Abstract
Purpose
Individual perspectives of long-term consequences decades after anterior cruciate ligament (ACL) injury are unexplored. We addressed experiences and the impact on life of former athletes >20 years post-ACL injury.
Methods
Individual interviews, analysed using Grounded Theory, were conducted with 18 persons injured mainly during soccer 20–29 years ago.
Results
A theoretical model was developed with the core category Re-orientation towards acceptance, overarching three categories illustrating the long-term process post-injury. Initially the persons felt like disaster had struck; their main recall was strong pain followed by reduced physical ability and fear of movement and re-injury. In the aftermaths of injury, no participant reached the pre-injury level of physical activity. Over the years, they struggled with difficult decisions, such as whether to partake or refrain from different physical activities, often ending-up being less physically active and thereby gaining body weight. Fear of pain and re-injury was however perceived mainly as psychological rather than resulting from physical limitations. Despite negative consequences and adjustments over the years, participants still found their present life situation manageable or even satisfying.
Conclusion
ACL injury rehabilitation should support coping strategies e.g., also related to fear of re-injury and desirable physical activity levels, also with increasing age.
More than 20 years after the ACL injury, the individuals despite re-orientation towards acceptance and a settlement with their life situation, still had fear of both pain and re-injury of the knee, with concerns about physical activity and gaining of body weight.
Patients with ACL injury may need better individual guidance and health advice on how to remain physically active, to find suitable exercises and to maintain a healthy body weight.
Education related to pain, treatment choices, physical activity, injury mechanisms in participatory discussions with the patient about the ACL injury may be beneficial early in the rehabilitation process to avoid catastrophizing and avoidance behaviour.
ACL injury rehabilitation needs to address coping strategies incorporating the psychological aspects of suffering an ACL injury, including fear of movement/secondary injury, in order to support return-to-sport and/or re-orientation over time.
IMPLICATIONS FOR REHABILITATION
Introduction
Rupture of the anterior cruciate ligament (ACL) is one of the most common traumatic knee injuries among physically active individuals, and in particular during sports activities accounting for about 75% of the injuries [Citation1,Citation2]. Injuries are more frequent in males, but females competing in certain sports activities run a 4–6 times higher risk of injury compared to males when participating in the same sports [Citation1]. Beyond the short-term consequences such as joint instability, muscle weakness, fear of re-injury and compromised functional ability [Citation3–7], the injury is also likely to drastically change their life and have an impact in the longer perspective. Many young, very active persons fail to return to the same level of physical activity or competitive sport [Citation2,Citation8,Citation9], and they also face a high risk of developing osteoarthritis [Citation10–12]. Research has addressed the outcome in the long term mostly survey data [Citation13,Citation14], while fewer studies have directly tested the physical performance outcomes in the very long term after injury also in relation to healthy-knee controls [Citation13,Citation15–18]. Altogether, the reports demonstrate consequences even as long as after 20 years or more, such as pain and reduced knee function [Citation5], reduced physical capacity and knee specific activity level [Citation13], decreased muscle strength [Citation15], reduced balance [Citation17,Citation19] and altered coordination in jump performance [Citation16,Citation18], independent of whether treated conservatively with physiotherapy alone [Citation14] or with reconstructive surgery in addition [Citation13,Citation15,Citation19]. In line with this, a recent meta-analysis also revealed impaired knee-related quality of life in ACL-injured individuals five years or more post-injury compared to population norms, and independent of treatment [Citation20]. To date, there is however little evidence on how individuals consider the impact of the injury and how they cope with the consequences over time into middle age or longer.
Treatment of course plays a large role for the experience and for the impact of injury. The preferred treatment strategy (surgery or not, in addition to physiotherapy), particularly with regards to the long-term outcomes is still under debate [Citation21,Citation22] and preferred treatment vary in different countries [Citation1,Citation23]. In either case, the rehabilitation programme is considered crucial for a successful return to sport [Citation24]. Further, as of today it is well known that suffering an ACL injury also is likely to lead to psychological consequences such as loss of identity or fear of re-injury preventing participation in sports or other physical activities [Citation25–28]. The belief in one’s own ability and general self-confidence may also gradually decrease over time, especially without support. Restoring psychological confidence may indeed be more difficult and time-consuming than restoring physical capacity [Citation25,Citation27,Citation28], and there may be gender-specific issues [Citation25,Citation29]. The existing qualitative studies have foremost addressed the process and outcome of suffering an ACL injury up to a few years post-injury [Citation30,Citation31], also in those who did not have surgery [Citation31]. Additional studies on the other hand provide perspectives 5–20 years after injury [Citation32,Citation33]. Ezzat et al. [Citation33] especially pointed out how a knee injury during the adolescent years can have a significant and long-lasting impact on life. The very long-term subjective experience of the injury after more than 20 years, including the subsequent rehabilitation process and the consequences of injury, have to our knowledge not been reported.
