Abstract
Purpose
In persons with a hip or knee flexion contracture ≥25°, fitting a prosthesis is said to be difficult. This systematic review aims to assess the evidence for fitting of a prosthesis in persons with a severe contracture (≥25°) after a lower limb amputation.
Method
PubMed, Embase, Scopus, CINAHL, and Orthotics & Prosthetics Virtual Library databases were searched from inception to December 2019, using database specific search terms related to amputation, prosthesis, and contracture. Reference lists of included studies were checked for relevant studies. Quality of the included studies was assessed using the critical appraisal checklist for case reports (Joanna Briggs Institute).
Results
In total, 13 case studies provided evidence for fitting of a prosthesis in more than 63 persons with a transtibial amputation and three with a transfemoral amputation, all of whom had a hip or knee flexion contracture ≥25°. Some studies found a reduction in contractures after prosthesis use.
Conclusions
Several techniques for fitting a prosthesis in case of a flexion contracture ≥25° were found. Contracture reduction occurred in some cases and was possibly related to prosthesis use. Fitting a transtibial or transfemoral prosthesis in persons with a lower limb amputation with a severe flexion contracture is possible.
This study provides information on prosthesis prescriptions and adaptations for persons with a transfemoral and transtibial amputation with a flexion contracture ≥25°.
The fitting of bent prostheses is not limited by prosthetic components and techniques.
Parallel to the use of bent prostheses, it is also important to treat the contracture.
IMPLICATIONS FOR REHABILITATION
Introduction
A hip or knee flexion contracture may occur in persons with a lower limb amputation [Citation1]. Approximately, 13% of persons with a transtibial (TT) amputation and 23% of persons with a transfemoral (TF) amputation develop a flexion contracture ≥25° [Citation2]. A flexion contracture of hip or knee limits full extension and can be caused by several factors [Citation3–6], including muscle imbalance [Citation3,Citation4]. For example, the more proximal the level of a transfemoral amputation, the more the hip extensor (gluteus maximus), and hip adductors (adductor longus and adductor magnus) are amputated [Citation4]. The strongest hip flexor (iliopsoas) as well as the hip abductors (gluteus medius and minimus); however, remain intact [Citation4]. Contractures can also be the result of prolonged immobilization or improper positioning [Citation3,Citation5]. The immobilization could induce the adhesion of synovial membrane fold contributing to contractures [Citation7]. Lying supine with a pillow underneath the knee or side-lying with hips and knees flexed can lead to hip and knee flexion contractures [Citation5,Citation6]. These incorrect positions may be maintained due to unawareness of a contracture [Citation8].
Strategies to prevent postoperative contractures include use of a prosthesis immediately post amputation [Citation9,Citation10], rigid dressings [Citation11], silicone liners [Citation12], pneumatic postoperative prostheses, proper positioning (lying prone to prevent hip flexion contractures), use of an extension board while sitting on a wheelchair, and active range of motion exercises [Citation5]. Stretching is another common strategy, but the effect of stretching on contracture prevention or treatment is unclear [Citation13]. Furthermore, in case of a proximal amputation, the lever is short. The success of contracture prevention also depends on a patient’s compliance with the prevention methods [Citation8]. Moreover, the effects of postoperative care are influenced by amputation level, skills of surgeons, surgical techniques [Citation4], and the patient’s age and comorbidities (diabetes, peripheral vascular disease, other infections) [Citation14,Citation15].
Hip or knee contractures influence walking biomechanics [Citation16] and lead to gait deviations [Citation17]. Contracture simulations in healthy individuals show that when the knee flexion contracture is more than 15°, the maximum axial load on both knees (contracture and non-contracture knees) increases [Citation18], and a knee flexion contracture of 30° changes trunk kinematics in all planes [Citation19]. Therefore, a knee flexion contracture may be associated with an increase in severity of knee osteoarthritis, knee pain, and back pain [Citation18,Citation19]. Low back pain has been reported in a person with a transfemoral amputation and a hip flexion contracture [Citation20].
Earlier receipt of a prosthesis improves mobility [Citation10,Citation11] and positively affects the emotional state and self-image of the prosthesis user [Citation15]. One review considered the ability to walk with a prosthesis as the main factor for improving quality of life [Citation21]. Moreover, not providing the prosthesis at all or delaying receipt of the prosthesis increases healthcare costs by approximately 25% [Citation22]. Consequently, not receiving a prosthesis due to a severe flexion contracture may hinder a person’s desire to ambulate, increase complications associated with prolonged periods of immobility, and lead to further limitations in activities of daily living.
