Abstract
Background
Patients in hospital following stroke express a desire to continue therapy tasks outside of treatment activities. However, they commonly describe experiences of boredom and inactivity. An enriched environment aims to provide opportunities for physical, cognitive and social activity and informed the development of a Communication Enhanced Environment (CEE) model to promote patient engagement in language activities.
Purpose
Explore patient perceptions of a CEE model, and barriers and facilitators to engagement in the model.
Methods
A qualitative description study from a larger project that implemented a CEE model into acute and rehabilitation private hospital wards in Western Australia. Semi-structured interviews were conducted with seven patients, including four with aphasia, within 22 days post-stroke who had access to the CEE model.
Results
Patients described variable experiences accessing different elements of the CEE model which were influenced by individual patient factors, staff factors, hospital features as well as staff time pressures. Those who were able to access elements of the CEE model described positive opportunities for engagement in language activities.
Conclusions
While findings are encouraging, further exploration of the feasibility of a CEE model in this complex setting is indicated to inform the development of this intervention.
Patient access to a CEE model is challenging in a hospital setting.
Patients who were able to access elements of the CEE model described positive opportunities for engagement in language activities.
Patients’ access to the CEE model was influenced by patient factors, staff factors, hospital features as well as staff time pressures.
Implications for rehabilitation
Introduction
It is recognised that the environment can influence neural remapping during early stroke recovery [Citation1]. However, the current hospital environment may reflect what is considered impoverished [Citation2–10] with patients following stroke spending large proportions of their day alone and inactive [Citation11]. Patients in hospital following a stroke express a desire to continue therapy tasks outside of treatment tasks, perceiving time outside of therapy as an opportunity to practise rehabilitation activities within the real-world environment [Citation12]. However, boredom is commonly experienced by patients which has the potential to negatively affect their engagement in rehabilitation [Citation13]. Patients report that a lack of meaningful activity is strongly associated with boredom [Citation13]. Boredom is highly correlated with depression and apathy and is perceived by patients to negatively affect their participation in stroke rehabilitation [Citation13]. Patients following stroke perceive a lack of stimulation and inactivity impacts their ability to “drive” their own rehabilitation outside of therapy, describing their time outside of their therapy as “dead and wasted” [Citation12].(p4) Nurses have been observed to be the most common communication partner for patients after their family members [Citation14]. However, nurses in a stroke rehabilitation unit report that time constraints often limit their capacity to comfort, talk with and provide education to patients [Citation15]. This lack of time for communication and education has also been identified by patients who “did not like to bother the busy nurse” [Citation16].
Aphasia is a communication disorder that occurs in approximately 30% of stroke survivors [Citation17] and affects all modalities of communication including speaking, listening, reading and writing. Aphasia is associated with higher levels of disability and has significant negative consequences for social participation, interpersonal relationships, autonomy, capacity to work and quality of life [Citation18]. Patients with aphasia (PWA) following stroke have been observed to spend less than 28% of their day communicating with others and 44% of their day alone during their first weeks of inpatient rehabilitation [Citation14]. Limited opportunities for language use, and engagement in meaningful activity and social interaction may negatively impact aphasia language recovery [Citation3] and have adverse consequences for health-related quality of life [Citation7]. This places PWA at increased risk of developing learned non-use of language as a result of inadequate opportunities for communication [Citation14].
An enriched environment (EE) aims to provide greater opportunities for physical, cognitive and social activity and has been shown to contribute to significant improvements in neuroplasticity, motor recovery and a trend towards significant improvements in cognition in animal stroke models [Citation19]. Application of EE in an acuteCitation7 and rehabilitation unit [Citation20] setting has been shown to significantly increase patient engagement in physical, cognitive and social activity. Aphasia is a complex language impairment and PWA may need support within an EE. The principles of EE informed the development of a Communication Enhanced Environment (CEE) model to facilitate engagement in language activities for patients following stroke, which incorporated the needs of those with aphasia [Citation21]. The definition of language activities encompassed any activity that involved the use of language including both solitary (i.e., reading, writing) and interactive (i.e., talking or listening to a communication partner) language activities. This CEE model was co-designed with hospital staff and considered hospital policies and procedures and incorporated evidence-based strategies, expert opinion, [Citation21] and staff and patient-perceived barriers and facilitators to their engagement in language activity following stroke [Citation22]. The CEE model sought to promote access to physically enhanced communal spaces, trained communication partners, resources, and organised social activities [Citation23]. Results from piloting the CEE model found that 71% of the model was reported to be available to the intervention group [Citation21]. Additionally, the intervention group who had access to the CEE model engaged in higher, but not significant, levels of language activities (600 of 816 observation time points, 73%) than the control group (551 of 835 observation time points, 66%) [Citation21].
