Abstract
Purpose
To further understand social and leisure (SL) participation after stroke and how it can be supported in a long-term perspective, this study aims to deepen the understanding of strategies used by long-term stroke survivors in relation to SL activities.
Materials and methods
The study has a qualitative design, using a grounded theory approach, and is based on in-depth interviews with 10 persons who had a stroke 15 years ago and four of their family members.
Results
The findings comprise nine different strategies used by the participants. These had two overarching purposes; to protect and re-construct the post-stroke self and to enable participation in valued SL activities despite challenges. The findings are summarized in one overarching theme: “Employing different strategies to balance costs and rewards of engagement in social and leisure activities”.
Conclusions
Strategies for SL participation involves balancing different priorities in life and can change over time as they are continuously influenced by various personal and environmental conditions. These findings contribute to an improved understanding of why and how people hold on to activities, give up activities and find new activities after a stroke. It also highlights the need for a long-term perspective on stroke rehabilitation and support.
Re-engagement in social and leisure activities after stroke is a long-term process and various types of support may be needed during different stages of recovery and adaptation.
Successful rehabilitation interventions build on an understanding of each individual’s priorities, goals and strategies and how these may change or manifest over time.
Special attention should be given to the individual’s perception of costs and benefits in relation to engagement in activities, and the role that it has for the person’s identity.
By providing knowledge and supporting the use of adequate coping strategies, rehabilitation professionals can help patients find a new and accepted post-stroke identity.
IMPLICATIONS FOR REHABILITATION
Background
Stroke is a global health problem and one of the most common reasons for long-lasting and complex disability among adults [Citation1,Citation2]. As an increasing number of people survive and age with the consequences of a stroke [Citation3] awareness has grown regarding the need for long-term support and rehabilitation. Experiencing a stroke can be a life-changing event that affects all areas of life, and its profound impact on identity, roles, relationships, activities and participation has been well described [Citation4,Citation5]. Difficulties taking part in previous leisure activities and social isolation are common [Citation6,Citation7]. This is an important problem, considering that participation in social and leisure activities is related to higher subjective well-being [Citation8,Citation9], less depressive symptoms [Citation10], improved functional recovery and survival [Citation11,Citation12] after stroke. The central role of social and leisure engagement for health in later life has been demonstrated among people with other chronic conditions [Citation13] and in the general population [Citation14].
Even though participation restrictions are common and seem to persist over time after stroke [Citation15,Citation16], recent long-term follow-up studies [Citation17,Citation18] show that several stroke survivors manage to reengage in social and leisure activities. Individual differences can partially be explained by factors such as age, previous participation, perceived recovery, mobility and social networks [Citation18,Citation19]. In a previous study [Citation20] we found that personal as well as environmental conditions influence people’s perceived capacity and motivation to participate in social and leisure activities long term after stroke. Existing research also suggests that people’s abilities to overcome challenges and to adapt their behaviour and attitude are central to social participation and community integration after stroke [Citation6,Citation7,Citation21]. Hence, researchers have emphasized the importance of supporting appropriate coping strategies throughout the long-term recovery and adaptation processes [Citation22]. It has also been stressed that successful rehabilitation interventions need to be grounded in an awareness of the stroke survivors’ own goals and strategies [Citation23].
The term “strategy” generally refers to a plan of action aimed at a certain goal. In the context of the present study, all goal oriented actions that directly or indirectly influence participation in social and leisure activities will be considered strategies in this broad sense. Thus, including, but not limiting the study to, what is most often termed coping strategies. Coping strategies can be behavioural as well as cognitive/psychological [Citation24] and are used to describe how people adapt to external or internal demands such as disabilities and ageing [Citation25].
To further understand social and leisure participation after stroke and how it can be supported in a long-term perspective, this study aims to deepen the understanding of strategies used by long-term stroke survivors in relation to social and leisure activities.
Methods
Study design
This study is part of a larger project on activity and participation long-term after stroke [Citation17,Citation19]. The current study has a qualitative design and is one of two interconnected studies based on the same interview material, of which the first [Citation20] focused on conditions for social and leisure participation after stroke, and the current, on strategies used by the stroke survivors. Both studies were guided by a grounded theory approach [Citation26]. This method was selected as it is especially suitable to explain behaviour and processes.