The Atlas of Limb Prosthetics suggests that fitting a prosthesis is difficult when the flexion contracture angle of the knee or hip is more than 25° [Citation23–25]. In contrast to this suggestion, many prostheses have been made for persons with a lower limb amputation and a flexion contracture [Citation26]. These prostheses tend to be bulky, which affects their cosmetic appearance [Citation24,Citation25]. Given that cosmetic appearance is highly associated with prosthesis satisfaction and is particularly important for the body image of women [Citation27], it is important to pay attention to this aspect in the fitting process.
There is a paucity of research on prosthesis fitting in persons with a severe hip or knee contracture [Citation28–30], even though such research is beneficial for rehabilitation clinicians when prescribing a lower limb prosthesis. Therefore, this systematic review aims to contribute to the evidence base regarding prosthesis prescription in persons with a flexion contracture. The specific aims of this study were to 1) explore whether prosthesis fitting is possible in persons with a hip or knee flexion contracture ≥25°, 2) discuss designs of TT and TF prostheses, and 3) illustrate the possibilities and problems related to prosthesis fitting in persons with a severe flexion contracture.
Methods
PubMed, Embase, Scopus, CINAHL databases were searched for studies on the fitting of lower limb prostheses in persons with severe hip or knee flexion contractures. The Orthotics & Prosthetics Virtual Library was also searched because it contains earlier issues of the Journal of Prosthetics & Orthotics that were published under the headings Newsletter: Prosthetics & Orthotics Clinic and Clinical Prosthetics & Orthotics. Search strategies included combinations of database specific search terms relating to amputation or prosthesis and contracture. The search term “prosthesis” was not used in the Orthotics & Prosthetic Virtual Library because all the articles in this database already concern either prostheses or orthoses (Appendix 1). No restrictions were applied for publication year, study type, or language. The last search was performed on 11 December 2019. (Supplementary Appendix 1, ).
Only primary research that concerned the fitting of lower limb prostheses in persons with a hip or knee flexion contracture was included. Titles and abstracts were assessed by two reviewers independently (JP, JHB). Inter observer-reliability was assessed using Cohen’s kappa [Citation31]. All titles and abstracts selected by at least one of the reviewers were included for full-text assessment. Papers written in another language than the reviewers were skilled in, were translated into English by persons who were able to read and write that language and English. Full-texts were assessed by two reviewers independently (JP, PUD), using the same criteria. In addition, the texts had to include severe hip or knee flexion contractures (≥25°). Any disagreement between the reviewers was discussed until consensus was reached. Next, included studies were assessed (JP, PUD) for quality using the critical appraisal checklist for case reports of the Joanna Briggs Institute [Citation32]. This tool has eight criteria; each criterion was scored 0 if the article did not meet the criterion and 1 if it did. Disagreement in quality assessment between the reviewers was discussed until consensus was met. This manuscript follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guideline [Citation33] (Supplementary Appendix 2).
Results
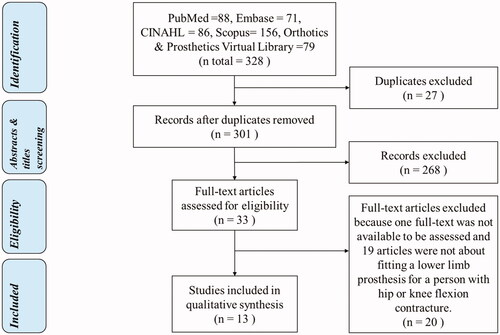
In total, 301 titles and abstracts were screened, and 33 full-texts were included for full-text selection (Inter observer agreement = 86%, kappa = 0.46). Besides not being a primary study and not including a human participant, 268 abstracts were excluded during screening because they concerned arthroplasties, endoprostheses, surgical techniques/experiences/options, postoperative care/treatments/complications, upper limb prostheses, and flexion angles <25° or mild contractures. After full-text selection, 13 studies published between 1958 and 2017 were included for methodological quality assessment (Inter observer agreement = 94%, kappa = 0.88) [Citation34–46], and 20 studies were excluded [Citation9,Citation47–65]. Studies translated into English included three studies written in Russian [Citation34,Citation54,Citation65], and 3 studies written in Dutch [Citation51], Croatian [Citation39], and Polish [Citation56], respectively. The quality sum scores ranged from two to seven (). Studies concerning TT prostheses are presented first and in chronological order.
Table 1. Quality assessment results of 13 case reports based on the Joanna Briggs Institute critical appraisal checklist.
