Abstract
Purpose
Investigate the impact of 12-weeks’ moderate-intensity resistance training on psychological parameters in ambulatory adults with Facioscapulohumeral, Becker, and Limb–girdle muscular dystrophy.
Methods
Seventeen adults with Facioscapulohumeral (n = 6), Limb–girdle (n = 6; types 2A, 2B, 2L, and 2I), or Becker (n = 5) muscular dystrophy took part. Participants were tested at baseline (PRE), after a 12-week control period (PRE2), and after a 12-week supervised resistance training programme (POST). Training included multi-joint and single-joint resistance exercises. Outcomes from self-report questionnaires were health-related quality of life, depressive symptoms, trait anxiety, self-esteem, and physical self-worth.
Results
No difference in outcome measures, except depressive symptoms, was found in the control period (PRE to PRE2). Symptoms of depression were reduced by 9% from PRE to PRE2 (p < 0.05) and by a further 19% from PRE2 to POST (p < 0.05). Other changes from PRE2 to POST were that trait anxiety reduced by 10%, self-esteem increased by 10%, physical self-worth increased by 20%, and quality of life improved in 8 domains (p < 0.05).
Conclusion
These findings demonstrate the positive impact of moderate-intensity resistance training on psychological health and quality of life in adults with Facioscapulohumeral, Becker, and Limb–girdle muscular dystrophies.
Resistance training can have a positive impact on psychological health and quality of life in adults with Facioscapulohumeral, Becker, and Limb–girdle muscular dystrophy.
Healthcare professionals should consider including moderate-intensity resistance training within the management and treatment programmes of adults with Facioscapulohumeral, Becker, and Limb–girdle muscular dystrophy.
Implications for rehabilitation
Introduction
Muscular dystrophy (MD) represents a heterogeneous group of neuromuscular conditions caused by mutations in various genes [Citation1]. These mutations cause an absence or decrease in one of the many proteins typically located within the muscle cell [Citation2], resulting in progressive muscle weakness and deterioration. The molecular basis of some MDs is better understood than others. Duchenne and Becker MD (BMD) exhibit an absence or reduced expression of the protein dystrophin in the plasma membrane of the muscle cell, respectively [Citation2,Citation3]. This causes instability within the cell membrane leaving muscle fibres susceptible to damage during contraction [Citation4]. The molecular basis of Facioscapulohumeral MD (FSHD) was long debated but the consensus now exists that inappropriate expression of the protein DUX4 within skeletal muscle causes deterioration through mechanisms, such as apoptosis and diminished muscle regeneration [Citation5,Citation6]. No universal mechanism for muscle deterioration exists in Limb–girdle MD (LGMD) as it encompasses more than thirty subtypes. Each subtype affects a distinct protein within the sarcolemma, cytosol, or nucleus of the muscle cell, but it is probable that most LGMDs result in membrane instability akin to Duchenne and BMD [Citation7]. FSHD, BMD, and LGMD differ in genotype and presentations of physical impairment, but each results in progressive reductions in muscle strength and physical function [Citation8].
While muscle weakness generates a multitude of physical challenges for those living with FSHD, BMD, and LGMD, the psychological aspects of living with a long-term condition can be equally, if not more, challenging. Various authors have reported poorer psychological health in adults with FSHD, LGMD, and/or BMD compared to normative reference values or control groups, including greater symptoms of depression [Citation9–11] and higher trait anxiety [Citation11]. Furthermore, numerous studies have documented poorer quality of life (QoL) in adults with FSHD, BMD, and/or LGMD [Citation10,Citation12–14], in both physical (e.g., physical function, role physical, bodily pain, and general health) and mental (e.g., social function, role emotion, mental health, and depressive moods) QoL domains.
Resistance training (RT) is a form of exercise that has been shown to positively influence mental health and QoL in a range of clinical populations. QoL was improved post-RT in adults with Parkinson’s disease [Citation15], older adults [Citation16], patients with chronic heart failure [Citation17], and multiple sclerosis [Citation18], to name a few. Symptoms of depression or anxiety were improved post-RT in older adults, breast cancer patients, and adults with osteoarthritis [Citation19]. Furthermore, RT has also been shown to improve self-perceptions in clinical populations. Global self-esteem and physical self-worth increased post-12 weeks’ RT in obese women [Citation20]. RT may also elicit beneficial effects on mental health, QoL, and self-perceptions in adults with MD, but this is yet to be investigated in any depth. One study considered the influence of a group exercise to music programme on QoL in adults with myotonic MD but reported no effect of the 14-week programme [Citation21]. However, the exercise programme was fundamentally an efficacy programme that did not induce any improvement in physical function. The lack of research in this area is likely due to historical discouragement of RT in individuals with MD [Citation22].
