Abstract
Purpose
The primary aim of this study was to investigate the concurrent validity of the PAM AM400 accelerometer for measuring physical activity in usual care in hospitalized patients by comparing it with the ActiGraph wGT3X-BT accelerometer.
Materials and methods
This was a prospective single centre observational study performed at the University Medical Centre Utrecht in The Netherlands. Patients admitted to different clinical wards were included. Intraclass Correlation Coefficients (ICCs) were computed using a two-way mixed model with random subjects. Additionally, Bland-Altman plots were made to visualize the level of agreement of the PAM with the ActiGraph. To test for proportional bias, a regression analysis was performed.
Results
In total 17 patients from different clinical wards were included in the analyses. The level of agreement between the PAM and ActiGraph was found strong with an ICC of 0.955. The Bland-Altman analyses showed a mean difference of 1.12 min between the two accelerometers and no proportional bias (p = 0.511).
Conclusions
The PAM is a suitable movement sensor to validly measure the active minutes of hospitalized patients. Implementation of this device in daily care might be helpful to change the immobility culture in hospitals.
Physical inactivity is common during hospital admission and the main cause of loss of muscle mass and physical fitness.
The PAM AM400 is a suitable movement sensor to validly measure the active minutes of hospitalized patients.
Implementation of this device in daily care might be helpful to change the immobility culture in hospitals.
IMPLICATIONS FOR REHABILITATION
Introduction
Physical inactivity is common during hospital admission and the main cause of loss of muscle mass and physical fitness frequently leading to long-lasting and permanent disability, known as hospital-associated disability [Citation1–4]. Only a small percentage of the amount of physical inactivity during a hospital stay can be attributed to medical restrictions [Citation5]. Inactivity is mainly the result of the hospital culture including convenient organization from the perspective of the hospital staff and the built environment [Citation5]. Hospital-associated disability is therefore considered as an iatrogenic effect that can be prevented [Citation6]. Although there is awareness in health care professionals about the importance of physical activity during a hospital stay, ambulation is one of the most often missed tasks [Citation7]. Providing patients and health care professionals with concrete solutions is suggested to increase the integration of physical activity in daily hospital care [Citation8].
Continuous and standardized physical activity monitoring during hospital stay might be a suitable concrete solution as it increases the visibility of inpatient physical (in)activity and at the same time can serve as input to evaluate and improve the physical activity level of individual patients. Accelerometers may offer an accurate way of measuring physical activity. High-quality devices that can assess body posture and energy expenditure in detail are commonly used in research settings [Citation9–11]. Unfortunately these devices are not suitable for use in daily hospital care as they are often expensive and lack user-friendliness [Citation12]. Although many consumer-oriented activity trackers like smartwatches are available, these devices are also less suitable for use in hospitalized patients. The most common location on the wrist can introduce bias due to arm movements in sitting and lying position, slow walking speed, decreased trunk rotation during walking and the frequent use of walking aids in the hospital [Citation13,Citation14]. Therefore, localization of the accelerometer on the ankle seems to be more appropriate in this target group [Citation15]. This also seems the best location for measuring physical activity in people with slower walking speeds, which is often the case in hospitalized patients [Citation11]. For these reasons the Personal Activity Monitor (PAM) AM300 [Citation16] was especially adapted for daily hospital use. The resulting PAM AM400 is designed as a small waterproof button cell with a long battery life that can easily and safely be attached at the ankle.
As the accuracy of the accelerometers varies between devices, population-specific validation studies are needed to determine their suitability in measuring the physical activity levels of hospitalized (older) adults [Citation11]. Therefore, the aim of this study was to investigate the concurrent validity of the PAM AM400 accelerometer for measuring physical activity in the hospitalized population by comparing it with the ActiGraph wGT3X-BT accelerometer which is often used in research settings [Citation17]. Because the validity might differ across various walking speeds (in particular lower walking speeds), the secondary aim was to investigate the association of walking speed with the level of agreement between the two accelerometers.
