 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
Children with cerebral palsy (CP) or spina bifida (SB) often have executive dysfunction affecting activity performance. With the Cognitive Orientation to daily Occupational Performance (CO-OP) Approach, children find their own way to perform activities, using problem-solving strategies and meta-cognitive thinking. The present study aimed to investigate the effectiveness of the CO-OP Approach in children with CP or SB, compared with conventional rehabilitation, in achieving self-identified activity goals, and to explore any generalization and transfer effects.
Method
Randomized controlled trial, CO-OP versus treatment as usual, 38 children (7–16 years) participated. Each child identified four goals (to study generalization and transfer, one remained untrained). Primary outcomes: Canadian Occupational Performance Measure (COPM) and Performance Quality Rating Scale (PQRS). Secondary outcomes assessed executive functions and self-rated everyday-life competence.
Results
Self-rated goal attainment (COPM) was significantly greater for both trained and untrained goals in the CO-OP group compared with the control group. The rating of observed performance (PQRS) was significantly higher for trained goals in the CO-OP group. The CO-OP group experienced fewer problems in everyday life after treatment. Executive functions did not differ significantly between groups.
Conclusion
CO-OP is more effective than ordinary treatment in achieving both trained and untrained goals.
CO-OP enables children with CP (MACS levels I–III) or SB without intellectual disabilities to reach self-identified goals.
CO-OP shows transfer effects to new activities and situations, which may enhance children’s self-efficacy.
CO-OP is an important complement to conventional rehabilitation services for children with CP and SB.
IMPLICATIONS FOR REHABILITATION
Introduction
Participating in and performing meaningful activities is important for the health, development and well-being of all children [Citation1,Citation2]. Children with different types of neuro-developmental disorders may, in addition to various physical impairments, have executive dysfunctions causing difficulties organizing activities, planning and initiating accordingly, keeping focused and finishing a task [Citation3–6]. This often leads to difficulties performing daily activities at home and school, and it also affects learning abilities and social functioning, thus placing those children at risk of participation restrictions. Children with neuro-developmental disorders such as cerebral palsy (CP) and spina bifida (SB) have been shown to exhibit cognitive as well as executive difficulties [Citation5,Citation7–13]. Consequently, rehabilitation methods addressing skills development and participation in children with these diagnoses must encompass all phases of the “process of doing”: both physical, cognitive and executive aspects [Citation14,Citation15].
The Cognitive Orientation to daily Occupational Performance (CO-OP) ApproachTM is a multifaceted client-centred and performance-based intervention approach [Citation16,Citation17]. It is a task-specific and goal-focused approach which has three aims: (i) enabling the person to increase his/her skills, (ii) teaching the use of self-generated cognitive strategies and (iii) promoting generalization and transfer to new situations and activities [Citation16,Citation17]. CO-OP has shown good evidence of treatment effect in persons of different ages with different diagnoses, including adults with stroke [Citation18] and children with developmental cordination disorder (DCD) [Citation19,Citation20], and evidence is currently emerging of effect in children with autism [Citation21,Citation22] and CP [Citation23–27]. In CO-OP, the person learns skills by finding his or her own way to solve problems through an interactive process involving collaboration with the therapist, who asks reflective questions. This approach enables clients to cognitively process each step of the performance, to understand what happens during the performance of the task and to identify their own strategies to improve performance – i.e., to develop meta-cognitive thinking [Citation14], which has been suggested to be the key to its generalization and transfer effect [Citation28]. CO-OP has been shown to be feasible for adolescents and young adults with SB and CP in a Swedish context [Citation29]. Hence it is important to investigate the effects of CO-OP in children with these neuro-developmental disorders.
This study aims to investigate the effectiveness of the CO-OP Approach in children (including adolescents) with CP or SB, compared with conventional rehabilitation, when it comes to achieving self-identified activity goals, and to explore any generalization and transfer effects.
Methods
This is the first of two reports from a multi-centre, randomized, controlled, cross-over clinical intervention trial. This report presents results from baseline (T1) to follow-up assessment (T2) in a CO-OP treatment group and a control group. The trial was of a pragmatic nature in the sense that the effects of the intervention were determined in real-life conditions, to produce results that could be applied directly in clinical settings [Citation30]. The study was approved by the Regional Ethical Review Board of Gothenburg, Sweden (Ref. No.: 323-16), and the protocol was registered with FoU VGR Researchweb (study record: 214861) and with ISRCTN (study record: 12888658).
Participants
Inclusion criteria were: children (aged 8–16 years) with CP at Manual Ability Classification System (MACS) level I–III [Citation31] and Gross Motor Function Classification System (GMFCS) level I–IV [Citation32] or with SB, with or without hydrocephalus and all levels of ambulation according to the Hoffer scale [Citation33], resident in four geographical and administrative regions in Sweden including both rural and urban areas. Participants had to have problems (self-perceived or experienced by parents) performing or organizing activities owing to perceived difficulties with initiative, planning, problem-solving and decision-making. They also had to follow the mainstream curriculum at compulsory school, be able to formulate their own goals and be able to communicate verbally in Swedish. Exclusion criteria were: communication using augmentative and alternative communication (AAC) or an intellectual disability diagnosed at enrolment.
