Abstract
Purpose
Hemiparesis and physical deconditioning following stroke lead to an increase in falls, which many individuals cannot get up from. Teaching stroke survivors to independently get off the floor (IGO) might mitigate long-lie complications. IGO was taught as part of a community-based, functional rehabilitation training programme (ReTrain). We explore the feasibility of teaching IGO and assess participant’s level of mastery, adherence, and injury risk.
Materials and methods
Videos of participants (n = 17) performing IGO at early, middle, and late stages of the ReTrain programme were compared to a manualised standard. A visual, qualitative analysis was used to assess technique mastery, adherence, and injury risk.
Results
Most participants (64%) achieved independent, safe practice of IGO. A good (73%) level of adherence to IGO and low incidence of risk of injury (6.8%) were observed. Deviations were made to accommodate for non-stroke related comorbidities.
Conclusions
IGO was successfully and safely practised by stroke survivors including those with hemiparesis. Trainers should be aware of comorbidities that may impede completion of IGO and modify teaching to accommodate individual need. Further research should assess if IGO can be utilised by individuals who have other disabilities with unilateral impairments and whether IGO has physical, functional and economic benefit.
Falls are common in stroke survivors, and many are unable to get up despite being uninjured, leading to long-lie complications or ambulance call-outs but non-conveyance to hospital.
Teaching the independently getting up off the floor (IGO) technique to stroke survivors was possible for those with or without hemiparesis, and remained safe despite modifications to accommodate an individual’s needs.
Individual assessment is needed to check if a stroke survivor is suitable for learning IGO including, but not limited to, their ability to safely get to the floor and to temporarily stand (without support) at the end of the technique.
Implications for rehabilitation
Introduction
There are over 1.2 million stroke survivors in the UK [Citation1], and two-thirds leave hospital with a chronic disability. These disabilities include physical, psychological, and cognitive impairments (e.g., hemiparesis, balance problems, fatigue, and depression [Citation2–6]) that impede mobility or the ability to manage their condition. Together these may lead to a lack of physical activity [Citation7] which in turn results in further physical deconditioning and reductions in mobility [Citation2].
These physical impairments result in 73% of stroke survivors falling within the first six months after their stroke [Citation8]. Serious injury following a fall is uncommon [Citation3]; however, half of all stroke survivors who fall are unable to get up off the floor by themselves [Citation9]. If a person is unable to get up after a fall, they may remain there for a long time (i.e., long-lie) and suffer further complications (e.g., hypothermia and dehydration) [Citation10]. Furthermore, stroke survivors report that fear of falling is an important factor contributing to reduced social participation [Citation9,Citation11] and loss of independence [Citation12]. Therefore, being able to get up off the floor independently after a fall is a crucial skill.
The Action for Rehabilitation from Neurological Injury (ARNI; www.arni.uk.com) approach was developed to generally help stroke survivors recover, including improving physical mobility. One of the key techniques developed was independently getting off the floor (IGO), a sequence of movements that accounts for unilateral impairment allowing someone to get up off the floor without assistance from aids, furniture, or other people. A recent Cochrane systematic review suggests that current interventions to prevent falls after stroke, including exercise-based programmes and risk assessments, have not reduced the rate of falls [Citation13]. It may, therefore, be prudent for research to investigate interventions designed to support stroke survivors after they have fallen; and the 2016 National Clinical Guideline for Stroke recommends this is done [Citation6]. Current techniques for teaching getting off the floor are aimed at the general older population and focus on backward chaining involving the use of a chair [Citation14], which is the standard technique for getting to and from the floor, but it is not necessarily applicable to stroke survivors with unilateral impairments or for helping people to be completely independent of aids or furniture. In the UK, very few older people are taught to get up after a fall [Citation15]; in stroke survivors, it is difficult to assess the implementation of current provision but many stroke survivors report having never been taught these skills. IGO offers a potential technique that could aid fall recovery for stroke survivors or people with other disabilities that result in unilateral impairments.
