Abstract
Purpose
Achondroplasia (ACH) is the most common form of skeletal dysplasia, resulting in disproportionate short stature and medical complications. We review the literature on physical functioning, psychosocial function, and quality of life (QoL) in ACH individuals compared to average stature individuals or other short stature conditions. Studies that assess the association between these outcomes and height, limb length/lengthening surgery in ACH patients are also summarized.
Materials and methods
PubMed/MEDLINE and Embase were searched through April 2021. Study inclusion criteria were: (1) quantitative design; (2) study population consisting solely/mainly of ACH patients; (3) reports of physical functioning, psychosocial functioning, and/or QoL. Included studies were summarized separately for pediatric and adult populations.
Results
Of 1664 records identified, 23 primary studies (sample size 8–437 participants) were included. Multiple tools were used across studies, including the generic PedsQL and SF-36 and height-specific QoLISSY.
Conclusions
The literature demonstrates that ACH patients experience limitations in physical functioning and poorer QoL outcomes compared to average stature people across the life span. This appeared to be at least in part due to disproportionate short stature. Future research to better characterize QoL in ACH patients will assist clinicians to better evaluate the effectiveness of management programs including novel interventions.
Patients with achondroplasia experience limitations in physical functioning and poorer quality of life throughout their life course when compared to average statured individuals.
Psychosocial issues are also heightened in adults with achondroplasia compared to average statured peers but are observed less frequently in children and adolescents with achondroplasia.
The overall impact that limb lengthening has on physical functioning and QoL remains unclear, although there is some evidence that greater height or upper limb length may lead to an improvement in these parameters.
Rehabilitation professionals should regularly assess physical functioning, psychosocial wellbeing, and quality of life in individuals with achondroplasia using condition-specific tools.
IMPLICATIONS FOR REHABILITATION
Introduction
Achondroplasia (ACH) is the most common type of skeletal dysplasia with a prevalence of approximately 1 in 25 000 live births worldwide [Citation1–4]. It is an autosomal dominant disorder with the majority of cases (>95%) related to a mutation (gly380Arg) in the gene encoding for fibroblast growth receptor 3 (FGFR3) [Citation1,Citation5]. The most obvious clinical feature of achondroplasia (ACH) is severe short stature (approximately −6 height standard deviation score [SDS] versus average stature per World Health Organization [WHO] adult height reference) with disproportionate bone growth manifesting as a long narrow trunk and rhizomelic shortening of the proximal part of the arms and legs [Citation6–8]. In addition to the core clinical feature of disproportionate short stature, the impaired endochondral skeletal growth in ACH manifests in multiple bone growth related morbidities such as leg bowing (or genu varum), foramen magnum stenosis and cervicomedullary compression, spinal curvature and stenosis, hydrocephalus, obstructive sleep apnea and recurrent otitis media [Citation1,Citation6,Citation9,Citation10]. The resultant short stature, shortened limbs, and medical complications substantially impact both physical and psychosocial aspects of daily life, and consequently patient quality of life (QoL), starting from a very early age [Citation8,Citation10]. Specific physical manifestations include functional limitations or decreased level of independence in carrying out activities of daily living (ADLs), such as grooming, bathing, grocery shopping, preparing meals, and climbing stairs [Citation11], while psychosocial function can be negatively impacted by depression, anxiety, low self-esteem, problems with peer relationships (e.g. bullying) and other behavioral and emotional problems.
Various studies have considered the association between stature/height, or changes in height (due to treatment) and QoL outcomes in the general population and other short stature conditions [Citation12–16]. Marked reductions in QoL scores were observed in individuals with height deficits −2 to −3 SDS, both in the general adult population [Citation12], and in young patients with growth hormone deficiency (GHD) or idiopathic short stature (ISS) [Citation13]. Recent publications have demonstrated that treatment with recombinant growth hormone in subjects with GHD/ISS is associated with improvement in QoL scores, across physical, emotional, and social domains [Citation14–16]. Given the severity of the height deficit in ACH, is more pronounced than that commonly observed in GHD/ISS, it may follow that patients with ACH could experience even greater QoL impacts. Further, in contrast to GHD/ISS, patients with ACH have few treatment options, which in other disease areas has been shown to be an independent predictor of QoL [Citation17]. For example, growth hormone treatment in ACH contributes to a relatively limited gain in final adult height, and no clear long-term benefits on body proportionality have been established [Citation18,Citation19]. In some countries, patients with ACH receive limb lengthening procedures that increase lower and upper limb length with the aim of improving stature and body proportionality [Citation5,Citation20–22]. These procedures typically require multiple surgeries, extended recovery time, risk of infection, and other complications related to stretching of non-skeletal tissues including nerves and blood vessels [Citation5,Citation23–25].
While the clinical features and medical complications of ACH have been well described [Citation1,Citation5,Citation9,Citation10,Citation26], functional limitations and psychosocial aspects associated with this condition, as well as patient QoL, have received less attention. A small number of systematic and narrative review papers briefly summarize existing studies investigating physical functioning, psychosocial functioning, and/or QoL in patients with ACH or skeletal dysplasia [Citation1,Citation9,Citation10,Citation27], however, no comprehensive review has focused on these outcomes in ACH. A clearer understanding of physical functioning, psychosocial functioning, and QoL in patients with ACH will assist clinicians to better evaluate the effectiveness of management strategies, including novel treatments. Therefore, this review aims to systematically identify primary studies investigating the outcomes of physical functioning, psychosocial functioning, and QoL in patients with ACH, and to summarize and critically appraise their findings with respect to individual instrument domains (or items), methodological characteristics, and limitations of the research design(s). We first reviewed studies that assessed these outcomes among patients with ACH, either descriptively and/or in comparison with reference populations, including average stature individuals or patients with other forms of short stature. Secondly, studies specifically aimed at describing the association between these outcomes and height, limb length or body proportionality, or treatment with limb lengthening surgery in patients with ACH were summarized.
Materials and methods
Population of interest
While the primary population of interest was patients with ACH (any age), a preliminary scoping review indicated that a considerable number of potentially relevant studies were performed among heterogeneous study populations comprised of numerous types of skeletal dysplasia (including ACH). Therefore, relevant studies with heterogenous samples that included patients with ACH were also reviewed.
Outcomes of interest
For the purposes of reporting in this review, study findings were grouped into three categories: (1) physical functioning (or functional independence in ADLs) (2) psychosocial functioning, and (3) QoL (or health-related QoL) based on the tools (assessments or questionnaires) that were used in the study [Citation28–31]. It is noted that these categories were not necessarily mutually exclusive, but allow for consistent reporting across the tools used in the identified studies. Studies that used tools to directly measure either physical limitations or activity restrictions (including mobility and self-care) were summarized under “physical functioning.” Studies that incorporated tools that directly assessed psychosocial functioning including symptoms of anxiety/depression, social difficulties, and/or level of coping were summarized under “psychosocial functioning.” In contrast to these first two categories that used direct measurement, the “QoL" category encompassed studies that measured the patient’s self-evaluation of (or perception/satisfaction with) physical or mental/psychosocial aspects of their daily life, well-being, or health status using multi-dimensional instruments. Depending on the instrument used, the physical domain(s) of QoL included the individuals’ perception of their general health or ability to perform ADLs, bodily pain, fatigue, sleep, and work capacity. The mental/psychosocial domain(s) of QoL included the individuals’ perception of their social/peer relationships, behavioural and/or emotional well-being, and coping ability. Within the QoL category, both generic scales and disease (or condition) specific scales were used [Citation29]. Generic scales are designed to study any health condition and therefore enable comparisons across populations. In disease-specific QoL scales, some or all questions related to potential direct effects of a particular condition (or treatment).
