Abstract
Purpose
To investigate the effects of a systematic tuning protocol for ankle foot orthosis footwear combinations (AFO-FC) using incrementing heel height on gait in children with cerebral palsy (CP).
Methods
Eighteen children with CP (10.8 ± 3 years, Gross Motor Function Classification System (GMFCS) I–II) underwent 3D gait analysis on a treadmill, while the AFO heel surface was systematically incremented with wedges. Children were subdivided based on their gait pattern, i.e., knee hyperextension (EXT) and excessive knee flexion (FLEX). Outcome measures included sagittal hip and knee angles and moments, shank to vertical angle (SVA), foot to horizontal angle, and gait profile score (GPS).
Results
For both groups, incrementing heel height resulted in increased knee flexion, more inclined SVA, and increased knee extension moments. This resulted in gait improvements for some children of the EXT-group, but not in FLEX. High variation was found between individuals and within-subject effects were not always consistent for kinematic and kinetics.
Conclusions
A systematic AFO-FC tuning protocol using incremented heel height can be effective to improve gait in children with CP walking with EXT. The current results emphasise the importance of including kinematics as well as kinetics of multiple instances throughout the gait cycle for reliable interpretation of the effect of AFO tuning on gait.
A systematic ankle foot orthosis footwear combinations (AFO-FC) tuning protocol using incremented heel height can improve gait in children walking with knee hyperextension.
Tuning results in changes throughout the gait cycle.
Little evidence is found for an optimal SVA of 10–12° at midstance.
For clinical interpretation, both joint kinematic and kinetic parameters should be considered throughout the gait cycle and evaluation should not be based on SVA only.
Implications for rehabilitation
Introduction
Children with cerebral palsy (CP) encounter difficulties in daily life motor activities, attributed to a non-progressive disturbance to the developing foetal or infant brain [Citation1–3]. Motor impairments of children with CP include increased muscle tone or spasticity, muscle contractures, muscle weakness, and impaired selective motor control, which are all associated with gait deviations [Citation1]. Different strategies are used to classify these deviations in clinical practice [Citation4]. For instance, using a classification based on knee kinematics in stance phase, patterns are often split in two subtypes: one group includes children walking with excessive knee flexion (FLEX) during stance, while another group of children presents too much or too early knee extension [Citation4–7].
Ankle foot orthoses (AFOs) are commonly prescribed in children with CP to counteract these gait abnormalities in order to improve walking performance and to prevent contractures and worsening of gait during development [Citation2,Citation5,Citation8–10]. By influencing the alignment of the ground reaction force (GRF) vector in relation to the hip and knee joint, an AFO can modify excessive moments acting around these joints enabling normalisation of joint kinematics [Citation8,Citation9,Citation11–13]. For children walking with FLEX, AFOs should counteract excessive forward inclination of the tibia for example using a ventral shell [Citation13,Citation14]. For children walking with knee hyperextension (EXT), an AFO should reach the opposite effect, preventing shank reclination [Citation6,Citation13]. Hence, appropriate choices concerning the design and materials, defining the mechanical properties of an AFO, are important for achieving the desired results [Citation9].
Apart from mechanical properties and design of the AFO, its effectiveness can be enhanced through tuning the AFO footwear combination (AFO-FC) [Citation8,Citation12,Citation15–17]. AFO-FC tuning has been described as the process of making small adjustments to the external design and/or mechanical properties of the AFO-FC, such as adapting the rocker profile or manipulating the heel-sole differential [Citation17,Citation18]. Through minor adjustments, alignment of the GRF vector with respect to the hip and knee joint can be changed, until the optimal outcome is obtained for an individual [Citation18].
A tuning-protocol using incrementing heel height to manipulate the heel-sole differential has been recommended for children with an EXT gait pattern [Citation11,Citation17,Citation18]. Biomechanically, incrementing heel height of a fixed AFO results in a forward shift of the knee joint centre with respect to the GRF vector at midstance (MST), accompanied by increased internal knee extensor moments, knee flexion angle, and a more inclined shank [Citation18–20]. Although the relation between incremented heel height, kinematics and kinetics seems consistent when investigating healthy adults [Citation19], the beneficial effect of tuning in children with CP is variable [Citation11,Citation12,Citation15]. For CP, although consistent results were found at group level, large variations exist between individuals as well as between studies [Citation12,Citation15,Citation17,Citation21]. In some children, tuning-manipulations did not result in expected biomechanical responses [Citation18], suggesting other factors might play a role within this group [Citation12,Citation18]. Therefore, although most studies endorse the importance of AFO-FC tuning, they further emphasise tuning is a highly individual process and recommend outcomes should always be evaluated at an individual level [Citation12,Citation15,Citation17,Citation18,Citation22].