Methods
Study design and setting
This was a cross-sectional single centre observational study performed at the University Medical Centre Utrecht in The Netherlands to determine the concurrent validity of the Personal Activity Monitor (PAM). The study protocol was approved by the medical ethical committee of the University Medical Centre Utrecht in The Netherlands (no. 16-817 and no. 15-653). All participants gave written informed consent. The STROBE checklist for reporting observational studies was used as a guideline in writing this study.
Accelerometers
For this study, the PAM (version AM400) and ActiGraph (version wGT3X-BT) accelerometers were used. The PAM accelerometer (Pam, Oosterbeek, The Netherlands) is a small sensor, especially designed for use in clinical hospital settings. To increase usability in daily care, a sensor was developed that was waterproof, cheap (<50 euros), easy to disinfect with alcohol and with long battery life. The resulting sensor is shaped like a small button cell with an incorporated battery that can last up to 12 months during full-time use (Supplementary Figure 1). The sensor is worn around the ankle using a soft elastic band (). Prior to the current study, the threshold for detecting movement for the PAM accelerometer was determined by comparing outcomes of the PAM (data logger version) with video recordings. In total, five hospitalized patients meeting the following inclusion criteria were included: (i) > 65 years, (ii) able to walk independently (with or without walking aid) and (iii) stable medical condition. During the measurements, participants were asked to perform tasks following a structured measurement protocol with physical activities and body postures related to hospital admission like transfers from bed to chair and walking at different speeds (). The protocol took a total of 19.5 min and was recorded on video. The data output of the PAM included the movement intensity by the degree of acceleration, expressed as Metabolic Equivalent of Task (MET) values per second. This output was compared to the moments where participants were physically active (i.e., making a transfer, rising from a chair, walking or cycling) according to the video recordings. Lying and sitting were defined as physically inactive. Based on this comparison, the threshold for the detection of ‘physical activity’ was set at 1.4 MET. Using this threshold the PAM showed to detect slow physical activities but to disregard insignificant movements of the lower extremity (like wiggling of the ankle). The PAM only registers movements above this threshold, defined as ‘active minutes’.
Figure 1. Scatterplot for the PAM and the ActiGraph. The X and Y axis represents the total number of active minutes per participant.
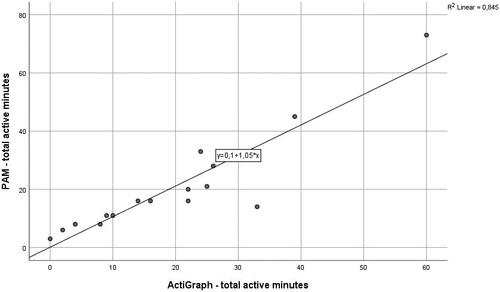
Figure 2. Bland–Altman plot for the PAM and ActiGraph. The X axis represents the mean of the active minutes of both accelerometers per participant. On the Y axis the middle line represents the mean difference between the two accelerometers, the upper and lower lines represent the limits of agreement (mean difference ± 1.96 SD).
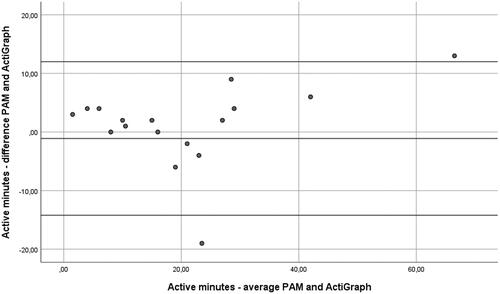
Table 1. Patient characteristics.
In the current study, the ActiGraph accelerometer (Pensacola, FL, USA) was used as a comparison. The ActiGraph captures and records high-resolution raw acceleration data, which is converted into a variety of objective activity measures. A systematic review on physical activity and sedentary behavior in older adults included 59 studies (n = 20,937 participants) that all used the ActiGraph accelerometer [Citation17]. This makes the ActiGraph a well-established accelerometer and suitable as a comparison for determining the concurrent validity of other accelerometers [Citation18]. In the current study the ActiGraph accelerometer was worn at the waist.
