Abstract
Purpose
Fear of falling (FoF) is a common and debilitating problem for older people. Most multicomponent interventions show only moderate effects. Exploring the effective components may help in the optimization of treatments for FoF.
Materials and methods
In a systematic review of five scientific literature databases, we identified randomized controlled trials with older community-dwelling people that included FoF as an outcome. There was no restriction on types of interventions. Two reviewers extracted information about outcomes and content of interventions. Intervention content was coded with a coding scheme of 68 intervention components. We compared all studies with a component to those without using univariate meta-regressions.
Results
Sixty-six studies, reporting on 85 interventions, were included in the systematic review. In the meta-regressions (n = 49), few components were associated with intervention effects at the first available follow up after the intervention, but interventions with meditation, holistic exercises (such as Tai Chi or Pilates) or body awareness were significantly more effective than interventions without these components. Interventions with self-monitoring, balance exercises, or tailoring were less effective compared to those without these components.
Conclusions
The identified components may be important for the design and optimization of treatments to reduce FoF.
Fear of falling (FoF) is a common and debilitating issue among older people and multicomponent interventions usually show only small to moderate effects on FoF.
This review and meta-analysis investigated 68 intervention components and their relation to intervention effects on FoF.
Interventions with meditation, holistic exercises (such as Tai Chi), or body awareness are more effective than interventions without these components.
Clinicians aiming to reduce FoF may recommend selected interventions to older people taking into account the current knowledge of intervention components.
Implications for rehabilitation
Introduction
The percentage of people aged 60 or over is projected to increase worldwide from 12% in 2015 to 22% in 2050 [Citation1]. One of the factors which is important in old age is fear of falling (FoF). The prevalence of FoF typically ranges between 21% and 85%, varying by the older population under study and the measure that is used [Citation2–5]. In 1990, FoF was conceptualized as “low perceived self-efficacy at avoiding falls”, when the Falls Efficacy Scale (FES) was developed to operationalize this construct [Citation6]. In previous studies, the term FoF has been used interchangeably to refer to cognitive based constructs (e.g., balance confidence or fall-related self-efficacy) and affect-based constructs (e.g., concern or worry about falling). In this review, “fear of falling” is used as an umbrella term and includes both constructs. Both people with and without any recent falls experience FoF [Citation8–10] and is associated with activity avoidance, social isolation, decreased physical functioning, and future falls [Citation2,Citation5,Citation11]. In addition, FoF is a debilitating condition that affects quality of life and may lead to premature nursing home admission [Citation2,Citation12]. Consequently, interventions to effectively reduce FoF in older community dwelling people are important.
The effects of interventions on FoF have been summarized in previous studies. Meta-analyses of the effectiveness of interventions to reduce FoF mostly focused on specific types of interventions, such as cognitive behavioral therapy (CBT) or exercise, which have shown small to moderate reductions in FoF [Citation13–16]. In addition to meta-analyses that focus on the effectiveness of single types of interventions, there are also meta-analyses that have compared the effectiveness of different types of interventions. In such an analysis of 24 studies by Rand et al., Tai Chi was associated with a moderate effect and other exercise and multifactorial interventions with a small effect [Citation17]. Furthermore, Jung et al. found a small to moderate effect of combined exercise and education interventions (n = 2) and a non-significant small effect for exercise only interventions (n = 3), suggesting that combining education and exercise is more effective than exercise alone [Citation18]. These studies indicate that different types of interventions can reduce FoF in older people, although often only small or moderate effects were found.
So far, interventions have been examined on a meta-level, i.e., they were labeled and analyzed according to their most prominent feature (e.g., cognitive behavioral approach, exercise, etc.). Less prominent features may contribute to the intervention effects as well. Interventions often include different components that are assumed to contribute towards the intervention effect, such as goal setting, self-monitoring, exercise, and nutritional supplementation. Studying the effectiveness of such components seems relevant for optimizing interventions. Studies in other areas have shown that different intervention components contribute to the outcome. For example, for cancer patients, the inclusion of social cognitive theory-based components like modeling of behavior, goal setting, and help in setting realistic expectations, were beneficial to improve overall quality of life [Citation19]. Classifying interventions according to their intervention components, may provide insight into components that could be strengthened or removed to optimize interventions and achieve larger or prolonged effects [Citation20]. Components to effectively reduce FoF have not yet been studied. In the present systematic review and meta-analysis of RCTs with FoF as outcome, we explore the association between specific intervention components and the reduction of FoF among community-dwelling older people. All intervention types are included and control groups received either no intervention or usual care.