The IGO technique has anecdotal support – it has been described as the “gatekeeper technique” due to its ability to improve confidence in stroke survivors [Citation16] – but it has been subject to little formal evaluation. Development work [Citation17] tested the feasibility of teaching IGO to those with hemiparesis that could already get off the floor with a chair or with minimal or moderate assistance, but not independently. It also examined safety of IGO technique in a laboratory setting using biomechanical analysis to identify risk of strain in “at risk” joints, but only once the technique was mastered. The present study builds on this work by examining the feasibility of teaching IGO in a community setting in stroke survivors with and without hemiparesis, who may not have been able to get up off the floor at all at the beginning of the study. Here, safety was examined whilst the technique was being learned, using a low-tech analysis approach suitable for assessing safety in a community setting that could be replicated in a multi-site trial. This was conducted as part of a pilot trial of the community-based rehabilitation training (ReTrain) programme for stroke survivors; a 24-week group-based functional rehabilitation programme for stroke survivors that manualised many of the core ARNI training principles and techniques, including IGO [Citation18,Citation19]. The pilot included a process evaluation, an examination of how well the manual – and the techniques contained within it – were delivered. The present study focuses on the fidelity analysis of IGO and examines: (aim 1) the feasibility of teaching IGO to stroke survivors; (aim 2) the level of adherence to the five stage standard of IGO when performing the technique, and any deviations from it; and (aim 3) the risk of injury when learning IGO.
Materials and methods
Participants
The full trial methods are reported elsewhere [Citation18,Citation19]. In summary, 48 participants were recruited to the ReTrain pilot randomised controlled trial (RCT). The inclusion criteria were people with a primary diagnosis of stroke, who had been post-discharge from NHS physical rehabilitation services for at least a month, were able to walk independently indoors with or without aids, had self-reported problems walking on stairs or uneven surfaces, had sufficient cognitive capacity and communication ability to follow verbal instructions, and were willing to accept randomisation. Potential participants who were under 18 years old or who had contraindications to moderate to vigorous exercise (based on the American College of Sports Medicine guidelines) [Citation20] were excluded from the study. All participants provided written informed consent. All work was conducted with the approval of NRES Committee South West – Cornwall & Plymouth (REC ref: 15/SW/04) and was registered under ClinicalTrials.gov Identifier: NCT02429180.
Intervention
ReTrain was a pilot feasibility RCT ultimately designed to assess whether the 24-week, group-based physical ReTrain programme improved functional mobility and health-related quality of life in stroke survivors [Citation18,Citation19]. However, the objectives of the pilot feasibility trial were to assess feasibility of delivering the study and the acceptability of the intervention to trainers and participants. After screening, eligible participants provided informed consent and were individually randomised 1:1 to either the intervention (ReTrain) or control (exercise advice booklet) arm. The ReTrain intervention is described more fully elsewhere [Citation18,Citation19]. Briefly, participants who received ReTrain took part in a 24-week exercise-based rehabilitation programme, comprising (a) one preliminary one-to-one with the trainer (lasting between 30 min and 1 hr), (b) 20 two-hour group exercise sessions ran twice weekly for 10 weeks, (c) follow-up one-to-one (lasting up to one hour), and (d) a total of three drop-in sessions, once per month, starting a month after the final group session. The group sessions were led by qualified exercise professionals (“trainers”) with experience delivering ARNI based rehabilitation to stroke survivors, with a ratio of one trainer to four participants. IGO was taught within these group exercise sessions, as part of a programme incorporating aerobic and strengthening exercises aimed at improving functional mobility.
IGO is a five-stage technique designed to help stroke survivors rise from sitting on the floor to standing without use of aids, using positions designed to compensate for hemiparesis and associated balance issues. For the purposes of the video analysis, we defined hemiparesis as observable one-sided weakness of either the upper or lower limb, or both. The full sequences of movements are detailed in the ARNI manual [Citation16]; in the ReTrain manual, the stages were condensed into five steps as summarised below:
Beginning from a seated position with hips abducted, the foot of the stronger leg is placed to groin.