The present paper therefor aims to explore the retrospective experiences of suffering an ACL injury, treatment decisions, the individual rehabilitation process and the personal consequences and implications after 20 years or more post-injury. Such knowledge might shed important light on key issues for successful rehabilitation in the long term following ACL injury and prognostic factors for coping with an ACL injury across the life span.
Methods
Study design and participants
This study used a qualitative study design in which individual interviews with persons who had suffered an ACL injury were conducted and analysed using the Grounded Theory (GT) method of constant comparisons [Citation34,Citation35]. GT is considered especially useful when illustrating a process over a longer period, as well as studying complex factors that influence health and illness [Citation36]. A result grounded in data can lead to a development of a theoretical model and conceptualize the studied phenomenon to understand it in more abstract terms.
Participants were recruited via a research programme involving a long-term follow-up of ACL-injured persons in northern Sweden. The programme addressed knee function, osteoarthritis and quality of life on average more than 23 years after an ACL injury (KACL20 study; [Citation13,Citation15]). In order to achieve a rich variation in the present sample, participants were chosen through purposive sampling from the larger programme cohort of 113 persons injured between 17 and 31 years ago, and represented both males and females, different ages at the time of injury and at present, and treated with either physiotherapy in combination with reconstructive surgery or physiotherapy alone. In total 23 persons were asked to participate, of which five declined. The final study sample thus consisted of 18 participants; eight females and ten males between 36 and 56 years of age and injured between 20 and 29 years ago (). All participants were injured during sports activities, (all except one were injured in soccer), and nine persons had been treated with physiotherapy in combination with reconstructive surgery while the remaining persons had physiotherapy only. The first four participants we interviewed had been treated with reconstructive surgery, three of them females, injured at young age. Additional information was considered needed and we recruited more males treated with reconstructive surgery. After that we interviewed participants, both females and males, who had not had an ACL reconstruction. The last recruitment aimed for males who had been injured at young age. Prior to data collection, the participants signed a consent form after having received verbal and written information about the study. The study was approved by the Regional Ethical Review Board, Umeå, Sweden, (Dnr 08–211 M).
Table 1. Background information of the participants who were all sports athletes. Participant nr 5 was injured in downhill skiing while all the other participants were injured in soccer.
Data collection
The interviews were conducted by three of the authors (AF, KS, ML), all physiotherapists; two with experience of ACL rehabilitation (KS, ML) and two with expertise of qualitative methods (AF, KS). The interviewers were not acquainted with any of the participants, nor had they taken any part in their rehabilitation. The interviews lasted between 30 and 55 min and were carried out in a quiet place chosen by the participants. All interviews were audio-recorded and transcribed verbatim.
A semi-structured interview guide was developed by firstly carrying out three test interviews that were not included in the final study. This information resulted in questions grouped into four themes; the ACL injury and the rehabilitation process in relation to “physical activity,” “social life,” “work life” and “the future.” In the theme “physical activity” the participants were asked to describe the impact of the injury, their experience of knee function in general and in particular during physical activity over the years. Regarding “social life” the participants were asked to reflect upon how the injury had influenced their social life, both family and friends up until the present day. To which extent the ACL injury had had an impact upon their career was accounted for under the theme “work life” and finally, under the theme “the future” the participants were encouraged to share their thoughts and concerns about the future, if any, in relation to their knee function. The same interview guide was used throughout the entire study and most often supplementary questions were asked, allowing further exploration of issues that were raised during the interviews.
Data analysis
Data collection and analysis were made in parallel, and all interviews were carefully and repeatedly read as a whole and in parts during the analytic procedure. Ideas that came up, related to the emerging results, were continuously written down in memos used in the analysis. During all steps of the analysis, all analysing authors independently performed the initial coding, followed by a mutual comparison and a final common negotiated outcome. The emerging final result was discussed repeatedly among the whole research team, and triangulation between authors was used to increase trustworthiness [Citation36].
The analysis started with an open coding, implying that each interview was read line-by-line and paragraph by paragraph and coded independently by two or three of the researchers (AF, KS, ML) and important information was coded relating to the text. The data program Open Code was used to facilitate the coding process (Umeå University, Department of Epidemiology). In the next step, the selective coding, codes with similar content were compiled to categories on a more abstract level and a core category which was central to all data was identified. In the last step, the axial coding, the categories were compared on how they related to each other and linked in a process over time, (after the ACL injury). In doing so, the three categories together with the core category were made for conceptualizing the process as a theoretical model. The model illustrates the participants’ experiences of suffering an ACL injury and its’ consequences in a long-term perspective. The model is further integrated with existing concepts and theories in the discussion.
Results
The analysis resulted in the core category Re-orientation towards acceptance and illustrates the process that the participants went through after the ACL injury. We here present a theoretical model, including three categories that characterise the re-orientation and that also reflect the different phases throughout the long-term process; Disaster striking, Constant considering and Coming to terms (, ). These three phases often overlapped and the time in each phase was not equal for all participants. Nevertheless, the experience and thus expressions of every participant reflected elements of all three phases. The phases are illustrated in , including representative examples of codes for each phase. Several quotes from the interviews are presented below in the categories delineating each phase and providing illustrations of the content.
