Abstract
Purpose
A high percentage of people with multiple sclerosis (PwMS) experience anxiety, which can negatively impact quality of life. Despite this, anxiety in PwMS remains under researched. This review aims to identify associates with anxiety in PwMS that are amenable to change, with a view to informing the development of interventions in the area.
Materials and methods
The following databases were searched for studies investigating anxiety in PwMS from 2015 to 2021: PsycINFO, PubMed, EMBASE, Web of Science. The search consisted of keywords relating to MS and fear, anxiety or worry. Once screening was completed by two reviewers, a narrative synthesis was used to analyze the data, with the MMAT used for quality appraisal.
Results
Of the 3117 unique abstracts screened, 39 studies met the criteria for inclusion. Evidence was found linking anxiety in PwMS to several modifiable factors broadly categorized as either psychological, social or lifestyle factors. Perceptions of self and one’s ability to cope/adjust to MS emerged as important psychological factors. Physical activity and social support from friends were also linked with improved anxiety outcomes.
Conclusions
Anxiety in PwMS is linked to a number of modifiable factors. Findings may help inform the development of rehabilitation interventions to decrease anxiety in MS.
This review highlights interventions which have successfully lowered anxiety in people with MS (PwMS); however, there is a clear need for the development of further interventions which target the pathologically specific concerns surrounding anxiety in this population.
We show how a number of factors amenable to change associate with anxiety, suggesting that these factors may be appropriate targets for anxiety interventions in PwMS.
Enhancing physical activity and self-efficacy are important means in which healthcare professionals can reduce anxiety in MS.
Identifying ways of encouraging positive coping and increasing social support are further targets for improving comorbid anxiety in PwMS.
Focusing on the modifiable factors highlighted here offers considerable potential for enhancing psychological wellbeing in this group.
Implications for rehabilitation
Multiple sclerosis (MS) is neurodegenerative disease characterized by inflammation of the spinal-cord and brain, demyelination, and axonal damage [Citation1]. MS is the most common disabling neurological disease in young people, with many people with MS (PwMS) experiencing symptoms of chronic pain, fatigue, and cognitive impairment [Citation2,Citation3]. MS has an unpredictable disease course, most commonly manifesting as a series of relapses (characterized by an emergence or worsening of symptoms) and remissions (characterized by “recovery” where there are no new active disease symptoms) [Citation1], although many PwMS experience more progressive forms of the disease which may involve a gradual worsening of symptoms. This unpredictability may create pathologically specific concerns in relation to worry, fear, and anxiety in PwMS [Citation4]. Reflecting this, mood-disorder comorbidity is common, with a recent review estimating that 30.5% of PwMS show clinically significant levels of depression, while an estimated 22.1% show clinically significant levels of anxiety, with both rates significantly exceeding prevalence rates seen in the general population [Citation5].
Despite this high prevalence and the existence of evidence to show the damaging effects of anxiety on quality of life for PwMS, anxiety remains under-researched in this population [Citation6,Citation7]. A recent systematic review investigating both pharmacological and psychological treatment options which target anxiety in PwMS found only one control study which targeted anxiety specific to a population with MS [Citation8]. Additionally, the focus of this study was limited to injection anxiety (which may be a dated dimension of anxiety as injectable therapies for MS have become much less common than other treatment options in recent years), with no significant improvement effects found [Citation9].
The specific need for psychological interventions for mood disorders in PwMS has previously been highlighted and is supported by evidence suggesting their potential effectiveness and relative lack of tolerability concerns for PwMS when compared with currently used pharmacological methods [Citation8]. Additionally, lesion studies have found that, unlike depression, anxiety does not appear to be linked with physical abnormalities detectable by magnetic resonance imaging (MRI) and, thus, it is suggested that anxiety is more likely to result from psychosocial pressures [Citation10,Citation11]. This clear dearth in treatment options stems, in part, from a lack of research in the field of anxiety in PwMS in general. Given this, more research is needed to fully understand the associates of anxiety in order to properly inform the development of interventions in this area [Citation12]. To date, only one previous systematic review has specifically investigated factors relating to anxiety in PwMS [Citation13]. The lack of attention given to the importance of anxiety in PwMS seems to be reflected in practical settings, with evidence suggesting there are a large number of patients with clinically significant levels of anxiety who are going untreated [Citation14].
This study describes a systematic review of recent literature investigating potentially modifiable associates of anxiety in PwMS. In addition to helping inform the development of targeted interventions by focusing solely on modifiable factors, it is hoped that this research will provide much needed assistance to clinicians in the identification of individuals with MS who carry a high risk of anxiety comorbidity [Citation5]. The importance of accurate and early anxiety diagnosis is supported by evidence suggesting how the lack of a diagnosis is linked with increased likelihood of damaging health behaviors in PwMS, including alcohol and substance abuse and smoking [Citation15]. Theoretically, by assisting with the identification of at-risk individuals, this type of research may lead to earlier and more accurate diagnoses.
Materials and methods
Search strategy
The review was conducted in accordance with PRISMA guidelines (see Supplementary material) and was preregistered at The Open Science Framework (osf.io). The following databases were searched for studies investigating anxiety in PwMS: PsycINFO, PubMed, EMBASE, and Web of Science. Through collaboration with a professional librarian a search strategy was formed. The search consisted of the keywords “multiple sclerosis” AND (anx* OR “fear” OR “worry”) and was adapted for use with each database. The search was restricted to studies published in English between January 2015 and July 2021. Specifically, searches of databases were initially conducted in January 2020 and updated in July 2021 to allow for the inclusion of more up-to-date research in the area, including those studies which focused on anxiety in the context of the COVID-19 pandemic. The limited timeframe was decided on due to the volume of studies anticipated in relation to anxiety (due to the broad search strategy), as well an acknowledgement of how the treatment and management of MS has changed significantly in recent years, which may have implications for the types of anxiety that PwMS may experience now compared to in previous years. For instance, the wider range of treatment options available has meant that there has been less reliance on injectable therapies, with a shift toward oral or infusion therapies [Citation15]. Many older studies in this population focused specifically on injection anxiety in PwMS [Citation16] which may be less commonly experienced today [Citation8,Citation9,Citation16,Citation17].