Materials and methods
The international prospective register of systematic reviews (PROSPERO) holds the protocol of this systematic review and meta-analysis, registration ID CRD42018080483. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used for the reporting of this review [Citation21] (supplementary file 1). Online supplementary information is available at the Journal website and the Open Science Framework, https://doi.org/10.17605/OSF.IO/SF67D
Search strategy
On 30 November 2020, the databases CENTRAL, CINAHL, EMBASE, PsycINFO, and PubMed were searched for articles published after 1 July 2005. Publication date was not an eligibility criterion and the systematic review performed by Zijlstra et al. was used to identify articles that were published before 1 July 2005 [Citation7]. To supplement the current systematic search, three additional search strategies were employed to identify articles published before and after 1 July 2005. First, experts that recently published about falling or FoF were contacted. Second, reviews and meta-analyses primarily directed at FoF were screened for potentially relevant articles. Lastly, protocol papers that emerged from the search strategy were used to identify published articles. Searches were filtered to include only publications written in Dutch or English. Keywords relating to FoF, randomized controlled trials and older adults were combined with “AND”. The full search strategy is available online (supplementary file 2).
Study selection process
Eligibility criteria
Criteria have been reported in detail elsewhere [Citation22]. In short, to be included, articles had to report on the results of a randomized controlled trial conducted in non-institutionalized populations with a mean age of ≥65 years. In addition, FoF had to be an outcome of the study and the control group could receive only usual care or nothing (including wait-list control). Articles were excluded when they were not written in English or Dutch or when they were aimed at populations with specific diseases or health conditions, such as Parkinson’s or stroke. The reason for using language as a criterion in addition to using it as a search filter, was that abstracts are often in English and scientific databases do not always recognize other languages from full texts.
Title and abstract screening
Two reviewers (authors MK and GARZ) screened the first 200 titles and abstracts independently. The following order was used in checking titles and abstracts against eligibility criteria: design of the study, age of the included sample, living situation of the sample, health of the study participants, FoF as outcome and language. The percentage of agreement between reviewers on whether to look at the full texts was 95.5%. A kappa of 0.67 suggested there was good interrater reliability [Citation23]. Consequently, the remaining titles and abstracts were screened for eligibility by one reviewer (author MK). An article also advanced to the full text phase when doubt remained after reading the title and abstract. In addition, articles from the review by Zijlstra et al. [Citation7] were screened against eligibility criteria of the current study, because the current study has one additional criterion for the control group.
Full text screening
To screen full texts, the following order of checking against criteria was applied: language, design of the study, control group, age of the included sample, living situation of the sample, health of the study participants, and FoF as outcome. One reviewer (author MK) screened all full texts. Studies were excluded when one or more criteria were not clear, e.g., if the age of the population was not reported. When doubt remained about inclusion, articles were discussed with a second reviewer (RC, GIJMK, or GARZ) and agreement was reached.
Data extraction
Pairs of two reviewers extracted data independently with a data-extraction form (authors MK, RC, GIJMK, KD, KLC, DK, SI, GARZ). Reviewers were not involved in data extraction of articles in which they were involved as a co-author. The extraction form can be found online. Extracted information included bibliographic information and information about the study design, population, content of the intervention, FoF measures and results, and risk of bias. For about 25% of the articles identified in the first round of searching (12 articles), the content of the interventions was independently screened for intervention components by two reviewers (authors MK and GARZ). In this study, intervention components were defined as “content-related ingredients of an intervention that have the potential to causally influence outcomes” [Citation24]. Examples of intervention components are goal setting, feedback, home modification, hip protectors, tailoring, increase in difficulty and discussion. A coding scheme was developed based on intervention mapping, the behavior change technique (BCT) taxonomy and falls taxonomy [Citation25–27], and refined in several rounds of consensus meetings. For an overview of the interventions components and coding conditions, see the coding scheme in supplementary file 3. When the component was mentioned as part of the intervention, it was coded as 1 (present). If not, it was coded as 0 (not present). When intervention descriptions were unclear regarding the presence of a certain component, the component was coded as missing. Aspects belonging to usual care were not coded, meaning that only components that were unique to the intervention group were extracted. Remaining intervention texts were coded by one reviewer (author MK). In case of any ambiguity during the coding process, a second reviewer (RC, KD, or GARZ) was consulted and agreement reached. Studies in which the intervention content was completely tailored and there was no clear indication of what participants could receive, were included in the overall meta-analysis but not in the meta-regressions (see below for the performed analyses). Results on FoF were extracted at two separate time points, i.e., the first and the last available assessment in the study at hand. Data were extracted for all intervention arms. We contacted authors when the data presented in an article were not suitable for meta-analysis, e.g., if results were presented in figures only. When the data could not be provided, the article was excluded for the meta-analysis. If a reference to a protocol or main study article was included in an article’s intervention description, this reference was checked for additional information about the intervention. Selection bias (two items), performance bias, detection bias, attrition bias, reporting bias, and other types of bias were assessed in a separate extraction form with the Cochrane Collaboration’s Tool to assess risk of bias in RCTs [Citation28].