Study procedures
Patients admitted to different clinical wards of the hospital were approached for participation after consultation with the coordinating nurse. Patients were eligible for inclusion when they were able to walk (with or without help or a walking aid). Patients with prescribed bedrest or patients planned for discharge during the day of inclusion were not eligible for inclusion. Patients had to give written informed consent to be included. Participants were asked to wear the accelerometers simultaneously for one day between 10 am and 4 pm. Additionally, participants were asked to perform a 4-meter walk test to determine comfortable walking speed [Citation19,Citation20].
Sample size calculation
Based on an expected ICC of 0.85 and a minimum acceptable ICC of 0.5 (two-tailed alpha = 0.05, power = 0.80) the statistical power analysis estimated a sample size of 17 patients [Citation21].
Statistical analyses
Normality tests were performed using the Kolmogorov-Smirnov test. Outcomes that were normally distributed were reported as means with standard deviation (SD). Non-normally distributed outcomes were reported as median with minimum and maximum values [Citation22].
The concurrent validity of the PAM was investigated by determining the level of agreement with the ActiGraph accelerometer. The total active minutes of the PAM was compared with the total active minutes of the ActiGraph accelerometer. The active minutes (MET ≥ 1.4) of the ActiGraph were determined by calculating a MET value according to the formula of Sasaki et al. [Citation23] for every 1 s epoch. The sum of all seconds with a score of MET ≥ 1.4 resulted in the total number of active minutes per participant.
Intraclass Correlation Coefficients (ICCs) were computed using a two-way mixed model with random subjects. The following classification was used to determine the level of agreement: <0.3 = weak, 0.3–0.7 = moderate and >0.7 = strong agreement [Citation24,Citation25]. Additionally, Bland-Altman plots were made to visualize the level of agreement of the PAM with the ActiGraph [Citation26]. For that purpose, the mean difference in active minutes between the accelerometers, and the upper and lower limits of agreement (mean difference ± 1.96 SD) were calculated [Citation26,Citation27]. To test for proportional bias, a regression analysis was performed for which a p < 0.05 indicated an unequal distribution of measurement points below and above the mean difference line [Citation27].
To investigate a possible relationship between walking speed and level of agreement between the two accelerometers, the correlation between the PAM-ActiGraph differences in active minutes and the 4-meter walking speed (meter per second) was determined using the Pearson correlation coefficient. IBM SPSS statistics (version 25) was used for all data analyses.
Results
Data collection took place between November 2019 and March 2020. Primarily, 19 hospitalized patients were included in the study. One participant was excluded from the data analyses because this participant was only able to move around on one leg with the use of a walking frame. A second participant was excluded as this participant was admitted only for a few hours. This led to a total inclusion of 17 patients. Participant characteristics are summarized in . The median (min-max) time that patients wore the accelerometers was 378 (163–422) minutes (). The mean (SD) active minutes registered by the PAM and ActiGraph were 21 (17) and 20 (15) min, respectively ().
Table 2. Physical activity outcomes and level of agreement statistics.
The level of agreement between the PAM and ActiGraph was found strong with an ICC of 0.955. visualises the association between the two accelerometers and shows the Bland-Altman plot. The Bland-Altman analyses () showed a mean difference of 1.12 min and no proportional bias (p = 0.511). The Pearson correlation coefficient between the PAM-ActiGraph differences in active minutes and walking speed is 0.163 (p = 0.579).
Discussion
This study shows a strong agreement (ICC 0.955) of the PAM AM400 accelerometer with the ActiGraph wGT3X-BT in measuring the active minutes of inpatients during an average hospital day. The PAM AM400 was especially developed for use in the hospital setting including patients with slower walking speeds and low intensive movement behavior. Although earlier studies have suggested that the ankle is a suitable location for detecting movement behavior, the location of the PAM at the ankle raised the question whether it would detect insignificant movements of the lower leg and thereby overestimate the active minutes of inpatients [Citation15,Citation28]. The excellent level of agreement with the ActiGraph, which was located at the waist during our study, suggests that the PAM ignores insignificant movements and does not overestimate the physical activity level of patients during a hospital stay.
