?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
To review the effects of external lumbar supports on various aspects of sensorimotor function including joint position sense (JPS), postural control, anticipatory postural adjustments (APAs), and compensatory postural adjustments (CPAs).
Methods
A systematic literature search was performed in PubMed, EMBASE, Scopus, Ovid, Cochrane library, and Web of Science. Two reviewers selected studies which assessed the effect of lumbosacral orthosis or kinesio-tape on JPS, postural control or APAs/CPAs in subjects with and without low back pain (LBP). The methodological quality of included studies was assessed using a modified version of Downs and Black’s checklist.
Results
Findings demonstrated moderate effects of lumbosacral orthosis on specific aspects of sensorimotor control including JPS and to a lesser extent standing stability. These domains were not or minimally affected by application of kinesio-tape. Both orthosis and kinesio-tape had negligible effects on APAs and CPAs.
Conclusions
The positive effects of lumbar orthosis on JPS or postural control were mostly observed in conditions where sources of proprioceptive feedback are impaired (such as LBP) or absent (standing with eyes closed on an unstable surface). However, evidence does not prove significant positive effects for the application of kinesio-tape to improve sensorimotor control.
Wearing lumbar orthosis leads to an improvement in joint position sense.
Postural stability seems to be affected to some extent by utilizing lumbar orthosis.
Clinicians can administer orthosis to improve sensorimotor adaptation, especially in conditions with poor proprioception.
Kinesio-tape had negligible effects on all domains of sensorimotor control.
Improvement of sensorimotor function as a result of application of kinesio-tape is questionable.
IMPLICATIONS FOR REHABILITATION
Introduction
When dealing with postural perturbations to the human spine, the central nervous system receives afferent inputs from proprioceptor receptors and other sensory systems such as visual or vestibular and then integrates and processes them in order to maintain postural stability [Citation1,Citation2]. Previous studies have frequently reported proprioception deficits in the lumbosacral region [Citation3,Citation4], altered feedforward and feedback mechanisms [Citation5,Citation6], delayed reflex response [Citation7,Citation8], and decreased postural stability [Citation9] in people with low back pain (LBP). Although the direction of the causal relationship between LBP and sensorimotor impairment is not yet clear [Citation10], the results of prospective longitudinal studies suggest an increased risk of developing an initial LBP episode in people with poor standing balance [Citation11] or delayed-onset muscle reactions [Citation7]. However, a reverse causal relationship may also exist; a sensorimotor disorder may be a consequence of pain or its cognitive aspects such as fear of pain [Citation10].
Among numerous therapeutic modalities, lumbar supports, especially lumbosacral orthoses and kinesio-tape, are frequently used for prevention and treatment of LBP. No definite conclusion can be drawn regarding some of the proposed mechanisms such as changes in sensorimotor function to explain the effect of lumbar supports on LBP. Several studies have examined the efficacy of lumbosacral orthosis and kinesio-tape on different domains of sensorimotor function including proprioception (or kinesthesia), postural control and postural adjustment, the results of which, however, were contradictory. For instance, the effect of external lumbar supports on proprioception has been inconsistently reported with some studies showing a positive effect [Citation12,Citation13], others showing no effect [Citation14,Citation15], and others again showing a negative effect [Citation12,Citation16,Citation17]. These inconsistent findings justify the need for a systematic review to synthesize the current evidence and to explain the variation between studies. Some previous reviews examined the efficacy of external lumbar supports [Citation18–21]; however, none of them have specifically focused on sensorimotor function. The core outcome measures in these reviews were pain and disability. The present systematic review used a qualitative approach to synthesize the available evidence in order to assess the effects of external lumbar supports on various aspects of sensorimotor function, namely, joint position sense (JPS), postural control in standing and sitting, anticipatory postural adjustments (APAs), and compensatory postural adjustments (CPAs) in patients with LBP and healthy subjects.
Materials and methods
Inclusion and exclusion criteria
The PICOS (P: Population; I: Intervention; C: Comparison; O: Outcome; S: Study design) framework was used to frame the eligibility criteria and to define the search terms. P was defined as “healthy subjects or patients with LBP,” I as “lumbosacral orthosis or kinesio-tape,” O as “JPS, postural control or APAs/CPAs,” and S as “pure within-subjects design or combined with between-subjects design” (). The C component was not applicable.
Table 1. Summary of inclusion and exclusion criteria.
Information sources and search strategy
The present systematic review was reported in accordance with guidelines outlined in the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) Statement. A systematic literature search was performed in the electronic databases of PubMed, EMBASE, Scopus, Ovid, Cochrane library, and Web of Science from the earliest possible entry until April 2021 to identify relevant studies. Literature search was completed by search in Google Scholar, citation tracking of all included articles and checking reference lists of included studies to identify additional eligible studies.
The specific search string used in PubMed is available as an online Supplementary material (Table S1). The search strategy was optimized for other databases through appropriate adjustments, and the results of search string per database were exported to EndNote.
Study selection
After completing the search process, two reviewers (F.A. and M.M.) independently screened the title and abstract of retrieved studies based on pre-identified inclusion/exclusion criteria.
Assessment of methodological quality
The two reviewers (F.A. and M.M.) assessed the methodological quality of included studies using a modified version of Downs and Black’s checklist, designed for assessing the quality of randomized and non-randomized studies. This checklist has a high internal consistency and inter-rater and intra-rater reliability [Citation22]. The modified version consists of four domains measuring quality of reporting, external validity, internal validity, and study power ().
Table 2. Modified version of Downs and Black’s checklist to assess risk of bias of included studies.
Data extraction
Information about participant’s demographic characteristics, inclusion/exclusion criteria, intervention characteristics, and test protocols was extracted from included articles by the first reviewer (F.A.) using a data extraction form, and verified by the second reviewer (M.M.).
Data analysis
Mean and standard deviation (SD) of all outcome measures and the number of participants per group were extracted by the first author (F.A.). When the data were presented separately for male and female participants in a study, the formula suggested by the Cochrane Handbook for Systematic Reviews of Intervention was used to combine mean, SD, and number of subjects of the two subgroups into a single group. Where SEM was only reported, SD was calculated using the formula: When range and median were only available, mean and SD were calculated using a method devised by Hozo et al. [Citation23]. When numerical data were only presented in figures, we used WebPlotDigitizer (https://automeris.io/WebPlotDigitizer) to extract the mean and SD or SEM from figure images.