Inclusion and exclusion criteria
Included studies must have collected primary data from adults with MS. Papers with mixed samples were only included if the sample was at some point split for analysis of the MS subgroup. In these cases, only findings specifically relating to analysis of the exclusively MS subgroup were reported in our review. If a study with a mixed sample only analyzed MS populations in conjunction with a mix of other neurological conditions, the study was excluded. Included studies must also have used a measure of anxiety, worry or fear, which was analyzed in relation to at least one other modifiable factor. Factors were classed as modifiable if they were considered to be reasonably amenable to change in a clinical context. Characteristics relating to participants’ socio-demographic or economic status were considered as unmodifiable for the purpose of this study and were therefore excluded. Similarly, studies which only explored anxiety in relation to overlapping constructs such as depression and stress were not included. This decision was made based on the large pool of existing evidence already inextricably linking anxiety to these factors. Validation/feasibility studies, posters and conference papers and studies with small samples (n < 30) were also excluded.
Selection process
First, all studies were uploaded to Rayyan.org which is an online application designed for systematic review screening [Citation18]. All study duplicates identified were removed by AF. Next abstracts were independently screened by both authors. Following abstract screening, all remaining full-texts were obtained and independently screened against the exclusion criteria. Any disagreements through the process were resolved through conversation.
Data extraction and analysis
During the screening phase, relevant data were extracted and put in tabular format independently by AF. This process was checked by RM with any disagreements resolved through discussion. Data extracted included study design, sample characteristics, such as age, gender, and type of MS, country in which the study was completed, a summary of relevant findings, and a list of any relevant measures used. Data were analyzed using the process of the narrative synthesis [Citation19]. Specifically, using reflective thematic analysis and through discussions among the two reviewers, a decision was made to classify identified modifiable factors under the broad categories of lifestyle, psychological, and social factors. Lifestyle factors were considered to be patterns of behavior which individuals have autonomy over. Social factors were categorized as factors which are related to the frequency, nature, and quality of interactions between the individual and others. Finally, psychological factors were categorized as mental states or processes, including attitudes, perceptions, and cognitive processes.
Quality assessment
The Mixed Methods Appraisal Tool (MMAT) was used to assess the quality of all included studies [Citation20]. The MMAT is a tool suitable for critical appraisal of a multitude of designs of empirical study, including cross-sectional, randomized controlled trials (RCTs) and cohort designs. As well as being widely employed in a number of recent systematic reviews, the MMAT has been used frequently in reviews involving PwMS [Citation21–23]. In addition, the MMAT has been shown to have a strong reliability, with an intra-class correlation of 0.8 suggesting agreement between individual reviewers [Citation24]. Following two screening questions, the tool is used to assess studies according to a series of five criteria which vary depending on the design of the study to be evaluated [Citation20]. Studies were scored based on their ability to satisfy these criteria, with studies satisfying three of the five criteria classified as “medium” quality studies. Studies that satisfied less or more criteria than this were classified as “low” or “high” quality studies, respectively. To ensure that recommendations for rehabilitation professionals can be based on the best available evidence, a decision was taken to exclude low quality studies from the analysis. This process was completed in tandem with the extraction of the outcome data.
Results
Overview
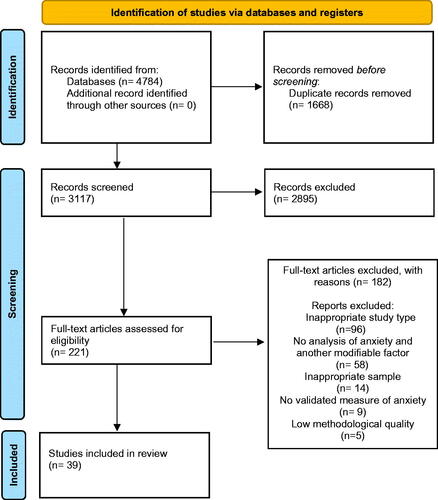
The initial search of online databases resulted in 4784 studies. After duplicate removal, 3116 unique entries remained. The abstracts of these studies were then screened against the exclusion criteria, which resulted in 221 studies moving to the full-text screening stage. One hundred and eighty-two of these studies were excluded, with the most common reason for exclusion being an inappropriate study type. Five studies were excluded due to low methodological quality following the quality appraisal process. This resulted in a final tally of 39 studies to be included in the narrative synthesis (see ).
Figure 1. PRISMA flow chart.
Study characteristics
displays summary data along with ratings of study quality. All included studies used a quantitative design, with cross-sectional designs (n = 23) being the most common, followed by RCTs (n = 9), and quantitative non-randomized studies (n = 7). Included studies were conducted in 15 different countries, with the USA being the most common (n = 8) followed by Iran (n = 6). The sample sizes of included studies ranged from 36 to 2399, with a total of 10 779 PwMS included in all studies. With the exception of one study [Citation62], all study samples had a majority female population, which is in line with MS population norms. All studies reported only on binary gender. The mean age of included study samples ranged from 24.2 to 58.3 years of age. Relapsing-remitting multiple sclerosis (RRMS) was the most common form of MS in all studies that provided this information, with a range of 61.9–100% of the sample. Descriptions of MS type were unavailable for nine studies.
