 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
People with Parkinson’s disease (hereafter Parkinson’s) can experience stigma through the attitudes and actions of others (enacted stigma) and through anticipation of enacted stigma and internalisation of negative stereotypes (felt stigma). Self-compassion may protect against the impact of stigma. This study aimed to investigate the relationships between self-compassion, stigma, and psychological distress among people with Parkinson’s.
Methods
A total of 130 people with Parkinson’s completed questionnaires measuring self-compassion, enacted and felt stigma, and depression, anxiety, and stress. Correlation, mediation, and moderation models were used to investigate relationships between variables.
Results
All variables correlated significantly in the expected directions. Felt stigma mediated the relationship between self-compassion and the three outcome variables – depression, anxiety, and stress. Self-compassion did not moderate the relationship between enacted stigma and distress and suggested enacted stigma was associated with distress, regardless of levels of self-compassion.
Conclusions
Self-compassion and both enacted and felt stigma are important predictors of distress for people with Parkinson’s. Part of the relationship between lower self-compassion and psychological distress appears to occur via the internalisation of stigma. These findings may be relevant to the development of individualised and societal interventions with the aim of improving the psychological wellbeing of people with Parkinson’s.
Self-compassion was associated with lower levels of psychological distress (i.e., depression, anxiety, and stress) and self-stigma partially mediated this relationship.
Self-compassion did not moderate the relationship between enacted stigma and psychological distress, suggesting enacted stigma increases distress, regardless of self-compassion.
The development and assessment of the effectiveness of compassion-focused interventions tailored for people with Parkinson’s may be important as well as systemic stigma focused interventions.
Implications for rehabilitation
Introduction
Parkinson’s disease (referred to throughout this paper as “Parkinson’s”: the preferred terminology by the charity Parkinson’s UK) is a neurodegenerative condition affecting around 0.3% of people worldwide [Citation1], with increasing prevalence after the age of 60 [Citation2]. Parkinson’s is classified as a movement disorder [Citation3], with affected individuals often experiencing problems with initiating movement (akinesia), slowed movement (bradykinesia), tremor, rigidity, gait disturbance, and speech difficulties [Citation4]. A number of other difficulties, e.g., with cognition, sleep, and eating [Citation5,Citation6], can also be experienced but it is often the psychological problems which individuals report as most disruptive to overall well-being [Citation7].
Indeed, a systematic review of the literature found that 35% of people with Parkinson’s experience clinically significant symptoms of depression [Citation8], while the prevalence of anxiety is estimated at 25% [Citation9]. Conceptualisations of these experiences have traditionally assumed a neurobiological basis, suggesting that psychological distress occurs as a direct consequence of pathological processes, such as changes in dopaminergic, serotonergic, and noradrenergic systems and fronto-striatal circuitry [Citation10–12]. However, in addition to the recognised role of neurobiological changes, growing evidence suggests that social and psychological factors are important in the development of psychological distress (see [Citation13] for a review). In particular, two currently little explored psychosocial factors that may be relevant to a more comprehensive understanding of psychological distress among people with Parkinson’s are stigma and self-compassion.
Goffman’s [Citation14] early conceptualisation of stigma described it as an individual attribute which is discredited by society, leading to loss of social status. Later, stigma was more comprehensively defined as a phenomenon whereby individuals are labelled, stereotyped, discredited, and discriminated against, based on certain attributes which are devalued by society, in a context where they have reduced power [Citation15]. “Enacted stigma” is a term used to describe the negative reaction that the stigmatised individual receives from others, through their attitudes and actions [Citation16]. When an individual expects or fears enacted stigma, this is known as “felt stigma”, or “internalised stigma” [Citation17]. Felt stigma may also involve identification with negative stereotypes and the application of discrediting attitudes to the self [Citation18]. Experiences of felt stigma have been found to be associated with feelings of shame and low self-esteem [Citation15,Citation19].
In the context of illness and impairment, where difference may be highly visible, individuals may be at a higher risk of stigmatisation [Citation20,Citation21] compared to non-affected individuals. People with Parkinson’s may present with visible differences through the more overt motor and facial symptoms and communication difficulties, increased dependence on others, and lifestyle changes necessitated by symptoms [Citation22], which can all lead to experiences of stigma [Citation22–25]. Research has demonstrated stigmatising views towards people with Parkinson’s held by both professionals [Citation26] and members of the public [Citation27,Citation28]. Furthermore, experiences of stigma have been found to be associated with heightened levels of anxiety, depression, and stress among people with Parkinson’s [Citation29–31]. Felt stigma has been found to be prevalent among people with Parkinson’s even in the absence of direct experience of enacted stigma, demonstrating the importance of implicit public attitudes [Citation29]. In addition, enacted stigma can contribute to the internalisation of stigma and experiences of psychological distress [Citation32]. Ma et al. [Citation29] found a stronger relationship between felt stigma and depression than enacted stigma and depression, suggesting that the internalisation of stigma is an important factor relating to the development of psychological distress.