Figure 1. Model of retrospective experiences of the process following having suffered an ACL injury and the perceived long term consequences.
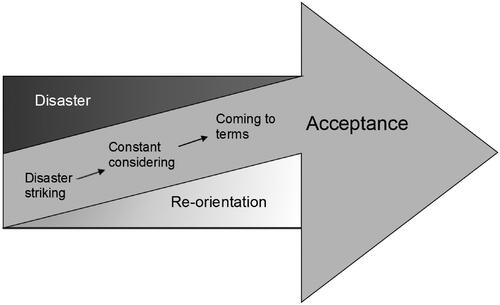
Table 2. Examples of quotes, codes, categories and core category emerging from the Grounded Theory analysis of retrospective experiences of suffering an ACL injury, seen in the long term after about 20 years or more.
Re-orientation towards acceptance
Over the years there was a long process of coming to terms with and accepting the consequences of the injury, finding suitable physical activities and new arenas of socializing, and the re-orientation in life. At the time of injury the participants felt like disaster had struck, and their main recall was strong pain, subsequently followed by reduced ability to move as they had been used to and strong fear of movement stemming both from pain and fear of being injured, all of which changed their life completely and abruptly. The participants’ passion for being physically active and engagement in their sports helped them through the rehabilitation process. However, none of the participants were able to return to their pre-injury level of physical activity, or to reach their desired level of activity. Some repeatedly tried to resume their former sports careers and succeeded for a period of time, while others ended it immediately because of re-injury. Over time the participants became less and less physically active. They struggled with difficult decisions, considering which physical activities to refrain from, and if partaking, often ending up choosing “safe” activities in order to avoid the fear of both pain and re-injury. The participants encountered problems finding desirable and acceptable physical activities and wanted more support for that from their physiotherapists. Participants reported that they gained weight and believed their reduced physical activity to be a causal factor. The participants were very conscious about their weight gain and motivated to lose weight but lacked guidance from physiotherapists. With increasing age, the participants chose physical activities that were less challenging and in particular less demanding for the knee, lowered their physical ambitions and reluctantly adapted to a physical activity level which they felt was of an average person of contemporary age where they felt as an average person of a contemporary age. The participants had slowly adjusted their knee-demanding activities and now in their forties found the situation manageable and their current life situation satisfactory despite the life changes.
Disaster striking
The initial phase, Disaster striking, illustrates the immediate time period following the injury, when the trauma had a major physical and mental impact on the participants. At the time of the interview many years post-injury, the participants still very clearly remembered the injury and its’ early consequences. An immediate conspicuous strong pain was often the participants’ first recall. The injury had happened so fast. The participants conveyed a retrospective view that their perception of their whole life situation changed dramatically in a few seconds. Not knowing the severity of the injury and its’ future consequences caused feelings of concern and worry.
During a soccer game, the field was wet, there was a fight over the ball, I was hit and I rotated my right leg and the foot was stuck so…I tore my knee …an extreme pain! It was the worst pain I have ever experienced. (Male, 23 years at injury, non-operated)
You weren’t exactly thrilled about getting your life ruined, because that’s what it felt like. (Female, 15 years at injury, non-operated)
The lack of insight of how severe the injury was led to energy-consuming anxiety for the participants, something that they in retrospect felt could have been avoided by better individual support from the healthcare service. An important issue for several of the participants in the acute phase was, to discuss more in depth whether to have re-constructive surgery or not. The females who were injured in their early teens particularly perceived that they had not been part of such discussions. In either case, these participants perceived that the physicians took a decision without consulting them sufficiently. However, females injured at an older age and males felt that they had participated in the decision together with the physician and were confident with their choice.
Person: It was so sad… (crying)
Interviewer: Did you have someone to talk to about the injury?
Person: Nobody…
Interviewer: Did you have any support?
Person: No…only from my family, nobody else…no…
(Female, 15 years at injury, non-operated)
This happened in 19xx… there was a discussion… I was with my physician, he is my “guru” when it comes to my knee, we discussed whether to operate or not, but decided to not operate. (Female, 22 years at injury, non-operated)
The injury resulted in decreased ability to move, which was perceived as sad and difficult to accept. At the time of the injury sports was an important part of the participants’ lives, and accounted for much of their leisure time and social context. Some participants were forced to end their sports career soon after the injury, while others tried repeatedly to return to their former sports activity and level but failed because of re-injury, whereas some succeeded to a certain extent.
