute a hindrance to receive optimal post-MI care. This includes issues related to patient-care provider communication, such as difficulties processing information and a lack of pedagogical skills among physicians. The importance of well-functioning communication has been highlighted by Esmaili et al. [Citation41]. In their research, they identified well-functioning communication as a core component of a patient-centred care among cardiac patients, with the potential to relieve stress and build a trusting patient-caregiver relationship. Moreover, meaningful and informative communication has been highlighted as essential for patients’ satisfaction with care and empowerment [Citation42], allowing access to the spiritual and emotional resources needed to cope with life-threatening diseases [Citation43]. This indicates a large potential of interventions aiming to improve patient-caregiver communication within healthcare settings. Our findings suggest that a well-timed provision of information, for example allowing some time to pass following the MI, could make information easier to process for the patient.
Cognitive self-efficacy, described by Berry et al. [Citation44] as “our combined sense of competence and confidence for a given task in a given domain” (e.g., decision making, memory, and verbal abilities), has been linked to cognitive impairment and may constitute an additional barrier to cardiac rehabilitation among elderly MI patients. As narrated in the data, this could present as a deterrence due to practicalities, such as difficulties navigating to the hospital, where a low cognitive self-efficacy could be related to a low perceived sense of control [Citation44]. Furthermore, adherence to medications, such as keeping track of dosages, names, and administration times, constituted a cognitive challenge for some of the participants. In their research Presseau et al. [Citation45], highlight memory, attention, and decision processes as a common barrier to treatment adherence following a MI. Among patients, behavioural regulation in the form of pill organisers and reminders could facilitate the incorporation of medication routines into daily life and thereby improve adherence over time [Citation45]. Likewise, patients described how their maintenance of an adequate level of self-care was a result of the development of various coping strategies. Similar strategies have been highlighted in previous research involving MCI patients [Citation30,Citation31], and involve the use of memory aids, the establishment of daily routines, and access to social support.
For some patients, social support was of great significance for a well-functioning self-care, this is in line with previous research identifying social support as an important factor for coping and positive change [Citation46]. However, this could potentially indicate a vulnerability over time in the event where social support networks might be lost. Hence, we stress the importance of a continuous assessment of patients’ self-care ability over time, as a part of the patient-centred care that has been recommended for elderly cardiac patients [Citation17]. This assessment should include the overall health and cognitive status, social network, and the objective living conditions (e.g., distance from service and housing), in order to identify individual barriers to a successful self-care. This form of assessment is a key component of Comprehensive Geriatric Assessment programs, where medical, social, and functional needs of older patients are identified and managed [Citation47]. When paired with strong long-term management, Comprehensive Geriatric Assessment has been associated with a positive impact on survival and functional status among elderly patients [Citation48]. Moreover, identifying and strengthening informal caregivers in their roles can be of great value in order to relieve stress, increase health and well-being and promote a well-functioning long-term rehabilitation [Citation49,Citation50].
The importance of a high level of individual care and support in the planning and implementation of cardiac rehabilitation has been highlighted in current guidelines for elderly patients [Citation17]. This includes identifying cognitive impairments, and other potential co-morbidities, in the patient’s clinical history and adapt information and educational interventions accordingly. Several patients describe positive experiences receiving guidance and education from healthcare staff following their MI. However, we have identified several healthcare-related challenges indicating that the individual focus emphasised in the guidelines could be implemented further, particularly with regard to the post-MI care provided at the local health centres. In fact, according to the patients, improvements in healthcare provider continuity and accessibility, as well as the provision of information tailored to their individual needs could make cognitive challenges associated with cardiac rehabilitation management easier to overcome. The development of a patient portal was suggested as a measure to increase healthcare accessibility among older MI patients. Indeed, previous research suggests that patient portal interventions lead to improvements in various outcomes among patients with chronic conditions, including self-efficacy, health knowledge, and medication adherence [Citation51]. Moreover, positive user experiences related to patient portals have been highlighted among elderly patients, including better management of health information and improved caregiver communication [Citation52]. However, barriers, including access and ability to use technology, have been reported and further research has been requested on how to integrate internet portals into older patients’ health management [Citation52].