Patient-centered outcomes that were not considered relevant for this review included: measures of motor development, functional body capacity (e.g. walking speed), neuropsychological, cognitive, and other psychological outcomes (e.g. IQ, executive function, body image), socio-economic status, and educational attainment.
Search strategy and study selection
A comprehensive literature search was performed on PubMed/MEDLINE and Embase using relevant terms, such as “achondroplasia”, “skeletal dysplasia,” “short stature,” “quality of life,” “functioning” and “psychosocial.” The following MeSH terms were used on PubMed: “achondroplasia,” “dwarfism,” “quality of life,” “health status” “activities of daily living,” “depression,” “anxiety,” “self-concept” (see Supplementary Table 1 for the full search strings for each database). Both databases were searched for articles published up until 4th April 2021. On Embase, the database search was restricted to human studies (“human”/de). In addition, reference lists of shortlisted articles and previously published review papers were screened for relevant articles that were not captured by the database search. We also performed forward citation chaining of shortlisted articles (using Google Scholar and/or PubMed).
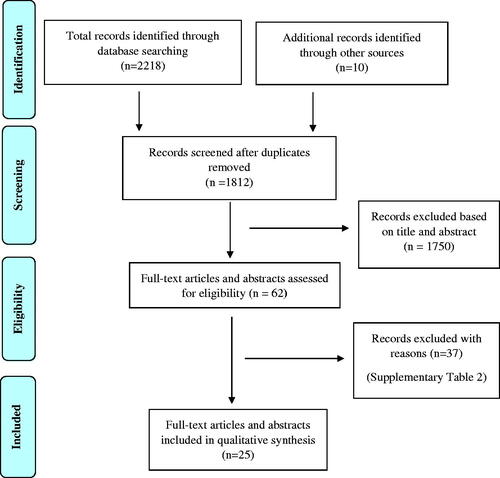
Records were considered eligible for screening if they had an abstract available in the English language but no a priori language restrictions were applied for full-text articles. Any conference abstracts that provided sufficient information were considered eligible for inclusion. All potentially eligible records were initially screened based on title and/or abstract (stage 1) using the following inclusion criteria: (1) primarily quantitative study design; (2) study population consisted solely of ACH patients, or if a heterogeneous sample, comprised largely of ACH patients and provided separate results on ACH; and (3) assessed at least one outcome of interest. Reviews, editorials, commentaries, book chapters, case studies, primarily methodological (e.g. piloting, validation), qualitative studies (e.g. focus groups), and quantitative studies that did not provide data relevant to the scope of this review were excluded. In addition, any studies that provided only “total” or “global” scores (or used a unidimensional measure) of QoL were not eligible for inclusion. Short-listed articles were further screened against the above criteria based on full-text screening (stage 2; not applicable for conference abstracts). Where inclusion of short-listed articles was questionable, this was discussed and resolved between 3 authors (CC, SHL, and JJ). A PRISMA diagram was used to illustrate the screening and selection process [Citation32].
Data extraction and synthesis
Data from full-text articles of included studies were extracted into tables capturing the following fields: reference (title, author, and publication year), period of data collection, length of follow-up (if applicable), country, aims, patient inclusion/exclusion criteria, response rate, sample characteristics (including sample size), study design, comparator (if applicable), relevant outcomes measures, key findings with respect to the topics of interest, study strength and limitations, and primary authors’ conclusion.
A critical appraisal approach was used whereby the strengths and limitations of included studies were identified and recorded. No formal risk of bias assessment was performed, and no studies were excluded because of poor methodological quality. Studies are presented with respect to different age groups (i.e. children and adults reported separately) and because some studies had broad aims covering more than one topic of interest, they contribute to multiple subsections of the results.
Results
Study selection
presents a PRISMA diagram of the search and selection process of eligible publications. Following the removal of duplicates, a total of 1812 records were generated from the literature search, including an additional 10 records identified from reference lists of shortlisted primary studies or review articles. 1750 of those records were excluded based on title and abstract and the remaining 62 records (54 full-text articles and 8 abstracts) underwent full-text screening as applicable. A total of 25 records (23 full-text articles and 2 abstracts) met the criteria and were included in the review; 2 full-text articles and 2 abstracts reported findings from the same cross-sectional studies, therefore 23 unique primary studies were reviewed (see Supplementary Table 2 for records excluded based on full-text screening and reasons for exclusion).
Characteristics of included studies
The 23 primary studies represent broad geography (Australia, Brazil, Germany, India, Japan, Korea, Norway, Puerto Rico, Spain, Switzerland, Turkey, and the US) (). The majority (n = 18) focused on patients with ACH; 8 in pediatric patients (children and/or adolescents, ≤18 years) [Citation33–41], 4 in adults (≥16years) [Citation42–45], and 6 included both pediatric and adult patients [Citation46–52]. All studies were observational in nature and most used a cross-sectional design (n = 13; total sample size range, 14–437 ACH patients), with 5 relatively smaller studies that used either a retrospective (n = 3) and prospective (n = 1) study design to assess the impact of limb lengthening surgery (total sample size range, 12–69 ACH patients).
Table 1. Study design, sample characteristics and instruments used in included studies (n = 23).
The remaining 5 studies (total sample size range, 8–361 patients) were performed with heterogenous samples of skeletal dysplasia or short stature conditions, of which at least 40% had ACH; 1 in pediatric patients [Citation53], 3 in adults [Citation54–56] and 1 study included both pediatric patients and adults [Citation57]. All 5 studies used a cross-sectional design and presented some data for ACH patients separately.
For the presentation of the data, studies were classified into one or more of the following broad categories based on the instruments used to assess relevant outcomes: (1) Physical functioning, (2) psychosocial functioning, and (3) quality of life (QoL). Because children and adults differ significantly in terms of their everyday activities, and how they may perceive and evaluate the impact of their health on their daily life or well-being (as reflected by the creation of different instruments with respect to age), findings are also presented separately by age (pediatric/adult patients).
Physical functioning, psychosocial functioning, and QoL among pediatric patients with ACH
Physical functioning
Ireland et al. [Citation33] cross-sectionally assessed the development of functional independence in a total of 35 children with ACH at the ages of 3 (n = 14), 5 (n = 12), and 7 (n = 9) years, using the Functional Independence Measure for Children (WeeFIM-II) tool. Relative to reference values from typically developing children, the mobility domain z-score of children with ACH did not change significantly between the age groups of 3 and 5 years (p = 0.95) but decreased significantly between the ages of 5 and 7 years (p = 0.001), and in the self-care domain, the z-score decreased significantly between the ages of 3 and 5 years (p = 0.005) but not between the ages of 5 and 7 years (p = 0.69), resulting in a functional performance gap in both domains. When exploring individual items, younger children (3 and 5-year-olds) with ACH required physical caregiver assistance for nearly all of the self-care and mobility tasks, whereas by 7 years of age, physical assistance was limited to half (4 out of 8) of the items in the self-care domain (grooming, bathing, dressing the upper body and toileting) and to 1 out of 5 mobility items (transfer- bath/shower).
