Abstract
Purpose
More positive outcome expectations and illness perceptions are associated with better outcomes for patients with several osteoarthritic orthopedic conditions. However, it is unknown whether these factors also influence outcomes of non-operative treatment for first carpometacarpal osteoarthritis (CMC-1 OA). Therefore, we assess the role of pre-treatment outcome expectations and illness perceptions in reports of pain and hand function 3 months after non-operative treatment for CMC-1 OA.
Materials and methods
We conducted a cohort study with 219 patients treated non-operatively for CMC-1 OA between September 2017 and October 2018. Patients were included in the study if they completed measures of pain and hand function, illness perceptions (scale: 0–10), and expectations (scale: 3–27) as part of routine outcome measurements. Pain and hand function were measured before treatment and 3 months after starting treatment using the Dutch version of the Michigan Hand Outcomes Questionnaire. Multivariable linear regression analysis was used to assess the influence of outcome expectations and illness perceptions on pain and hand function.
Results
Both positive outcome expectations (B = 0.64; 95% CI [0.1–1.2]) and a better illness understanding (an illness perception subdomain; B = 1.53; 95% CI [0.2–2.9]) at baseline were associated with less pain at 3 months. For hand function, similar estimates were found.
Conclusions
We found that positive outcome expectations and a better illness understanding, were associated with a better outcome of non-operative treatment for CMC-1 OA.
Non-operative treatment can often be successful for patients with arthritis of the thumb.
Outcome expectations and illness perceptions are associated with pain and hand function 3 months after non-operative treatment for thumb base osteoarthritis.
Improving the outcome expectations and illness perceptions of patients through better education could improve the outcome of non-operative treatment.
IMPLICATIONS FOR REHABILITATION
Introduction
Carpometacarpal osteoarthritis of the thumb (CMC-1 OA) is a disabling illness where non-operative treatment can often be successful [Citation1]. The incidence of CMC-1 OA is estimated at 7.5%, of which 20% seeks treatment [Citation2]. Usually, treatment is started non-operatively with orthosis, injections, or hand therapy. As a recent study indicated, a good outcome of non-operative treatment for CMC-1 OA may delay and often prevent surgical treatment [Citation3]. Given the considerable variation in treatment outcome for CMC-1 OA and modest patient satisfaction [Citation4], it is important to understand which pre-treatment factors are associated with a better outcome of non-operative treatment for CMC-1 OA.
To date, it is mostly unknown which factors are associated with a better outcome of non-operative treatment for CMC-1 OA. One study found no predictive factors for treatment outcome over and above baseline pain and function [Citation1]. However, in this study, the psychological mindset of patients at the start of the treatment was not assessed.
Several aspects of the influence of patient mindset on the outcome of treatment have been assessed before. For example, studies have found that patients who experience more psychological distress and who have a stronger tendency to catastrophize pain may benefit less from CMC-1 OA treatments [Citation5–8]. However, these studies are limited as they did not adjust for baseline disease severity.
Two additional and potentially important aspects of the patient mindset are the extent to which a patient has positive expectations about the efficacy of the treatment, and the illness perceptions of the patients. Several studies in other conditions have demonstrated a positive association between outcome expectations and better patient-reported treatment outcomes across a variety of medical conditions including OA [Citation9–14]. However, no prior studies have prospectively examined the role of expectations and illness perception on outcomes of non-operative treatment in CMC-1 OA.
Therefore, we investigated the association between treatment outcome expectations and illness perceptions and patient-reported pain and hand function 3 months after starting non-operative treatment of CMC-1 OA patients, while adjusting for baseline pain, function, psychological distress, and catastrophic thinking about pain.
Methods
Context
The study was performed at Xpert Clinic and Handtherapie Nederland, comprising of 22 outpatient clinics for hand surgery and therapy in the Netherlands, and took place between September 2017 and October 2018, after approval by the local Medical Ethical Committee (Rotterdam, NL/sl/MEC-2018-1088). Patients were treated by hand therapists who received the same internal training on how to treat CMC-1 OA with hand therapy. Participants received treatment under the supervision of (generally) the same therapist, using a standardized protocol. All therapists are certified physical therapists with extensive experience as a hand therapist.
Patients
All patients receiving non-operative treatment for CMC-1 OA who completed psychological screening questionnaires before treatment and the Michigan Hand Outcomes Questionnaire (MHQ) before treatment and 3 months after treatment were included in the cohort. Details of the data collection have been published earlier [Citation15]. Patients and therapists were not blinded to the treatment.