Recruitment end eligibility
The participants were invited in slightly different manners depending on the organization of the rehabilitation centres and the demographics of the different regions. All children from selected municipalities in the four regions – both metropolitan and rural – who met the inclusion criteria were identified in medical records and invited to participate. In one region, children were also invited by means of e-mails sent to parents who were members of the national association for children and young people with physical disabilities (RBU). Recruitment started in the first region on 1 June 2017 and ended in the fourth region on 30 August 2019. For validation purposes, the number of children invited was checked against the number of children registered as having the diagnoses concerned in the national follow-up programmes for cerebral palsy (CPUP) and myelomeningocele (MMCUP). This showed that most children meeting the inclusion criteria in the selected municipalities had probably been identified.
Parents and children aged at least 15 were asked for written consent while children below 15 were informed and asked for assent.
Procedure and allocation
All participants with consent were invited to undergo a baseline assessment (T1) consisting of a structured interview with the children using the Child Occupational Self-Assessment – Swedish version (COSA-S) [Citation34], goal-setting using the Canadian Occupational Performance Measure (COPM) [Citation35] and neuro-psychological tests using five sub-tests from the Delis–Kaplan Executive Function System (D-KEFS) [Citation36]. In addition, the Behaviour Rating Inventory of Executive Function (BRIEF) [Citation37] was distributed for self-rating at home along with a prepaid reply envelope.
At T1, each child him- or herself set four goals using the COPM. One of those goals (randomly selected) remained untrained during the treatment period, to enable the study of generalization and transfer effects. The untrained goal was selected using the following procedure: First, each child freely chose one of the four goals. This was to make sure that the children would remain motivated for the training. Second, the assessor chose one of the three remaining goals, favouring concrete ones. Finally, the child selected the goal that was to remain untrained by picking one of two sealed envelopes.
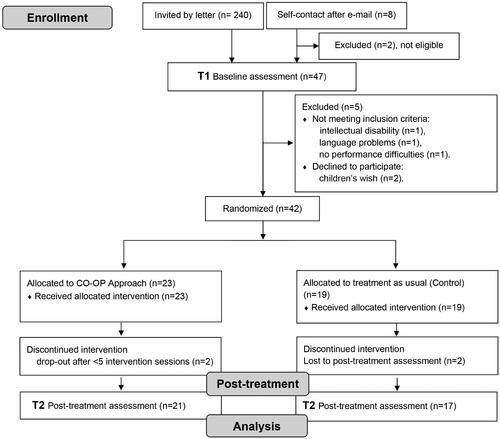
After T1, participants () were randomly allocated either to an 11-session intervention with CO-OP in addition to treatment as usual (CO-OP group) or to treatment as usual only (control group). Randomization to groups was performed in clusters. Owing to the low prevalence of SB in Sweden, all children with SB were randomized in a single cluster, regardless of their region. The children with CP were randomized in four clusters, one for each region. Randomization numbers were generated using a function for random-sample selection in Microsoft Excel. Note that information about group allocation was not revealed either to the children or to the assessors and therapist until after T1, meaning that they were all blinded to group allocation when the children were assessed and set their goals.
Figure 1. CONSORT 2010 flow diagram. Flow chart showing initially contacted patients, excluded before randomisations, enrolled participants, number of participants in each intervention group, and number of evaluated participants after treatment.
Post-treatment assessments were conducted immediately after the last CO-OP session. COPM and COSA interviews were conducted by the same assessor as at T1, who were not blinded at this point. For the neuro-psychological testing, most assessments at T2 were made by the same psychologist as at T1, although another psychologist carried out one assessment at T2.
Four children were lost to post-treatment assessment. Two of them were in the CO-OP group (both diagnosed with CP); the reason stated was in both cases that the child attained the first goal, was very satisfied with this and chose to terminate participation. The other two were in the control group (one with CP, one with SB) and the reasons for discontinuation differed: in one case, the family claimed a lack of time; in the other, the child did not show up at T2, without an explanation.
No adverse events were reported from any of the groups.
Interventions
CO-OP approachTM
In line with its established format, CO-OP was carried out over eleven sessions (one preparatory session followed by ten treatment sessions), approximately once a week (45–60 min per session) [Citation16] and mainly in each child’s usual environment. In the initial preparatory session, the therapist introduced the child to the global strategy of Goal–Plan–Do–Check, which he or she then used when working to achieve the goals. The therapist guided the child in discovering his or her own plan for performance, and the child implemented the plan and checked whether it worked or needed to be modified. In line with the CO-OP format [Citation16], work was first carried out on a single goal, whereupon the second and third goals were progressively added. All occupational therapists (OTs) who conducted CO-OP treatment were certified CO-OP therapists, and none was the respective child’s treating OT at his or her rehabilitation centre. During the intervention period, the CO-OP therapists met occasionally with the first or last author to discuss fidelity issues concerning the CO-OP format and key features.