In a cross-sectional assessment of pain and physical function in patients with skeletal dysplasia, Alade et al. [Citation57] provided descriptive data on mobility and ADLs in a population of 38 older children and adolescents aged 10–17 years with ACH. The majority of participants had good walking ability per Bleck scale and were able to bath, dress, and toilet independently (>94.5%); only one child was categorized as “poor” walking ability (i.e. walking is possible but not functional), two children were not able to bath/dress themselves and one child could not toilet independently.
Psychosocial functioning
Thompson et al. [Citation34] were the first to cross-sectionally assess behavioral and emotional problems and adaptive behavior of 16 children with ACH (5.5–14 years) in comparison to typically developing children using the Child Behaviour Checklist (CBCL) parent report form and the Vineland Adaptive Behavior Scales (VABS). The composite mean score from the VABS was significantly lower in ACH compared to typically developing children (p < 0.017), whereas no significant differences were observed for parental concerns regarding internalizing problems (summary scale combining anxious/depressed, withdrawn-depressed, and somatic complaints domains) and externalizing problems (summarizing rule-breaking and aggressive behavior domains) as measured by the CBCL. Similarly, Wigg et al. [Citation35] assessed behavioral and emotional problems of 14 children with ACH (6–16 years) using the CBCL parent form. While statistically significant differences between ACH and reference values from typically developing children were observed for some of the CBCL scales, parent ratings did not, overall, reach clinical significance, with very few rating their children in the clinically impaired range in certain domains (i.e. anxiety and thought problems: 2 out of 14 patients rated in the impaired range; externalizing behaviour problems and social problems: 1 out of 14 rated in the impaired range).
Rohenkohl et al. [Citation46,Citation47] cross-sectionally assessed emotional and behavioral problems in 89 children, adolescents, and young adults with ACH (8–29 years) in comparison with a reference population of average statured children, using the Strength and Difficulties Questionnaire (SDQ). ACH patients had a higher (more impaired) average score in the difficulties-with-peers-domain (p = 0.001); however, lower (less impaired) scores were observed for ACH patients in the domains of emotional problems (p = 0.004), behavior problems (p < 0.001) and hyperactivity (p = 0.010).
A cross-sectional study by Nishimura & Hanaki [Citation36] assessed the psychosocial profiles and adaptation of 73 children and adolescents with ACH (8–18 years) in terms of their short stature-related stress and in comparison to a healthy cohort of typically developing children. They utilized an inventory of scales based on a psychological stress model comprised of stressors, coping process, coping resource, and adaptation outcome domains (SCALE 1–8). Although the children with ACH experienced short stature-related unpleasant experiences or stressors more frequently, especially in the physical inconvenience subscale, there was no evidence of any psychosocial maladaptation.
Quality of life
Included studies that assessed QoL in patients with ACH used multi-dimensional tools consisting of both physical and psychosocial domains or dimensions. Three cross-sectional studies assessed QoL in young patients with ACH (see Supplementary Table 3a for data from the three studies). Firstly, Witt et al. [Citation37] assessed QoL in 73 children with ACH (5–14 years) in comparison to a healthy reference population of typically developing children using the generic Paediatric Quality of Life Inventory (PedsQL) scale. Children with ACH showed significantly lower QoL scores across all domains (physical, social, emotional, school) from both the child- and parent-report (p ≤ 0.01), except the child-report of the emotional domain.
Two studies assessed QoL in young ACH patients using the short stature specific Quality of Life in Short Stature Youth (QoLISSY) questionnaire. Rohenkohl et al. [Citation46,Citation47] assessed height-specific QoL in 89 children, adolescents, and young adults with ACH (8–29 years; 33 [37%] patients aged 18–29 years) and compared to a reference population of patients with other forms of short stature (GHD/ISS). Young patients with ACH reported lower scores in the physical (p < 0.001) and social domains of height-related QoL (p = 0.006) compared to GHD/ISS patients. No statistically significant differences were observed for the “emotional,” “coping,” and (height-related) “beliefs” domains. Similarly, Lorne et al. [Citation53] assessed height-related QoL in a small, heterogeneous sample of 8 children and adolescents with skeletal dysplasia (8–18 years; 4 out of 8 had ACH). All seven children and adolescents with skeletal dysplasia who completed the assessment reported lower mean scores for physical, social, and emotional QoL than GHD/ISS patients; of the three participants with ACH who returned their self-report, two reported lower individual scores for the physical, emotional and coping domains, and all three reported lower scores for the social domain. Parent-reported mean scores were even lower than those reported by the children themselves in all domains (N.B. No statistical comparisons were reported for this study). The items reported to most affect children across the physical domain were: (1a) “Because of my height I have trouble reaching things than others of my age” and (1b)” Because of my height I depend on others”; and across the social domain: (2a) “Being asked about my height at school bothers me,” (2b) “Others mistake me for being younger than I am” and (2c) “It hurts to be left out of things because of my height.”
Physical functioning, psychosocial functioning, and QoL among adults with ACH
Physical functioning
Alade et al. [Citation57] provided descriptive data on mobility and ADLs for 159 adults with ACH (≥18 years) which noted that between 10% and 20% reported difficulties with mobility and activities of daily living. Approximately 15% were not able to walk up a flight of stairs independently; 20% could not walk the length of one city block and 13% were categorized as having “poor” walking ability as per the Bleck scale. In terms of ADLs, approximately 11% were not able to bath or dress, 11% could not toilet independently, 16% could not cook or do basic housework tasks, and 16% could not shop for groceries.
Psychosocial functioning
Three cross-sectional studies assessed the psychological well-being of adults with ACH. Jennings et al. [Citation54] assessed the prevalence of depression and anxiety in a cross-section of adults with skeletal dysplasias (18–81 years), including ACH, using the Patient Health Questionnaire-8 (PHQ-8) and Generalized Anxiety Disorder-7 (GAD-7) scales. Out of 192 responses provided from the subset of patients with ACH, 14.1% scored 10 or greater on the PHQ-8 consistent with current depression, and 17.7% scored 10 or greater on the GAD-7 consistent with current anxiety. Moreover, 25% and 21.9% of patients with ACH had a prior diagnosis of depression or anxiety, respectively.
Rodriquez-Gomez et al. [Citation43] assessed the psychological well-being of adults with ACH (n = 22; 21–75 years), using the Beck Depression Inventory (BDI-II), Beck Anxiety Inventory (BAI), Beck Hopelessness Scale (BHS), and the Symptom Checklist-90-R (SCL-90-R) scales. From the BDI scale, 32% reported mild to severe depressive symptoms; 55% reported mild to severe symptoms associated with anxiety (in BAI scale) and 18% reported mild to severe symptoms associated with hopelessness (in BHS scale); 22.7% reported mild to severe symptoms in at least one of the sub-scales in SCL-90-R, particularly the obsessive-compulsive, paranoid and depressive subscales.