Intervention
All patients were clinically diagnosed with CMC-1 OA based on presenting complaints and clinical signs. As defined in the Dutch guideline [Citation16] for primary CMC-1 OA, all patients were offered non-operative treatment first, including an orthosis and/or hand therapy. In general, treatment consisted of prescribing a custom-made or prefabricated thumb orthosis (usually including CMC-1 positioned in palmar and radial abduction and slight metacarpophalangeal flexion) and one to two 25-min sessions of hand therapy per week for a total of 12 weeks. The first 6 weeks of treatment aimed at correcting the position of the CMC-1 into a more stable position of palmar and radial abduction and prevention of flexion and adduction. This included coordination and mobility exercises [Citation4] (4–6 times/day, 10–15 repetitions). The last 6 weeks of treatment were mainly focused on improving active stability and pinch strength and also included functional exercises [Citation4] (2–3 times/day up until 50–100 repetitions). Additional or fewer sessions could be planned based on the therapist’s judgment and the availability of the participant. A more detailed description of the treatment has been reported in previous papers [Citation1,Citation4].
Outcome measures
The primary endpoint for this study was 3 months after starting non-operative treatment. As the primary outcome, we used the pain subscale of the Dutch version of the MHQ [Citation17], measured as part of routine outcome measurements. The MHQ is a validated patient-reported outcome measure (PROM) to assess patients’ pain and hand functioning [Citation17,Citation18]. The secondary outcome was the hand function subscale of the MHQ. The questions of these subscales result in a 0 (severe pain or dysfunction)–100 (no pain or dysfunction) score. All data were collected as part of routine outcome measurement using GemsTracker electronic data capture tools [Citation19]. After the initial diagnosis, a hand therapist assigns prespecified routine outcome measures to all patients in the clinic. Patients receive emails to complete online questionnaires at preset time points. This system has been described in more detail in an earlier publication [Citation15]. Completing questionnaires is encouraged and facilitates evaluation of progress throughout the treatment, but completing questionnaires is not required for any part of the treatment.
Baseline demographics
Baseline characteristics of all patients (including age, sex, workload, duration of complaints, hand dominance, smoking status, and body mass index) were collected by the therapist during the first consultation.
Patient mindset
To assess patients’ baseline mindset, patients completed four questionnaires: (i) the Patient Health Questionnaire (PHQ-4) [Citation20], a screening tool for depression and anxiety that results in a score from 0 (no psychological distress) to 12 (high psychological distress), (ii) the Pain Catastrophizing Scale (PCS) [Citation21], a questionnaire to assess a patient’s tendency to catastrophize pain. The PCS ranges from 0 (no pain catastrophizing) to 52 (high pain catastrophizing), (iii) the Credibility/Expectancy Questionnaire (CEQ) [Citation22], a questionnaire that measures patients’ outcome expectations and credibility of the treatment and results in a score from 3 (low expectations and credibility) to 27 (high expectations and credibility). The CEQ specifically asks patients how much they “feel” or “think” the treatment will reduce symptoms and the physical limitation due to symptoms of their CMC-1 OA. In this study, we only evaluated the 3-item expectancy subscale of the CEQ. iv) The Brief Illness Perceptions Questionnaire (B-IPQ) [Citation23], a questionnaire that measures how patients perceive their illness on eight separate domains, using a single 0–10 question for each domain. The fourth question of the IPQ asks patients how they think the treatment will affect their illness. Since this construct is evaluated using the expectancy domain of the CEQ as well, this item of the B-IPQ was not used in our analyses. We used the validated Dutch versions of all questionnaires [Citation24–26].
Data analysis
First, we assessed the univariable associations of all baseline characteristics with pain and hand function at 3 months. However, in this analysis, we adjusted for baseline MHQ because we previously found that baseline pain and function were strongly related to the outcome [Citation3]. Then, to assess which patient characteristics and mindset variables were independently associated with outcome, we performed two multivariable linear regressions with pain and hand function as outcomes. In addition to an overall multivariable model, we developed a stepwise multivariable model to assess the contribution of the different sets of variables to the explained variance (R2). First, we added patient and disease characteristics to the model, second, we added psychological distress and pain catastrophizing, and finally, we added outcome expectations and illness perceptions. We added psychological distress and pain catastrophizing first because previous literature has shown associations between these variables and pain and hand function [Citation5,Citation6]. The relationship between outcome expectations, illness perceptions, and outcomes is unknown. Therefore, we added these variables last.