Transtibial prosthetic designs for persons with a severe knee flexion contracture
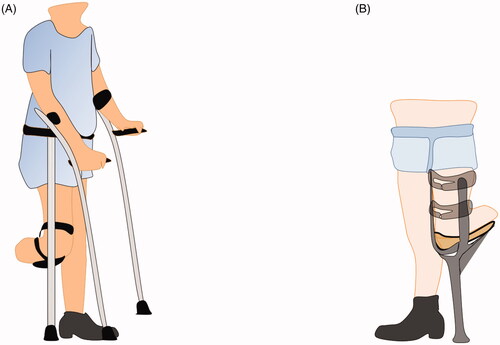
Ten studies reported on TT prostheses in persons with knee flexion contractures (). Prostheses designs allowed for the fitting of a prosthesis in persons with a knee contracture up to 90°. Body weight was transferred from the residual limb via a socket () or a kneeling platform or bearer () to the ground by means of a crutch (), sidebars with knee hinges ( and ) or a shank and a foot (). Suspensions used were self-suspension by belts or Velcro straps ( and ), a thigh corset (), or a socket trimline above the femoral condyles (). Some designs enabled adjustment of socket angles once the contracture improved ().
Figure 2. A shows a socket connected with a crutch; B shows a socket connected with a thigh corset, a shank, and foot by metal sidebars; C shows a transtibial socket connected with a shank and a foot.
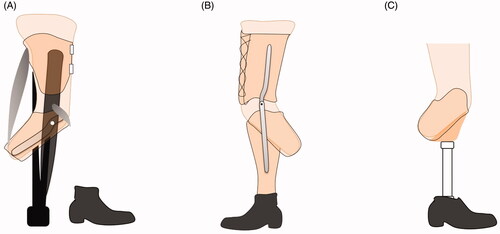
Table 2. Summary of prostheses designs and fitting results.
For TT prostheses with sidebars (), the knee hinge joint was optional. If used, it can be locked or unlocked depending on the person’s ability to control the knee joint [Citation40]. An extra joint can be added for sitting [Citation42].
Transfemoral prosthetic designs for persons with a severe hip flexion contracture
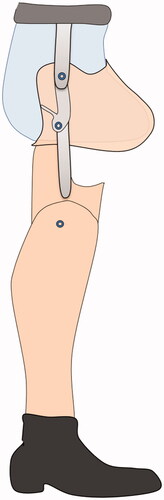
Five studies reported about the fitting of TF prostheses (). One case reported on a bilateral amputation (TT and TF) [Citation35,Citation41]. Similar to TT prostheses, TF prostheses consisted of a socket, knee, shank, and foot. In some cases, an extra joint was added underneath the socket to increase range of flexion during sitting [Citation35,Citation44] ().
Aesthetic considerations regarding TT and TF prostheses for severe flexion contractures
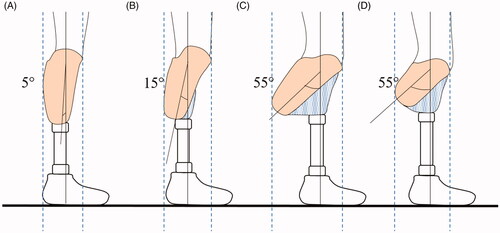
When sitting, a bent prosthesis sticks out [Citation35,Citation42,Citation44] (). An extra joint added underneath the concerned joints helps to increase range of motion and cosmesis [Citation35,Citation42,Citation44] (). This extra knee joint, attached underneath the socket of a person with a bilateral TT with a 45° knee flexion contracture was illustrated recently [Citation66]. In a person with a TF amputation who had a hip flexion contracture, a similar technique was used by adding an extra hinge connecting the socket and the knee joint or another prosthetic knee joint underneath the TF socket [Citation35] (). The socket also sticks out when standing and walking. The extent to which the socket sticks out depends on the flexion contracture angle and the length of the residual limb ( and ). A small flexion contracture can be accommodated more easily than a larger flexion contracture ( and ). A short residual limb length can also be accommodated more easily and has better cosmesis than a longer residual limb ( and ). This is in line with a case report on a person with a 50° knee flexion contracture and a residual limb length of 3 cm [Citation42]. Conversely, persons with a long residual limb are more likely to have a bulky stump and may experience difficulties when getting dressed. However, a long residual limb may provide a larger lever arm for controlling a prosthesis.
Figure 5. A shows a transtibial amputee sitting with a bent knee prosthesis without an extra joint; B shows a transfemoral amputee sitting with a bent hip prosthesis with a flexion contracture plate; C shows compensation material to offset the socket; D and E show transtibial and transfemoral amputees with an extra joint underneath the socket to increase the seating cosmetic.
