Abstract
Purpose
Mindfulness-based interventions (MBIs) are effective treatments for stress, anxiety, and depression in PwMS. However, low adherence and high attrition may limit effectiveness. Qualitative research can provide important insights into MBI acceptability, accessibility, and implementation. This systematic review and meta-aggregation evaluated qualitative research findings on the use of MBIs for PwMS.
Methods
Systematic searches were undertaken in six major electronic databases. Studies using qualitative or mixed methods were included. Two reviewers screened, data extracted, and critically appraised studies. Meta-aggregation was performed following the Joanna Briggs Institute approach, extracting findings, developing categories, and synthesizing findings.
Results
Six eligible papers, including 136 PwMS were included in meta-aggregation. 136 findings were extracted, grouped into 17 categories, with four synthesized findings: (1) “accessing mindfulness,” (2) “a sense of belonging,” (3) “experiencing mindfulness,” and (4) “making mindfulness more relevant and sustainable for PwMS.”
Conclusions
MBIs for PwMS need to take into consideration disability which can limit accessibility. Online MBIs (synchronous and asynchronous) appear acceptable alternatives to traditional face-to-face courses. However, PwMS benefit from shared (mindful) experiencing and highlight MBI instructors as crucial in helping them understand and practice mindfulness. Involving PwMS in design, delivery, and iterative refinement would make MBIs more relevant to those taking part.
Both face-to-face and online Mindfulness-based interventions (MBIs) appear acceptable to PwMS and, ideally, people should be offered a choice in training modality.
PwMS derive benefit from undertaking MBIs with their peers, where a sense of camaraderie and belonging develop through shared (mindful) experiences.
Instructors delivering MBIs for PwMS should be knowledgeable about the condition; participants describe how the instructor has a key role in helping them practice mindfulness effectively in the context of unpleasant experiences associated with MS.
MBIs tailored for PwMS should include a pre-course orientation session, clearly articulate how mindfulness practices can help with MS, provide well-organized course materials in large font size, and deliver individual mindfulness practices flexibly depending on participant need.
IMPLICATIONS FOR REHABILITATION
Introduction
Multiple sclerosis (MS) is a chronic, progressive neurodegenerative condition [Citation1], associated with multiple comorbidities [Citation2] and complex disabilities [Citation3]. Common physical symptoms include pain [Citation4], fatigue [Citation5], and impairment of sleep [Citation6]. People with multiple sclerosis (PwMS) often report that having the condition is stressful [Citation7], with anxiety and depression occurring more than three times as frequently in PwMS versus controls [Citation8]. Addressing these symptoms in PwMS can be challenging and new treatments that are safe, accessible, acceptable, effective, and affordable are urgently needed.
Mindfulness-based interventions (MBIs) derive from ancient Buddhist and Yogic meditation techniques, secularized and manualized in the 1980s for use in healthcare settings to help people cope with chronic pain and stress [Citation9]. Through core meditations focused on breath, body, and movement, plus psychoeducation on stress, group discussion, and regular home practices, MBIs are designed to teach participants to “pay attention, in a particular way, on purpose, in the present moment, non-judgementally” [Citation10]. Mechanisms of action are incompletely understood, but likely relate to a combination of improvements in mindfulness [Citation11,Citation12], cognitive and emotional reactivity [Citation11], amount of home practice completion [Citation13], and other common factors [Citation14] such as instructor characteristics, group processes and peer support [Citation15]. Recent systematic reviews and meta-analyses have demonstrated that MBIs are effective treatments for PwMS with small-moderate beneficial treatment effects on stress (Standardized mean difference – SMD = 0.55, 95% confidence interval – CI95 0.25–0.85), anxiety (SMD = 0.35, CI95 0.15–0.55), depression (SMD = 0.35, CI95 0.17–0.53) [Citation16] and fatigue (SMD = 0.24, CI95 0.08–0.41) [Citation17]. However, adherence to MBIs for PwMS is only 60%, and attrition can be high (range 0–39%) [Citation16–18]. Previous studies have focused largely on younger PwMS (average age 41) who remain ambulant [Citation16–18] and thus are not necessarily representative of the MS population at large [Citation8]. Furthermore, a range of MBIs have been used in previous studies (Mindfulness-Based Stress Reduction – MBSR; Mindfulness-Based Cognitive Therapy; a mix of MBSR and MBCT; MBCT minus mindful-movement), the MBI often being modified in advance without apparent justification, blurring potential treatment mechanisms, and thus the optimal MBI and how it fits in the bigger picture of care for PwMS remains unclear. Quantitative systematic reviews and meta-analyses provide robust evidence for the effectiveness of MBIs for PwMS but do not typically consider participants’ experiences with MBIs or their perspectives on MBI acceptability, accessibility, or the nuanced factors influencing adherence and attrition, which can be context-dependent [Citation19]. As such, quantitative reviews are limited in their ability to inform the optimization of MBIs. Qualitative research methods, on the other hand, allow more detailed exploration of participant expectancy, experience, and perspectives for intervention optimization, besides having the potential to unearth hitherto unanticipated mechanisms of change [Citation20]. For example, when a quantitative study reports low levels of adherence and/or high levels of attrition, reasons accounting for these findings can be explored in depth using methods like semi-structured interviews or focus groups.
Recently, the application of the systematic review methodology has been applied to qualitative research findings via meta-aggregation [Citation21]. Meta-aggregation is a research method founded in pragmatism [Citation22] that can be used to produce rigorous, auditable, and robust qualitative evidence synthesis [Citation22]. Meta-aggregation is a qualitative descriptive method, which is used to collate and summarize findings from primary research studies. Unlike interpretive methods to qualitative syntheses, such as meta-ethnography, or realist synthesis, no attempt is made to create new meaning or conceptual understanding from synthesized findings. Instead, the purpose is to provide practical “lines of action” to guide policy and practice decisions based on synthesized findings that can be clearly traced back to those reported in original studies [Citation21].
Through a series of systematic reviews and meta-analyses we have explored previously the impact of MBIs on mental wellbeing [Citation16], physical symptoms [Citation17], and quality of life (under review) in PwMS. However, no previous evidence synthesis has systematically explored the qualitative research data pertaining to the use of MBIs for PwMS, from the perspective of patients and families, the health professionals who care for them, or those delivering the MBIs.
The overarching objective of this systematic review and meta-aggregation is to identify, evaluate and synthesize qualitative research findings on the use of MBIs in healthcare for PwMS.
Methods
Protocol and registration
A protocol was registered prospectively with PROSPERO, Centre for Reviews and Dissemination, University of York: CRD42019124361.
Inclusion criteria
Eligible studies were identified on the basis of SPIO criteria – Study, Population, Intervention, Outcome [Citation23]. Studies included those reporting solely qualitative data or those of mixed-methods design reporting qualitative data that could be extracted, including but not limited to phenomenology, grounded theory, ethnography, action research, or feminist research. The population of interest was PwMS of any age, sex, gender identity, ethnicity, socio-economic status, or stage of illness. The intervention had to be an MBI based on either MBSR [Citation24] and/or MBCT [Citation25]. Outcomes constituted themes related to participant experience, perceived effects, or barriers and facilitators to PwMS participating in these interventions. provides an overview of eligibility criteria.