Analysis
The means, standard deviations (SDs), and numbers of participants of the intervention and control group were used to estimate the standardized mean difference (SMD) in FoF for each study. Calculation of standardized effects is appropriate when different measures are pooled [Citation29]. If regression coefficients representing mean differences between the intervention and control group were reported, these were used instead of follow-up means. Standard errors (SEs) or 95% confidence intervals (95% CI) were used to calculate SDs if these were not reported. See the online material for an overview of the applied formulas. If appropriate, scales were inverted to make sure a high score represented a high level of FoF. The following interpretation was used for the B: 0.2 is a small effect, 0.5 is a moderate effect, and 0.8 is a large effect [Citation30].
We pooled SMDs at the first available follow up after the intervention with random effects meta-analysis. We started with estimating main effects on FoF in an overall meta-analysis. Subsequently, we estimated associations between intervention components and the SMD at the first available follow up with univariate meta-regression. The regression coefficient represents the difference in the SMD between interventions with (coded as 1) and without (coded as 0) the component in question. In case of multiple intervention arms, the intervention arm listed first in the article’s abstract was the one used in the primary analyses. Statistical significance was set at p < 0.05.
The following pre-specified sensitivity analyses were performed to investigate the robustness of the results and the methodological decisions: (I) using the other intervention arm of a study in meta-regressions, if more than one intervention arm was involved, (II) removing the cluster RCTs from the meta-regressions, (III) using the results of the latest assessment to perform meta-regressions, (IV) using study quality (the number of high risk bias items) as a continuous variable in a meta-regression, (V) restricting analyses to studies with the best study quality (two high risk bias items), (VI) performing a separate meta-analysis on cognitive-based FOF measures (e.g., FES, Activities-specific Balance Confidence Scale (ABC)) and affect-based FOF measures (e.g., Falls Efficacy Scale-International (FES-I), the Survey of Activities and Fear of Falling in the Elderly (SAFFE)), and (VII) removing outliers from the meta-regressions. Furthermore, two of our components deviated from the BCT and falls taxonomy and we performed sensitivity analysis in which we (VIII) combined the components “support”, “motivational strategy – supervisor”, and “motivational strategy – peer”, as is the case in the BCT taxonomy, and (IX) combined “walking strategies” and “balance”, as is the case in the falls taxonomy. Lastly, we (X) combined the components “assistive devices” and “home adaptation”, as home adaptations such as a grab bar could also be defined as an assistive device.
To assess statistical heterogeneity (an estimate of between study variation), I2 and Q test statistics were used. The following interpretations from the Cochrane handbook were used: “0–40%: might not be important; 30–60%: may represent moderate heterogeneity*; 50–90%: may represent substantial heterogeneity*; 75–100%: considerable heterogeneity *” [Citation31]. We investigated components that could occur in a range of intervention types, e.g., in home visits, cognitive behavioral interventions, or exercise interventions. As we pooled different types of interventions, we expected heterogeneity in the overall meta-analysis to be high. The intervention components could potentially explain some of the heterogeneity. Egger’s test was used to statistically assess publication bias. In addition, funnel plots were visually inspected for publication bias. Outliers were determined by inspection of the forest and funnel plot. All analyses were performed with STATA version 15 (College Station, TX), metan package.