Self-compassion is defined as a non-judgemental acknowledgement of one’s own suffering and a self-directed response based upon “kindness, concern and support” [Citation33,p.121]. Self-compassion is considered an important element of emotional regulation, access to which is affected by early relational experiences [Citation34,Citation35]. The development of self-compassion affects how we cope with difficult life events and experiences – how we appraise threats, experience affiliative emotions, view and relate to ourselves and self-soothe. Across a range of populations, self-compassion has been shown to be positively associated with psychological wellbeing [Citation36] and negatively associated with symptoms of depression and anxiety [Citation37]. The one previous study on self-compassion in Parkinson’s found it predicted depression, anxiety, and stress, but not life satisfaction [Citation38]. Furthermore, it has been demonstrated that interventions aimed at increasing self-compassion can alleviate psychological distress in people with neurological problems – for example, traumatic brain injury [Citation39], dementia [Citation40], and multiple sclerosis [Citation41].
Self-compassion may directly affect self-stigma in Parkinson’s. Self-compassion has been shown to directly relate to different forms of self-stigma in a variety of other populations [Citation42–45]. In addition, considering processes related to stigma which may be directly relevant to people with Parkinson’s, self-compassion has been shown to be associated with fewer negative, self-critical thoughts, less rumination about unpleasant evaluation and less embarrassment [Citation46] and has been associated with lower feelings of shame in other serious illness [Citation47]. Thus, in addition to self-compassion’s direct effect on psychological distress, it may also affect distress indirectly via its effect on self-stigma.
Furthermore, Wong et al. [Citation48,Citation49] suggest that there are specific cognitive, emotional, and social mechanisms through which self-compassion affects the impact of enacted stigma. Specifically, Wong et al. propose a mediated-moderation model whereby self-compassion first moderates the relationship between external and internal stigma and second moderates the relationship between external stigma and negative outcomes. This latter moderation will be our focus here. Cognitively, an individual with higher self-compassion may be more able to appraise accurately the threats of stigmatisation and positively reframe experiences of enacted stigma, allowing them to feel safer and more content and less distressed. Wong et al. [Citation48] also describe how self-compassion can facilitate the processing and regulation of emotions, allowing an individual to cope better with enacted stigma and therefore experience less distress. Finally, it is suggested that more self-compassionate individuals are both more able to seek social support, and are more forgiving of stigma enactments; this may in turn reduce anxieties about social rejection due to the stigmatised attribute [Citation48]. However, it is currently unclear if/how these relationships between self-compassion and stigma are applicable to people with Parkinson’s.
Consequently, the overall aim of this study was to investigate the relationships between the constructs of stigma, self-compassion, and psychological distress (as measured by depression, anxiety, and stress scores) among people with Parkinson’s. It was expected that individuals who experienced more stigma would have higher levels of depression, anxiety, and stress, and that more self-compassionate individuals would experience lower levels of depression, anxiety, and stress. It was hypothesised that more self-compassionate individuals would experience less felt stigma and this in turn would lead to less depression, anxiety, and stress, i.e., felt stigma would mediate the relationship between self-compassion and distress. Second, following Wong et al.’s model, it was hypothesised that self-compassion would moderate the relationship between enacted stigma and distress.
Methods
Participants
A total of 153 individuals consented to take part in the study; however, two did not provide any data and nine had multiple measures, including demographics missing so were removed. A further four participants were missing one measure but as listwise deletion is acceptable for up to approximately 5% of the data [Citation50], these were deleted. Eight participants were from outside the UK and their data were removed due to the possible different impact of different cultures and context on stigma. The participants were therefore 130 individuals with a self-reported diagnosis of Parkinson’s.
A priori power calculations were conducted to determine the sample size required based on the primary research question, the mediation analysis. A bias-corrected bootstrapped mediation analysis with medium effect sizes between the independent and mediator variables () and the mediator and dependent variables (
) (
=0.39) requires 71 participants to be adequately powered [Citation51]. Therefore, the sample of 130 participants was adequate.
Participants were asked to confirm that they met the inclusion criteria for the study, namely that they had a diagnosis of Parkinson’s, had had their diagnosis for a minimum of 6 months and were aged 18 years or older. It was presumed that participants had sufficient cognitive ability to undertake the survey, although as it was completed anonymously, this was not formally assessed. Four individuals contacted the researcher for paper copies of the questionnaires, which were posted along with stamped addressed envelopes for their return; however, only one was returned. The remainder of the sample completed the questionnaires in online format.