All analyses were conducted using R statistical computing, version 3.3.4. For all tests, a p-value of ≤0.05 was considered statistically significant. We assumed that all relationships were linear and the model residuals were normally distributed. We confirmed these assumptions. A power calculation using G Power (version 3.1), based on a multivariable model, indicated that a sample of 159 patients was needed to detect a small to medium effect (f = 0.1) of the patient mindset on outcomes given a power of 0.8 and alpha of 0.05.
The funder played no role in the design, conduct, or reporting of this study.
Results
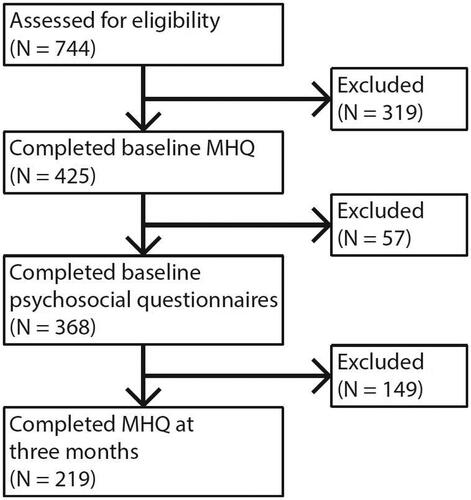
Between September 2017 and October 2018, we included 219 patients. shows the flow of patients throughout the study and reasons for exclusion. 87% of all patients who completed the MHQ also completed all mindset questionnaires while at 3 months, 60% of these patients also completed the MHQ. There were no significant differences between patients who did and did not complete all necessary questionnaires.
presents the baseline demographic characteristics and mindset variables of all patients that are included in the analysis. Patients had a mean age (SD) of 60 (7) years old and the majority were female (76%). On average, the MHQ pain subscale at 3 months improved by 10 points (p < 0.001, 95% CI [Citation8–12]), and the MHQ hand function subscale increased by 5 points (p < 0.001, 95% CI [Citation3–7]) compared to baseline.
Table 1. Baseline patient and psychosocial characteristics of the study population (n = 219 patients receiving non-operative treatment for first carpometacarpal osteoarthritis).
In the univariable analyses, where we only adjusted for baseline MHQ values, being a smoker was associated with more pain at 3 months. Additionally, having more positive outcome expectations was associated with less pain and increased hand function at 3 months (see ).
Table 2. Multivariable associations between MHQ at 3 months and individual predictors, adjusted for baseline MHQ, indicating the association of the different variables with the MHQ outcome.
In the multivariable analyses a more positive outcome expectation and a better illness understanding (an illness perception subdomain) of patients’ illness were associated with less pain (see ). For hand function, a more positive outcome expectation was associated with better hand function at 3 months. and illustrate the magnitude of the effect of pre-treatment expectations and illness perceptions on pain and hand function at 3 months, illustrating both the systematic effects and the relatively large variation between subjects.
Figure 2. Effect plots of association between outcome expectations (a) and illness understanding (b) and pain at 3 months. All points represent individual patients. Jitter, minimal random variance, has been added to display overlapping points. Higher Michigan Hand Outcomes Questionnaire (MHQ) pain score on the y-axis represents less pain. Higher scores on the x-axis represent more positive outcome expectations or better understanding.
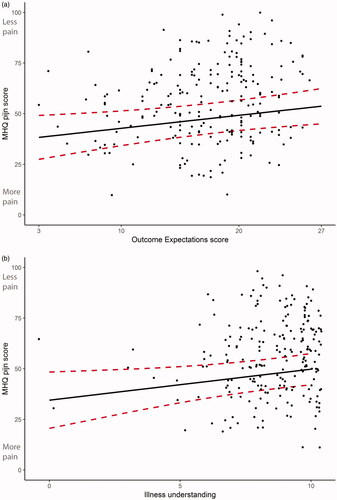
Figure 3. Effect plots of association between expectations and hand function at 3 months. All points represent the scores of individual patients. Jitter has been added to display overlapping points. Higher Michigan Hand Outcomes Questionnaire (MHQ) hand function score on the y-axis represents more hand function. Higher scores on the x-axis represent more positive outcome expectations.
