?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
To evaluate the effects of a combination of wheelchair mobility skills (WMS) training and exercise training on physical activity (PA), WMS, confidence in wheelchair mobility, and physical fitness.
Methods
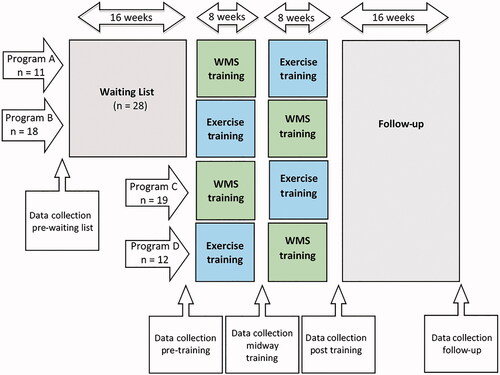
Youth using a manual wheelchair (n = 60) participated in this practice-based intervention, with a waiting list period (16 weeks), exercise training (8 weeks), WMS training (8 weeks), and follow-up (16 weeks). Repeated measures included: PA (Activ8), WMS (Utrecht Pediatric Wheelchair Mobility Skills Test), confidence in wheelchair mobility (Wheelchair Mobility Confidence Scale), and physical fitness (cardiorespiratory fitness, (an)aerobic performance) and were analysed per outcome parameter using a multilevel model analyses. Differences between the waiting list and training period were determined with an unpaired sample t-test.
Results
Multilevel model analysis showed significant positive effects for PA (p = 0.01), WMS (p < 0.001), confidence in wheelchair mobility (p < 0.001), aerobic (p < 0.001), and anaerobic performance (p < 0.001). Unpaired sample t-tests underscored these effects for PA (p < 0.01) and WMS (p < 0.001). There were no effects on cardiorespiratory fitness. The order of training (exercise before WMS) had a significant effect on confidence in wheelchair mobility.
Conclusions
A combination of exercise and WMS training appears to have significant positive long-term effects on PA, WMS, confidence in wheelchair mobility, and (an)aerobic performance in youth using a manual wheelchair.
Exercise training and wheelchair mobility skills (WMS) training can lead to a sustained improvement in physical activity (PA) in youth using a manual wheelchair.
These combined trainings can also lead to a sustained increase in WMS, confidence in wheelchair mobility, and (an)aerobic performance.
More attention is needed in clinical practice and in research towards improving PA in youth using a manual wheelchair.
Implications for rehabilitation
Introduction
Youth with or without a disability benefit physically and mentally from a physical active lifestyle [Citation1,Citation2]. It has been shown that low levels of physical activity (PA) are more prevalent among youth (children and adolescents) with a physical disability compared to their typically developing peers [Citation3,Citation4]. Youth using a manual wheelchair are markedly less physically active than their ambulatory peers with or without a physical disability [Citation5–8]. Bloemen et al. [Citation5] found that youth using a manual wheelchair with spina bifida were 2.5 times less physically active than typically developing peers. These low levels of PA in youth using a wheelchair are worrisome and need attention.
Evidence for the effectiveness of interventions aimed at increasing PA in youth using a manual wheelchair is lacking, as there has been very limited research undertaken in this population [Citation9]. Most intervention studies in youth with a physical disability focused on increasing PA in youth with cerebral palsy and were limited to participants who were able to stand or walk [Citation8–11]. Recent systematic reviews [Citation10,Citation11] in youth with a physical disability concluded there was no or conflicting evidence on effectiveness of interventions aimed at increasing PA.
In this study, we were interested in increasing the wheelchair propulsion time in youth using a manual wheelchair, as wheelchair propulsion is the largest component of PA in wheelchair users. We aimed to increase wheelchair propulsion time through improving three modifiable determinants of PA: wheelchair mobility skills (WMS), confidence in wheelchair mobility, and physical fitness [Citation12–14]. Two studies in children with a disability [Citation15,Citation16] showed high-intensity interval training (HIIT) to have positive results on physical fitness. High intensity interval training consists of intermittent bouts of activity and rest, which is similar to the active behaviour of youth [Citation17]. Current literature in adult wheelchair users [Citation18,Citation19] shows that WMS and confidence in wheelchair mobility and physical fitness are modifiable factors, either through exercise training (physical fitness) [Citation18] or WMS-training (WMS and confidence in wheelchair mobility) [Citation19]. These studies have focused on the effect of one type of training, i.e., WMS training or exercise training, on respectively WMS and confidence in wheelchair mobility or physical fitness. Recently, Kirby et al. [Citation20] suggested to focus on both WMS-training and exercise training during rehabilitation of people with a spinal cord injury, as there are significant positive relationships between WMS, confidence in wheelchair mobility, and physical fitness. Whether the relationships and benefits of these training programs in adults are similar in youth using a manual wheelchair is unclear as there is barely any research in this population for WMS-training [Citation21] and exercise training [Citation9]. Moreover, and to the best of our knowledge, the effect of a combination of WMS-training and exercise training on PA is unknown in adults and youth using a manual wheelchair.