Procedure
The Patient and Public Involvement Volunteers from Parkinson’s UK provided feedback on the initial design. Ethical approval was granted by the Lancaster University Faculty of Health and Medicine Research Ethics Committee (reference: FHMREC18052). The study was advertised on the Parkinson’s UK website, in the Parkinson’s UK online newsletter, and on the social media platform Twitter and was active between November 2018 and March 2019. Potential participants were presented with a link to an “Information for Participants” page and invited to either complete an online survey or to contact the first author to request a hard copy. Participants were asked to confirm that they had read and understood the “Information for Participants” and gave their consent for their data to be used in the research.
Materials
A demographic and clinical information questionnaire asked about age, gender, ethnic group or background, current place of living (country), current living arrangements, partnership status, employment status, time since diagnosis, and current treatment for Parkinson’s (e.g., whether they used medication, deep brain stimulation, an apomorphine pump, etc.).
Validated measures
Functional Status Questionnaire (FSQ) [Citation52] – physical function subscales
The first subscale contains three items designed to assess functioning in basic activities of daily living (ADLs), such as washing and dressing and moving around the home. The second subscale has six items and measures functioning in intermediate ADLs, such as completing housework and physical activities outside of the home. Items are scored from four (usually did with no difficulty) to one (usually did not do because of health), with the additional option, “usually did not do for other reasons”, which scores zero. Scaled scores (between 0 and 100) are derived from the total scores for each subscale, with higher scaled scores representing higher levels of functional ability. Each subscale has a “warning zone” cut-off score, above which functional ability is deemed “good”. On the “basic activities of daily living” scale this is 88 and on the “intermediate activities of daily living” scale this is 78. In a systematic review of disability rating scales for people with Parkinson’s [Citation53], this measure was recommended for both clinical and research use. It has previously shown good internal consistency [Citation52] and in the current study Cronbach’s alpha was 0.72 for basic ADLs and 0.86 for intermediate ADLs. This was used to situate the sample in terms of severity of physical symptoms.
Self-Compassion Scale
The Self-Compassion Scale (SCS) [Citation54] is a 26-item validated measure of self-compassion, consisting of six subscales: self-kindness, self-judgment, common humanity, isolation, mindfulness, and over-identification. It has been used previously with people with Parkinson’s [Citation38]. The total self-compassion score is the mean of the six subscale means and ranges from 1 to 5, with a higher score indicating greater self-compassion. Neff [Citation54] reports that the scale’s internal consistency is high (Cronbach’s alpha = 0.92), as is the test–retest reliability (r= 0.93). In the current study, Cronbach’s alpha was 0.93.
Stigma Scale for Chronic Illness
The Stigma Scale for Chronic Illness (SSCI) [Citation19] is a 24-item multiple-choice questionnaire, designed and validated for use with people with Parkinson’s (as well as other chronic illnesses). The first 13 items measure felt stigma (possible score range 13–65) and the remaining 11 items measure enacted stigma (possible score range 11–55). The total score measures overall stigma. A higher total score indicates more stigma. Cronbach’s alpha in the current study was 0.95 for the total score, 0.93 for the felt stigma scale, and 0.94 for the enacted stigma scale.
Depression, Anxiety, and Stress Scale
The Depression, Anxiety, and Stress Scale – 21-item version (DASS-21) [Citation55] is a validated questionnaire designed for use with both clinical and non-clinical populations as a dimensional, rather than diagnostic, tool. The scale is comprised of 21 items, falling into three 7-item subscales: depression, anxiety, and stress, each with scores ranging from 0 to 21. A total score is generated for each subscale, with a higher score indicating a higher level of depression, anxiety, or stress. Cronbach’s alphas have previously been found to be 0.94 for depression, 0.87 for anxiety, and 0.91 for stress [Citation56] and in the current study were 0.96 for depression, 0.73 for anxiety, and 0.92 for stress. Although this scale has been used previously with people with Parkinson’s (e.g., [Citation57,Citation58]), further inspection of the anxiety scale revealed that the item “I experienced trembling (e.g., in the hands)” was reducing the internal consistency of the scale. When this item was removed, Cronbach’s alpha increased to 0.80, indicating good internal consistency. Therefore, this item was removed for the subsequent analyses and a six-item anxiety scale was used (score range 0–18).
Data analysis
The data were tabulated in the software IBM SPSS Statistics (Version 25.0, Armonk, NY). One extreme data point in the “enacted stigma” variable was winsorised (replaced with the next highest score), to reduce the likelihood of biasing the results [Citation59]. The “enacted stigma”, “depression”, and “stress” data were all skewed towards lower scores. For the regressions, all relationships met the assumptions of linearity, homoscedasticity of residuals and normality of error distributions. Cronbach’s alphas for each of the questionnaire measures were ascertained, and Spearman’s rho correlation coefficients were calculated due to the non-normal distribution of some test scores.