Results
Study selection
A flowchart of the study selection process is shown in . A total of 12 551 unique records from five literature databases were screened. After screening the titles and abstracts and reading the full texts, 99 articles reporting on 66 unique trials could be included in the systematic review. The data of several studies (n = 15) were unsuitable for inclusion in the meta-analyses because intervention descriptions or scales used to measure FoF were unclear, or means or SDs were missing and data could not be retrieved by estimation or contacting the author. Fifty-one studies with data on 52 intervention groups were included in meta-analysis.
Figure 1. Flowchart of study selection process. Adapted from Moher et al. [Citation21].
![Figure 1. Flowchart of study selection process. Adapted from Moher et al. [Citation21].](/cms/asset/766b52a9-319f-46a8-b372-d7986a29bc38/idre_a_1969452_f0001_c.jpg)
Description of studies
A full description of included studies, including their designs, primary outcomes, sample characteristics, and FoF measures is available online. Briefly, most studies were parallel group RCTs (n = 57), but cluster RCTs (n = 5) and crossover RCTS (n = 4) were also present. Designs with three (n = 15) or four (n = 2) arms were included, but the majority of studies had two study arms (n = 49). Twenty-one studies assessed FoF more than once after the intervention. The risk of bias scoring can be viewed online and in supplementary file 5. In short, the number of high risk of bias items ranged from two to four out of the total of seven items. Due to the nature of the interventions, blinding was impossible and the two items regarding blinding of participants and personnel and outcome assessors (performance bias and detection bias) were always scored with a high risk of bias.
Description of components
Sixty-six studies reported on 85 interventions. See supplementary file 4 for an overview of intervention components per intervention and supplementary file 3 for a detailed description of intervention components. A total of 68 different components were identified. A mean of 11 components (range 2–46) was reported in the interventions. Great diversity of components was evident in the studies, such as discussion, education, balance exercises, strength exercises, graded tasks, relaxation, feedback, goal setting, diet, energy conservation, visualization, and home adaptation. Components most frequently embedded in the interventions were balance exercises (n = 35), an increase in difficulty (n = 52), motivating the participants (n = 29), repetition (n = 80), strength training (n = 39), tailoring (n = 52), and a warm-up (n = 30). Some components rarely occurred. For example, podiatry and feedback by peers only occurred twice and visualization and providing participants with hip protectors only occurred once. For three studies [Citation32–34], the content of the intervention was completely tailored to the individual and there was no clear indication of what participants received.
Meta-analysis
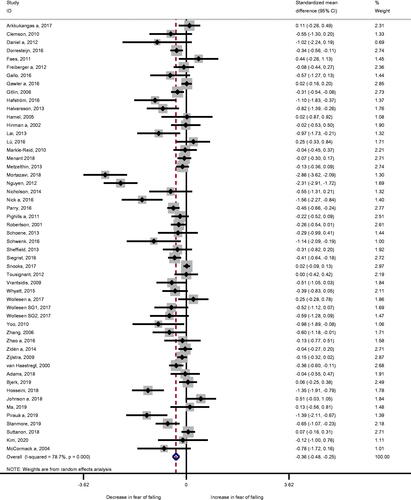
All interventions pooled together were associated with a small to moderate reduction in FoF at the first available assessment after the intervention (, B: −0.36; 95% CI: −0.48; −0.25; I2: 78.7%, p < 0.001; n = 52). There was significant publication bias (p < 0.001) and six outliers could be determined [Citation35–40]. Without these six outliers, the remaining interventions were associated with a small reduction in FoF (B: −0.20; 95% CI: −0.28; −0.12; I2: 52.3%; p < 0.001; n = 46). The overall estimates for cognitive-based and affect-based measures were similar (–0.37 and −0.36, respectively, sensitivity analysis V). Additional results, such as the funnel plot and the forest plots for sensitivity analyses are available online.
Meta-regression
Of 68 components, 66 could be included in univariate meta-regressions. For the remaining two components, there were no studies with the component that could be included in the meta-regression. The univariate meta-regressions showed that most intervention components were not significantly associated with effects on FoF (see supplementary file 3 and ). Body awareness (B: −0.53; 95% CI: −0.93; −0.13; n = 11 out of 49), holistic exercises (B: −0.67; 95% CI: −1.10; −0.24; n = 9 out of 49) and meditation (B: −0.79; 95% CI: −1.35; −0.23; n = 5 out of 49) were significantly associated with a decrease in the SMD, meaning they were more effective in reducing FoF than interventions without these components. The intervention components balance (B: 0.45; 95% CI: 0.11; 0.78; n = 22 out of 49), self-monitoring (B: 0.44; 95% CI: 0.02; 0.86; n = 10 out of 48), and tailoring (B: 0.52; 95% CI: 0.16; 0.87; n = 28 out of 47) were significantly associated with an increase in the SMD. This indicates that interventions with these components were significantly less effective in reducing FoF than studies without these components. Bubble plots that visualize the results of the aforementioned significant components are available online (see supplementary file 6).