This study sought to explore patient perceptions of communication interactions and language activity including the perceived barriers and facilitators to engagement in the CEE model during their hospital admission. The specific research questions were:
What are patients’ perceptions of communication interactions and language activities during their hospital admission following stroke where the CEE model was implemented in usual care?
What do patients perceive to be barriers and facilitators to engagement in the CEE model?
Methods
Design
This qualitative study was conducted as part of a larger project which developed, implemented, and evaluated a CEE model within two hospital wards.
There were three phases to the larger project:
Before phase: observed and quantified the usual care ward environments.
Implementation phase: developed and implemented the CEE model.
After phase: assessed the implementation and explored the effects of the Communication Enhanced Environment model.
Participants in this study were recruited to the after phase of the larger project where the CEE model was embedded in usual care. Semi-structured interviews were conducted between November 2018 to December 2019, within thirteen months of embedding a CEE model in the hospital wards. Ethics approval was obtained from Hollywood Private Hospital Research Ethics Committee (HPH431) and Edith Cowan University Research Ethics Committee (ECU HREC 12149). The trial protocol can be accessed via the supplementary file of a publication from the larger project [Citation22].
Methodological framework
A qualitative descriptive approach was utilised to explore patients’ experiences, perspectives and insights [Citation23]. This approach values description without the need for deep conceptualisation, or abstraction. It remains close to the words of the participants, seeks an accurate, comprehensive account of events as they choose to present them with only a low level of interpretation [Citation23,Citation24]. Qualitative description has been identified as an appropriate qualitative approach to inform the development and refinement of an intervention involving a vulnerable participant group [Citation23].
Setting
This study was conducted on two hospital wards, one acute/slow stream rehabilitation ward and one rehabilitation ward, at a private hospital in Perth, Western Australia. The acute/slow stream rehabilitation ward had 30 beds with patients following stroke and other medical conditions. There were 26 individual rooms and two shared rooms with two beds per room. The rehabilitation ward had 44 beds with patients following stroke and other medical, orthopaedic and post-surgical conditions. There were 36 individual rooms, and four shared rooms with two beds in each room. Patients ate breakfast in their rooms. Patients were usually encouraged to have lunch and dinner in a communal dining area. A reduction in the nurse-to-patient ratio occurred during the study period. The number of stroke admissions on the participating wards reduced over the study period which was not anticipated by the researchers. Please refer to the larger study’s main results paper [Citation21] for details of the staff levels and stroke admissions during the study period (in press).
Participant selection
All consecutively admitted patients following stroke were screened by two hospital site champions (a senior physiotherapist and a speech pathologist) for eligibility to participate in this study from November 2018 to December 2019, following implementation of a CEE model on the wards. This provided a sample that was aligned with naturally occurring heterogeneity of stroke survivors, rather than a purposive sample, to reflect the ‘real-world’ nature of this intervention. The larger study aimed to include eight patients following stroke in the after phase (PWA = 4; patients without aphasia (PWOA) = 4), a convenience sample to allow for patient observations across allocated time frames in the larger study (see related publication [Citation22] for further details). Despite the focus of aphasia within a CEE model, this intervention also sought to meet the communication needs and experiences of inactivity for those without aphasia therefore PWOA were also included in this study.
Patients were eligible for inclusion if they were: admitted to the participating wards and were within 21 days post-stroke at the time of recruitment; had the ability to provide informed consent as determined by the hospital medical team; a Glasgow Coma Scale [Citation25] score greater than 10 at the time of screening; an estimated length of stay greater than 14 days; and adequate English proficiency to participate in interviews. Patients were excluded if they: had a hearing impairment without hearing aids or had a vision impairment which impacted on reading; were medically unstable; had a documented diagnosis of dementia, traumatic brain injury, previous aphasia or current untreated depression; or were a participant in another research trial which may have affected the outcome measures of this study. PWA were identified through usual ward aphasia screening completed by the ward speech pathologist. The presence of aphasia was confirmed with a Western Aphasia Battery-Revised [Citation26] Aphasia Quotient less than 93.7.
Twelve patients met the inclusion and exclusion criteria. These patients were approached by the site champions to obtain verbal consent to meet the first author to discuss participation in the study. Eight patients consented to participate in the study. One participant withdrew their consent prior to the commencement of data collection (they did not provide a reason). Data collection was completed for seven participants (PWA = 4, PWOA = 3). Participant demographics, stroke and aphasia characteristics are summarised in .
Table 1. Patient demographics, stroke and aphasia characteristics.