For JPS error and traditional center of pressure (COP) time-series measures, the results of original studies were replicated using bar charts to compare single groups before and after wearing external lumbar support. The study results were sub-grouped in accordance with the type of intervention (tape and/or orthosis) and the length of intervention (immediate and/or longer-term). The immediate effect was defined as the changes in the outcome measures observed in a single session immediately after application of external lumbar supports, whereas longer-term effect was characterized as the effect measured after a course of treatment, either short-term (hours or days) or long-term (months). Mean, SD, and significance results for other measures of postural control and postural adjustments were presented in the tables.
Results
Literature search
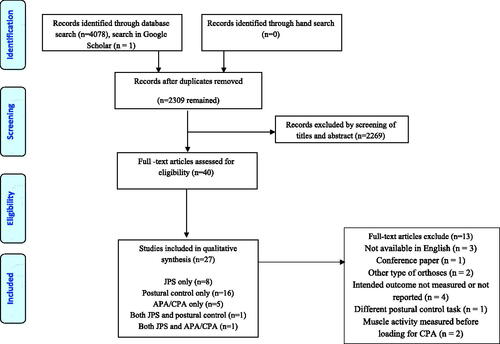
Screening titles and abstracts yielded 40 potentially eligible studies out of 2309 retrieved studies. Detailed review of their full text resulted in the exclusion of 13 studies [Citation24–36]. Hand search of reference list of included studies did not yield further study. From the remaining 27 studies, eight studies were included for review of JPS, 16 studies for postural control, and five studies for APAs/CPAs with one study reporting both JPS and postural control [Citation15] and another one reporting both JPS and APAs/CPAs [Citation37] ().
Characteristics of studies
Overview of participants’ characteristics
Of the 27 included studies, 11 studies examined healthy individuals [Citation13,Citation15,Citation16,Citation38–45], 12 studies examined only LBP patients [Citation37,Citation46–56], and four studies evaluated both healthy individuals and LBP patients [Citation12,Citation14,Citation17,Citation57] (). With the exception of one study in which participants had lumbar discopathy [Citation51], most studies examined patients with non-specific LBP.
Table 3. Study design, demographic, inclusion/exclusion criteria, and intervention characteristics of all included studies.
All but three studies [Citation15,Citation41,Citation45] reported the age range of the participants, ranging from 18 to 65 years. Fourteen studies reported pain duration [Citation12,Citation14,Citation17,Citation37,Citation46–49,Citation52–57] with pain lasting at least >3 months in all studies with the exception of one where patients had LBP with at least 4-week duration [Citation14]. When using 0–10-point pain rating scales, pain intensity varied from 1.5 to 7.7 between studies. The LBP-related disability level was evaluated by Roland-Morris Disability Questionnaire (RMDQ) [Citation14] and Oswestry Disability Index (ODI) [Citation37,Citation46–50,Citation54–56]. The mean RMDQ and ODI disability scores were 5.02 and 21.5% (16.3–39.3%), respectively, indicating the inclusion of patients with mild to moderate functional disability in these studies. The length of intervention varied from a few minutes to 12 weeks.
JPS
Description of intervention and outcome measures
Eight studies evaluated the effect of external supports on JPS. Of the five studies evaluating the effect of orthosis, one study used rigid orthosis [Citation16] and others used soft and/or semi-rigid orthosis, with two studies examining only the immediate effects [Citation13,Citation14], one assessing only longer-term effects (4 weeks [Citation37]) and two assessing both immediate and longer-term effects (2 h [Citation12] and 3 weeks [Citation16]) (). Of the three studies examining the effect of kinesio-tape [Citation15,Citation17,Citation56], one assessed the immediate effects [Citation17] and the two others longer-term effects (30 min [Citation15] and 3 days [Citation56]). Out of eight studies, three studies included only healthy individuals [Citation13,Citation15,Citation16], two studies [Citation37,Citation56] only patients with LBP and the other three studies [Citation12,Citation14,Citation17] both healthy individuals and patients with LBP.
Since all eight studies measured active JPS using absolute error (AE) as an outcome measure (), only AE results were presented in the bar plots. JPS was measured in sitting position in five studies [Citation14–17,Citation37] and in standing position in three studies [Citation12,Citation13,Citation56]. In two studies, the target was set in neutral-spine-posture [Citation15,Citation16] by returning from flexion in one study [Citation15] and from axial rotation in the other one [Citation16]. The target was set at a position far from neutral-spine-posture, i.e., flexion in six studies [Citation12,Citation13,Citation15,Citation17,Citation37,Citation56], extension in three studies [Citation12,Citation37,Citation56], lateral bending in one study [Citation12], and rotation in one study [Citation14].
Table 4. Measurement protocol of studies investigating the effects of orthosis and kinesio-tape on JPS.
Difference between pre-test/intervention and post-test/intervention
The immediate effects of orthosis were examined in 14 experimental conditions (i.e., n = 14) contributed by four studies (). JPS error was reduced (JPS improved) by wearing orthosis in a total of five conditions related to two studies. In conditions with improved JPS, the participants were either LBP patients (n = 3, one study) or healthy individuals (n = 2, two studies). In the other 14 experimental conditions investigating the longer-term effects (n = 14, three studies), wearing orthosis was associated with improvement (n = 3, one study) in LBP patients, or deterioration of JPS (n = 3, two studies) in healthy subjects.
Figure 2. Bar plot representing the immediate and longer-term effect of lumbar orthosis on absolute JPS error in healthy and LBP people.
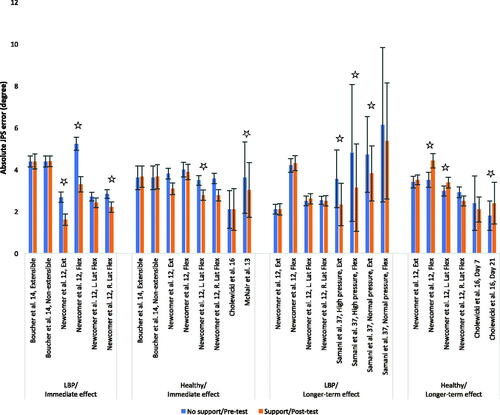
The two experimental conditions related to a single study investigating the immediate effect of kinesio-tape in LBP patients (n = 1) or healthy subjects (n = 1) showed that kinesio-tape was associated with increased JPS error (). In the other five conditions contributed by two studies examining the longer-term effects, no significant differences were found.