Therefore, the aim of this study was to: (1) study both the short-term and long-term effects of a combined WMS-training and exercise training on PA and modifiable determinants of PA, including WMS, confidence in wheelchair mobility, and physical fitness in youth using a manual wheelchair and (2) explore differences in outcomes based on the order of training, i.e., WMS-training before or after exercise training.
Methods
Participants
In this practice based study, a convenience sample of participants was recruited at six rehabilitation centres/schools for special education in the Netherlands. Participants were included if they were: between 7 and 18 years of age, bimanually propel their wheelchair, use wheelchair on a daily basis, able to understand the spoken Dutch language, able to understand simple instructions and had a problem related to WMS, physical fitness, and/or PA. Participants were excluded if they had undergone a medical intervention during the previous six months that could have affected the intervention study outcomes (e.g., botox-injections). Local physiotherapists (PT), occupational therapists (OT), or physical education (PE) teachers approached and informed suitable participants and their parents.
Procedure
This intervention study is part of the Let’s Ride study from the Fit-for-the-Future consortium and registered at trialregister.nl, registration number NTR5791. The Institutional Review Board of the University Medical Center Utrecht approved the study protocol for the Let’s Ride intervention study (protocol number 15-136). Participants aged 12 years and over and all parents signed the informed consent form before enrolment in this study. Participants were placed in peer groups of 4–7 participants per rehabilitation centre or school. Groups were allocated to one of the four programs in this study (). Program A and B were placed on the 16-week waiting list after the first assessment. This group was created due to limited facilities of running multiple groups simultaneously in a rehabilitation centre or school. Program C and D started training after the first assessment. All participants followed 8-weeks WMS training followed by 8-weeks exercise training (program A and C) or 8-weeks exercise training followed by 8-weeks WMS training (program B and D).Training programs were carried out during the school year and were not interrupted by school holidays that lasted more than one week. The group training sessions were given twice per week by two or three local PT, OT, or PE teachers and each session lasted 30 min. The presence of the participant was documented in every session and participants were included in the analysis of the training results if they attended ≥10 sessions of WMS-training and ≥10 sessions of exercise training.
All participants had four assessments: pre-training, midway-training, post-training, and follow-up. Participants in program A and B had one extra assessment before the waiting list period. All tests during an assessment period were administered within a two-week time frame at the participant’s rehabilitation centre/school for special education in the gymnasium or laboratory under similar conditions (e.g., optimal tire pressure and floor).
Intervention
WMS training
The WMS-training program was developed by “KJ Projects”, a WMS school with over 10 years of experience in teaching WMS to both children and adults [Citation22]. WMS sessions were aimed at learning to propel efficiently, going up, and down curbs, holding a wheelie and negotiating the physical environment outdoors. Before starting the training sessions, the PT, OT, and PE teachers received a three hour training by the research team and KJ Projects. In combination with the two weekly training sessions by local PT, OT, or PE teachers, there were three training sessions at the start, in the middle and at the end of the WMS-training program given by KJ projects. Parents and/or close relatives observed and participated in these three training sessions to stimulate and motivate the participants to practice at home. In addition, all participants received an individual video instruction on how to practice their skills at home.
Exercise training
A HIIT protocol was chosen as a form of exercise training, as this form of training is a time-effective method of improving physical fitness in youth [Citation23]. This training protocol has recently been used in a study with children with a disability, including a small sample of wheelchair users [Citation15]. Results showed a significant improvement in anaerobic performance and aerobic performance after HIIT training [Citation15]. The used HIIT protocol in our study, number of series (8–12 series) and active recovery time (90–120 s), is described by Zwinkels et al. [Citation15] for children with a disability. All participants performed a HIIT in their own wheelchair, aimed at improving their physical fitness (aerobic performance, cardiorespiratory fitness, and anaerobic performance) through series of 30-s all-out exercises. The 30-s all out exercises were easily executable sprint exercises such as, go back and forward between two cones. The group training sessions were given in the school’s gym by two or three PT, OT, or PE teachers, who had received a training on the intervention by the research team.