Intervention
The CEE model comprised of communication partner training for staff, access to language and communication promoting resources and equipment, and enhancement and access to communal areas (communal areas were only available on the rehabilitation ward) (). The CEE model was then embedded in the usual care ward environments over an 11-week period prior to participant recruitment. Please refer to the larger study’s main results paper [Citation21] (in press) for more details on the CEE model initiatives and implementation process. Availability of the CEE model was monitored for each participant by the hospital site champions (). All patients were on the talking program. The afternoon tea was not run for two PWA because of low staffing and one PWOA did not attend the afternoon tea because of a clash with a Physiotherapy session. Volunteer orientation to the ward occurred for two PWA. Two PWA declined the electronic tablet loan. One PWA had access to the communal area. Two PWA and two PWOA attended the afternoon tea. Although communal dining and access to communal areas were targeted within the CEE model, patients had limited access to communal areas as a result of circumstances which were not anticipated by the researchers. One of the participating wards moved during the study period (implementation phase) to become a combined acute/slow stream rehabilitation ward. This new ward did not have a communal area. Additionally, patients on the rehabilitation ward did not have access to the communal dining area for meals due to limited staffing capacity to transfer patients into these areas. This was likely the result of a reduction in the nurse-to-patient ratio that occurred during the study period. Please see the larger study’s main results paper [Citation21] for further details (in press). The CEE model and aphasia communication partner training were provided to multidisciplinary team members: rehabilitation nurses (n = 8); acute/slow stream rehabilitation nurses (n = 8); volunteers (n = 20); physiotherapists (n = 17); occupational therapists (n = 7); an occupational therapy assistant (n = 1); a dietitian (n = 1); social workers (n = 5); speech pathologists (n = 4); and a speech pathology assistant (n = 1). However, training was not provided to all ward staff as attendance to training was voluntary and some staff opted not to receive training, some staff were unable to attend the training sessions as a result of personal leave, and some new or casual relief staff who were present on the ward at the time of patient recruitment and data collection were not working on the ward during the implementation phase of the larger study when training was provided.
Table 2. The CEE model initiatives and participant involvement in each initiative.
Interviewer characteristics
Data collection was completed by the first author, a female speech pathologist (Bachelor of Speech Pathology, Honours) with seven years clinical experience working in the hospital setting, and eight years research experience including conducting interviews and focus groups. Rapport with participants was developed over a three-day data collection period involving 12 h of patient observations (as part of the larger study).
The larger project formed the basis of the first author’s PhD to develop and investigate a CEE model. Rigour was enhanced through the utilisation of strategies during data collection and analysis to ensure the authenticity of the data and the credibility of the findings to maintain the integrity of the data and research findings. These strategies included clarifying participant responses during interviews, second review of themes and ensuring the data were driven by the participants. To ensure the data were participant driven, the interviewer waited until the participant had finished telling their stories before asking probing questions to clarify or seek further information [Citation30].
Data collection methods
Patients were not informed about the CEE model. They were informed that the researcher wanted to explore the effect of the hospital environment on patient activity and patient perspectives about in-patient activity. One PWA requested to have two family members present during the interviews, otherwise the interviews were conducted in a one-on-one setting within the participant’s hospital room. This allowed in-depth discussion and probing to facilitate their discussion about potentially distressing or sensitive topics [Citation30]. Interviews with PWA were conducted using supported communication strategies [Citation29] to facilitate participation and successful information exchange. All audio-recorded interviews were conducted within 22 days post-stroke and lasted between 20–45 min. The interviewer took field notes during the interviews to capture participants’ use of non-verbal communication during the interviews such as their use gesture, facial expression and writing.
An interview guide was used for all interviews (). In addition to the questions in the interview guide, participants were also asked to discuss their experiences with each CEE model initiative they had been exposed to. Additionally, questions were also asked of individuals based on comments they made regarding the environment during the participant observation component of the larger study. Clarification of participant responses and the interviewer’s interpretations of these responses were completed during the interviews to confirm the data were representative of participants’ opinions, experiences and perceptions. This was completed during data collection, rather than after data analysis, as patients may not have recognised their individual personal story within the data as a result of the breaking up and categorisation of data during analysis [Citation30]. Additionally, reading deficits are common in aphasia therefore returning transcripts for member checking may not have been accessible to this participant group.
Table 3. Patient interview guide.
Data analysis
All interviews were transcribed verbatim. The data were analysed within NVivo 12 [Citation31] computer software with the data coded according to content. The codes were identified from the data and then organised into categories as common themes recurred through the interviews. These categories were grouped according to thematic content to identify the main themes. The data surrounding the quotes were categorised with the coded quotes, to maintain the context of the data during coding. Ongoing critical review of themes were conducted including a re-review of the data and themes completed by the first author. A second author reviewed the themes to help ensure that categorisation was data driven [Citation23].