For clinical evaluation, the tuning-protocol proposed by Owen [Citation17] is often used in CP, based on optimisation of orientation of the shank with respect to the vertical (shank to vertical angle, SVA). Within this protocol, MST has been described as a crucial phase [Citation12,Citation15,Citation17,Citation19]. As a golden standard, an SVA of 10–12° at MST is presumed to facilitate appropriate shank progression throughout stance phase, allowing optimal control of knee moments [Citation23]. However, this golden standard is mostly based on clinical experience or studies in healthy adults [Citation17,Citation23]. Up to now, little information is available on the strength of the relation between SVA at MST and other gait outcomes in patients, while this relation is not necessarily the same for atypical gait patterns [Citation20].
Another limitation of patient-focused studies on AFO-FC tuning is that most studies compared the tuned AFO-FC to the non-tuned condition [Citation12,Citation15,Citation17]. Although this evaluates the intervention as a treatment, this approach gives limited understanding on how children respond to systematic AFO-manipulations. Specific choices made by clinicians or researchers within the tuning process differ between children, complicating comparison between patients. Additionally, walking speed is inconsistent between conditions and results are limited to a small number of selected foot strikes on a force plate in an overground laboratory. Systematic evaluation of multiple parameters, might help to understand how children with CP adapt their gait pattern in response to AFO-FC tuning.
Hence, the aim of the present study is to investigate the effect of systematic AFO-FC modulation using incremented heel height, on gait in children with CP. Differences between conditions (heel height) are evaluated for children walking with a knee extension gait pattern, as well as for children walking with FLEX. Additionally, to gain understanding on the mechanisms affecting outcomes of AFO-FC tuning, the relation between SVA at MST and gait parameters is investigated at different instances throughout the gait cycle. It is hypothesised that incremented heel height results in increased knee and hip flexion angles and increased net internal extension moments in stance phase. Furthermore, we expect this will lead to clinical improvements in case baseline AFO-FC is not sufficient to correct EXT in stance phase. Although we do not expect incrementing heel height will result in clinically beneficial effects for children walking with FLEX, the FLEX-group is included to investigate whether different responses would occur compared to children walking with EXT. Finally, it is hypothesised that changes will be most pronounced at MST and that the overall gait pattern will be most normalised when SVA at MST is between 10° and 12° [Citation17].
Materials and methods
Participants
Eighteen children with unilateral (n = 10) or bilateral (n = 8) spastic CP were included in this study (five female, 13 male; age 10.83 ± 2.9 years, range 6–17 years). All children were referred for clinical gait analysis to undergo AFO tuning as part of standard orthotic care. The following inclusion criteria were used: spastic CP, age between 6 and 18 years, able to understand and follow instructions, ability to walk independently without devices (Gross Motor Function Classification System (GMFCS) I–II), customised AFO allowing no or only limited ankle range of motion, minimal contractures of the m. triceps surae allowing a neutral ankle angle (i.e., 0° plantarflexion), nor a knee joint contracture larger than 10°. AFOs were prescribed by a multidisciplinary team (rehabilitation physician, orthotist, paediatric physical therapist), among others based on the child’s gait type, age, weight, and motor functioning. Written informed consent was given by the parents as well as children with CP if older than 12 years. The study protocol was approved by the local medical ethics committee of the VU University Medical Centre.
Intervention
Clinical gait analysis was performed on an instrumented treadmill with embedded force plates, surrounded by a projected virtual landscape (GRAIL system, Motek Medical B.V., Amsterdam, The Netherlands). Children walked at a fixed self-chosen comfortable walking speed. Before the start of the measurements, a practice session was performed for treadmill walking which continued until children, parents, and experimenters confirmed that a representative gait pattern and walking speed were reached. A safety harness was used during all walking trials, hanging loosely from the ceiling.
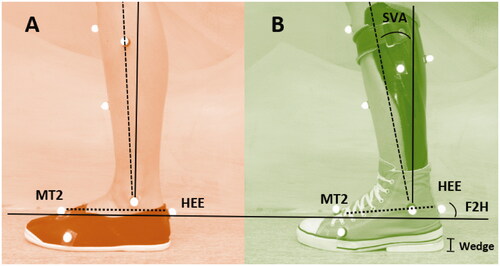
The protocol included five different walking conditions, measured in separate trials. Walking speed was constant for all conditions. During the first condition, children walked on textile, non-supporting shoes (NS-SHOES) with a flexible sole, as a representation of their barefoot walking pattern since true barefoot walking was not allowed on the treadmill for injury prevention (). Second, children walked with their custom-made AFOs, combined with their own, flat-soled confection shoes. In three following trials, heel height of the AFO-FC was incremented by placing a wedge of 5 mm, 10 mm, and 15 mm under the heel surface of the shoe (). Each walking trial lasted for at least 30 s and was stopped when a sufficient number of valid strides were collected (i.e., 10 clean strides on each belt). In case of bilateral AFOs, both AFO-FC’s were tuned symmetrically, but only data of the most affected leg was included in analyses.
