Abstract
Purpose
Given the limited attention on a combined exercise and education approach for those with chronic musculoskeletal pain disorder such as fibromyalgia, the purpose of this was to evaluate the efficacy of a combined exercise and education programme on symptoms and physical fitness in participants with fibromyalgia.
Materials and methods
Using a prospective observational cohort study, participants with fibromyalgia (n = 75) volunteered. The 6-minute-walk-test (6MWT) and revised-fibromyalgia-impact-questionnaire (FIQR) were used before, after (6 weeks) and 6-months post an exercise and education programme.
Results
Forty-three participants (age = 49.7 ± 15.2 y) completed the 6-week programme, with improvements observed for the 6MWT (67 m, p < 0.001) and FIQR (11 AU, p < 0.001), though only two (6MWT) and five (FIQR) participants, respectively, achieved the minimal clinically important difference (MCID). Using 74% of the intial sample, a small-to-moderate improvement in scores were observed across the 6-month period for the 6MWT (37 m, p = 0.002) and FIQR (3 AU, p = 0.01), with only two participants achieving the MCID for the 6MWT.
Conclusions
The results in this study indiciate small-to-moderate improvements in the 6MWT and FIQR after a combined exercise and education programme, with direct delivery being more effective.
A six-week exercise and education programme elicited moderate, short-term (6 weeks) benefits on physical fitness and key symptoms in patients with fibromyalgia.
On average, these benefits were sustained in the long-term (6 months) following the programme but were small-to-moderate and lower than the MCID.
Regular follow-up may be required to improve adherence to the education and exercise programme and maintain or increase the observed improvements in 6MWT and FIQR.
Implications for rehabilitation
Introduction
Fibromyalgia is a chronic musculoskeletal pain disorder [Citation1–3] that is characterised by widespread pain lasting longer than three months [Citation2,Citation4], fatigue, poor sleep and cognitive impairment [Citation5]. These symptoms may result in physical and psychological dysfunction which impact on general well-being, function and quality of life (QOL) [Citation6]. Further, patients diagnosed with fibromyalgia may incur significant direct and indirect healthcare costs [Citation7] as a result of absenteeism from work [Citation8]. Effective management of patients with fibromyalgia is, therefore, paramount with the promotion of long-term self-management strategies potentially reducing the use of healthcare resources [Citation9].
Management of symptoms associated with fibromyalgia often include medication, though the benefits appear limited [Citation10]. Opiates, for example, have limited pain relieving benefits in patients with fibromyalgia [Citation11], whilst antidepressants (low dose Amitriptyline) and neuro-modulating anti-epileptics (Gabapentin and Pregabalin) are often recommended [Citation12]. Such medication, however, can cause major side-effects (i.e., nausea, vomiting, dry mouth and drowsiness) [Citation5,Citation13] that impact on patient’s daily lives [Citation10]. That said, the use of pharmacological intervention may be necessary to support other strategies for the management of fibromyalgia. Indeed, the European League Against Rheumatism (2017) recommends that non-pharmacological strategies (e.g., education, exercise, cognitive behavioural therapy) be used in the first instance and then, where necessary, supported by an individualised approach which may include pharmacological intervention depending on symptoms associated with the condition [Citation14].
To date, research has sought to determine the beneficial effect of exercise on symptoms associated with fibromyalgia [Citation3,Citation15], with excercise serving to moderate the reduction in physical function and activity tolerance observed in 80 to 90% of cases [Citation16–19]. Two recent systematic reviews and meta-analyses have reported beneficial effects of exercise on pain, physical function, fatigue, balance and sleep quality [Citation3,Citation15]. These findings generally concur with the worth of Bidonde et al. [Citation20] who concluded exercise can slightly reduce pain intensity and improve physical functioning in patients with fibromyalgia as well as Geneen et al.’s [Citation21] review of reviews across several diagnoses associated with chronic pain. Whilst these results are promising and incorporate a large pooled sample, only a small-to-moderate effect was observed, with large heterogenity [Citation3,Citation15,Citation20,Citation21]. In part, the heterogeneity is likely explained by the approach used across studies when concerning the type of exercise used; the duration, frequency and intensity of the intervention; and patient demographics and baseline scrore. Such information is also essential to determine the quality and replicability of these studies.They included studies deemed poor quality due the reasons above and the lack of adequately powered studies [Citation20,Citation21], suggesting caution is needed when interpreting the change in symptoms of fibromyalgia. There is also a paucity of research exploring the long-term benefits of an exercise intervention (>6 months), with Bidonde et al. [Citation20] including only three studies in their review that provided low-quality evidence that exercise had any long-term benefit. As such, further research is required to examine the short- and long-term effects of exercise on symptoms of fibromyalgia whilst being entirely transparent with information about patients and the intervention as well as ensuring adequate statistical power in light of the high attrition rates and low compliance [Citation18]. It is well-documented that attirition rate is high in patients with fibromyalgia [Citation18] due to patients experiencing post-exercise muscle soreness and perceptions of tiredness [Citation22], and that this should be accounted for in future studies.