I had to quit everything (after the injury). All sport, it was really sad. I was only 15 years old … county team in volleyball … but I had to give up (Female, 15 years at injury, operated)
It was the physicians who … it was just to give up. It was just… “quit with this (soccer).” It was really upsetting … I was so young so I didn’t know any better … this with surgery … if it would have helped so I could have become more physically active …. this is what I think about a lot, if it could have made the situation different as of today?(Female, 15 years at injury, non-operated)
Then I went back to work and also performed rehabilitation exercises for 6 months, three times a week. And then I played soccer for seven more years [not at the pre-injury level of activity/soccer]. But eventually when it happened … when after 12–13 times the knee dislocated, I quit. I stopped when I was just over 35 years old. You have to quit some time. (Male, 28 years at injury, non-operated)
Constant considering
This phase concerns how the participants dealt psychologically and socially with the ACL injury and its’ consequences and how they were forced to make changes and alternative choices in their lives. The reason for many of these lifestyle modifications was fear of both pain and re-injury. The fear did not, however, stem from actual physical limitations, but related mainly to psychological barriers and a fear of re-injury with the accompanying pain. The participants knew that the knee was stable enough to perform physical and specific sports activities but they could not overcome the fear. The fear was still present a long time after the injury occurred and resulted in a mental barrier where the belief that they were going to suffer a re-injury was so strong that the participants avoided certain physical activities. If they ever decided to overcome their fear it was because they wanted to participate in activities together with their families. The participants described a constant consideration of the risk of re-injury when challenged to do physical activity, in relation to the pleasure of performing it. They by the time decided to avoid risky activities and chose instead “safe” activities that they could somehow control to a greater extent.
… you are afraid to … to get re-injured, quite easily. That it (the knee) is going to get injured so you will hurt yourself. That’s probably what makes it limiting and you don’t really do what you like to do. It’s probably in my head a lot. I have missed a great deal over the years by saying … "no, I can’t do that because my knee might not cope.” (Male, 23 years at injury, operated)
But then there is a risk that you avoid things just because you somehow already have decided that you can’t do it. That it actually is more up here (pointing to her head) than in the knee. So it’s a balancing act where you’ve thought, come on, you could at least try jogging. (Female, 15 years at injury, non-operated)
Besides the pleasure of being physically active, sports had filled a social need, since many of their friends were involved in the same sport. The females who were injured during their early teen years particularly experienced a social loss and difficulties in maintaining contact with friends who were involved in the same sport or team. They described a sensation of becoming an outsider and the sorrow of sitting on the side being merely a spectator as well as having to end their sports career.
It was the circle of friends you had when you were training… My friends were in the soccer team so it was really sad when it didn’t work out any longer. You had to find other interests …You still had your friends, but they were out in the evenings, at practice. (Female, 22 years at injury, operated)
This was not as notable for the males, or the females injured at an older age. Some participants returned to their sport after the rehabilitation, while others found a new role and became coaches in the team or just stayed around the team to maintain their social contacts.
Then I chose to become a coach instead. I started to train a boys’ team. I did that for two or three years. Then we had our own children and when they grew up there was soccer training. I coached them for 10 years. I was also coach for another team … you don’t just let go … I missed the chit-chat in the locker room and prior to the games … it didn’t become just my team. This was my remaining contact with soccer then. (Male, 23 years at injury, non-operated)
The feeling of being limited, including the impression of being left out due to physical limitations, also occurred later in life in the longer perspective in for example social gatherings with work or friends. Sometimes it was perceived as manageable and other times it was associated with frustration and bitterness. In family contexts as of today some participants felt limited and it spilled over to their family situation. This often had to do with restricting their own children’s physical activities due to the participants’ own negative experiences. Other participants encouraged their children to engage in physical activities and sports that the children felt were fun and enjoyed.
What if your child suddenly wants to go downhill when they’re ten, can I go with them? Should I go? You may have to be involved in the choice of sports. Will I deny my child activities because I cannot cope with them myself any longer? (Female, 13 years at injury, operated)
None of the participants were able to perform physical activity to the same level as before their injury. They had problems finding desirable and acceptable physical activities and wanted more support from physiotherapists to find suitable ways of staying active.
Maybe it’s mental … I don’t know…I practice downhill skiing, I can’t play soccer, I can’t play floorball, I can’t play tennis … all these rapid (movements). (Male, 23 years at injury, non-operated)
If I could train in a group … it would be easier to train in a group, to get (support), it is difficult to do it yourself. Or get a training programme or home excises that I know are helpful, from a physiotherapist, I can easily do it at home, half an hour, every day … if I got a manual which would be helpful. (Male, 23 at injury, non-operated)
Over time, when the consequences of the injury became more and more evident, the participants became less and less physically active and put on weight gradually. Many years after the injury the participants still battled against their weight gain and were now very motivated to lose weight. Looking back, they would have liked to have had guidance on diet and weight control exercise, something that was not provided by the health care services.
Suddenly I had a lot of time, I didn’t do much…watched tv. I gained weight…now I can see I gained 4–5 kilos … and not until after being 30 I realised “why do I carry around these extra kilos?”(Female, 18 years at injury, operated)
Two years after I had quit playing soccer (due to the injury) I had gained 18 kilos. I was less physically active and ate the same amount as when I was physically active …it’s bad for the knee. (Male, 20 years at injury, operated)
I really would like to run, but it feels like I’m too heavy now… I slowly gained weight…it started soon after I stooped training. I trained three, four or five times a week before and then … nothing or rehab training that wasn’t so physical. I have tried repeatedly to lose weight but failed, I don’t know what to do. (Female, 15 years at injury, operated)
Coming to terms
The phase Coming to terms was characterized by the participants reporting that they more or less accepted their situation and the restrictions that the ACL injury caused. It was considered important to have a positive attitude and to be determined to make the best of the situation. This conviction made it easier to accept the new life situation. Instead of wondering about what could have been, the focus of the participants was more on realistic expectations.