Gollust et al. [Citation42] assessed self-esteem in adults with ACH (n = 189; 19–89 years) in comparison with their unaffected first-degree relatives (FDRs; n = 136; 20–84 years), using the Rosenberg self-esteem scale and found that adults with ACH had significantly lower self-esteem mean score than their FDRs (p < 0.0001).
Quality of life
Five cross-sectional studies assessed QoL of adults with ACH using the Medical Outcomes Study 36-item/12 item Short Form (SF-36/SF-12) scale and compared this data to country-level normative data from the general population (see Supplementary Table 3b for data from studies that assessed QoL in adults with ACH). In Matsushita et al. (Japan) [Citation48], the SF-36 physical component summary (PCS; primarily summarizing physical functioning, role-physical, bodily pain, and general health domains) was shown to be significantly lower across all age groups between 18 and 67 years (n = 108; p < 0.005), unlike results from Mahomed et al. (United States) [Citation44] where PCS was significantly lower for patients aged 34 to 55 only (n = 437; range, 19–89 years; p < 0.05). The SF-36 mental component summary score (MCS; primarily summarizing mental health, social functioning, role emotional, and vitality domains) was not significantly different than normative data across age groups in both studies [Citation44,Citation48]. In addition, Matsushita et al. [Citation48] reported that the SF-36 role/social component summary (RCS; primarily summarizing social functioning, role-physical and role-emotional domains) was lower in the older adults with ACH (50–69 years old) compared to the general population of similar age.
Dhiman et al. (United States) [Citation55] used the SF-12 scale (a shorter version of the SF-36) to assess QoL in adults with skeletal dysplasia (n = 189; 56.4% with ACH; 19–80 years). They found that both the mean and median PCS and MCS scores were significantly lower in adults with skeletal dysplasia compared to normative data from the general US population and that age greater than 40 years was a statistically significant predictor of lower than median PCS after adjusting for gender, race, education, and employment status (p = 0.02). Among the subset of patients with ACH in this study (n = 106), 39% had lower than median PCS scores and 48% had lower than median MCS scores. Similarly, Johansen et al. (Norway) [Citation56] assessed QoL in adults with skeletal dysplasia and other short stature conditions (n = 44; 43% with ACH; 16–61 years) in comparison with country-level data from the general population. Patients with short stature had lower QoL across all four physical (physical functioning, bodily pain, role-physical and general health; p < 0.001) and four mental (mental health, social functioning, role-emotional, and vitality; p ≤ 0.002) SF-36 subscales. Within the short stature group, increasing age was negatively associated with the physical functioning (p = 0.005), role physical (p = 0.002), bodily pain (p = 0.007), general health (p = 0.043), and vitality (p = 0.02) subscales after adjusting for gender, height, and level of education. Regardless of age, patients with ACH in this study reported higher mean scores than people with other skeletal dysplasia diagnoses in the subscales for bodily pain and physical functioning, however, none of the differences were statistically significant. Overall, these findings are consistent with a more recent report from Yonko et al. (US) [Citation45], who reported lower scores specifically in adults with ACH (n = 24; 19–66 years) compared with the general US population across all 8 physical and mental scales of the SF-36.
Gollust et al. [Citation42] assessed QoL in a cross-section of adults with ACH (n = 189; 19–89 years) as compared to unaffected first-degree relatives using the Ferrans and Powers Quality of Life Index (QLI) scale. QoL was lower in adults with ACH across both the physical (health & functioning) and all three psychosocial domains (social & economic, psychological & spiritual, family; p < 0.001) compared to their first-degree relatives. Using the WHOQOL-BRIEF scale, Cervan et al. [Citation49] studied QoL in adolescents and adults with ACH (15–54 years; n = 22) compared to unaffected controls matched for age and sex, and found the physical domain to be significantly lower in females with ACH (n = 14; p = 0.002); no significant differences were shown for the three psychosocial domains (psychological, social relationships, environmental) in either men or women.
Association between physical functioning, psychosocial functioning, or QOL and height/limb length or treatment with limb lengthening in patients with ACH
Limb length and body proportionality
Kiemann et al. [Citation38] and Topfer et al. [Citation39] assessed the impact of lower and upper limb length, tibia-fibula length ratio, and humerus-trunk length ratio on functional independence in mobility and self-care in a cross-section of 14 children with ACH (4–12 years) using the WeeFIM-II tool. The severity of lower limb shortening (femur length) was moderate to strongly correlated with restrictions on the mobility domain (Pearson’s correlation coefficient [r] for all 5 items > 0.68, p < 0.01) [Citation38]. An atypical humerus-trunk ratio was the strongest predictor of poorer performance on the self-care domain, after adjusting for age, humerus length, and other upper limb impairments (adjusted R-squared = 0.54) [Citation39].
Height and/or lower limb lengthening
Matsushita et al. [Citation48] cross-sectionally assessed the association between height on QoL and ADLs in a sample of adolescents and adults (10–67 years; n = 184) with ACH (Supplementary Table 4 provides data from studies that explored the association between height and/or limb lengthening on physical functioning, psychosocial functioning, and/or QoL in ACH) [Citation48]. The SF-36 PCS score was significantly higher in patients who had height 140 cm or greater (n = 45; as mainly achieved by lower limb lengthening) compared to shorter patients (100–139cm; n = 130; p < 0.001; mean age was similar between groups); no statistically significant difference was observed in mean MCS or RCS between the two height groups. Regardless of age, mean PCS was statistically significantly lower than the standard (normative) value from the general population in shorter ACH patients (100–139 cm; p < 0.005), but it did not differ from the standard value for the ACH patients with a height greater than 140 cm. In addition, taller patients reported higher ADL scores, more specifically on getting in and out of vehicles (p < 0.001) and stepping up the stairs (p < 0.001) and showed less use of nursing care services (p = 0.033) and wheelchair use (p = 0.005) compared to shorter patients. In multivariate regression models, height was positively associated with SF-36 PCS (β = 0.30; p < 0.003) after adjusting for humeral lengthening and other medical treatments, including spine surgery; neither SF-36 MCS nor RCS scores were associated with height in multivariate models. In agreement with these findings, Johansen et al. [Citation56] reported a specific positive association between height (range: 94–156 cm) and the physical functioning subscale of the SF-36 (after adjusting for age, gender, and level of education) in 44 adults with short stature (43% had ACH), such that greater height was associated with higher scores.
Kim et al. [Citation50] retrospectively assessed the impact of lower (femoral and tibial) limb lengthening on physical functioning, self-esteem, and QoL in 22 young patients with ACH (8–25 years at initial surgery) in comparison with a group of ACH patients who had not undergone surgery (n = 22; matched for age, sex, and pre-operative height), using the American Academy of Orthopedic Surgeons (AAOS) lower extremity, Rosenberg self-esteem, and SF-36 scales, respectively. On average, the Rosenberg self-esteem score was higher in patients who underwent surgery (p < 0.001); there was no statistically significant difference in the mean AAOS lower extremity score or mean SF-36 MCS score between the two groups, whereas a borderline statistically higher mean SF-36 PCS score was observed in the non-surgical group of ACH patients (p = 0.0508).