The stronger hand is placed behind trunk on the floor; pivoting on the stronger knee, the stronger hip is quickly raised from the floor.
The weaker leg is swung around to the front of the body and placed upright with foot flat on the floor. The stroke survivor is now in a “tripod” position, consisting of a single arm, an upright leg, and a kneeling leg.
With the stronger hand placed on the floor, the stronger knee is quickly raised and pivoted outwards, planting the stronger foot on the floor. Both feet are now flat on the floor, with the torso being supported by the stronger hand.
Come to stand by shifting weight backwards off hands, using bodyweight to bring the torso slowly upright.
Data analysis
For each participant, video recordings of IGO were planned for three time points during the intervention: early (1–4 weeks), middle (5–7 weeks), and late (8–10 weeks). Additional written consent was taken at each session when videos were recorded; participants also gave their consent for the videos to be used with any publications associated with the study, and could choose to have their face obscured to hide their identity. The point at which the first set of videos were captured influenced when the later videos were taken, with at least three weeks between each filming. Where multiple videos of the IGO technique within the same time period were taken, one video was selected (by LH) for analysis which demonstrated the participant’s best performance in terms of progression through the technique. This “best performance” selection was done to give an idea of the extent to which the participant could do the technique, in order to meet aim 1 “assess mastery of IGO at each time point”. Where there was no difference in performance, videos were then selected if they showed a particular part of the standard being demonstrated, a modification to the standard or the need for a modification. If there was any uncertainty about which videos to analyse, a second opinion was sought from a senior researcher (SD), and a consensus reached.
Initially, a handheld digital camcorder (Sony Handycam DCR-SR72) was used, but due to its poor film quality, researchers switched to using their mobile phones. All video data file names were anonymised, and labelled according to the time point at which they were recorded (early, middle, and late), and stored on secure university servers, in line with the Data Protection Act [Citation21] and per the local NHS research ethics committee approval (15/SW/0074) for the study. Videos were then deleted from the recording device.
Analysis of the videos for IGO mastery, fidelity and safety was an iterative process and informed by the ReTrain development work [Citation22]. For this previous work, a rating system was developed and piloted. Elements of this rating system relevant to answering the present research question were selected to form the analysis plan used in the current study (). Videos were watched and analysed via a three-step approach for each time point. Videos were watched and analysed multiple times to ensure all risk to participants were recorded.
Table 1. IGO videos analysis plan.
Feasibility of teaching IGO (aim 1) was assessed by participants’ ability to master the IGO technique. Participants were considered to have mastered IGO when they were rated as independent both from aids (e.g., a chair) and from other people (e.g., physical support, verbal prompting). Independence from aids was rated as a yes or no category. The degree of assistance required from another person was rated using a six item independence scoring system (Appendix 1), which was based on the Functional Independence Measure [Citation23]. These modifications had been used in our preliminary work [Citation22]. On this measure, greater scores indicated more independence, with 1 designating total assistance required and 6 designating ability to complete IGO to a stable standing position without physical help or verbal support from another person. Two researchers (LH and SD) independently assessed independence in videos taken across the latest available time point for each participant. Interrater reliability was assessed using a linear weighted Cohen’s kappa. Where there was inconsistency between raters, ratings were discussed and a consensus reached. A summary of the mastery of IGO at each time point in the intervention will be presented.
Level of adherence to IGO standards (aim 2) was assessed by comparing the videos with the technique presented in the ReTrain Trainer Manual [Citation16] (which was also demonstrated by ARNI founder Tom Balchin in footage taken during development work). After watching the videos, qualitative descriptions of adherence to the standard IGO were made and deconstructed into the five stages described in the ReTrain manual. A qualitative approach was taken in order to capture detail across a potential range of deviations. The furthest stage of the technique reached for each time point of the intervention was recorded, to demonstrate participant progression and to allow for comparisons between participants and across time points. Any deviations from the standard were summarised (an example of the data is included in Appendix 2). Examples of deviations from the standard will be presented qualitatively.