The treating OTs at the respective rehabilitation centres responsible for the children in the CO-OP group were informed about all four goals and instructed not to work on any of them, to ensure that such training would take place only with the CO-OP certified OT.
Treatment as usual
Up to the age of 18, children with disabilities in Sweden are entitled to register with the rehabilitation centre of their geographical region. If they register, they are served by a multi-disciplinary team aiming to provide information, guidance and treatment to meet the children’s needs with regard to medical, motor, cognitive and social development as well as everyday-life issues. Interventions are given both in the clinic but also in the child’s natural environment. “Treatment as usual” in the present study represents the current usual practice, meaning that the child and his or her family have an ongoing contact with the team, which uses a family-centred approach based on the family’s wishes and current needs [Citation38,Citation39]. The treating OTs at the respective rehabilitation centres responsible for the children in the control group were informed that the children had formulated four goals using COPM. However, they received information about the exact wording only for the untrained goal; they were instructed not to work on that goal during the study period. By contrast, the other three goals were not shared with the treating OTs and hence they did not receive any directions about how to address those goals. This was intended to ensure that they would choose the methods that they typically use.
Primary outcome measures
All primary outcome measures were administered at both T1 and T2.
COPM is an interview-based, client-centred outcome measure intended to capture a person’s self-perception of his or her performance and satisfaction with the performance of the selected goals as well as to capture change over time [Citation35]. It uses a 10-point VAS scale and has good psychometric properties in terms of both validity and reliability for children older than 5 years with neuro-developmental disorders [Citation35,Citation40]. A change of two or more points is considered clinically relevant [Citation35].
The Performance Quality Rating Scale (PQRS) is an observer-rated scale, specially designed for the CO-OP Approach to objectively assess and evaluate changes in the quality of a person’s performance of the self-selected goals. PQRS has good internal responsiveness and test-retest reliability for use in children with disabilities [Citation41]. In the present study, the children’s performance of each goal was documented by video recording, either by filming the live performance if possible or through a film in which the child and/or parent described how the child was doing. A certified CO-OP therapist blinded for group allocation and chronological order of recordings rated the video recordings on the 10-point PQRS scale, where higher scores indicate more efficient performance; a change of two or more points is considered clinically relevant according to previous research [Citation25] and following the COPM scale [Citation35].
Secondary outcome measures
All secondary outcome measures were administered at both T1 and T2, except that BRIEF was used only at T1.
COSA [Citation34] was used to study transfer effects to participation in other areas of everyday life. It captures the child’s own perception of competence in different activities and his or her evaluation of those activities on two 4-point Likert scales (competence scale and value scale). COSA consists of 25 items presented as statements about everyday occupations at school, at home and with friends. In this study, the Swedish version (COSA-S) was used for two purposes: (i) to help the children identify highly valued everyday areas where they perceived performance problems, so as to facilitate appropriate goal setting, and (ii) as an outcome measure (the competence scale only) to evaluate change in the children’s perception of competence in different everyday areas. COSA has been found to be valid for use in children with disabilities [Citation34].
D-KEFS [Citation36] was used to assess the children’s executive abilities and investigate whether the interventions had any effect on those abilities. The following D-KEFS sub-tests were used: (i) the Trail Making Test: TMT 2, Number Sequencing (assessing visual scanning and motor speed), and TMT 4, Number and Letter Sequencing (assessing cognitive flexibility and attentional control), (ii) Verbal Fluency conditions, Letter Fluency and Category Fluency (assessing attentional control, goal setting and cognitive flexibility as well as fluent production of verbal material), and (iii) the Tower Test (assessing goal setting, planning, rule learning and inhibition).
BRIEF was used for the children’s self-assessment and their parents’ assessment of the behavioural aspects of executive function in everyday life. It consists of eight sub-scales which yield an index of Behavioral Regulation (BRI) and an index of Meta-cognition (MI) as well as summary score called a Global Executive Composite (GEC). BRIEF was used to establish baseline descriptions of the participants.
Data analysis
Data were analysed using SPSS 26. Non-parametric statistical methods were used because of the ordinal nature of the data in COPM, PQRS and COSA-S and because a normal distribution could not be expected for all D-KEFS sub-tests. The level of significance was set at p ≤ 0.05.
To identify the number of goals with a clinically relevant improvement (≥2 points) from T1 to T2, individual calculations were performed for each goal and for both COPM and PQRS, separately for trained and untrained goals. The difference between the groups in the proportion of all goals reaching clinically relevant improvement was tested for significance using Fisher’s exact test. The non-parametric effect size for that difference between the groups in the proportion of improved goals was calculated using phi-coefficient interpretation following Cohen as: 0.1 = small, 0.3 = medium and 0.5 = large effect size [Citation42]. For the primary outcome measures, the median of the differences between T1 and T2 was also calculated for each group, separately for trained (n = 3 for each participant) and untrained (n = 1 for each participant) goals, and differences between T1 and T2 were compared as between the groups using the Mann – Whitney U test.