Results
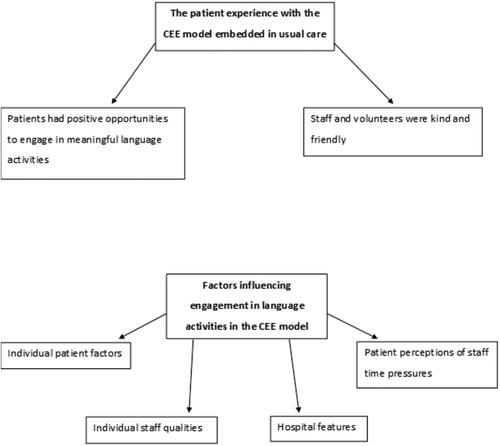
The themes were related to patients’ experiences of a CEE model and factors influencing their engagement in elements of the CEE model. Patient experiences were predominantly related to positive encounters with the model initiatives and the impression that staff and volunteers were friendly and caring. Factors influencing engagement with the CEE model were related to individual patient factors, individual staff qualities and hospital features. See for visual representation of the results.
The patient experience with the CEE model embedded in usual care
Patients had positive opportunities to engage in meaningful language activities
Overall, the elements of the CEE model appeared to provide patients with opportunities to engage in solitary and interactive language activities. Patients reported their enjoyment participating in meaningful activities within their experiences with different elements of the CEE model including the afternoon tea, the talking program, tablet loans and joint Speech Pathology-multidisciplinary sessions. Patients perceived that staff and volunteers engaging with them contributed to them feeling welcomed and supported.
Yes, they both took me [walking] and we went down one corridor and another and up, and up, and up, that sort of thing…it was very good [joint Speech Pathology-multidisciplinary sessions] (PWA1)
I’ve been um, I’ve been meeting with people socially [afternoon tea] a couple of very nice people and chatted. Mainly they’ve chatted, haven’t been much to it [sic] but I listen to it quite a bit (PWA2)
There was a young lady… I was having a bad day… it was an awful day, and she was very kind she sat and talked to me for a while … it was very good [to talk to her] she was very kind… it was very easy [volunteer talking program] (PWA1)
Yeah, a lot of people [come into my room and talk to me] …I find it good, that’s good. They don’t have to do that … what was it like? Good, you just feel welcomed in the place [talking program] (PWOA1)
Yes, it was very good to have the iPad except that I forgot how to use it again… someone came to my rescue I think [tablet loans for audiobooks and communication apps] (PWA1)
I found it quite enlightening to get my point across from [sic] to someone that works at the hospital as a volunteer. It was quite interesting, and they seem interested in me… it made me feel more receptive to them because they seem to be interested in me [volunteer talking program] (PWA3)
Staff and volunteers were kind and friendly
Patients perceived staff and volunteers as friendly as they offered help and were happy and kind when interacting with them, which contributed to patients’ positive perceptions of care. This may have also contributed to patient engagement in interactions with staff and volunteers.
Well, they seem younger and freer and happy (PWA2)
People in here are fantastic they really are… they always check to make sure you’re alright, always willing to help (PWOA1)
They are always willing to help, and they will do whatever they can, every request, they will try to do it (PWOA2)
I thought the staff were very nice, and very nice, yes [sic] (PWA4)
Factors influencing engagement in language activities in a CEE model
Individual patient factors
Patients talked about their own preferences, abilities or restrictions that influenced their participation and engagement in various elements of the CEE model. These included their initiative in seeking out communication opportunities or modifying their physical surroundings to increase the accessibility of the environment, their desire to be social, and their personalities.
Well, I’m an old chatter box. What you, what you [sic], all you have to do when you talk to people is smile and then they’re right (PWA2)
I got offered an iPad. I refused it…one, I don’t like apple, two, it wasn’t really interactive, it was pretty much this a f a is a pic [sic] picture… (PWA3)
I don’t need to call people to come to get something… the phone, so if it’s facing that way and I’m sitting this side, I can’t reach that side, so every time I make sure it’s facing me and that I can reach (PWOA2)
Patients talked about the impact of their experiences with negative moods and tiredness which reduced their engagement in language activities.
The first few days I was ah, very lethargic, I didn’t feel like doing anything and feeling uh, feeling lazy and not wanting to do anything… I could not think of going on to the computer, that tired (PWOA2)
I’m an avid reader but I haven’t been able to settle down and read in the place, I don’t know why, it’s just a peculiarity, must be the [my] mood (PWOA3)
They also talked about their physical limitations such as mobility, hearing impairments and aphasia affecting their autonomy and independence, and restricting their opportunities to engage in language activities.
Well, I don’t talk a lot because I’m a bit slow now and I’ve got to think mostly before I speak, so I haven’t gone a long way with that (PWA1)
It was stultifying, you’re lying on the bed and you’re just completely at liberty to doze off there’s nothing to stop you, so that’s what you do… It’s just restriction of course. If I was able to walk up and down the passage I’d get up and do that, so it’s an artificial barrier that’s been put there that I haven’t had to deal with before… a big barrier and that affects you in a whole host of ways, you know… you ring the bell it could be 15 minutes before they turn up and um you get caught short so it’s not good you see something in the corner there. I can’t get over there unless I ring the bell and get the nurse to take me, you know, so the boundaries are even smaller than they look when you first walk in here. For somebody who is reasonably active like me finds it quite hard, yeah so, they’re the moans and groans (PWOA3)
Individual staff qualities
Although patients talked about positive experiences with staff in a CEE model, they also discussed their reliance on staff to engage in the CEE model. Some patients relied on staff to assist with setting up hearing aids, charging or explaining how to use a tablet, and running the afternoon tea. This theme was more prevalent for patients who were more dependent and reliant on staff to assist in engaging in the CEE model.