Additionally, we found no significant correlation between walking speed and the level of agreement of the two accelerometers. Although this result should be interpreted with caution due to the low sample size, it indicates that the agreement of the PAM and the ActiGraph is independent of the walking speed. Therefore, the results of this study indicate that the PAM accelerometer is a valid device for measuring physical activity in daily hospital care.
Currently, inpatient movement behavior is mainly collected for research purposes [Citation4,Citation9,Citation29,Citation30]. We consider the quantification of inpatient movement behavior in daily clinical hospital care as an important step towards changing the immobilizing culture within hospitals. When measuring inpatient movement behavior is adopted in daily hospital care, similar to the daily measurement of temperature and heart rate, it will be more likely that patients’ movement behavior will be integrated into the clinical reasoning process of the healthcare professionals and that addressing a patients’ movement behavior will remain on the priority list of healthcare professionals [Citation7].
Having an inexpensive, user-friendly and easy-to-use tool that can validly measure physical activity is a necessity to achieve adoption in daily hospital care. Because of its low price (less than 50 US Dollars/Euros), long term use (battery lasts up to 12 months) and usability (patients report not noticing the device during the day and the device is always ready to use), we consider the PAM a suitable measurement instrument in the daily hospital care. Therefore, the PAM accelerometer has been integrated into the electronic patient health record in some Dutch hospitals to measure inpatient physical activity levels continuously. This increases the insight into patients’ their physical activity level in nursing and medical staff.
Nevertheless, allowing health care professionals to measure and visualize inpatient movement behavior will not result in the adoption of this new metric automatically. The implementation of physical activity as a new metric in clinical care needs dedicated attention. A recent systematic review shows that physical activity interventions using accelerometers were the most successful when they integrated multiple behavior change techniques and guidance by a health care professional [Citation31]. Therefore, currently studies are performed on suitable interventions and implementation strategies.
Furthermore, although ‘active minutes’ is a simple and intuitive outcome for physical activity, there remains research to be done on the determination of what the most important physical activity metrics are related to patient outcomes. This may in turn prove helpful in motivating change in the immobilizing culture in hospitals. Furthermore, a uniform outcome measure will contribute to research in this area.
Limitations
We have chosen to compare the PAM accelerometer with the ActiGraph accelerometer to determine concurrent validity [Citation18]. Although the ActiGraph is considered as a well-established comparison, it cannot be considered as a gold standard. A comparison with video recordings would have resulted in a more robust validation. However, video recordings of patients during an average hospital day are ethically undesirable. For the level of agreement analyses, participants wore the accelerometers between 9 am and 4 pm. Measuring physical activity for a continuous period of 24 h would have better reflected physical activity levels in the real-life hospital setting. However, as it was our goal to compare accelerometers, a variation in physical activities was required which was most likely to be registered during the daytime. The duration of total wear time and the amount of physical activity were considered less important. Although our sample size is comparable to similar studies and the ICC reached statistical significance, a larger sample size would have led to better generalizability of the results and would have made it possible to compare ICC’s between participants with different walking speeds [Citation32]. Finally, we did not include patients with neurological deficits. Since that population may have more physical and unilateral impairments, our results should not be generalized to patients with neurological deficits.
Conclusion
In conclusion, we state that the PAM AM400 is a suitable movement sensor to validly measure the active minutes of hospitalized patients. Implementation of this device in daily hospital care might be helpful to change the immobility culture in hospitals.
Supplementary_material.docx
Download MS Word (74.8 KB)Disclosure statement
The authors confirm that there are no conflicts of interest to disclose.
References
- Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51(4):451–458.
- Brown CJ, Redden DT, Flood KL, et al. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57(9):1660–1665.
- van de Port IG, Valkenet K, Schuurmans M, et al. How to increase activity level in the acute phase after stroke. J Clin Nurs. 2012;21(23–24):3574–3578.
- Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol A Biol Sci Med Sci. 2013;68(3):331–337.
- Zisberg A, Shadmi E, Gur-Yaish N, et al. Hospital-associated functional decline: the role of hospitalization processes beyond individual risk factors. J Am Geriatr Soc. 2015;63(1):55–62.