You have accepted your lot, so to speak. So you live with it, because it, somehow, works out socially. (Male, 23 years at injury, non-operated)
In order to avoid knee pain, to achieve better knee function and to feel more secure and stable in certain knee loading activities, the participants continued with regular knee-specific training and less demanding physical activities. For example, soccer was replaced by walking, and running was replaced by cycling.
From the time of the injury til now I have had proper knee rehabilitation, four rehabilitation periods with training for my knee and my injury. (Female, 22 years at injury, operated)
You find different values. I’m running, I go downhill skiing, some cross-country skiing…I would like to … in fact I have tried… but I am so afraid… I know that playing soccer doesn’t work. You have to find other solutions. (Male, 23 years at injury, operated)
Running was too much for the knee… I have tried to choose other activities, cycling, spinning, aqua gym to get this… to get tired. Depending on the knee function I have adjusted my activities, it’s been very successful. (Female, 22 years at injury, non-operated)
Growing older could also imply finding other important activities and values in life. The participants had reached an age where socialising was no longer through physical activity and sports to the same extent but could be through other activities, for example, related to their children’s activities. When doing so they felt more like “everybody else.” Even though the consequences of the injury had negatively affected the participants’ lives in many ways they still, some to a greater extent than others, were quite content with their current life situations.
I started to understand that there are other things in life, not only sports. You start thinking about the future … Yes I am positive, I don’t have any problems. The only thing is to not gain weight, to keep up with training and no soccer. No more competitions. (Male, 20 years at injury, non-operated)
I’m still physically active but I have chosen other sports compared to when I was injured…it was mainly soccer, now it is more about fitness. You grow older (laughing) you have to accept it sometime. (Male, 24 years at injury, non-operated)
Discussion
While previous research mainly addresses the process and outcome up until the first few years after ACL injury, this report presents the long-term perspectives of suffering an ACL injury and the subsequent rehabilitation process. It encompasses the personal consequences including how life is experienced as of today when the participants are roughly in their forties or fifties. The participants reported that they had faced both physical and mental challenges throughout the years, even up until the present day. Despite this, they had been able to handle the subsequent challenges and to retain a generally positive attitude. Thus, they were able to re-orient towards acceptance and were at the time of the study mostly quite content with their current life situations. Despite fear of pain and re-injury, and while having to make life adjustments because of the knee injury, their life situation as of today was manageable.
The significance of acceptance is supported by Ezzat et al. [Citation33] who investigated attitudes and beliefs about physical activity and the development of post-traumatic osteoarthritis in young adults after knee injury. The results show that the knee injury had a substantial and long lasting impact on the young adults’ physical abilities in sport. They accepted, to a varying degree, the consequences of the injury and they made adjustments regarding their physical activity participation. This is also in line with the main results in our study. Acceptance is an important and growingly used concept in pain rehabilitation, yet complex and with varying definitions [Citation37]. In individuals with long-term pain, it has been described as a personal and individualized process with varying degrees of resistance to or readiness for acceptance [Citation38]. Acceptance was an integral part of the (rehabilitation) process moving forward from a pain-focused life towards a meaningful life, despite the pain. Acceptance was more than coming to terms with pain, it implied getting back on track in life through making choices and active change [Citation38], which was also evident for the participants in our study.
Both physical and mental aspects during rehabilitation have been highlighted in previous research [Citation25–30], and indicating quite a long process in restoring confidence in movement ability which is essential in order to promote an active lifestyle. According to Antonovsky’s [Citation39] concept ‘sense of coherence’ (SOC), persons suffering from both physical and mental stress can still experience good health. SOC consists of three factors: comprehensibility, a sense of understanding events in your life, manageability, a belief that you have the necessary resources to take care of things and meaningfulness, a sense of feeling involved and having important things in life as a source of satisfaction. Based on our participants’ experiences of the onset of injury and the time period following the injury, their initial SOC seemed to be quite low and especially their manageability, since the participants had not yet had the time to develop resources to cope with what had happened. Over time, the participants expressed how their strategies to cope developed and at the time of the interviews they had gradually accepted the consequences of the injury, and their SOC was evidently higher compared to when the injury occurred, or than in the beginning of the rehabilitation process.