Lastly, a researcher (LH) watched the videos to assess for any risk of injury when learning IGO (aim 3). The assessment of risk was informed by previous IGO work assessing safety [Citation17], and LH underwent specialist manual handling training, to help understand correct handling techniques for the population. Any potential risks such as extreme joint angle at knee or wrist, or risk of fall observed were scored as no risk, mild/moderate risk, and high risk. When incidences of potential risk were identified by LH, SD (a registered physiotherapist) made the final judgement on the risk score from a clinical perspective. Incidence of risk will be presented as percentages.
Results
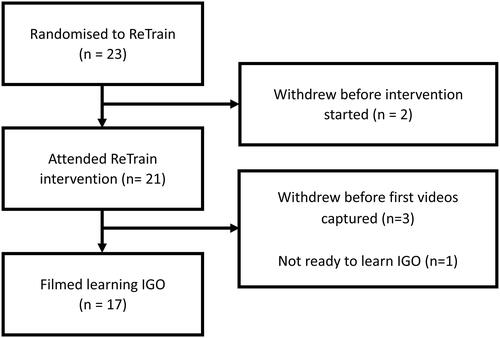
Of the 23 participants allocated to the ReTrain intervention group, two participants withdrew after randomisation. Three participants dropped out of the intervention before the first recordings were captured. One participant was not taught IGO as, although they could walk independently with aids, they were predominantly a wheelchair user and a joint decision was made with them that they were not ready to learn IGO at the time of the intervention. Therefore, 17 participants were filmed learning IGO (). See for the characteristics of these participants. Forty-four videos were analysed; some recordings did not happen because a participant had withdrawn from the intervention (n = 4), they were absent on the recording day (n = 2), or were not ready to learn IGO at that time point in the intervention (n = 1).
Table 2. Characteristics of participants videos during the intervention (n = 17).
To examine the feasibility and acceptability of teaching IGO to stroke survivors (aim 1), the ability to master IGO was assessed. By the end of the intervention, 11 out of 17 (64%) participants were able to fully master IGO, as they were judged to be independent of both trainer and aids ().
Table 3. Mastery of IGO at each time point by participants with and without hemiparesis.
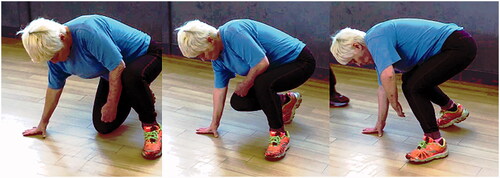
One participant mastered IGO at the early time point, and 10 participants had mastered IGO by the middle time point. No loss in mastery was observed at the later time point. Differences were observed between how quickly participants progressed with the technique (). Participants with hemiparesis varied more in the time it took to learn the technique without the use of the chair than participants without hemiparesis. Upon closer analysis of the videos, it showed that stage 4, when participants place their stronger hand on the floor and then had to quickly raise the stronger knee from the floor (), was the point in the technique when participants struggled to get up without a chair, especially for those with hemiparesis. By the end of the intervention (late time point), participants with hemiparesis were just as likely to be able to get off the floor independent of the chair as those without hemiparesis.
Figure 2. A participant independently completing stage 4 of IGO (left side paresis). Source: Authors.
Of the six participants that did not fully master IGO, one was not able to get off the floor by the final time point. Of the remaining five, two still required the use of a chair. All five were not able to complete IGO without support from a trainer; two participants were rated level 4 on the independence measure (meaning they still required a degree of physical support from the trainer), and three were rated level 5 (meaning they required verbal support only). A greater proportion of participants with hemiparesis (50% versus 27% of those without) were unable to complete the technique independent of a trainer. Interrater reliability was substantial (using Cohen’s criteria, κ = 0.68).