- Sourdet S, Lafont C, Rolland Y, et al. Preventable iatrogenic disability in elderly patients during hospitalization. J Am Med Dir Assoc. 2015;16(8):674–681.
- Kalisch BJ, Landstrom G, Williams RA. Missed nursing care: errors of omission. Nurs Outlook. 2009;57(1):3–9.
- De Klein K, Valkenet K, Veenhof C. Perspectives of patients and health-care professionals on physical activity of hospitalized patients. Physiother Theory Pract. 2021;37(2):307–314.
- Valkenet K, Veenhof C. Validity of three accelerometers to investigate lying, sitting, standing and walking. Submitted. 2018.
- Anderson JL, Green AJ, Yoward LS, et al. Validity and reliability of accelerometry in identification of lying, sitting, standing or purposeful activity in adult hospital inpatients recovering from acute or critical illness: a systematic review. Clin Rehabil. 2018;32(2):233–242.
- Lim SER, Ibrahim K, Sayer AA, et al. Assessment of physical activity of hospitalised older adults: a systematic review. J Nutr Health Aging. 2018;22(3):377–386.
- Valkenet K, Veenhof C. Validity of three accelerometers to investigate lying, sitting, standing and walking. PLOS One. 2019;14(5):e0217545.
- Sung PS, Lee KJ, Park WH. Coordination of trunk and pelvis in young and elderly individuals during axial trunk rotation. Gait Posture. 2012;36(2):330–331.
- Swinnen E, Baeyens JP, Pintens S, et al. Walking more slowly than with normal velocity: the influence on trunk and pelvis kinematics in young and older healthy persons. Clin Biomech. 2013;28(7):800–806.
- Mannini A, Intille SS, Rosenberger M, et al. Activity recognition using a single accelerometer placed at the wrist or ankle. Med Sci Sports Exerc. 2013;45(11):2193–2203.
- Vooijs M, Alpay LL, Snoeck-Stroband JB, et al. Validity and usability of low-cost accelerometers for internet-based self-monitoring of physical activity in patients with chronic obstructive pulmonary disease. Interact J Med Res. 2014;3(4):e14.
- Gorman E, Hanson HM, Yang PH, et al. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. Eur Rev Aging Phys Act. 2014;11:35–49.
- Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745.
- Peters DM, Fritz SL, Krotish DE. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther. 2013;36(1):24–30.
- Peel NM, Kuys SS, Klein K. Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci. 2013;68(1):39–46.
- Walter SD, Eliasziw M, Donner A. Sample size and optimal designs for reliability studies. Statist Med. 1998;17(1):101–110.
- Ghasemi A, Zahediasl S. Normality tests for statistical analysis: a guide for non-statisticians. Int J Endocrinol Metab. 2012;10(2):486–489.
- Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. J Sci Med Sport. 2011;14(5):411–416.
- Fleiss JL. The design and analysis of clinical experiments. New York: John Wiley & Sons, Inc; 1986.
- Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310.
- Giavarina D. Understanding bland Altman analysis. Biochem Med. 2015;25(2):141–151.
- Svarre FR, Jensen MM, Nielsen J, et al. The validity of activity trackers is affected by walking speed: the criterion validity of Garmin Vivosmart® HR and StepWatch™ 3 for measuring steps at various walking speeds under controlled conditions. PeerJ. 2020;8:e9381.
- Valkenet K, Bor P, van Delft L, et al. Measuring physical activity levels in hospitalized patients: a comparison between behavioural mapping and data from an accelerometer. Clin Rehabil. 2019;33(7):1233–1240.
- Fazio S, Stocking J, Kuhn B, et al. How much do hospitalized adults move? A systematic review and meta-analysis. Appl Nurs Res. 2020;51:151189.
- de Leeuwerk M, Bor P, van der Ploeg H, et al. The effectiveness of physical activity interventions using activity trackers during or after inpatient care: a systematic review and meta-analysis of randomized controlled trials. Int J Behav Nutr Phys Act. 2022.
- Liao JJ. Sample size calculation for an agreement study. Pharm Stat. 2010;9(2):125–132.