I haven’t offered very much [at the afternoon tea] only because sometimes we’ve gone early in the morning… I’ve just had a shower then we whipped off quickly. I haven’t had time to get organised hearing aids and things like that, so I have been missing a lot of what was being said… yeah, I tried to [get my hearing aids] but they go too quickly, too early, they don’t wait, so I couldn’t set up and I’m battling to hear properly (PWA1)
Yes it [electronic tablet] [laughs] went off… the battery… powered off… no nobody did, no [charged the electronic tablet] …it is quite interesting [audiobook on the electronic tablet] you know what I had so far. It’s sad that it just went straight away, it went … the battery went out (PWA4)
Staff individual qualities such as their accents, whether they were perceived as being friendly, whether they gave time to interactions with patients despite being busy or whether they prioritised other clinical tasks, or whether or not staff were perceived to be patient, influenced patient engagement in language activities.
Some of the staff are willing to understand and give you time to formulated [sic] what you want to say, so that’s good… some people they don’t have the patience. I’ve had a couple of issues, run ins, with people where they haven’t taken tim [sic], the time to try and understand what I’m trying to say and I’m getting frustrated because I think they’re not listening (PWA3)
Um, well people who don’t speak our language maybe I don’t hear properly, you know, their conversation is a little bit different to ours and so you miss some of the things (PWA1)
Hospital features
Patients talked about a range of hospital-related factors impacting their ability to engage with the CEE model initiatives. Patients described the physical environment restricting their access to communication opportunities as they perceived they needed to stay in their rooms. They talked about the nature of busy time periods and quieter periods on the weekends resulting in variable opportunities for interactions with staff and other patients. They also described the limitation of scheduled therapy sessions which affected access to elements of the CEE model such as attending the weekly scheduled afternoon tea.
There’s a lot that I wish I could have been doing, I mean walking around the building talking to people, having a coffee, a bad coffee, or just going outside amongst the trees listening to the breeze but I can understand why they want to keep people like me contained because they want to keep track of me and what’s going on (PWA3)
Yeah, the weekends, it’s just a feeling, I suppose the whole place virtually closes down which is from Friday night onwards, so the physio [sic] so the physios halve, there’s no physios on, on Sunday, so that eliminates any sort of outside the ward type of activity, so for the rest of it, there’s not much of it, not at all. Staff seem to be reduced. You get the feeling that it’s all closed down (PWOA3)
Well, I don’t communicate a lot, though they have these afternoon teas, but I’ve never been in a position to go to one [because of scheduled Physiotherapy sessions], so the only time I communicate with other patients is at the physio sessions and they’re all business, so mostly it’s mostly the nurses I communicate with (PWOA3)
Patient perceptions of staff time pressures in the hospital environment
Patient perceptions of staff time pressures in the hospital environment related to both staff individual factors as well as hospital related factors. Patients talked about their perceptions of staff time constraints impacting their engagement in language activities and communication interactions with staff. Patients described about how staff were “rush[ing]” and “buzzing around” which contributed to their perception of them being busy. This may reflect staff appearing to be busy and as a result, patients did not want to contribute further to this. Patients also talked about experiences where staff told them they were too busy. Therefore, this theme is likely reflective of the busy hospital environment and time constraints related to clinical demands in this environment, as well as staff’s individual ways of working in a busy environment, for example, their ability to manage a busy caseload without appearing as though they are rushing.
No, I couldn’t get nurses [to help with the electronic tablet], they were too busy. Everyone said the nurse will help you, but they said “no”, they are too busy (PWA1)
They’re always buzzing around. I have a bit of a chat with the doctor when he comes around but that’s limited too because of their busy schedule (PWOA3)
It’s not their fault they’ve only got a limited amount of time… it’s rush, rush, rush… sometimes it’s been emotionally draining cos you feel like what’s the point? What am I doing? But you eventually learn to live with it and understand the system… I can understand the staff frustration because they feel rush, rush, rush, and they have a limited amount of time per patient. It’s not the staff’s [sic] fault, it’s not management’s fault, it’s just the way things work out (PWA3)
Discussion
This study revealed patient perceptions of communication interactions and language activity, and their perceptions of barriers and facilitators to engagement in the CEE model during their in-patient hospital admission. Patients described variable experiences accessing different elements of the CEE model which were influenced by a range of perceived individual patient factors, staff factors, hospital features as well as staff time pressures. For those that were able to access elements of the CEE model, they described positive opportunities for engagement in language activities. Preliminary results suggest a trend towards increased patient engagement in language activities when the CEE model was embedded in usual stroke care, [Citation18] and results from this study indicate that those who were able to access elements of the CEE model viewed their experiences positively.