Figure 3. Bar plot representing the immediate and longer-term effect of kinesio-tape on absolute JPS error in LBP and/or healthy people.
Postural control
Description of intervention and outcome measures
Sixteen studies [Citation15,Citation38,Citation39,Citation43–53,Citation55,Citation57] evaluated the effect of orthoses (n = 11) or kinesio-tape (n = 5) on postural control (). Of the 11 studies which used orthosis, four studies administered a rigid orthosis [Citation43,Citation45,Citation51,Citation52] and others used soft and/or semi-rigid orthoses. Eight of these 11 studies examined the immediate effect [Citation38,Citation43–45,Citation47,Citation51,Citation53,Citation57]; the length of intervention in studies examining longer-term effects was 4 weeks [Citation48,Citation49,Citation52]. The tape application method was inconsistent between the five studies administering kinesio-tape [Citation15,Citation39,Citation46,Citation50,Citation55]. The length of intervention varied from a few minutes to 7 days. Six out of the 16 studies included only healthy subjects [Citation15,Citation38,Citation39,Citation43–45], one study [Citation57] both healthy subjects and LBP patients, and nine other studies only LBP patients [Citation46–53,Citation55].
Table 5. Measurement protocol of studies investigating the effects of orthosis and kinesio-tape on postural control.
Out of 16 studies, 11 studies assessed postural control during standing [Citation39,Citation46–53,Citation55,Citation57] and five studies during sitting [Citation15,Citation38,Citation43–45]. In all 11 studies, postural control was assessed during standing on firm surface. Additionally, proprioceptive feedback was manipulated in five of these studies by standing on foam surface [Citation47–49,Citation55,Citation57]. The effect of orthoses or kinesio-tape on the postural control has been evaluated in either eyes-open (EO) [Citation50,Citation52] or eyes-closed (EC) condition [Citation51] or both EO and EC conditions [Citation46–50,Citation53,Citation55,Citation57]. Among studies assessing sitting posture, four studies evaluated postural control while sitting on an unstable surface in EO (n = 2) [Citation15,Citation38], EC (n = 1) [Citation43], or in both EO and EC (n = 1) [Citation44] conditions. One study investigated the postural control in EC condition while sitting on a stable surface [Citation45].
The most commonly used COP parameters to quantify postural sway in the included studies were sway area, amplitude, and velocity. Where both sway amplitude and velocity were available, only sway velocity measures were included as they are more reliable [Citation58] and represent both spatial and temporal aspects of COP oscillations; otherwise, sway amplitude measures were included.
Difference between pre-test/intervention and post-test/intervention: standing
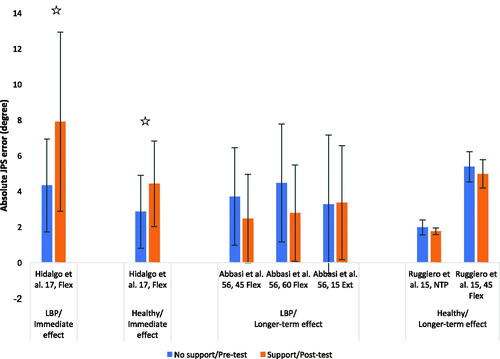
A decrease in the amount of COP fluctuations was found in three conditions out of 15 experimental conditions contributed by four studies investigating the immediate (n = 6, three studies) and/or longer-term (n = 9, one study) effects of orthosis in LBP patients (). All three conditions were related to a single study assessing longer-term effects of orthosis on postural stability tasks while standing on foam with EC.
Figure 4. Bar plot representing the immediate and/or longer-term effect of lumbar orthosis on standing stability (COP velocity (upper panel) and area (lower panel)) in LBP subjects. Asterisks indicate significant differences. RSEO: rigid-surface eyes-open; RSEC: rigid-surface eyes-closed; FSEO: foam-surface eyes-open; FSEC: foam-surface eyes-closed.
The immediate and or longer-term effects of kinesio-tape on standing postural control have been investigated in 22 conditions contributed by three studies, but no significant change was observed in any of the testing conditions ().
Figure 5. Bar plot representing the immediate and longer-term effect of kinesio-tape on standing stability in LBP (upper panel) and the longer-term effect in healthy subjects (lower panel). RSEO: rigid-surface eyes-open; RSEC: rigid-surface eyes-closed; FSEO: foam-surface eyes-open; FSEC: foam-surface eyes-closed. In the study of Toprak Celenay and Ozer Kaya [Citation50], mean and SD were estimated on the basis of range and median values. Jassi et al.: mean sway velocity between AP and ML direction.
![Figure 5. Bar plot representing the immediate and longer-term effect of kinesio-tape on standing stability in LBP (upper panel) and the longer-term effect in healthy subjects (lower panel). RSEO: rigid-surface eyes-open; RSEC: rigid-surface eyes-closed; FSEO: foam-surface eyes-open; FSEC: foam-surface eyes-closed. In the study of Toprak Celenay and Ozer Kaya [Citation50], mean and SD were estimated on the basis of range and median values. Jassi et al.: mean sway velocity between AP and ML direction.](/cms/asset/dceb71aa-f5dc-493e-848f-cf7e13883176/idre_a_2043464_f0005_c.jpg)
Additional variables
Assessment of the immediate effects of orthosis on standing postural control using NeuroCom Balance Master showed reduced COP velocity (quantified in degrees/second) in the most challenging conditions (i.e., standing on foam surface with EO and EC) in both LBP patients and healthy controls [Citation57] (Table S2). Longer-term effects of both soft and rigid orthoses were examined in LBP patients using the Biodex Balance System, and the results showed a decrease in mediolateral stability index (MLSI) and overall stability index (OSI) in the rigid orthosis group and a decrease in anteroposterior stability index (APSI), MLSI, and OSI in the soft orthosis group [Citation52]. No significant changes were found when longer-term effects of orthosis on the dynamical structure of COP were examined in LBP patients [Citation48].