A series of mediation analyses were run using Hayes’ Process Tool [Citation60], which employs a bias-corrected bootstrap model, with 5000 bootstrap samples. In the first model, self-compassion was entered as the predictor variable, felt stigma as the mediator variable, and depression as the outcome variable. This was repeated with anxiety and stress as outcomes. Finally, a series of moderation analyses were conducted using Hayes’ Process Tool [Citation60], with enacted stigma as the predictor, self-compassion as the moderator with depression, anxiety, and stress as the outcomes in turn.
Results
Demographic and clinical characteristics
Details of demographics are given in . Of the 130 participants whose data were included in the study, 74 (57%) identified as female. The ages of participants ranged from 36 to 89 years, with a mean of 65 years. Most participants (95%) identified their ethnic group or background as “white British” and 89% reported living in England. The majority of participants (69%) reported being retired from work. Participants had held their diagnosis of Parkinson’s for between six months and 30 years, with a median of four years. In terms of comparisons with other studies, the mean age of the current participants was slightly younger (average age of onset is estimated to be around 70 [Citation61]) and participants had on average lived fewer years with the disease (cf., [Citation62], where average number of years with a diagnosis was 9.6).
Table 1. Demographic and clinical characteristics of sample.
The majority of participants (92%) were taking prescribed oral medication to treat their Parkinson’s symptoms. There was a wide range of functional ability among the sample as measured by FSQ scores. On the “basic activities of daily living” scale, 63% of participants scored above the “warning zone” cut-off score of 88, indicating a “good” level of basic functional ability. On the “intermediate activities of daily living” scale, 48% of participants scored above the “warning zone” cut-off score of 78.
Descriptive statistics for standardised measures
shows the means, standard deviations and ranges for the sample on each of the standardised measures. Of note, the mean total stigma score on the SSCI among the sample was 48.8: somewhat higher than a chronic illness sample mean (11% of whom had Parkinson’s) of 42.7 [Citation19]. Mean scores on the DASS-21 variables fell in the “mild” range for depression and stress, and the “moderate” range for anxiety. Forty percent, 55%, and 33% had scores in the moderate–very severe range for depression, anxiety (seven-item), and stress, respectively.
Table 2. Descriptive statistics for standardised measures.
Correlational analyses
A correlation matrix is displayed in . Moderate to strong relationships were observed between self-compassion and depression, anxiety, and stress. As expected, higher self-compassion was associated with lower levels of depression, anxiety, and stress. A weak correlation was observed between self-compassion and enacted stigma, while a moderate correlation was observed between self-compassion and felt stigma. Again, these relationships were in the expected directions, with higher self-compassion associated with lower levels of stigma. As anticipated, there were moderate to strong correlations between felt stigma and depression, anxiety, and stress with higher levels of felt stigma associated with higher levels of depression, anxiety, and stress. Moderate relationships in the same direction were also observed between enacted stigma and the DASS-21 variables.
Table 3. Spearman’s rho correlations between variables.
Mediation analysis to test whether felt-stigma mediated the relationship between self-compassion and distress
Since the demographic and clinical variables (excluding the FSQ) correlated only weakly with the questionnaire measures (<0.40), they were not included as covariates in the models. Given the moderate associations between FSQ scores and the stigma scales, both FSQ variables were initially entered as covariates. However, they did not have any great impact upon the findings so are not included in the models presented for clarity of presentation. The main findings of the mediation analyses are displayed in .
Figure 1. Mediation models. (a) Mediation diagram for depression. (b) Mediation diagram for anxiety. (c) Mediation diagram for stress.
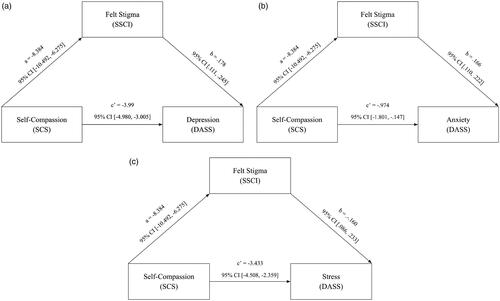
The indirect effect (ab= −1.494, SE = 0.384, 95% CI [–2.302, –0.794]) indicated a significant effect of self-compassion on depression through felt stigma, with completely standardised indirect effect of –0.200. The direct effect remained significant with higher self-compassion predicting lower depression scores (c′= −3.99, SE = 0.499, 95% CI [–4.980, −3.005]).
The indirect effect (ab=–1.391, SE = 0.321, 95% CI [–2.067, –0.826]) indicated a significant effect of self-compassion on anxiety through felt stigma, with a completely standardised effect size of –0.281. A direct effect of self-compassion on anxiety also remained, with higher self-compassion predicting lower anxiety scores (c′=–0.974, SE = 0.418, 95% CI [–1.801, –0.147]).
Finally, the indirect effect (ab= −1.338, SE = 0.389, 95% CI [–2.172, –0.636]) indicated a significant effect of self-compassion on stress through felt stigma with a completely standardised effect size of −1.86. A direct effect of self-compassion on stress also remained, with higher self-compassion predicting lower stress scores (c′= −3.433, SE = 0.543, 95% CI −4.508, −2.359]).