The discouragement of RT in dystrophic populations stemmed from concerns that RT could cause extensive damage during contraction in dystrophic muscle [Citation4]. Such caution originated from findings of greater damage in dystrophic than healthy muscle following exposure to maximal eccentric contractions in the mdx mouse model of Duchenne MD [Citation23]. Despite being specific to dystrophin-deficient muscle, these findings promoted discouragement of resistance exercise across each type of MD. However, a recent meta-analysis reported that whilst muscular exercise was not found to be associated with strength improvements in muscular dystrophy, it was not harmful [Citation24]. Additionally, numerous recent studies that were not included within this meta-analysis demonstrate increased muscle strength or physical function following low to moderate intensity resistance exercise in ambulatory boys with Duchenne MD (isometric leg resistance exercises) [Citation25], mdx mice (isometric contractions) [Citation26], Myotonic dystrophy type 1 (multi-joint resistance exercises) [Citation27], and Myotonic dystrophy type 2 (full-body resistance programme) [Citation28]. Furthermore, in adults with FSHD, BMD, and LGMD, our primary study found positive effects of 12 weeks’ moderate-intensity RT on muscle strength and physical function, using a 13% increase in knee flexion maximum voluntary contraction torque and a 36, 18, and 24% reduction in the time taken to perform a sit-to-stand, stair ascent and stair descent task, respectively [Citation29].
Given the known psychological benefits of RT in other populations and the improvements we reported in strength and physical function post-RT in adults with FSHD, BMD, and LGMD [Citation29], the current paper will explore the impact of RT on psychological parameters in the same group of participants. Therefore, this study aims to examine the impact of 12-weeks’ moderate-intensity RT on QoL, depressive symptoms, trait anxiety, self-esteem, and physical self-worth in adults with FSHD, BMD, and LGMD.
Method
Participants
Seventeen adults with three variants of MD (FSHD, BMD, and LGMD) took part. The specific types of LGMD were 2A (n = 2), 2B (n = 2), 2I (n = 1), and 2L (n = 1). Participants were recruited from The Neuromuscular Centre (Winsford, UK) where they regularly (weekly, bi-weekly, or monthly) received physiotherapy consisting of passive stretching activities for 1 h. Participant characteristics for each MD group and a grouped average for MD are presented in . In line with other studies that have grouped multiple MDs for analysis, such as FSHD and LGMD [Citation30] and BMD and LGMD [Citation31], we have combined all participants as “adults with MD.”
Table 1. Participant characteristics and anthropometrics at baseline (PRE) for each MD group and the combined MD group.
All participants were considered ambulatory (able to walk at least 7 m, with or without assistive walking aids), were of sound intellectual status, and were in otherwise good health without any uncontrolled co-morbidity or cardiac issues. Participants had not previously undertaken structured RT and self-reported that they did not undertake more than 1 h of intense physical activity or 3 h of low-moderate physical activity per week (according to their interpretation of intense and moderate physical activity).
The Manchester Metropolitan University Ethics Committee granted ethical approval and all participants provided written informed consent before participating in the study. All procedures complied with the World Medical Association Deceleration of Helsinki [Citation32].
Procedures
Participants attended three repeat testing sessions, which were identical between participants and sessions. Baseline measures were taken at the initial testing session (PRE), followed by a second testing session 12 weeks later (PRE2). Between PRE and PRE2 participants were asked to maintain their habitual physical activity and prescribed physiotherapy sessions, which provided a control period. After PRE2, participants completed a 12-week RT programme of moderate-intensity followed by a third testing session (POST) within 2 weeks of completing the RT. The participants acted as their controls because of the progressive nature of MD and the inherent variance within the conditions. Although not as robust as randomised control trials, this single-arm non-crossover design (where participants act as their control) is encouraged for longitudinal interventions in heterogenous populations like the current one [Citation33]. This study design mitigates the possible variability of the training response within a population and it is consistent with previous RT studies [Citation34].
The 12-week, twice a week, supervised RT programme has been described previously [Citation29] and resulted in significant improvements in maximum knee flexion strength, sit-to-stand time, stair ascent time, and stair descent time, in the same cohort of participants under study.