Sampling and participants
The study is based on individual in-depth interviews with ten stroke survivors, who all had a first-ever stroke 15 years earlier, and four of their family members. The participants were recruited from the Lund Stroke Register (LSR), a population based register of all persons with first-ever stroke in the uptake area of Skåne University Hospital in Lund, Sweden [Citation27]. The original sample (March 2001 – February 2002) consisted of 416 people. Among those still alive (n = 108, as of March 2016), 15 potential participants were selected, utilizing a purposive sampling strategy [Citation28]. The sampling built on quantitative data collected at stroke onset and at follow-ups after 16 months and 10 years, and aimed for variation regarding age, gender, functional status, living situation and frequency of social and leisure activities. In line with grounded theory methodology [Citation26], sampling, data collection and analysis were performed in parallel to determine the need for additional sampling. When eight participants had consented and been interviewed, two additional participants were recruited to ensure that the study included the perspectives of those with mild to severe disabilities and a wide age span. In addition, four family members (two adult children and two spouses) were interviewed to complement and enrich the narratives told by the participants with stroke and to further understand their supportive role. Theoretical saturation was employed to determine the final sample size.
The final sample included five women and five men with stroke (age 33–88 years, median 76). At the time of the interviews, nine participants lived in ordinary housing. Seven lived with a spouse. All were retired or on sick leave except one participant who was working full time. Two participants had sustained a recurrent stroke. Two participants were wheelchair users. Otherwise, the majority were independent in personal care and indoor mobility but experienced some mobility limitations outside home. Four participants experienced difficulties in their everyday life related to cognitive impairments and one had verbal communication problems. Additional characteristics of the participants at stroke onset and previous follow-ups are outlined in .
Table 1. Characteristics of the participants with stroke (n = 10) based on data collected at stroke onset, 16 months and 10 years after stroke.
Data collection
The participants were initially contacted by telephone and asked to participate. All were offered to have someone close to them accompany them during the interview. Accordingly, one participant, who had communication difficulties, was supported by a spouse. Another, by an adult child. All interviews were conducted by the first author (AN) in the participants’ homes (in one case a residential care facility) and lasted 1–1½ h. The interviews focused on participation in social and leisure activities, defined as social or solitary activities engaged in for pleasure, relaxation, or other emotional satisfaction (in contrast to demands or necessities of daily living). A semi-structured interview guide was used to cover central topics, but the interviews allowed the participants to speak freely and for additional topics to emerge. The interview guide was slightly modified throughout the data collection to target concepts that required further development. The interviewer also individualized the content of each interview based on previously collected follow-up data. If the participants had problems recalling the past, the interviewer referred to information concerning his/her previous functional status or life situation to evoke memories of different time periods. A separate interview guide was constructed for the family members, focusing on their role and experiences related to their relative’s participation in social and leisure activities. Field notes were made during and immediately after each session describing the contextual conditions, the interview situation and emerging reflexions. Interviews were recorded and transcribed verbatim and then imported and further analysed in the qualitative data analysis programme NVivo [Citation32].
Data analysis
The interviews were analysed using a grounded theory constant comparative method [Citation28]. This approach aims to create a theoretical framework grounded in the collected data, and takes into consideration the context in which something happens, causal conditions, strategies and consequences [Citation26,Citation33]. Whereas our previous study shed light on personal and environmental conditions for social and leisure participation [Citation20], the current study focused on the behavioural and cognitive strategies used by the participants. To gain a deeper understanding of the participants’ strategies, their underlying goals and rationales as well as the consequences were considered in the analysis. The narratives of the participants with stroke formed the foundation of the analysis, and experiences shared by the family members complemented and enriched the data.
The analysis was an iterative process consisting of several steps, including open coding, development of categories and sub-categories through constant comparison, identification of relations between categories, and finally integration of categories into a central theme [Citation26]. The first author (AN) performed all initial coding and created preliminary categories. Thereafter, she and the last author (EML) worked together to develop the analysis. AN has a clinical background as a physiotherapist with several years of experience in stroke rehabilitation as well as previous experience in qualitative research. EML is an experienced occupational therapist and researcher, also in qualitative methodology. The emerging findings were validated and revised several times after discussions with all authors. In addition, preliminary results were challenged at interdisciplinary research seminars, and any inconsistencies in the analysis were discussed. During this process the authors were also encouraged to constantly re-consider their own pre-understandings. Even though the analysis allowed for interpretation of meaning by the researchers, all emerging concepts and categories were regularly checked against the interview data. In addition to the transcribed interviews, field notes and memos were used to increase the researchers’ insights and awareness of self during the analysis. In the final phases of the analysis, existing theoretical frameworks on activity, participation, coping and ageing were used to enhance the understanding of the findings.
Ethical considerations
The study was approved by the regional ethical review board in Lund (no. 2016/179). Verbal and written information was provided, and participants were informed about their right to refrain from answering any questions or to withdraw from the study at any time. All data was handled confidentially, preventing identification of individuals.