In those that mastered IGO, a good level of adherence to the IGO standard technique was observed (aim 2). By the end of the programme, of the 11 participants that completed IGO independently of both aids and trainer, two (18%) participants could complete the technique with full adherence to all five stages. Five (45%) participants had minor deviations in one stage, two (18%) in two stages, and two (18%) in three stages. Overall 15 minor deviations were observed, indicating 73% adherence to the ReTrain manualised standard. Deviations from a stage were considered to be minor where the performance was similar to the manualised standard, in that it still sufficiently represented the main components of IGO that differentiate it from other methods of transferring from floor to standing. Of the 15 minor deviations recorded, nine occurred when participants made a fourth point of contact with the floor, i.e., placing two hands instead of one on the floor, because they did not have hemiparesis. Four occurred because the participant did not need to place their foot in their groin in stage one before pivoting onto the knee. No major deviations, whereby the performance of the stage was not comparable to the manualised standard, were found in those who got off the floor independently. By definition, those participants who required assistance from a trainer or aids to get off the floor did not adhere to IGO, as an essential requirement of the technique is that it is performed independently.
Across the programme, the main reasons for deviating from the IGO standard fell into two categories: stroke-related impairments and non-stroke-related comorbidities. For the first category, stroke-related impairments, three participants with hemiparesis struggled with correctly positioning their paretic leg upright. For example, one participant with severe hemiparesis struggled due to poor control of his paretic leg which meant he could not swing it around his body, and his lack of balance without support from his unaffected arm meant he could not use his hands to pull his leg upright with feet flat. He solved this problem by rotating on his good knee, and the hip rotation brought his paretic leg upright, which enabled him to complete IGO with his paretic leg in a safer, more stable position ().
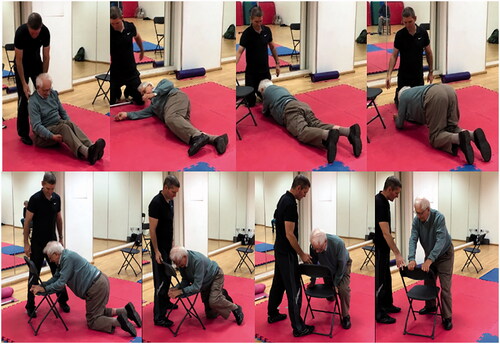
For the second category, deviations arising from non-stroke related comorbidities, the following provides an example of the main issues. One participant was unable to reach stage 2 because the pain from his arthritic knees prevented him from pivoting on one knee. He instead opted to roll onto his front and shuffle back up onto both hands and knees. From there, he could get one leg upright and stand using a chair, as arthritis also prevented him from completing the rotation to stand (). This was a more significant deviation, with the technique being incomparable to the IGO standard until stage 4. The use of a chair meant he also failed to meet the criteria of independence of aids.
Figure 4. Major modification to the IGO standard – participant unable to adhere to the IGO standard until stage 4, where use of chair achieves only partial adherence. Source: Authors.
Despite the modifications to the standard, there was a low incidence of risk observed (aim 3), with three incidences (6.8%) of mild/moderate risk across 44 videos, none of which resulted in injury to the participant. Two out of three incidences were caused by the trainer using poor manual handling techniques when they were helping participants get to the floor. The third incidence was a potential risk of knee strain.
Discussion
This study aimed to examine (1) the feasibility and acceptability of teaching IGO to stroke survivors; (2) adherence to the manualised IGO standard and any deviations from it; and (3) the risk of injury. IGO was deemed feasible in that the majority of stroke survivors mastered the technique, adhered closely to the standard, and there was little incidence of risk even when modifications were used. By the end of the intervention, 11 out of 17 participants mastered the full IGO technique by being independent of aids (e.g., a chair) and being able to practice the technique without physical assistance or supervision (e.g., verbal prompting) from another person, in this case a trainer. Five were able to get off the floor, but still required assistance from another person or the use of a chair. As the majority of the stroke survivors were able to master IGO, it suggests that teaching IGO was feasible and acceptable.