In short, the RT programme was progressive, at a moderate intensity, and individual to each participant’s needs and functional capability. It included a 5-min warm-up, 5-min of balance training, four resistance exercises that were the same for all participants, and six resistance exercises that were specific to each participant. The four resistance exercises that all participants completed were two multi-joint exercises (step-ups and freestanding or assisted squats) and seated knee flexion and knee extension on a knee extension and leg curl machine (Pro Heavy Duty, XS Sports). Step-ups were onto a box of various heights (specific to each ability) and were progressive. Squats were assisted by placing a Swiss ball between the wall and the lower back to support posterior balance, or they were completed on an adapted physiotherapy treatment bed that enabled a squat like movement (simultaneous flexion and extension of the hip, knee, and ankle joint) to be undertaken whilst lay on a plinth at any gradient between horizontal and vertical. The training load (i.e., the proportion of bodyweight involved in the squat-like movement) was increased by increasing the gradient of the plinth. A visual representation and detailed description of this have been provided previously [Citation29]. Subsequently, six individual resistance exercises were undertaken. These were single-joint exercises selected by the research team, which were based on a needs analysis that was undertaken for each participant at PRE. They included variations of hip flexion, hip extension, plantar flexion, dorsiflexion, hip abduction, hip adduction, hip internal rotation, or hip external rotation exercises.
For the first 3 weeks, participants completed two sets of 10 repetition maximums (RM) for each exercise, thereafter three sets of 10 RM were completed. Participants completed each exercise repetition at a velocity of 2 s concentric and 4 s eccentric [Citation35], with 1-min rest between sets. The 10RM training load was checked every 3 weeks and increased if the participant could lift the current load for 12 repetitions. This load and volume are consistent with other MD training studies [Citation31,Citation36,Citation37] and what is advised by The American College of Sports Medicine [Citation38]. Participants were instructed to complete each exercise through a full range of movements. If participants were unable to do this, due to the weight of their body or limb, assistance was given manually by the investigator or using rubber exercise bands. Alternatively, the movement was completed in a gravity-neutral position, such as knee flexion in a side-lying position.
Outcome measures
Health-related quality of life – the 36-item short-form health survey version 2
The Short Form Health Survey has 36 questions on functional health and well-being, which assess QoL from the participant’s perspective [Citation39]. Participants rated themselves on a multiple-choice scale per question. The answers are summarised into four physical domains (Physical Function, Role Physical, Bodily Pain, and General Health), four mental domains (Vitality, Social Function, Role Emotion, and Mental Health), and two-component health scores (Physical Component score and Mental Component score). Scores range between 0 and 100 on each domain. Higher scores indicate better QoL. The scale has excellent test-retest reliability with intraclass correlation coefficients (ICC) above 0.80 [Citation39].
Depressive symptoms – The Beck Depression Inventory
The Beck Depression Inventory is a self-report questionnaire with 21 multiple-choice questions that measure depressive symptom severity. It has excellent reliability, with a test-retest ICC of 0.96 [Citation40]. Participants score each question from 0 (least) to 3 (most), with a total sum score indicating overall depressive symptom severity from 0 to 63. Higher scores indicate increased severity of depressive symptoms. The cut scores are as follows: ≤10 indicates zero to minimal depressive symptoms, 11–20 indicates mild depressive symptoms, 21–30 indicates moderate depressive symptoms, and ≥31 indicates severe depressive symptoms.
Trait anxiety – State-Trait Anxiety Inventory
The trait subscale of the State-Trait Anxiety Inventory [Citation41] is a multiple-choice questionnaire that measures trait anxiety (a predisposition to long-lasting and persistent feelings of anxiety that are not restricted to particular circumstances). The trait sub-scale has excellent test-retest reliability, with a reported ICC of 0.86 [Citation41]. The scale includes 20 statements for participants to score between 1 (not at all) and 4 (very much so) to indicate how they feel generally. Total scores can range between 20 and 80, with higher scores indicating more severe trait anxiety.
Self-esteem – Rosenberg Self-Esteem Scale
The Rosenberg Self-Esteem Scale is a measure of global self-esteem [Citation42] that has excellent reported reliability, with an ICC of 0.90 [Citation43]. It has 10 questions that assess positive and negative feelings towards the self. Participants rate themselves on a 4-point Likert scale, with total scores ranging from 10 to 40. The higher the score the higher their self-esteem.