Upper limb lengthening
Kim and colleagues [Citation51] retrospectively assessed the impact of additional humeral lengthening on self-esteem and QoL in young ACH patients who had previously undergone lower (femoral) limb lengthening (n = 12; 6–20 years at the time of initial surgery). Both Rosenberg self-esteem (p = 0.0007) and SF-36 PCS/MCS (p = 0.0368/p= p = 0.0013) scores were higher (improved) when assessed post-operatively.
Balci et al. [Citation40] retrospectively assessed physical functioning following bilateral humeral lengthening in a sample of young patients with ACH (n = 18; 6–15 years at the time of surgery) using the Disabilities of the Arm, Shoulder, and Hands (DASH) scale. Post-operative DASH score was significantly lower (improved) at the final review (p = 0.037). With respect to individual items, preparing a meal, placing an object over the head, washing the back and hair, going outside, doing daily and social activities, and feeling more capable of doing daily activities, were the most improved functional scores. More recently, Matsushita et al. [Citation48] cross-sectionally assessed the association between humeral lengthening in adolescents and adults with ACH (10–67 years; n = 184; 31 had a history of humeral lengthening) and QoL using the SF-36 scale and found no statistically significant associations with any of the three SF-36 component summary scores (PCS, MCS, and RCS) after adjusting for height and past medical treatments.
Lower and upper limb lengthening
Leiva-Gea et al. [Citation52] prospectively assessed independence in mobility and self-care in a sample of young ACH patients following a staged (simultaneous) lower limb (Stage 1 [S1]) and upper (Stage 2 [S2]) limb lengthening protocol (n = 21; 9–25 years at the time of surgery). Mean height and arm span was approximately 107.7 cm (SD = 7.1) and 95.0 cm (SD = 8.2) before S1 and after S2 was 126.5 cm (SD = 9.2) and 122.7 cm (SD = 7.8), respectively. Functionality was improved in all patients; the majority of them achieved independence without any type of help for eating (98%), toileting (71%), and dressing (76%) as well as improved mobility (stairs – 86%; bathroom – 95%) after both stages. No formal tool was used but the functionality was categorized by level of independence and indirectly with arm span and range of joint motion (hip, knee, ankle, and elbow) measurements.
Using the pediatric PedsQL scale, Batibay et al. [Citation41] retrospectively assessed QoL in young patients with ACH who mainly underwent lower limb lengthening (n = 49; 3–13 years at the time of initial surgery), with a subgroup of patients who also underwent upper limb lengthening (n = 22), in comparison with similarly aged patients not undergoing limb lengthening surgery. There were statistically significant differences between the surgery and the non-surgery groups, though the former group had higher average scores in both the physical and psychosocial domains of PedsQL. However, patients who also had upper humeral lengthening had significantly higher scores in both the physical (p = 0.004) and psychosocial (p = 0.043) domains than those who only underwent lower limb lengthening.
Discussion
Physical functioning, psychosocial functioning, and QoL are relevant outcomes in ACH and important endpoints in the treatment of disproportionate short stature. Although there is a paucity of literature overall, this review has highlighted quantitative research studies investigating each of these concepts in children, adolescents, and/or adults with ACH.
ACH versus average stature (or other short stature conditions): physical functioning and physical domains of QoL
Studies using a direct measure of functional independence (WeeFIM-II) in children with ACH suggest that, compared to normally developing peers, these children are delayed in their ability to independently carry out certain everyday tasks and therefore require more physical caregiver assistance (specifically in grooming, bathing, dressing, toileting and transfer to bath/shower), especially at younger ages (up to 7 years) [Citation33], and that these challenges are strongly associated with shortened limbs [Citation38,Citation39]. While physical limitations or the need for caregiver assistance may become milder or less prevalent as children with ACH move into adolescence, marked impairments appear to exist in adulthood with about 11–20% of adults with ACH experiencing significant difficulties in mobility and ADLs, including bathing, dressing, and toileting [Citation57]. In addition to disproportionate short stature, the high prevalence of chronic pain in this population (approximately 64–75%) may also contribute to poor physical function among adults with ACH [Citation55,Citation57,Citation58].
The perception of the individual regarding physical functioning forms at least a part of the physical domain of QoL across the included studies, with two studies reporting a relatively lower level of QoL in the physical domain among young patients with ACH compared to reference populations of typically developing children [Citation37] or those with GHD/ISS [Citation46,Citation47]. Witt et al. showed that the physical domain of QoL was reduced in children with ACH compared to healthy (average statured) individuals of the same age, as measured by the generic PedsQL which takes childhood-related aspects into account [Citation37]. These differences may reflect physical restrictions and limitations (as summarized above) and as previously reported (qualitatively) by young patients with ACH and confirmed by their parent’s perception [Citation59,Citation60]. When the QoLISSY questionnaire, which is considered an appropriate condition-specific instrument for evaluating height-related QoL in young patients with ACH [Citation61], was used, the physical domain of height-related QoL was characterized as “poor” in young ACH patients and was lower than patients with endocrine short stature (ISS/GHD) [Citation46,Citation47]; this was expected given the more pronounced height deficit seen in ACH. Overall, these findings suggest that the significant reduction in the physical domain of QoL in young patients with ACH is at least partially attributable to the perceived impact of short stature.
Among adults with ACH, the physical component or domain(s) of QoL was consistently lower compared with the general population or otherwise average-statured individuals, especially in older age groups [Citation42,Citation44,Citation45,Citation48,Citation49,Citation55,Citation56]. This age-related trend can possibly be explained by the increased frequency of musculoskeletal complaints that manifest later in adulthood, including symptoms of spinal stenosis (e.g. back pain and/or pain in one or both legs) and chronic lumbar pain [Citation26,Citation44,Citation48]. These findings should be interpreted recognizing that generic instruments such as the SF-36 were used in all adult studies. A potential limitation is that generic instruments often measure “status” (i.e. perceived level of impairment or satisfaction), without taking into account the “importance” or relative meaning of the various components of QoL in each individual domain [Citation29]. The Ferrans and Powers QLI scale, which is used in one of the included studies [Citation42], addresses this issue by incorporating importance rating along with satisfaction rating and thereby moving away from the health-related focus [Citation29].
ACH versus average stature (or other short stature conditions): psychosocial functioning and mental/psychosocial domains of QoL
Witt et al. [Citation37] reported reduced scores in the social and school domains of QoL compared to averaged statured children of the same age, possibly reflecting the social challenges that children with ACH face in their everyday life, such as getting along with other kids [Citation59,Citation60]. However, despite these day-to-day social challenges, the available literature suggests that children and adolescents with ACH do not appear to experience behavioral and emotional problems or maladjustment more frequently or to a greater extent than average statured peers, as measured by CBCL, SDQ, and SCALE 1–8 [Citation34–36,Citation47]. In addition, neither of the two studies by Witt et al. [Citation37] and Rohenkohl et al. [Citation46,Citation47] showed significant differences in the emotional domain of QoL in the child report(s), as measured by the PedsQL and QoLISSY, respectively. Moreover, Rohenkhol et al. reported that a positive attitude toward body height (as assessed by the QoLISSY additional “beliefs” domain), but not height per se, was strongly associated with better (total) height-related QoL in young patients with ACH [Citation46,Citation47]. This suggests that at least some young ACH patients may have learned to accept themselves as they are and be satisfied with themselves [Citation37].