Whilst exercise appears to provide a small-to-moderate effect on symptoms of fibromyalgia, patient education, which includes education activities planned by health professionals, can play an integral part in pain management programmes for patients with chronic pain conditions and improve their health beahviours and/or status [Citation2,Citation23]. Education can reduce hyper-vigilance and raise awareness of the impact negative thoughts and feelings have on healthy behaviour, thereby assisting patients in behavioural changes. It can also support patients through assurances the condition is legitimate and non-life-treatening [Citation2]. A recent systematic review on patient education and symptoms of fibromyalgia provided an overall positive picture, with symptons of pain, physical function, anxiety, feelings of coping and overall impact as measured by the fibromyalgia impact questionnaire [Citation2]. Due to the large heterogeneity across the the studies, a pooled effect could not be determined and therefore, the magnitude of improvement in commonly measured symptoms is unknown. Further, García-Rios et al. [Citation2] also express concerns over the overall quality, with most studies demonstrating limited quality due to lack of blinding of the outcomes assessors. As such, future research ought to address these concerns in order to continue to build the evidence-based for the inclusion of education session with fibromyalgia patients.
Given both exercise and education appear to provide some benefit individually, albeit of a small-to-moderate magnitude, the use of combined exercise and education programmes might be a suitable strategy for patients with chronic musculoskeletal disorders [Citation16]. Using a variety of skills including cognitive behavioural therapy, the aim of these programmes is to assist patients in developing self-management strategies and coping skills to improve independent management of their condition. There is, however, conflicting evidence with regards to the short-term effectiveness of combined exercise and education on reducing pain and the overall impact of the condition in patients with fibromyalgia [Citation24]. Research suggests that there is little scientific evidence for the effectiveness of combined exercise and education rehabilitation on pain and disability in patients with fibromyalgia [Citation25]. However, it is postulated that this combined approach could be beneficial for decreasing pain as well as increasing overall physical fitness [Citation26,Citation27]. The long-term carryover effect of combined exercise and education programmes on patients with fibromyalgia also remains unclear in many studies [Citation24,Citation25,Citation28]. Therefore, research is required to further clarify the short- and long-term effectiveness of combined exercise and education programmes.
The primary objective of this study was to determine the effects of a 6-week combined exercise and education programme on physical fitness and symptoms in patients with fibromyalgia. The secondary objective was to determine the effects of the programme 6 months following its completion. It was hypothesised that the 6-week programme improves fitness and symptoms and that these changes would be evident at the 6-month follow-up.
Methods
A prospective observational cohort study was used to evaluate the effectiveness of a 6-week combined exercise and education programme in a hospital in the Northwest of England. Ethics approval was granted by the Faculty of Health, Psychology and Social Care at Manchester Metropolitan University (Ph/16/1).
Patients
Patients with fibromyalgia were referred to the Physiotherapy Department from Rheumatology consultants and Rheumatology Clinical Assessment Services. A sample of convenience was used with a target sample of 46 required. This number was based on the work of Burckhardt et al. [Citation29] who reported a partial eta squared of 0.10. Using a repeated measures within-subject design with alpha set at 0.05 and beta at 0.80, a sample of 46 participants was required (G*Power, 3.1.9.4). A total of 100 participants were initially invited to allow for a 30% dropout rate [Citation26] whilst achieving a sufficient statistical power. Of those invited; 75 participants provided written informed consent and 25 did not reply. On arrival to the first session, 3 participants withdrew from the study before starting, resulting in a sample size of 72.
A team of physiotherapists experienced in chronic pain management subsequently assessed all patients with fibromyalgia referred to the Physiotherapy Department to ensure their suitability for the programme. Screening for inclusion and exclusion criteria was then conducted in the hospital. Inclusion criteria included participants who were ≥18 years and had a diagnosis of fibromyalgia as confirmed by either rheumatology consultants or Rheumatology Clinical Assessment Services using the American fibromyalgia diagnostic criteria [Citation30,Citation31]. Participants were excluded if they had a severe unstable medical condition [Citation28], a physical impairment (e.g., acute musculoskeletal injury or recent surgery) presenting with safetly concerns [Citation32,Citation33] or were unable to communicate in English. Participants were also excluded if they had a severe active and uncontrolled psychiatric disorder requiring a mental health practitioner [Citation34] or had severe cognitive impairment, leading to inability to participate in a group setting [Citation34].