This study has limitations that may affect the interpretation of the results. The low representation of female MI patients (one out of nine) may have influenced the findings. In fact, cardiac rehabilitation utilization has been found to be particularly low among women, with barriers including lower referral rates and higher age of presentation [Citation53]. This may indicate the presence of additional challenges among elderly female MI patients; however, these experiences could not be fully explored within this study. Moreover, we acknowledge the risk of recall bias, where patients may have issues remembering details and aspects of their illness history and presentation. In addition, social desirability bias [Citation54] may influence the data due to the risk of participants wanting to provide the “right answers” to please the interviewer or avoid the potential stigma that could be associated with cognitive decline. Furthermore, we experienced a high refusal rate in the recruitment phase, this might introduce a risk of selection bias where participants with absent or a higher degree of issues related to cognition or self-care could have chosen not to participate. A lower refusal rate could potentially have been achieved had participants been contacted earlier in relation to the point of recruitment. As the participants first were enrolled within the parent study, some weeks often passed before they were contacted by the interviewer, potentially resulting in a fading interest to participate.
The rigour of telephone interviews has been debated in the qualitative literature [Citation55], with criticism including a lack of visual cues and how this may impede the interviewers’ ability to build and maintain rapport, as well as risk missing important aspects of the communication process (e.g., facial expressions and body language). In the present study, we chose telephone interviews as a mode of data collection in order to include a broader range of patients; for example, patients living in regions outside of Uppsala and elderly with potentially limiting co-morbidities, and thus aiming to decrease the risk of selection bias. In fact, this mode of interview was preferred among the patients due to its practicality. Furthermore, several advantages of telephone interviews, which potentially contribute to an increased participation rate, have been highlighted in the literature [Citation55], including it being more cost-effective, less time-consuming, and less intrusive.
Conclusions
Our findings suggest that elderly MI patients are positioned in a changing and complex life context, in which the MI experience is marginalised, and cognitive decline normalized. Even so, several cognitive challenges associated with cardiac rehabilitation were highlighted among the patients, with a particular emphasis on patient–caregiver communication and treatment adherence.
In order to facilitate cardiac rehabilitation management among older MI patients, it is important to take their complex context into account – continuously assessing their individual challenges and strengthening coping strategies that maintain a well-functioning self-care. Furthermore, the post-MI care, at the local health centres, in particular, need to be strengthened and maybe further optimized, in order to achieve a care provision that maintains continuity and is easily accessible.
The present study should be considered as exploratory in its nature, hence future research to investigate the topic further is encouraged, possibly utilising a quantitative or mixed methods approach, as this would facilitate the inclusion of a larger sample of participants as well as the application of objective cognitive measures. Furthermore, we strongly advice future qualitative research to include the perspectives of family members or informal caregivers as this would provide valuable information and a deeper understanding of elderly patients’ self-care management following a MI.
Acknowledgements
The authors would like to acknowledge the patients in the study who have shared their time and experiences so generously. Furthermore, the authors acknowledge the work of the cardiac nurses at the university hospital in Uppsala, who have contributed greatly by recruiting patients to the MIMCI project.
Disclosure statement
The authors declare no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Funding
References
- Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1151–1210.
- Khan MA, Hashim MJ, Mustafa H, et al. Global epidemiology of ischemic heart disease: results from the Global Burden of Disease Study. Cureus. 2020;12(7):e9349.
- Moran AE, Forouzanfar MH, Roth GA, et al. The global burden of ischemic heart disease in 1990 and 2010: the Global Burden of Disease 2010 Study. Circulation. 2014;129(14):1493–1501.
- Menezes AR, Lavie CJ, Milani RV, et al. Cardiac rehabilitation and exercise therapy in the elderly: should we invest in the aged? J Geriatr Cardiol. 2012;9(1):68–75.
- Yan RT, Yan AT, Tan M, et al. Age-related differences in the management and outcome of patients with acute coronary syndromes. Am Heart J. 2006;151(2):352–359.
- Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148(6):427–434.
- Winblad B, Palmer K, Kivipelto M, et al. Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256(3):240–246.
- DeCarli C. Mild cognitive impairment: prevalence, prognosis, aetiology, and treatment. Lancet Neurol. 2003;2(1):15–21.