Patients’ preferences for and ability to engage in elements of the CEE model were highly individual. For example, some patients declined elements of the CEE model, such as the loaned electronic tablet. Some patients were able to initiate activities within their rooms and sought out communication opportunities, whereas others who were restricted to their bedside were more reliant on staff who were perceived to be busy. Some patients reported the impact of their mood and levels of fatigue on their desire to engage in activity. Therapy schedules limited one patient’s opportunities to attend the afternoon tea and engage in communication activities in the evenings and on weekends. The challenges that patients experienced in accessing the CEE model are in line with a recent Phase II feasibility study exploring EE [Citation32]. The study found individual driven enrichment activities were difficult for patients to access and were rarely within sight or reach [Citation32]. Within the larger project associated with the current study, 71% of the CEE model was reported to be available to the intervention group [Citation21]. However, this qualitative exploration of patient experiences with the CEE model embedded in usual care reveals the complex nature of accessing the CEE model in the hospital setting. Contextual issues are considered a common barrier limiting the implementation of evidence in practice [Citation33] and highlight the challenging nature of implementing interventions in a busy, complex ward environment. Further exploration of the feasibility and uptake of the CEE model will need to be addressed within the hospital setting as a next step in exploring the CEE model in this complex setting.
The CEE model did not involve a bedside pack, which may have exacerbated patients’ reliance on time-poor staff, and the impact of reduced staffing after hours and on weekends. This was particularly evident for patients who were more physically dependent and less autonomous in initiating interactions or modifying the physical environment to aid communication accessibility. Previous studies investigating an EE found that patients’ reduced mobility acted as a barrier to engaging activities within the model [Citation34]. These patients were: more reliant on staff to engage in activities such as transferring into communal areas; more likely to be restricted to activities at their bedside; and more likely to report feelings of boredom [Citation34]. Boredom is associated with a loss of autonomy and sense of control and contributes to patients becoming passive recipients of care, which may have negative implications for stroke recovery [Citation13]. Planned future development of the CEE model will include the provision of a bedside pack which would include individualised language activities such as music, books, magazines and word puzzles. It will also include prescribed communication therapy resources to provide more variety in language activities to cater to different individual preferences. However, the accessibility of the bedside pack will be an important consideration to promote patient-driven access which incorporates the needs of those who are dependent for their mobility in busy hospital settings to reduce the impact of relying on busy staff.
In this study, some patients talked about negative experiences with staff who did not take the time to interact with them, staff who told patients they were too busy, or patients’ perceptions of staff being impatient when engaging with them, which appeared to contribute to feelings of hopelessness. In the usual care hospital environment prior to implementing the CEE model, time limitations were identified by hospital staff as having a negative effect on their ability to engage in communication with patients [Citation22]. Staff also reported avoiding interactions with PWA if they felt unskilled or felt they were unable to support communication breakdowns [Citation22]. Within the current study, communication partner training was not provided to all ward staff, therefore patients interacted with both trained and untrained staff. Additionally, there were reductions in staffing levels during the data collection period which may have contributed to staff time pressures, and patients’ perceptions of staff time pressures [Citation21]. Research suggests interactions with health professionals who lack training and skills in interacting with PWA can be disempowering for PWA and can increase the potential for adverse events in hospital [Citation26]. Previous studies have found that communication partner training can save time and reduce frustration for staff, reduce the burden of caring for PWA, reduce the risk of preventable adverse events and improve patients’ overall health care experience [Citation16,Citation35–38]. Therefore, it is essential to ensure all staff who interact with PWA receive communication partner training to provide supportive communication behaviours in order to minimise the impact of unskilled staff on patient experiences and their long-term health outcomes.
Patient experiences, including communication and social opportunities, were different for each participant within the CEE model because of their individual levels of deficit or personal preferences. However, there were points of commonality in that patients largely perceived staff and volunteers as kind and friendly, and reported enjoying engaging in meaningful activity for those that were able to access the CEE model. Patients talked about feeling welcomed and enlightened by their experiences interacting with staff and volunteers, and largely viewed them as kind and caring. Patients valued staff who were willing to help, and appreciated being ‘checked’, something which patients perceived were behaviours staff “didn’t have to do”. Patients’ perceptions of care during their stroke recovery appeared to be entwined with positive interactions and willingness by staff and volunteers to assist patients to engage in communication interactions and language activities. Patients also reported engaging in meaningful social interactions and activities while engaging in CEE model initiatives including attending the afternoon tea, using the loaned electronic tablets to listen to audiobooks, participating in joint Speech Pathology-multidisciplinary therapy sessions and talking with staff and volunteers within the talking program. Patients also described feelings of disappointment in missing out on social activities within the CEE model. For patients who were able to access the intervention, the CEE model appeared to provide opportunities to engage in enjoyable and meaningful activities and appeared to promote care through kind and friendly interactions with staff.