Main outcome variables
The six-minute walk test (6MWT) was used as the primary outcome measure and involved determining the maximal distance a participant can walk in 6 minutes at baseline, post 6 weeks and after 6 months. The 6MWT is widely used in the clinical community as a simple, practical and inexpensive measure of functional exercise capacity in populations with underlying health issues [Citation35]. The objective is for patients to walk the greatest total distance in a 6-minute period. The minimally clinically important difference (MCID), which refers to the smallest change in the outcome perceived as important, beneficial, or would lead to a change in management [Citation36] of patients with fibromyaligia is ≥156 m [Citation35]. The revised fibromyalgia impact questionnaire (FIQR) was used as the secondary outcome measure in this study. It is a validated multidimensional self-report questionnaire [Citation37] and measures the overall severity of fibromyalgia including intensity of pain, physical function, fatigue, morning tiredness, depression, anxiety, job difficulty and overall well-being [Citation38]. All 21 questions are based on an eleven-point numeric rating scale from 0 to 10, with a higher total score indicative of a greater negative impact on the participants’ condition [Citation39]. The MCID for the FIQR in patients with fibromyaligia is reported to be 27 points or 45.5% [Citation40]. Outcome measures were collected by an assistant physiotherapist – who was blinded to the aim of the study – and recorded the values at baseline, 6 weeks and 6 months post programme.
Procedures
Participants attended a 90-min session once a week for 6 weeks. The programme consisted of weekly exercise and education sessions that focused on goal setting, explaining pain, pacing and planning, exercise, sleep hygiene and managing flare-ups. This was delivered by physiotherapists, occupational therapists and pain specialist nurses (Supplementary Material 1). The weekly 60-minute education sessions were interactive group-based sessions. Participants were actively involved in problem-solving and peer learning to enhance self-efficacy and self-management. Participants’ targets and individual goals set at the start of the programme were also evaluated within the sessions.
For safety reasons, groups were divided into two exercise classes and performed weekly graded exercises for a maximal duration of 30 min that generally included a series of aerobic, strengthening, functional and proprioceptive exercises (Supplementary Material 2). Each session included a 5-minute warm up and cool down, with the exercise in week one lasting 10 minutes and progressing to 20 minutes by week 6. In brief, the warm-up included walking and high stepping followed by a series of static stretches of major muscle groups each held for 10–30 s. The main exercise block was focused on developing cardiovascular function, strength and balance through the inclusion of exercises such as walking, step ups, sit-to-stand, stairs climbing, wall-based press-ups and core strengthening exercises (Supplementary Material 2). These were all completed in a circuit with each exercise performed for 1 minute and progressing to 2 minutes by the end of the intervention period. Supervision was provided by the intervention physiotherapists who had at least 5 years musculoskeletal experience in the management of patients with chronic pain. Participants were then provided with a copy of the exercise programme along with specific details to encourage and facilitate them to exercise in their leisure time post-intervention.
Statistical analysis
As the study was completed in two distinct phases, separate analysis was completed. Normality was assessed for scale data using the Shapiro–Wilk statistic. To determine the change in the 6MWT and FIQR questionnaire across the 6-week intervention period, a paired sample t-test was used to determine the probability and standardised mean difference (SMD) [(M2-M1)/SD pooled)] to provide a measure of the magnitude of change with 95% confidence intervals (SMD ± 95%CI) Changes in FIQR were interpreted using the Wilcoxon statistic and SMD with 95%CI. Changes across the three time-points for the 6MWT and FIQR questionnaire were assessed using a repeated measures’ ANOVA and Freidman’s ANOVA, respectively. Specific comparisons were made with Bonferroni adjustment and accompanied with SMD ± 95%CI. All SMDs were interpreted using the following thresholds: 0.2, small; 0.5, moderate; 0.8, large [Citation41]. Inferential statistics were completed using Statistical Packages for Social Science (Version 26; Armonk, NY, IBM Corp).
Results
In total, 72 participants provided consent, though 29 failed to attend the first assessment session resulting in 43 participants completing the assessments and 6-week programme. At 6 months, a further 11 participants dropped out without giving a reason resulting in a total of 32 participants (74%). The final sample were aged 49.7 ± 15.2 years and included 5 men and 27 females with a mean disease duration of 7.7 ± 5.9 years and diagnosis duration of 1.6 ± 1.7 years. Twenty-three participants were unemployed, whilst seven participants were involved in full- or part-time employment.