Physical self-worth – The Physical Self-Perception Profile
The Physical Self-Perception Profile is a reliable (test-retest ICCs between 0.74 and 0.91) self-report questionnaire [Citation44]. It has 30 questions that assess physical self-worth in the global domain and self-perceptions in four sub-scales: sport competence, body attractiveness, physical strength, and physical conditioning and exercise. An additional eight questions provide a measure of the importance attached by the participant to each of the four sub-scales.
Data analysis
Each questionnaire was scored according to the relevant manual and analysed in Microsoft Excel. QoL data were scored using Health Outcomes Scoring Software 4.5 (Quality Metric Health Outcomes™, Lincoln, UK). Self-esteem and physical self-worth data were omitted for one participant as The Rosenberg Self-Esteem Scale and Physical Self-Perception Profile were not completed by this participant at PRE.
Statistical analysis
All statistical analysis was completed using IBM SPSS Statistics 24 software. The critical level of significance was set at p ≤ 0.05. Data are presented as means ± standard deviations.
Data are grouped as one MD group rather than three separate groups, as has been done previously [Citation31]. Data were checked against the parametric assumptions. For parametric data, differences between the testing sessions (PRE, PRE2, and POST) were analysed using a one-way repeated measures ANOVA, with the least significant difference pairwise comparisons where appropriate. If data did not pass Mauchly’s test of sphericity (p < 0.05), a Greenhouse-Geisser correction was applied. From the ANOVA, the observed power was also reported. Variables that violated parametricity were compared between testing sessions using Friedman’s ANOVA. In these cases, Wilcoxon signed-rank tests were used post-hoc to determine the source of significant effects, with the critical level of significance adjusted for multiple comparisons using the Bonferroni adjustment method (0.05/3) so that significance was accepted if p ≤ 0.017. Physical self-worth data in the following domains violated the parametric assumption of the normal distribution: Sport, Strength, Body, Sport Importance, Strength Importance, Body Importance, and Condition Importance. Quality of life data in the following domains violated the parametric assumption of the normal distribution: Physical Function, Social Function, and Role Emotion. All other outcome variables were parametric.
Results
Demographics and anthropometrics
Age, stature, and body mass did not significantly differ between the MD sub-groups at PRE (p > 0.05; ). Body mass did not significantly change (p > 0.05) between repeat testing sessions (PRE: 87.9 ± 17.3 kg; PRE2: 89.2 ± 19.0 kg; POST: 88.1 ± 18.1 kg). Mean adherence to the RT programme was 97%, with no adverse effects reported by participants. Thirteen participants completed all 24 training sessions, two participants completed 23 sessions, one participant completed 22 sessions, and one participant completed 18 training sessions. Data for all 17 participants were included in the analysis, regardless of the number of training sessions completed.
Health-related quality of life
A main effect of testing session was found in the Physical Component score (p = 0.005, observed power of 0.86), Mental Component score (p = 0.048, observed power of 0.60), Physical Function (p = 0.023), Role Physical (p = 0.002, observed power of 0.92), Bodily Pain (p = 0.024, observed power of 0.70), General Health (p = 0.003, observed power of 0.91), Vitality (p < 0.001, observed power of 0.98), and Social Function domains (p = 0.012). No significant difference was found in the Role Emotion (p = 0.052) or the Mental Health (p = 0.061) domains between testing sessions ().
Table 2. Quality of life in each domain for PRE, PRE2, and POST.
Table 3. Global and domain specific physical self-worth for PRE, PRE2, and POST.
Post-hoc analysis showed that the Physical Component score did not differ between PRE and PRE2 (p > 0.05) but increased by 11% from PRE to POST (p = 0.016) and by 15% from PRE2 to POST (p = 0.004). The Mental Component score did not differ between PRE and PRE2 (p > 0.05) but increased by 10% from PRE to POST (p = 0.038) with no significant difference between PRE2 and POST (p = 0.071). Physical Function did not differ between PRE and PRE2 (p > 0.017) but increased by 41% from PRE to POST (p = 0.003) with no significant difference between PRE2 and POST (p = 0.052). Role Physical did not differ between PRE and PRE2 (p > 0.05) but increased by 33% from PRE to POST (p = 0.003) and by 25% from PRE2 to POST (p = 0.003). Bodily Pain did not differ between PRE and PRE2 (p > 0.05) or between PRE and POST (p > 0.05) but increased by 29% from PRE2 to POST (p = 0.013). General Health did not differ between PRE and PRE2 (p > 0.05) but increased by 20% from PRE to POST (p = 0.012) and by 27% from PRE2 to POST (p = 0.004). Vitality did not differ between PRE and PRE2 (p > 0.05) but increased by 26% from PRE to POST (p = 0.006) and by 32% from PRE2 to POST (p < 0.001). Social Function did not differ between PRE and PRE2 (p > 0.017) but significantly increased by 32% from PRE to POST (p = 0.002) and by 25% from PRE2 to POST (p = 0.008).