Table 1. Meta-regression results for intervention components for the first available follow-up after the intervention.
Overall, our sensitivity analyses confirmed the robustness of the results (see the footnotes in for an overview of results from sensitivity analyses). The changes that did occur mainly followed from repeating the meta-regressions with the results of the last assessment (sensitivity analysis III) and repeating meta-regressions without outliers (sensitivity analysis VII). When repeating meta-regressions with a smaller sample of 15 studies that measured FoF at a later time point, most previously mentioned significant associations disappeared. For tailoring, this sensitivity analysis could not be performed due to a lack of studies without tailoring. When six outliers identified based on the funnel plot were removed, tailoring, self-monitoring, body-awareness, holistic exercises, and meditation were no longer associated with the SMD. Study quality (sensitivity analysis IV) was not significantly associated with the SMD.
Discussion
Overall, the interventions in our meta-analysis (n = 52) resulted in a small-to-moderate reduction in FoF in community-dwelling older people (SMD-0.36 [95% CI: −0.48; −0.25]). We explored the content of interventions, as a first step to gaining insight into the contribution of specific components to this reduction. We identified 68 different components, of which 66 could be included in univariate meta-regressions. Most of these intervention components were not associated with an intervention effect on FoF. However, interventions with body awareness exercises, holistic exercises, or meditation were significantly more effective in reducing FoF than interventions without these components. In contrast, interventions with balance training, self-monitoring, or tailoring were significantly less effective in reducing FoF than interventions that did not include these components. Considering long-term effectiveness, only 15 interventions in our meta-regressions included more than one follow up. When we analyzed these studies, most previously mentioned components were no longer significant. However, it is likely this analysis was underpowered and therefore, long-term effects are still uncertain. Other sensitivity analyses generally confirmed the robustness of these results. When six outliers identified based on the funnel plot were removed, a different pattern of associations appeared in which tailoring, self-monitoring, body-awareness exercises, holistic exercises, and meditation were no longer identified as significant. However, four of the six outliers were highly effective studies of holistic exercise interventions, often including elements of body awareness and meditation, but not self-monitoring or tailoring. As the associations disappear when these effective studies are removed, this could indicate that holistic exercise, body awareness, and meditation are among the most effective components to reduce FoF. The intervention studies included in our meta-analysis consistently scored a high risk of bias on two items, regarding blinding of participants and personnel (performance bias) and outcome assessment (detection bias). It is worthwhile to stress that it is very difficult to achieve blinding in these kind of studies (in comparison with, e.g., pharmacological trials) [Citation41]. Furthermore, when participants are aware of their group allocation and outcome measurement is based on self-report, the potential for detection bias is high.
To the best of our knowledge, no previous meta-analyses have examined the content of interventions on the level of components for the outcome FoF. Usually, the content of interventions is classified according to their most prominent feature. Rand et al. [Citation17] conducted a meta-analysis of 24 studies and found larger effects on FoF for Tai Chi than for other exercise interventions or multifactorial interventions, which is in line with the findings of the current study. Kendrick et al. [Citation16] found no significant differences in effect on FoF by exercise type in their meta-analysis of 24 exercise interventions. This difference in results with the current study may be due to differences in analysis methods and eligibility criteria or the inclusion of more recent studies, such as the study by Mortazavi et al. [Citation37], presenting a highly effective Tai Chi intervention.