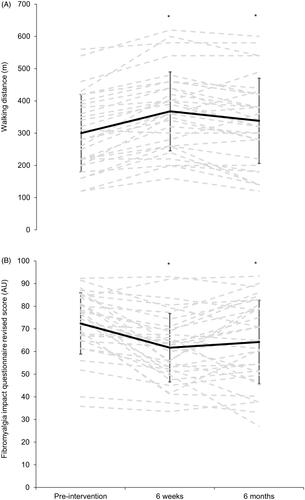
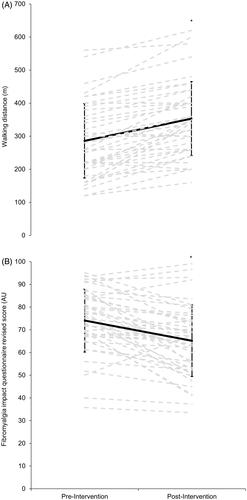
With the assumptions of normality met, the pre-post change in the 6MWT across the 6-week intervention (n = 43) indicated a mean increase in total distance covered (t = 8.787, p = <0.001) of 67 ± 41 m and a standardised mean difference of 0.59 ± 0.18 (). A reduction in the FIQR (n = 43) was observed across the 6-week intervention period (Z = −4.377, p = 0.001) with a mean change of −8.9 ± 11.4 AU (SMD = −0.63 ± 0.28).
Figure 1. Mean (solid black line) and individual (dashed grey line) in walking distance (A) and fibromyalgia impact questionnaire revised (B) across the 6-week intervention period (n = 43).
Using the sample of 32 participants who completed all three assessments, results indicated a significant time-effect for the 6MWT across the intervention period (F = 27.473, p < 0.001; SMD = 1.88). Between-time comparisons indicated differences between baseline and 6 weeks (mean change = 67 m; 95%CI = 49 to 86 m, p < 0.001; SMD ± 95%CI = 0.52 ± 0.11), and baseline and 6 months (mean change = 38 m; 95%CI = 10 to 66 m; p = 0.005; SMD ± 95%CI = 0.27 ± 0.14). There was a reduction in distance covered during the 6MWT between the 6-week and 6-month assessment (-29 m; 95%CI = −51 to −7; p = 0.006; SMD ± 95%CI = −0.31 ± 0.15). The standard deviation of the change was slightly larger between 6 weeks and 6 months compared to baseline and 6 weeks, suggesting greater response variability to the removal of the supervised intervention (50 m) when compared to supervised (41 m).
A change in FIQR scores was evident across the three time points (F = 25.750, p < 0.001) (). With Bonferroni correction, differences were observed between baseline and post-6 weeks (Z = 4.591, p < 0.001; SMD ± 95%CI = −0.77 ± 0.34) and baseline and 6 months (Z = 2.571, p < 0.001; SMD ± 95%CI = −0.59 ± 0.39) but not 6 weeks and 6 months (Z = 1.421, p < 0.16; SMD ± 95%CI = 0.16 ± 0.27) (). The response variability was greater between the 6-week and 6-month assessments (3.4 AU) when compared to the intervention period (1.6 AU).
Discussion
The aim of this study was to determine the effectiveness of a combined exercise and education programme on physical fitness and symptoms associated with fibromyalgia. This study demonstrated a short-term benefit of a six-week programme on 6MWT and FIQR measures that remained above baseline at 6 months.
The results of this study suggest that the programme used was effective for eliciting a moderate improvement in the 6MWT at 6 weeks and small improvement at 6 months when compared to baseline. Such findings correspond with previous studies demonstrating a mean improvement in the 6MWT after 6 weeks [Citation22] (72 m; frequency twice a week), 16 weeks [Citation26] (28 m; frequency twice a week), 20 weeks [Citation42] (15 m; frequency once a week) and 24 weeks [Citation42] (40 m; frequency once a week). The results do, however, contrast with studies by Cabonell-Baeza et al. [Citation27] and Buckhardt et al. [Citation29] who reported minimal change in 6MWT distance. These results may reflect variances in the type of exercise programme included. This study included land-based walking, whilst Cabonell-Baeza et al. [Citation27] completed walking tasks in a swimming pool, for example. The mean baseline distance covered in this study was substantially lower (∼300 m) than other studies investigating interventions for patients with fibromyalgia, reporting between 457 and 487 m [Citation26,Citation29,Citation43,Citation44]. This suggests that the sample of participants selected in this study were highly disabled and deconditioned [Citation45]. Whilst our results do indiciate that a combined exercise and education programme can increase the mean walking distance in disabled and deconditioned patients, and that physiotherapists can use this or a similar programme to elict improvements in physical fitness, it is important to consider the MCID. Indeed, the mean improvement observed was less than the MCID reported in patients with fibromyaligia that is associated with changes in the fibromalgia impact questionnaire (156 m [Citation35]). That said, none of the studies reviewed observed a mean score within this region, but were more in-line with the MCID observed in other populations such as those with heart failure and lung disease [Citation35]. In this study, only two participants recorded a change that exceeded 156 m at 6 weeks. Our findings suggest that phsiotherapists can be confident that an exercise and education programme can elicit a moderate increase in 6MWT for most patients with fibromyalgia, but that they might need to use a more indvidualised approach, provide exercise and education for a longer period than 6 weeks and/or supplement the programme with home-based activities that have been shown to improve performance in a 6MWT to acheive the MCID.