Table 1. Sample demographic and quality appraisal data.
Measures of anxiety/fear
Twenty of the 39 studies included used the Hospital Anxiety and Depression Scale (HADS) [Citation63] as their measure of anxiety, with the State Trait Anxiety Index (STAI) [Citation64] (n = 9) and the Hamilton Anxiety Rating Scale (HAM-A) [Citation65] (n = 4) used in some studies. The Depression Anxiety and Stress Scale (DASS-21) [Citation66] (n = 2) and the Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety Subscale [Citation67] (n = 2) were used in two studies each. The Beck Anxiety Inventory (BAI) [Citation68], the Brief Symptom Inventory (BSI) [Citation69], and the Generalized Anxiety Disorder Assessment (GAD-7) [Citation70] were used to assess anxiety in individual studies. Other measures included the Falls Efficacy Scale International (FES-I) [Citation71] (n = 2) to assess fear of falling, a single item Visual Analog Scale (VAS) measure [Citation43] (n = 1) to assess fear of wheelchair dependency, and the fear of relapse scale to assess fear of MS relapse [Citation72].
Quality assessment
Following the exclusion of low-quality studies (n = 5), the remaining 39 studies showed evidence of methodological quality in at least three of the five areas that the MMAT appraises. It should be noted, however, that some of the quantitative descriptive studies failed to provide evidence to substantiate the representativeness of their sample. Furthermore, more than half of these studies failed to address the risk of nonresponse bias. Sampling strategies, statistical methods, and the measurements used in the included quantitative descriptive studies were of a good standard.
Narrative synthesis
Due to the heterogeneity of the associates being investigated in the studies reviewed, as well as the heterogeneity in outcome measures, a meta-analysis was not a suitable way of analyzing results. Thus, a process of narrative synthesis [Citation19] was deemed to be the best way to interpret findings of this review. Results were explored under the following headings based on the nature of the associate investigated: Psychological factors, social factors, and lifestyle factors (see for summary).
Table 2. Classification of associate categories.
Psychological factors
A total of 20 studies investigated anxiety in relation to some psychological associate. The majority of these associates related to either (1) participants’ ability to adjust and/or regulate their responses to change or difficulty or (2) participants’ perception of themselves.
Ability to adjust/cope with MS
Thirteen studies dealt with some dimension of participants’ ability to adapt to, or address, different circumstances relating to their disease. Overall, these 13 studies indicate that anxiety is associated with coping strategies. For example, two studies found significant independent associations between high resilience and lower anxiety [Citation53,Citation55]. Similarly, Van Damme et al. [Citation32] explored how participants’ approach to goals related to their anxiety, finding that tenacious goal pursuit (the adjustment of life circumstances to help goal achievement), flexible goal pursuit (the adjustment of life goals based on constraining life circumstance), and acceptance [Citation32] significantly predicted variance in anxiety. Grech et al. [Citation30] found higher use of acceptance and behavioral disengagement coping to mediate the relationship between low executive functioning and higher anxiety. The inverse was true of higher use of adaptive coping, which mediated the relationship between high executive function and lower trait anxiety. Prakash et al. [Citation37] similarly found a significant positive association between anxiety and maladaptive emotional regulation strategy. Here, maladaptive emotional regulation strategy refers to a pattern of attempts to exert control over one’s own emotional state which results in negative affective and goal-related outcomes. It is worth noting that, despite these findings, the relationship between adaptive strategy use and anxiety was not significant. Oz and Oz [Citation58] administered a psychoeducation intervention which successfully increased the use of problem-focused coping in participants, where participant anxiety also decreased following the intervention. Anagnostouli et al. [Citation25] found participants had significantly lower levels of anxiety following a cognitive-behavioral stress management program. Meanwhile, three studies [Citation46,Citation47,Citation60] found a statistically significant inverse association between mindfulness and anxiety, suggesting that this is another potential coping strategy that may benefit PwMS. In addition, De la Torre Gabriel et al. [Citation60] found that after a mindfulness intervention, the largest significant impact out of all factors assessed was on anxiety. In another study highlighting the importance of adjustment, Güner et al. [Citation61] found a significant correlation between anxiety and automatic thoughts and dysfunctional attitudes. Here, dysfunctional attitudes and automatic thoughts (both general and disease-related) were conceptualized as obstacles in the adaption process in individuals with MS. Finally, Alschuler et al. [Citation55] found that intolerance of uncertainty (and not optimism) was significantly and independently associated with anxiety in PwMS.
Perception of self
Eight studies investigated how participants’ self-perceptions are related to anxiety. This included four studies which investigated the relationship between anxiety and self-efficacy, with an additional study investigating falls self-efficacy. While most of these studies suggest self-efficacy as a potential mechanism for reducing anxiety, some mixed findings are evident. Jongen et al. [Citation35,Citation40] investigated the effects on anxiety of treatment programs which aimed to improve self-efficacy in PwMS. While significantly lower anxiety was found in participants with RRMS 12 months after treatment compared to at baseline, no such effect was found for participants with progressive MS [Citation40]. Following another intervention to increase self-efficacy, participants had reduced anxiety symptoms one month after treatment, but not at three- and six-month follow-ups [Citation35]. A further study found a significant negative correlation between both anxiety and self-efficacy and anxiety and self-esteem in a sample of young adults with MS [Citation27]. In contrast, Casey et al. [Citation33] found no significant correlation between anxiety and self-efficacy. In the one study which investigated falls self-efficacy, it was found that fear of falling significantly predicted the variance in falls self-efficacy [Citation29].