Moreover, most participants and trainers adhered well to the IGO standard. Partial adherence was seen when deviations were intentionally made to accommodate individual need; these were planned and undertaken with support from the trainer. The stroke survivors in our study had a wide range of impairments, and this meant that not all were able to achieve stable standing independent of aids even though the majority were still able to get up off the floor with some assistance (e.g., physical assistance or verbal support). For example, the IGO technique was designed to compensate for hemiparesis following a stroke, but it does not take into account non-stroke related comorbidities (e.g., arthritis) that may require major deviation from the manualised standard. Although independence from the use of aids was the ultimate aim of IGO, getting off the floor using the chair (or other aid) was still considered a valuable skill by those participants. For the participant in , despite the major deviation from the standard and lack of independence from aids, learning to get up using a chair was still an achievement, as the participant could not get up at all when he started the intervention. Even this degree of mastery may provide sufficient increase in a stroke survivor’s confidence that they can (in some circumstances) help themselves to get up after a fall and so reduce the risk of long-lie or need to call an ambulance to help pick them up.
From these results, it is clear that it is feasible to teach IGO to a range of stroke survivors with various stroke-related impairments and non-stroke-related comorbidities; however, it was not always possible to anticipate mastery for each individual participant at the start of the intervention. A participant with an amputated leg was not considered capable of learning IGO during the early time point, but trainers were surprised to find that the participant could successfully master IGO on their first attempt later in the programme. As IGO training was delivered within a wider strength and conditioning programme, muscle conditioning may have been a crucial determinant of the feasibility of mastering IGO [Citation24]. As such IGO may benefit from being delivered as part of a wider rehabilitation programme. Non-physical limitations such as confidence and cognition can also moderate the potential of a stroke survivor to achieve IGO [Citation2]. General anxiety about falling could hinder progression, and research has indicated that just being on the floor can cause anxiety in elderly patients [Citation10]. Measures of fear of falling could be included (e.g., the Falls Efficacy Scale International [Citation25]) in future studies to explore any changes in stroke survivors’ fear after learning IGO. In our study, half of all participants who were unable to get off the floor without a trainer required only verbal prompting. Future research could consider the utility of teaching this technique to family or carers that may be able to offer this verbal assistance were the stroke survivor to fall in their company, in line with recommendations in the National Clinical Guidelines for Stroke [Citation6]. Further research is also needed to assess if IGO has potential benefits for people with other disabilities that have unilateral impairments.
Our participants reported that just knowing they could get themselves up from the floor (after mastering IGO) gave them more confidence in their physical mobility. Further research is therefore needed to measure the potential wider personal benefits. For example, evaluating changes in self-efficacy regarding walking on uneven surfaces, slopes and in crowds, as well as more general confidence in being able to visit friends or attending social events. Such assessment could determine the benefits of IGO on participation and activity, in turn improving quality of life.
Previous development work used biomechanical analysis to make preliminary assessments of joint strain and found no indications that the IGO technique was risky for knee and wrist joints; however, this work only examined IGO once it was learned [Citation22]. This current research extends the previous work by showing that IGO is a low risk technique even whilst being learnt, including when deviations are needed from the standard technique. Two of the three incidences of risk recorded were caused by a trainer’s manual handling when helping participants get to the floor and can be easily addressed through improved trainer preparation such as teaching the trainers to use safe techniques to get participants onto the floor, e.g., backward chaining or the support of a chair. In addition to allowing the safe practice of the IGO technique, these getting to the floor techniques should give stroke survivors another functional skill to use. For example, it could be beneficial for practising the floor exercises and for improving activities of daily life (e.g., housework or playing with children).
Strengths and limitations
Qualitative analysis was deemed appropriate because of the complexity of the video data analysed. This was the main approach as only some elements of adherence were possible to quantify numerically; however, conclusions from the data were supported with a robust methodology, including fully documented data analysis process, a framework used for data extraction based on a manualised standard and preliminary research for consistency between participants, and independent verification procedures. Although deviations were described using a qualitative approach, the observed ability to get up from the floor without assistance from other people, or furniture or aids is a categorical objective outcome; having such an outcome will be useful for evaluating further research in this area, and can be assessed by a blinded outcome assessor in a future RCT. Another strength of the study was the use of video recording; it was an affordable way to collect data from multiple participants at multiple time points and allowed for multiple researchers to assess the IGO technique and trainer handling. Being video recorded may be distracting to participants, affecting their potential to complete the technique to the best of their ability, but no participant reported any concerns during the filming. We provide a practical solution to assessing IGO adherence and safety in the community, future studies could quantify the level of adherence in a laboratory.