Since COSA-S lacks a sum score, the analysis of this outcome measure was strictly descriptive.
For the neuro-psychological tests of executive function, raw scores were transformed into age-equivalent scaled scores (mean = 10, SD = 3), with higher values indicating better performance relative to age-specific norms. These age-corrected scores were used for all statistical calculations. Descriptive statistics with means and medians for the test results are presented, and the differences between T1 and T2 for all D-KEFS sub-tests were compared as between the groups using the Mann–Whitney U test. For within-group comparisons, non-parametric statistics were used (the Wilcoxon signed-rank test) and effect sizes were calculated according to the formula and interpreted in accordance with Cohen [Citation43]. Finally, with regard to BRIEF, raw data for the three index scales were transformed into a T-score (mean = 50, SD = 10) where a score >60 is considered to indicate executive difficulties [Citation37]. Descriptive data are presented.
Results
A total of 42 children were randomized but 4 discontinued the study, meaning that 38 children participated (n = 21 in the CO-OP group and n = 17 in the control group (). Of the 38 participating children, 11 had SB and 27 had CP; 22 were males; and the mean age was 12 years and 5 months (range: 7–16) ().
Table 1. Participants’ demographics.
There was no significant difference at baseline between the CO-OP group and the control group in BRIEF ratings by either parents or children ().
Table 2. BRIEF scores: children’s self-reports and parent’s report at baseline (T1), CO-OP group and control group.
The goals chosen by the children varied from simple to complex. Some of them did not directly concern how to perform something but rather how to organize things and get them done in time. In some cases, a goal was formulated as daring to do something that the child had previously avoided because it caused anxiety and worry. The goals can be broken down into the following activity areas: Preparing meals, Self-care, Home life, Organization of school and homework, Leisure, Orienting oneself in one’s environment, and Societal life; see Appendix 1. An absolute majority of the treatment sessions were performed face-to-face, but two sessions were performed via video link owing to illness in the child or therapist.
According to the regular OTs in the control group (treatment-as-usual group), the type of interventions they provided to the children during the relevant period were mainly compensatory interventions (such as technical aids or adaptations to activities or the environment) but also involved advice to parents and/or schools about how they could enhance the child’s ability. The number of sessions varied and was individually adjusted.
Primary outcome
COPM
There were significant differences between the groups in the proportion of clinically relevant improvements (≥2 points) to ratings of goals on the COPM performance scale, in favour of the CO-OP group. This was seen for both trained goals (p < 0.001, effect size Phi= −0.49) and for untrained goals (p = 0.008, effect size Phi= −0.48) ().
Table 3. Proportion of goals with an increase of ≥2 points between T1 and T2.
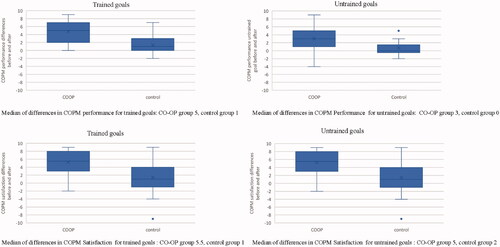
The median difference on the COPM performance scale between T1 and T2 was 5 points in the CO-OP group and 1 point in the control group for trained goals. For untrained goals, the median difference was 3 points in the CO-OP group and 0 points in the control group (). The CO-OP group had a significantly greater difference in self-rated performance between T1 and T2 than the control group both in terms of trained and untrained goals, (trained goals p < 0.001 and untrained goals p = 0.008).
Figure 2. Boxplots showing differences between T1 and T2 in children’s rating of COPM performance and satisfaction for trained and untrained goals. Boxplot diagram showing median and interval differences in self-rated performance and satisfaction with COPM between baseline and post-treatment assessment. The picture shows ratings from both the children in the group who received CO-OP training and from those in the control group, for both trained and untrained goals.
In the CO-OP group, 15 out of 21 children improved ≥2 points in self-rated performance on all three trained goals; in the control group, only 2 out of 17 children did. Further, 15 children in the CO-OP group and 4 children in the control group improved their self-rated performance of the untrained goal.
Regarding the COPM rating of satisfaction, a significantly larger proportion of trained goals having improved by ≥2 points was found for the CO-OP group (p < 0.001, effect size Phi= −0.48). However, there was no significant difference in the COPM satisfaction rating for untrained goals between the groups (p = 0.318, effect size Phi= −0.19) (). The median difference on the satisfaction scale for trained goals was 5.5 points in the CO-OP group and 1 point in the control group. For untrained goals, the median difference was 5 points in the CO-OP group and 2 points in the control group (). The CO-OP group had a significantly greater difference in self-estimated satisfaction between T1 and T2 than the control group in terms of trained goals (p < 0.001) but not for untrained goals (p = 0.107).