Figure 1. Lower leg/foot markers for (A) NS-SHOES (non-supportive textile shoes) and (B) AFO-footwear combination. Heel height was incremented by placing wedges of 5, 10, and 15 mm below the heel surface of the shoe (indicated with I, (B)). Shank to vertical angle (SVA) was calculated as the orientation of the shank (knee joint centre to ankle joint centre), to the vertical in the sagittal plane. Foot to horizontal angle (F2H) was calculated as the position of the foot (MT2-HEE) to the horizontal in the sagittal plane. Note that markers remained attached to the shoe and AFO for all AFO walking trials.
3D motion capture was used to collect passive marker data (Vicon, Oxford, UK, sample frequency 100 Hz). First, 26 reflective passive markers were placed on anatomical landmarks according to the updated version of the human body model (HBM) [Citation24–26]. Since palpation of bony landmarks was not possible for foot markers when wearing AFOs, a standardised protocol was developed for marker placement. A goniometer was used to ensure alignment of markers perpendicular to the segments. Foot markers (calcaneus and second metatarsal bone) were placed on equal height from the shoe sole without wedges, aligned to the longitudinal axis of the foot. Medial and lateral malleolus markers were placed with the proximal goniometer-arm aligned to the shank and the distal arm aligned to the foot markers. Markers remained attached in-between all AFO walking trials. Marker placement was always performed by the same experienced operator.
Data processing and outcomes
Strides were selected based on visual inspection and data were excluded from analysis when children were running, standing still, tripping, or distracted. Additionally, data were excluded for kinetic analysis when children placed a left foot on the right belt, and vice versa. All strides were time normalised from initial contact (IC) to consecutive IC, detected following Zeni et al. [Citation27]. Data processing was performed using the Gait Offline Analysis Tool (version 4.2, Motek Medical B.V., Amsterdam, The Netherlands) combined with custom written Matlab scripts (MathWorks, Natick, MA).
Participants were subdivided into two groups, based on sagittal knee angle during barefoot walking compared to reference data of 41 typically developing (TD) children walking on a treadmill [Citation28]. Children were classified as FLEX when the sagittal knee angles at MST were flexed more than mean +1SD compared to age-matched reference values in the NS-SHOES condition, while children were classified as EXT when the sagittal knee angle at MST was more extended than mean +1SD compared to TD [Citation7]. In case knee flexion-extension angles were within the mean-SD range of the reference data, children were classified as FLEX when presenting a continuous internal knee extension moment during stance, while children who showed full knee extension and/or presented an internal knee flexion moment were classified as EXT.
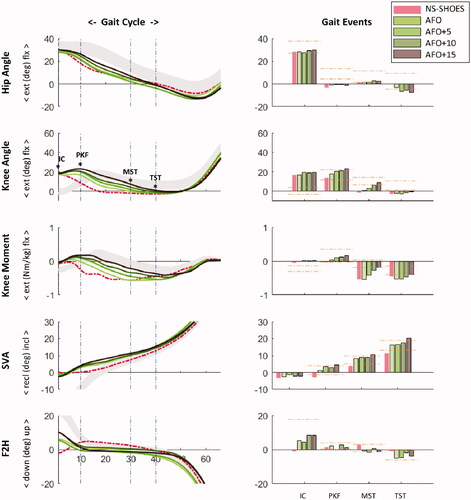
For SVA, the orientation of the shank was defined as a virtual line from the knee joint centre to the ankle joint centre, which were defined by the lateral and medial epicondyles and malleoli, respectively. SVA was calculated as the angle between this line and the vertical in the global sagittal plane with respect to the laboratory (). For quantification of the foot position during stance in the sagittal plane, the foot to horizontal angle (F2H) was calculated, where the orientation of the foot was based on markers on the calcaneus and 2nd metatarsal bone (). SVA and knee and hip joint flexion-extension angles and internal moments were calculated at multiple predefined events of the gait cycle: just after IC (mean of 1–5% stance phase), instance of peak knee flexion in stance (PKF), MST, and at the instance of peak knee extension in terminal stance (TST; between MST and toe off) (). MST was defined as the instance when the midpoint of the shank of the swinging leg crossed the knee joint centre of the stance leg. Note that these gait events reflect distinct instances of the gait cycle and do not represent the conventional phases as defined by Perry et al. [Citation29,Citation30]. As a measure of overall gait quality, the gait profile score (GPS) was calculated, with treadmill-based data of TD children as reference [Citation28,Citation31].