Mental recovery after an ACL injury appears to take a longer time than the physical recovery [Citation27–29], which was also evident in our participants. Even 20 years or more after the injury, there was still fear of both pain and re-injury. Psychological, social and contextual factors are influential in all phases (direct after injury, during rehabilitation, and long term) of a traumatic sport-related knee injury. A clinical understanding of the importance of these factors during all phases may facilitate management of the injury and promote return to sport and thus leading to higher health-related quality of life [Citation40]. The participants in our study described their fear as their main barrier to greater physical activity and how they gave up on certain physical activities without even trying. Fear of pain and re-injury are common after an ACL injury and can be a hindrance for returning to sports even in young persons in the first year after injury [Citation5,Citation6] and can also cause difficulties during rehabilitation. The fear-avoidance model [Citation41] may offer an explanation how people who suffer an injury may start catastrophizing, which may lead to fear of pain and re-injury/movement and avoidance behaviour. This is more common in people with knee osteoarthritis following ACL reconstruction, compared to those without osteoarthritis [Citation42] and it was also reported by some of our participants. Avoidance behaviour can turn into a vicious circle, excluding one activity after another leading to conservation of fear, less physical activity, increased pain, deconditioning and disuse of the body and disability [Citation41]. Therefore, adapting a broad multimodal approach in the rehabilitation process, provided by a multidisciplinary team with shared common goals, addressing both physical and psychological factors seem to be crucial for successful rehabilitation.
Our participants’ mental health was negatively affected by the feeling of being an outsider, no longer involved in the team and thus without teammates. This could also have contributed to low meaningfulness [Citation39]. Belonging to a team has a big social impact on the individual, and loosing that context of being a part of the team creates frustration, loneliness and a sense of being forgotten implying an altered social identity [Citation25]. As a consequence, the injured person may feel like an outsider if not able to participate in important decisions in their sports team or their health care for example. This was the case among our participants who reported a lack of involvement in decisions such as whether to be operated or not, particularly for the females injured at a young age. Having an active role in all rehabilitation phases is highly valued by injured athletes, including engaging in decision making and being respected [Citation40]. Patients also appear to have more confidence in surgical treatment compared to conservative treatment when it comes to regaining function in the injured knee [Citation30], and believe that surgical treatment is associated with an improved likelihood of returning to the previous level of sport [Citation26].
Incentives for clinical progress in ACL injury rehabilitation
Our participants experienced lack of guidance from the physiotherapists on how to remain physically active, to find suitable exercises and to maintain a healthy weight. Increased body mass index has been demonstrated to be related to worse quality of life and more depressive symptoms in the long term (5–20 years) following ACL injury [Citation43]. Others have also emphasized the need to implement current evidence in rehabilitation programs to improve long-term outcome post-ACL injury [Citation44], since only ∼60% make a full recovery [Citation2] and more than 50% develop osteoarthritis [Citation10]. Thing [Citation25] emphasized the need for personal guidance and health advice during the rehabilitation process after an ACL injury. Integration of Cognitive behavioral therapy (CBT) in physiotherapy programs has shown good results for recovery of persons with pain and fear avoidance in other musculoskeletal conditions [Citation45]. Educating and explaining for example pain and stress mechanisms and having participatory discussions with the patient (psychoeducation) about the ACL injury and the planned rehabilitation may be beneficial early in the rehabilitation process to avoid catastrophizing and avoidance behaviour. For instance, the perceived personal importance of exercise has been demonstrated crucial in influencing activity levels following ACL reconstruction [Citation46]. Such psychoeducation with an active role of the patient should be promoted by physicians and physiotherapists to probe the patient’s feelings and reporting of (maladaptive) thoughts about the ACL injury in order to detect possible avoidance behaviour. Fear of reinjury/avoidance may be diagnosed using clinical tools such as the Tampa Scale for Kinesiophobia [Citation47]. If fear of movement and re-injury have already become evident, graded exposure activity may be effective as treatment [Citation48]. Acceptance and Commitment Therapy (ACT), stemming from CBT, may also be integrated in physiotherapy treatment [Citation49]. ACT focuses on the importance of living a good, meaningful life and at the same time accepting challenges and suffering such as accepting thoughts connected to a traumatic knee injury, fear of pain, movement and re-injury. ACT may help individuals to shift focus from struggling to control pain and to relate to pain and fear in a more flexible way leading to increased activity and physical functioning. ACT for treatment of long-term pain has shown promising evidence but more research is needed [Citation50].
Strengths and limitations
The trustworthiness of our results needs to be discussed. In order to elucidate the participants’ experiences of an ACL injury, from a broad perspective including varied views, we aimed for a rich variation in the sample, which we consider was achieved. The interviews addressed a long time period which can be both a strength and a weakness. Participants were both females and males, of different ages at onset of injury, and treated with either physiotherapy in combination with reconstructive surgery or physiotherapy alone. The participants were active in sports when they suffered their injury, which may explain why so much of the result is related to sports. Sports were an important part of the participants’ lives when they were injured and have remained so for many of them, even if they have ended their own careers as athletes. On the other hand, all of our participants except one were injured in soccer, and we also had few young males. We however included both individuals who had surgery and those who had not, which is representative for current national context, ∼ half of the injured persons in Sweden get reconstruction (https://aclregister.nu), while in other countries e.g., US, reconstruction is much more common. All these factors may affect the transferability of our results.