Moderation analyses to test whether self-compassion moderated the relationship between enacted stigma and distress
Self-compassion did not moderate the relationship between enacted stigma and depression. The interaction term was not significant (0.006, SE = 0.053, 95% CI [–0.098, 0.111]), with R2 change <0.001 (p = 0.905). Similarly, self-compassion did not moderate the relationship between enacted stigma and anxiety. The interaction term was not significant (–0.007, SE = 0.042, 95% CI [–0.090, 0.077]), with R2 change <0.001 (p = 0.875). Finally, self-compassion did not moderate the relationship between enacted stigma and stress. The interaction term was not significant (0.054, SE = 0.055, 95% CI [–0.054, 0.162]), with R2 change of 0.004 (p = 0.325).
Discussion
This study tested relationships between stigma, self-compassion, and psychological distress (depression, anxiety, and stress). Significant relationships were observed between self-compassion and the psychological distress variables, with higher self-compassion associated with lower levels of depression, anxiety, and stress. This fits with previous findings about such relationships in the wider population [Citation37] as well as in Parkinson’s specifically [Citation38]. Also, as expected and in keeping with previous research [Citation29–31], significant correlations were found between felt stigma and depression, anxiety, and stress, with higher levels of felt stigma associated with higher levels of distress. Similarly, moderate relationships in the same direction were found between enacted stigma and depression, anxiety, and stress. As observed in other populations [Citation42–44], self-compassion was observed to significantly correlate with felt-stigma with higher self-compassion associated with less felt-stigma.
As predicted, felt stigma mediated the relationship between self-compassion and psychological distress. Part of the relationship between self-compassion and psychological distress among people with Parkinson’s appears to occur via the extent of the internalisation of stigma; people who are higher in self-compassion experience less felt stigma, and therefore, experience lower levels of distress. If individuals who are higher in self-compassion are less prone to feelings of shame [Citation34] then it follows that they may be less likely to attribute negative Parkinson’s-related stereotypes to themselves, or internalise potentially shaming identities. Lesser experiences of felt stigma are then associated with lower levels of psychological distress, as supported by previous research with people with Parkinson’s [Citation29].
However, contrary to expectations, self-compassion did not moderate the relationship between enacted stigma and distress. The relationship between stigma and distress was consistent, regardless of the level of self-compassion. The null result may be partly due to issues of power. The sample size of 130 had only approximately 18% power to find the 0.4% variance change identified in the stress model. However, the variance change in the depression and anxiety models were less than 0.1%, so may not be meaningful, even if a study could be adequately powered to find them. The use of self-report here may also have limited the study. It is possible people with Parkinson’s who are higher in self-compassion may report less enacted stigma (even when they are exposed to it) because they cognitively appraise experiences of enacted stigma less negatively [Citation48], and thus the relationship between stigma and stress appears to be stronger than it actually is for this group. However, the null findings may also point to the importance of the impact of enacted stigma on distress, regardless of levels of self-compassion, in that higher levels of enacted stigma led to higher distress for all groups. Nonetheless, given the strong relationship between self-compassion and distress, it should be noted that those with greater self-compassion tend to have lower levels of distress overall.
A key limitation of this study was the demographics of the sample. A large majority of participants described their ethnic background as white British and therefore the findings may not extend to other groups. Additionally, although Parkinson’s is more common among men [Citation63], in this study, the majority of participants (57%) identified as female. However, the sample was also relatively young, with a mean age of 65 years, at which sex ratios for incidence are more equal [Citation64]. The relatively young age may also account for the fact that participants had lived with Parkinson’s for fewer years than reported in other studies [Citation62]. The relatively young average age of the sample may also account for the level of functional ability among the sample and the fact that no participants reported living in sheltered housing, residential homes, or care homes, despite this being fairly common for people with Parkinson’s in the UK [Citation65]. The younger age of the sample may be attributable to the online advertising of the survey. Although the option was given to receive a paper copy of the survey in the post, younger people are more likely than older people to participate in research advertised on the internet and social media [Citation66]; therefore, the recruitment strategy was likely to be biased and even completing the survey by post may not have been possible for those with more severe tremor or other motor problems. In addition, participants had to have sufficient cognitive ability to complete the survey. Thus, in summary, the findings cannot be generalised to older people, to those with more severe disease and to those with a greater level of cognitive impairment. Participants also self-identified as having Parkinson’s – their diagnosis was not confirmed. We also did not collect data on current treatments for mood such as psychological therapy or medication so cannot comment on their influences on the relationships presented.