Figure 2. Time-normalised gait curves (left panel) and accompanying values at specific gait events (right panel) for a 9 y old girl walking with knee hyperextension (EXT), for sagittal hip and knee angles, internal knee moment, shank to vertical angle (SVA), and foot to horizontal angle (F2H). NS-SHOES: non-supportive flexible shoes (red/dashed), AFO: ankle foot orthosis (green), with incremented heel height of 5, 10, and 15 mm. Vertical dash-dotted lines (left) represent timing of gait events (initial contact (IC), peak knee flexion (PKF), midstance (MST), and maximal knee extension at terminal stance (TST)). Horizontal dash-dotted lines (right) represent mean ± 1SD of typically developing children. Positive foot to horizontal angles indicate an upwards positioned forefoot, with respect to the floor surface. Recl: reclined; incl: inclined.
Statistical analysis
Patient characteristics as well outcomes of NS-SHOES walking trials were compared between groups (FLEX-EXT) with an independent samples t-test. Furthermore, the effects of AFOs and incrementing heel height were tested with a repeated measures analysis of variance (ANOVA). First, NS-SHOES condition was compared to walking with the AFO without wedge (within factor: NS-SHOES versus AFO; between factor: gait type FLEX-EXT). Additionally, a separate ANOVA was performed to test the effect of incremented heel height (within factor: AFO, AFO + 5, AFO + 10, and AFO + 15; between factor: gait type FLEX-EXT). A Bonferroni correction was used to correct for multiple comparisons.
To quantify the relation of SVA at MST with respect to sagittal knee angles, internal knee moments and SVA at multiple gait events, linear generalised estimation equations (GEEs) analyses were performed including the AFO-conditions only. This method was chosen, as it accounts for multiple observations within persons. For the relation between SVA at MST and GPS, a quadratic term was included within the regression, since this relation was expected to follow a parabolic curve rather than a linear relationship with an optimum SVA of 10–12°. All statistical analyses were performed with IBM SPSS Statistics, version 22 (SPSS Inc., Chicago, IL). For all tests, the level of significance was set at p = 0.05.
Results
Participants
Patient and AFO characteristics are presented in . Nine children were classified as EXT and nine children as FLEX (). One child in the FLEX-group presented exclusive toe walking for his most affected leg during all conditions (i.e., no heel contact). Since he wore bilateral AFOs, the least affected leg was analysed. No differences were found between groups for weight (p = 0.40), length (p = 0.47), walking speed (p = 0.12), or barefoot GPS (p = 0.27). For barefoot walking, significant differences between groups were found at MST for flexion-extension angles of the hip (FLEX: 9 ± 6° and EXT: 2 ± 5°; p = 0.01), knee (FLEX: 21 ± 5° and EXT: 8 ± 7°; p < 0.001), and SVA (FLEX: 15 ± 3° and EXT: 8 ± 4°; p = 0.001) (; ).
Figure 3. Effect of ankle foot orthoses with incremented heel height (AFO, +5, +10, and +15 mm) on sagittal hip, knee, shank to vertical (SVA), and foot to horizontal (F2H) angles. Group results (mean-SD) are presented for children walking with excessive knee flexion gait pattern (FLEX) and knee hyperextension (EXT). NS-SHOES: non-supportive flexible shoes; AFO: ankle foot orthosis; incl: inclined; recl: reclined; up: forefoot up with respect to floor; down: forefoot down with respect to floor (i.e., representing heel rise). Note that no significant interaction effect was found between group and heel height.
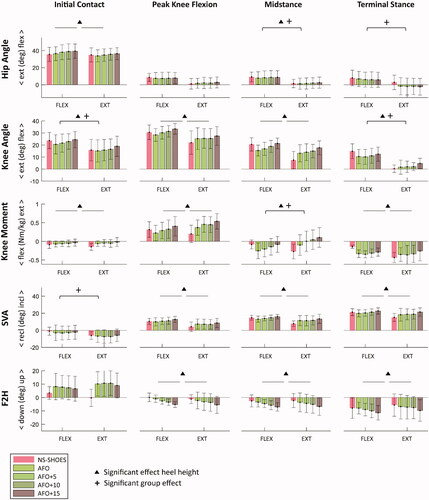
Table 1. Characteristics of the participants and their ankle foot orthoses (AFOs).
Table 2. Group results (mean ± SD) of children walking with excessive knee flexion (FLEX) and knee hyperextension (EXT).
NS-SHOES versus AFO
The AFO resulted in decreased knee moments and F2H at IC as well as increased hip extension at TST for both groups compared to walking on the non-supportive flexible gymnastic shoes (NS-SHOES, ). Significant interaction effects indicated that the AFO resulted in different effects between groups (EXT/FLEX) for sagittal knee angles at MST, F2H at IC, and internal knee moments at PKF and TST. GPS did not change significantly while walking with AFO in both groups (; ).