Four additional studies investigated other facets of participants’ perception of themselves and their illness in general. Bogart [Citation31] found that stronger disability identity (which involves affirming one’s status a member of a group that experiences disability) was a unique predictor of lower anxiety. Orr et al. [Citation14] found that anxiety symptoms, but not a clinical diagnosis of anxiety, was significantly associated with a perceived need for mental health care. Valvano et al. [Citation45] found a significant correlation between stigma and anxiety, with stigma indirectly affecting anxiety through “cognitive fusion”. Cognitive fusion here refers to a common experience in which an individual has difficulty distinguishing between their thoughts and their experiences. However, direct effects of stigma on anxiety were found to be non-significant. Giordano et al. [Citation43] was the only study to investigate associates relating to fear for wheelchair dependency. This study found a significant negative association between fear for wheelchair dependency and risk knowledge. Given the diversity of measures used here, we cannot be confident of the precise role of illness and self-perceptions on anxiety.
Lifestyle factors
A total of 14 studies investigated the association between some modifiable lifestyle factor and anxiety. The most commonly investigated lifestyle associate here was physical activity, investigated in eight studies. Seven of these eight studies found significant results linking exercise to improved anxiety outcomes. For example, Taspinar et al. [Citation62] found significant improvements in anxiety symptoms in an MS population following an eight-week calisthenic exercise program. Similarly, Hasanpour-Dehkordi et al. [Citation34] found that participants had significantly lower anxiety symptomology compared to controls following a 12-week yoga intervention. Additionally, Fleming et al. [Citation54] conducted a home-based Pilates intervention specifically aimed at reducing anxiety in PwMS which was successful in doing so. Both studies investigating the relationship between fear of falling and a lifestyle factor found significant results. Notably, Kalron et al. [Citation38] found that insufficiently active individuals had significantly increased fear of falling, with further analysis showing that fear of falling significantly predicted the variance in physical activity. Seddighi-Khavidak et al. [Citation56] found that lavender oil use during balance exercises was associated with significantly lower fear of falling than when the exercises were completed without lavender oil. Keikhaei et al. [Citation44] found significantly lower state and trait anxiety in an MS population following a motor-balance exercise intervention, adding to the evidence linking physical activity with improvements in anxiety. Coote et al. [Citation36] compared the effects of coupling an exercise program with two types of education program, one focused on attention control and another based on social cognitive theory (SCT). SCT outlines the relationship between an individual’s behavior and observation of other people’s behaviors, personal characteristics, and an individual’s environment. Specifically, this study included self-efficacy, outcome expectations, goal-setting, barriers, and benefits as principal components of the SCT education intervention. Significant improvements in anxiety were found at three and six-month follow-ups for the SCT group. However, no significant effects on anxiety were found in the attention control group. In contrast to many of the findings outlined above, Gascoyne et al. [Citation41] found no association between physical activity as measured by a SNAP (smoking, nutrition, alcohol, and physical activity) model and prevalence or severity of anxiety symptoms.
A few studies, including Gascoyne et al. [Citation41], investigated the relationship between anxiety and smoking or alcohol consumption. Gascoyne et al. [Citation41] found a significant association between smoking status, but not alcohol consumption, and anxiety severity. Pham et al. [Citation48] found a significant relationship between anxiety and smoking (using crude and adjusted odds ratios). However, when confounders were adjusted for, no significant relationship was found. Pham et al. [Citation48] also found no significant association between alcohol consumption and anxiety. In contrast to these findings, McKay et al. [Citation28] conducted a prospective study which found a significant association between anxiety at baseline and both alcohol dependence and smoking. It should be noted however that, despite this association at baseline, alcohol dependence had no significant effect on the participants’ odds of developing anxiety symptoms, at either the one- or two-year follow-ups. Contentti et al. [Citation50] found no association between cannabis use and anxiety. Similarly, Ramezani et al. [Citation51] found no association between smoking and anxiety in PwMS. Finally, Hanna and Strober [Citation59] found no association between substance abuse and anxiety. Finally, in the only study in our sample to investigate money management skills, it was found that individuals with efficient money management skills had lower state anxiety than inefficient individuals [Citation42].
Social factors
Six studies investigated social factors relating to anxiety. For example, Henry et al. [Citation26] found a negative correlation between anxiety and social support from friends. This relationship was confirmed as significant by a path analysis. Additionally, there was a significant negative correlation found between anxiety and social support from family and from significant others [Citation26]. However, these relationships did not stand up to more statistically robust analysis. Ratajska et al. [Citation57] found that higher social support was significantly negatively associated with lower state and trait anxiety and found evidence to suggest that this association remains stable over time. Hanna and Strober [Citation59] and Altınkaynak Yılmaz and Ozdelikara [Citation52] also found statistically significant negative associations between anxiety and social support. While Sparling et al. [Citation39] looked at social participation, rather than social support, the study’s findings add to the evidence that there may be an association between friendships and reduced anxiety symptomology. The study found that participants who interacted with friends in-person at least once per week were less anxious than those with less frequent friend interactions. Importantly, no such effect was found for participants who had regular interactions with friends in an online setting. Finally, Shaygannejad et al. [Citation49] found a significant correlation between fear of disease relapse in people with RRMS and social support.
Discussion
This review aimed to establish the extent to which recent research has investigated modifiable associates of anxiety in MS. While some findings were mixed, results suggest that a range of lifestyle, social, and psychological factors may play a role in the experience of anxiety in PwMS. These findings offer some insight into how psychological wellbeing might be improved in this group, paving the way for targeted interventions in the area.