Demographic and morphologic parameters
Parents of the participant completed one general questionnaire at the first assessment regarding age, diagnosis, functional mobility level [Citation24], type of wheelchair, and level of education of their child. They also completed a short questionnaire at the other assessments about possible factors that could influence the participants performance (e.g., illness or injuries). At each assessment, body mass and wheelchair mass was determined using a calibrated (wheelchair) scales (Kern MWS 300K100M) from the local rehabilitation centre/school for special education. Height was assessed in supine position with an non-stretchable tape from head to heel or with arm span (fingertip to fingertip, with arms abducted 90°and elbow and wrists straight) when participants were unable to fully extent their hips or knees due to contractures [Citation25].
Outcome measures
Physical activity: active wheelchair use
An objective assessment of time spent in “active wheelchair use” was measured with a small accelerometer, the Activ8 activity monitor (2M Engineering BV, Valkenswaard, The Netherlands) [Citation26]. The Activ8 has shown to be valid for distinguishing the classification “active wheelchair use” from the classification “non-propulsive wheelchair use” [Citation27]. The counts thresholds used to separate active from non-propulsive wheelchair use were modified for youth using a manual wheelchair based on earlier pilot data. For the purpose of this study, active wheelchair use is defined as independent wheelchair propulsion at normal speed, high speed, or manoeuvring. Participants were asked to wear an Activ8 in a stretchable wristband on the dorsal side of the wrist on their dominant arm for seven consecutive days. A second Activ8 was securely fastened as close as possible to the axle of the wheel on the same side as the dominant arm. The use of this combination of accelerometers makes it possible to distinguish active propulsion from assisted driving. The total amount of PA consists of more than active wheelchair use, including activities such as swimming and transfers in/out of wheelchair. However, the aim of this intervention is to increase the active propulsion of the everyday wheelchair and the Activ8 is a valid device for detecting this component of PA [Citation27]. Only data of participants with a minimal wear time of eight hours/day on at least two school-days and one weekend-day were analysed [Citation6]. The main outcome for PA is the amount of “active wheelchair use” expressed as a percentage of wear time per day.
Wheelchair mobility skills
The WMS were assessed using the recently developed Utrecht Pediatric Wheelchair Mobility Skills Test 2.0 (UP-WMST 2.0) [Citation28,Citation29]. The UP-WMST 2.0 is a performance-based measure of WMS with good validity and test–retest reliability [Citation28]. It consists of 15 items measuring different WMS such as propelling forwards/backwards, turning, ascending a platform, and holding a wheelie. The UP-WMST 2.0 was administered by a PT, OT, or PE teacher, who had received a two hour training (theory and practice) on how to administer the UP-WMST 2.0 in youth using a manual wheelchair. The main outcome is a total score ranging from 0 to 51, with a higher score representing more advanced WMS.
Confidence in wheelchair mobility
For confidence in wheelchair mobility, the recently developed and validated Wheelchair Mobility Confidence Scale (WheelCon-Mobility) for Dutch Youth was used [Citation30]. In this questionnaire, participants are asked to rate on a five-point Likert scale how confident they feel about doing different wheelchair mobility activities independently and safely, such as manoeuvring your wheelchair in small spaces or going up and down a curb. Participants were asked to complete the questionnaire independently or with the help of a research team member when they were unable to read the questions themselves. The main outcome of this 31-item questionnaire is a total score ranging from 31 to 155, with a higher score indicating a higher confidence in wheelchair mobility.
Physical fitness
Aerobic fitness
The Shuttle Ride Test (SRiT) is a maximal graded aerobic exercise field test where participants propel their wheelchair back and forth over a distance of 10 m with increasing speed. This test has shown to be reliable and valid in youth (cerebral palsy, spina bifida, and osteogenesis imperfecta) using a manual wheelchair [Citation31–33]. The SRiT was administered by two experienced researchers following the protocol of Verschuren et al. [Citation32]. The VO2 (ml/min) during the SRiT was recorded with a calibrated mobile gas analysis system (Cortex Metamax B3; Cortex Medical GmbH, Leipzig, Germany). The relative VO2peak (ml/min/kg) was determined as the highest value of VO2 (ml/min) during the last 30 s of the SRT, divided by the body mass (kg). The researcher used subjective criteria (lack of motivation, pain, distraction) to determine if the participant had shown real maximal effort to achieve the highest number of shuttles. The main outcome of the SRiT is the number of shuttles (ranging from 0.5 to 23) as a measure of aerobic performance and the relative VO2peak (ml/min/kg) as a measure of cardiorespiratory fitness. Data were excluded from analysis for “number of shuttles” and “relative VO2peak” when maximal effort was not achieved.