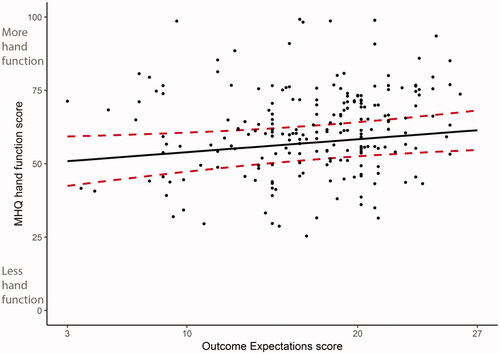
Table 3. Multivariable linear regression model for pain and hand function at 3 months, adjusted for all covariates, indicating the adjusted contributions of all variables in a multivariable model.
Stepwise linear regression analysis revealed that 32% of the variance in pain at 3 months could be explained by patient characteristics and baseline pain. No additional variance could be explained by psychological distress and pain catastrophizing, but outcome expectations and illness perceptions explained an additional 5% of the variance over and above all other variables (Supplementary Table S1). For hand function, 28% of the variance at 3 months could be explained by patient characteristics and baseline hand function. An additional 1% could be explained by psychological distress and pain catastrophizing and outcome expectations and illness perceptions explained an additional 4% over and above all other variables (Supplementary Table S2).
Discussion
We investigated the relationship between the psychological mindset of CMC-1 OA patients at the start of a non-operative treatment and patient-reported pain and hand function at 3 months after treatment. We found that two aspects of the patient mindset, positive outcome expectations, and a better illness understanding, were independently associated with a better outcome of non-operative treatment for CMC-1 OA. After adjusting for patient characteristics, pain catastrophizing, and psychological distress, we found that two aspects of the patient mindset, positive outcome expectations, and a better illness understanding, were independently associated with a better outcome of non-operative treatment for CMC-1 OA.
Our finding that more positive outcome expectations are associated with better outcomes is in line with several other studies [Citation27,Citation28]. For example, Blanchard et al. [Citation27] found that women with higher self-efficacy and outcome expectations were more likely to be active during cardiac rehabilitation and Lurie et al. [Citation28] found that lumbar disc herniation patients with more positive outcome expectations had better outcomes and were more physically active during cardiac rehabilitation.
Several mechanisms may explain the relationship between outcome expectation and PROMs. For example, studies indicate that having more positive treatment outcome expectations may trigger psychobiological mechanisms, such as anxiety reduction, positive affectivity, cognitive reinterpretation, treatment adherence, and conditioning [Citation29–31]. This is confirmed in studies showing that interventions aimed to optimize patients’ outcome expectations have improved outcomes [Citation32–35]. Future studies could investigate how different expectation management strategies affect patients with CMC-1 OA and evaluate their effects on outcomes in daily clinical practice.
In addition to outcome expectations, our results show that patients that report a better illness understanding have less pain at 3 months. This is in line with findings from Hanusch et al. [Citation11], who found that better illness understanding was associated with better early recovery after total knee arthroplasty. Moreover, Mosleh et al. [Citation36] found that patients with coronary heart disease who reported better illness understanding were more likely to adhere to exercise therapy.
While we studied associations, several studies have investigated strategies to change patients’ illness perception. For instance, Lee et al. [Citation37] educated trauma patients on the theory of illness perceptions and asked them to identify inadequate perceptions. In this study, they found that these patients obtained more positive illness perceptions, however, the influence on outcome was unfortunately not studied. Future studies may investigate if incorporating these strategies in the treatment of CMC-1 OA also leads to a more positive illness perception and, most importantly, to better outcomes.
In contrast with previous literature, we did not find any associations between outcomes of non-operative treatment for CMC-1 OA and pain catastrophizing or psychological distress. For example, the papers by Das De et al. [Citation6] and Lozano-Calderon et al. [Citation7] showed that these factors play an important role in patients with CMC-1 OA. However, in these studies post-treatment PROMs were not adjusted for pre-treatment PROMs, which might explain the difference with our own findings. As CMC-1 OA complaints are known to be associated with pain catastrophizing and psychological distress before treatment [Citation38], it may be worthwhile to further investigate potential indirect pathways through which these mindset variables affect treatment outcomes in CMC-1 OA.
The strengths of our study are its longitudinal design and the fact that this is the first to study the influence of expectations alongside other psychosocial factors on outcome of non-operative treatment of CMC-1 OA. More specifically, most upper-extremity studies do not take pre-treatment symptoms into account when investigating the role of the patients’ mindset, even though pre-treatment symptoms play an important role in predicting outcomes in upper-extremity conditions [Citation3,Citation39].