Findings
The findings showed that the participants used different strategies in relation to their engagement in social and leisure activities. However, two overarching purposes were identified; to protect and re-construct the post-stroke self and to enable participation in valued social and leisure activities. This involved balancing engagement in social and leisure activities with the demands of daily life while facing challenges related to stroke as well as to ageing. This resulted in participants either holding on to activities, giving up activities or finding new activities. As personal and environmental conditions changed over time, this was an ongoing process that involved continuous re-evaluation of strategies. During this process the participants constantly had to make priorities, evaluate personal and environmental barriers and resources and weigh expected cost and rewards of engagement in activities (). The findings are summarized in the overarching theme: “Employing different strategies to balance costs and rewards of engagement in social and leisure activities”. In , the main categories that represent the two overarching purposes and nine sub-categories that represent the different strategies used in relation to each of these are presented. The two main categories do not oppose each other but comprise different types of strategies. The first, “protecting and re-constructing the self”, describes the participants engagement in or avoidance of certain social and leisure activities based on their individual priorities, values and attitudes. The second, “enabling participation in valued social and leisure activities”, comprises more practically oriented strategies used by the participants to overcome challenges related to participation in social and leisure activities.
Figure 1. The dynamic process of employing different strategies for social and leisure participation after stroke.
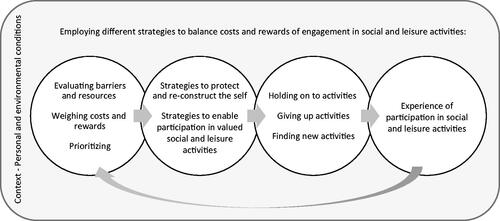
Table 2. Theme, main categories and sub-categories representing strategies for participation in social and leisure activities after stroke.
Protecting and re-constructing the self
The participants employed behavioural as well as cognitive strategies to protect their physical and mental well-being. The strategies could either serve to protect the pre-stroke identity or aim towards building a new one.
Building identity and meaning through social and leisure engagement
As part of re-constructing the self after stroke and to promote their well-being throughout the ageing process, the participants strived to hold on to, or find new, social and leisure activities that strengthened their identity and sense of meaning. They gave up activities that were not perceived as meaningful or conflicted with their self.
Activities that were perceived as meaningful most often provided some kind of reward and matched individual interest, abilities and self-perception. Some activities were immediately self-rewarding in terms of enjoyment, relaxation or social interaction. These included being in the nature, listening to music, reading books, singing in a choir or going to the theatre. Other activities, such as gardening, were also valued because they provided routines and kept the participants occupied.
Participants chose activities that strengthened their identity by making them feel capable or competent. For example, one participant enjoyed being responsible for all computer-based tasks in the household to feel up-to-date. Activities that involved helping others could contribute to feeling needed or important:
Taking care of the grandchildren when they were small and got ill, that has in a way… has disappeared now. Sometimes you don’t feel needed. Then when the 14-year-old calls and asks: Can you pick me up from school? Of course we do. And we always have a snack, that’s important. And that lifts my spirits and I enjoy it so much!
[participant no. 3]
Not being able to perform an activity as before could mean it was perceived as no longer meaningful, and the motivation to engage decreased. Participants also avoided activities that contributed to a feeling of being incompetent. For example, one participant who played golf before stroke gave it up because he could no longer perform to his own satisfaction. Avoiding the activity protected his self as well as his appearance in front of others. Another participant described having stopped going to an activity centre for disabled people because she could not identify with the other attendants.
Prioritizing independence and daily life responsibilities
Prioritizing responsibilities such as work, caring for a family member or managing household chores could mean giving up social and leisure activities. Such priorities changed over time depending on the current life situation. For some, independently performing all household chores contributed to feeling capable and not a burden to others, which helped explain their reluctance to accept help with such chores even though it required a lot from them. However, this could also have negative consequences on their long-term well-being. A couple of participants who had returned to work shortly after the stroke believed the increased strain of working had contributed to chronic pain and exhaustion, which now limited their social and leisure participation. One of them described what he wished he had learned back then:
Maybe to learn what I never learned to do…you know, saying no, I have enough to do now. But I never did [say no], so I was buried in work up to my ears … Yes I need to learn to say stop … I have always been to kind in that way.
[participant no. 7]
Avoiding high-risk activities
Another way of protecting oneself was to reduce the risk of negative consequences such as injuries, pain, extreme fatigue or recurrent stroke. For this reason, some participants avoided activities perceived as high-risk. For example, some had stopped cycling or taking walks to reduce the risk of falling accidents, and others avoided strenuous activities that could lead to pain or fatigue. Cutting down on leisure activities was described as a way to reduce stress and minimize the risk of recurrent stroke. Further, activities were avoided to reduce the risk of disappointment or other types of mental suffering. This was exemplified by one participant who had given up social outings (i.e., going to the theatre or restaurants) due to his repeated negative experiences of delayed or cancelled trips using special transport services. Thus, giving up activities could lead to reduced social and leisure participation, but could also reduce risks of negative consequences that would restrict participation in the long run.
Coping with change
The participants’ behavioural strategies were closely linked to how they mentally coped with their stroke as well as with other changes in life. The interviews revealed two different mental coping strategies; accepting change or waiting for recovery. Depending on which of these two approaches the participants had adopted, different strategies were used in relation to social and leisure engagement.