The modifiable factors most frequently investigated in relation to anxiety in MS were psychological factors, categorized broadly as those relating to (1) an individual’s self-perceptions, and (2) their ability to cope with MS. Self-efficacy was the most researched construct relating to self-perceptions here [Citation27,Citation33,Citation35,Citation40], with this body of evidence suggesting that, overall, there is an inverse relationship between self-efficacy and anxiety in PwMS. This finding is unsurprising given that associations between self-efficacy and anxiety have been well-established in general populations [Citation73,Citation74]. One explanation for this comes from SCT, which proposes that higher self-efficacy helps individuals to feel more in control over potential threats, and thus, helps them to avoid apprehensive thought processes associated with anxiety [Citation75]. Our results suggest that this might be of particular importance in reducing anxiety in younger populations and those with RRMS; however, further research is necessary to investigate the effect of age on this relationship. It is also less clear as to the effects self-efficacy has on those with progressive MS, implying that any interventions designed to target anxiety should be tailored according to an individual’s disease status.
Our review also shows how anxiety in MS is associated with an individual’s ability to cope with, and adjust to, their disease. While there was some variance in the specific concepts examined in the studies reviewed, there is evidence to suggest that developing interventions around these concepts of adjustment could have, and have had, beneficial effects on anxiety for PwMS. Notably, results unanimously suggest that higher levels of acceptance, as well as related concepts such as disability identity were associated with lower levels of anxiety [Citation30,Citation32,Citation58]. Similarly, three studies showed robust evidence of an association between mindfulness and improved anxiety outcomes [Citation46,Citation47,Citation60]. Given existing evidence supporting the efficacy of mindfulness interventions generally [Citation76], as well as their efficacy when delivered online to an MS population [Citation77], the utility of these interventions is promising, particularly for PwMS wishing to improve anxiety symptoms while maintaining social distance. In addition, there was substantial evidence linking anxiety outcomes to a range of regulatory strategies, including stress-management, psychosocial adjustment, tenacious goal pursuit, and flexible goal pursuit [Citation32,Citation40]. Conversely, coping and regulatory strategies such as problem-focused coping, dysfunctional attitudes, and maladaptive emotional regulation, were associated with higher levels of anxiety [Citation32,Citation37]. Given these clear links between coping strategies and anxiety outcomes, it may be pertinent for MS service providers to assess the current coping strategies that PwMS depend on, as well as considering how best to foster more adaptive coping strategies associated with improved anxiety outcomes in MS.
Another notable finding from our review was the robust evidence supporting associations between physical activity and anxiety [Citation33,Citation34,Citation38,Citation54,Citation62]. This finding was unsurprising given the wealth of evidence from both general and MS populations highlighting beneficial effects of physical activity [Citation78,Citation79]. Learmonth and Motl [Citation80], who found links between improved quality of life and increased physical activity in PwMS, suggests that these benefits can at least be partially explained by improved self-efficacy, which, as we have shown, has also been linked to improved anxiety outcomes. The wealth of evidence tying physical activity to improved physical symptoms in PwMS means it is already recommended and prioritized in clinical practice and rehabilitation [Citation81,Citation82]; however, our findings serve to emphasize the importance of physical activity for the treatment of anxiety comorbidities, further strengthening the case for developing targeted exercise programs for PwMS.
Surprisingly, despite a wealth of evidence linking smoking and alcohol consumption to adverse outcomes for PwMS [Citation83,Citation84], there were inconclusive results regarding the relationship of these behaviors with anxiety in our review [Citation28,Citation41,Citation48,Citation51]. One explanation for this may be offered by Pham et al. [Citation48], who found that depression partially or fully mediated the relationship between smoking and anxiety [Citation28,Citation41,Citation48,Citation51]. Similarly, investigation of links between cannabis consumption, as well as substance use found no significant links between these behaviors and anxiety outcomes [Citation50,Citation59]. While the review findings mirror those from some studies conducted on general populations [Citation85], results of these individual studies do not provide enough evidence to make generalized conclusions, suggesting further research is warranted in this area.
There is more evidence to support the role of social support in reducing anxiety in MS. Of the six studies investigating social factors in our review, all of these highlighted the importance of social interactions and support in improved anxiety symptomology [Citation26,Citation39,Citation49,Citation52,Citation57,Citation59]. The context of these social interactions may be crucial however, with Sparling et al. [Citation39] finding how weekly interactions with friends in-person was linked with better anxiety outcomes, while no such link was found between anxiety and online interactions. This finding could be expected, given the emerging evidence linking higher social media use with higher levels of anxiety [Citation86,Citation87]. More research is required, however, to identify the specific aspects of social networks that could be improved to better address the social and emotional needs of PwMS in the context of the Covid-19 pandemic and beyond. Interestingly, in those studies that investigated different sources of social support (i.e., support from friends, family, and/or significant others), social support from friends was consistently linked to better anxiety outcomes, while evidence linking anxiety and support from family and significant others was less conclusive [Citation26,Citation49,Citation52]. Overall, these findings suggest that the relationship between anxiety and social factors is significant and further research is warranted to evaluate methods of improving social support in PwMS.