Incrementing heel height
Incrementing heel height resulted in increased hip flexion, knee flexion, internal knee extension moment, and a more inclined SVA in almost all gait phases for both groups (p < 0.001; , ). Only SVA and F2H at IC, and hip flexion angle at PKF and TST were unaffected by heel height.
The absence of interaction effects between gait type and heel height, indicates that the effect of tuning was comparable between both groups. Only for hip moment at TST, a significant interaction effect indicated that incrementing heel height resulted in decreased hip moments for EXT (p < 0.001), while no effect was observed for FLEX (p = 0.807).
Relation SVA midstance
presents the relation between SVA at MST and outcome parameters. Significant relations were found between SVA at MST and all included gait parameters (p < 0.01), except knee moment at MST (p = 0.958) and GPS (p = 0.344). Although GEE analysis does not allow direct quantification of correlation coefficients, visual inspection indicated large spreading and hence great variability between effects. The strongest correlation seems to be identified for SVA at TST. Additionally, the correlation appears relatively strong for knee angles and SVA, while the linear fit could explain less of the variance in knee moments. A table with detailed information on GEE outcomes has been added as an appendix.
Figure 4. Individual shank to vertical angle (SVA) at midstance scattered against sagittal knee angles (upper row), sagittal internal knee moment (second row) and SVA (third row) at initial contact, midstance (MST) and terminal stance for different walking conditions. Mean data of each condition are presented for all individuals. Regression lines (dotted) are presented when generalised estimation equations (GEE) analysis indicated a significant relation (p < 0.05). Grey squares represent reference data of typically developing children (±1SD) [Citation28]. NS-SHOES: non-supportive flexible shoes; AFO: ankle foot orthosis, incremented with 5, 10, and 15 mm wedge below the heel surface. GPS: gait profile score.
![Figure 4. Individual shank to vertical angle (SVA) at midstance scattered against sagittal knee angles (upper row), sagittal internal knee moment (second row) and SVA (third row) at initial contact, midstance (MST) and terminal stance for different walking conditions. Mean data of each condition are presented for all individuals. Regression lines (dotted) are presented when generalised estimation equations (GEE) analysis indicated a significant relation (p < 0.05). Grey squares represent reference data of typically developing children (±1SD) [Citation28]. NS-SHOES: non-supportive flexible shoes; AFO: ankle foot orthosis, incremented with 5, 10, and 15 mm wedge below the heel surface. GPS: gait profile score.](/cms/asset/73cb12a1-fbdc-412f-a203-baa6aa622acf/idre_a_1970829_f0004_c.jpg)
Discussion
AFO-FC tuning using incremented heel height has been advocated to correct EXT in patients with CP [Citation12,Citation17]. By preventing excessive strain on the posterior structures of the knee, it is expected to lower the risk of injuries or damage in the long-term [Citation7,Citation12,Citation17]. The present study investigated the effects of a systematic AFO-FC tuning protocol on gait in children with CP. In line with our hypothesis, incrementing heel height resulted in a more inclined SVA, increased knee flexion angle, and increased internal knee extension moment at MST [Citation17,Citation19,Citation21,Citation32]. Effects of the tuning protocol were comparable between children walking with EXT and children who walked with FLEX. For the EXT-group, this meant incremented heel height resulted in more normalised knee kinematics and kinetics in the sagittal plane for some individual children, compared to non-tuned condition (). This is in line with previous studies [Citation12,Citation15,Citation17] and confirms that AFO-FC tuning has potential to effectively improve knee kinematics and kinetics at MST for children walking with EXT, thereby optimising the effectiveness of an AFO [Citation12,Citation15,Citation17,Citation19].
Between individual children of the EXT-group, however, much variation was found. While for some children gait improved with wedges, for others incremented heel height adversely influenced the gait pattern, which is supported by an absence of significant main effects on GPS (). In some cases, this could be attributed to the fact that the incremented heel height led to an overcorrection towards FLEX, since the baseline AFO condition (no wedge) was sufficiently effective to normalise knee angles. For other children, however, results of incrementing heel height were inconsistent between outcome parameters. For instance, an increased shank inclination did not always correspond to a high knee extensor moment. This is supported by the absence of a significant relation between SVA and knee moments at MST on group level (). This is surprising, since tuning is assumed to affect alignment of the knee joint centre with respect to the GRF, consequently leading to changes in the knee moment [Citation19,Citation20]. Our results, however, suggest children with CP might compensate for the more inclined shank by adaptations in other joints or the trunk, most likely to prevent high demands on knee extensor muscles. Additionally, we did not consider the footplate stiffness within our analyses, while this might affect the possibility to compensate for a change in heel height. In short, our results indicate that the relation between SVA, knee angles and knee moments might not be straightforward in children with CP. Hence, including joint moments into analyses when tuning AFOs could provide relevant additional information.