Table 1. Eligibility criteria.
Search strategy
A comprehensive search strategy was developed for use in six major electronic databases, including AMED, ASSIA, the Cochrane Database of Systematic Reviews, EMBASE, MEDLINE, and PsycINFO. Our initial search was carried out in May 2020; we updated this in April 2021. Supplementary Appendix 1 details our search strategy for use in MEDLINE. We searched from 1980 to the date of search, given that MBIs were first developed and piloted in the 1980s. We included only studies published in English, among human subjects, in the peer-reviewed academic literature.
Study selection, storage, and screening
We used COVIDENCE to import, store and screen search results. Two independent reviewers “broad screened” the full list of titles/abstracts, using keywords such as “multiple sclerosis” and “mindfulness” to identify potentially relevant studies for inclusion. Following this, full papers of those studies identified as potentially relevant were “narrow screened” by two independent reviewers using SPIO [Citation23] categories.
Data collection
We used a standardized data extraction template for use in meta-aggregation, developed for people with stroke in a previous, published meta-aggregation [Citation26], adapted to the specific context of this study. For example, we also sought data on the type of MS, degree of disability (i.e., Expanded disability status scale – EDSS), type of MBI (i.e., MBSR or MBCT). Extracted data were then entered into an evidence table.
Quality appraisal
Given our broad inclusion criteria in terms of types of qualitative studies, we chose to use a generic quality appraisal tool, the Critical Appraisal Skills Programme (CASP) for Qualitative Studies. The CASP tool comprises 10 questions for researchers to consider in relation to quality in qualitative research. Researchers can answer either “Yes” – criteria met; “Can’t tell” – if it is unclear, and “No” if it is clear that the criteria have not been met. The final CASP tool question asks researchers to consider the overall value of the study. A score of 6 on the CASP tool was considered to indicate a sufficient level of methodological quality to merit inclusion in this review. Two reviewers assessed each study independently, convening finally to discuss assessments. Recourse was available in advance for further discussion with a senior reviewer, should discrepancies remain – in the event this was not necessary.
Evidence synthesis and reporting
We used the Joanna Briggs Institute (JBI) manual [Citation27] approach to qualitative synthesis to guide the conduct of this meta-aggregation and the 21-item ENhancing Transparency in the REporting the synthesis of Qualitative research (ENTREQ) [Citation28] statement as a guide to ensure we reported the key stages of our research. In brief, two independent reviewers (RS, SS) extracted findings from each study included in the review. The reviewers then met to discuss and finalize a list of extracted findings. Consensus findings were then grouped together into categories based on similarity of meaning. As a final step, categories were then aggregated into synthesized findings, which were then shared with the group (ML, SWM, MW, RS, SS) for discussion, refinement, and development of consensus.
Results
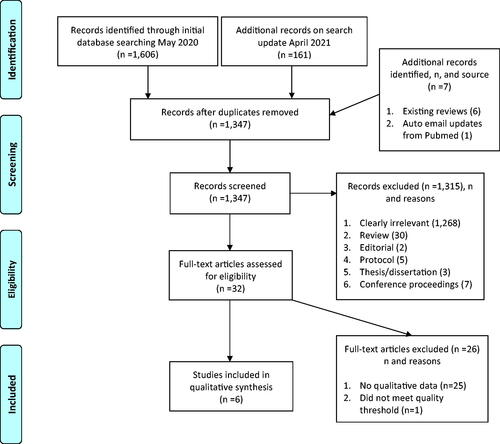
Searches of the electronic databases in May 2020 generated an initial 1,606 potential papers for inclusion. A search update in April 2021 generated an additional 161 potential papers. Following deduplication, there were 1347 potential papers. After the broad screening, 32 were selected for narrow screening using SPIO criteria. Reasons for exclusion at the broad screening included studies clearly not relevant (1258), review article (30), editorial (2), protocol (5), thesis/dissertation (3), conference proceedings (7). At narrow screening, 25 studies were excluded due to not reporting any qualitative data, whilst one study that did report qualitative data was also excluded as it did not meet predefined quality criteria, with no unequivocal or credible findings [Citation29]. Finally, six studies were deemed eligible and selected for inclusion in this study [Citation30–35]. presents a PRISMA flowchart detailing our search process.
Study characteristics
All six papers reported qualitative findings relating to the experience of PwMS (total PwMS n = 136) taking part in MBIs. Three studies [Citation31,Citation33,Citation34] also included qualitative data from other relevant stakeholders (n = 18; MBI instructors/experts n = 6, MS clinicians n = 12). All six studies were part of mixed-method analyses, five associated with randomized controlled trials (RCTs) [Citation36,Citation37], one a non-randomized controlled trial [Citation38]. Three studies took place in the UK [Citation33–35], two in Australia [Citation30,Citation31], and one in the United States [Citation32]. Two papers were derived from the same research group [Citation33,Citation34], analyzing data from different stakeholders, one focused on MBI acceptability [Citation34], the other on perceived barriers and facilitators to implementation [Citation33]. Study participant numbers ranged from n = 14–55.
Study analysis methods
The first study in this area used deductive thematic analysis of MBI participant feedback, with interview questions focused on putative mediators of beneficial change following training in mindfulness [Citation35]. Inductive coding was used to capture outlying themes.
The next study used inductive thematic framework analysis to generate initial coding for participants and MBI instructors following the first iteration of MBSR, then used themes generated to code subsequent participant and MBI instructor feedback in a second iteration of the MBSR course [Citation34]. A linked study then used a Normalization Process Theory (NPT) framework to code previously identified participant and MBI instructor data, alongside new data collected from MS clinicians using a topic guide based on core NPT constructs [Citation33].
A further study used reflexive thematic analysis with both inductive and semantic coding [Citation32]. Interview questions focused on the overall experience of the MBI, usefulness of the content, and delivery modality.
Another study used content analysis to assess participant entries to daily home practice diaries, weekly reflective journals and post-intervention questionnaires, questions focusing on recruitment, practicality, acceptability, and integration of mindfulness practices into daily life; data coded deductively thereafter [Citation30].
The most recent study utilised inductive thematic analysis of participant data deriving from semi-structured interviews with questions focused on perceived psychological difficulties associated with having MS, existing coping strategies, MBIs, cognitive behavioural therapy (CBT), perceptions about the use of internet-based interventions, including therapy preferences, perceived barriers, and facilitators to participation and adherence [Citation31].
provides an overview of study characteristics.
Table 2. Included studies.
Participant characteristics
Three studies reported detailed participant demographics [Citation30,Citation31,Citation34]. The other studies referred the reader to linked quantitative studies where such data were available in relation to the quantitative analysis but was of limited relevance as sample sizes varied between quantitative and qualitative arms of the respective studies. Where reported, ages ranged from 21 to 66 [Citation30,Citation31,Citation34]. Where reported, most participants were female [Citation30,Citation31,Citation34], one study reporting on female participants only, by default [Citation32]. Ethnicity was reported in one study [Citation34]. In the one study that reported socioeconomic status (SES) very few with low SES and low educational attainment were included [Citation34]. All MS phenotypes appear to have been represented, though most had relapsing-remitting variants. One study included those with progressive phenotypes only [Citation35].