Our interview guide was discussed and decided upon by all authors after pilot interviews. Triangulation between authors [Citation35] was used, which is likely to have contributed to a more nuanced discussion and data analysis since the authors have diverse backgrounds and experiences. The insider perspective [Citation35] was represented by (ML, CH) who are clinically active as physiotherapists working with ACL-injured patients and by (KS, CH) who have solid experience of research regarding ACL injuries. The outsider and methodological perspectives were represented by (AF, KS) who have extensive experience of qualitative methods and occupational health (AF). The fact that almost all of the authors have experiences from the field in question may be an advantage as well as a disadvantage. Being familiar with what it means to suffer an ACL injury, as well as the treatment and rehabilitation procedures, made it easier to understand the data but may also lead to less objectivity. The authors were not acquainted in any way with the participants, which prevented bias in the data by way of personal relations. The results have been thoroughly discussed between all authors as well as with other groups of researchers who found the results to be credible. Therefore, we consider our findings to be trustworthy.
Conclusions
An ACL injury affects the individual both physically and mentally, in the short term and the long term, leading to adjustments in terms of physical activities, leisure activities and social life [Citation13,Citation15,Citation18,Citation28,Citation31]. Our study explores how persons who have suffered an ACL injury experience the course of the injury and their life situation over the years up until about 20 years later, and thus how the injury has influenced their life in the long term. The injury and its’ consequences were most difficult to deal with during the initial years after the injury, when the sorrow and sense of alienation were most evident, particularly in relation to giving up sports. More than 20 years after the injury, the individuals had re-oriented towards acceptance and were after all quite content with their life situation despite remaining fear of both pain and re-injury of the knee, and concerns about physical activity and gaining body weight. The experiences called for better guidance from the health care in this context. Further research on the psychological aspects of suffering an ACL injury is needed in order to enhance the rehabilitation outcome and support re-orientation when necessary.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Nordenvall R, Bahmanyar S, Adami J, et al. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40(8):1808–1813.
- Ardern CL, Taylor NF, Feller JA, et al. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48.
- Pernin J, Verdonk P, Si Selmi TA, et al. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010;38(6):1094–1102.
- Nebelung W, Wuschech H. Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21(6):696–702.
- Wierike SCM, Ven der Sluis A, van den Akker-Scheek I, et al. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sports. 2013;23:527–540.
- Lentz T, Zeppieri G, Jr George S, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43(2):345–353.
- Ardern CL, Taylor NF, Feller JA, et al. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and Meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552.
- Ardern CL, Webster KE, Taylor NF, et al. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and Meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606.
- Lai CC, Ardern CL, Feller JA, et al. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with Meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138.
- Lie MM, Risberg MA, Storheim K, et al. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019;53(18):1162–1167.
- Ajuied A, Wong F, Smith C, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and Meta-analysis. Am J Sports Med. 2014;42(9):2242–2252.
- Poulsen E, Goncalves GH, Bricca A, et al. Knee osteoarthritis risk is increased 4–6 fold after knee injury – a systematic review and meta-analysis. Br J Sports Med. 2019;53(23):1454–1463.
- Tengman E, Brax Olofsson L, Nilsson KG, et al. Anterior cruciate ligament injury after more than 20 years: I. Physical activity level and knee function. Scand J Med Sci Sport. 2014;24:6 e491–e500.
- Konrads C, Reppenhagen S, Belder D, et al. Long-term outcome of anterior cruciate ligament tear without reconstruction: a longitudinal prospective study. Int Orthop. 2016;40(11):2325–2330.
- Tengman E, Brax Olofsson L, Stensdotter AK, et al. Anterior cruciate ligament injury after more than 20 years: II. Concentric and eccentric knee muscle strength. Scand J Med Sci Sport. 2014;24:6 e501–e509.
- Markström J, Tengman E, Häger C. ACL-reconstructed and ACL-deficient individuals show differentiated trunk, hip, and knee kinematics during vertical hops more than 20 years post-injury. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):358–367.
- Stensdotter A-K, Tengman E, Brax Olofsson L, et al. Deficits in single-limb stance more than 20 years after ACL injury. Eur J Physiother. 2013;15(2):78–78.
- Tengman E, Grip H, Stensdotter AK, et al. Anterior cruciate ligament injury about 20 years post-treatment: a kinematic analysis of one-leg hop. Scand J Med Sci Sports. 2015;25(6):818–827.
- Negahban H, Mazaheri M, Kingma I, et al. A systematic review of postural control during single-leg stance in patients with untreated anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22(7):1491–1504.
- Filbay S, Culvenor AG, Ackerman IN, et al. Quality of life in anterior cruciate ligament-deficient individuals: a systematic review and Meta-analysis. Br J Sports Med. 2015;49(16):1033–1041.
- Brukner P, Khan K. Clinical sports medicine. 3rd ed. Sydney: McGraw-Hill; 2007.
- Frobell RB, Roos HP, Roos EM, et al. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013;346:f232.