In line with our hypothesis, the effects of incrementing heel height were comparable between groups, as indicated by the absence of significant interaction effects (, ). Although we did not expect incrementing heel height to result in clinically beneficial effects for children walking with FLEX, the FLEX-group was included to investigate whether different responses would occur compared to children walking with EXT. For the FLEX-group, this means incrementing heel height only resulted in more FLEX, thereby worsening the gait pattern. Although no systematic difference was found for tuning effects between groups, gait patterns were variable and various compensations were observed in both the FLEX and EXT-group. This suggests compensation strategies are not merely dependent on the gait pattern and hence are important to consider when evaluating AFO-FC tuning at individual level in all children with CP, regardless of their gait pattern.
Temporal MST has been indicated to play a key role in the gait cycle and is described as the phase most sensitive for AFO-FC tuning [Citation17,Citation18,Citation33]. Our results confirm that tuning is related to changes in hip and knee joint angles and knee moments at MST [Citation17,Citation19,Citation21]. Nevertheless, we also found effects of tuning throughout the stance phase. Furthermore, our results show that, at an individual level, the condition where SVA at MST was closest to the reference data of TD children (grey square box), was not necessarily the most optimal condition concerning other gait parameters (). Additionally, our results indicate that effects of tuning at MST are not independent of changes at other phases of the gait cycle. Considering these findings, decisions for choosing a child’s individual optimal AFO configuration should be a balanced decision looking at effects throughout the gait cycle, taking into account both kinematic and kinetic variables.
The goal of AFO-FC tuning is to optimise AFO effectiveness, reflected by overall gait performance. Based on the work of Owen [Citation17], we hypothesised an SVA at MST of 10–12° to correspond to minimal GPS and least deviations from normal in kinematic and kinetic outcome parameters. Since GPS scores have a non-linear character and worse gait patterns always lead to higher scores, it was expected to find a u-shaped relation to SVA with minimal scores around the most optimal SVA. In contrast to our hypothesis, no significant relation was found, indicating little evidence for an optimal SVA, nor that this optimum would be around 10–12°. Several factors could play a role. First, due to methodological differences, SVA of the present study was considerably smaller than reported in previous literature, for both CP as well as the included set of TD children who showed an SVA of 7.5° (SD: range 5–10). In the present study, SVA was calculated using the midline of the shank, instead of using additional markers on the frontal side [Citation19,Citation34]. Although this might have induced an offset, we assume that it only played a limited role on outcomes, since the effect is consistent between subjects and SVA was calculated the same way for the reference data. Second, SVA was calculated in the global sagittal plane with respect to the laboratory. Although this is comparable to most other studies [Citation12,Citation17,Citation19,Citation21], it may induce an error when children walk with segment rotations, causing misalignment of the investigated planes. Third, GPS is an overall gait score and it does not discriminate between clinically relevant phases, joints, or outcomes [Citation31,Citation35,Citation36]. Danino et al. [Citation35] previously reported relatively low sensitivity of GPS to AFO-interventions, when compared to other outcome measures [Citation35]. In line with these results and other studies, no change was found for GPS between AFO and barefoot, even though significant improvements towards reference data were found in hip and knee angles and SVA [Citation35,Citation36]. Another factor that may have limited the improvements of GPS as a result of AFOs, is that AFOs limit ankle range of motion, therewith negatively affecting the ankle dorsiflexion–plantarflexion pattern, possibly outbalancing positive effects that may have occurred in other joints.
The current study was performed on a treadmill, while most clinical tuning studies are performed in a conventional overground gait lab [Citation12,Citation15]. The advantage of treadmill walking is that it enables investigators to impose a constant walking velocity between conditions and data analysis could be performed on many continuous strides. Therefore, we were able to investigate the results of tuning without confounding effects of walking velocity between conditions. On the downside, this fixed velocity may complicate translation of our effects to daily life overground walking, since AFOs influence walking speed [Citation36]. Another aspect of treadmill walking is that there are potential differences to overground walking [Citation37–40]. To investigate whether and how treadmill walking may influence the effect of AFO-FC tuning, a pilot study was conducted before implementation of the protocol in clinical routine. This pilot study, comparing the effects of AFO-FC tuning on a treadmill to overground walking, confirmed similar tuning effects between overground and treadmill walking, when investigating the currently used protocol in healthy adults. However, some consistent differences were found, highlighting the importance of using treadmill-specific reference data for outcome parameters, especially for joint kinetics. Results of this pilot study can be found in the Supplementary material.