MBI intervention characteristics
Three studies [Citation30,Citation32,Citation35] offered instructor-led, live/“synchronous” online MBIs, two exclusively (both based on MBCT, one using Skype [Citation35]; another using Zoom [Citation30]), and the other offering MBSR either online (using Zoom [Citation32]), or in-person based on transportation issues or distant place of residence. Of the exclusively online interventions, one using Skype delivered a modified MBCT course, minus mindful movement, with cognitive and educational content tailored to common MS symptoms, whilst another using Zoom delivered “Mindfulness 4 Multiple Sclerosis,” again based on MBCT. One study offered an “asynchronous,” interactive web-based MBI based on MBSR, shortened to five 15-min modules delivered over eight weeks, content tailored based on feedback from PwMS, MS clinicians, and mindfulness experts [Citation31]. Three studies reported data from face-to-face MBIs, two in a National Health Service center for Integrative Care [Citation33,Citation34], one in a facility that provided “ample handicap parking and easy access.” [Citation32]. One face-to-face study started out with standard MBSR and adapted a subsequent course iteration based on participant feedback from course 1 [Citation34]. The study that offered both synchronous online (Zoom) and face-to-face options used MBSR, augmented with sleep training educational content [Citation32]. Two studies offered an orientation session followed by eight weekly sessions [Citation32,Citation34]. No study offered the full “dose” of MBSR or MBCT (none included a day retreat); one [Citation31] shortened the course to five weekly sessions instead of eight. Session length ranged from 15 min to 2.5 h. All studies included some tailoring for PwMS (alteration [Citation33,Citation34] or removal of mindful movement [Citation31,Citation35], shortened sessions [Citation31,Citation32]). All studies recommended home practices, but the duration was not specified in one. For a full overview of intervention characteristics see Supplementary Appendix 2.
MBI instructor characteristics
Among the online MBIs, a live, synchronous MBCT course was delivered by the study author, a health psychologist, and a newly qualified mindfulness practitioner [Citation35]. In a further study, using a live synchronous MBI based on MBCT, the MBI was delivered by a clinical psychologist registered as a mindfulness practitioner [Citation30]. A web-based MBI based on MBSR was delivered asynchronously, but participants had access to the study team via weekly telephone calls to check understanding of the practices and troubleshoot technical difficulties [Citation31]. Another study, offering synchronous online or face-to-face MBIs, delivered MBSR in both instances via a certified instructor with over 10 years of experience [Citation32]. The final study delivered face-to-face, group-based MBSR via two integrative medicine physician facilitators, certified to teach MBIs, with an average of 7.5 years of teaching experience [Citation33,Citation34].
Accessibility and inclusion
Internet access and baseline evidence of psychological distress on the General Health Questionnaire-12 (GHQ-12) were required to participate in one study [Citation35], which included only those with progressive MS phenotypes. Another excluded participants’ lacking internet access or with high baseline stress on the Kessler Psychological Distress Scale [Citation30]. Those with active suicidality were ineligible in five studies [Citation30,Citation32–35]. Those currently receiving other psychological interventions or with prior MBI experience were commonly excluded, except in one study [Citation30]. People with cognitive impairment, active psychosis, or active substance abuse were also commonly excluded.
Quality appraisal
One study [Citation32] was awarded “Yes” on all nine domains of the CASP qualitative checklist, two on eight [Citation34,Citation35], two on seven [Citation31,Citation33], one on six [Citation30]. These studies all fulfilled the pre-defined quality inclusion criterion for this review. Full details of the quality assessment are available in .
Table 3. Quality appraisal (critical skills appraisal programme [CASP] checklist for qualitative studies).
Qualitative synthesis
One-hundred and thirty-six qualitative findings from 136 PwMS from across the six studies included in the qualitative synthesis were extracted and grouped into 17 categories. Categories with similar meanings were then amalgamated into four synthesized findings: (1) accessing mindfulness, (2) a sense of belonging, (3) experiencing mindfulness, and (4) making mindfulness more relevant and sustainable for PwMS. delineates categories and label descriptions. depicts synthesized findings. Below, each synthesized finding is described, substantiated with illustrative verbatim quotes, reflecting the views of PwMS and their experiences of taking part in an MBI, MBI instructors, and MS clinicians.
Table 4. Categories: label and description.
Table 5. Synthesized findings from categories.
Accessing mindfulness
Accessing mindfulness related to why PwMS were motivated to access mindfulness courses, referral criteria and process for MS clinicians, how the course was physically accessed by participants, the delivery modality (i.e., face-to-face, or online), and the continued accessing of support for ongoing mindfulness practice after the course was finished.
Common motivations for PwMS to seek access to mindfulness were related to finding new ways to help with stress, pain, and impaired sleep.
I’m trying to find other ways to solve my problems of falling asleep without drugs, to be honest with you…it seemed like mindfulness makes sense as a potential solution to at least help with some of my MS problems. (Se, Pg. 4, P11) [Citation32]
However, both PwMS and MS clinicians had limited knowledge of what an MBI could offer. One MS clinician-reported they would be more likely to seek out mindfulness for their patients if they knew that those delivering the intervention were suitably qualified and experienced in working with PwMS.
I would want to know the experience of the facilitator of the group… I would prefer a facilitator who has a bit of experience of MS. (Si19, Additional file 6, C6, quote 4) [Citation33]
Another MS clinician highlighted a lack of funding to support MBIs in a publicly funded healthcare system and the need for greater collaboration with third sector charitable organizations.
I guess if there was any way of maybe linking in with organisations such as the MS Society there’s maybe a bigger scope for getting it out there a bit more if it was kind of a joint venture and there was an element of cross funding, they might be a bit more amenable. (Si19, Additional file 6, C5, quote 5) [Citation33]
In terms of physical access for face-to-face MBIs, PwMS highlighted the importance of accommodating for disability, including dedicated parking. Travel to and from the venue was cited as a source of stress, again relating to parking, or when long journeys on public transport were required. These experiences underpinned some PwMS preferring an online MBI.
And I don’t drive, and I know there are people in our community who have limited accessibility or they can’t drive, so online was perfect. (Se, Pg. 5, P3) [Citation32]
I really enjoyed the online version of mindfulness program as I didn’t have to travel anywhere and could stay in the comfort of my own home. (Du, Pg. 5) [Citation30]
PwMS that preferred face-to-face MBIs over online ones outlined concerns relating to perceived security issues associated with the internet and the inability to interface with IT systems. One participant noted that an online intervention raised sensory and cognitive challenges that were potentially less marked in face-to-face groups.