Participants who had accepted the changes the stroke had imposed on their life situation were more inclined to focus on the present than on the past. They focused on what they currently could do and on the positive aspects of life, sometimes by comparing their own situation to others who were worse off. For some, this meant giving up previous activities, but also finding new ones or new ways of engaging in them. Thus, acceptance most often facilitated participation as it increased motivation and the likelihood of finding activities that were perceived as meaningful and not in conflict with their identity. For most participants, acceptance had grown over time as they gradually adapted to a new normality.
It’s almost like it was before…I just have to think a bit differently. I mean, I do the same things as everyone else but it just takes longer./…/Sometimes I think I should have done it this or that way, but now I have to spend this amount of time instead. I am okay with that.
[participant no. 1]
Participants who kept waiting for improvement tended to be more focused on the past, and saw recovery as the main road to re-engagement in social and leisure activities. Hence, their strategies were more focused on holding on to previous activities rather than finding new ones or adopting compensatory strategies. Even though waiting for recovery could be a barrier for participation, hope of improvement could serve as a motivator for exercise and other efforts to improve capacity, potentially promoting participation in the long term. However, the more passive type of coping appeared related to depressive symptoms and lack of initiative.
Participant: “There is no point in me existing, because no one needs me, I do nothing, I am of no use at all, I do nothing…, and yet I am too afraid to die.”
Interviewer: “Is there anything that could help you, do you think, to get back that joy of living?”
Participant: “To be healthy.”
[participant no. 9]
Enabling participation in valued social and leisure activities
Most participants had tried to resume previous social and leisure activities after the stroke. For some, this was not a problem whereas others experienced greater difficulties. Time and ageing brought additional challenges. To be able to engage in valued social and leisure activities despite of such challenges, participants used strategies involving being persistent, optimizing capacity, adapting or replacing social and leisure activities and reducing other responsibilities.
Being persistent and not giving up
Several participants described that their main strategy towards resuming previous activities involved persistence and to continue trying despite difficulties:
You continue, no complaining. My daughter said, I can help you, but no I do it myself. And maybe you drop things once or twice, but then you learn.
[participant no. 2]
Persistence, I never give up. I always carry through. And I benefited from having that drive, if you can call it that. It was like that when I was working as well. Things could take a long time, but I never gave up, I didn’t.
[participant no. 5]
Optimizing physical and cognitive capacity
Optimizing capacity involved actions to attain or maintain the physical and cognitive capacity needed to participate in certain valued activities, for example through exercise or skills training. Initially after the stroke, several participants had engaged in rehabilitation programs or own training to regain lost functions. The current strategies mainly aimed at maintaining capacity. As pain or depressive symptoms could be barriers for engagement in valued activities, taking action to reduce these problems through medication or psychological treatment were other forms of capacity enhancing strategies. Several participants perceived that an improved capacity was the only way they could participate in valued activities. As expressed by one participant who had tried to improve his aerobic capacity to be able to ride his bike to the town and to the fishing lake:
Interviewer: “Could it work, somehow…what do you think could enable you go there anyway?”
Participant: “I really don’t know… I have thought quite a bit about it, what one could do, but… the fact is I have done what I can. I got an exercise bike that I use a bit. But… I used it more before, I have lost stamina now compared to how it was.”
[participant no. 7]
Adapting activity performance
Various forms of strategies were used to hold on to previous social and leisure activities. Instead of avoiding activities that were challenging or associated with risks, the participants took precautionary measures such as bringing their mobile phone to be able to call if something happened or putting up a handrail by their outer stairs to be able to enter their garden. Moreover, mobility devices and different types of tools (e.g., automated garden tools) were used to compensate for reduced strength or balance. A participant who, for a long time, had avoided making public speeches out of fear of losing the words, could later resume his engagement by using a manuscript. Participants also adapted their activity performance by doing parts of an activity, stopping earlier and taking breaks. Some described that recognizing and adapting to the signals of their body were something they had learned over time. Another strategy was to relocate activities to the home or close surroundings to reduce the need for transportation. Several participants accepted help from others. Even though community based services (e.g., special transport services) were used, participants preferred receiving help from friends and family members as it was more flexible. Moreover, most community based support primarily targeted activities of daily living rather than social and leisure activities. Those who no longer could perform an activity themselves sometimes participated through others. This was exemplified by one participant who engaged in gardening and bingo by giving instructions to her husband who performed the tasks:
Husband: “Well, I am also there, so I place the markers for her.”
Participant: “I show him where.”
Interviewer: “You show him where to place the markers?”
Husband: “Yes exactly!”