The long-term effects of the exercise and education programme were evaluated over a 6-month period. The change in 6MWT when compared to baseline is encouraging, albeit small, suggesting that participants did improve overall fitness levels. It is important to note however, that only two patients reported a change that exceeded the MCID at 6 months and therefore, physiotherapists must be aware that, when delivering an exercise and education programme, the magnitude of change is unlikely to meet the MCID for most individuals. Whether the small changes were due to a carryover effect of the 6-week supervised period or due to continued engagement is unknown and warrants further exploration. As such, monitoring adherence to the exercise programme away from the clinic is essential by physiotherapists or others within the patient’s wider support network. The reduction in 6MWT distance between the 6-week and 6-month assessments where a mean change of −29 m was observed supports the inclusion of supervised exercise sessions that are undertaken with the support of a physiotherapist. One study reported similar reductions, with an average decrease of 25 m at 3 months, once the 6-week supervised programme had ended [Citation22], whilst other studies reported no significant changes at 6 and 24 months following a combined exercise and education programme (467 m cf. 506 m cf. 512 m) [Citation43]. It is possible that the reduction is due to a lack of adherence as well as the removal of social interactions between the participant and peers [Citation22,Citation32], thus reducing the social capital. Sharing experiences, providing social support and goal setting are likely to be important aspects in managing chronic pain conditions and should be encouraged in patients with fibromyalgia during and after the programme [Citation46].
At 6 weeks, a moderate improvement in the FIQR questionnaire was observed in this study, which is consistent with previous studies [Citation28,Citation47] and addreses some the limitations reported by García-Rios et al. [Citation2] such as the blinding process. Other land-based exercise programmes using the FIQR as an outcome measure have identified improvements (−7%) in scores after a 12-week (twice per week; 60 min per session), gym-based exercise programme (−8%) [Citation48] and combined 6-week education, flexibility and fitness exercise programme totalling 15 h (−7%) [Citation29]. Whilst positive, it is important to highlight that the mean change observed across all studies is less than the MCID (27 points or 45.5%; [Citation40]), with only 5 patients achieving this threholds at 6 weeks in this study. The moderate improvement observed in this study may be due to the benefits derived from group treatment which may facilitate a better understanding of fibromyalgia symptoms and assist in developing better coping strategies through education and sharing of experiences [Citation44]. The exercise and education components were both comprehensive and interactive, giving participants the skills to manage and problem-solve their condition independently, thereby assisting in behavioural change. Similar to this study, previous research used both exercise and education components in their programmes [Citation29,Citation44]. The exercise component was, however, variable between studies both in the type, duration and frequency of exercise sessions [Citation10,Citation28,Citation29,Citation43,Citation47]. Furthermore, most studies used land-based exercises including cardiovascular exercise, flexibility and strength work [Citation26,Citation28,Citation29]. Some studies used exercises in the pool only [Citation49], whereas others used a combination of land-based exercises and hydrotherapy [Citation47]. Recently published recommendations noted no difference in the effectiveness when exercise was performed on land or in water [Citation50]. Precise prescription and duration of exercise remains unclear in the literature [Citation49] and might explain the high variability in responses across studies [Citation3,Citation26,Citation28]. Programme length was also variable between studies ranging between 6 weeks to 6 months, with sessions completed between once to three times a week [Citation22,Citation24,Citation45]. In this study, it appears that a single session for 6 weeks is sufficient to elicit a moderate improvement in FIQR, but that its unlikely all participants will achieve a change that exceeds the MCID. As such, further research is required to expore the most effective mode of delivery of exercise, education or a combination of both to achieve a MCID in FIQR without placing a large burden on patients and the service provider with respect of finanaces, staff hours and the use of facilities. Whilst we demonstrated that a combined approach might be a feasible method, further work is needed to optimise the intensity, volume, frequency and exercise:education ratio whilst considering the individual needs of the patients. It is possible that some patients could have benefited from a more personalised exercise and education programme whilst others favour the group-based approach due to the social interaction and a sense they completeing the programme collectively rather than as individuals.