Several factors should be considered when interpreting our results. First of all, we only included children who were able to walk without assistive devices and did not have any severe contractures of the knee or ankle joint. Therefore, some caution is in place when translating these findings to children who are more severely affected. Furthermore, EXT can present in different forms, occurring in either early and/or late stance [Citation7,Citation41]. Due to the small number of children included in the present study, no distinction was made for the timing of hyperextension, although this may have affected our results [Citation18]. For this reason, not all children in the EXT-group had full knee extension in MST while walking with an AFO. Second, many children showed high stride-to-stride variability, having some strides classified as EXT, while other strides could be classified as excessive flexion. Since children were grouped on mean strides, some children were classified as FLEX, while a number of their strides showed hyperextension. An interesting next step would be to investigate whether and how these factors may affect AFO-FC tuning in a larger group of children. Third, the majority of children within the present study used a carbon posterior leaf spring AFO (). Although incremented heel height was effective to impose SVA responses, these AFOs typically allow some dorsiflexion, which may have influenced the results. Therefore, results could be different for rigid AFOs, in which the ankle is completely fixed. Finally, due to practical reasons and time constraints, conditions were not imposed in a randomised order and the protocol always started with the barefoot condition. Therefore, effects of habituation to treadmill walking or incremented heel height might have affected our results, although we expect these effects to be relatively small [Citation40].
In conclusion, our results show that a systematic AFO-FC tuning protocol using incrementing heel height induces increased knee flexion angles, knee extension moments, and SVA at MST in children with CP. For children walking with EXT, this can result in improvement of the knee kinematics. No improvement was found at group level for overall gait performance expressed by GPS. Given variation between participants, an inconsistent relation with knee moments, and changes occurring at multiple instances of the gait cycle, it is advised to evaluate the effects of tuning carefully, using a balanced combination of kinematics and kinetics throughout the gait cycle, based on specific individual needs of the patient.
Poster_Laura_-_Can_we_use_treadmills_for_optimization_of_AFOs_-_poster_ISB.pdf
Download PDF (645 KB)Supplemental_material_R1.docx
Download MS Word (15.1 KB)Acknowledgements
The authors thank Carlijn Hendriks for her help in implementation of the protocol and setting up the pilot study. Additional thanks to Marjolein Piening and Koen Wishaupt for their help with data collection.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- Graham HK, Rosenbaum P, Paneth N, et al. Cerebral palsy. Nat Rev Dis Prim. 2016;2:15082.
- Novak I, Morgan C, Fahey M, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep. 2020;20(2):3.
- Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy. Dev Med Child Neurol Suppl. 2007;109(Suppl.):8–14.
- Papageorgiou E, Nieuwenhuys A, Vandekerckhove I, et al. Systematic review on gait classifications in children with cerebral palsy: an update. Gait Posture. 2019;69:209–223.
- Becher JG. Pediatric rehabilitation in children with cerebral palsy. JPO. 2002;14(4):143–149.
- Choisne J, Fourrier N, Handsfield G, et al. An unsupervised data-driven model to classify gait patterns in children with cerebral palsy. J Clin Med. 2020;9(5):1432.
- Švehlík M, Zwick EB, Steinwender G, et al. Genu recurvatum in cerebral palsy – part A: influence of dynamic and fixed equinus deformity on the timing of knee recurvatum in children with cerebral palsy. J Pediatr Orthop B. 2010;19(4):366–372.
- Ridgewell E, Dobson F, Bach T, et al. A systematic review to determine best practice reporting guidelines for AFO interventions in studies involving children with cerebral palsy. Prosthet Orthot Int. 2010;34(2):129–145.
- Wright E, DiBello SA. Principles of ankle-foot orthosis prescription in ambulatory bilateral cerebral palsy. Phys Med Rehabil Clin N Am. 2020;31(1):69–89.
- Firouzeh P, Sonnenberg LK, Morris C, et al. Ankle foot orthoses for young children with cerebral palsy: a scoping review. Disabil Rehabil. 2019;43(5):726–738.
- Butler PB, Nene AV. The biomechanics of fixed ankle foot orthoses and their potential in the management of cerebral palsied children. Physiotherapy. 1991;77(2):81–88.
- Jagadamma KC, Coutts FJ, Mercer TH, et al. Optimising the effects of rigid ankle foot orthoses on the gait of children with cerebral palsy (CP) – an exploratory trial. Disabil Rehabil Assist Technol. 2015;10(6):445–451.
- Morris C, Bowers R, Ross K, et al. Orthotic management of cerebral palsy: recommendations from a consensus conference. NeuroRehabilitation. 2011;28(1):37–46.
- Davids JR, Rowan F, Davis RB. Indications for orthoses to improve gait in children with cerebral palsy. J Am Acad Orthopaed Surg. 2007;15:178–188.
- Eddison N, Healy A, Needham R, et al. The effect of tuning ankle foot orthoses–footwear combinations on gait kinematics of children with cerebral palsy: a case series. Foot. 2020;43:101660.
- Kane KJ, Lanovaz JL, Musselman KE. Physical therapists' use of evaluation measures to inform the prescription of ankle-foot orthoses for children with cerebral palsy. Phys Occup Ther Pediatr. 2019;39(3):237–253.