Limitations of this review
Almost all included studies relied solely on self-reported measures of anxiety or fear. While self-reported measures are useful from a feasibility standpoint and as such are used commonly, they can also be subject to several biases, including social desirability bias, which can impact results. Additionally, studies which investigated social support in relation to anxiety used self-reported measures, which is particularly concerning as individuals with high anxiety can be prone to distorted perspectives as to the amount or quality of the social support they receive [Citation12]. Furthermore, most studies used a cross-sectional design, which makes it difficult to assess the directionality of the relationships explored. Through the quality appraisal process, it became evident that many studies could not provide clear evidence as to the representativeness of their sample; however, by excluding studies of low quality, we can be more confident in the strength of the review findings. Further limitations are that studies not available in English were not included in this review. In addition, only peer-reviewed journal articles were included, with unpublished studies and any form of “grey literature” meeting exclusion criteria. Unfortunately, this makes included articles more likely to have some level of publication bias as unpublished material is more likely to include findings of non-significant relationships.
Conclusions
The findings of this review highlight links between anxiety in MS and a number of diverse factors, all of which are amenable to change. Specifically, we show how anxiety in PwMS is linked to a variety of psychological, social, and lifestyle factors. Key concepts linked with improved anxiety outcomes include a positive perception of self, an ability to adapt to the challenges of MS, adequate social support (particularly from friends) and an active lifestyle. These results have a number of potential implications for those working in MS rehabilitation, as well as for PwMS themselves. In particular, we argue that further research is needed to develop interventions with can target these modifiable factors in order to reduce the experience of anxiety in those with MS.
Supplemental Material
Download MS Word (28.5 KB)Disclosure statement
The authors declare no conflicts of interest.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- Thompson AJ, Baranzini ES, Geurts J, et al. Multiple sclerosis. Lancet. 2018;391(10130):1622–1636.
- Rahn K, Slusher B, Kaplin A. Cognitive impairment in multiple sclerosis: a forgotten disability remembered. In: Cerebrum: the Dana forum on brain science. Vol. 2012. Dana Foundation; 2012.
- Dua T, Rompani P, Multiple Sclerosis International Federation, et al. Atlas: multiple sclerosis resources in the world. Geneva, Switzerland: World Health Organization; 2008.
- Thornton EW, Tedman S, Rigby S, et al. Worries and concerns of patients with multiple sclerosis: development of an assessment scale. Mult Scler. 2006;12(2):196–203.
- Boeschoten RE, Braamse AMJ, Beekman ATF, et al. Prevalence of depression and anxiety in multiple sclerosis: a systematic review and meta-analysis. J Neurol Sci. 2017;372:331–341.
- Alsaadi T, El Hammasi K, Shahrour TM, et al. Depression and anxiety as determinants of health-related quality of life in patients with multiple sclerosis – United Arab Emirates. Neurol Int. 2017;9(4):7343–7378.
- Hviid LE, Healy BC, Rintell DJ, et al. Patient reported outcomes in benign multiple sclerosis. Mult Scler. 2011;17(7):876–884.
- Fiest KM, Walker JR, Bernstein CN, et al. Systematic review and meta-analysis of interventions for depression and anxiety in persons with multiple sclerosis. Mult Scler Relat Disord. 2016;5:12–26.
- Mohr DC, Cox D, Merluzzi N. Self-injection anxiety training: a treatment for patients unable to self-inject injectable medications. Mult Scler. 2005;11(2):182–185.
- Zorzon M, de Masi R, Nasuelli D, et al. Depression and anxiety in multiple sclerosis. A clinical and MRI study in 95 subjects. J Neurol. 2001;248(5):416–421.
- Morrow SA. Anxiety is more important than depression in MS – yes. Mult Scler. 2018;24(4):440–441.
- Bruce JM, Arnett P. Clinical correlates of generalized worry in multiple sclerosis. J Clin Exp Neuropsychol. 2009;31(6):698–705.
- Butler E, Matcham F, Chalder T. A systematic review of anxiety amongst people with multiple sclerosis. Mult Scler Relat Disord. 2016;10:145–168.
- Orr J, Bernstein CN, Graff LA, et al. Factors associated with perceived need for mental health care in multiple sclerosis. Mult Scler Relat Disord. 2018;25:179–185.
- Marrie RA, Reingold S, Cohen J, et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler. 2015;21(3):305–317.
- Bigaut K, Cohen M, Durand-Dubief F, et al. How to switch disease-modifying treatments in multiple sclerosis: guidelines from the French Multiple Sclerosis Society (SFSEP). Mult Scler Relat Disord. 2021;53:103076.
- Mohr DC, Cox D, Epstein L, et al. Teaching patients to self-inject: pilot study of a treatment for injection anxiety and phobia in multiple sclerosis patients prescribed injectable medications. J Behav Ther Exp Psychiatry. 2002;33(1):39–47.
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
- Lisy K, Porritt K. Narrative synthesis: considerations and challenges. JBI Evid Implement. 2016;14(4):201.
- Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inform. 2018;34(4):285–291.
- Quinn E, Hynes SM. Occupational therapy interventions for multiple sclerosis: a scoping review. Scand J Occup Ther. 2021;28(5):399–414.
- Ow N, Mozafarinia M, Mayo NE. Quality of life measures in pediatric multiple sclerosis: a systematic review and meta‐analysis. Dev Med Child Neurol. 2021;63(9):1051–1058.
- Power M, Arafa N, Wenz A, et al. Perceptions of fatigue and fatigue management interventions among people with multiple sclerosis: a systematic literature review and narrative synthesis. Int J Ther Rehabil. 2021;28(6):1–21.
- Pace R, Pluye P, Bartlett G, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53.
- Anagnostouli M, Babili I, Chrousos G, et al. A novel cognitive-behavioral stress management method for multiple sclerosis. A brief report of an observational study. Neurol Res. 2019;41(3):223–226.
- Henry A, Tourbah A, Camus G, et al. Anxiety and depression in patients with multiple sclerosis: the mediating effects of perceived social support. Mult Scler Relat Disord. 2019;27:46–51.