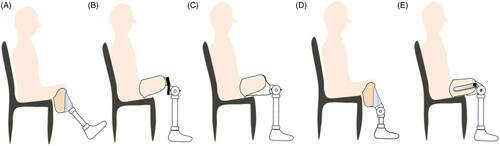
Figure 6. shows different degrees of transtibial socket flexion and path of the weight line dropping from mid socket and passing through the ankle. The distance between the 2 dotted lines shows the bulkiness of the socket in which the greatest distance is the bulkiest prosthesis. For the same residual limb length, the bulkiest is the most flexed socket (C > B > A), and for the same angle, it is the longer residual limb length (C > D).
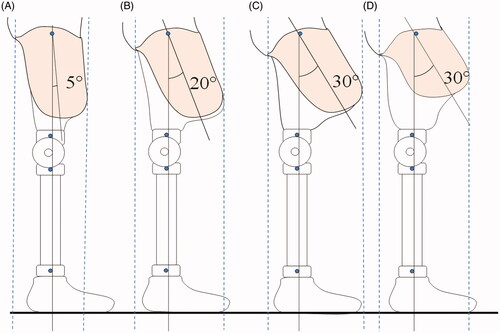
Figure 7. shows different degrees of transfemoral socket flexion and path of the weight line dropping from trochanter, falling in front of the knee and passing through the ankle. The distance between the two dotted lines shows the bulkiness of the socket in which the greatest distance is the bulkiest prosthesis. For the same residual limb length, most bulkiness occurs in the most flexed socket (C > B > A) and, for the same angle, it occurs in the longer residual limb (C > D).
Discussion
There are several possibilities for fitting a TT or TF prosthesis in persons with a severe flexion contracture of the knee, hip, or even both joints. The case reports included in this study date back to 1958. Despite the limited technology available at the time, prostheses could still be made and fitted. Generally, a TT prosthesis includes a socket, shank, and foot, which are connected to the residual limb by means of a suspension system. Similar designs were used in TF cases, but these designs employed a knee joint. Prosthetic knee joints and orthotic knee joints (sidebars and with knee hinges) are both used to connect the thigh part and the shank and to enable motion of the knee.
Alignment and biomechanics of a bent prosthesis in persons with a severe hip or knee flexion contracture
For persons with a severe flexion contracture, the socket is set to accommodate the angle of the knee or hip flexion contracture. An increase in socket flexion can create excessive pressure on the anterior proximal tibia, the patellar tendon, the patella of a TT residual limb, and the posterior aspect of a TF residual limb. For that reason, the knee and tibial crest area should be sufficiently supported within the socket, or a liner should be used to disperse the pressure over the residual limb and prevent skin breakdown [Citation36,Citation40,Citation43,Citation46]. Other solutions include using a thigh corset or quadrilateral brim in order to enable appropriate weight distribution between the tibia and thigh [Citation36,Citation38] or using a total contact socket [Citation40,Citation43].
During walking, a hip flexion contracture limits the hip extension required for walking stability. After heel strike, when the ground reaction force passes behind the knee, knee-buckling occurs, opposed by contraction of hip extensors, knee joint mechanics, and prosthesis alignment [Citation67–69]. The voluntary control of the hip may not be possible in persons with a large hip flexion contracture [Citation67,Citation68], and they may compensate this by tilting the pelvis anteriorly and increasing lumbar lordosis [Citation70]. However, none of the included case studies reported on this mechanism. In some persons, knee hinges with a locking mechanism were used to ensure knee stability [Citation35].
Persons with both hip and knee flexion contractures may not be able to stabilize the knee sufficiently using the knee or hip muscles. In studies that included persons with both hip and knee contractures, knee extension aids were added to the prosthesis [Citation36,Citation38]. In persons with severe hip and knee flexion contractures, anterior trunk bending occurs if the person is standing and gait aids (crutches) need to be provided for support [Citation38]. Anterior trunk bending may increase knee stability and the crutches enable weight sharing.
Persons with a transfemoral amputation but without a contracture demonstrated restrictions in hip motions, in which an amputated hip flexes and extends less [Citation71,Citation72]. This effect did not only limit their ability to control the prosthetic knee during early stance, but also reduced knee flexion during swing. The prosthesis could be shortened to facilitate toe clearance [Citation71]. However, a study showed that a shorter prosthetic side (mean =1.1 cm (SD = 0.5) increased postural and gait asymmetries, and it may be associated with impaired balance and back pain [Citation71].