Longer-term use of kinesio-tape reduced static APSI and OSI obtained from Biodex Balance System in LBP patients [Citation50].
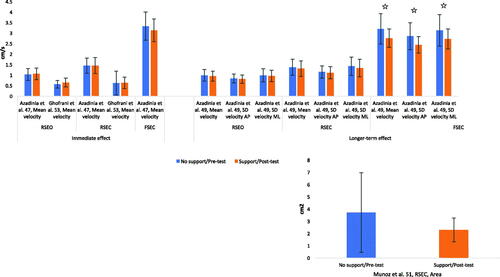
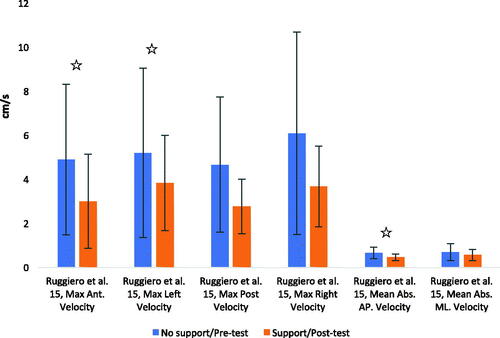
Difference between pre-test/intervention and post-test/intervention: sitting
Significant changes were found in three out of a total of 13 conditions contributed by four studies examining the immediate effects of wearing orthosis on sitting postural stability in healthy subjects (). The changes included a decrease in the COP mean velocity during sitting on the stable surface with EC (n = 2, one study) or an increased COP variance during sitting on a highly unstable surface with EC following wearing a lordotic LSO (n = 1, one study).
Figure 6. Bar plot representing the immediate effect of lumbar orthosis on sitting stability (COP velocity (upper panel) and variance (lower panel)) in healthy people. Asterisks indicate significant differences. SSEC: stable-surface eyes-closed; USEO: unstable-surface eyes-open; USEC: unstable-surface eyes-closed.
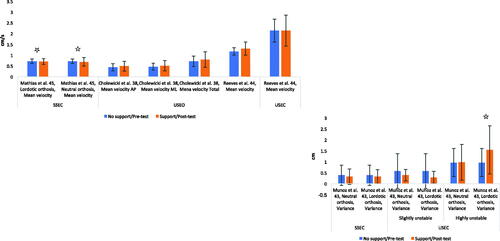
Three conditions from six conditions related to a single study examining the longer-term effects of kinesio-tape application on sitting postural stability found kinesio-tape application to be associated with reduced COP variables ().
Figure 7. Bar plot representing the longer-term effect of kinesio-tape on sitting stability with eyes-open in healthy people. Asterisks indicate significant differences.
APAs and CPAs
Description of intervention and outcome measures
Five studies [Citation37,Citation40–42,Citation54] examined the effect of orthoses (three studies) or kinesio-tape (two studies) on APAs and/or CPAs (). Among studies examining the efficiency of orthosis, two studies assessed the longer-term effects by utilizing a rigid orthosis applied for 3 weeks [Citation40] or a semi-rigid orthosis in combination with NSAIDs for 4 weeks [Citation37]. The only study which examined the immediate effects of orthosis used soft elastic belts [Citation41]. Two of these five studies evaluated the effect of kinesio-tape alone [Citation42] or in combination with routine physical therapy [Citation54], but with inconsistent methods of taping. The intervention lasted one hour in one of the studies [Citation42], and 12 weeks in another one [Citation54]. Of these five studies, the participants were healthy individuals in three studies [Citation40–42] and chronic LBP patients in two studies [Citation37,Citation54].
Table 6. Measurement protocol of studies investigating the effects of orthosis and kinesio-tape on anticipatory and compensatory postural adjustments.
Two studies evaluated the effect of orthoses using CPA paradigms [Citation40,Citation41], one study examined the effect of kinesio-tape using only an APAs paradigm [Citation54], and two studies investigated the effect of orthoses [Citation37] or kinesio-tape [Citation42] using both APAs and CPAs paradigms. To assess APAs, expected perturbation was exerted by fast arm raising in sitting [Citation54] or standing position [Citation42] or by releasing a swinging pendulum in a standing position [Citation37]. To assess CPA, unexpected perturbation was administered by applying a sudden loading into the subject's hand [Citation41,Citation42] or by impacting of a swinging pendulum to the pelvis while standing [Citation37] or by a sudden force release in flexion, extension, and lateral bending through a cable connected to the thoracic region during the semi-seated position [Citation40].
Difference between pre-test/intervention and post-test/intervention: APAs
The longer-term effects of orthosis in response to predictable perturbation in LBP patients were investigated in four muscles. All these belonged to one study [Citation37], in which a semi-rigid LSO was prescribed in two different pressure levels (normal- and high-pressure). Out of eight assessments (four muscles × two orthosis conditions) per outcome, only three statistically significant benefits in favor of orthoses were observed, including a decrease in the amplitude of EMG of erector spinae (ES) muscle in the both groups of normal- and high-pressure orthosis, and earlier activation of transversus abdominis (TrA) muscle in the normal-pressure orthosis group.
The longer-term effects of tape application on the timing of muscle activity in response to predictable perturbations (i.e., APAs) were investigated in seven muscles contributed by two studies. The significant findings included earlier activation of ES and multifidus muscles in healthy subjects in one study, and earlier activation of obliquus externus (OE) abdominis and TrA muscles in LBP patients in another study.
Difference between pre-test/intervention and post-test/intervention: CPA
None of two studies examining the immediate or longer-term effects of orthosis on onset delays in six muscles reported significant changes. When the immediate or longer-term effects on amplitude of activity were examined in five muscles contributed by two studies, significant changes were found in a few experimental conditions. The significant findings included reduced activity of right OE and right rectus abdominis in healthy subjects in one study examining the immediate effects, and reduced activity of ES in LBP patients in another study examining the long-term effects of wearing orthosis with high pressure.
In a single study examining the longer-term effect of kinesio-tape in healthy subjects, none of five studied muscles showed significant changes.