[participant no. 6]
Replacing valued social and leisure activities
If participants were not able to overcome the experienced difficulties, activities were sometimes replaced with others that suited their current abilities and life situation. For example, strenuous outdoor activities could be replaced by less demanding activities such as watching television, listening to music and reading books. One participant who had used to go hiking with her husband before the stroke had replaced this with outings in various parks, him driving her in the wheelchair. As the perceived value of hiking were mainly related to the nature experience and spending quality time with her husband, the outings served to fill this gap. Finding new activities was a process that often required active engagement and own initiatives. One participant described that he tried different things and gradually found his way to suitable activities. Others found new activities through patient organisations or parasport centers.
Reducing domestic responsibilities
Some participants chose to spare their time and energy by passing over household chores to family members or payed services, or by moving from an own house to an apartment to reduce the workload. Strategies such as relocation could be based on financial and practical as well as emotional reasons. It also had different consequences on participation. For one participant, moving into a centrally located apartment promoted his participation through improved accessibility to social and leisure activities. For another, such relocation meant reduced possibilities to exercise her gardening interest and to socialize with her previous neighbours.
Discussion
The findings of this study show that, long-term after stroke, participation in social and leisure activities continues to be a dynamic process that involves holding on to activities, giving up activities and finding new ones. Recovery and adaptation, as well as changes in life situation and health due to ageing, can lead to re-prioritizations and re-evaluation of strategies over time. A central finding was that even though different strategies were used by the participants they had the same overarching purposes, that is, to enable participation in valued activities while also protecting and re-constructing the post-stroke self. Moreover, similar strategies could lead to different consequences depending on the context. As in a study among people with acquired brain injury [Citation34], we found that the strategies as well as their outcomes were influenced by different personal and environmental factors. Thus, combining the findings reported here with those of our previous study [Citation20] provides an enhanced understanding of how strategies used to engage in social and leisure activities long-term after stroke are influenced by, for example, previous experiences, financial situation, social networks, knowledge and attitudes.
Not only behavioural strategies, but also how people mentally cope with changes in their lives emerged as a central component to participation. These findings are in line with previous research suggesting that people’s ability to accept their stroke-related problems and adapt their behaviour and attitude are central factors to social participation post stroke [Citation7,Citation21]. The mental strategies of accepting change or waiting for improvement can be seen as different ways to maintain a sense of comprehensibility. Comprehensibility is the extent to which events are perceived as making logical sense and is a central component of Antonovsky’s theory of sense of coherence (SOC) [Citation35]. According to this theory, a person with a strong SOC is more likely to believe that he or she can meet demands. SOC has also been suggested as a mediator between impairments and participation restrictions [Citation36]. Our findings indicate that a person who has a low confidence in his or her own ability after stroke may be more inclined to give up on previous activities. However, abandoning or replacing certain activities in favour of those that matter the most can also be an efficient strategy that promote participation and well-being. Thus, understanding the rationales behind each individual’s decisions, and their consequences, are key to providing the right type of support.
The mental strategy of waiting for improvement can also be understood through the findings of Wallenbert and Jonsson [Citation37] who revealed the inner conflict that can occur about whether or not to develop new daily habits after stroke. Although adaptation and change of activities would be beneficial for participation, it also represents giving up possible improvements and a sense of compromising future recovery and independence. This dilemma can lead to a state of waiting to get better or waiting for the situation to change. As a result, few new activities are established. This highlights the importance of supporting people with stroke towards positive emotional responses [Citation38]. In addition, rehabilitation professionals need to be aware of the coping strategies adopted by each patient in order to address relevant issues. That is, if a patient considers recovery of impairment as the only road towards participation, he or she will likely not be ready for suggestions of compensatory strategies.
Our participants chose to engage in activities that strengthened their self and avoided those that did not, suggesting that engagement in social and leisure activities can be part of a person’s struggle to maintain a positive or familiar identity after stroke. These findings relate to those of Charmaz [Citation39] who described how chronic illness disrupts the taken-for-granted notions about self, as well as the daily habits that support this self. As described by Charmaz, different activities and contexts are assigned certain qualities and symbolic values. Therefore, engaging in activities such as hiking, attending lectures, taking care of the grandchildren or managing the home could contribute to maintaining the image of oneself as a physically active, intellectual, caring or independent person. Moreover, by avoiding activities that could no longer be performed satisfactorily, our participants protected their pre-stroke identity. By accepting change and adopting new (or adapted) activities, they started to reconstruct their post-stroke self. Thus, an important task for rehabilitation professionals is to support people towards building a new and accepted identity after stroke. Considering that stroke recovery as well as accepting and adapting to a new situation is a long-term process [Citation40], individual needs will likely vary during different stages. Therefore, implementation of routine follow-ups over an extended period of time, with a possibility to address identified needs, is required.