Study limitations
A limitation of our study is the non-response rate during our study; 87% of all patients who completed the MHQ also completed all mindset questionnaires while at 3 months, 60% of these patients also completed the MHQ. However, there were no significant differences in baseline characteristics between the non-responders and the patients included in the analysis, suggesting no selection bias on the reported analyses. Furthermore, this percentage of missing data is representative of routine longitudinal data collection. For example, Crijns et al. [Citation40] found similar rates of missing data in hand surgery patients.
Conclusion
Our finding that higher outcome expectation leads to better outcomes may challenge the common belief in orthopedic surgery, hand surgery, and hand therapy that a patient should not have too high expectations [Citation41]. Discussing outcome expectations at the start of the non-operative treatment, in particular, with patients who appear skeptical about the potential treatment benefits, might contribute to better outcomes. Our results also indicate that explaining the illness to a patient may improve the outcome of treatment. Therefore, it might be worthwhile for clinicians to ensure that the patient understands the etiology and prognosis of their illness.
Supplementary_Tables_REVISED.pdf
Download PDF (312.8 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Tsehaie J, Spekreijse KR, Wouters RM, Slijper HP, et al. Outcome of a hand orthosis and hand therapy for carpometacarpal osteoarthritis in daily practice: a prospective cohort study. J Hand Surg Am. 2018;43:1000–1009.e1.
- Chaisson CE, Zhang Y, McAlindon TE, et al. Radiographic hand osteoarthritis: incidence, patterns, and influence of pre-existing disease in a population based sample. J Rheumatol. 1997;24:1337–1343.
- Tsehaie J, Spekreijse KR, Wouters RM, et al.; Hand-Wrist Study Group. Predicting outcome after hand orthosis and hand therapy for thumb carpometacarpal osteoarthritis: a prospective study. Arch Phys Med Rehabil. 2018;100(5):844–850.
- Wouters RM, Tsehaie J, Slijper HP, et al. Exercise therapy in addition to an orthosis reduces pain more than an orthosis alone in patients with thumb base osteoarthritis: a propensity score matching study. Arch Phys Med Rehabil. 2018;100(6):1050–1060.
- Becker SJ, Bot AG, Curley SE, Jupiter JB, et al. A prospective randomized comparison of neoprene vs thermoplast hand-based thumb spica splinting for trapeziometacarpal arthrosis. Osteoarthritis Cartilage. 2013;21(5):668–675.
- Das De S, Vranceanu AM, Ring DC. Contribution of kinesophobia and catastrophic thinking to upper-extremity-specific disability. J Bone Joint Surg Am. 2013;95(1):76–81.
- Lozano-Calderon SA, Souer JS, Jupiter JB, et al. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand. 2008;3(3):271–275.
- Makarawung DJ, Becker SJ, Bekkers S, et al. Disability and pain after cortisone versus placebo injection for trapeziometacarpal arthrosis and de Quervain syndrome. Hand. 2013;8(4):375–381.
- Waljee J, McGlinn EP, Sears ED, et al. Patient expectations and patient-reported outcomes in surgery: a systematic review. Surgery. 2014;155(5):799–808.
- Smeets RJ, Beelen S, Goossens ME, et al. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin J Pain. 2008;24:305–315.
- Hanusch BC, O’Connor DB, Ions P, et al. Effects of psychological distress and perceptions of illness on recovery from total knee replacement. Bone Joint J. 2014;96-B(2):210–216.
- Dalili Z, Bayazi MH. The effectiveness of mindfulness-based cognitive therapy on the illness perception and psychological symptoms in patients with rheumatoid arthritis. Complement Ther Clin Pract. 2019;34:139–144.
- Zyrianova Y, Kelly BD, Sheehan J, et al. The psychological impact of arthritis: the effects of illness perception and coping. Ir J Med Sci. 2011;180:203–210.
- Berner C, Erlacher L, Fenzl KH, et al. A cross-sectional study on self-reported physical and mental health-related quality of life in rheumatoid arthritis and the role of illness perception. Health Qual Life Outcomes. 2018;16:238.
- Selles RW, Wouters RM, Poelstra R, et al. Routine health outcome measurement: development, design, and implementation of the hand and wrist cohort. Plast Reconstr Surg. 2020;146(2):343–354.