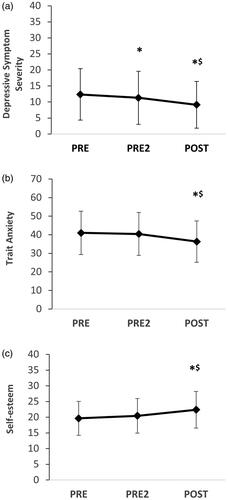
Depressive symptoms
Depressive symptoms were significantly different between testing sessions (p = 0.010, observed power of 0.79, ). Depressive symptoms decreased by 9% from PRE to PRE2 (p = 0.009), by 26% from PRE to POST (p = 0.005), and by 19% from PRE2 to POST (p = 0.048).
Trait anxiety
Trait anxiety was significantly different between testing sessions (p = 0.015, observed power of 0.76, ). Trait anxiety did not significantly differ between PRE and PRE2 (p > 0.05). Trait anxiety decreased by 11% from PRE to POST (p = 0.016) and by 10% from PRE2 to POST (p = 0.049).
Self-esteem
Self-esteem significantly differed between testing sessions (p = 0.004, observed power of 0.89, ). Self-esteem did not differ between PRE and PRE2 (p > 0.05). Self-esteem increased by 14% from PRE to POST (p = 0.001) and by 10% from PRE2 to POST (p = 0.038).
Physical self-worth
Global physical self-worth significantly differed between testing sessions (p = 0.023, observed power of 0.70, ). Global physical self-worth did not differ between PRE and PRE2 (p > 0.05). Global physical self-worth increased by 20% from PRE to POST (p = 0.043) and by 20% from PRE2 to POST (p = 0.023).
Findings were varied in the distinct domains of physical self-worth (). No difference between testing sessions was found in the sport competence domain, physical strength domain, physical condition, and exercise importance domain, body attractiveness importance domain, or the physical strength importance domain (p > 0.05). The main effect of the testing session was found in three domains; physical condition and exercise (p ≤ 0.001, observed power of 0.99), body attractiveness (p = 0.023), and sports competence importance (p = 0.004).
Post-hoc tests showed that physical self-worth in the physical condition and exercise domain did not differ between PRE and PRE2 (p > 0.05), increased by 18% (p = 0.004) from PRE to POST and increased by 18% (p = 0.001) from PRE2 to POST. Post-hoc tests showed that physical self-worth in the body attractiveness domain did not differ between PRE and PRE2 (p > 0.017) or between PRE and POST (p > 0.017) but increased by 9% from PRE2 to POST (p = 0.008). Post-hoc tests showed that physical self-worth in the sport competence importance domain did not differ between PRE and PRE2 (p > 0.017) or between PRE and POST (p > 0.017) but scores increased by 25% from PRE2 to POST (p = 0.004).
Discussion
This study examined the influence of a 12-week, twice-a-week, moderate-intensity RT programme on psychological health and QoL in a group of ambulatory adults with FSHD, BMD, and LGMD. Beneficial effects of the RT programme were evident in QoL, the severity of depressive symptoms, trait anxiety, and levels of self-esteem and physical self-worth.
In the present study, QoL improved in numerous physical and mental domains (Role Physical, Bodily Pain, General Health, Vitality, Social Function, and the Physical Component score) from immediately before to post completion of the RT programme (PRE2 – POST), compared to stable values during the 12-week control period (PRE – PRE2). These improvements ranged between 15 and 32% and provide evidence that supports the effectiveness of moderate-intensity RT to improve QoL in adults with these MDs (FSHD, BMD, and LGMD). This finding of a positive impact of RT on QoL differs from that reported in adults with myotonic dystrophy following completion of a 14-week group exercise to music programme [Citation21]. This discrepancy between studies is likely due to the type of MD studied and the focus on efficacy and adherence to group exercise in the earlier study in myotonic dystrophy. It is well-accepted that myotonic dystrophy differs vastly from the other eight types of MD because it affects nearly every system in the body [Citation3]. In addition, the moderate intensity of the RT used in our study induced physical [Citation29] and mental health improvements, adaptations that were not reported in the study in myotonic dystrophy. It is likely that the low intensity of the previous training study [Citation21], with no improvements in functional outcomes, reflects the nature of their investigation into exercise adherence and efficacy. Indeed, the dose-response and intensity response of RT on mental health outcomes is established in other populations [Citation45] and may explain the disparity between ours and the previous study.