- Woodford HJ, George J. Cognitive assessment in the elderly: a review of clinical methods. QJM. 2007;100(8):469–484.
- Eshkoor SA, Hamid TA, Mun CY, et al. Mild cognitive impairment and its management in older people. Clin Interv Aging. 2015;10:687–693.
- Deckers K, Schievink SHJ, Rodriquez MMF, et al. Coronary heart disease and risk for cognitive impairment or dementia: systematic review and meta-analysis. PLoS One. 2017;12(9):e0184244.
- Gharacholou SM, Reid KJ, Arnold SV, et al. Cognitive impairment and outcomes in older adult survivors of acute myocardial infarction: findings from the Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status Registry. Am Heart J. 2011;162(5):860–869.
- Zhao E, Lowres N, Woolaston A, et al. Prevalence and patterns of cognitive impairment in acute coronary syndrome patients: a systematic review. Eur J Prev Cardiol. 2020;27(3):284–293.
- Gwaltney C, Reaney M, Krohe M, et al. Symptoms and functional limitations in the first year following a myocardial infarction: a qualitative study. Patient. 2017;10(2):225–235.
- Thombs BD, Bass EB, Ford DE, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006;21(1):30–38.
- World Health Organization. Rehabilitation after cardiovascular diseases, with special emphasis on developing countries. Report of a WHO Expert Committee. WHO Tech Rep Ser. 1993;831:1–122.
- Piepoli MF, Corrà U, Benzer W, et al. Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17(1):1–17.
- Steca P, Monzani D, Greco A, et al. Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS One. 2017;12(8):e0183905.
- Leung Yinko SSL, Maheswaran J, Pelletier R, et al. Sex differences in health behavior change after premature acute coronary syndrome. Am Heart J. 2015;170(2):242–248.
- Yehle KS, Chen AMH, Plake KS, et al. A qualitative analysis of coronary heart disease patient views of dietary adherence and web-based and mobile-based nutrition tools. J Cardiopulm Rehabil Prev. 2012;32(4):203–209.
- Salzwedel A, Heidler M-D, Meng K, et al. Impact of cognitive performance on disease-related knowledge six months after multi-component rehabilitation in patients after an acute cardiac event. Eur J Prev Cardiol. 2019;26(1):46–55.
- Alosco ML, Spitznagel MB, van Dulmen M, et al. Cognitive function and treatment adherence in older adults with heart failure. Psychosom Med. 2012;74(9):965–973.
- Davis KK, Dennison Himmelfarb CR, Szanton SL, et al. Predictors of heart failure self-care in patients who screened positive for mild cognitive impairment. J Cardiovasc Nurs. 2015;30(2):152–160.
- Baird C, Lovell J, Johnson M, et al. The impact of cognitive impairment on self-management in chronic obstructive pulmonary disease: a systematic review. Respir Med. 2017;129:130–139.
- Currie K, Rideout A, Lindsay G, et al. The association between mild cognitive impairment and self-care in adults with chronic heart failure: a systematic review and narrative synthesis. J Cardiovasc Nurs. 2015;30(5):382–393.
- Rodrigues P, Santos M, Sousa MJ, et al. Cardiac rehabilitation after an acute coronary syndrome: the impact in elderly patients. Cardiology. 2015;131(3):177–185.
- Menezes AR, Lavie CJ, Forman DE, et al. Cardiac rehabilitation in the elderly. Prog Cardiovasc Dis. 2014;57(2):152–159.
- Wallert J, Olsson EM, Pingel R, et al. Attending heart school and long-term outcome after myocardial infarction: a decennial SWEDEHEART Registry Study. Eur J Prev Cardiolog. 2020;27(2):145–154.
- Perk J, Hambraeus K, Burell G, et al. Study of patient information after percutaneous coronary intervention (SPICI): should prevention programmes become more effective? EuroIntervention. 2015;10(11):e1–e7.
- Johansson MM, Marcusson J, Wressle E. Cognitive impairment and its consequences in everyday life: experiences of people with mild cognitive impairment or mild dementia and their relatives. Int Psychogeriatr. 2015;27(6):949–958.