This study demonstrated that the moderate improvement in the FIQR scores were maintained at 6 months following the programme despite a small increase in score (2.4%) compared to 6 weeks. However, no patients reported a change >27 points or above 45.5%, suggesting that despite our programmes improving symptoms, it was generally below that deedmed clinically important [Citation40]. Previous studies have reported a minimal difference in FIQR scores at 8 months with the mean data indicating a return to baseline (56 AU cf. 57 AU) [Citation27]. In agreement with the change in the 6MWT, the observed difference in FIQR at 6 months may reflect a more disabled population as indicated by the high baseline scores (73 AU) compared with that previously observed (48–56 AU) [Citation26,Citation47]. This suggests that continued support or periodic follow-up may be required to encourage continued motivation for participation and adherence [Citation29,Citation46], although a more tailored approach to exercise and education and follow up by a therapist might be required for some. Furthermore, it is well-reported that pain [Citation22,Citation38], fatigue and post-exercise muscle soreness are contributors to poor adherence [Citation50] and therefore, careful consideration by physiotherapists for the progression of an exercise programme is essential. In order to reduce post-exercise soreness and maximise compliance, exercises in this study were graded and patients were encouraged to use a diary to record their activity for their own recall [Citation49] with a view that this would promote adherence until behavioural change was achieved. This might not have been the case and a follow up session to review the diary might have been worthwhile and should be included in future research and/or clinical practice. The inclusion of skills such as relaxation, sleep hygiene strategies and graded activity as part of the education aspect was a key part of this study and might have contributed to the small positive findings in this study. It is important to identify behavioural patterns and assist patients in learning new behaviours and thinking styles that are consistent with living with chronic pain over time.
Whilst this study builds on the evidence and supports the use of a combined exercise and education approach to elicit small-to-moderate improvements in the 6MWT and FIQR in patients with fibromyalgia, and tries to address several of the limtiations in the literature, some still remain. Firstly, a control group was not included and therefore the beneficial effect of the intervention compared to usual management or no management is unknown. Secondly, a group exercise and education approach was used and therefore, we are unable to provide any comment on the benefits and limtiations of this method compared to an alternative such as an individualised approach. Thirdly, the group of patients were heterogeneous with regards to age and disease duration that might explain the varied responses to the intervention. Our study also demonstrated a high attrition rate (∼26%) from the end of the intervention until 6 months (26%) in this population that resulted in our results being slightly underpowered. This finding is consistent with research exploring the effects of exercise [Citation3] and education [Citation2] where, for example, García et al. [Citation2] reported only two studies include >85% of the baseline sample at follow-up. We were unable to determine the exact reason for this high attrition rate and further research is required to understand the factors contributing to a lack of continuation in the exercise and education programme. Finally, documentation on adherence was not recorded during the period following the intervention; therefore, it is difficult to explain the variability of results. Further research is therefore required to explore drop-out rates and the impact of long-term adherence on the efficacy of this intervention in patients with fibromyalgia. Such insight is required before the true effectiveness of a combined exercise and education programme is known and may need to consider regular sessions to ensure the observed improvement in maintained over a prolonged period.
Conclusion
In conclusion, this prospective observational cohort study evaluated the efficacy of a 6-week group-based exercise and education programme. The results indicate a moderate improvement in physical fitness and key symptoms in patients with fibromyalgia following a 6-week combined exercise and education programme. These benefits were sustained for at least 6 months after completion of the programme but to a lesser degree and and we observed that few achieved a change that equalled the MCID. This study suggests that a carefully designed, graded and progressive exercise programme in conjunction with education may be effective for eliciting small-to-moderate improvements in the FIQR and 6MWT but that similar challenges were faced when concerning attrition, statistical power and eliciting large changes in 6MWT and FIQR.
Ethical approval
This study was approved by the Faculty of Health, Psychology and Social Care at Manchester Metropolitan University (Ph/16/1) and all participants signed written informed consent after they had been informed of the details of the study.
Author contributions
NL and JC were responsible for the conception and organisation of the research project, designed and executed all procedures. ND was responsible for data analysis and presentation. NL wrote the initial draft whilst JC and ND critically reviewed the manuscript. All authors contributed to the writing of the final manuscript and approved the final version.
Supplementary Material 2
Download MS Word (12.5 KB)Supplementary Material 1
Download MS Word (13.8 KB)Acknowledgments
The authors would like to thank the therapists who assisted in the delivery of the programmes. Special thanks to Mr. William Morris for his dedication and support with data collection. Finally, we would like to thank all the participants who participated in this study. This research has not been previously presented in any format including conferences, congress abstract or pre-publication archiving.
Disclosure statement
The authors declare that they have no conflict of interest.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Sluka KA, Clauw DJ. Neurobiology of fibromyalgia and chronic widespread pain. Neuroscience. 2016;338:114–129.