Contracture causes gait asymmetries [Citation18,Citation19,Citation43,Citation73], which are already higher in amputees compared with able-bodied persons (23% force asymmetry in persons with an unilateral lower limb amputation and 10% in able-bodied persons [Citation17]). In the long term, greater force on the intact limb may lead to degeneration of weight-bearing joints and joint pain [Citation17]. Lower loading on the amputated limb may lead to osteopenia and subsequently, osteoporosis [Citation17]. A simulation study suggested that persons with a transtibial amputation with 10% loss of muscle strength require compensation from other muscles to minimize gait deviation, resulting in a higher metabolic cost [Citation74]. For those reasons, persons with a severe hip or knee contracture will likely have an increase in gait deviations, require more energy to walk with the bent prosthesis, and have a higher risk of knee and/or back problems.
Therefore, it is essential to consider exercises, stretching, splinting, or other contracture treatments to relieve the knee flexion contracture in addition to the prosthesis use. In the reports about a bent knee pylon or kneeling bearer, the knee was held in 90° flexion during walking, but there was still a reduction in flexion contracture [Citation37]. Although they are easy to fabricate and cost-effective [Citation37], in some cases the knee flexion contracture increased after the use of a bent knee pylon [Citation37,Citation38]. Hence, no matter what type of prosthetic device is fitted, the receivers should be trained in stretching and exercising their limbs. For example, adaptive training sessions were given to a person with a TT amputation with a knee flexion contracture [Citation43]. After four months of training, improvements were found in the knee’s range of motion, the level of functioning, and the person’s quality of life [Citation43].
When flexion contracture changes, the prosthesis should be realigned [Citation43]. Before dynamic alignment, which takes place during walking, a prosthesis is set on the bench first (bench alignment). For stability, prosthetic components are set in such a way that a vertical reference line falls from mid socket to anterior of the ankle centre of a SACH foot [Citation75]. Likewise, in a TF prosthesis, the weight line dropping from trochanter should fall in front of the knee and pass through the ankle [Citation67–69] ( and ). Determining appropriate weight bearing from the bent socket to a foot can be challenging.
In some cases, a temporary or trial prosthesis was fitted first; once the contracture was reduced or gait improved, the definitive prosthesis was made [Citation41,Citation45]. Some prosthetic components such as socket or foot connectors/adaptors allow some degree of alignment adjustment [Citation43]. Moreover, the fabrication technique can be facilitated by using a socket connector with a preset flexion angle and offset length to reduce the time and labour needed for fabrication [Citation76]. Different offset lengths and preset flexion angles are available, depending on the manufacturer [Citation76–78]. If the flexion plate is designed for fabricating a TF prosthesis with a hip flexion contracture (), the plate can be flipped and used for the TT prosthesis fabrication as well [Citation78].
Although it is possible to fit a prosthesis in persons with a severe flexion contracture, prevention of contractures is important. When occurred, contractures should be treated prior to, parallel to, and after prosthesis fitting since a flexion contracture is a predictor of unsuccessful rehabilitation [Citation79].
Limitations of the study
Most case studies used were published before the year 2000, which means the prosthetic materials used may not represent current technologies. Although case reports report on novelties and offer educational value, their generalizability is limited [Citation80]. Reporting bias may be present because cases may have been selectively reported based on successful fitting results [Citation80]. Due to the study design, combining the results of studies was not possible. Three studies [Citation34,Citation39,Citation40] had very low quality scores; they only met two or three out of the eight checklist criteria. Outcomes were generally described as “a stable gait” or “able to participate in activities” and details of the gait characteristics in each walking phase were not provided. Many studies did not report on adverse effects of the use of bent prostheses. Only one study reported on how the alignment of the bent TT prosthesis affected kinematics and kinetics of walking [Citation43]. In some of the cases described, a decrease in the flexion contracture was found, probably due to the prosthesis fit, exercise training and, most importantly, the person’s compliance. However, only one study reported in detail about the types of therapy provided together with the use of prosthesis [Citation43]. Lastly, the protocol of this review study was not registered prior to the study.
Conclusions
Fitting a prosthesis in a person with a flexion contracture ≥25° can be challenging, but it is certainly possible, as this study has illustrated. Even in case of severe contractures and highly complex cases, fitting a prosthesis remains possible. However, the level of evidence to support certain choices regarding prosthetic adaptations remains low.
In their decision-making process, clinicians should consider the person’s motivation to walk as a more important determining factor than a flexion contracture ≥ 25°. A strong motivation to walk or participate in activities has helped prosthesis users overcome esthetic issues and gait deviations. Because a severe hip or knee contracture can hinder walking and lead to other subsequent problems, interventions to reduce the contracture should be employed along with the use of bent prostheses.
Supplementary Appendix 2
Download MS Word (19.7 KB)Supplementary Appendix 1
Download MS Word (13 KB)Disclosure statement
The authors report no conflicts of interest.
References
- Yoo S. Complications following an amputation. Phys Med Rehabil Clin N Am. 2014;25(1):169–178.