Limitations of the study must be noted. The broad timeframe of the filming of the first video (i.e., within the first four weeks of starting the intervention) was not sensitive enough to map a participant’s progression of learning the technique in the early time point; the first set of videos could be taken at either week one or week four. This does not affect the analysis of adherence to the manualised standard but may have impaired the evaluation of feasibility by not showing an accurate participant baseline. For a future RCT, it is therefore recommended to take a baseline set of videos, to enable clearer observations of progression in the intervention group as well as comparing to a control group. Longer follow-ups could also be introduced to see whether IGO can be maintained after the end of the intervention. Due to restricted resources, the initial risk assessments of joints were only performed by one assessor. At risk joints scores were however, double checked by a registered clinician. Due to the small sample size, there is a lack of generalisability; however, the large quantity of video data and time-consuming process of analysis meant larger samples would have been unfeasible for the present study. However, the recommendations arising from this report will inform a future definitive trial of ReTrain.
Our clinical practical recommendations are that the IGO training is suitable, and likely to be beneficial, for the range of stroke survivors who are within a Modified Rankin Scale score of 2–3 (and possibly some with a score of 4 depending on individual assessment). Criteria for commencing IGO training are twofold, first that they are cognitively able to safely follow verbal exercise instructions and second that they have the ability to stand unsupported for at least 30 s, i.e., not immediately fall over once standing but have time to obtain any walking aid they might need (this minimum unsupported standing duration was recommended by Tom Balchin but could be adjusted according to individual assessment). We found that those with low mood, those who lack motivation or confidence, or have other co-morbid conditions (e.g., osteoarthritis, lower limb amputation) can still benefit. The IGO programme could also be adapted for people with mild cognitive impairment, such as those with memory loss. This would likely require teaching IGO to their primary carer/partner too, who could prompt recall of the technique stages, providing the participant was still capable of following these verbal instructions safely.
Overall, the IGO standard technique was mastered by stroke survivors with different impairments and most adhered to the manualised standard. Partial adherence arose when intentional modifications to the standard were made under trainer guidance to accommodate individual needs. Observed instances of modification were recorded and can be used to provide further guidance to trainers to ensure intervention safety is retained. IGO was generally well-accepted by participants with or without hemiparesis and the technique remained safe despite individualised modifications. A future definitive RCT is warranted to determine the clinical and cost effectiveness of teaching this technique as part of rehabilitation following stroke.
Authors contributions
LH led video analysis work with assistance from AS; LH drafted the original report; KW provided critical feedback and drafted the first version of the manuscript; SD led the research team and supervised LH with AS and RC; RC prepared protocol, ethical submission and amendments, managed the project, contributed to analysis and the writing of this paper; LP drafted protocol and contributed to analysis; RA, SD, and LP provided stroke rehabilitation expertise. All authors commented on and approved the manuscript.
Acknowledgements
The authors thank the participants of the ReTrain pilot trial, the Peninsula Patient Involvement Group with the ReTrain Stroke Service User Group for their help and the ARNI trainers who delivered the intervention for being so cooperative and willing throughout the video data collection process. Thanks to Tom Balchin from the ARNI Institute for training our trainers. We also thank our Trial Steering Committee: Ailie Turton (University of the West of England), Siobhan Creanor (Plymouth University), Debbie Neal (Bournemouth University), Justin Smallwood (Patient and Public representative), and Gail Seymour (University of Exeter – Sponsor), and our independent clinical trial adverse event adjudicator, Chris Clark.
Protocol Version: 5 Date: 20/04/2016. Published version available here: http://bmjopen.bmj.com/content/6/10/e012375.full
Trial registration number: NCT02429180.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
Participants did not consent for datasets to be stored or accessed outside of the research team. Therefore, no datasets have been made publicly available.