- Uccelli MM, Traversa S, Ponzio M. A survey study comparing young adults with MS and healthy controls on self-esteem, self-efficacy, mood and quality of life. J Neurol Sci. 2016;368:369–373.
- McKay KA, Tremlett H, Fisk JD, et al. Adverse health behaviours are associated with depression and anxiety in multiple sclerosis: a prospective multisite study. Mult Scler. 2016;22(5):685–693.
- Comber L, Coote S, Finlayson M, et al. An exploration of fall-related, psychosocial variables in people with multiple sclerosis who have fallen. Br J Occup Ther. 2017;80(10):587–595.
- Grech LB, Kiropoulos LA, Kirby KM, et al. Coping mediates and moderates the relationship between executive functions and psychological adjustment in multiple sclerosis. Neuropsychology. 2016;30(3):361–376.
- Bogart KR. Disability identity predicts lower anxiety and depression in multiple sclerosis. Rehabil Psychol. 2015;60(1):105–109.
- Van Damme S, De Waegeneer A, Debruyne J. Do flexible goal adjustment and acceptance help preserve quality of life in patients with multiple sclerosis? Int J Behav Med. 2016;23(3):333–339.
- Casey B, Uszynski M, Hayes S, et al. Do multiple sclerosis symptoms moderate the relationship between self-efficacy and physical activity in people with multiple sclerosis? Rehabil Psychol. 2018;63(1):104–110.
- Hasanpour-Dehkordi A, Jivad N, Solati K. Effects of yoga on physiological indices, anxiety and social functioning in multiple sclerosis patients: a randomized trial. J Clin Diagn Res. 2016;10(6):VC01–VC05.
- Jongen P, van Mastrigt G, Heerings M, et al. Effect of an intensive 3-day social cognitive treatment (can do treatment) on control self-efficacy in patients with relapsing remitting multiple sclerosis and low disability: a single-centre randomized controlled trial. PLOS One. 2019;14(10):e0223482.
- Coote S, Uszynski M, Herring MP, et al. Effect of exercising at minimum recommendations of the multiple sclerosis exercise guideline combined with structured education or attention control education – secondary results of the step it up randomised controlled trial. BMC Neurol. 2017;17(1):119–114.
- Prakash RS, Schirda B, Valentine TR, et al. Emotion dysregulation in multiple sclerosis: impact on symptoms of depression and anxiety. Mult Scler Relat Disord. 2019;36:101399.
- Kalron A, Aloni R, Givon U, et al. Fear of falling, not falls, impacts leisure-time physical activity in people with multiple sclerosis. Gait Posture. 2018;65:33–38.
- Sparling A, Stutts LA, Sanner H, et al. In-person and online social participation and emotional health in individuals with multiple sclerosis. Qual Life Res. 2017;26(11):3089–3097.
- Jongen PJ, Heerings M, Ruimschotel R, et al. An intensive social cognitive program (can do treatment) in people with relapsing remitting multiple sclerosis and low disability: a randomized controlled trial protocol. BMC Neurol. 2016;16(1):81.
- Gascoyne CR, Simpson S, Chen J, et al. Modifiable factors associated with depression and anxiety in multiple sclerosis. Acta Neurol Scand. 2019;140(3):204–211.
- Yael G, Nancy C, John D. Money management in multiple sclerosis: the role of cognitive, motor, and affective factors. Front Neurol. 2019;10:1128.
- Giordano A, Liethmann K, Köpke S, et al. Risk knowledge of people with relapsing-remitting multiple sclerosis: results of an international survey. PLOS One. 2018;13(11):e0208004.
- Keikhaei A, Sargazi GH, Saeedinezhad F, et al. The effect of motor-balance exercise on MS patients' anxiety and fatigue of Zahedan, Iran, 2014–2015. Med Sci. 2018;22(89):92–98.
- Valvano A, Floyd RM, Penwell-Waines L, et al. The relationship between cognitive fusion, stigma, and well-being in people with multiple sclerosis. J Context Behav Sci. 2016;5(4):266–270.
- Mioduszewski O, MacLean H, Poulin PA, et al. Trait mindfulness and wellness in multiple sclerosis. Can J Neurol Sci. 2018;45(5):580–582.
- Pagnini F, Cavalera C, Rovaris M, et al. Longitudinal associations between mindfulness and well-being in people with multiple sclerosis. Int J Clin Health Psychol. 2019;19(1):22–30.
- Pham T, Jetté N, Bulloch AGM, et al. The prevalence of anxiety and associated factors in persons with multiple sclerosis. Mult Scler Relat Disord. 2018;19:35–39.
- Shaygannejad V, Mirmosayyeb O, Nehzat N, et al. Fear of relapse, social support, and psychological well-being (depression, anxiety, and stress level) of patients with multiple sclerosis (MS) during the COVID-19 pandemic stage. Neurol Sci. 2021;42(7):2615–2614.
- Contentti EC, López PA, Criniti J, et al. Use of cannabis in patients with multiple sclerosis from Argentina. Mult Scler Relat Disord. 2021;51:102932.
- Ramezani N, Ashtari F, Bastami EA, et al. Fear and anxiety in patients with multiple sclerosis during COVID-19 pandemic; report of an Iranian population. Mult Scler Relat Disord. 2021;50:102798.
- Altınkaynak Yılmaz T, Ozdelikara A. The effect on the anxiety level of the social support given to multiple sclerosis patients. Perspect Psychiatr Care; 2021.