- García-Rios MC, Navarro-Ledesma S, Tapia-Haro RM, et al. Effectiveness of health education in patients with fibromyalgia: a systematic review. Eur J Phys Rehabil Med. 2019;55(2):301–313.
- Bravo C, Skjaerven LH, Sein-Echaluce LG, et al. Effectiveness of movement and body awareness therapies in patients with fibromyalgia: a systematic review and meta-analysis. Eur J Phys Rehabil Med. 2019;55(5):646–657.
- Smythe HA, Moldofsky H. Two contributions to understanding of the “fibrositis syndrome”. Bull Rheum Dis. 1997;28(1):928–931.
- Bellato E, Marini E, Castoldi F, et al. Fibromyalgia syndrome: etiology, pathogenesis diagnosis, and treatment. Pain Res Treat. 2012;2012:426130.
- Mease PJ, Arnold LM, Crofford LJ, et al. Identifying the clinical domains of fibromyalgia: contributions from clinician and patient Delphi exercises. Arthritis Rheum. 2008;59(7):952–960.
- White KP, Speechley M, Harth M, et al. The London fibromyalgia epidemiology study: the prevalence of fibromyalgia syndrome in London, Ontario. J Rheumatol. 1999;26(7):1570–1576.
- Henriksson CM, Liedberg GM, Gerdle B. Women with fibromyalgia: work and rehabilitation. Disabil Rehabil. 2005;27(12):685–694.
- Fitzcharles MA, Ste-Marie PA, Goldenberg DL, National Fibromyalgia Guideline Advisory Panel, et al. 2012 Canadian guidelines for the diagnosis and management of fibromyalgia syndrome: executive summary. Pain Res Manag. 2013;18(3):119–126.
- Shelton TPH. Current guidelines and best-practice evidence in the pharmacological management of fibromyalgia. J Physiother Pain Assoc. 2017;43:11–20.
- Stisi S, Cazzola M, Buskila D. Etiopathogenic mechanisms of fibromyalgia syndrome. Rheumatismo. 2008;60(1):25–35.
- Goldenberg DL. Pharmacological treatment of fibromyalgia and other chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2007;21(3):499–511.
- Joint Formulary Committee. British National Formulary (online). BMJ Group and Pharmaceutical Press, London. 2020.
- Macfarlane GJ, Kronisch C, Dean LE, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318–328.
- Estévez-López F, Maestre-Cascales C, Russell D, et al. Effectivness of exercise on fatigue and sleep quality in fibromyalgia: a systematic review and meta-analysis of randomized trials. Arch Phys Med Rehabil. 2020. DOI:10.1016/j.apmr.2020.06.019
- Garrido-Ardila EM, González-Lopez-Arza MV, Jimenez-Palomares M, et al. Effectiveness of acupuncture vs. core stability training in balance and functional capacity of women with fibromyalgia: a randomized controlled trial. Clin Rehabil. 2020;34(5):630–645.
- Mannerkorpi K, Svantesson U, Broberg C. Relationships between performance-based tests and patients' ratings of activity limitations, self-efficacy, and pain in fibromyalgia . Arch Phys Med Rehabil. 2006;87(2):259–264.
- Busch AJ, Overend TJ, Schachter CL. Fibromyalgia treatment: the role of exercise and physical activity. Int J Clin Rheumatol. 2009;4(3):343–376.
- Busch AJ, Schachter CL, Overend TJ. Exercise for fibromyalgia: a systemic review. J Rheumatol. 2008;35(6):1130–1144.
- Bidonde J, Busch AJ, Schachter CL, et al. Aerobic exercise training for adults with fibromyalgia. Cochrane Database of Sys Rev. 2017;6:CD012700.
- Geneen LJ, Moore RA, Clark C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Database of Sys Rev. 2017;1:CD011279.
- Gowans SE, deHueck A, Voss S, et al. A randomized, controlled trial of exercise and education for individuals with fibromyalgia. Arthritis Care Res. 1999;12(2):120–128.
- Williams DA. The role of non-pharmacologic approaches in the management of fibromyalgia. CNS Spectr. 2009;14(12 Suppl 16):10–12.
- Hauser W, Bernardy K, Arnold B, et al. Efficacy of multicomponent treatment in fibromyalgia syndrome: a meta-analysis of randomized controlled clinical trials. Arthritis Rheum. 2009;61(2):216–224.
- Van Koulil S, Effting M, Kraaimaat WV, et al. Cognitive-behavioural therapies and exercise programmes for patients with fibromyalgia: state of the art and future directions. Ann Rheum Dis. 2007;66(5):571–581.
- Rooks DS, Gautam S, Romeling M, et al. Group exercise, education, and combination self-management in women with fibromyalgia: a randomized trial. Arch Intern Med. 2007;167(20):2192–2200.