Anaerobic performance
The Muscle Power Sprint Test (MPST) is an anaerobic performance test in youth using a manual wheelchair, where participants propel their wheelchair six times at maximal speed over a distance of 15 m with a break of 10 s between each sprint to turn around and get ready for the next sprint. This test has shown to be reliable and valid in youth using a manual wheelchair [Citation34,Citation35]. The MPST was administered by a member of the research team who recorded the time per sprint. Afterwards, the time per sprint was converted to power as a measure of anaerobic performance.
Total mass is calculated as body mass plus wheelchair mass. Participants with power assisted wheels (Ewheels) were excluded from analysis. The main outcome of the MPST is the mean and peak power of the six sprints.
Data analyses
Statistical analysis was performed using SPSS for Windows (version 25.0, SPSS Inc., Chicago, IL). Characteristics of the participants, such as gender, diagnosis, and functional mobility level are described categorically and the participants age, height, weight, and years of experience in wheelchair use are presented as a mean with the standard deviation (SD) for the total group (program A–D), waiting list group (program A and B), and split for order of training (program A, C or program B, D). Data were checked for normality and characteristics and baseline scores were compared between the waiting list group (program A and B) and total group (program A–D) and between the orders of training (program A, C or program B, D) using chi-square test or independent sample t-tests.
Aim (1): the short-term and long-term effect of combined WMS and exercise training per outcome parameter was calculated using a multilevel model analyses with a random intercept for participant and time (pre-training, post-training, and follow-up) as a categorical factor. The pre-waiting list assessment was not added as a time value in the model, as we did not expect different outcomes for participants who were placed on the waiting list before commencing the combined training program. As a secondary analysis, we performed unpaired sample t-tests for all outcome measures to determine if the change in outcomes after the training period (post-training minus pre-training of program A and program D) was significantly different from the normal variation in outcomes during the waiting list period (pre-training minus pre-waiting list of program A and B). Due to the heterogeneity of this population, analysis in the total sample using an unpaired sample t-test (program A–D) was the preferred method over a paired t-test in a half of the sample (program A and B). Due to the use of multiple testing, we have set the significance level at p < 0.01 to prevent type-I errors. Cohen’s D effect size was calculated for the unpaired sample t-tests with effect sizes classified as small (d= 0.2), medium (d= 0.5), large (d= 0.8), and very large (d= 1.3) [Citation36].
Aim (2): the order of training (WMS training before or after exercise training) was added to the multilevel model analyses per outcome parameter to determine if program A and C had a significant different effect from program B and D.
Results
A total of 60 youth using a manual wheelchair in daily life participated in this study. For the effectiveness of the intervention, data of 12 participants were discarded. They could either not continue training due to unrelated medical problems (n = 3), left school during the training period (n = 1), declined to participate (n = 2), or did not attend ≥10 trainings sessions per type of training (n = 6). From the remaining group of 48 participants, the mean adherence for exercise training was 14.2 (SD 1.6) out of the 16 training sessions and the mean adherence for WMS training was 14.3 (SD 1.7) out of the 16 training sessions. The characteristics of the total group (program A–D) are described in and subsequently split for waiting list group (program A and B), WMS before exercise training (program A and C), and exercise before WMS training (program B and D). There were no significant differences in characteristics or baseline scores between the waiting list group and total group (, ). There were no significant differences in characteristics or pre-training scores between the orders of training, except for more years of experience in wheelchair use in program A and C compared to program B and D ().
Figure 2. Line graph of the change in mean score over time for the total group, program A and C, and program B and D per outcome parameter. *Significant difference in outcome for order of training. UP-WMST: Utrecht Pediatric Wheelchair Mobility Skills Test; SRiT: Shuttle Ride Test; MPST: Muscle Power Sprint Test.
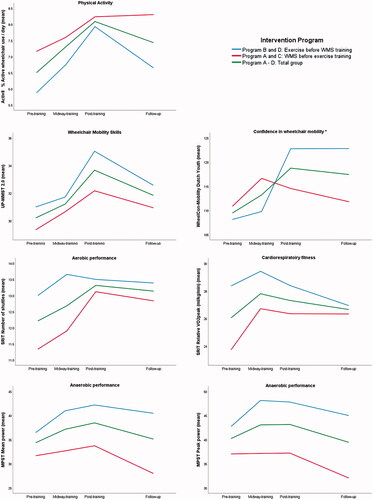
Table 1. Characteristics of participants.