It just takes a little more effort or a little bit more focus, paying attention a little bit to be able to connect with the other participants. In an onsite setting you can probably hear things a little bit better. You can just look in all directions and there you have a participant around you, and this [online], you have to look at each picture on the screen in front of you, and there might be movement going on in two different places. You have to focus on which one is the talking head or which one is not the talking head, that’s all. (Se, Pg. 5, P5) [Citation32]
On the other hand, another participant using a synchronous online format described the virtual platform as simple and easy to use, noting she would not be able to attend had it not been delivered online.
It’s easy [Zoom]. It’s so easy. I click on a link; I don’t have to put in a password. I played around with it on my phone and it didn’t take me long at all to learn how to do it. The easiest things are very hard for me, so it was just simple. One click to see the video and then another click to hear the audio and you’re in, so it worked good. (Se, Pg. 6, P5) [Citation32]
For me, it would be getting home from work, rush to eat, and then rush out to get somewhere else. There would’ve probably been a lot of times I didn’t make it to class if it wasn’t here [online]. (Se, Pg. 6, P5) [Citation32]
MS clinicians highlighted a perceived need for rapid and flexible access to MBIs for their patients, at times of need, and that ongoing access would be preferable to one-off courses.
It’s something I would sort of like to have quick access to for patients, particularly at times of diagnosis which is a time of emotional crisis. (Si19, Additional file 6, quote 9) [Citation33]
A sense of belonging
A sense of belonging related to what it was like for PwMS to come together as a group (among others with MS exclusively) to practice mindfulness, both face-to-face and synchronous online training. In three studies participants described initial trepidation about seeing other PwMS more disabled than themselves, a potential barrier to participation.
It seems silly because you live with MS every day, but actually sometimes when it’s spoken [the term MS] in front of you makes it very real indeed, so that, I think, I found difficult at times. I like that group aspect of it, in general, just at times I felt like “ouch!”. (Bo, Pg. 14) [Citation35]
If I see somebody very disabled by their MS, it’s really confronting and upsetting to me, because well, I’m lucky that it’s not me now, but there’s no way of telling what it will be like in the future, and that’s really scary. (Ses, P14, Pg. 5) [Citation31]
A consistent finding across studies of group-based MBIs was a sense of shared identity, solidarity, and belonging, which brought with it the opportunity to network and share ideas about how to cope with MS.
Well, it’s always nice to have the camaraderie of people in similar situations. In this case, it was all women, which most of us with MS are, or more of us. (Se, Pg. 6, P13) [Citation32]
Camaraderie…we learn a lot of things off each other…I only know one person with MS my age, and luckily she lives close, but it’s nice to be able to talk to other people, even if it’s just in passing, like how was your week, just understanding like we’ve all probably had some of the same things happen to us, and it feels like a nice community to be able to not, I don’t know, we have something in common. (Se, Pg. 5, P3) [Citation32]
The weekly live sessions were a great opportunity to hear other people’s experiences and problems they face as we are all different. Found the live sessions helped me to stay focused. (Du, Pg. 5) [Citation30]
Commonality of the disease I found very helpful cause you’re all going through and can share the same difficulties and often the same fears. (Bo, Pg. 14) [Citation35]
Experiencing mindfulness
Experiencing mindfulness constituted developing an understanding of the mindfulness approach to one’s experiences (particularly with regards to having MS), and the important role of the MBI instructor(s) in facilitating participation and effecting positive change. Participants spoke about their fear of becoming more mindful, particularly with regards to distressing and unpleasant experiences, but also identified benefits from staying present with moment-by-moment experiences. The development of compassion towards oneself and acceptance of MS was also discussed in this context, as was a perceived beneficial change in relating to others.
Participants did not always know what to expect from the mindfulness course. For some the approach was counter-intuitive, for others there was a fear of what training in mindfulness skills might unearth.
If something happens to me like I couldn’t move my arms or my legs I didn’t focus on oh I can’t do that I just thought I’m going to make them move I’m going to do that and I felt as if other people were oh I’ve got a pain, oh I’ve got this, I’ve got that and I thought I can’t do that, I can’t sit and listen to that. . I wasn’t getting anything out of it as in I tend to try and focus on the positivity, the positivity, the exercising, the pushing myself. (Si19, Additional file 6, P9) [Citation33]
I had a reservation that it might make me unhappy, because not understanding, very much about it, I thought I’m not really sure if I’m quite ready to accept what I’m going to learn about myself. I did think about that at the start and I do feel like I’m not scared by it anymore. (Bo, Pg. 11) [Citation35]
An MS clinician felt it was important to manage expectations upfront and set realistic treatment goals prior to undertaking an MBI.
I think there are some misunderstandings about what people are expecting to achieve. So, I would hope any courses would start off by being clear about what the goals or lack of goals actually are and modify expectations. (Si19, Additional file 6, C4, quote 2) [Citation33]
In one study, after it became clear that expectations between participants and the MBI instructors were mismatched, the subsequent MBI course was modified to include an orientation session. This change was seen as positive by the MBI instructors and in a subsequent study, an orientation session was included on this basis.
The intro week was very important. It worked well. We had a bunch that started in week one who were right up for it, they were enthusiastic, they’d had the taster, they knew what they were coming into and it really worked well. (Si18, Pg. 8, I2) [Citation34]
However, even with an orientation session, it was not always clear to participants why they were doing what they were.
I think at the beginning I was confused about what we were supposed to do because every week it was like adding another thing and I would get overwhelmed, like I have to do a body scan and a mediation of this and try the kindness thing. It felt like I don’t know what I should do…I just tried different things on different days, but in the beginning, I wasn’t sure. (Se, Pg. 6, P3) [Citation32]
In group-based MBIs, the course instructors were identified as having an important role in facilitating engagement, understanding, and participation.
Angeliki brings people into things and encourages them in really well which is great…getting that group mentality embedded is quite important. (Bo, Pg. 14) [Citation35]
…they were very good at talking through the actual meditation practice, they were approachable, they became involved in the group, they were easy to speak to, they always checked if everybody was ok. (Si18, Pg. 6, P42) [Citation34]
Indeed, in an individual, asynchronous, web-based MBI, the importance of access to an MBI instructor for learning, even if over the phone, was highlighted by one participant.
To me, I would like follow-up contact. Especially if you develop a rapport with somebody, it’s good to have follow-up contact. That definitely helps with learning a concept, to get a certain amount of rapport and follow-up. (Ses, P1, Pg. 6) [Citation31]
The mindfulness approach was experienced differently by participants. For one, becoming mindful demarked a change from automatic responding towards a greater appreciation of underlying emotional and somatic processes.
Rather than have an automatic cycle between how you feel, your emotions your body your mind, it lays it out a little bit more. (Bo, P12) [Citation35]
Through practicing mindfulness, participants described an enhanced ability to choose how to respond to moment-by-moment experience, in some instances using the practices adaptively to cope with unpleasant experiences.
If you know you’re responding in a particular way you can steer it in another direction, if necessary. You can follow the reflex response if you want or you wish to. You have the choice. It was interesting to think actually I can have a bigger control over my response. (Bo, Pg. 13) [Citation35]
Meditation and body scan are an amazing distraction if you need to remain calm and still. I used it at the dentist and found that my body was not tense or focussed on the drill while I was practising it. Very useful time to use it. (Du, Pg. 5) [Citation30]
Other participants described developing a novel appreciation of the present moment, in some cases being awestruck by this shift in awareness, which felt good. Another participant described a shift from focusing on the loss of function to a deeper appreciation of her abilities that were still present.