Assessment of methodological quality
Out of 27 included studies, 11 articles received the complete score of reporting bias (). Aims (item 1) and outcomes (item 2) were clearly described by all studies. Nine studies did not describe the characteristics of participants in the experiment (item 3) and eight studies did not clearly describe the details of the administered external support (item 4). Only two studies failed to clearly describe the details of their findings (item 5). All but four studies provided an estimate of variance of their data (item 6). Eight studies did not declare actual p values for the main outcome measures (item 7).
Table 7. Methodological quality rating of included studies.
Neither of the included studies reported the source population of the selected sample (item 8) and the representative of the sample (item 11). Therefore, all studies obtained zero score for external validity.
For internal validity, only in three studies assessors were blinded (item 10). With the exception of two studies, the rest of studies did not perform data dredging (item 11). Appropriate statistical tests (item 12) were used in all but four studies. Only three studies reported the acceptable reliability of their outcome measures (item 13). With the exception of few (n = 5), all studies reported random allocation to group and/or experimental conditions (item 14). More than half of the included studies (n = 14) failed to provide information regarding power calculation (item 15).
Discussion
The present systematic review investigated the change in sensorimotor function following immediate and longer-term application of external lumbar supports. Findings supported moderate effects of lumbosacral orthosis on specific aspects of sensorimotor control such as JPS and to a lesser extent postural stability (standing). Kinesio-tape had negligible effect on all domains of sensorimotor control. These findings will be discussed below in further detail.
JPS
Wearing orthosis was associated with immediate slight improvement of JPS for both LBP (one out of two studies [Citation12,Citation14]) and healthy (two out of four studies [Citation12–14,Citation16]) groups. Since none of studies assessed JPS using targets located at neutral-spine-posture, it is hard to attribute the positive findings to a specific type of target-matching task. However, if we assume that positions farther from neutral-spine-posture are more dependent on proprioceptive input as they are less practiced, then the role of orthotic devices in enhancing proprioceptive feedbacks play a more crucial role in non-neutral positions. Additionally, forces applied by the orthosis to the body, are likely larger in farther from neutral posture, which may enhance effect of the orthosis. However, further investigation is needed to explore posture dependency and the underlying mechanism of target-matching tasks on the relationship between lumbar supports and JPS.
Longer-term effects of orthosis on enhancement of JPS were positive for LBP (one out of two studies [Citation12,Citation37]) but negative for healthy subjects (two out of two studies [Citation12,Citation16]). One plausible explanation is that both groups may, over time, rely more on information provided by the orthosis and less on proprioception. This would work out negative for healthy individuals with normal proprioception but improve JPS in LBP patients with impaired proprioception.
The limited evidence regarding the effect of tape application on lumbar position sense showed mixed results. In terms of immediate effects of kinesio-tape, the results of the single included study [Citation17] showed an increase of JPS error in both LBP and healthy groups. This is not consistent with the findings reported for longer-term effects by the other two included studies. They both reported no change of proprioceptive acuity either in healthy [Citation15] or LBP subjects [Citation56]. Even though the study of Abbasi et al. [Citation56] outperformed other two studies in terms of studied population (LBP with impaired proprioception), taping method (star shape technique as the most effective method) and duration of intervention (72 h), there was only a tendency towards improvement of JPS following application of kinesio-tape (). The insignificant findings could be due to limited sample size and consequently a lack of power of this specific study. Additionally, it is surprising that the direction of the non-significant effect (positive) is also opposite to the short-term effects (negative).
Postural control
Standing
No data regarding the effect of orthosis on standing postural control in healthy subjects exist when considering traditional COP measures. Only one of four studies [Citation47,Citation49,Citation51,Citation53] assessing postural control in LBP found a small positive effect following longer-term application of orthosis. The results of this study [Citation49] showed that wearing orthosis reduced postural sway in the most difficult postural condition, i.e., standing on foam surface with EC. Indication of postural improvement following application of orthosis was also found when postural control was measured using other parameters and/or instruments. For instance, in the study of Mi et al. [Citation57] wearing orthosis was associated with immediate decrease of postural sway when standing on foam with either EO or EC in both healthy and LBP groups. Similarly, LBP patients showed improvement of postural control when standing on a movable support surface (Biodex Balance System) following longer-term application of orthosis [Citation52]. These findings are consistent with the results of a systematic review [Citation59] which showed larger COP displacement in patients with LBP compared to healthy subjects during standing in more challenging conditions, such as standing on an unstable surface or with EC. Since LBP patients rely more on visual inputs [Citation9] and ankle strategy [Citation60] to maintain postural stability due to impaired lumbar proprioception, it makes sense that demands on lumbar proprioception increase in the absence of visual inputs or standing on an unstable surface (which disrupts afferent information from foot mechanoreceptors). In such cases, wearing orthosis may have improved the ability to detect body position by increasing tactile sensation, which in turn reduces postural sway.
When postural control was analyzed using traditional COP measures, none of the studies [Citation39,Citation46,Citation55] found an effect of kinesio-tape following either immediate or longer-term application. Only the single study that measured postural control when standing on a dynamic support surface (Biodex Balance System) [Citation50] reported improvement of postural stability following longer-term use of kinesio-tape in patients with LBP. If we assume that postural control should be improved through enhancing proprioceptive feedback, absence of a positive effect of kinesio-tape on JPS leaves no surprise to see postural control is unaffected following application of kinesio-tape.
Sitting
Among studies that evaluated the effect of orthosis on sitting postural stability using traditional COP parameters, only two out of four studies [Citation38,Citation43–45] reported an effect of wearing orthosis in healthy subjects. The results were contradictory, with one study [Citation45] reporting a small amount of improvement (decrease) in postural sway as a result of immediate effect of wearing of orthosis (either neutral or lordotic orthosis) and the other one [Citation43] finding a negative impact of wearing lordotic lumbosacral orthosis on postural stability during sitting on a highly unstable surface. This discrepancy could be attributed to the task difficulty. Whereas Mathias and Rougier [Citation45] measured orthosis effects in a stable seated position with the feet unsupported (making correction by lower extremity possible), Munoz et al. [Citation43] tested participants in a highly unstable position with both feet placed on a foot support (excluding correction by lower extremity). With an increased seat instability in the latter condition, larger adjustments are needed to be imposed by trunk to control balance. However, it is possible that orthosis makes it difficult for trunk to compensate this large amount of external perturbation. Given that all studies investigated only the immediate effects in healthy subjects, the longer-term effects of orthosis especially in LBP patients are unclear.