We also found that the strategies used by the participants aimed to balance the expected costs and rewards of engagement in activities. As described in the cost-benefit model proposed in relation to participation in physical activities [Citation41], expected costs can comprise effort, time, unwanted outcomes, and missing out on other activities. Rewards or benefits can entail anticipated positive feelings and other gains achieved during or through the activity. Based on the cost-benefit model, motivation to perform a given activity will be high if the expected benefits outweighs the expected costs, but low if benefits and costs are of similar magnitude.
In addition, our findings revealed that whether or not an activity was prioritized depended on if it was perceived as meaningful. According to the ValMO-model [Citation42] the experience of meaning is related to the perceived value of activities. Concrete value may be a product, improved capacities and skills, or avoidance of negative consequences. Symbolic value is characterized by what an activity signifies for a person, for example strengthening his or her identity. Self-reward value comes from performing activities that are perceived as enjoyable in themselves. Among our participants, we found that both concrete and symbolic as well as self-reward values were direct or indirect reasons for engaging in certain activities. Accordingly, when helping patients to find new social and leisure activities, or new ways of performing them, it is crucial to understand the specific values and rewards that an activity or context provides for this person. To understand the perceived costs of engagement, the patient’s life situation as a whole as well as his or her own perceived capacity also needs to be taken into account.
It should be acknowledged that the strategies identified in this study may not be specific to people with stroke but could reflect the general processes of adaptation that people engage in throughout life. For example, it has been suggested that as physical function declines with age, older individuals turn to activities that are more sedentary, boosting participation in the cognitive/sedentary domain [Citation43]. According to the selective optimization with compensation theory [Citation44] certain strategies are used to maintain a higher level of functioning in the face of loss or decline. Selection means focusing attention on fewer, more important goals or rescaling/reconstructing goals. Optimization involves persistence, acquisition of new skills or resources and practice of skills. Compensation maintains a given level of functioning despite impairments for example through assistive devices and help from others. Several of the strategies used by our participants relate to those described. However, even though participation in leisure activities generally decreases with age [Citation45], the lower levels of community and leisure participation demonstrated among people with stroke compared to age-matched healthy people [Citation46,Citation47] indicate that they face grater challenges or have lower abilities to overcome them. Moreover, elderly stroke survivors may be particularly vulnerable to participation restrictions due to the combined effect of stroke and ageing [Citation48].
Based on the few existing long-term studies, participation in activities tend to increase during the first 12 months after a stroke and then remain relatively stable [Citation3,Citation16,Citation49], though at a lower level then pre-stroke [Citation18]. The studies that have explored the long-term adaptation process after stroke [Citation22,Citation40,Citation50] describes experiences of initial loss and disruption of the former self, struggles to reclaim activities and identity, and finding meaning through a new and changed life. The importance of supporting appropriate coping strategies throughout this long-term process has been stressed [Citation22]. Hence, additional support may be needed in later phases after stroke for survivors to regain full participation. In line with a recent study [Citation51] showing that many people with stroke perceive poor occupational balance, our findings indicate that stroke survivors with long-lasting impairments and fatigue may require guidance by occupational and physical therapists to achieve a sustainable balance between different areas of life, including engagement in social and leisure activities.
Methodological considerations
As this study aimed to explore processes and behaviours it was undertaken using a grounded theory approach [Citation26,Citation33]. According to Corbin and Strauss [Citation26], processes concern how people adapt to changes in their environment, and hence, relevant to understanding the strategies used after experiencing a stroke. In grounded theory, as in most qualitative research methods, the researcher strives for sensitivity (to what the data says) rather than objectivity, and the findings are considered an interpreted illustration of the studied reality, constructed through the researcher’s interaction with the participants and influenced by his/her perspective, previous knowledge and research tradition [Citation33]. To strengthen the validity of our analysis, the authors supported each other in remaining open to new ideas and emerging findings. The different clinical and research backgrounds of the authors, representing physiotherapy (AN), gerontology (SI), nursing (A-CJ), neurology (AL) and occupational therapy (EML, SI), contributed to an interdisciplinary and nuanced understanding of the findings. In line with the principles of grounded theory, we used a purposive and theoretical sampling procedure. As qualitative studies do not aim to be representative but rather strive for transferability, our sampling strategy aimed for variation in order to gain different perspectives and rich data. A notable strength of this study is that the participants were recruited from a population based cohort, including people with communicative difficulties and those living in residential care, that is, groups often excluded in stroke research. It is possible that if other participants had been interviewed, additional perspectives had been shared. Pilot interviews were performed to improve and develop the interview guide. Limitations include the retrospective data collection with potential risk of recall bias. Considering the cross sectional design of the present study, conclusions regarding how strategies change over time after stroke are limited. Thus, longitudinal prospective studies are needed to further understand how strategies develop in the long term after stroke.