Effects of combined WMS-training and exercise training on PA
The median amount of days with sufficient wear time of the Activ8 for pre-training, post-training, and follow-up are respectively: 6 days, 7 days, and 6 days. Missing data per measurement instrument are reported in Appendix A. No significant differences were found for baseline characteristics of participants with missing data of the Activ8 at pre-training, post-training, and follow-up, except for gender at pre-training (Appendix A).
For the total group, the combined intervention of WMS and exercise training had a significant positive effect (p = 0.01) on PA as measured with the Activ8 (pre-training 6.5% (standard error (SE) 2.4), post-training 8.1% (SE 3.2), and follow-up 7.5% (SE 2.5)) (). Post hoc analysis showed that the short-term effect was an absolute average increase from 53 min/day before training to 66 min/day after the combined training. Looking at the follow up data, there was a sustained improvement with no significant (p = 0.73, 95% CI [–0.7, 1.1]) differences at follow-up in “active wheelchair use” per day.
Table 2. Short- and long-term effects per outcome parameter of combined exercise and wheelchair mobility skills training using a multilevel model analyses.
Unpaired sample t-test (see ) showed a large effect (d= 1.2), with an increase in “active wheelchair use” of 1.1% (SD 2.1%) (n = 21) after the training period that was significantly different (p < 0.01) from the decline of 1.1 (SD 1.2%) that occurred during the waiting list period (n = 14).
Table 3. Unpaired sample t-test total group and waiting list group.
Effects of combined WMS-training and exercise training on determinants of PA
The WMS, confidence in wheelchair mobility, and physical fitness, with the exception of relative VO2peak, improved significantly over time (pre-training, post-training, and follow-up) in the total group (, ). Missing data per assessment and parameter are reported in Appendix A.
When looking at differences in change with the unpaired sample t-test during the training period compared to the waiting list period, there was a significant change of 3.5 (SD 3.6) points in WMS after the training period compared to a change of 0.3 (SD 3.7) after the waiting list period. We found a non-significant difference between the waiting list period and training period for confidence in wheelchair mobility (p = 0.03), number of shuttles (p = 0.07), relative VO2peak (p = 0.03), mean power (p = 0.37), and peak power (p = 0.62).
Effect of the order of WMS and exercise training
We found a significant effect of order of training when added to the multilevel model for confidence in wheelchair mobility (p = 0.01) (). We found no significant effect of order of the training for all the other outcomes.
Discussion
The aim of this intervention in youth using a manual wheelchair was to evaluate the short-term and long-term effect of a combined WMS-training and exercise training on PA and three determinants of PA: WMS, confidence in wheelchair mobility, and physical fitness. In this study, we found increasing levels of PA and positive changes in determinants of PA after the combined training program, which were maintained at follow-up, with the exception of cardiorespiratory fitness.
Despite the heterogeneity of the participants in this practice based intervention study, positive results in increased PA over time are supported by a significant difference, with a large effect size, in change of PA during the training period compared to the waiting list period. The increase of 13 min per day is a relative increase of 25% in time spent physically active per day. This is an important and clinically relevant increase, as any improvement of PA can lead to numerous health benefits [Citation1]. Moreover, greater health benefits can be achieved by people who have an inactive lifestyle [Citation1]. The results of this study also show that youth using a manual wheelchair are very inactive with 53 min/day of active wheelchair use before commencing the combined training programs.
For the assessment of PA, we were able to assess the largest component of PA for wheelchair users, which is the percentage of time spent actively propelling their manual wheelchair per day. While it would be preferable to assess the total amount of PA, at the start of this study in 2015, the Activ8 was the best available activity monitor for wheelchair users, which did appear to be user friendly [Citation27]. In this study, we did experience some technological challenges in the use of the Activ8. Even though the soft stretchable armband did appear to be child friendly, participants reported more and more a dislike to wear the armband due to an itchy feeling or esthetical reasons. This led to decreased willingness to wear to monitor for multiple days and resulted in more missing data of the Activ8 in the final assessments, i.e., post-training and follow-up. Consequently, the results reported for PA are collected in a smaller sample. Even with this small heterogeneous sample, significant sustainable changes were seen after the 16 week combined training program.