Strengths and limitations
To our knowledge, this is the first study to investigate patient insights into their experiences in hospital following stroke with a CEE model implemented in usual care. This study assists in determining the value of a CEE model. This study provided valuable insights into patient experiences of communication interactions and language activity, and their perceptions of barriers and facilitators to engagement in the CEE model initiatives during their hospital admission with the CEE model implemented in usual care. Findings from this study will inform the ongoing development of the CEE model.
As this was a pilot study, there was a relatively small participant sample size. Future studies with larger sample sizes may provide a wider range of perspectives particularly given the factors influencing patient engagement in a CEE model may be different for each participant. Some participants had difficulty accessing the CEE model and were therefore less able to describe their experiences of the model. Additionally, the activities and experiences discussed by patients may be related to patients’ broader experience of their admission and therefore may not be directly attributable to the CEE model specifically. This study was completed at a private hospital therefore the results may not be directly transferrable to other healthcare contexts.
Conclusion
This exploration of patient experiences with the CEE model embedded in usual care reveals the complex nature of accessing the CEE model in the hospital setting. Patients described variable experiences accessing different elements of the CEE model which were influenced by a range of individual patient factors, staff factors, hospital features as well as staff time pressures. For those who were able to access elements of the CEE model, they described positive opportunities for engagement in language activities. The CEE model was perceived to provide patients with opportunities to engage in meaningful language activities which appeared to positively influence their perceptions of their hospital admission. Despite the expected individuality of patient feedback, there were common findings which demonstrate that perceptions of care are entwined with positive interactions and willingness by staff and volunteers to assist patients to engage in meaningful activities. The findings of this study highlight the impact of the hospital ward environment on patient experience and demonstrate the potential for environmental interventions such as the CEE model to improve patient health care experience and stroke outcomes. However, further exploration of the feasibility and uptake of the intervention will need to be addressed within the hospital setting as the next step in exploring a CEE model in this complex setting.
Reporting guidelines checklist
The consolidated criteria for reporting qualitative studies (COREQ [Citation39]) was used to guide the reporting of this study (Appendix A).
Acknowledgement
The authors sincerely thank all the stroke survivor participants in this study who were willing to share their insights into their experiences in hospital during their early recovery. The authors thank the hospital working party team who developed and embedded the CEE model and all the staff who participated in this research. The authors extend this thank you to Claire Tucak, Millie Gallan-Dwyer, Sarah Wynn and Toni Dalzell for all their work in the design and development of this study and to Dominie Scott, Jamie Smith and Lana Rojas for their willingness to assist the site champions in screening potential study participants.
Disclosure statement
The authors have no other competing interests to declare.
Data availability statement
Data are available upon reasonable request. Data are stored in the Edith Cowan University data storage repository. These data will be available in a de-identified format by request through the first author ORCiD https://orcid.org/0000-0001-6221-3229. The availability and use of the data are governed by Edith Cowan University Research Ethics.
Additional information
Funding
References
- Kolb B, Teskey GC. Age, experience, injury, and the changing brain. Dev Psychobiol. 2012;54(3):311–325.
- Anåker A, von Koch L, Heylighen A, et al. "It's Lonely": patients' experiences of the physical environment at a newly built stroke unit”. Herd. 2019;12(3):141–152.
- King A, McCluskey A, Schurr K. The time use and activity levels of inpatients in a co-located acute and rehabilitation stroke unit: an observational study. Top Stroke Rehabil. 2011;18(6):654–665.
- Maben J, Griffiths P, Penfold C, et al. One size fits all? Mixed methods evaluation of the impact of 100% single-room accommodation on staff and patient experience, safety and costs. BMJ Qual Saf. 2016;25(4):241–256.
- McDonald MW, Hayward K, Rosbergen IC, et al. Is environmental enrichment ready for clinical application in human post-stroke rehabilitation. Front Behav Neurosci. 2018;12:135.
- Persson E, Anderberg P, Kristensson Ekwall A. A room of one's own: being cared for in a hospital with a single-bed room design. Scand J Caring Sci. 2015;29(2):340–346.
- Rosbergen ICM, Grimley RS, Hayward KS, et al. Embedding an enriched environment in an acute stroke unit increases activity in people with stroke: a controlled before-after pilot study. Clin Rehabil. 2017;31(11):1516–1528.
- Shannon MM, Lipson-Smith R, Elf M, et al. Bringing the single versus multi-patient room debate to vulnerable patient populations: a systematic review of the impact of room types on hospitalized older people and people with neurological disorders. Intell Build Int. 2018. DOI:10.1080/17508975.2018.1548339.