Regarding psychosocial functioning in adults with ACH, the study from Jennings et al. identified a substantial percentage of adults with anxiety and depression [Citation54]. There are many factors contributing to an individual’s mental health. For instance, Jennings et al. noted that those participants with skeletal dysplasia (including ACH) also experienced chronic pain, which was significantly associated with prior mental health diagnoses [Citation54]. Among individuals, without skeletal dysplasias, the association between depression, anxiety, and chronic pain has also been reported [Citation62–65]. In addition, 4 out of the 6 included studies that assessed QoL in adults with ACH reported reductions in the mental component or psychosocial domain(s) compared to the general population or average statured individuals [Citation42,Citation48,Citation55,Citation56].
Regardless of etiology, short stature has been associated with decreased self-esteem, anxiety, and other psychosocial issues, but whether short stature in and of itself leads to those problems remains a controversial issue [Citation42]. The physical environment in which patients with ACH live can present a myriad of physical, social, and emotional challenges on a persistent and daily basis from a very early age, affecting every aspect of their lives, and yet in order to be resilient and not be paralyzed by this constant reminder of their short stature, patients with ACH may have developed healthy coping mechanisms that help them adapt and achieve a more positive perception of their condition as well as a higher QoL than they would otherwise achieve [Citation37,Citation42]. This is an example of the “disability paradox” and an area of future research needs [Citation66].
The importance of height
Two studies reported positive associations between height and the physical domain of QoL and/or functioning. Matsushita et al. showed that ACH patients with height 140 cm or higher (mainly achieved by lower limb lengthening and growth hormone treatment) have a relatively higher level of physical QoL and perform better in pre-defined ADLs, such as climbing stairs [Citation48]. These findings must be interpreted in context with potential limitations in the design of this study. The study population comprised a wide age range (10–67 years), however, neither age itself, nor age-related musculoskeletal complaints/pain, which appear from other studies to play a role in QoL and/or physical function of adults with ACH or skeletal dysplasia [Citation44,Citation55,Citation57,Citation67], were controlled for in the multivariate analysis for height. For example, although the mean (SD) age in the two height groups was largely comparable (100–139 cm: 26.02 years [SD = 15.7]; 140–159 cm: 26.60 years [SD = 8.26]), additional data provided by the authors (personal communication) note that the shorter (<140 cm) group did contain a higher proportion of older patients. As such, some observations regarding lower physical QoL or functionality in the shorter group may be explained, at least in part, by age. Johansen et al. identified a specific positive association between height and the physical functioning dimension of QoL in a clinically heterogeneous sample of adults with skeletal dysplasias and other short stature conditions [Citation56]. Although many participants in this study were patients with ACH (43%), these findings may not be generalizable to the adult ACH population. Both studies used a generic instrument (SF-36) to assess the association between height and QoL. Further investigations that use condition-specific instruments, while considering other factors potentially associated with physical functioning and QoL (such as age and medical complications) could further our understanding of the role of this modifiable factor.
Impact of limb lengthening
Studies assessing the impact of lower limb lengthening on physical functioning and QoL provided inconsistent findings. One study reported an improvement in mobility and self-care following simultaneous lower and upper (humeral) limb lengthening, however, this study did not use standardized tools to assess functionality or QoL, and conclusions were based primarily on an indirect assessment of arm span and joint range of motion [Citation52]. Three further studies showed humeral lengthening improves physical functioning and/or generic QoL (as measured by the SF-36 or PedsQL) [Citation40,Citation41,Citation51]. In contrast, Kim et al. and Batibay et al. reported no improvement in physical functioning or QoL in patients with ACH who (mainly) underwent lower limb lengthening [Citation41,Citation50]. As suggested by Kim et al., the findings of their case-control study could be explained by the fact that long and complicated surgical procedures such as bilateral lower limb lengthening are likely to be followed by post-operative complications or sequelae causing a decline in these outcome measures[Citation50]; however, it is worth mentioning that Batibay et al. found only minimal, non-statistically significant differences in mid-term QoL between patients with transient or minor complications (as observed in the study) and those without complications [Citation41]. Furthermore, any limited improvement in QoL scores as a result of a gain in height may not have been adequately captured by the generic SF-36 or PedsQL questionnaires used in these studies. Further investigations on the impact of upper and lower limb lengthening using condition-specific instruments to assess functionality and/or QoL with a long-term follow-up are warranted.
Limitations
A total of 23 primary studies were reviewed, and the study population and other characteristics must be considered when interpreting the generalizability of the results. Firstly, several studies had a small sample size, with some of them having as few as 8–14 participants, and studies were limited to a restricted number of countries. Most of the included studies were conducted with participants recruited from patient associations (or individual clinics), such as the Little People of America (LPA) [Citation42,Citation44,Citation54,Citation55,Citation57], and patients choosing to participate may differ in characteristics or health status from both non-participants or those individuals who are not members of a patient association. Further, response rates were low (22–35%) in some surveys [Citation42,Citation46–48,Citation57], and lastly, 5 studies included clinically heterogeneous study populations (i.e. ACH and other skeletal dysplasias or short stature conditions) and thus may not be generalizable to ACH patients [Citation53–57], however, these studies generally included a significant proportion of participants with ACH and reported useful information specific to the ACH population.
In terms of study design, almost all the included studies are cross-sectional and/or retrospective in nature. This limits casual interpretations of data from certain studies, particularly those that examined the impact of gain in height or limb length as a result of limb lengthening surgery [Citation40,Citation41,Citation48,Citation50]. Moreover, studies that focused on the impact of limb lengthening surgery in ACH were performed with relatively small, highly selective samples of strongly motivated patients with carers who have understood the benefits and risks of the surgery. This may have introduced selection bias, possibly resulting in an overly enhanced perception of the patient’s functioning and well-being as a result of the surgery [Citation51].
It is also important to emphasize that included studies may differ substantially from one another in terms of study design, samples characteristics, and/or instruments used to assess relevant outcomes and is therefore difficult to compare or combine findings of multiple studies in order to draw certain conclusions
The review methodology itself has limitations. These include the lack of a more formal risk of bias and/or quality assessment for included studies. For example, the available literature, if any, on the psychometric validity (i.e., content and construct validity) of each of the instruments for use in patients with ACH, was not systematically reviewed. For this reason, we cannot assume all the instruments used in included studies are sensitive to the burden of illness or height (and therefore may underestimate or overestimate the impact of ACH). In addition, other than disproportionate short stature (as a core feature of ACH) and limb lengthening surgery, it was out of the scope of this review to summarize and evaluate the evidence available on a range of other factors associated with physical functioning, psychosocial functioning and/or QoL in ACH, including medical complications (e.g. symptomatic spinal stenosis) and other medical treatments (e.g. spine surgery) [Citation44,Citation48,Citation58,Citation67], chronic pain [Citation54,Citation55,Citation57], low self-esteem [Citation42], psychiatric illness diagnoses [Citation45], and social support [Citation55]. Further work would be needed to holistically evaluate the current state of knowledge of the non-medical impact of ACH
Conclusion
While ACH is associated with multi-systemic life-long complications, many patients are able to adapt functionally and psychologically. However, the available literature on QoL and physical functionality demonstrate that this population does experience worse outcomes compared to average stature people of similar age. Future research is warranted to better characterize the functional and psychosocial impact of disproportionate short stature as well as to prospectively assess the effects of limb lengthening and other relevant treatments in this patient population. This would require the development and application of validated condition-specific frameworks and tools for measuring meaningful impact in these individuals while taking into account the multi-faceted challenges that they face [Citation61,Citation68–70]. Having a clearer understanding of the impact of disproportionate short stature in patients with ACH will assist individuals, clinicians, families, and society as a whole to identify and implement more efficient and effective strategies, including both medical treatment options and environmental adaptations, to promote greater independence, resilience, and enhancements in quality of life.