- Sbragia E, Colombo E, Pollio C, et al. Embracing resilience in multiple sclerosis: a new perspective from COVID-19 pandemic. Psychol Health Med. 2021;1–9.
- Fleming KM, Coote SB, Herring MP. Home-based Pilates for symptoms of anxiety, depression and fatigue among persons with multiple sclerosis: an 8-week randomized controlled trial. Mult Scler. 2021;27(14):2267–2279.
- Alschuler KN, Roberts MK, Herring TE, et al. Distress and risk perception in people living with multiple sclerosis during the early phase of the COVID-19 pandemic. Mult Scler Relat Disord. 2021;47:102618.
- Seddighi-Khavidak M, Tahan N, Akbarzadeh-Baghban A. Comparing the effects of vestibular rehabilitation with and without lavender oil scents as an olfactory stimulus on balance, fear of falling down and activities of daily living of people with multiple sclerosis: a randomized clinical trial. Disabil Rehabil. 2020;1–7.
- Ratajska A, Glanz BI, Chitnis T, et al. Social support in multiple sclerosis: associations with quality of life, depression, and anxiety. J Psychosom Res. 2020;138:110252–110252.
- Oz HS, Oz F. A psychoeducation program for stress management and psychosocial problems in multiple sclerosis. Niger J Clin Pract. 2020;23(11):1598–1606.
- Hanna M, Strober LB. Anxiety and depression in multiple sclerosis (MS): antecedents, consequences, and differential impact on well-being and quality of life. Mult Scler Relat Disord. 2020;44:102261.
- De la Torre Gabriel G, Mato I, Doval S, et al. Neurocognitive and emotional status after one-year of mindfulness-based intervention in patients with relapsing-remitting multiple sclerosis. Appl Neuropsychol Adult. 2020;1–10.
- Güner MC, Yazar MS, Meterelliyoz KŞ. Cognitive predictors of depression and anxiety in individuals with newly diagnosed multiple sclerosis. Eur J Psychiatry. 2020;34(4):202–210.
- Taspinar O, Aydın T, Celebi A, et al. Psychological effects of calisthenic exercises on neuroinflammatory and rheumatic diseases. Z Rheumatol. 2015;74(8):722–727.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Spielberger CD, Gorsuch RL, Lushene RE, et al. State-trait anxiety inventory. Palo Alto (CA): Mind Garden; 1983.
- Hamilton MAX. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55.
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343.
- Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18(3):263–283.
- Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897.
- Derogatis LR, Spencer PM. Brief Symptom Inventory: BSI. Vol. 18. Upper Saddle River (NJ): Pearson; 1993.
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097.
- Yardley L, Beyer N, Hauer K, et al. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005;34(6):614–619.
- Khatibi A, Moradi N, Rahbari N, et al. Development and validation of fear of relapse scale for relapsing-remitting multiple sclerosis: understanding stressors in patients. Front Psychiatry. 2020;11:226.
- Tahmassian K, Moghadam NJ. Relationship between self-efficacy and symptoms of anxiety, depression, worry and social avoidance in a normal sample of students. Iran J Psychiatry Behav Sci. 2011;5(2):91.
- Mills N, Pajares F, Herron C. A reevaluation of the role of anxiety: self‐efficacy, anxiety, and their relation to reading and listening proficiency. Foreign Lang Ann. 2006;39(2):276–295.
- Bandura A. Self-efficacy conception of anxiety. Anxiety Res. 1988;1(2):77–98.
- Jayewardene WP, Lohrmann DK, Erbe RG, et al. Effects of preventive online mindfulness interventions on stress and mindfulness: a meta-analysis of randomized controlled trials. Prev Med Rep. 2017;5(C):150–159.
- Bogosian A, Chadwick P, Windgassen S, et al. Distress improves after mindfulness training for progressive MS: a pilot randomised trial. Mult Scler. 2015;21(9):1184–1194.
- Conn VS. Anxiety outcomes after physical activity interventions: meta-analysis findings. Nurs Res. 2010;59(3):224–231.
- Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: a systematic review to inform guideline development. Arch Phys Med Rehabil. 2013;94(9):1800–1828.e3.
- Learmonth YC, Motl RW. Physical activity and exercise training in multiple sclerosis: a review and content analysis of qualitative research identifying perceived determinants and consequences. Disabil Rehabil. 2016;38(13):1227–1242.
- Dalgas U, Ingemann-Hansen T, Stenager E. Physical exercise and MS recommendations. Int MS J. 2009;16(1):5–11.
- Halabchi F, Alizadeh Z, Sahraian MA, et al. Exercise prescription for patients with multiple sclerosis; potential benefits and practical recommendations. BMC Neurol. 2017;17(1):1–11.
- Wang Y, Wang Y, Li R, et al. The epidemiology of alcohol consumption and multiple sclerosis: a review. Neurol Sci. 2015;36(2):189–196.
- Paz-Ballesteros WC, Monterrubio-Flores EA, de Jesús Flores-Rivera J, et al. Cigarette smoking, alcohol consumption and overweight in multiple sclerosis: disability progression. Arch Med Res. 2017;48(1):113–120.
- Haynes JC, Farrell M, Singleton N, et al. Alcohol consumption as a risk factor for anxiety and depression: results from the longitudinal follow-up of the National Psychiatric Morbidity Survey. Br J Psychiatry. 2005;187(6):544–551.
- Vannucci A, Flannery KM, Ohannessian CM. Social media use and anxiety in emerging adults. J Affect Disord. 2017;207:163–166.
- Baltacı Ö. The predictive relationships between the social media addiction and social anxiety, loneliness, and happiness. Int J Progress Educ. 2019;15(4):73–82.