- McIlvane JM, Popa MA, Robinson B, et al. Perceptions of illness, coping, and well-being in persons with mild cognitive impairment and their care partners. Alzheimer Dis Assoc Disord. 2008;22(3):284–292.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Ritchie J, Lewis J, Elam G, et al. Designing and selecting samples. In: Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R, editors. Qualitative research practice: a guide for social science students & researchers. 2nd ed. Thousand Oak (CA): SAGE Publications Ltd.; 2013. p. 111–145.
- Malterud K. Qualitative research: standards, challenges, and guidelines. The Lancet. 2001;358(9280):483–488.
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320(7226):50–52.
- Lewis J, Ritchie J, Ormstron R, et al. Generalising from qualitative research. In: Ritchie J, Lewis J, McNaughton Nicholls C, Ormston , editors. Qualitative research practice: a guide for social science students & researchers. 2nd ed. Thousand Oak (CA): SAGE Publications Ltd.; 2013. p. 347–366.
- Birks M, Chapman Y, Francis K. Memoing in qualitative research: probing data and processes. J Res Nurs. 2008;13(1):68–75.
- Partridge JSL, Dhesi JK, Cross JD, et al. The prevalence and impact of undiagnosed cognitive impairment in older vascular surgical patients. J Vasc Surg. 2014;60(4):1002–1011.
- Faircloth CA, Boylstein C, Rittman M, et al. Sudden illness and biographical flow in narratives of stroke recovery. Sociol Health Illn. 2004;26(2):242–261.
- Clarke LH, Bennett E. ‘You learn to live with all the things that are wrong with you’: gender and the experience of multiple chronic conditions in later life. Ageing Soc. 2013;33(2):342–360.
- Esmaeili M, Cheraghi MA, Salsali M. Cardiac patients’ perception of patient-centred care: a qualitative study. Nurs Crit Care. 2016;21(2):97–104.
- Blackburn J, Ousey K, Goodwin E. Information and communication in the emergency department. Int Emerg Nurs. 2019;42:30–35.
- Young WC, Nadarajah SR, Berger AM. Supportive medical care in life-threatening illness: a pilot study. Palliat Support Care. 2016;14(6):680–685.
- Berry JM, West RL. Cognitive self-efficacy in relation to personal mastery and goal setting across the life span. Int J Behav Dev. 1993;16(2):351–379.
- Presseau J, Schwalm JD, Grimshaw JM, et al. Identifying determinants of medication adherence following myocardial infarction using the Theoretical Domains Framework and the health action process approach. Psychol Health. 2017;32(10):1176–1194.
- Holder GN, Young WC, Nadarajah SR, et al. Psychosocial experiences in the context of life-threatening illness: the cardiac rehabilitation patient. Palliat Support Care. 2015;13(3):749–756.
- Parker SG, McCue P, Phelps K, et al. What is Comprehensive Geriatric Assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–155.
- Stuck AE, Siu AL, Wieland GD, et al. Comprehensive geriatric assessment: a meta-analysis of controlled trials. The Lancet. 1993;342(8878):1032–1036.
- Schulz R, Beach SR, Czaja SJ, et al. Family caregiving for older adults. Annu Rev Psychol. 2020;71:635–659.
- Carlozzi NE, Sherman CW, Angers K, et al. Caring for an individual with mild cognitive impairment: a qualitative perspective of health-related quality of life from caregivers. Aging Ment Health. 2018;22(9):1196–1204.
- Han H-R, Gleason KT, Sun C-A, et al. Using patient portals to improve patient outcomes: systematic review. JMIR Hum Factors. 2019;6(4):e15038.
- Sakaguchi-Tang DK, Bosold AL, Choi YK, et al. Patient portal use and experience among older adults: systematic review. JMIR Med Inform. 2017;5(4):e38.
- Galati A, Piccoli M, Tourkmani N, et al. Cardiac rehabilitation in women: state of the art and strategies to overcome the current barriers. J Cardiovasc Med. 2018;19(12):689–697.
- Bergen N, Labonté R. “Everything Is Perfect, and We Have No Problems”: detecting and limiting social desirability bias in qualitative research. Qual Health Res. 2020;30(5):783–792.
- Farooq MB, de Villiers C. Telephonic qualitative research interviews: when to consider them and how to do them. MEDAR. 2017;25(2):291–316.