- Nederlandse Vereniging Voor Plastische Chirurgie. Conservatieve en Chirurgische Behandeling van Primaire Artrose van de Duimbasis. Amsterdam, N-Holland, The Netherlands: NVvH; 2014.
- Huijsmans R, Sluiter H, Aufdemkampe G. Michigan Hand Outcomes Questionnaire-DLV: een vragenlijst voor patienten met handfunctieproblemen. Fysiopraxis. 2001;9:38–41.
- Chung KC, Pillsbury MS, Walters MR, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23:575–587.
- Zorgbedrijven EMaE. version 1.8.2. 2019. Available from: https://gemstracker.org.
- Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621.
- Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524–532.
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73–86.
- Broadbent E, Petrie KJ, Main J, et al. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–637.
- de Raaij EJ, Schroder C, Maissan FJ, et al. Cross-cultural adaptation and measurement properties of the Brief Illness Perception Questionnaire-Dutch Language Version. Man Ther. 2012;17(4):330–335.
- Timmermans I, Versteeg H, Meine M, et al. Illness perceptions in patients with heart failure and an implantable cardioverter defibrillator: dimensional structure, validity, and correlates of the brief illness perception questionnaire in Dutch, French and German patients. J Psychosom Res. 2017;97:1–8.
- Mertens VC, Moser A, Verbunt J, et al. Content validity of the credibility and expectancy questionnaire in a pain rehabilitation setting. Pain Pract. 2017;17:902–913.
- Blanchard C, Arthur HM, Gunn E. Self-efficacy and outcome expectations in cardiac rehabilitation: associations with women’s physical activity. Rehabil Psychol. 2015;60:59–66.
- Lurie JD, Henderson ER, McDonough CM, et al. Effect of expectations on treatment outcome for lumbar intervertebral disc herniation. Spine. 2016;41:803–809.
- Morrison JD, Stuifbergen AK. Outcome expectations and physical activity in persons with longstanding multiple sclerosis. J Neurosci Nurs. 2014;46:171–179.
- Stetler C. Adherence, expectations and the placebo response: why is good adherence to an inert treatment beneficial? Psychol Health. 2014;29(2):127–140.
- Geers AL, Miller FG. Understanding and translating the knowledge about placebo effects: the contribution of psychology. Curr Opin Psychiatry. 2014;27:326–331.
- Rief W, Shedden-Mora MC, Laferton JA, et al. Preoperative optimization of patient expectations improves long-term outcome in heart surgery patients: results of the randomized controlled PSY-HEART trial. BMC Med. 2017;15:4.
- Lo SHS, Chang AM, Chau JPC. Stroke self-management support improves survivors’ self-efficacy and outcome expectation of self-management behaviors. Stroke. 2018;49(3):758–760.
- Kube T, Glombiewski JA, Rief W. Using different expectation mechanisms to optimize treatment of patients with medical conditions: a systematic review. Psychosom Med. 2018;80:535–543.
- Kube T, Rief W, Gollwitzer M, et al. Introducing an EXperimental Paradigm to investigate Expectation Change (EXPEC). J Behav Ther Exp Psychiatry. 2018;59:92–99.
- Mosleh SM, Almalik MM. Illness perception and adherence to healthy behaviour in Jordanian coronary heart disease patients. Eur J Cardiovasc Nurs. 2016;15(4):223–230.
- Lee BO, Chien CS, Hung CC, Chou PL. Effects of an in-hospital nursing intervention on changing illness perceptions in patients with injury. J Adv Nurs. 2015;71:2540–2550.
- Hoogendam L, van der Oest MJW, Tsehaie J, et al.; Hand-Wrist Study Group. Psychological factors are more strongly associated with pain than radiographic severity in non-invasively treated first carpometacarpal osteoarthritis. Disabil Rehabil. 2019;1–6. DOI:10.1080/09638288.2019.1685602.
- MacDermid JC, Valdes K, Szekeres M, et al. The assessment of psychological factors on upper extremity disability: a scoping review. J Hand Ther. 2018;31:511–523.
- Crijns TJ, Bernstein DN, Gonzalez R, et al. Operative treatment is not associated with more relief of depression symptoms than nonoperative treatment in patients with common hand illness. Clin Orthop Relat Res. 2020;478:1319–1329.
- Waljee JF, Chung KC. Commentary regarding “Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis”. J Hand Surg Am. 2015;40:491–492.