When looking at the determinants of PA, we aimed to improve three determinants through a combined WMS-training and exercise training. We found a significant improvement in WMS of 7.1% (3.5 points) on the UP-WMST 2.0, which was maintained at follow-up. This improvement in WMS is smaller than the effects of WMS training in adults (14.0%, 95% CI [7.4, 20.8]) [Citation19]. Subgroup analysis in the meta-analysis of Keeler et al. [Citation19] showed that training was more effective in new wheelchair users. Youth using a manual wheelchair in this study had an average of 8 years of experience in using a wheelchair, which could explain the smaller effects on WMS. Nonetheless, small improvements in WMS, such as being able to go up a curb (+1 point), could already lead to more independence outdoors and have a positive effect on PA. More importantly, there is no significant decline in training effects between post-training and at 16-weeks of follow-up as is similar in adult wheelchair users [Citation19], which implies WMS were maintained during the follow up period.
For confidence in wheelchair mobility, we found a significant increase in the WheelCon-Mobility for Dutch Youth [Citation30] after the combined training. The growth in confidence levels was mainly gained after WMS training (), with a significantly larger increase in the group that started with exercise training (program B and D). This could be explained by Bandura et al.’s social cognitive theory [Citation37], were the experience of mastering of a new skill, i.e., WMS, is the most effective way of improving ones confidence. Participants in program B and D mastered on average more WMS skills, possibly leading to a bigger increase in confidence compared to participants in program A and C. These results suggest that exercise before WMS training might be the preferred order of training when aiming to improve confidence in wheelchair mobility.
The short-term effect of the combined training on anaerobic performance was a significant increase in mean (+4.1 W) and peak power (+3.0 W). In the longer term, we found a non-significant decline between post-training and follow-up, which was especially prominent in program A and C. This trend for a decline could be explained by one of the limitations of this study, where we were unable to assess participants who had graduated from school (n = 4) and left the program between post-training and follow-up. This led to missing data not at random, but with missing data of older and heavier participants, leaving younger and therefore lighter participants at follow-up assessment. For the power calculations in the MPST, the total weight of the participant is an important factor for the outcome. The four participants who had left school all had a mean power at post-training that was two to four times higher than the average mean power of the total group. Secondary analyses without these four participants showed a smaller decline in anaerobic performance at follow-up.
For aerobic fitness, we found similar positive results as Zwinkels et al. [Citation15], with a significant increase of shuttles on the SRiT (+1 shuttle) as a measure of aerobic performance and no change in relative VO2peak as a measure of cardiorespiratory fitness. Surprisingly, we did find a non-significant positive effect on relative VO2peak after the waiting list period. It is unclear what caused these results during the waiting list period. Possibly, there were seasonal effects (pre-waiting list measurement was assessed at the start of school year) that might have influenced the cardiorespiratory fitness during the waiting list period. For the results of the combined training, we found an increase in shuttles with similar O2 uptake, which implies more efficient propulsion after the combined training and at follow-up. These results are in line with a functional exercise study in ambulatory children with spina bifida [Citation38]. The increase in efficiency may be explained by the fact that the training intensity was limited by the propelling capacities of the child rather than the cardiorespiratory limitation. Recently, Zwinkels et al. [Citation15] also concluded that the HIIT training protocol used is not an effective form of exercise training to increase cardiorespiratory fitness in youth who use a wheelchair. It is possible that reaching high intensities in 30 s exercise bouts is less attainable through wheelchair propulsion due smaller active muscle mass than running based exercises [Citation39].
One of the limitations of this study was the “one size fits all” training approach, where all participants received a WMS-training and exercise training, regardless of the large variation at baseline in PA and the determinants of PA. In , the changes in scores over time are visually presented per order of training, and show that the greatest improvement for PA, confidence in wheelchair mobility, and aerobic performance are in the groups that had lower scores at pre-training. It is possible that participants with a relatively high physical fitness or more advanced WMS did not benefit from the exercise or WMS-training as much as the participants with a relatively low physical fitness or more basic WMS. At the same time, HIIT training did challenge each child to exercise at his/her own maximal level during the high intensity intervals. The small training groups with peers seemed motivating to go as fast as possible during exercise training and encouraging to learn new WMS from seeing their peers mastering a new skill.