Several findings that may be relevant to current practice are observed. First, in falls prevention, balance training and tailoring are generally considered as beneficial [Citation42–45]. However, in the current study, interventions including balance training or tailoring were less effective for reducing FoF compared to interventions that did not include these components. Second, self-monitoring was less effective in the current study, while self-monitoring has previously demonstrated effectiveness for a range of health behaviors, including taking up exercise [Citation46]. There may be several reasons for these apparent inconsistencies. Falls and FoF are different concepts that may require different treatments with different intervention components, i.e., effective intervention components may differ for FoF and falls risk. For instance, tailoring could help older people become more aware of their fall risk, which can be beneficial for the intention to participate in fall prevention programs [Citation43,Citation47], but may not be beneficial for FoF. In a qualitative study, some persons with Parkinson’s disease, indicated the awareness of their risk of falling increased their FoF [Citation48]. Furthermore, without returning to “multicomponent” interventions, it may be possible that analyzing a combination of two or more components may provide more insight. Combinations of components may be required to reduce FoF. For instance, balance exercises may need to be offered in combination with cognitive restructuring in order to reduce FoF or repetition may be beneficial for exercise, but not for discussion. The theoretical underpinning required to formulate hypotheses and to investigate combinations with standard meta-regression techniques is lacking so far. Other data-driven techniques, like meta-CART, require sufficient data for the intervention components under study [Citation49]. The current meta-analysis lacked sufficient data for some components. Lastly, other aspects of interventions and their effect on FoF may need to be taken into account. For example, for FoF, interventions may need to be longer, for participants not only to master skills, but also to gain confidence by incorporating these skills in daily life.
The strengths of the current study include its systematic survey of five scientific databases, rigorous quality assessment and its detailed overview of intervention components. This study was also subject to several limitations, leading to recommendations for future research. First of all, because of the diversity of interventions that included FoF as an outcome, there were no suitable pre-existing overall taxonomies that could be used in coding our components. Therefore, our components guide was tailor made to suit our study and future studies may provide additional validation. Furthermore, we considered this an exploratory study and we did not use a correction for multiple testing. This may have caused a risk of type 1 error. Moreover, we came across a large variation in the level of detail of intervention descriptions and some interventions reported only a few main components. It is possible that some interventions did not report on the presence of certain components, causing bias in the results. For example, studies often did not report whether the desired behavior was demonstrated. Reporting in the included studies was also not detailed enough to determine the delivered dose or actual compliance with the intervention, hence we only considered planned delivery of components. Future studies should include detailed reporting on intervention content and actual delivery to facilitate future meta-analyses, for example by following the TiDieR checklist. An approach like intervention component analysis (ICA, [Citation50]) may also be considered. The informal evidence that is taken into account in ICA, may reveal components that are not included in intervention descriptions. In addition, some intervention components rarely occurred in our sample of studies and power may have been lacking in our analyses. For example, only one study included the intervention component visualization. Future studies on such components are necessary to properly investigate their effectiveness with meta-analysis. Furthermore, the components identified as promising in the current study can be used to develop or adapt interventions and to accumulate more evidence on these components. For example, the type of tailoring may be investigated [Citation51]. Lastly, a strong theoretical rationale about intervention components and characteristics – and their interaction – is required to formulate hypothesis that can be tested with multivariate meta-regression techniques.
Conclusions
Our analyses indicate that interventions with body awareness, holistic exercises, and meditation were more effective than interventions without these components. Interventions with tailoring, motivation by the supervisor, balance exercises, or self-monitoring were less effective than interventions without these components. These components may be emphasized or de-emphasized, respectively, when designing or optimizing interventions to reduce FoF, in order to prevent its disabling consequences in community-dwelling older people. Clinicians should consider including these components in their treatments for FoF, also taking into account costs and culture.
Supplemental Material
Download MS Excel (40.4 KB)Supplemental Material
Download PDF (97.6 KB)Supplemental Material
Download MS Word (40 KB)Supplemental Material
Download MS Word (19.6 KB)supplementary_file_6_bubble_plots_16-06-2021.docx
Download MS Word (62.7 KB)supplementary_file_5_references_of_included_studies_08-06-2021.docx
Download MS Word (120.3 KB)supplementary_file_2_search_strategy_08-06-2021.docx
Download MS Word (29.5 KB)Acknowledgements
The authors acknowledge the following people for their contribution in the expert consultation process: Dr. Will Young, Dr. Nimali Jayasinghe, Prof. Christophe Büla, Prof. Helen Lach, Prof. Elizabeth W. Peterson, and Prof. Stephen Lord. The authors thank Dr. Estelle Gallo, Dr. Silke Metzelthin, Dr. Ellen Freiberger, Dr. Monika Siegrist, Dr. Steve Parry, and Dr. Yves Lajoie for providing data. The authors thank Gregor Franssen for providing advice on the search strategy and Arthur Loonen and Mae Lim for assisting with data-extraction.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
The data that support the findings of this study are openly available in Open Science Framework at https://doi.org/10.17605/OSF.IO/SF67D.