Conclusions
Our findings indicate that although people have lived many years with the consequences of stroke, re-engagement in social and leisure activities is a long-term process that constantly has to be balanced against other priorities in life. To enable participation in valued social and leisure activities while also protecting and re-constructing the post-stroke self, people employ different strategies that balance the costs and rewards of engagement. These findings contribute to an improved understanding of why and how people manage to hold on to activities long term after experiencing a stroke as well as reasons for giving up activities and motivations for finding new ones. This knowledge can support more effective communication between healthcare professionals and patients so that interventions are grounded in and support the patients’ own goals and strategies during different stages of recovery and adaptation. It can also aid identification of those at high risk of long-term participation restrictions due to dysfunctional coping strategies. Importantly, our findings support the need for a long-term perspective on stroke rehabilitation that stretches beyond the first year, and the need for community-based support that specifically targets participation in valued social and leisure activities.
Acknowledgements
We would like to thank the participants that willingly shared their experiences with us.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990–2013: the GBD 2013 study. Neuroepidemiology. 2015;45(3):161–176.
- Adamson J, Beswick A, Ebrahim S. Is stroke the most common cause of disability? J Stroke Cerebrovasc Dis. 2004;13(4):171–177.
- Wolfe C, Crichton S, Heuschmann P, et al. Estimates of outcomes up to ten years after stroke: analysis from the prospective South London stroke register. PLoS Med. 2011;8(5):e1001033.
- Hole E, Stubbs B, Roskell C, et al. The patient’s experience of the psychosocial process that influences identity following stroke rehabilitation: a metaethnography. ScientificWorldJournal. 2014;2014:349151.
- Salter K, Hellings C, Foley N, et al. The experience of living with stroke: a qualitative meta-synthesis. J Rehabil Med. 2008;40(8):595–602.
- Northcott S, Moss B, Harrison K, et al. A systematic review of the impact of stroke on social support and social networks: associated factors and patterns of change. Clin Rehabil. 2016;30(8):811–831.
- Woodman P, Riazi A, Pereira C, et al. Social participation post stroke: a meta-ethnographic review of the experiences and views of community-dwelling stroke survivors. Disabil Rehabil. 2014;36(24):2031–2043.
- Sveen U, Thommessen B, Bautz-Holter E, et al. Well-being and instrumental activities of daily living after stroke. Clin Rehabil. 2004;18(3):267–274.
- Boosman H, Schepers VP, Post MW, et al. Social activity contributes independently to life satisfaction three years post stroke. Clin Rehabil. 2011;25(5):460–467.
- Tse T, Douglas J, Lentin P, et al. Reduction in retained activity participation is associated with depressive symptoms 3 months after mild stroke: An observational cohort study. J Rehabil Med. 2017;49(2):120–127.
- Venna V, McCullough L. Role of social factors on cell death, cerebral plasticity and recovery after stroke. Metab Brain Dis. 2015;30(2):497–506.
- Otto CM. Heartbeat: social isolation is associated with increased mortality after acute myocardial infarction or stroke. Heart. 2018;104(18):1471–1473.
- Son JS, Janke MC. Contributions of leisure-based selective optimization with compensation and leisure activity expenditure to the health of adults with arthritis. J Leis Res. 2015;47(1):34–57.
- Chang PJ, Wray L, Lin Y. Social relationships, leisure activity, and health in older adults. Health Psychol. 2014;33(6):516–523.
- Teasdale TW, Engberg AW. Psychosocial consequences of stroke: a long-term population-based follow-up. Brain Inj. 2005;19(12):1049–1058.
- Jansen HE, Schepers VP, Visser-Meily JM, et al. Social activity one and three years post-stroke. J Rehabil Med. 2012;44(1):47–50.
- Norlander A, Jönsson AC, Ståhl A, et al. Activity among long-term stroke survivors. A study based on an ICF-oriented analysis of two established ADL and social activity instruments. Disabil Rehabil. 2016;38(20):2028–2037.
- Singam A, Ytterberg C, Tham K, et al. Participation in complex and social everyday activities six years after stroke: predictors for return to pre-stroke level. PLoS One. 2015;10(12):e0144344.
- Norlander A, Carlstedt E, Jönsson AC, et al. Long-term predictors of social and leisure activity 10 years after stroke. PLoS One. 2016;11(2):e0149395.
- Norlander A, Iwarsson S, Jönsson AC, et al. Living and ageing with stroke: an exploration of conditions influencing participation in social and leisure activities over 15 years. Brain Inj. 2018;32(7):858–866.
- Walsh ME, Galvin R, Loughnane C, et al. Factors associated with community reintegration in the first year after stroke: a qualitative meta-synthesis. Disabil Rehabil. 2015;37(18):1599–1608.
- Williams S, Murray C. The lived experience of older adults’ occupational adaptation following a stroke. Aust Occup Ther J. 2013;60(1):39–47.