- Pohjolainen T. A clinical evaluation of stumps in lower limb amputees. Prosthet Orthot Int. 1991;15(3):178–184.
- Farmer SE, James M. Contractures in orthopaedic and neurological conditions: a review of causes and treatment. Disabil Rehabil. 2001;23(13):549–558.
- Jaegers SMHJ, Arendzen JH, De JHJ. Changes in hip muscles after above-knee amputation. Clin Orthop Relat Res. 1995;(319):276–284.
- Coletta EM. Care of the elderly patient with lower extremity amputation. J Am Board Fam Pract. 2000;13(1):23–34.
- Goldberg T. Postoperative management of lower extremity amputations. Phys Med Rehabil Clin N Am. 2006;17(1):173–180.
- Sasabe R, Sakamoto J, Goto K, et al. Effects of joint immobilization on changes in myofibroblasts and collagen in the rat knee contracture model. J Orthop Res. 2017;35(9):1998–2006.
- Ghazali MF, Razak NAA, Osman NAA, et al. Awareness, potential factors, and post-amputation care of stump flexion contractures among transtibial amputees. Turk J Phys Med Rehabil. 2018;64(3):268–276.
- Burgess EM, Zettl JH. Immediate post-surgical prosthetics. Proceedings of the 1966 Assembly of the American Orthotic and Prosthetic Association; 1966. p. 105–112.
- Ali MM, Loretz L, Shea A, et al. A contemporary comparative analysis of immediate postoperative prosthesis placement following below-knee amputation. Ann Vasc Surg. 2013;27(8):1146–1153.
- van Velzen AD, Nederhand MJ, Emmelot CH, et al. Early treatment of trans-tibial amputees: retrospective analysis of early fitting and elastic bandaging. Prosthet Orthot Int. 2005;29(1):3–12.
- Chin T, Toda M. Results of prosthetic rehabilitation on managing transtibial vascular amputation with silicone liner after wound closure. J Int Med Res. 2016;44(4):957–967.
- Katalinic OM, Harvey LA, Herbert RD, et al. Stretch for the treatment and prevention of contractures (Review). Cochrane Database Syst Rev. 2017;91(1):11–24.
- Huang ME, Nelson VS, Flood KM, et al. Limb deficiency and prosthetic management. 3. Complex limb deficiency. Arch Phys Med Rehabil. 2006;87(3):15–20.
- Smith DG, McFarland LV, Sangeorzan BJ, et al. Postoperative dressing and management strategies for transtibial amputations: a critical review. J Rehabil Res Dev. 2003;40(3):213–224.
- Attias M, Chevalley O, Bonnefoy-Mazure A, et al. Effects of contracture on gait kinematics: a systematic review. Clin Biomech (Bristol, Avon). 2016;33:103–110.
- Gailey R, Allen K, Castles J, et al. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–30.
- Harato K, Nagura T, Matsumoto H, et al. Knee flexion contracture will lead to mechanical overload in both limbs: a simulation study using gait analysis. Knee. 2008;15(6):467–472.
- Harato K, Nagura T, Matsumoto H, et al. A gait analysis of simulated knee flexion contracture to elucidate knee-spine syndrome. Gait Posture. 2008;28(4):687–692.
- Traballesi M, Porcacchia P, Averna T, et al. Prognostic factors in prosthetic rehabilitation of bilateral dysvascular above-knee amputee: is the stump condition an influencing factor? Eura Medicophys. 2007;43(1):1–6.
- Davie-Smith F, Coulter E, Kennon B, et al. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: a systematic review of the literature. Prosthet Orthot Int. 2017;41(6):537–547.
- Miller TA, Paul R, Forthofer M, et al. Impact of time to receipt of prosthesis on total healthcare costs 12 months postamputation. Am J Phys Med Rehabil. 2020;99(11):1026–1031.
- Bowker JH, Thomson RG. Management of musculoskeletal complications. In: Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. 1st ed. St. Louis, Toronto, London: American Academy of Orthopaedic Surgeons; 1981.
- Bowker JH, Michael JW. Atlas of limb prosthetics: surgical, prosthetic and rehabilitation principles. 2nd ed. St. Louis (MO): American Academy of Orthopaedic Surgeons; 1992.
- Bowker JH. The art of prosthesis prescription. In: Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. 3rd ed. Rosemont (IL): American Academy of Orthopaedic Surgeons; 2004.
- Webling DD, Fahrer M. Early bent knee prostheses: ancestors of K9. Br Med J (Clin Res Ed). 1986;293(6562):1636–1637.
- Murray CD, Fox J. Body image and prosthesis satisfaction in the lower limb amputee. Disabil Rehabil. 2002;24(17):925–931.