A further possible limitation of this study was the use of the DASS-21 as an outcome measure for anxiety. Johnson et al. [Citation67] examined the factor structure of the DASS-21 for people with Parkinson’s and found that, while the depression and stress subscales fit the factor structures well, the anxiety subscale loaded poorly onto the factor structure and had problems with internal consistency. Similarly, in the current study, an item was removed in order to bring internal consistency to an acceptable level, and even with the new six-item subscale Cronbach’s alpha was notably lower than the other two subscales. Johnson et al. [Citation67] suggest that this problem may be related to the emphasis within the subscale upon physiological symptoms of anxiety, which may have significant overlap with other difficulties experienced by people with Parkinson’s. Consequently, the findings of this study relating to anxiety should be interpreted more cautiously.
Mediation analysis with correlational or observational data has limitations in how the findings can be interpreted, since cause and effect cannot be inferred [Citation60]. It may be that some of the relationships identified in this study are bi-directional, or that there are additional factors which mediate or moderate the relationships found. There may also be underlying factors contributing to the relationships which were not controlled. For example, people with lower levels of education have been found to demonstrate less self-compassion [Citation68].
The importance of self-compassion in the models suggests that interventions aimed at increasing self-compassion may be helpful for people with Parkinson’s. There is a growing evidence base for the use of compassion-focussed therapy, which has a strong focus on reducing experiences of shame and developing feelings of compassion towards the self and others [Citation35], for reducing distress among people with neurological illness and injury [Citation38–40]. It may be hypothesised, based on the findings of this study, that this approach might also be helpful for people with Parkinson’s to reduce overall levels of distress.
Although approaches aimed at increasing self-compassion at the individual level may be helpful for reducing distress, it is important to also consider how the wider social and relational context contributes to distress for people with Parkinson’s [Citation32]. The findings here suggest that enacted stigma increases distress, regardless of levels of self-compassion and highlights the importance of interventions to reduce enacted stigma. Enacted stigma is clearly a societal problem, being defined as the attitudes and behaviour of others in society on the basis of some socially discredited attribute [Citation16]. Heijnders and Van Der Meij [Citation69] reviewed a number of interventions for reducing health-related stigma. They suggest that interventions should take place at multiple levels – interpersonally (in the person with the stigmatised attribute’s immediate relational environment), organisationally, in the community, and at government and structural levels. Based on Heijnders and Van Der Meij’s [Citation69] findings, types of stigma-reduction interventions for people with Parkinson’s might include providing education and training, increasing the visibility of people with Parkinson’s in communities, advocacy programmes, and lobbying for the rights of people with Parkinson’s.
Given the expanding evidence-base for compassion-focussed psychological interventions and the importance of self-compassion for wellbeing more generally, developing and assessing the effectiveness of compassion-focused interventions tailored for people with Parkinson’s could be worthy of future research. A number of psychological therapies either explicitly (e.g., compassion-focussed therapy [Citation34]) or more implicitly (acceptance and commitment therapy [Citation70]) aim to increase levels of compassion towards the self. Given that people with Parkinson’s disease may develop cognitive impairment and/or communication problems, it would be important to consider the need to individually tailor therapeutic interventions [Citation71]. This may include the use of strategies which are commonly employed to support the delivery of talking therapy in the context of traumatic brain injury or dementia where compassion focused interventions have been used successfully [Citation39,Citation40]. Strategies could include providing both oral and written communication, incorporating memory aids such as audio recording devices, providing shorter sessions, and checking understanding and summarising ideas throughout the session. If the person with Parkinson’s disease agreed it could also help to include a family member or close friend in the session to help them implement the compassion-focused strategies outside of the session.
Further research might also build upon the current study by considering further the interaction of felt and enacted stigma to investigate how enacted stigma becomes internalised. Additionally, there are likely to be other factors apart from stigma which mediate or moderate the relationship between self-compassion and psychological distress for people with Parkinson’s (e.g., coping). Finally, research could investigate predictors of self-compassion (e.g., early attachment experiences) to predict those who are likely to be vulnerable to low self-compassion and hence high distress. A better understanding of all these relationships might be useful for guiding interventions to support people with Parkinson’s who are experiencing psychological distress.
Disclosure statement
The authors report no conflicts of interest.
References
- Pringsheim T, Jette N, Frolkis A, et al. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2014;29(13):1583–1590.
- Tysnes OB, Storstein A. Epidemiology of Parkinson's disease. J Neural Transm. 2017;124(8):901–905.
- Fahn S. Classification of movement disorders. Mov Disord. 2011;26(6):947–957.
- Moustafa AA, Chakravarthy S, Phillips JR, et al. Motor symptoms in Parkinson's disease: a unified framework. Neurosci Biobehav Rev. 2016;68:727–740.
- Rana AQ, Ahmed US, Chaudry ZM, et al. Parkinson's disease: a review of non-motor symptoms. Expert Rev Neurother. 2015;15(5):549–562.
- Stacy M. Nonmotor symptoms in Parkinson’s disease. Int J Neurosci. 2011;121(Suppl. 2):9–17.