Only one study [Citation15] evaluated longer-term effects (30 min) of kinesio-tape on sitting postural stability in healthy subjects and found a decrease in some COP velocity parameters. However, their findings could be related to a placebo effect because the same results were found in sham group. Moreover, according to the pretest/posttest design in their study, the evaluations were repeated 30 min after the tape application without controlling the order effect. Therefore, it is possible that the results have been subjected to a learning effect. Furthermore, the validity of outcome measures such as maximum velocity used in this study which are calculated based on only a single data point of the whole measurement trial is questionable [Citation61].
APAs and CPAs
Studies investigating measures of postural adjustments reported mostly no effect of either orthosis or kinesio-tape. All studies measured the response of multiple trunk muscles to verify postural adjustments. Since the majority of studies reported no change of muscular activity in most or all muscle groups, it is possible that the rare positive effects are coincidental. However, the limited number of studies investigating APAs/CPAs makes it hard to draw firm conclusion regarding the efficacy of orthosis and kinesio-tape.
Methodological quality
The overall quality was relatively similar between studies that found an effect and those that did not find an effect, specifically determined per population (LBP and healthy) and duration of effect (immediate and longer-term). Detailed inspection of important parameters such as sample size and reliability of measures did not show a difference between the two groups of studies neither. The fact that many studies did not find an effect does not seem to be a power problem. Most non-significant results also showed almost equal bars in the figures.
Proposed mechanisms of actions
Various mechanisms have been hypothesized to explain change of JPS and postural control following use of lumbar orthosis, where the most significant effects were located. Enhanced proprioceptive acuity through stimulation of cutaneous mechanoreceptors is one of the proposed mechanisms. Previous research has noted that feedbacks from skin receptors improve various aspects of motor control including proprioception [Citation62] and postural sway [Citation63]. However, the skin contribution to improved JPS following application of orthosis can rapidly decrease over time. For instance, Newcomer et al. [Citation12] found a reduction in JPS as an immediate effect of wearing orthosis in LBP patients but no change after two hours of wearing orthosis. A possible justification for these findings is the rapid adaptation of cutaneous receptors and losing their sensitivity to tactile pressure over time [Citation64]. Furthermore, based on the findings of the study by Samani et al. [Citation37], the JPS error decreased after 4 weeks of wearing orthosis. Given that they evaluated proprioception without wearing an orthosis, the improvement in proprioception could not be attributed to an increase in tactile sensation.
Some researchers suggest that orthoses decrease trunk muscle co-contraction and the activity of back-extensor muscles during daily activities by passively stiffening the trunk [Citation65]. This gives rise to reducing muscular fatigue [Citation66] which can lead to improvement of lumbar spine proprioception [Citation67] and even postural sway [Citation68]. External lumbar supports may also enhance sensorimotor function by increasing perception of security and confidence [Citation69]. Alteration of brain regional activity is another proposed mechanism for improved proprioception. The change in brain activity during active lower extremity movement was examined while manipulating proprioceptive feedback by wearing a tight brace, a moderate tight sleeve and no brace/sleeve [Citation70]. The findings showed higher level of brain activation while wearing external supports especially tight brace which provoke proprioception the most. Despite the above propositions, the exact mechanism by which external lumbar supports increase proprioception or its indirect measures, i.e., postural control, is still unclear.
Limitations
In this study, definition of proprioception was narrowed to JPS and among different measures of JPS only AE was analyzed. This was due to the limited number of studies which investigated other aspects or measures of JPS as well as an attempt to decrease the heterogeneity of outcome measures which helps to improve the interpretation of results. Despite narrowing down the outcome measures, we were still not able to perform a meta-analysis and hence could not provide a precise estimate of the total effect size.
This review also included studies that used different external lumbar supports with various materials, structures, or fittings which implies that findings should be interpreted cautiously because these factors may affect functioning of sensorimotor control. For instance, some evidence suggests that only a non-extensible (non-elastic) lumbar orthosis can increase trunk stiffness and thereby reduce trunk muscle co-contraction [Citation71]. However, Boucher et al. [Citation14] did not show a difference between the two types of extensible and non-extensible orthoses. It is quite possible that the pattern of sensorimotor behavior emerges as a result of interaction of lumbar orthoses with other components of the motor system. For instance, Munoz et al. [Citation43] findings suggest that the effect of an orthosis on sitting postural stability can be neutral, positive, or negative based on the degree of seat instability and the structure of the orthosis.
Even though more positive findings have been reported for lumbosacral orthoses, no definitive conclusion can be drawn whether they deliver better outcomes than kinesio-tapes. It would be ideal if these two types of external lumbar supports were compared directly or if there was no difference in the way that studies were conducted, for example in terms of studied population, design, methods of assessment, etc.
Conclusions
Given that enhancing proprioception and its indirect measure, i.e., postural control, has been postulated as a putative mechanism of action of lumbar orthosis and kinesio-tape, there was a demand for a review to summarize all past research and deliver a clear and comprehensive overview of evidence on this topic. As the first review to synthesize evidence on the effect of external lumbar supports on sensorimotor control, our results indicate moderate effect of lumbar orthosis on neuromuscular adaptation. However, there was no substantial evidence for an effect of kinesio-tape. Future randomized clinical trials with high-quality methodology and long-term follow-up are warranted to determine the efficacy of external lumbar support in terms of sensorimotor performance.
Supplementary_material.docx
Download MS Word (43.8 KB)Disclosure statement
The authors report no conflicts of interest.
References
- Mergner T, Rosemeier T. Interaction of vestibular, somatosensory and visual signals for postural control and motion perception under terrestrial and microgravity conditions—a conceptual model. Brain Res Brain Res Rev. 1998;28(1–2):118–135.
- Radebold A, Cholewicki J, Polzhofer GK, et al. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine (Phila Pa 1976). 2001;26(7):724–730.
- Tong MH, Mousavi SJ, Kiers H, et al. Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Arch Phys Med Rehabil. 2017;98(1):120–136.e2.
- Brumagne S, Cordo P, Lysens R, et al. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine. 2000;25(8):989–994.
- Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976). 1996;21(22):2640–2650.
- Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. J Spinal Disord. 1998;11(1):46–56.
- Cholewicki J, Silfies SP, Shah RA, et al. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine (Phila Pa 1976). 2005;30(23):2614–2620.
- Reeves N, Cholewicki J, Milner T. Muscle reflex classification of low-back pain. J Electromyogr Kinesiol. 2005;15(1):53–60.
- Mazaheri M, Coenen P, Parnianpour M, et al. Low back pain and postural sway during quiet standing with and without sensory manipulation: a systematic review. Gait Posture. 2013;37(1):12–22.
- Hodges PW, Moseley GL. Pain and motor control of the lumbopelvic region: effect and possible mechanisms. J Electromyogr Kinesiol. 2003;13(4):361–370.
- Takala E-P, Viikari-Juntura E. Do functional tests predict low back pain? Spine. 2000;25(16):2126–2132.
- Newcomer K, Laskowski ER, Yu B, et al. The effects of a lumbar support on repositioning error in subjects with low back pain. Arch Phys Med Rehabil. 2001;82(7):906–910.
- McNair PJ, Heine PJ. Trunk proprioception: enhancement through lumbar bracing. Arch Phys Med Rehabil. 1999;80(1):96–99.
- Boucher J-A, Roy N, Preuss R, et al. The effect of two lumbar belt designs on trunk repositioning sense in people with and without low back pain. Ann Phys Rehabil Med. 2017;60(5):306–311.
- Ruggiero SA, Frost LR, Vallis LA, et al. Effect of short-term application of kinesio tape on the flexion-relaxation phenomenon, trunk postural control and trunk repositioning in healthy females. J Sports Sci. 2016;34(9):862–870.
- Cholewicki J, Shah KR, McGill KC. The effects of a 3-week use of lumbosacral orthoses on proprioception in the lumbar spine. J Orthop Sports Phys Ther. 2006;36(4):225–231.
- Hidalgo B, Gobert F, Bragard D, et al. Effects of proprioceptive disruption on lumbar spine repositioning error in a trunk forward bending task. J Back Musculoskelet Rehabil. 2013;26(4):381–387.
- Nelson NL. Kinesio taping for chronic low back pain: a systematic review. J Bodyw Mov Ther. 2016;20(3):672–681.
- Mostafavifar M, Wertz J, Borchers J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Phys Sportsmed. 2012;40(4):33–40.
- van Duijvenbode IC, Jellema P, van Poppel MN, et al. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev. 2008;2008(2):CD001823.
- Landauer F, Trieb K. An indication-based concept for stepwise spinal orthosis in low back pain according to the current literature. J Clin Med. 2022;11(3):510.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
- Mark K, Yang AA. The effect of soft lumbar corset on postural stability in patients with chronic low back pain during standing. Prosthet Orthot Int. 2015;416:39.
- Myung J-H, Yang K-H, Lee S-S, et al. The effects of abdominal belt and taping on balance ability. J Korea Soc Neurother. 2017;21(3):35–40.
- Ju H-P, Choi S-A, Jeong D-H, et al. Effect of abdominal compression belt on static balance during one leg standing in low back pain patients. Korea Propriocept Neuromusc Fac Assoc. 2017;15(3):353–360.
- Grüneberg C, Bloem B, Honegger F, et al. The influence of artificially increased hip and trunk stiffness on balance control in man. Exp Brain Res. 2004;157(4):472–485.
- van der Burg JCE, Pijnappels M, van Dieën JH. The influence of artificially increased trunk stiffness on the balance recovery after a trip. Gait Posture. 2007;26(2):272–278.
- Kadri MA, Violette M, Dallaire M, et al. The immediate effect of two lumbar stabilization methods on postural control parameters and their reliability during two balance tasks. J Man Manip Ther. 2021;29(4):235–239.
- Larivière C, Boucher J-A, Mecheri H, et al. Maintaining lumbar spine stability: a study of the specific and combined effects of abdominal activation and lumbosacral orthosis on lumbar intrinsic stiffness. J Orthop Sports Phys Ther. 2019;49(4):262–271.
- Ludvig D, Preuss R, Larivière C. The effect of extensible and non-extensible lumbar belts on trunk muscle activity and lumbar stiffness in subjects with and without low-back pain. Clin Biomech. 2019;67:45–51.
- Bernardelli RS, Scheeren EM, Fuentes Filho AR, et al. Effects of kinesio taping on postural balance in patients with low back pain, a randomized controlled trial. J Bodyw Mov Ther. 2019;23(3):508–514.
- Shahvarpour A, Preuss R, Larivière C. The effect of extensible and non-extensible lumbar belts on trunk postural balance in subjects with low back pain and healthy controls. Gait Posture. 2019;72:211–216.
- Pfeifer K, Vogt L, Klingler J, et al. Sensomotor function while wearing lumbar support ortheses. Z Orthop Ihre Grenzgeb. 2001;139(1):12–18.
- Cholewicki J, Juluru K, Radebold A, et al. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J. 1999;8(5):388–395.
- Thomas JS, Lavender SA, Corcos DM, et al. Effect of lifting belts on trunk muscle activation during a suddenly applied load. Hum Fact. 1999;41(4):670–676.
- Samani M, Shirazi ZR, Hadadi M, et al. A randomized controlled trial comparing the long-term use of soft lumbosacral orthoses at two different pressures in patients with chronic nonspecific low back pain. Clin Biomech. 2019;69:87–95.
- Cholewicki J, Reeves NP, Everding VQ, et al. Lumbosacral orthoses reduce trunk muscle activity in a postural control task. J Biomech. 2007;40(8):1731–1736.
- Toprak Celenay S, Ozkan T, Unluer NO. Short-term effects of trunk kinesio taping on trunk muscle endurance and postural stability in healthy young adults: a randomized controlled trial. Turk J Physiother Rehabil. 2019;30(2):89–96.
- Cholewicki J, McGill KC, Shah KR, et al. The effects of a three-week use of lumbosacral orthoses on trunk muscle activity and on the muscular response to trunk perturbations. BMC Musculoskelet Disord. 2010;11(1):1–10.