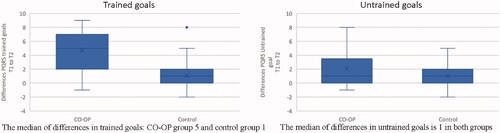
PQRS
The proportion of goals with a clinically relevant improvement (≥2 points) on the PQRS scale between T1 and T2 was significantly larger in the CO-OP group than in the control group for trained goals (p < 0.001, effect size Phi=-0.45) but not for untrained goals (p = 0.197, effect size Phi= −0.23) (). For trained goals, the median difference on the 10-point PQRS scale was 5 points in the CO-OP group and 1 point in the control group. For untrained goals, the median difference was 1 in both groups (). The CO-OP group had a significantly greater difference in the objective estimates of performance between T1 and T2 than the control group had in terms of trained goals (p < 0.001) but not for untrained goals (p = 0.243).
Figure 3. Boxplots showing differences between T1 and T2 in blinded rating of PQRS for trained and untrained goals. Boxplot diagram showing the median and interval for differences between baseline and post-treatment assessment in objective, blinded assessment of goal attainment with PQRS, for both the group that received CO-OP training and for the control group, in both trained and untrained goals.
Secondary outcomes
D-KEFS
Between-group comparisons of the differences between baseline (T1) and follow-up (T2) did not attain significance for any of the D-KEFS sub-tests (TMT 2: p = 0.728; TMT 4: p = 0.170; Verbal fluency: p = 0.729; Semantic fluency: p = 0.794; Tower test p = 0.862).
However, within-group analysis showed that both groups improved significantly between T1 and T2 in scaled scores on the TMT 2 whereas only the control group did so on TMT 4 (both test attention-related). The CO-OP group showed significant improvement between T1 and T2 in scaled scores for problem-solving (Tower Test), with medium effect sizes, but the control group did not ().
Table 4. Results for executive function, D-KEFS sub-tests in CO-OP group and control group, within-group analysis.
Large variation in test performance was noted for D-KEFS: some participants improved markedly from baseline to follow-up while others deteriorated.
COSA-S
At T1, the median number of self-reported problems on the COSA-S was 5 in each group. Participants in both groups reported a reduction in the number of self-reported problems on the competence scale between T1 and T2. In the CO-OP group, the median number of problems was reduced to 4, and 14 out of 21 participants rated a reduction of problems at T2 (p = 0.015). In the control group, the median number of problems remained 5 at T2, and 11 out of 17 participants rated a reduction of problems (p = 0.214).
Discussion
The results of the present study showed higher goal achievement for trained goals in both subjective and objective ratings in the CO-OP group than in the control group. Effect sizes were moderate but bordering on large. A generalization and transfer effect on subjective ratings using COPM for untrained goals was seen in the CO-OP group but not in the control group. Transfer – in the sense that a person transfers the improved performance of a trained skill to an untrained one [Citation44] – is a crucial [Citation45] yet rarely demonstrated outcome of rehabilitation interventions [Citation46], although it has in fact been observed in previous studies of CO-OP [Citation28,Citation47]. Given that CO-OP is person-centred throughout the intervention process, it is encouraging to note that the participants in the CO-OP group themselves felt, to a greater extent than the participants in the control group, that they handled their performance problems better after the intervention, including with regard to the untrained goals. Interestingly, this finding was not accompanied by any significant differences in improvement between the groups in executive function as measured using the D-KEFS sub-tests – even though there was an indication that problem-solving ability had improved in the CO-OP group.
Although the median reduction between T1 and T2 in the number of problems, as measured using COSA-S, was larger in the CO-OP group, it is also an important finding that participants in both groups considered themselves to have fewer competence problems in everyday life at T2. In fact, this may even seem contradictory, considering that competence is often related to self-efficacy [Citation48]. One possible interpretation is that this is an effect of expectation in both groups as well as – and probably above all – an effect of the fact that the children in both groups were invited to reflect upon their own perception of their competence and upon what was important to them, and also invited to set their own goals. For clients to be treated as capable of discussing how competent they are and what is important to them, and being trusted as capable of working with self-identified goals, has in fact been described as a crucial element of person-centred care [Citation49–51]. Hence the present results suggest that, even in the “treatment as usual” condition, person-centred care in the sense of treating the children as competent persons who can formulate their own goals and values actually had an important effect. This indicates that such person-centred care should always be provided alongside family-centred care. However, in the CO-OP Approach, person-centredness is taken one step further in that it represents a key element of the whole treatment process, where the person’s involvement in all steps of the process is what creates the requisite conditions for a good outcome, as suggested by self-efficacy theory [Citation52,Citation53]. Against this background and given the positive outcome on COPM for untrained goals, it is possible to assume that the CO-OP training gave the participants an enhanced sense of self-efficacy.
For the untrained goals, objective ratings of performance using PQRS showed no significant differences between the groups – in contrast to the subjective ratings of the same goals. This might be because the ratings were based on a single film sequence providing a snapshot of the activity, which may have masked smaller differences. Additionally, this study only used one untrained goal and one PQRS rater while other similar studies have used two untrained goals and two raters; if this had been the case here as well, the result might have been different.