- The Rehabilitation of Individuals with Lower Limb Amputation Work Group. VA/DoD Clinical practice guideline for rehabilitation of individuals with lower limb amputation. Department of Veterans Affairs, Department of Defense; 2017. Available from: https://www.healthquality.va.gov/guidelines/Rehab/amp/VADoDLLACPG092817.pdf
- Geertzen J, Van Der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: rehabilitation process and prosthetics. Part 2. Prosthet Orthot Int. 2015;39(5):361–371.
- Geertzen J, Van Der Linde H, Rosenbrand K, et al. Dutch evidence-based guidelines for amputation and prosthetics of the lower extremity: amputation surgery and postoperative management. Part 1. Prosthet Orthot Int. 2015;39(5):351–360.
- McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–282.
- Moola S, Munn Z, Tufanaru C, et al. Appendix 7.4 Critical appraisal checklist for case reports. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute reviewer’s manual. Adelaide: Joanna Briggs Institute; 2017.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.
- Beliakov PD. Prosthesis apparatus for elimination of flexion contracture of the knee joint after leg amputation. Ortop Travmatol Protez. 1958;19(1):62–63.
- Alexander J, Herbison G. Prosthetic rehabilitation of a patient with bilateral hip-flexion contractures: report of a case. Arch Phys Med Rehabil. 1965;46(10):162–165.
- Ruskin AP, Rosner H, Saperstein H. Bent-knee prosthesis. Geriatrics. 1970;25(7):109–114.
- Pennell CR, Mayfield GW. Bent knee pylon for the below-knee amputee. Bull Prosthet Res. 1973;10(19):77–83.
- Titner H. Fitting and fabrication of a prosthesis for a severe flexion contracture: case study. Bull Prosthet Res. 1973;10(19):84–87.
- Gajsak K. The problem of stumps in flexion contracture (author’s transl). Lijec Vjesn. 1977;99(6):143–144.
- Bannister PJ. The prosthetic problems of below knee amputees with flexion contractures. Aust J Physiother. 1978;24(1):21–25.
- Alexander J. Irreversible contractures: an impediment to prosthetic rehabilitation. Am Acad Orthotists Prosthetists. 1980;4(3):1–2.
- Hays RD, Leimkuehler JP, Miknevich MA, et al. An alternative bent-knee prosthesis. Arch Phys Med Rehabil. 1992;73(11):1118–1121.
- Kim SB, Ko CY, Son J, et al. Relief of knee flexion contracture and gait improvement following adaptive training for an assist device in a transtibial amputee: a case study. J Back Musculoskelet Rehabil. 2017;30(2):371–381.
- Freed MM. Modified prosthesis compensating for above-knee amputation with fixed hip contracture. Arch Phys Med Rehabil. 1962;43:254–255.
- Lippmann HI. Rehabilitation of the lower extremity amputee with marked flexion contractures: report of two cases. Arch Phys Med Rehabil. 1967;48(3):147–149.
- Biedermann WG. Management of short above-knee amputees. Orthot Prosthetics. 1976;30(4):21–29.
- Slivkov P. Flexion contractures and muscle power in bilateral above knee amputees (Bulgarian). Ortop i Travmatol. 1975;12(2):95–98.
- Amstutz MW. Unique treatment approach for a patient with a below-the-knee amputation. Phys Ther. 1981;61(1):37–39.
- Fergason JR, Blanck R. Prosthetic management of the burn amputation. Phys Med Rehabil Clin N Am. 2011;22(2):277–299.
- Gottschalk F. The importance of soft tissue stabilization in trans-femoral amputation: English version. Orthopäde. 2016;45(S1):1–4.
- Hacking HGA, Lo-A-Njoe BAE, Visser-Meily JMA. Multipele amputaties wegens sepsis; toch mogelijkheden voor functioneel herstel? Ned Tijdschr Geneeskd. 1999;143(21):1073–1077.
- Haga N, Karita T, Amao R, et al. Successful ambulation by surgical conversion in a complex form of epigastric heteropagus. J Pediatr Orthop B. 2009;18(6):394–396.
- Sol-Bi K, Jeicheong R, Ho SJ, et al. ISPO World Congress 2015 – Abstract list: enhancement of knee range of motion and gait features in a trans-tibial amputee with knee flexion contractures via an adaptive training for an assistive device program. Prosthet Orthot Int. 2015;39(1_suppl):6.
- Sanin VG, Moreynis KI, Kim OA. Clinico anatomical features of prosthesis of women with hip stumps (Russian). Ortop Travmatol i Protez. 1976;9:49–52.