- Alaszewski A, Alaszewski H, Potter J. The bereavement model, stroke and rehabilitation: a critical analysis of the use of a psychological model in professional practice. Disabil Rehabil. 2004;26(18):1067–1078.
- Blalock SJ, DeVellis BM, Holt K, et al. Coping with rheumatoid arthritis: is one problem the same as another? Health Educ Q. 1993;20(1):119–132.
- Audulv A, Packer T, Hutchinson S, et al. Coping, adapting or self-managing - what is the difference? A concept review based on the neurological literature. J Adv Nurs. 2016;72(11):2629–2643.
- Corbin JM, Strauss AL. Basics of qualitative research: techniques and procedures for developing grounded theory. 4th ed. Los Angeles: SAGE Publications; 2015.
- Hallström B, Jönsson AC, Nerbrand C, et al. Lund Stroke Register: hospitalization pattern and yield of different screening methods for first-ever stroke. Acta Neurol Scand. 2007;115(1):49–54.
- Patton MQ. Purposeful sampling and case selection: overview of strategies and options. In: Patton MQ, editor. Qualitative research & evaluation methods: integrating theory and practice. 4th ed. Thousand Oaks (CA): SAGE Publications; 2015. p. 264–272.
- Wityk R, Pessin M, Kaplan R, et al. Serial assessment of acute stroke using the NIH Stroke Scale. Stroke. 1994;25(2):362–365.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198.
- van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–607.
- Bazeley P, Jackson K. Qualitative data analysis with NVivo. 2nd ed. London: SAGE Publications; 2013.
- Charmaz K. Constructing grounded theory. 2nd ed. Thousand Oaks (CA): SAGE Publications; 2014.
- Häggstrom A, Lund ML. The complexity of participation in daily life: a qualitative study of the experiences of persons with acquired brain injury. J Rehabil Med. 2008;40(2):89–95.
- Antonovsky A. Health, stress, and coping. San Francisco (CA): Jossey-Bass; 1979.
- Schnyder U, Buchi S, Morgeli H, et al. Sense of coherence - a mediator between disability and handicap? Psychother Psychosom. 1999;68(2):102–110.
- Wallenbert I, Jonsson H. Waiting to get better: a dilemma regarding habits in daily occupations after stroke. Am J Occup Ther. 2005;59(2):218–224.
- Ellis-Hill C, Payne S, Ward C. Using stroke to explore the life thread model: an alternative approach to understanding rehabilitation following an acquired disability. Disabil Rehabil. 2008;30(2):150–159.
- Charmaz K. The self as habit: the reconstruction of self in chronic illness. OTJR Occup Participation Health. 2002;22:31–41.
- Arntzen C, Borg T, Hamran T. Long-term recovery trajectory after stroke: an ongoing negotiation between body, participation and self. Disabil Rehabil. 2015;37(18):1626–1634.
- Studer B, Knecht S. A benefit-cost framework of motivation for a specific activity. Prog Brain Res. 2016;229:25–47.
- Erlandsson LK, Eklund M, Persson D. Occupational value and relationships to meaning and health: elaborations of the ValMO-model. Scand J Occup Ther. 2011;18(1):72–80.
- Finkel D, Andel R, Pedersen NL. Gender differences in longitudinal trajectories of change in physical, social, and cognitive/sedentary leisure activities. J Gerontol B Psychol Sci Soc Sci. 2018; 73(8):1491–1500.
- Baltes PB, Baltes BM. Psychological perspectivers on successful aging: the model of selective optimization with compensation. In: Baltes PB, Baltes BM, editor. Successful aging: perspectives from the behavioural sciences. Cambridge: Cambridge University Press; 1990. p. 1–34.
- Agahi N, Ahacic K, Parker MG. Continuity of leisure participation from middle age to old age. J Gerontol B Psychol Sci Soc Sci. 2006;61(6):340–346.
- Desrosiers J, Bourbonnais D, Noreau L, et al. Participation after stroke compared to normal aging. J Rehabil Med. 2005;37(6):353–357.
- Skolarus LE, Burke JF, Brown DL, et al. Understanding stroke survivorship: expanding the concept of poststroke disability. Stroke. 2014;45(1):224–230.
- de Graaf JA, van Mierlo ML, Post MWM, et al. Long-term restrictions in participation in stroke survivors under and over 70 years of age. Disabil Rehabil. 2018;40(6):637–645.
- Engel-Yeger B, Tse T, Josman N, et al. Scoping review: the trajectory of recovery of participation outcomes following stroke. Behav Neurol. 2018; 2018:5472018–5472022.
- Erikson A, Karlsson G, Tham K. Living with the long-term consequences 11–13 years after stroke: a phenomenological study. J Rehabil Med. 2016;48(10):847–852.
- Kassberg AC, Nyman A, Larsson Lund M. Perceived occupational balance in people with stroke. Disabil Rehabil. 2021;43(4):553–558.