Executive function is a difficult construct to measure. It has been argued that tests of executive function do not properly reflect everyday performance, meaning that their ecological validity is questionable [Citation54]. When it comes to reliability, children with neuro-developmental disorders often display fatigue and their performance can vary considerably from time to time [Citation55,Citation56]. The present study indicates that the participating children perceived themselves as having become better at dealing with new situations although there was no measurable improvement to executive functions. This result is interesting in that it confirms the suggestion made in the International Classification of Functioning and Health (ICF) that an intervention does not necessarily have to affect bodily functions in order to have an effect at the level of activity and participation. Similar findings have been made in other studies [Citation25]. Further, CO-OP is a meta-cognitive approach [Citation18,Citation57] which introduces a new dimension [Citation14] that helps children find their own ways of thinking and performing, so that they can handle new situations in ways that suit them. Given that many children with a neuro-developmental diagnosis such as CP or SB have problems performing activities involving attentional control and problem-solving [Citation9,Citation58] and that they find it hard to keep a task in mind from beginning to end, this meta-cognitive approach could be particularly beneficial to them.
Study strengths and limitations
The present study has some limitations, and its results should be interpreted in the light of those. Although the research design is strong, the study sample was small, and this may have prevented the detection of changes in some of the measures. Even so, both significant and clinically relevant effects were in fact seen for the primary outcome measures. That the administrator of the COPM was not blinded at T2 can be seen as a limitation, but it is a well-known problem that it is sometimes difficult to hide the condition of treatment. However, it is a strength of the present study that the assessors were blinded at T1, when the goals were set, and also that the rater of objective goal attainment (PQRS) was blinded to group allocation and chronological order at both T1 and T2. Further, the fact that the study includes children from different regions and rehabilitation centres reduces the risk of bias relating to therapist effects in the control group and increases the generalizability of the results. The randomization clusters were limited by the fact that both diagnoses, and SB in particular, have a low prevalence in Sweden. It would have been interesting to compare the CO-OP treatment with another treatment of a more defined nature than “treatment as usual,” but the purpose was to compare CO-OP with the existing rehabilitation services typically provided in Sweden. A pragmatic design where CO-OP represented an addition to the existing rehabilitation services was chosen because performing an activity in real life depends on many different parameters and so cannot be studied in a laboratory situation where all parameters are controlled. What is more, we did not consider it ethically acceptable to deprive children of their usual rehabilitation contacts for the duration of the intervention. This pragmatic choice of design in fact strengthens the results: they have actually been obtained in the real-world Swedish rehabilitation context, with no changes being made to any other conditions. Moreover, it should be considered a strength that the present results confirm those of previous studies of similar groups of children [Citation23,Citation24,Citation26,Citation59–61] and those of studies carried out in the same Swedish context [Citation29].
Finally, the present study restricts itself to reporting baseline and (immediately) post-treatment results. However, it is important for the effects of any rehabilitation intervention to be sustained over time, which is why longer-term results will be presented in a future report from the same trial.
Conclusions
According to the present study, the CO-OP Approach is an important complement to conventional rehabilitation services for children with cerebral palsy and spina bifida. Compared with treatment as usual only, it yielded higher both subjective and objective ratings for attainment of self-chosen trained goals. In addition, and maybe even more notably, it yielded higher self-rated goal attainment for untrained goals, suggesting a generalization and transfer effect that probably helped the children enhance their sense of self-efficacy. The present study suggests that children with cerebral palsy (MACS levels I–III) or spina bifida without intellectual disabilities can benefit from the CO-OP Approach when it comes to reaching self-identified goals, and that this may enhance their self-efficacy.
Acknowledgements
The authors would like to thank the children and their families who participated in the study. We would also like to thank the occupational therapists and rehabilitation centres that participated, and Linus Lind for conducting part of the assessments.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Roberts AEK, Bannigan K. Dimensions of personal meaning from engagement in occupations: a metasynthesis. Can J Occup Ther. 2018;85(5):386–396.
- Michelsen SI, Flachs EM, Damsgaard MT, et al. European study of frequency of participation of adolescents with and without cerebral palsy. Eur J Paediatr Neurol. 2014;18(3):282–294.
- Bünger A, Urfer-Maurer N, Grob A. Multimethod assessment of attention, executive functions, and motor skills in children with and without ADHD: children’s Performance and parents’ perceptions. J Atten Disord. 2021;25(4):596–606.
- Kelly NC, Ammerman RT, Rausch JR, et al. Executive functioning and psychological adjustment in children and youth with spina bifida. Child Neuropsychol. 2012;18(5):417–431.
- Whittingham K, Bodimeade HL, Lloyd O, et al. Everyday psychological functioning in children with unilateral cerebral palsy: does executive functioning play a role? Dev Med Child Neurol. 2014;56(6):572–579.
- Zukerman JM, Devine KA, Holmbeck GN. Adolescent predictors of emerging adulthood milestones in youth with spina bifida. J Pediatr Psychol. 2011;36(3):265–276.
- Bodimeade HL, Whittingham K, Lloyd O, et al. Executive function in children and adolescents with unilateral cerebral palsy. Dev Med Child Neurol. 2013;55(10):926–933.