Correction Statement
This article was originally published with errors, which have now been corrected in the online version. Please see Correction (http://dx.doi.org/10.1080/09638288.2022.2074388).
Additional information
Funding
References
- Fact sheet ageing and health [Internet]. World Health Organization; 2018 [cited 2018 Sep 4]. Available from: http://www.who.int/news-room/fact-sheets/detail/ageing-and-health
- Scheffer AC, Schuurmans MJ, Van Dijk N, et al. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24.
- Lavedán A, Viladrosa M, Jürschik P, et al. Fear of falling in community-dwelling older adults: a cause of falls, a consequence, or both? PLOS One. 2018;13(3):e0194967.
- Tomita Y, Arima K, Tsujimoto R, et al. Prevalence of fear of falling and associated factors among Japanese community-dwelling older adults. Medicine. 2018;97(4):e9721.
- Malini FM, Lourenço RA, Lopes CS. Prevalence of fear of falling in older adults, and its associations with clinical, functional and psychosocial factors: the frailty in Brazilian Older People-Rio De Janeiro study. Geriatr Gerontol Int. 2016;16(3):336–344.
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):239–243.
- Zijlstra G, Van Haastregt J, Van Rossum E, et al. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc. 2007;55(4):603–615.
- Halfens R, Meesterberends E, Neyens J, et al. Landelijke prevalentiemeting zorgproblemen rapportage resultaten 2015. Maastricht: CAPHRI; 2016.
- Zijlstra GAR, van Haastregt JCM, van Eijk JTM, et al. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing. 2007;36(3):304–309.
- Makino K, Makizako H, Doi T, et al. Fear of falling and gait parameters in older adults with and without fall history. Geriatr Gerontol Int. 2017;17(12):2455–2459.
- Meulen E, Zijlstra G, Ambergen T, et al. Effect of fall-related concerns on physical, mental, and social function in community-dwelling older adults: a prospective cohort study. J Am Geriatr Soc. 2014;62(12):2333–2338.
- Cumming RG, Salkeld G, Thomas M, et al. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol Ser A. 2000;55(5):M299–M305.
- Liu T-W, Ng GY, Chung RC, et al. Cognitive behavioural therapy for fear of falling and balance among older people: a systematic review and meta-analysis. Age Ageing. 2018;47(4):520–527.
- Chua CHM, Jiang Y, Lim DS, et al. Effectiveness of cognitive behaviour therapy-based multicomponent interventions on fear of falling among community-dwelling older adults: a systematic review and meta-analysis. J Adv Nurs. 2019;75(12):3299–3315.
- Papadimitriou A, Perry M. Systematic review of the effects of cognitive and behavioural interventions on fall-related psychological concerns in older adults. J Aging Phys Act. 2019;28:1–43.
- Kendrick D, Kumar A, Carpenter H, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;2014(11):CD009848.
- Rand D, Miller WC, Yiu J, et al. Interventions for addressing low balance confidence in older adults: a systematic review and meta-analysis. Age Ageing. 2011;40(3):297–306.
- Jung D, Lee J, Lee S-M. A meta-analysis of fear of falling treatment programs for the elderly. West J Nurs Res. 2009;31(1):6–16.
- Graves KD. Social cognitive theory and cancer patients' quality of life: a meta-analysis of psychosocial intervention components. Health Psychol Rev. 2003;22(2):210–219.
- Vestjens L, Kempen GI, Crutzen R, et al. Promising behavior change techniques in a multicomponent intervention to reduce concerns about falls in old age: a Delphi study. Health Educ Res. 2015;30(2):309–322.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Kruisbrink M, Delbaere K, Kempen GI, et al. Intervention characteristics associated with a reduction in fear of falling among community-dwelling older people: a systematic review and meta-analysis of randomized controlled trials. Gerontologist. 2021;61(6):e269–e282.
- 7.2.6 measuring agreement [Internet]. The Cochrane Collaboration; 2011 [cited 2019 Jan 30]. Available from: https://handbook-5-1.cochrane.org/chapter_7/7_2_6_measuring_agreement.htm
- Kühne F, Ehmcke R, Härter M, et al. Conceptual decomposition of complex health care interventions for evidence synthesis: a literature review. J Eval Clin Pract. 2015;21(5):817–823.