While the obvious strength of this study was the practice-based approach, with outcomes measures that can be applied in clinical practise and a heterogeneous sample that is representative for this population, this type of study does come with methodological imitations. The heterogeneity of the sample makes it more difficult to show significant results due to the large confidence intervals. Even so, this study showed positive results which are immediately relevant for daily practice in schools for special education or rehabilitation centres. The intervention in a school setting has disadvantages, such as limited time for assessments and drop-outs due to graduation, which leads to missing data that potentially could have confounded the results of this study. Future research towards PA in school settings should also take into account possible seasonal variations due to the school program, e.g., decreased or increased PA over the summer holidays. A benefit of the practice-based design was the involvement of PT, OT, and PE teachers in assessments and interventions. This will help future implementation of study results, which has already happened in the rehabilitation centres in the Netherlands that were involved in this study.
Conclusions
A combination of exercise and WMS training appears to have a clinically relevant and significant increase in PA in youth using a manual wheelchair. The combined training also had a positive effect on WMS, confidence in wheelchair mobility, aerobic performance, and anaerobic performance. More insight is needed towards finding an effective form of exercise training for improving cardiorespiratory fitness in youth using a manual wheelchair. Exercise before WMS training is the preferred order of training, when aiming to improve confidence in wheelchair mobility.
Acknowledgements
This study is part of the Fit For the Future collaboration; H. Wittink, A. Dallmeijer, R van den Berg-Emons. We would like to thank all children, adolescents, and their parents for participation in this study. We are especially grateful to all the participating health care professionals of Rehabilitation centre: Heliomare, De Trappenberg, De Hoogstraat, Blixembosch and Roessingh and School for special education Roosendaal for organising and administering the training sessions with us. We would also like to thank KJ-Projects for sharing their expertise in training wheelchair mobility skills with us and all the participating children, parents, and health care professionals. We would like to thank Phelie Maguire for the proof reading of this manuscript and finally we would like to thank all the participating students who have enthusiastically contributed to the data collection and analysis in the Let’s ride study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Weggemans RM, Backx FJG, Borghouts L, et al. The 2017 Dutch physical activity guidelines. Int J Behav Nutr Phys Act. 2018;15(1):58.
- Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809.
- Rimmer JA, Rowland JL. Physical activity for youth with disabilities: a critical need in an underserved population. Dev Neurorehabil. 2008;11(2):141–148.
- Burghard M, de Jong NB, Vlieger S, et al. 2017 Dutch Report Card+: results from the first physical activity report card plus for Dutch youth with a chronic disease or disability. Front Pediatr. 2018;6:122.
- Bloemen MAT, van den Berg-Emons RJG, Tuijt M, et al. Physical activity in wheelchair-using youth with spina bifida: an observational study. J Neuroeng Rehabil. 2019;16(1):9.
- Claridge EA, Bloemen MAT, Rook RA, et al. Physical activity and sedentary behaviour in children with spina bifida. Dev Med Child Neurol. 2019;61(12):1400–1407.
- Van Den Berg-Emons RJ, Bussmann JB, Stam HJ. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil. 2010;91(12):1856–1861.
- Ganz F, Hammam N, Pritchard L. Sedentary behavior and children with physical disabilities: a scoping review. Disabil Rehabil. 2020. DOI:10.1080/09638288.2020.1723720
- O'Brien TD, Noyes J, Spencer LH, et al. Systematic review of physical activity and exercise interventions to improve health, fitness and well-being of children and young people who use wheelchairs. BMJ Open Sport Exerc Med. 2016;2(1):e000109.
- Bloemen M, Van Wely L, Mollema J, et al. Evidence for increasing physical activity in children with physical disabilities: a systematic review. Dev Med Child Neurol. 2017;59(10):1004–1010.
- Reedman S, Boyd RN, Sakzewski L. The efficacy of interventions to increase physical activity participation of children with cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2017;59(10):1011–1018.
- Van Der Ploeg HP, Van Der Beek AJ, Van Der Woude LHV, et al. Physical activity for people with a disability: a conceptual model. Sports Med. 2004;34(10):639–649.
- Bloemen MAT, Verschuren O, van Mechelen C, et al. Personal and environmental factors to consider when aiming to improve participation in physical activity in children with Spina Bifida: a qualitative study. BMC Neurol. 2015;15(1):11.
- Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC Pediatr. 2016;16(1):9.
- Zwinkels M, Verschuren O, de Groot JF, et al. Effects of high-intensity interval training on fitness and health in youth with physical disabilities. Pediatr Phys Ther. 2019;31(1):84–93.
- Lauglo R, Vik T, Lamvik T, et al. High-intensity interval training to improve fitness in children with cerebral palsy. BMJ Open Sport Exerc Med. 2016;2(1):e000111.
- Bailey RC, Olson J, Pepper SL, et al. The level and tempo of children’s physical activities: an observational study. Med Sci Sports Exerc. 1995;27(7):1033–1041.