Several QoL parameters, such as the Mental Component score and Physical Function domain, improved from PRE to POST but did not statistically differ in the control period (PRE to PRE2) or the RT period (PRE2 to POST). This can be explained by small but non-significant improvements between PRE and PRE2, which rendered the magnitude of change between PRE2 and POST insufficient to reach significance. This suggests that improvements in these QoL parameters from PRE to POST were due to the combined effects of enrolment on the study itself and the RT programme.
In terms of mental health, symptoms of depression and trait anxiety were reduced by 19 and 10% from immediately before to post-completion of the present RT programme, respectively. During the initial 12-week control period, between PRE and PRE2, trait anxiety scores remained stable. However, symptoms of depression were reduced by 9% during the control period. It is possible that symptoms of depression were influenced purely by enrolment onto the study, an outcome measure well-known to be improved from placebo interventions [Citation46]. Nevertheless, it is important to highlight that symptom of depression were reduced by a greater amount (19%) from immediately before to post-RT (PRE2 to POST), compared to the reduction found during the control period (9%). These findings are in line with studies in other clinical populations that also report reductions in symptoms of depression or anxiety post-RT, such as older adults, breast cancer patients, and adults with osteoarthritis [Citation19].
Our RT programme had a positive effect on participant’s self-perception, which agrees with previous research that reported improved self-esteem and physical self-worth post-RT in an obese population [Citation20]. Our data show that global self-esteem increased by 10% from immediately before to post-completion of the RT programme, with no change during the 12-week control period. Global physical self-worth increased by 20% from immediately before to post-completion of the RT programme, again with no change during the 12-week control period.
With regards to the specific domains of physical self-worth, changes following the RT programme were found in the physical condition and exercise and body attractiveness domains. Self-perceptions in these two areas increased by 18 and 9%, respectively, with no change during the control period. The importance placed on these two domains did not differ post-RT, which highlights that the participants’ self-perceptions in these two areas improved but the relative importance they placed on these areas remained the same. The final domain of physical self-worth that changed from immediately before to post-RT was sport competence importance, which increased by 25%. Thus, self-perceptions of sport competence remained stable, but participants placed more importance on their perceived sport competence post-RT. It is not clear why more importance was attached to the sport competence domain post-RT, but it may be due to greater exposure to an active environment through participation in the RT programme itself. Although heightened importance of each domain reduces overall physical self-worth, this finding together with increased perceptions of physical condition and body attractiveness may help individuals to continue with the RT programme, or other physical activities, long term, since they now attach more importance to an area related to sport.
This study is novel in the finding that 12-weeks of moderate-intensity RT can improve psychological parameters and QoL in a population of adults with FSHD, BMD, and LGMD. The results provide support for the inclusion of moderate-intensity RT in the management and treatment of ambulatory adults with FSHD, BMD, and LGMD. The clinical implications of the current findings are that RT may be an innovative approach to improve psychological health and QoL in adults with FSHD, BMD, and LGMD. Alongside previous research that has shown RT to improve muscle strength and/or functional performance in Duchenne MD [Citation25], Myotonic MD [Citation27,Citation28] and the same participants as the current study [Citation29], this study provides further evidence of the positive role of moderate-intensity resistance training in the management of FSHD, BMD, and LGMD. From a holistic perspective, RT may be an effective tool to enhance the health of adults living with FSHD, BMD, and LGMD. Future research should seek to examine whether baseline characteristics, such as muscle strength and years since disease onset, influence psychological improvements post-resistance training in adults with these conditions.
It is important to note the main limitations of the current study. The participants comprised three types of MD (FSHD, BMD, and LGMD) who were grouped to represent ambulatory adults with MD. Although no evidence exists at present to suggest that these three types of MD will exhibit different training adaptations, future studies should seek to establish the influence of RT on each type of MD in isolation. In addition, the FSHD and LGMD groups included a greater number of males than females. As such, there is less confidence in the findings when applied to females with these MD conditions. Further research with a larger sample of participants and an equal proportion of males and females would be advantageous to substantiate these findings.
To conclude, our data demonstrate the beneficial effects of a 12-week, twice a week, moderate-intensity RT programme compared to a control period on QoL, depressive symptoms, trait anxiety, self-esteem, and physical self-worth in ambulatory adults with FSHD, LGMD, and BMD. The findings support the inclusion of moderate-intensity RT in the management and treatment programmes of adults with FSHD, BMD, and LGMD.