Supplementary_Material_Constantinides_C_et_al_CLEAN.docx
Download MS Word (67.7 KB)Acknowledgments
The authors would like to thank other members of the team for assisting with the different stages of this work, including helpful comments on the manuscript.
Disclosure statement
SHL and JQ are full-time employees and stockholders of BioMarin Pharmaceutical Inc. CC was a temporary employee and JJ a full-time employee of BioMarin Pharmaceutical Inc. at the time of this work. PJI has received fees from BioMarin for participating in advisory boards.
Additional information
Funding
References
- Pauli RM. Achondroplasia: a comprehensive clinical review. Orphanet J Rare Dis. 2019;14(1):1.
- Coi A, Santoro M, Garne E, et al. Epidemiology of achondroplasia: a population-based study in Europe. Am J Med Genet A. 2019;179(9):1791–1798.
- Waller DK, Correa A, Vo TM, et al. The population-based prevalence of achondroplasia and thanatophoric dysplasia in selected regions of the US. Am J Med Genet A. 2008;146A(18):2385–2389.
- Foreman PK, Kessel F, Hoorn R, et al. Birth prevalence of achondroplasia: a systematic literature review and meta-analysis. Am J Med Genet A. 2020;182(10):2297–2316.
- Horton WA, Hall JG, Hecht JT. Achondroplasia. Lancet. 2007;370(9582):162–172.
- Wright MJ, Irving MD. Clinical management of achondroplasia. Arch Dis Child. 2012;97(2):129–134.
- Vajo Z, Francomano CA, Wilkin DJ. The molecular and genetic basis of fibroblast growth factor receptor 3 disorders: the achondroplasia family of skeletal dysplasias, Muenke craniosynostosis, and Crouzon syndrome with acanthosis nigricans. Endocr Rev. 2000;21(1):23–39.
- Merker A, Neumeyer L, Hertel NT, et al. Growth in achondroplasia: development of height, weight, head circumference, and body mass index in a European cohort. Am J Med Genet A. 2018;176(8):1723–1734.
- Fredwall SO, Maanum G, Johansen H, et al. Current knowledge of medical complications in adults with achondroplasia: a scoping review. Clin Genet. 2020;97(1):179–197.
- Ireland PJ, Pacey V, Zankl A, et al. Optimal management of complications associated with achondroplasia. Appl Clin Genet. 2014;7:117–125.
- Hays RD, Reeve BB. Measurement and modeling of health-related quality of life. Amsterdam (The Netherlands): Elsevier; 2008. p. 241–252.
- Christensen TL, Djurhuus CB, Clayton P, et al. An evaluation of the relationship between adult height and health-related quality of life in the general UK population. Clin Endocrinol. 2007;67(3):407–412.
- Bullinger M, Sommer R, Pleil A, et al. Evaluation of the American-English Quality of Life in Short Stature Youth (QoLISSY) questionnaire in the United States. Health Qual Life Outcomes. 2015;13:43.
- Quitmann J, Bloemeke J, Silva N, et al. Quality of life of short-statured children born small for gestational age or idiopathic growth hormone deficiency within 1 Year of Growth Hormone Treatment. Front Pediatr. 2019;7:164.
- Gonzalez Briceno LG, Viaud M, Beltrand J, et al. Improved general and height-specific quality of life in children with short stature after 1 year on growth hormone. J Clin Endocrinol Metab. 2019;104(6):2103–2111.
- Stephen MD, Varni JW, Limbers CA, et al. Health-related quality of life and cognitive functioning in pediatric short stature: comparison of growth-hormone-naïve, growth-hormone-treated, and healthy samples. Eur J Pediatr. 2011;170(3):351–358.
- Sprengers RW, Teraa M, Moll FL, et al. Quality of life in patients with no-option critical limb ischemia underlines the need for new effective treatment. J Vasc Surg. 2010;52(4):843–849.
- Harada D, Namba N, Hanioka Y, et al. Final adult height in long-term growth hormone-treated achondroplasia patients. Eur J Pediatr. 2017;176(7):873–879.
- Miccoli M, Bertelloni S, Massart F. Height outcome of recombinant human growth hormone treatment in achondroplasia children: a meta-analysis. Horm Res Paediatr. 2016;86(1):27–34.
- Ginebreda I, Campillo-Recio D, Cárdenas C, et al. Surgical technique and outcomes for bilateral humeral lengthening for achondroplasia: 26-year experience. Musculoskelet Surg. 2019;103(3):257–262.
- Hosny GA. Humeral lengthening and deformity correction. J Child Orthop. 2016;10(6):585–592.
- Aldegheri R, Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001;10(3):238–247.
- Schiedel F, Rödl R. Lower limb lengthening in patients with disproportionate short stature with achondroplasia: a systematic review of the last 20 years. Disabil Rehabil. 2012;34(12):982–987.
- Shirley ED, Ain MC. Achondroplasia: manifestations and treatment. J Am Acad Orthop Surg. 2009;17(4):231–241.
- Kim SJ, Pierce W, Sabharwal S. The etiology of short stature affects the clinical outcome of lower limb lengthening using external fixation. A systematic review of 18 trials involving 547 patients. Acta Orthop. 2014;85(2):181–186.
- Hunter AG, Bankier A, Rogers JG, et al. Medical complications of achondroplasia: a multicentre patient review. J Med Genet. 1998;35(9):705–712.
- Thompson S, Shakespeare T, Wright MJ. Medical and social aspects of the life course for adults with a skeletal dysplasia: a review of current knowledge. Disabil Rehabil. 2008;30(1):1–12.
- EUPATI [Internet]. Patient-reported outcomes (PROs) assessment. Utrecht (The Netherlands): EUPATI; 2021 [cited 2021 Apr 6]. Available from: https://toolbox.eupati.eu/resources/patient-reported-outcomes-pros-assessment/
- Cohen JS, Biesecker BB. Quality of life in rare genetic conditions: a systematic review of the literature. Am J Med Genet Part A. 2010;152(5):1136–1156.
- Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–649.
- Slade A, Isa F, Kyte D, et al. Patient reported outcome measures in rare diseases: a narrative review. Orphanet J Rare Dis. 2018;13(1):61.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Ireland PJ, Mcgill J, Zankl A, et al. Functional performance in young Australian children with achondroplasia. Dev Med Child Neurol. 2011;53(10):944–950.