- Hicks AL, Martin Ginis KA, Pelletier CA, et al. The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord. 2011;49(11):1103–1127.
- Keeler L, Kirby RL, Parker K, et al. Effectiveness of the Wheelchair Skills Training Program: a systematic review and meta-analysis. Disabil Rehabil Assist Technol. 2019;14:391–409.
- Kirby RL, de Groot S, Cowan RE. Relationship between wheelchair skills scores and peak aerobic exercise capacity of manual wheelchair users with spinal cord injury: a cross-sectional study. Disabil Rehabil. 2020;42(1):114–121.
- Sawatzky B, Rushton PW, Denison I, et al. Wheelchair skills training programme for children: a pilot study. Aust Occup Ther J. 2012;59(1):2–9.
- 2021. Available from: https://wheelchairskillsteam.nl/
- Eddolls WTB, McNarry MA, Stratton G, et al. High-intensity interval training interventions in children and adolescents: a systematic review. Sports Med. 2017;47(11):2363–2374.
- Graham HK, Harvey A, Rodda J, et al. The Functional Mobility Scale (FMS). J Pediatr Orthop. 2004;24(5):514–520.
- Chen WY, Lin YT, Chen Y, et al. Reference equations for predicting standing height of children by using arm span or forearm length as an index. J Chin Med Assoc. 2018;81(7):649–656.
- Horemans H, Kooijmans H, van den Berg-Emons R, et al. The Activ8 activity monitor: validation of posture and movement classification. J Rehabil Assist Technol Eng. 2020;7:2055668319890535.
- Leving MT, Horemans HLD, Vegter RJK, et al. Validity of consumer-grade activity monitor to identify manual wheelchair propulsion in standardized activities of daily living. PLoS One. 2018;13(4):e0194864.
- Sol ME, de Groot JF, Zwinkels M, et al. Utrecht Pediatric Wheelchair Mobility Skills Test: reliability, validity, and responsiveness in youths using a manual wheelchair. Phys Ther. 2019;99(8):1098–1106.
- Sol ME, Verschuren O, de Groot L, et al. Development of a wheelchair mobility skills test for children and adolescents: combining evidence with clinical expertise. BMC Pediatr. 2017;17(1):51.
- Sol ME, Bloemen MAT, Verschuren O, et al. Wheelchair Mobility Confidence Scale for Dutch youth using a manual wheelchair. Disabil Rehabil Assist Technol. 2019;15(6):684–691.
- Bloemen MAT, de Groot JF, Backx FJG, et al. Wheelchair shuttle test for assessing aerobic fitness in youth with spina bifida: validity and reliability. Phys Ther. 2017;97(10):1020–1029.
- Verschuren O, Zwinkels M, Ketelaar M, et al. Reproducibility and validity of the 10-meter Shuttle Ride Test in wheelchair-using children and adolescents with cerebral palsy. Phys Ther. 2013;93(7):967–974.
- Bongers BC, Rijks EBG, Harsevoort AGJ, et al. 10-m Shuttle Ride Test in youth with osteogenesis imperfecta who use wheelchairs: feasibility, reproducibility, and physiological responses. Phys Ther. 2016;96(5):679–686.
- Bloemen MA, Takken T, Backx FJ, et al. Validity and reliability of skill-related fitness tests for wheelchair-using youth with spina bifida. Arch Phys Med Rehabil. 2017;98(6):1097–1103.
- Verschuren O, Zwinkels M, Obeid J, et al. Reliability and validity of short-term performance tests for wheelchair-using children and adolescents with cerebral palsy. Dev Med Child Neurol. 2013;55(12):1129–1135.
- Sullivan GM, Feinn R. Using effect size—or why the p value is not enough. J Grad Med Educ. 2021;4(3):279–282.
- Bandura A, Freeman W, Lightsey R. Self-efficacy: the exercise of control [Internet]. New York; 1999 [cited 2020 Jun 9]. Available from: https://connect.springerpub.com/content/sgrjcp/13/2/158.full.pdf
- De Groot JF, Takken T, Van Brussel M, et al. Randomized controlled study of home-based treadmill training for ambulatory children with spina bifida. Neurorehabil Neural Repair. 2011;25(7):597–606.
- Raymond J, Davis GM, Fahey A, et al. Oxygen uptake and heart rate responses during arm vs combined arm/electrically stimulated leg exercise in people with paraplegia. Spinal Cord. 1997;35(10):680–685.