Acknowledgements
The authors gratefully acknowledge the contribution of staff, patients, and patient's family members at the Neuromuscular Centre.
Disclosure statement
The authors declare that there is no conflict of interest.
Data availability statement
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
References
- Huml RA. Muscular dystrophy: a concise guide. Cham (Switzerland): Springer; 2015.
- Cohn RD, Campbell KP. Molecular basis of muscular dystrophies. Muscle Nerve. 2000;23(10):1456–1471.
- Emery AEH. The muscular dystrophies. Lancet. 2002;359(9307):687–695.
- Aartsma-Rus A. Dystrophin analysis in clinical trials. J Neuromuscul Dis. 2014;1(1):41–53.
- Tawil R, Van Der Maarel SM, Tapscott SJ. Facioscapulohumeral dystrophy: the path to consensus on pathophysiology. Skelet Muscle. 2014;4(1):12–27.
- Tawil R, Kissel JT, Heatwole C, et al. Evidence-based guideline summary: Evaluation, diagnosis, and management of facioscapulohumeral muscular dystrophy: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology and the practice issues review panel of the American Association of Neuromuscular & Electrodiagnostic Medicine. Neurology. 2015;85(4):357–364.
- Murphy AP, Straub V. The classification, natural history and treatment of the limb girdle muscular dystrophies. J Neuromuscul Dis. 2015;2(s2):S7–S19.
- Mercuri E, Muntoni F. Muscular dystrophies. Lancet. 2013;381(9869):845–860.
- Peric M, Peric S, Stevanovic J, et al. Quality of life in adult patients with limb–girdle dystrophies. Acta Neurol Belg. 2018;118(2):243–250.
- Padua L, Aprile I, Frusciante R, et al. Quality of life and pain in patients with facioscapulohumeral muscular dystrophy. Muscle Nerve. 2009;40(2):200–205.
- Mori-Yoshimura M, Mizuno Y, Yoshida S, et al. Psychiatric and neurodevelopmental aspects of Becker muscular dystrophy. Neuromuscul Disord. 2019;29(12):930–939.
- Grootenhuis MA, de Boone J, van der Kooi AJ. Living with muscular dystrophy: health related quality of life consequences for children and adults. Health Qual Life Outcomes. 2007;5(1):31.
- Jacques MF, Stockley RC, Onambele-Pearson GL, et al. Quality of life in adults with muscular dystrophy. Health Qual Life Outcomes. 2019;17(1):121.
- O'Dowd DN, Bostock EL, Smith D, et al. Psychological parameters impact health-related quality of life in mental and physical domains in adults with muscular dystrophy. Neuromuscular Disorders. 2021;31(4):328–335.
- Ferreira RM, Alves W, Lima TA, et al. The effect of resistance training on the anxiety symptoms and quality of life in elderly people with Parkinson's disease: a randomized controlled trial. Arq Neuropsiquiatr. 2018;76(8):499–506.
- Kekalainen T, Kokko K, Sipila S, et al. Effects of a 9-month resistance training intervention on quality of life, sense of coherence, and depressive symptoms in older adults: randomized controlled trial. Qual Life Res. 2018;27(2):455–465.
- Lans C, Cider A, Nylander E, et al. Peripheral muscle training with resistance exercise bands in patients with chronic heart failure. Long-term effects on walking distance and quality of life; a pilot study. ESC Heart Fail. 2018;5(2):241–248.
- Cakit BD, Nacir B, Genç H, et al. Cycling progressive resistance training for people with multiple sclerosis: a randomized controlled study. Am J Phys Med Rehabil. 2010;89(6):446–457.
- O' Connor PJ, Herring MP, Caravalho A. Mental health benefits of strength training in adults. Am J Lifestyle Med. 2010;4(5):377–396.
- Megakli T, Vlachopoulos SP, Thøgersen-Ntoumani C, et al. Impact of aerobic and resistance exercise combination on physical self-perceptions and self-esteem in women with obesity with one-year follow-up. Int J Sport Exerc Psychol. 2017;15(3):236–257.
- Kierkegaard M, Harms-Ringdahl K, Edstrom L, et al. Feasibility and effects of a physical exercise programme in adults with myotonic dystrophy type 1: a randomized controlled pilot study. J Rehabil Med. 2011;43(8):695–702.