- Soh SE, Morris ME, McGinley JL. Determinants of health-related quality of life in Parkinson's disease: a systematic review. Parkinsonism Relat Disord. 2011;17(1):1–9.
- Reijnders JSAM, Ehrt U, Weber WEJ, et al. A systematic review of prevalence studies of depression in Parkinson's disease. Mov Disord. 2008;23(2):183–189.
- Dissanayaka NNW, Sellbach A, Matheson S, et al. Anxiety disorders in Parkinson's disease: prevalence and risk factors. Mov Disord. 2010;25(7):838–845.
- Aarsland D, Kramberger MG. Neuropsychiatric symptoms in Parkinson's disease. J Parkinsons Dis. 2015;5(3):659–667.
- Remy P, Doder M, Lees A, et al. Depression in Parkinson's disease: loss of dopamine and noradrenaline innervation in the limbic system. Brain. 2005;128(Pt 6):1314–1322.
- Kano O, Ikeda K, Cridebring D, et al. Neurobiology of depression and anxiety in Parkinson’s disease. Parkinsons Dis. 2011;2011:143547.
- Garlovsky JK, Overton PG, Simpson J. Psychological predictors of anxiety and depression in Parkinson’s disease: a systematic review. J Clin Psychol. 2016;72(10):979–998.
- Goffman E. Stigma: notes on a spoiled identity. New York: Simon & Schuster; 1963.
- Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385.
- Scambler G. Epilepsy: the experience of illness series. London: Routledge; 1989.
- Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25(8):875–884.
- Watson AC, Corrigan P, Larson JE, et al. Self-stigma in people with mental illness. Schizophr Bull. 2007;33(6):1312–1318.
- Rao D, Choi SW, Victorson D, et al. Measuring stigma across neurological conditions: the development of the Stigma Scale for Chronic Illness (SSCI). Qual Life Res. 2009;18(5):585–595.
- Campbell C, Deacon H. Unravelling the contexts of stigma: from internalisation to resistance to change. J Community Appl Soc Psychol. 2006;16(6):411–417.
- Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs. 2000;32(1):243–248.
- Hermanns M. The invisible and visible stigmatization of Parkinson's disease. J Am Assoc Nurse Pract. 2013;25(10):563–566.
- Bramley N, Eatough V. The experience of living with Parkinson’s disease: an interpretative phenomenological analysis case study. Psychol Health. 2005;20(2):223–235.
- Caap-Ahlgren M, Lannerheim L, Dehlin O. Older Swedish women's experiences of living with symptoms related to Parkinson's disease. J Adv Nurs. 2002;39(1):87–95.
- Nijhof G. Parkinson’s disease as a problem of shame in public appearance. Sociol Health Illn. 1995;17(2):193–205.
- Tickle-Degnen L, Zebrowitz LA, Ma H. I. Culture, gender and health care stigma: practitioners' response to facial masking experienced by people with Parkinson's disease. Soc Sci Med. 2011;73(1):95–102.
- Hemmesch AR. The detrimental effects of atypical nonverbal behavior on older adults' first impressions of individuals with Parkinson's disease. Psychol Aging. 2014;29(3):521–527.
- Moore S, Knowles S. Beliefs and knowledge about Parkinson’s disease. E-J Appl Psychol. 2006;2(1):15–21.
- Ma H-I, Saint-Hilaire M, Thomas CA, et al. Stigma as a key determinant of health-related quality of life in Parkinson’s disease. Qual Life Res. 2016;25(12):3037–3045.
- Simpson J, Lekwuwa G, Crawford T. Predictors of quality of life in people with Parkinson's disease: evidence for both domain specific and general relationships. Disabil Rehabil. 2014;36(23):1964–1970.
- Schrag A, Jahanshahi M, Quinn NP. What contributes to depression in Parkinson’s disease? Psychol Med. 2001;31(1):65–73.
- Simpson J, McMillan H, Reeve D. Reformulating psychological difficulties in people with Parkinson’s disease: the potential of a social relational approach to disablism. Parkinsons Dis. 2013;2013:608562.
- Neff, K, Dahm K. Self-compassion: what it is, what it does, and how it relates to mindfulness. In: Ostafin B, Robinson M, Meier B, editors. Handbook of mindfulness and self-regulation. New York: Springer; 2015. p. 121–137.
- Gilbert P. Introducing compassion-focused therapy. Adv Psychiatr Treat. 2009;15(3):199–208.
- Gilbert P. Compassion focussed therapy: distinctive features. London: Routledge; 2010.
- Zessin U, Dickhäuser O, Garbade S. The relationship between self-compassion and well-being: a meta-analysis. Appl Psychol Health Well Being. 2015;7(3):340–364.
- MacBeth A, Gumley A. Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clin Psychol Rev. 2012;32(6):545–552.