- Bottcher L. Children with spastic cerebral palsy, their cognitive functioning, and social participation: a review. Child Neuropsychol. 2010;16(3):209–228.
- Bottcher L, Flachs EM, Uldall P. Attentional and executive impairments in children with spastic cerebral palsy. Dev Med Child Neurol. 2010;52(2):e42–e47.
- Jacobson LA, Tarazi RA, McCurdy MD, et al. The Kennedy Krieger Independence Scales-Spina Bifida Version: a measure of executive components of self-management. Rehabil Psychol. 2013;58(1):98–105.
- Piovesana AM, Ross S, Whittingham K, et al. Stability of executive functioning measures in 8-17-year-old children with unilateral cerebral palsy. Clin Neuropsychol. 2015;29(1):133–149.
- Pirila S, van der Meere JJ, Rantanen K, et al. Executive functions in youth with spastic cerebral palsy. J Child Neurol. 2011;26(7):817–821.
- Tuminello ER, Holmbeck GN, Olson R. Executive functions in adolescents with spina bifida: relations with autonomy development and parental intrusiveness. Child Neuropsychol. 2012;18(2):105–124.
- Öhrvall AM, Bergqvist L, Hofgren C, et al. “With CO-OP I'm the boss” – experiences of the cognitive orientation to daily occupational performance approach as reported by young adults with cerebral palsy or spina bifida. Disabil Rehabil. 2020;42(25):3645–3652.
- Stubberud J, Langenbahn D, Levine B, et al. Goal Management Training improves everyday executive functioning for persons with spina bifida: self-and informant reports six months post-training. Neuropsychol Rehabil. 2014;24(1):26–60.
- Polatajko HJ, Mandich A. Enabling occupation in children: the cognitive orientation to daily occupational performance (CO-OP) approach. Ottawa (ON): CAOT Publications ACE; 2004.
- Polatajko HJ, Mandich AD, Missiuna C, et al. Cognitive orientation to daily occupational performance (CO-OP): part III–the protocol in brief. Phys Occup Ther Pediatr. 2001;20(2–3):107–123.
- Poulin V, Korner-Bitensky N, Bherer L, et al. Comparison of two cognitive interventions for adults experiencing executive dysfunction post-stroke: a pilot study. Disabil Rehabil. 2017;39(1):1–13.
- Izadi-Najafabadi S, Gill KK, Zwicker JG. Training-induced neuroplasticity in children with Developmental Coordination Disorder. Curr Dev Disord Rep. 2020;7(2):48–58.
- Thornton A, Licari M, Reid S, et al. Cognitive Orientation to (Daily) Occupational Performance intervention leads to improvements in impairments, activity and participation in children with Developmental Coordination Disorder. Disabil Rehabil. 2016;38(10):979–986.
- Skowronski JM, Engsberg JR. Blended Approach to Occupational Performance (BAOP): guidelines enabling children with autism. Open J Occup Ther. 2017;5(1).
- Wilson J, Mandich A, Magalhaes L. Concept mapping: a dynamic, individualized and qualitative method for eliciting meaning. Qual Health Res. 2016;26(8):1151–1161.
- Cameron D, Craig T, Edwards B, et al. Cognitive Orientation to daily Occupational Performance (CO-OP): a new approach for children with cerebral palsy. Phys Occup Ther Pediatr. 2017;37(2):183–198.
- Gimeno H, Brown RG, Lin JP, et al. Cognitive approach to rehabilitation in children with hyperkinetic movement disorders post-DBS. Neurology. 2019;92(11):e12–e24.
- Gimeno H, Polatajko HJ, Cornelius V, et al. Rehabilitation in childhood-onset hyperkinetic movement disorders including dystonia: treatment change in outcomes across the ICF and feasibility of outcomes for full trial evaluation. Eur J Paediatr Neurol. 2021;33:159–167.
- Jackman M, Novak I, Lannin NA, et al. The cognitive orientation to daily occupational performance (CO-OP) approach: best responders in children with cerebral palsy and brain injury. Res Dev Disabil. 2018;78:103–113.
- Novak I, Morgan C, Fahey M, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep. 2020;20(2):3.
- Houldin A, McEwen SE, Howell MW, et al. The cognitive orientation to daily occupational performance approach and transfer: a scoping review. OTJR (Thorofare N J). 2018;38(3):157–172.
- Peny-Dahlstrand M, Bergqvist L, Hofgren C, et al. Potential benefits of the cognitive orientation to daily occupational performance approach in young adults with spina bifida or cerebral palsy: a feasibility study. Disabil Rehabil. 2020;42(2):228–239.
- Chalkidou K, Tunis S, Whicher D, et al. The role for pragmatic randomized controlled trials (pRCTs) in comparative effectiveness research. Clin Trials. 2012;9(4):436–446.
- Eliasson AC, Krumlinde-Sundholm L, Rosblad B, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48(7):549–554.
- Palisano RJ, Rosenbaum P, Bartlett D, et al. Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. 2008;50(10):744–750.