- Thompson NM, Hecht JT, Bohan TP, et al. Neuroanatomic and neuropsychological outcome in school-age children with achondroplasia. Am J Med Genet. 1999;88(2):145–153.
- Wigg K, Tofts L, Benson S, et al. The neuropsychological function of children with achondroplasia. Am J Med Genet A. 2016;170(11):2882–2888.
- Nishimura N, Hanaki K. Psychosocial profiles of children with achondroplasia in terms of their short stature-related stress: a nationwide survey in Japan. J Clin Nurs. 2014;23(21–22):3045–3056.
- Witt S, Kolb B, Bloemeke J, et al. Quality of life of children with achondroplasia and their parents - a German cross-sectional study. Orphanet J Rare Dis. 2019;14(1):194.
- Kiemann C, Johnston L, Topfer C, et al. Travels’ impairments predict gross motor function and participation of school-aged children with achondroplasia [abstract]. Dev Med Child Neurol. 2017;59(S3):86.
- Topfer C, Ireland P, Kiemann C, et al. Upper limb function in achondroplasia and its relationship with upper limb musculoskeletal impairments [abstract]. Dev Med Child Neurol. 2018;60(S1):45–46.
- Balci HI, Kocaoglu M, Sen C, et al. Bilateral humeral lengthening in achondroplasia with unilateral external fixators: is it safe and does it improve daily life? Bone Joint J. 2015;97-B(11):1577–1581.
- Batıbay SG, Balcı Hİ, Bayram S, et al. Quality of life evaluation following limb lengthening surgery in patients with achondroplasia. Indian J Orthop. 2020;54(1):39–46.
- Gollust SE, Thompson RE, Gooding HC, et al. Living with achondroplasia in an average-sized world: an assessment of quality of life. Am J Med Genet A. 2003;120A(4):447–458.
- Rodriguez-Gomez J, Aldarondo A, Vidot F, et al. Achondroplasia: a pilot study on the psychosocial and medical features of a sample in Puerto Rico. Bol Asoc Med P R. 2015;107(3):58–65.
- Mahomed NN, Spellmann M, Goldberg MJ. Functional health status of adults with achondroplasia. Am J Med Genet. 1998;78(1):30–35.
- Yonko EA, Emanuel JS, Carter EM, et al. Quality of life in adults with achondroplasia in the United States. Am J Med Genet. 2021;185(3):695–701.
- Rohenkohl AC, Bullinger M, Quitmann J. [Quality of life in children, adolescents, and young adults with achondroplasia]. Orthopade. 2015;44(3):212–218. German.
- Rohenkohl AC, Sommer R, Bestges S, et al. [Living with achondroplasia- how do young persons with disproportional short stature rate their quality of life and which factors are associated with quality of life?] Z Kinder Jugendpsychiatr Psychother. 2015;43(6):433–441. German.
- Matsushita M, Kitoh H, Mishima K, et al. Physical, mental, and social problems of adolescent and adult patients with achondroplasia. Calcif Tissue Int. 2019;104(4):364–372.
- Cervan MP, Da Silva MCP, Lima RLDO, et al. Comparative study of quality of life level between achondroplasics and non-achondroplasics subjects. J Bras Psiquiatr. 2008;57(2):105–111.
- Kim SJ, Balce GC, Agashe MV, et al. Is bilateral lower limb lengthening appropriate for achondroplasia?: midterm analysis of the complications and quality of life. Clin Orthop Relat Res. 2012;470(2):616–621.
- Kim SJ, Agashe MV, Song SH, et al. Comparison between upper and lower limb lengthening in patients with achondroplasia: a retrospective study. J Bone Joint Surg Br. 2012;94(1):128–133.
- Leiva-Gea A, Delgado-Rufino FB, Queipo-de-Llano A, et al. Staged upper and lower limb lengthening performing bilateral simultaneous surgery of the femur and tibia in achondroplastic patients. Arch Orthop Trauma Surg. 2020;140(11):1665–1676.
- Lorne H, Newman CJ, Unger S. Is height important for quality of life in children with skeletal dysplasias? Eur J Med Genet. 2020;63(4):103816.
- Jennings SE, Ditro CP, Bober MB, et al. Prevalence of mental health conditions and pain in adults with skeletal dysplasia. Qual Life Res. 2019;28(6):1457–1464.
- Dhiman N, Albaghdadi A, Zogg CK, et al. Factors associated with health-related quality of life (HRQOL) in adults with short stature skeletal dysplasias. Qual Life Res. 2017;26(5):1337–1348.
- Johansen H, Andresen I-L, Naess EE, et al. Health status of adults with short stature: a comparison with the normal population and one well-known chronic disease (rheumatoid arthritis). Orphanet J Rare Dis. 2007;2:10.
- Alade Y, Tunkel D, Schulze K, et al. Cross-sectional assessment of pain and physical function in skeletal dysplasia patients. Clin Genet. 2013;84(3):237–243.
- Ain MC, Abdullah MA, Ting BL, et al. Progression of low back and lower extremity pain in a cohort of patients with achondroplasia. SPI. 2010;13(3):335–340.
- Quitmann J, Witt S, Rohenkohl A, et al. Quality of life in young patients with achondroplasia. Qualitative comparison of the perspectives of patients and parents. Monatsschr Kinderheilkd. 2014;162(5):428–434.
- Witt S, Rohenkohl A, Bullinger M, et al. Understanding, assessing and improving health-related quality of life of young people with achondroplasia - a collaboration between a patient organization and academic medicine. Pediatr Endocrinol Rev. 2017;15(1):109–118.
- Bloemeke J, Sommer R, Witt S, et al. Cross-cultural selection and validation of instruments to assess patient-reported outcomes in children and adolescents with achondroplasia. Qual Life Res. 2019;28(9):2553–2563.
- Bair MJ, Wu J, Damush TM, et al. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890–897.
- Kroenke K, Wu J, Bair MJ, et al. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–973.
- McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1):127–133.
- Ohayon MM, Schatzberg AF. Chronic pain and major depressive disorder in the general population. J Psychiatr Res. 2010;44(7):454–461.
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48(8):977–988.
- Fredwall SO, Steen U, De Vries O, et al. High prevalence of symptomatic spinal stenosis in norwegian adults with achondroplasia: a population-based study. Orphanet J Rare Dis. 2020;15(1):123.
- Bloemeke J, Sommer R, Witt S, et al. Piloting and psychometric properties of a patient-reported outcome instrument for young people with achondroplasia based on the international classification of functioning disability and health: the achondroplasia personal life experience scale (APLES). Disabil Rehabil. 2019;41(15):1815–1825.
- Ireland PJ, Savarirayan R, Pocovi T, et al. Development of the screening tool for everyday mobility and symptoms (STEMS) for skeletal dysplasia. Orphanet J Rare Dis. 2021;16(1):40.
- Pfeiffer KM, Brod M, Smith A, et al. Assessing physical symptoms, daily functioning, and well‐being in children with achondroplasia. Am J Med Genet. 2021;185(1):33–45.