- Failla MJ, Arundale AJH, Logerstedt DS, et al. Controversies in knee rehabilitation: anterior cruciate ligament injury. Clin Sports Med. 2015;34(2):301–312.
- Kyritis P, Witvrouw E. Return to sport after anterior cruciate ligament reconstruction: a literature review. J Nov Physiother. 2014;41:93.
- Thing L. Voices of the broken body the resumption of non-professional female players’ sports careers after anterior cruciate ligament injury. The female player's dilemma: is she willing to run the risk? Scand J Med Sci Sports. 2006;16(5):364–375.
- Heijne A, Axelsson K, Werner S, et al. Rehabilitation and recovery after anterior cruciate ligament reconstruction: patients’ experiences. Scand J Med Sci Sports. 2008;18(3):325–335.
- Olofsson L, Fjellman-Wiklund A, Söderman K. From loss towards restoration: experiences from anterior cruciate ligament injury. Adv Physiother. 2010;12(1):50–57.
- Scott SM, Perry MA, Sole G. Not always a straight path: patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil Rehabil. 2018;40(19):2311–2317.
- Fältström A, Hägglund M, Kvist J. Factors associated with playing football after anterior cruciate ligament reconstruction in female football players. Scand J Med Sci Sports. 2016;26(11):1343–1352.
- Thorstensson C, Lohmander L, Frobell R, et al. Choosing surgery: patients’ preferences within a trial of treatments for anterior cruciate ligament injury: a qualitative study. BMC Musculoskelet Disord. 2009;10:100.
- Österberg A, Kvist J, Dahlgren AM. Ways of experiencing participation and factors affecting the activity level after non-reconstructed anterior cruciate ligament injury: a qualitative study. J Orthoped Sports Physical Ther. 2013;43(3):17–183.
- Filbay SR, Crossley KM, Ackerman IN. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: a qualitative study. J Physiother. 2016;62(2):103–110.
- Ezzat AM, Brussoni M, Whittaker JL, et al. A qualitative investigation of the attitudes and beliefs about physical activity and post-traumatic osteoarthritis in young adults 3–10 years after an intra-articular knee injury. Phys Ther Sport. 2018;32:98–108.
- Bryant A, Charmaz K. (eds). The Sage handbook of grounded theory. Los Angeles: SAGE Publications; 2007.
- Dahlgren L, Emmelin M, Winkvist A. Qualitative methodology for international public health. 2. ed. Umeå: Epidemiology and Public Health Sciences, Department of Public Health and Clinical Medicine, Umeå University; 2007.
- Strauss AL, Corbin JM. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks, Calif.: SAGE: 1998.
- Lauwerier LC, Van Damme S, Goubert L, et al. Acceptance: what’s in a name? A content analysis of acceptance instruments in individuals with chronic pain. J Pain. 2015;16(4):306–317.
- Biguet G, Nilsson Wikmar L, Bullington J, et al. Meanings of “acceptance” for patients with long-term pain when starting rehabilitation. Disabil Rehabil. 2016;38(13):1257–1267.
- Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med. 1993;36(6):725–733.
- Truong L, Mosewich A, Holt C, et al. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br J Sports Med. 2020;54(19):1149–1156.
- Vlaeyen JW, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153(6):1144–1147.
- Hart HF, Collins NJ, Ackland DC, et al. Is impaired knee confidence related to worse kinesiophobia, symptoms, and physical function in people with knee osteoarthritis after anterior cruciate ligament reconstruction? J Sci Med Sport. 2015;18(5):512–517.
- Filbay SR, Ackerman IN, Russell TG, et al. Return to sport matters-longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sports. 2017;27(5):514–524.
- Risberg MA, Grindem H, Øiestad BE. We need to implement current evidence in early rehabilitation programs to improve long-term outcome after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2016;46(9):710–713.
- Brunner E, De Herdt A, Minguet P, et al. Can cognitive behavioural therapy based strategies be integrated into physiotherapy for the prevention of chronic low back pain? A systematic review. Disabil Rehabil. 2013;35(1):1–10.
- Gignac MA, Cao X, Ramanathan S, et al. Perceived personal importance of exercise and fears of re-injury: a longitudinal study of psychological factors related to activity after anterior cruciate ligament reconstruction. BMC Sports Sci Med Rehabil. 2015;7:4. eCollection.
- George SZ, Lentz TA, Zeppieri G, et al. Analysis of shortened versions of the tampa scale for kinesiophobia and pain catastrophizing scale for patients after anterior cruciate ligament reconstruction. Clin J Pain. 2012;28(1):73–80.
- Vlaeyen J, Morley S, Linton SJ, et al. Pain-related fear: exposure-based treatment for chronic pain. Seattle: IASP Press: 2012.
- Hayes SC, Luoma JB, Masuda A, et al. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25.
- Hughes LS, Clark J, Colclough JA, et al. Acceptance and commitment therapy (ACT) for chronic pain: a systematic review and Meta-analyses. Clin J Pain. 2017;3(6):552–568.