- Singh I, Subhan Z, Krishnan M, et al. Loneliness among older people in hospitals: a comparative study between single rooms and multi-bedded wards to evaluate current health service within the same organisation. J Gerontol Geriatr. 2016;2(3):1015.
- West T, Bernhardt J. Physical activity in hospitalised stroke patients. Stroke Res Treat. 2012;2012:813765–813713.
- Janssen H, Ada L, Bernhardt J, et al. Physical, cognitive and social activity levels of stroke patients undergoing rehabilitation within a mixed rehabilitation unit. Clin Rehabil. 2014;28(1):91–101.
- Eng X, Brauer SG, Kuys SS, et al. Factors affecting the ability of the stroke survivor to drive their own recovery outside of therapy during inpatient stroke rehabilitation. Stroke Res Treat. 2014;2014:626538
- Kenah K, Bernhardt J, Cumming T, et al. Boredom in patients with acquired brain injuries during inpatient rehabilitation: a scoping review. Disabil Rehabil. 2018;40(22):2713–2722.
- Godecke E, Armstrong E, Hersh D, et al. Missed Opportunities: communicative interactions in early stroke recovery. Conference presentation at Stroke Society of Australasia Annual Scientific Meeting; 2014. Hamilton Island, Queensland
- Ball JE, Murrells T, Rafferty AM, et al. 'Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf. 2014;23(2):116–125.
- McCabe C. Nurse-patient communication: an exploration of patients' experiences. J Clin Nurs. 2004;13(1):41–49.
- Engelter AT, Gostynski M, Papa S, et al. Epidemiology of aphasia attributable to first ischemic stroke: incidence, severity, fluency, etiology, and thrombolysis. Stroke. 2006;37(6):1379–1384.
- Kruithof WJ, van Mierlo ML, Visser-Meily JM, et al. Associations between social support and stroke survivors' health-related quality of life: a systematic review. Patient Educ Couns. 2013;93(2):169–176.
- Janssen H, Bernhardt J, Collier JM, et al. An enriched environment improves sensorimotor function post–ischemic stroke. Neurorehabil Neural Repair. 2010;24(9):802–813.
- Janssen H, Ada L, Bernhardt J, et al. An enriched environment increases activity in stroke patients undergoing rehabilitation in a mixed rehabilitation unit: a pilot non-randomized controlled trial. Disabil Rehabil. 2014;36(3):255–262.
- D’Souza S, Godecke E, Ciccone N, et al. Investigation of the implementation of a communication enhanced environment on an acute and a rehabilitation ward: a before-and-after pilot study. Clin Rehabil. (in press).
- D'Souza S, Godecke E, Ciccone N, et al. Hospital staff, volunteers' and patients' perceptions of barriers and facilitators to communication following stroke in an acute and a rehabilitation private hospital ward: a qualitative description study. BMJ Open. 2021;11(5):e043897.
- Neergaard MA, Olesen F, Andersen RS, et al. Qualitative description: the poor cousin of health research? BMC Med Res Methodol. 2009;9:52–57.
- Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2(7872):81–84.
- Kertesz A. Western aphasia Battery- Revised. San Antonio, TX: Harcourt Assessment; 2006.
- NIH stroke scale [Internet]. Bethesda, Md, National Institute of Neurological Disorders and Stroke (U.S.). 2011. [cited 2016 Feb 10]. Available from https://www.ninds.nih.gov/sites/default/files/NIH_Stroke_Scale.pdf.
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699.
- Kagan A. Supported conversation for adults with aphasia: methods and resources for training conversation partners. Aphasiology. 1998;12(9):816–830.
- Milne J, Oberle K. Enhancing rigour in qualitative description: a case study. J Wound Ostomy Continence Nurs. 2005;32(6):413–420.
- NVivo qualitative data analysis software. QSR International Pty Ltd. Version. 12. 2018.
- Janssen H, Ada L, Middleton S, et al. Altering the rehabilitation environment to improve stroke survivor activity: a phase II trial. Int J Stroke. 2021. DOI:10.1177/17474930211006999.
- Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283:112376. DOI:10.1016/j.psychres.2019.04.025.
- White JH, Bartley E, Janssen H, et al. Exploring stroke survivor experience of participation in an enriched environment: a qualitative study. Disabil Rehabil. 2015;37(7):593–600.
- McGilton K, Sorin-Peters R, Sidani S, et al. Focus on communication: increasing the opportunity for successful staff-patient interactions. Int J Older People Nurs. 2011;6(1):13–24.
- Legg C, Young L, Bryer A. Training sixth-year medical students in obtaining case-history information from adults with aphasia. Aphasiology. 2005;19(6):559–575.
- Street RL, Makoul G, Arora NK, et al. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301.
- Hersh D, Godecke E, Armstrong E, et al. Ward talk”: nurses’ interaction with people with and without aphasia in the very early period poststroke. Aphasiology. 2016;30(5):609–628.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
Appendix a
Appendix A. Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.