I’m talking about like two minutes to actually appreciate things that you would never have done before, I’m terrified of birds but during the course I found myself at the kitchen window being in awe of a robin and it was amazing it was nothing else mattered in those two minutes and it made me feel really good. (Si18, Pg. 7, P35) [Citation34]
Learning about finding some insignificant little facet of daily living, and not just immersing yourself in it, being very grateful and thankful of it… when I was gardening, having my fingers down in the soil and planting the flowers … not just appreciating the beauty of it, but appreciating the life that’s in it and all of the components that make that plant, like worms and the bugs and the sun and the rain and all of these little things that go into it. Just things that you knew existed, but you never spent time thinking about it and it kind of makes me very grateful, very thankful to be alive and to be able to experience it… being grateful for the abilities that I do have and not really mourning or giving a whole lot of space in my head for the things that I no longer can do. (Se, Pg. 4, P5) [Citation32]
The MBI instructors felt that physical illness and impairment resulting from MS presented a delicate context in which to introduce self-compassion practices.
We did teach compassion practices … but it was also a new and interesting idea that once one demonstrates compassion towards one- self, and I think people actually, you know, this was, actually brought up … that in MS the body is turning against itself and it’s interesting to try and be, actually advocate kindness towards the body. (Si18, Pg. 6, I1) [Citation34]
Indeed, PwMS reported an enhanced awareness of self-criticism and harshness towards themselves, something which appeared to change over the course of the MBI, with an increased sense of acceptance towards MS also being reported.
An awful lot of MS people, we get really bad sort of spastic muscle spasms and I used to get so angry … you know sort of like shouting and swearing and things because there is nothing you can do except wait until it goes, but I learned to be calmer about the episodes, more gentle about it and that really worked very well and that still works. (Si18, Pg. 7, P45) [Citation34]
I really truly think that I’ve moved on, quite a few steps towards acceptance of this god-awful condition that we’ve all got. I can say it quite cheerfully and be quite pragmatic. (Bo, P11) [Citation35]
Making MBIs more relevant and sustainable for PwMS
In all studies in this review, participants suggested they would recommend mindfulness to other PwMS. Indeed, some PwMS suggested they would be more likely to see the value and participate in an MBI if recommended by another person with the condition, or by a doctor. There was no consensus on the best time to learn mindfulness in the MS journey. Making MBIs more relevant for PwMS centered around addressing preconceptions among PwMS about MBIs, learning new skills and gaining information that might help with specific MS-related symptoms, and tailoring MBI materials to PwMS by including scientific evidence of benefit, having testaments from PwMS about usefulness, and by providing worked case examples.
In one study participants described how their presuppositions about mindfulness may have influenced involvement.
It’s based on Eastern philosophies and I thought, I can relate a little bit to that. If you were really task driven, I think you’d struggle with it. (Bo, P14) [Citation35]
I’m not really into these sorts of self-help; you know thinking about and analysing things and whatever I’m just a sort of getting on with it more pragmatic person. (Bo, P15) [Citation35]
PwMS emphasized they would be more likely to participate in an MBI if knowing it would address specific symptoms, particularly if recommended by their doctor.
If it’s something like ‘Yeah we can help to work on that anxiety, or work on some things’ and its geared towards people with MS, I think that would be really helpful. (Ses, P2, Pg. 6) [Citation31]
I think it would make it less likely for me to get benefit from it because I’d be so skeptical. If one of my doctors said, or if my psychiatrist who had MS said, [to do it] I certainly would. (Ses, P8, Pg. 6) [Citation31]
Participants and MS clinicians both highlighted the importance of involving PwMS in design and delivery of MBIs for this population, and both stakeholder groups felt case examples, were beneficial.
I don’t think you can have mixed abilities walking round and everybody happy. I just felt the delivery needed to be a bit more sensitive to the needs of people with MS and MS is very different from chronic fatigue or any other thing like that. it might have been better to have somebody who has actually been ill or not been well to have an input into the delivery on the course. (Si19, Additional file 6, quote 1) [Citation33]
If I had a case to go by, I could say yeah ok that sounds familiar, and then go from there…because with a lot of the stuff it’s like is this supposed to happen? Does it happen to people with MS or does it happen to everyone? So it would be good to have case studies. (Ses, P3, Pg. 6) [Citation31]
Participants emphasized the need to provide participants with a package of course materials, to help with organization, and that font size should be large to accommodate for visual impairment (a common comorbidity among PwMS) [Citation8].
I’m not that organized, so now I have to go back because I really want to print everything because I want to organize it, because I want to save it for future use…Well, like I have papers all over the place now, so I really want to go back and organize it. (Se, Pg. 6, P4) [Citation32]
It’s silly, but the helpful thing is the font size for me. I have to put my glasses on, but I really like that. (Se, Pg. 6, P6) [Citation32]
As mindfulness was new to many participants, there was a lot of contextual learning. The iterative nature of the learning was emphasized and appreciated.
I didn’t know that with this class, it was going to require so much relearning and rethinking the process of it. I thought oh, it’s just going to be presenting one plan, here’s what you do and that will fix it. But no, this is gradually learning something, like learning a language. You just learn a little bit more and you take it in and it’s just a gradual process. (Se, Pg. 5, P5) [Citation32]
A layered approach to learning mindfulness was suggested as beneficial by participants, starting out with shorter practices and building from there.
I like that it was a stepping-stone, that it started off with easier things to do, like a ten-minute body scan or whatever, and then it got more difficult…I liked the layers. (Se, Pg. 5, P1) [Citation32]
MBI instructors reported a perception that participants’ experience of physical disability had to be carefully acknowledged when teaching PwMS about mindfulness and that the implementation of meditation practices done in an informed and flexible manner.
You really had to take on board disability. . to see how it played out in people’s lives. .because we were with them so long and just having to really witness and hear about it. (Si19, Additional file 6, I2, quote 7) [Citation33]
Cautious about the walking, very carefully framing that, adapting the mindful movement, making lots of choice, as the body scan, whether people are lying or sitting. (Si19, Additional file 6, I1, quote 12) [Citation33]
This fitted with participant accounts of initial difficulties with some of the practices which served to accentuate a sense of disability that in some cases may have been suppressed.
On a personal matter because of the tremor in my right hand I can’t write now so if there’s anything involving writing I found it personally embarrassing to me because it was barely legible so I didn’t like they parts of the course. (Si19, Additional file 6, P16, quote 6) [Citation33]
I hated the body scan because it was making me think about my body and it was making me aware of things that I wasn’t aware of because I was blanking them out of my mind. (Si18, Pg. 6, P45) [Citation34]
Perceived benefits reported by participants related to perspective-taking and modification of habitual response patterns in relation to common MS symptoms such as stress, pain, sleeping difficulties, and anger.