- Owen E. The importance of being earnest about shank and thigh kinematics especially when using ankle-foot orthoses. Prosthet Orthot Int. 2010;34(3):254–269.
- Butler PB, Farmer SE, Stewart C, et al. The effect of fixed ankle foot orthoses in children with cerebral palsy. Disabil Rehabil Assist Technol. 2007;2(1):51–58.
- Kerkum YL, Houdijk H, Brehm MA, et al. The shank-to-vertical-angle as a parameter to evaluate tuning of ankle-foot orthoses. Gait Posture. 2015;42(3):269–274.
- de Jong LAF, Kerkum YL, de Groot T, et al. Assessment of the shank-to-vertical angle while changing heel heights using a single inertial measurement unit in individuals with incomplete spinal cord injury wearing an ankle-foot-orthosis. Sensors. 2021;21(3):985.
- Jagadamma KC, Coutts FJ, Mercer TH, et al. Effects of the tuning of ankle foot orthoses–footwear combination (AFO-FC) on gait of children with cerebral palsy (CP). Physiotherapy. 2011;97:eS543.
- van Beeten B, Hartman A, Houdijk H. Optimizing knee kinematics in mid-stance by tuning the ankle foot orthoses–footwear combination of children with cerebral palsy: a case series. Gait Posture. 2015;42:S88–S89.
- Borghese NA, Bianchi L, Lacquaniti F. Kinematic determinants of human locomotion. J Physiol. 1996;494(Pt 3):863–879.
- Van Den Bogert AJ, Geijtenbeek T, Even-Zohar O, et al. A real-time system for biomechanical analysis of human movement and muscle function. Med Biol Eng Comput. 2013;51(10):1069–1077.
- Flux E, van der Krogt MM, Cappa P, et al. The human body model versus conventional gait models for kinematic gait analysis in children with cerebral palsy. Hum Mov Sci. 2020;70(February):102585.
- Falisse A, Van Rossom S, Gijsbers J, et al. OpenSim versus human body model: a comparison study for the lower limbs during gait. J Appl Biomech. 2018;34(6):1–502.
- Zeni JA, Richards JG, Higginson JS. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture. 2008;27(4):710–714.
- Oudenhoven LM, Booth ATC, Buizer AI, et al. How normal is normal: consequences of stride to stride variability, treadmill walking and age when using normative paediatric gait data. Gait Posture. 2019;70:289–297.
- Harlaar J. Phases of gait and gait events: some redefining. Gait Posture. 2014;39:S100–S101.
- Perry J, Davids JR. Gait analysis: normal and pathological function. J Pediatr Orthop. 1992;12(6):815.
- Baker R, McGinley JL, Schwartz MH, et al. The gait profile score and movement analysis profile. Gait Posture. 2009;30(3):265–269.
- Eddison N, Chockalingam N. The effect of tuning ankle foot orthoses–footwear combination on the gait parameters of children with cerebral palsy. Prosthet Orthot Int. 2013;37(2):95–107.
- Abel MF, Juhl GA, Vaughan CL, et al. Gait assessment of fixed ankle-foot orthoses in children with spastic diplegia. Arch Phys Med Rehabil. 1998;79(2):126–133.
- de Jong LAF, Kerkum YL, van Oorschot W, et al. A single inertial measurement unit on the shank to assess the shank-to-vertical angle. J Biomech. 2020;108:109895.
- Danino B, Erel S, Kfir M, et al. Are gait indices sensitive enough to reflect the effect of ankle foot orthosis on gait impairment in cerebral palsy diplegic patients? J Pediatr Orthop. 2016;36(3):294–298.
- Ries AJ, Novacheck TF, Schwartz MH. The efficacy of ankle-foot orthoses on improving the gait of children with diplegic cerebral palsy: a multiple outcome analysis. PM R. 2015;7(9):922–929.
- Jung T, Kim Y, Kelly LE, et al. Biomechanical and perceived differences between overground and treadmill walking in children with cerebral palsy. Gait Posture. 2016;45:1–6.
- van der Krogt MM, Sloot LH, Buizer AI, et al. Kinetic comparison of walking on a treadmill versus over ground in children with cerebral palsy. J Biomech. 2015;48(13):3577–3583.
- van der Krogt MM, Sloot LH, Harlaar J. Overground versus self-paced treadmill walking in a virtual environment in children with cerebral palsy. Gait Posture. 2014;40(4):587–593.
- Oudenhoven L, Ettema S, Dallmeijer A, et al. The effect of habituation on differences in energy cost between overground and treadmill walking in typically developing children. Gait Posture. 2020;81(4):247–248.
- Klotz MCM, Wolf SI, Niklasch M, et al. Kinematic differences in primary genu recurvatum gait in cerebral palsy – early vs late onset. Gait Posture. 2015;42:S19–S20.