- Ansved T. Muscle training in muscular dystrophies. Acta Physiol Scand. 2001;171(3):359–366.
- Petrof BJ. The molecular basis of activity-induced muscle injury in Duchenne muscular dystrophy. Mol Cell Biochem. 1998;179(1-2):111–123.
- Gianola S, Castellini G, Pecoraro V, et al. Effect of muscular exercise on patients with muscular dystrophy: a systematic review and meta-analysis of the literature. Front Neurol. 2020;11:958.
- Lott DJ, Taivassalo T, Cooke KD, et al. Safety, feasibility, and efficacy of strengthening exercise in Duchenne muscular dystrophy. Muscle Nerve. 2021;63(3):320–326.
- Lindsay A, Larson AA, Verma M, et al. Isometric resistance training increases strength and alters histopathology of dystrophin-deficient mouse skeletal muscle. J Appl Physiol. 2019;126(2):363–375.
- Lessard I, Gaboury S, Gagnon C, et al. Effects and acceptability of an individualized home-based 10-week training program in adults with myotonic dystrophy type 1. J Neuromuscul Dis. 2021;8(1):137–149.
- Kontou E, Papadopoulos C, Papadimas G, et al. Effect of exercise training on functional capacity and body composition in myotonic dystrophy type 2 patients. Muscle Nerve. 2021;63(4):477–483.
- Bostock EL, O'Dowd DN, Payton CJ, et al. The effects of resistance exercise training on strength and functional tasks in adults with limb–girdle, Becker and facioscapulohumeral dystrophies. Front Neurol. 2019;10:1216.
- Nakayama T, Kuru S, Okura M, et al. Estimation of net muscle volume in patients with muscular dystrophy using muscle CT for prospective muscle volume analysis: an observational study. BMJ Open. 2013;3(10):e003603.
- Sveen ML, Andersen SP, Ingelsrud LH, et al. Resistance training in patients with limb–girdle and Becker muscular dystrophies. Muscle Nerve. 2013;47(2):163–1699.
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194.
- Hecksteden A, Faude O, Meyer T, et al. How to construct, conduct and analyze an exercise training study. Front Physiol. 2018;9:1007.
- Narici MV, Roi GS, Landoni L, et al. Changes in force, cross-sectional area and neural activation during strength training and detraining of the human quadriceps. Eur J Appl Physiol Occup Physiol. 1989;59(4):310–319.
- Keeler LK, Finkelstein LH, Miller W, et al. Early phase adaptations of traditional speed vs. superslow resistance training on strength and aerobic capacity in sedentary individuals. J Strength Condit Res. 2011;15(3):309–314.
- Tollback A, Eriksson S, Wredenberg A, et al. Effects of high resistance training in patients with myotonic dystrophy. Scand J Rehabil Med. 1999;31:9–16.
- Lindeman E, Leffers P, Spaans F, et al. Strength training in patients with myotonic dystrophy and hereditary motor and sensory neuropathy: a randomized clinical trial. Arch Phys Med Rehabil. 1995;76(7):612–620.
- American College of Sports Medicine. American College of Sports Medicine position stand: progression models in resistance training for healthy adults. Medicine and Science in Sports and Exercise. 2002;341:687.
- Ware JE. SF-36 Health Survey update. Spine. 2000;25(24):3130–3139.
- Sprinkle SD, Lurie D, Insko SL, et al. Criterion validity, severity cut scores, and test–retest reliability of the Beck Depression Inventory—II in a university counseling center sample. J Counsel Psychol. 2002;49(3):381–385.
- Spielberger CD, Gorsuch RL, Lushene RE, et al. Manual for the State-Trait Anxiety Inventory STAI (Form Y). Palo Alto (CA): Consulting Psychologists Press; 1983.
- Rosenberg M. Society and the adolescent self-image. Princeton (NJ): Princeton University Press; 1965.
- Sinclair SJ, Blais MA, Gansler DA, et al. Psychometric properties of the Rosenberg Self-Esteem Scale: overall and across demographic groups living within the United States. Eval Health Prof. 2010;33(1):56–80.
- Fox KR, Corbin CB. The-physical-self-perception profile: development and preliminary validation. J Sport Exerc Psychol. 1989;11(4):408–430.
- Singh NA, Stavrinos TM, Scarbek Y, et al. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol A. 2005;60(6):768–776.
- Tang TZ, DeRubeis RJ, Hollon SD, et al. Personality change during depression treatment: a placebo-controlled trial. Arch Gen Psychiatry. 2009;66(12):1322–1330.