It didn’t change the sensations as such it changed my way of thinking about the sensation…my thought process, I wasn’t stressing about “oh my goodness this is, there’s a tingling here”, I was more relaxed about it and I accepted it you know. (Si18, Pg. 7, P12) [Citation34]
If I was to trip and stumble, rather than just get shouty in my head and swearing or whatever I’ll actually think about it but if I do it twice, if I trip twice I will then just go back to my old automatic angry response. (Bo, P13) [Citation35]
I’ve also noticed that I’m sleeping better at night - even if I have a shorter sleep it is uninterrupted, and I wake up feeling rested. (Du, Pg. 5) [Citation30]
Indeed, participants described mindfulness as providing them with tools to help them cope with MS.
Using the focusing techniques and accepting techniques for difficult problems that have been very invaluable. They are the tools that I will use. I see them as tools that you can use the same way you use a knife, a fork to eat your food, you know, use them as tools to help me manage my condition. (Bo, P11) [Citation35]
In terms of making MBIs more relevant within existing healthcare systems, MS clinicians advised seeing their patients derive benefit would be valuable, as would feedback from MBI instructors.
It’s whether they come back and say: “that was great” and stuff. “I’ve had some mindfulness and I feel much better for it.” And then if that can be backed up by the clinician, the clinician sending something which suggests, you know, here’s the score before and after treatment, that’d be good. (Si19, Additional file 6, C1, quote 13) [Citation33]
In terms of making MBIs more sustainable, PwMS suggested weekly emails or telephone reminders during the course, or booster sessions once the course was completed.
I’d be more likely to actually use the reminder if it was e-mail, because then I can sort of flag it and keep track of it. (Ses, P10, Pg. 6) [Citation31]
A drop in thing would be brilliant. I think we all asked, said we’d love to come back in three months and teach us all again. It’s the only course I’ve ever been on where I would actually be very happy to start at week 1 again because I know how worthwhile it all is and what good it has done me. And with just a bit of discipline from myself will continue for me in the future so I did think it was great. (Si19, Additional file 6, quote 11) [Citation33]
Discussion
Summary of main findings
This meta-aggregation has presented qualitative research findings from six studies assessing the experiences and views of MBIs by PwMS, MBI instructors, and MS clinicians. Across categories, four synthesized findings are described relating to accessing mindfulness, a sense of belonging that PwMS experience in group-based MBIs, how PwMS experience mindfulness, and how MBIs might be made more relevant and sustainable for PwMS. These synthesized findings can be used to inform the design and delivery of MBIs for PwMS, taking into consideration key stakeholder views, summarized below.
Making MBIs accessible to PwMS
Many PwMS and their clinicians know little about MBIs, the benefits these interventions can offer this population, and how to access an MBI for PwMS. PwMS who undertake MBIs report a desire for continued access, as do their clinicians. Access barriers to MBIs for PwMS relate to the work involved in attending a weekly face-to-face class for eight weeks where facilities for those with disabilities may be limited and thus for many an online MBI represents an acceptable alternative.
A sense of belonging
For many PwMS, a valued component of MBIs relates to a shared sense of belonging and camaraderie with others who face similar challenges. A group MBI may allow a useful forum for shared (mindful) experiencing, networking, and information exchange among PwMS that individual, asynchronous online MBIs might not.
Experiencing mindfulness
The MBI approach is not intuitive for all PwMS and involves a lot of learning about a novel (mindful) way to approach their experiences. PwMS appreciate the layered MBI approach, and the instructor has a key role in helping PwMS make sense of the practices, ensuring they are done correctly, and that distressing and unpleasant experiences are managed carefully.
Making mindfulness more relevant and sustainable for PwMS
PwMS seek out mindfulness training to help with symptoms such as stress, pain, and sleep impairment. In return, common symptoms and impairments should be taken into consideration in the design and delivery of MBIs for PwMS. Learning materials that are well organized, available in large font, that make it clear why mindfulness can help with MS are recommended by PwMS. Case examples of common MS symptoms and issues appear particularly relevant and helpful.
Comparison with existing literature
In keeping with the findings of this current study, the challenge of accessing face-to-face MBI training has been highlighted by people with stroke [Citation39], amyotrophic lateral sclerosis (ALS) [Citation40], and those with spinal cord injury (SCI) [Citation41]. Stroke survivors and people with ALS both describe that traveling to attend in-person mindfulness sessions as a challenge that might put them off [Citation39] whilst people with SCI report a perceived lack of provision for wheelchair user access rendering online training their only option [Citation41]. However, like PwMS, stroke survivors and people with ALS note benefit from sharing (mindful) experiences with their peers in a group setting [Citation39,Citation40]; something that may be underestimated by MBI instructors [Citation15]. People with SCI, like PwMS, highlight that MBI delivery style can impact the relevance and acceptability of the intervention, where a failure by MBI instructors to appreciate that distinct neurological impairment(s) (e.g., tetraplegia) can prevent participation in certain meditation practices (i.e., body scan) [Citation41]. Stroke survivors also highlight how cognitive difficulties make maintaining focus during longer mindfulness practices a challenge [Citation39]. Like PwMS, stroke survivors emphasize the crucial role of the MBI instructor [Citation39]. Both stroke survivors and people with ALS describe similar benefits to PwMS from practicing mindfulness, such as feeling relaxed [Citation39], less anxious, sleeping better, an enhanced ability to attend to the present moment, and improvements in family relationships [Citation40].
Strengths and limitations of the primary studies
This present study has highlighted a relative lack of published qualitative research studies into the experience and views of PwMS accessing MBIs. Indeed, no purely qualitative studies were identified. A low level of published qualitative studies in rehabilitation research has been highlighted as an important issue in need of attention [Citation42], though indications are this is improving [Citation43]. Mixed-methods health services research funding has increased in recent years [Citation44] and the approach is endorsed by highly influential research bodies, including the UK Medical Research Council [Citation45]. The value of a mixed-methods approach is apparent in this context when considering that the evidence derived from quantitative evidence syntheses [Citation16,Citation17] highlights issues with attrition and adherence from MBIs for PwMS, suggesting a need to explore further participant experience, acceptability, and accessibility.
In general, participant demographics were poorly reported in the studies included in this review. Although a range of ages, both sexes, and all MS phenotypes appear to have been included, poor reporting in individual studies limits interpretation and generalizability of findings from a review such as this, where very little detail was available regarding ethnicity, education level, marital/relationship, and employment status of participants. From those studies included in this review, PwMS with greater levels of disability (EDSS > 7.0) and/or cognitive impairment may be being excluded from studies. High levels of physical disability correlate closely with a greater degree of cognitive impairment in PwMS [Citation46]. Cognitive impairment is common in PwMS and treatment options are limited [Citation47]. A recent meta-analysis has indicated positive effects on cognitive functioning following MBI training in general populations [Citation48] whilst recent pilot studies among PwMS suggest benefit [Citation49–51].