- Lavender SA, Shakeel K, Andersson GB, et al. Effects of a lifting belt on spine moments and muscle recruitments after unexpected sudden loading. Spine (Phila Pa 1976). 2000;25(12):1569–1578.
- Voglar M, Sarabon N. Kinesio taping in young healthy subjects does not affect postural reflex reactions and anticipatory postural adjustments of the trunk: a pilot study. J Sports Sci Med. 2014;13(3):673.
- Munoz F, Rouboa A, Rougier P. The balance control effects on sitting posture induced by lumbosacral orthosis wear vary depending on the level of stability. Appl Ergon. 2013;44(4):511–516.
- Reeves NP, Everding VQ, Cholewicki J, et al. The effects of trunk stiffness on postural control during unstable seated balance. Exp Brain Res. 2006;174(4):694–700.
- Mathias M, Rougier P. In healthy subjects, the sitting position can be used to validate the postural effects induced by wearing a lumbar lordosis brace. Ann Phys Rehabil Med. 2010;53(8):511–519.
- Abbasi S, Rojhani-Shirazi Z, Shokri E, et al. The effect of kinesio taping on postural control in subjects with non-specific chronic low back pain. J Bodyw Mov Ther. 2018;22(2):487–492.
- Azadinia F, Ebrahimi-Takamjani I, Kamyab M, et al. Immediate effects of lumbosacral orthosis on postural stability in patients with low back pain: a preliminary study. Arch Bone Joint Surg. 2019;7(4):360.
- Azadinia F, Ebrahimi-Takamjani I, Kamyab M, et al. Effects of lumbosacral orthosis on dynamical structure of center of pressure fluctuations in patients with non-specific chronic low back pain: a randomized controlled trial. J Bodyw Mov Ther. 2019;23(4):930–936.
- Azadinia F, Ebrahimi-Takamjani I, Kamyab M, et al. A RCT comparing lumbosacral orthosis to routine physical therapy on postural stability in patients with chronic low back pain. Med J Islam Repub Iran. 2017;31:26.
- Toprak Celenay S, Ozer Kaya D. Immediate effects of kinesio taping on pain and postural stability in patients with chronic low back pain. J Bodyw Mov Ther. 2019;23(1):206–210.
- Munoz F, Salmochi J-F, Faouen P, et al. Low back pain sufferers: is standing postural balance facilitated by a lordotic lumbar brace? Orthop Traumatol Surg Res. 2010;96(4):362–366.
- Kang J-I, Kwon H-M, Jeong D-K, et al. The effects on postural control and low back pain according to the types of orthoses in chronic low back pain patients. J Phys Ther Sci. 2016;28(11):3074–3077.
- Ghofrani M, Olyaei G, Talebian S, et al. Immediate effects of lumbosacral belt on postural control during challenging tasks in patients with chronic low back pain. J Mod Rehabil. 2017;11:119–126.
- Bae SH, Lee JH, Oh KA, et al. The effects of kinesio taping on potential in chronic low back pain patients anticipatory postural control and cerebral cortex. J Phys Ther Sci. 2013;25(11):1367–1371.
- Jassi FJ, Del Antônio TT, Azevedo BO, et al. Star-shape kinesio taping is not better than a minimal intervention or sham kinesio taping for pain intensity and postural control in chronic low back pain: a randomized controlled trial. Arch Phys Med Rehabil. 2021;102(7):1352–1360.e3.
- Abbasi S, Rasanani M-RH, Ghotbi N, et al. Short-term effect of kinesiology taping on pain, functional disability and lumbar proprioception in individuals with nonspecific chronic low back pain: a double-blinded, randomized trial. Chiropr Man Ther. 2020;28(1):1–10.
- Mi J, Ye J, Zhao X, et al. Effects of lumbosacral orthoses on postural control in individuals with or without non-specific low back pain. Eur Spine J. 2018;27(1):180–186.
- Salavati M, Hadian MR, Mazaheri M, et al. Test–retest reliability [corrected] of center of pressure measures of postural stability during quiet standing in a group with musculoskeletal disorders consisting of low back pain, anterior cruciate ligament injury and functional ankle instability. Gait Posture. 2009;29(3):460–464.
- Koch C, Hänsel F. Non-specific low back pain and postural control during quiet standing—a systematic review. Front Psychol. 2019;10:586.
- Brumagne S, Janssens L, Knapen S, et al. Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J. 2008;17(9):1177–1184.
- Palmieri R, Ingersoll C, Stone M, et al. Center-of-pressure parameters used in the assessment of postural control. J Sport Rehabil. 2002;11(1):51–66.
- Collins DF, Refshauge KM, Todd G, et al. Cutaneous receptors contribute to kinesthesia at the index finger, elbow, and knee. J Neurophysiol. 2005;94(3):1699–1706.
- Krishnamoorthy V, Slijper H, Latash ML. Effects of different types of light touch on postural sway. Exp Brain Res. 2002;147(1):71–79.
- Röijezon U, Clark NC, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 1: basic science and principles of assessment and clinical interventions. Man Ther. 2015;20(3):368–377.
- Cholewicki J. The effects of lumbosacral orthoses on spine stability: what changes in EMG can be expected? J Orthop Res. 2004;22(5):1150–1155.
- Saito H, Sekiguchi M, Yamada H, et al. Comparison of postural changes and muscle fatigue between two types of lumbar support: a prospective longitudinal study. Fukushima J Med Sci. 2014;60(2):141–148.
- Enoka RM, Baudry S, Rudroff T, et al. Unraveling the neurophysiology of muscle fatigue. J Electromyogr Kinesiol. 2011;21(2):208–219.
- Davidson BS, Madigan ML, Nussbaum MA. Effects of lumbar extensor fatigue and fatigue rate on postural sway. Eur J Appl Physiol. 2004;93(1–2):183–189.
- Bernhardt T, Anderson GS. Influence of moderate prophylactic compression on sport performance. J Strength Condition Res. 2005;19(2):292–297.2.0.CO;2]
- Thijs Y, Vingerhoets G, Pattyn E, et al. Does bracing influence brain activity during knee movement: an fMRI study. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1145–1149.
- Cholewicki J, Lee AS, Peter Reeves N, et al. Comparison of trunk stiffness provided by different design characteristics of lumbosacral orthoses. Clin Biomech. 2010;25(2):110–114.