- Eldredge LKB, Parcel, GS, Kok G, et al. Planning health promotion programs: an intervention mapping approach. 3rd ed. San Francisco: Jossey-Bass; 2011.
- Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
- Lamb SE, Becker C, Gillespie LD, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials. 2011;12:125.
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(2):d5928.
- 9.2.3.2 the standardized mean difference [Internet]. The Cochrane Collaboration; 2011 [cited 2019 Jan 30]. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_2_3_2_the_standardized_mean_difference.htm
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates; 1988.
- 9.5.2 identifying and measuring heterogeneity [Internet]. The Cochrane Collaboration; 2011 [cited 2019 Jan 30]. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm
- Metzelthin SF, van Rossum E, de Witte LP, et al. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: cluster randomised controlled trial. BMJ. 2013;347:f5264.
- Snooks HA, Anthony R, Chatters R, et al. Support and assessment for fall emergency referrals (SAFER) 2: a cluster randomised trial and systematic review of clinical effectiveness and cost-effectiveness of new protocols for emergency ambulance paramedics to assess older people following a fall with referral to community-based care when appropriate. Health Technol Assess. 2017;21(13):1–218.
- van Haastregt JC, Diederiks JP, van Rossum E, et al. Effects of a programme of multifactorial home visits on falls and mobility impairments in elderly people at risk: randomised controlled trial. BMJ. 2000;321(7267):994–998.
- Hafström A, Malmström E-M, Terdèn J, et al. Improved balance confidence and stability for elderly after 6 weeks of a multimodal self-administered balance-enhancing exercise program: a randomized single arm crossover study. Gerontol Geriatr Med. 2016;2:2333721416644149.
- Hosseini L, Kargozar E, Sharifi F, et al. Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: a randomized control trial. J Exerc Rehabil. 2018;14(6):1024–1031.
- Mortazavi H, Tabatabaeicher M, Golestani A, et al. The effect of Tai Chi exercise on the risk and fear of falling in older adults: a randomized clinical trial. Mater Sociomed. 2018;30(1):38–42.
- Nguyen MH, Kruse A. A randomized controlled trial of tai chi for balance, sleep quality and cognitive performance in elderly Vietnamese. Clin Interv Aging. 2012;7:185–190.
- Nick N, Petramfar P, Ghodsbin F, et al. The effect of yoga on balance and fear of falling in older adults. PM R. 2016;8(2):145–151.
- Pirauá ALT, Cavalcante BR, de Oliveira VMA, et al. Effect of 24-week strength training on unstable surfaces on mobility, balance, and concern about falling in older adults. Scand J Med Sci Sports. 2019;29(11):1805–1808.
- Boutron I, Tubach F, Giraudeau B, et al. Blinding was judged more difficult to achieve and maintain in nonpharmacologic than pharmacologic trials. J Clin Epidemiol. 2004;57(6):543–550.
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;2012(9):CD007146.
- Yardley L, Nyman SR. Internet provision of tailored advice on falls prevention activities for older people: a randomized controlled evaluation. Health Promot Int. 2007;22(2):122–128.
- Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1(1):CD012424.
- Yardley L, Bishop FL, Beyer N, et al. Older people's views of falls-prevention interventions in six European countries. Gerontologist. 2006;46(5):650–660.
- Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701.
- Hill A-M, Etherton-Beer C, Haines TP. Tailored education for older patients to facilitate engagement in falls prevention strategies after hospital discharge—a pilot randomized controlled trial. PLOS One. 2013;8(5):e63450.
- Jonasson SB, Nilsson MH, Lexell J, et al. Experiences of fear of falling in persons with Parkinson's disease – a qualitative study. BMC Geriatr. 2018;18(1):44.
- Li X, Dusseldorp E, Meulman JJ. Meta-CART: a tool to identify interactions between moderators in meta-analysis. Br J Math Stat Psychol. 2017;70(1):118–136.
- Sutcliffe K, Thomas J, Stokes G, et al. Intervention component analysis (ICA): a pragmatic approach for identifying the critical features of complex interventions. Syst Rev. 2015;4(1):140–113.
- Schepens SL, Panzer V, Goldberg A. Randomized controlled trial comparing tailoring methods of multimedia-based fall prevention education for community-dwelling older adults. Am J Occup Ther. 2011;65(6):702–709.