All studies included in this review employed a qualitative descriptive methodology as part of mixed-methods assessments. In one case, the mixed methods approach was used to explore potential MBI treatment mechanisms, where the RCT reported large reductions in distress, explained in part (27–31%) by decentring; linked qualitative data revealed unmeasured common factors such as group dynamics and expectancy might also be contributing, and these factors could thus be hypothesis tested in a future quantitative study [Citation35,Citation36]. Other studies used mixed methods more so to answer complex questions pertaining to feasibility, acceptability, accessibility, perceived effects, potential effectiveness, or to understand more clearly factors accounting for adherence and attrition [Citation30,Citation33,Citation34,Citation37]. In one case, the mixed methods approach was used to address the feasibility, acceptability, and potential effectiveness of an online synchronous MBI vs face-to-face [Citation32,Citation38]. The final study opted for a mixed-methods approach to allow end-user co-development of a web-based asynchronous MBI for PwMS, to address acceptability and relevance, and hone content before moving on to an efficacy study [Citation31].
Mixed methods research allows a more comprehensive assessment when evaluating feasibility, acceptability, accessibility, and implementation of MBIs, where triangulation [Citation52] of data can assist in the development and testing of research hypotheses. However, where researchers have pre-conceived research questions, the focus of data collection and analysis may miss important views of PwMS and caveats on the acceptability and accessibility of these interventions. Although findings from this study provide a helpful pointer, how MBIs work generally, and specifically in the context of PwMS remains incompletely understood. Elsewhere, in people with chronic mental and physical health conditions (non-MS), an interpretative qualitative synthesis [Citation53] using meta-ethnography has helped develop a testable working model of MBIs, outlining a change process encompassing transitioning from “perceived safe certainties” of maladaptive responding patterns that exist prior to undertaking mindfulness training, through “safe uncertainty” as the MBI practices become more familiar and provide “safe” approaches to perceiving and dealing with challenging experience(s), to an eventual “grounded flexibility” where the MBI practices are embedded with an increased sense of self-efficacy, flexibility in responding and acceptance of the illness experience.
Strengths and weaknesses of this review
This review follows a series of quantitative systematic reviews and meta-analyses which evaluated the effectiveness of MBIs for PwMS. As such, the research team had a high degree of familiarity with the literature in this area with refined search criteria. However, it remains possible that relevant studies may have been missed during the database searches and due to resource constraints, we were unable to include articles in languages other than English – important when considering the origins of Mindfulness as a construct derived from Asia. Another important point is that two of the included studies [Citation33,Citation34] in this review were authored by the primary author of this meta-aggregation. Steps to address potential researcher bias included the use of multiple reviewers (RS, SS, MW), conscious efforts to practice reflexivity during the data extraction, analysis, and reporting phases [Citation54,Citation55], in addition to having senior academic oversight on the overall study and discussion of findings (ML, SWM).
Suggested “lines of action”
This systematic review and meta-aggregation adds several important insights regarding the use of MBIs for PwMS, typically not addressed in quantitative reviews on the topic, whereby recommendations can now be made regarding the following lines of action:
Population – PwMS who are older, more physically disabled, or have cognitive impairment should be included in future studies of feasibility, acceptability, accessibility, and effectiveness of MBIs.
Purpose – PwMS have identified that the MBI should focus on common MS symptoms, such as stress, anxiety, pain, and sleep impairment.
Design – The experience of PwMS suggests that their involvement in the iterative development of MBIs is important and that these interventions should take account of common MS impairments.
Formatting – PwMS have indicated MBSR and MBCT are both acceptable MBIs for this population, with no clear preference being expressed.
Instructor characteristics – PwMS have reported that an experienced and approachable MBI instructor plays a crucial role in learning to be mindful; something that may need careful consideration when designing asynchronous online MBIs for this population.
Method of delivery – PwMS report that face-to-face and online (synchronous and asynchronous), group or individual are acceptable MBI delivery methods.
Content – PwMS indicate tailoring of MBI content to improve its direct relevance to people with the condition is helpful, that is, via case examples.
Course materials – PwMS suggest these should be well organized and take account of visual impairment.
Promoting uptake – PwMS have highlighted that endorsement by other PwMS and/or their MS clinician would make them more likely to undertake MBI training.
Promoting adherence – PwMS have indicated that email prompts are helpful reminders to keep up the practices during the course, whilst post-course booster sessions are also likely beneficial when it comes to sustaining the benefits of mindfulness beyond course completion.
Conclusions
MBIs for PwMS need to take into consideration common symptoms and impairments associated with the condition where disability can limit access and participation. Face-to-face, synchronous, and asynchronous online all appear acceptable course formats for PwMS. However, PwMS undertaking an MBI value a sense of belonging that develops through shared (mindful) experiencing and highlight the critical role MBI instructors play in helping participants learn to be mindful. How MBIs are taught, their relevance, and sustainability could all be enhanced for PwMS by involving those affected in course design, delivery, and iterative refinement.
MAgg_Appendices_DR.docx
Download MS Word (20.6 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ramagopalan SV, Dobson R, Meier UC, et al. Multiple sclerosis: risk factors, prodromes, and potential causal pathways. Lancet Neurol. 2010;9(7):727–739.
- Marrie RA, Cohen J, Stuve O, et al. A systematic review of the incidence and prevalence of comorbidity in multiple sclerosis: overview. Mult Scler. 2015;21(3):263–281.
- Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of cochrane reviews. Cochr Database System Rev. 2019;(1):CD012732.
- Foley PL, Vesterinen HM, Laird BJ, et al. Prevalence and natural history of pain in adults with multiple sclerosis: systematic review and meta-analysis. Pain®. 2013;154(5):632–642.
- Wood B, Van Der Mei I, Ponsonby A-L, et al. Prevalence and concurrence of anxiety, depression and fatigue over time in multiple sclerosis. Mult Scler J. 2013;19(2):217–224.
- Marrie RA, Reider N, Cohen J, et al. A systematic review of the incidence and prevalence of sleep disorders and seizure disorders in multiple sclerosis. Mult Scler. 2015;21(3):342–349.
- Malcomson K, Lowe-Strong A, Dunwoody L. What can we learn from the personal insights of individuals living and coping with multiple sclerosis? Disabil Rehabil. 2008;30(9):662–674.
- Simpson RJ, McLean G, Guthrie B, et al. Physical and mental health comorbidity is common in people with multiple sclerosis: nationally representative cross-sectional population database analysis. BMC Neurol. 2014;14(1):128.
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47.
- Kabat-Zinn J. Wherever you go, there you are: mindfulness meditation in everyday life. Hyperion; 1994.
- Gu J, Strauss C, Bond R, et al. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and Meta-analysis of mediation studies. Clin Psychol Rev. 2015;37:1–12.
- Alsubaie M, Abbott R, Dunn B, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev. 2017;55:74–91.
- Parsons CE, Crane C, Parsons LJ, et al. Home practice in Mindfulness-Based cognitive therapy and Mindfulness-Based stress reduction: a systematic review and Meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav Res Ther. 2017;95:29–41.
- Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14(3):270–277.
- Van Aalderen JR, Breukers WJ, Reuzel RP, et al. The role of the teacher in mindfulness-based approaches: a qualitative study. Mindfulness. 2014;5(2):170–178.