Additional information
Funding
References
- Department of Health. Quality and outcomes framework (QOF) achievement data 2015/16; 2016. Available from: http://bit.ly/2hQNsMB
- Billinger SA, Arena R, Bernhardt J, et al. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(8):2532–2553.
- Forster A, Young J. Incidence and consequences of falls due to stroke: a systematic inquiry. BMJ. 1995;311(6997):83–86.
- Verheyden GSAF, Weerdesteyn V, Pickering RM, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev. 2013;10(10):CD008728.
- Billinger SA, Coughenour E, Mackay-Lyons MJ, et al. Reduced cardiorespiratory fitness after stroke: biological consequences and exercise-induced adaptations. Stroke Res Treatment. 2012;2012:1–11.
- Intercollegiate Stroke Working Party. National clinical guideline for stroke. London: Royal College of Physicians; 2016.
- Shepherd AI, Pulsford R, Poltawski L, et al. Physical activity, sleep, and fatigue in community dwelling stroke survivors. Sci Rep. 2018;8(1):7900.
- Batchelor FA, Mackintosh SF, Said CM, et al. Falls after stroke. Int J Stroke. 2012;7(6):482–490.
- Tinetti ME, Liu WL, Claus EB. Predictors and prognosis of inability to get up after falls among elderly persons. JAMA. 1993;269(1):65–70.
- Simpson JM, Salkin S. Are elderly people at risk of falling taught how to get up again? Age Ageing. 1993;22(4):294–296.
- Walsh M, Galvin R, Horgan NF. Fall-related experiences of stroke survivors: a meta-ethnography. Disabil Rehabil. 2017;39(7):631–640.
- Schmid AA, Arnold SE, Jones VA, et al. Fear of falling in people with chronic stroke. Am J Occup Ther. 2015;69(3):6903350020.
- Denissen S, Staring W, Kunkel D, et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev. 2019;10(10):CD008728.
- Cox TB, Williams K. Fall recovery intervention and its effect on fear of falling in older adults. Activ Adapt Aging. 2016;40(2):93–106.
- Goodwin V, Martin FC, Husk J, et al. The national clinical audit of falls and bone health-secondary prevention of falls and fractures: a physiotherapy perspective. Physiotherapy. 2010;96(1):38–43.
- Balchin T. The successful stroke survivor: a new guide to functional recovery from stroke. Lingfield (UK): ARNI Trust; 2011.
- Dean SG, Leon P, Warmoth K, et al. Independently getting off the floor: a feasibility study of teaching people with stroke to get up after a fall. Int J Ther Rehabil. 2019;26(2):1–17.
- Dean SG, Poltawski L, Forster A, et al. Community-based rehabilitation training after stroke: protocol of a pilot randomised controlled trial (ReTrain). BMJ Open. 2016;6(10):e012375.
- Dean SG, Poltawski L, Forster A, et al. Community-based rehabilitation training after stroke: results of a pilot randomised controlled trial (ReTrain) investigating acceptability and feasibility. BMJ Open. 2017;15(8):e018409.
- ACSM. American College of Sports Medicine Guidelines for Exercise Testing and Prescription. Philadelphia: American College of Sports Medicine; 2005.
- Legislation.gov.uk. The Data Protection Act (1998); 1998. Available from: http://www.legislation.gov.uk/ukpga/1998/29/contents
- Dean S, Goodwin V, Poltawski L, et al. IGO: a technique for people with stroke to independently get up off the floor a before-and-after case series study. Harrogate: UK Stroke Forum; 2013.
- Keith RA, Granger CV, Hamilton BB, et al. The Functional Independence Measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18.
- Burton E, Farrier K, Lewin G, et al. Are interventions effective in improving the ability of older adults to rise from the floor independently? A mixed method systematic review. Disabil Rehabil. 2020;42(6):743–753.
- Delbaere K, Close JC, Mikolaizak AS, et al. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing. 2010;39(2):210–216.
Appendix 1.
Appendix 2.
Summary of deviations or modifications from IGO standard