- Ward RS, Hayes-Lundy C, Schnebly WA, et al. Rehabilitation of burn patients with concomitant limb amputation: case reports. Burns. 1990;16(5):390–392.
- Wasiak K. Analysis of prognostic factors for locomotion in patients after amputation of the tibia performed due to atherosclerotic critical limb ischemia. Ortop Traumatol Rehabil. 2005;7(4):411–417.
- Liao SJ, Schnell A. A functional above-the-knee prosthesis for geriatric patients. J Bone Joint Surg Am. 1964;46(6):1292–1294.
- Chand N, Srivastava RK, Maish AR. Hanging stump prosthesis without socket for bad above-knee stumps. Prosthet Orthot Int. 1985;9(3):154–156.
- Radcliffe CW. Four-bar linkage prosthetic knee mechanisms: kinematics, alignment and prescription criteria. Prosthet Orthot Int. 1994;18(3):159–173.
- Haslam ET. Prosthetic prescription for the geriatric amputee. Prosthetics Int. 1965;2:212–214.
- Traub JE. Developmental research in private facility. Orthop Prosthet Appl J. 1961;168–173.
- Loro A, Franceschi F, Mosha ECP, et al. A survey of amputations at Dodoma Regional Hospital, Tanzania. Prosthet Orthot Int. 1990;14(2):71–74.
- Radcliffe CW, Johnson NC, Foort J. Some experience with prosthetic problems of above-knee amputees. Artif Limbs. 1957;4(1):41–75.
- Wilson AB. Recent advances in above-knee prosthetics. Artif Limbs. 1968;12(2):1–27.
- Kondrashin NI, Gusulaev GM. Correction of the flexion contractures of the leg stump with the Volkov-Oganesyan apparatus. Ortop Travmatol i Protez. 1979;12:34–37.
- Krajbich JI, Pinzur MS, Potter BK, et al. Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. 4th ed. Rosemont (IL): American Academy of Orthopaedic Surgeons; 2016.
- Schuch CM, Pritham CH. Transfemoral amputation: prosthetic management. In: Smith DG, Michael JW, Bowker JH, editors. Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. 3rd ed. Rosemont (IL): American Academy of Orthopaedic Surgeons; 2004.
- Muller MD. Transfemoral amputation: prosthetic management. In: Krajbich JI, Pinzur MS, Potter LBK, Stevens PM, editors. Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. 4th ed. Rosemont (IL): Academy of Orthopaedic Surgeons; 2016. p. 537–554.
- Radcliffe CW. Functional considerations in the fitting of above-knee prostheses. Artif Limbs. 1955;2(1):35–60.
- Lusardi MM, Nielsen CC. Orthotics and prosthetics in rehabilitation. 2nd ed. St. Louis (MO): Saunders Elsevier; 2007.
- Gaunaurd I, Gailey R, Gomez-Marin O, et al. Postural asymmetries in transfemoral amputees. Prosthet Orthot Int. 2011;35(2):171–180.
- Rabuffetti M, Recalcati M, Ferrarin M. Trans-femoral amputee gait: socket-pelvis constraints and compensation strategies. Prosthet Orthot Int. 2005;29(2):183–192.
- Pruziner AL, Werner KM, Copple TJ, et al. Does intact limb loading differ in servicemembers with traumatic lower limb loss? Clin Orthop Relat Res. 2014;472(10):3068–3075.
- Esposito ER, Miller RH. Maintenance of muscle strength retains a normal metabolic cost in simulated walking after transtibial limb loss. PLoS One. 2018;13(1):1–19.
- Radcliffe CW, Foort J. The patellar-tendon-bearing below-knee prosthesis. Berkeley (CA) and San Francisco (CA): Biomechanics Laboratory, University of California; 1961.
- Mantelmacher HL. Prosthetic socket centering block. European Patent; EP2790613B1; 2004 [cited 2018 Aug 16]. Available from: https://patentimages.storage.googleapis.com/e6/aa/1d/1af7542ac484da/EP2790613B1.pdf
- Slemker TC, Schall SR. Flexion contracture TKA adaptor. U.S.; US 6,991,658 B2. [cited 2018 Aug 16]. Available from: https://patentimages.storage.googleapis.com/50/8c/a2/852946c4fc0116/US6991658.pdf
- Krosin R. The pin lock reference manual for prosthetists. Ohio: Hanger Prosthetics & Orthotics. 2005.
- Munin MC, Espejo-De Guzman MC, Boninger ML, et al. Predictive factors for successful early prosthetic ambulation among lower-limb amputees. J Rehabil Res Dev. 2001;38(4):379–384.
- Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes. 2014;7:264–267.