- Simpson R, Simpson S, Ramparsad N, et al. Mindfulness-based interventions for mental well-being among people with multiple sclerosis: a systematic review and Meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry. 2019;90(9):1051–1058.
- Simpson R, Simpson S, Ramparsad N, et al. Effects of mindfulness-based interventions on physical symptoms in people with multiple sclerosis – a systematic review and meta-analysis. Mult Scler Relat Disord. 2020;38:101493.
- Simpson R, Booth J, Lawrence M, et al. Mindfulness based interventions in multiple sclerosis-a systematic review. BMC Neurol. 2014;14(1):15.
- Beatty L, Binnion C. A systematic review of predictors of, and reasons for, adherence to online psychological interventions. Int J Behav Med. 2016;23(6):776–794.
- Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350:h1258.
- Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing Meta-aggregation. Int J Evid Based Healthc. 2015;13(3):179–187.
- Hannes K, Lockwood C. Pragmatism as the philosophical foundation for the joanna briggs meta-aggregative approach to qualitative evidence synthesis. J Adv Nurs. 2011;67(7):1632–1642.
- Richardson WS, Wilson MC, Nishikawa J, et al. The well-built clinical question: a key to evidence-based decisions. ACP J Club. 1995;123(3):A12–A13.
- Kabat-Zinn J. Full catastrophe living: the program of the stress reduction clinic at the university of Massachusetts medical center. New York (NY): Delta; 1990.
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. New York (NY): Guilford Press; 2012.
- Lawrence M, Pringle J, Kerr S, et al. Stroke survivors’ and family members’ perspectives of multimodal lifestyle interventions for secondary prevention of stroke and transient ischemic attack: a qualitative review and meta-aggregation. Disabil Rehabil. 2016;38(1):11–21.
- Lockwood CP, Munn Z, Rittenmeyer L, et al. Systematic reviews of qualitative evidence. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Adelaide (Australia): JBI; 2020.
- Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
- Spitzer E, Pakenham KI. Evaluation of a brief community‐based mindfulness intervention for people with multiple sclerosis: a pilot study. Clin Psychol. 2018;22(2):182–191.
- Dunne J, Chih HJ, Begley A, et al. A randomised controlled trial to test the feasibility of online mindfulness programs for people with multiple sclerosis. Mult Scler Relat Disord. 2021;48:102728.
- Sesel A-L, Sharpe L, Beadnall HN, et al. Development of a web-based mindfulness program for people with multiple sclerosis: qualitative co-design study. J Med Internet Res. 2021;23(3):e19309.
- Sessanna L, Nisbet P, Alanazi N, et al. The experience of participating in an 8-week mindfulness based stress reduction plus sleep retraining course among women living with multiple sclerosis. Clin Nurs Res. 2021;30(5):558–566.
- Simpson R, Simpson S, Wood K, et al. Using normalisation process theory to understand barriers and facilitators to implementing mindfulness-based stress reduction for people with multiple sclerosis. Chronic Illn. 2019;15(4):306–318.
- Simpson R, Byrne S, Wood K, et al. Optimising mindfulness-based stress reduction for people with multiple sclerosis. Chronic Illn. 2018;14(2):154–166.
- Bogosian A, Hughes A, Norton S, et al. Potential treatment mechanisms in a mindfulness-based intervention for people with progressive multiple sclerosis. Br J Health Psychol. 2016;21(4):859–880.
- Bogosian A, Chadwick P, Windgassen S, et al. Distress improves after mindfulness training for progressive MS: a pilot randomised trial. Mult Scler. 2015;21(9):1184–1194.
- Simpson R, Mair FS, Mercer SW. Mindfulness-based stress reduction for people with multiple sclerosis–a feasibility randomised controlled trial. BMC Neurol. 2017;17(1):94.
- Lorenz RA, Auerbach S, Nisbet P, et al. Improving sleep among adults with multiple sclerosis using mindfulness plus sleep education. West J Nurs Res. 2021;43(3):273–283.
- Jani BD, Simpson R, Lawrence M, et al. Acceptability of mindfulness from the perspective of stroke survivors and caregivers: a qualitative study. Pilot Feasibility Stud. 2018;4(1):57.
- Marconi A, Gragnano G, Lunetta C, et al. The experience of meditation for people with amyotrophic lateral sclerosis and their caregivers – a qualitative analysis. Psychol Health Med. 2016;21(6):762–768.
- Hearn JH, Finlay KA, Sheffield D. ‘Trying to bring attention to your body when you’re not sure where it is’: an interpretative phenomenological analysis of drivers and barriers to mindfulness for people with spinal cord injury. Br J Health Psychol. 2021;26(1):161–178.
- Slade SC, Patel S, Underwood M, et al. Rigorous qualitative research in sports, exercise and musculoskeletal medicine journals is important and relevant. London (UK): BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2018.
- VanderKaay S, Moll SE, Gewurtz RE, et al. Qualitative research in rehabilitation science: opportunities, challenges, and future directions. Disabil Rehabil. 2018;40(6):705–713.
- Coyle CE, Schulman-Green D, Feder S, et al. Federal funding for mixed methods research in the health sciences in the United States: recent trends. J Mixed Meth Res. 2018;12(3):305–324.
- MedicalResearchCouncil. Developing and evaluating complex interventions: new guidance. London (UK): Medical Research Council; 2008.
- Lynch SG, Parmenter BA, Denney DR. The association between cognitive impairment and physical disability in multiple sclerosis. Mult Scler. 2005;11(4):469–476.
- Mitolo M, Venneri A, Wilkinson ID, et al. Cognitive rehabilitation in multiple sclerosis: a systematic review. J Neurol Sci. 2015;354(1–2):1–9.
- Lao S-A, Kissane D, Meadows G. Cognitive effects of MBSR/MBCT: a systematic review of neuropsychological outcomes. Conscious Cogn. 2016;45:109–123.
- Blankespoor RJ, Schellekens MP, Vos SH, et al. The effectiveness of mindfulness-based stress reduction on psychological distress and cognitive functioning in patients with multiple sclerosis: a pilot study. Mindfulness. 2017;8(5):1251–1258.
- Manglani HR, Samimy S, Schirda B, et al. Effects of 4-week mindfulness training versus adaptive cognitive training on processing speed and working memory in multiple sclerosis. Neuropsychology. 2020;34(5):591–604.
- De la Torre GG, Mato I, Doval S, et al. Neurocognitive and emotional status after one-year of mindfulness-based intervention in patients with relapsing-remitting multiple sclerosis. Appl Neuropsychol: Adult. 2020. DOI:10.1080/23279095.2020.1732388
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ. 2010;341:c4587.
- Malpass A, Carel H, Ridd M, et al. Transforming the perceptual situation: a meta-ethnography of qualitative work reporting patients’ experiences of mindfulness-based approaches. Mindfulness. 2012;3(1):60–75.
- Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320(7226):50–52.
- Hammersley M. Reading ethnographic research: a critical guide. Harlow (UK): Longman; 1990.