- Carbonell-Baeza A, Aparicio VA, Ortega FB, et al. Does a 3-month multidisciplinary intervention improve pain, body composition and physical fitness in women with fibromyalgia? Br J Sports Med. 2011;45(15):1189–1195.
- Hammond A, Freeman K. Community patient education and exercise for people with fibromyalgia: a parallel group randomized controlled trial. Clin Rehabil. 2006;20(10):835–846.
- Burckhardt CS, Mannerkorpi K, Hedenberg L, et al. A randomized, controlled trial of education and physical training for women with fibromyalgia. J Rheumatol. 1994;21(4):714–720.
- Jones GT, Atzeni F, Beasley M, et al. The prevalence of fibromyalgia in the general population: A comparison of the American college of Rheumatology 1990, 2010, and modified 2010 classification criteria. Arthritis Rheumatol. 2015;67(2):568–575.
- Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172.
- Wolfe F. New American College of Rheumatology criteria for fibromyalgia: a twenty-year journey. Arthritis Care Res (Hoboken)). 2010;62(5):583–584.
- Bailey A, Starr L, Alderson M, et al. A comparative evaluation of a fibromyalgia rehabilitation program. Arthritis Care Res. 1999;12(5):336–340.
- Giannotti E, Koutsikos K, Pigatto M, et al. Medium-/Long term effects of a specific exercise protocol combined with patient education on spine mobility, chronic fatigue, pain, aerobic fitness and level of disability in Fibromyalgia. Biomed Res Int. 2014;2014:1–9.
- Kaleth AS, Slaven JE, Ang DC. Determining the minimal clinically important difference for six-minute walk distance in fibromyalgia. Am J Phys Med Rehabil. 2016;95(10):738–745.
- Johnston BC, Ebrahim S, Labra C, et al. Minimally important difference estimates and methods: a protocol. BMJ Open. 2015;5(10):e007953.
- Bennett RM, Friend R, Jones KD, et al. The revised fibromyalgia impact questionnaire (FIQR): Validation and psychometric properties. Arthritis Res Ther. 2009;11(4):R120.
- Arthritis Foundation. Walk with ease: your guide to walking for better health, improved fitness and less pain. 2nd ed. Alanta, Georgia: Arthritis Foundation; 1997.
- Williams DA, Arnold LM. Measures of fibromyalgia: Fibromyalgia Impact Questionnaire (FIQ), Brief Pain Inventory (BPI), Multidimensional Fatigue Inventory (MFI‐20), Medical Outcomes Study (MOS) Sleep Scale, and Multiple Ability Self‐Report Questionnaire (MASQ). Arthritis Care Res. 2011;63(S11):S86–S97.
- Surendran S, Mithun CB. Estimation of minimum clinically important difference in fibromyalgia for FIQR using bpi as the anchor measure. Ann Rheum Dis. 2018;77(2):845.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New Jersey: Lawrence Earlbaum Associates; 1988.
- Mannerkorpi K, Nordeman L, Ericsson A, GAU Study Group, et al. Pool exercise for patients with fibromyalgia or chronic widespread pain: a randomised controlled trial and subgroup analyses. J Rehabil Med. 2009;41(9):751–760.
- Ayan C, Alvarez MJ, Alonso-Cortes B, et al. Health education home-based program in females with fibromyalgia: a pilot study. J Back Musculoskelet Rehabil. 2009;22(2):99–105.
- King SJ, Wessel J, Bhambhani Y, et al. Predictors of success of intervention programs for persons with fibromyalgia. J Rheumatol. 2002;29(5):1034–1040.
- Mannerkorpi K, Ahlmen M, Ekdahl C. Six-and-24-month follow-up of pool exercise therapy and education for patients with fibromyalgia. Scand J Rheumatol. 2002;31(5):306–310.
- Meyer BB, Lemley KJ. Utilizing exercise to affect the symptomology of fibromyalgia: a pilot study. Med Sci Sports Exerc. 2000;32(1):1691–1697.
- Cedrashi C, Desmeules J, Rapiti E, et al. Fibromyalgia: a randomised, controlled trial of a treatment programme based on self-management. Ann Rheum Dis. 2004;63(3):290–296.
- Richards SCM, Scott DL. Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. BMJ. 2002;325(7357):185–187.
- Fink L, Lewis D. Exercise as a treatment for fibromyalgia: a scoping review. J Nurse Prac. 2017;13(8):546–551.
- Campbell R, Evans M, Tucker M, et al. Why don't patients do their exercises? Understanding non-compliance with physiotherapy in patients with osteoarthritis of the knee. J Epidemiol Community Health. 2001;55(2):132–138.