- Hoffer MM, Feiwell E, Perry R, et al. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg Am. 1973;55(1):137–148.
- Kramer J, ten Velden M, Kafkes A, et al. Child Occupational Self Assessment (COSA), version 2.2 in swedish: Barns mening om aktiviteter - självskattning av kompetens och betydelse (COSA-S). Nacka: Sveriges Arbetsterapeuter; 2016.
- Law M, Baptiste S, Carswell A, et al. Canadian Occupational Performance Measure (COPM). (5th ed. rev. 2019 ed. öob, 5:e upplagan), editor. Nacka: Sveriges Arbetsterapeuter; 2020.
- Delis DC, Kaplan D, Kramer JH. Delis-Kaplan executive function system (D-KEFS) technical manual. Swedish version; Pearson Assessment ed. San Antonio (TX): Psychological Corporation; 2001.
- Gioia GA, Isquith PK, Guy SC, et al. BRIEF behaviour rating inventory of executive functions. Professional manual. Lutz (FL): Psychological Assessment Resources; 2000.
- Götalandsregionen HHV. https://www.vgregion.se/en/f/habilitation–health/patients-at-hoh/habilitation/.
- Region Stockholm HH. https://www.habilitering.se/.
- Kang M, Smith E, Goldsmith CH, et al. Documenting change with the Canadian Occupational Performance Measure for children with cerebral palsy. Dev Med Child Neurol. 2020;62(10):1154–1160.
- Martini R, Rios J, Polatajko H, et al. The performance quality rating scale (PQRS): reliability, convergent validity, and internal responsiveness for two scoring systems. Disabil Rehabil. 2015;37(3):231–238.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Erlbaum; 1988.
- Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18.
- McEwen S, Houldin A. Generalization and transfer in the CO–OP approach. In: Dawson DR, McEwen SE, Polatajko HJ, editors. Cognitive orientation to daily performance in occupational therapy. Bethesda (MD): AOTA Press; 2201. p. 31–42.
- Geusgens CA, Winkens I, van Heugten CM, et al. Occurrence and measurement of transfer in cognitive rehabilitation: a critical review. J Rehabil Med. 2007;39(6):425–439.
- Rutledge KJ, van den Bos W, McClure SM, et al. Training cognition in ADHD: current findings, borrowed concepts, and future directions. Neurotherapeutics. 2012;9(3):542–558.
- Scammell EM, Bates SV, Houldin A, et al. The Cognitive Orientation to daily Occupational Performance (CO-OP): a scoping review. Can J Occup Ther. 2016;83(4):216–225.
- Holahan LF. Quality-in-doing: competence and occupation. J Occup Sci. 2014;21(4):473–487.
- Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. Am Psychol. 2002;57(9):705–717.
- Melin J, Nordin A, Feldthusen C, et al. Goal-setting in physiotherapy: exploring a person-centered perspective. Physiother Theory Pract. 2021;37(8):863–880.
- Quaye AA, Coyne I, Soderback M, et al. Children’s active participation in decision-making processes during hospitalisation: an observational study. J Clin Nurs. 2019;28(23–24):4525–4537.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
- Stevens D, Anderson DI, O’Dwyer NJ, et al. Does self-efficacy mediate transfer effects in the learning of easy and difficult motor skills? Conscious Cogn. 2012;21(3):1122–1128.
- Wallisch A, Little LM, Dean E, et al. Executive function measures for children: a scoping review of ecological validity. OTJR (Thorofare N J). 2018;38(1):6–14.
- Bergqvist L, Ohrvall AM, Ronnback L, et al. Evidence of construct validity for the modified mental fatigue scale when used in persons with cerebral palsy. Dev Neurorehabil. 2020;23(4):240–252.
- Lindsay S. Child and youth experiences and perspectives of cerebral palsy: a qualitative systematic review. Child Care Health Dev. 2016;42(2):153–175.
- Dawson DR, McEwen SE, Polatajko HJ. Cognitive orientation to daily occupational performance in occupational therapy – using the CO-OP ApproachTM to enable participation across lifespan. Bethesda (MD): AOTA Press; 2017.
- Tarazi RA, Zabel TA, Mahone EM. Age-related differences in executive function among children with spina bifida/hydrocephalus based on parent behavior ratings. Clin Neuropsychol. 2008;22(4):585–602.
- Jackman M, Novak I, Lannin N, et al. Effectiveness of Cognitive Orientation to daily Occupational Performance over and above functional hand splints for children with cerebral palsy or brain injury: a randomized controlled trial. BMC Pediatr. 2018;18(1):248.
- Steinhart S, Raz-Silbiger S, Beeri M, et al. Occupation based telerehabilitation intervention for adolescents with myelomeningocele: a pilot study. Phys Occup Ther Pediatr. 2021;41(2):176–191.
- Ghorbani N, Rassafiani M, Izadi-Najafabadi S, et al. Effectiveness of cognitive orientation to (daily) occupational performance (CO-OP) on children with cerebral palsy: a mixed design. Res Dev Disabil. 2017;71:24–34.