- Stutts LA, Speight KL, Yoo S, et al. Positive psychological predictors of psychological health in individuals with Parkinson's disease. J Clin Psychol Med Sett. 2020;27(1):182–189.
- Ashworth F, Gracey F, Gilbert P. Compassion focused therapy after traumatic brain injury: theoretical foundations and a case illustration. Brain Impair. 2011;12(2):128–139.
- Collins RN, Gilligan LJ, Poz R. The evaluation of a compassion-focused therapy group for couples experiencing a dementia diagnosis. Clin Gerontol. 2018;41(5):474–486.
- Nery-Hurwit M, Yun J, Ebbeck V. Examining the roles of self-compassion and resilience on health-related quality of life for individuals with multiple sclerosis. Disabil Health J. 2018;11(2):256–261.
- Hilbert A, Braehler E, Haeuser W, et al. Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity. 2014;22(1):79–85.
- Heath PJ, Brenner RE, Vogel DL, et al. Masculinity and barriers to seeking counseling: the buffering role of self-compassion. J Couns Psychol. 2017;64(1):94–103.
- Wasylkiw L, Clairo J. Help seeking in men: when masculinity and self-compassion collide help seeking in men: when masculinity and self-compassion collide. Psychol Men Masculin. 2016;19(2):234–242.
- Touriño R, Acosta FJ, Giráldez A, et al. Suicidal risk, hopelessness and depression in patients with schizophrenia and internalized stigma. Actas Esp Psiquiatr. 2018;46:33–41.
- Leary MR, Tate EB, Adams CE, et al. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904.
- Williams SL, Fekete EM, Skinta MD. Self-compassion in PLWH: less internalized shame and negative psychosocial outcomes. Behav Med. 2021;47(1):60–68.
- Wong CCY, Knee CR, Neighbors C, et al. Hacking stigma by loving yourself: a mediated-moderation model of self-compassion and stigma. Mindfulness. 2019;10(3):415–433.
- Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity. 2011;10(3):352–362.
- Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–576.
- Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18(3):233–239.
- Jette AM, Davies AR, Cleary PD, et al. The Functional Status Questionnaire: reliability and validity when used in primary care. J Gen Intern Med. 1986;1(3):143–149.
- Shulman LM, Armstrong M, Ellis T, et al. Disability rating scales in Parkinson's disease: critique and recommendations. Mov Disord. 2016;31(10):1455–1465.
- Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–250.
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Sydney: Psychology Foundation; 1995.
- Antony MM, Cox BJ, Enns MW, et al. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176–181.
- Birtwell K, Dubrow-Marshall L, Dubrow-Marshall R, et al. A mixed methods evaluation of a mindfulness-based stress reduction course for people with Parkinson's disease. Complement Ther Clin Pract. 2017;29:220–228.
- Troeung L, Egan SJ, Gasson N. A waitlist-controlled trial of group cognitive behavioural therapy for depression and anxiety in Parkinson's disease. BMC Psychiatry. 2014;14:19.
- Field A. Discovering statistics using IBM SPSS statistics. 5th ed. London: Sage; 2018.
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. 2nd ed. New York: The Guilford Press; 2018.
- Van Den Eeden SK, Tanner CM, Bernstein AL, et al. Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am J Epidemiol. 2003;157(11):1015–1022.
- Bäckström D, Granåsen G, Domellöf ME, et al. Early predictors of mortality in parkinsonism and Parkinson disease a population-based study. Neurology. 2018;91(22):E2045–E2056.
- Wooten GF, Currie LJ, Bovbjerg VE, et al. Are men at greater risk for Parkinson's disease than women? J Neurol Neurosurg Psychiatry. 2004;75(4):637–639.
- Moisan F, Kab S, Mohamed F, et al. Parkinson disease male-to-female ratios increase with age: French Nationwide Study and meta-analysis. J Neurol Neurosurg Psychiatry. 2016;87(9):952–957.
- Porter B, Henry SR, Gray WK, et al. Care requirements of a prevalent population of people with idiopathic Parkinson's disease. Age Ageing. 2010;39(1):57–61.
- Topolovec-Vranic J, Natarajan K. The use of social media in recruitment for medical research studies: a scoping review. J Med Internet Res. 2016;18(11):e286.
- Johnson AR, Lawrence BJ, Corti EJ, et al. Suitability of the Depression, Anxiety, and Stress Scale in Parkinson's disease. J Parkinsons Dis. 2016;6(3):609–616.
- López A, Sanderman R, Ranchor AV, et al. Compassion for others and self-compassion: levels, correlates, and relationship with psychological well-being. Mindfulness. 2018;9(1):325–331.
- Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–363.
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy. Washington: American Psychological Association; 2009.
- Zarotti N, Eccles FJR, Foley JA, et al. Psychological interventions for people with Parkinson's disease in the early 2020s: where do we stand? Psychol Psychother. 2021;94(3):760–797.
