Abstract
Purpose
(1) To estimate the proportion of Dutch wheelchair users with spinal cord injury (SCI) who meet different SCI exercise guidelines; (2) to evaluate which demographic and lesion characteristics are associated with meeting these guidelines; (3) whether meeting these guidelines is associated with physical fitness and health.
Materials and methods
Based on the PASIPD questionnaire items, participants were allocated to meeting two SCI aerobic exercise guidelines, which differ in exercise load. Differences in personal, lesion, fitness, and health characteristics between groups were tested with a one-way ANOVA. Multiple regression analyses were performed to evaluate if meeting guidelines was associated with better fitness and health. Statistical significance was accepted at p < 0.05.
Results
Of the 358 included participants, 63.1% met at least one aerobic exercise guideline. Being female, older age, having tetraplegia, and lower educational level were associated with a lower likelihood to meet the aerobic exercise guidelines. Meeting aerobic exercise guidelines showed a positive association with all respiratory and exercise capacity parameters. Limited associations were found between meeting exercise guidelines and health.
Conclusions
Meeting exercise guidelines was associated with better respiratory functions and exercise capacity with additional fitness and some body composition benefits in higher exercise activity levels.
Meeting SCI exercise guidelines are associated with better respiratory functions and exercise capacity with additional fitness and body composition benefits when higher exercising at higher activity levels, emphasizing the value and importance of regular exercise in individuals with SCI.
IMPLICATIONS FOR REHABILITATION
Introduction
Being physically active has many potential benefits, such as reduced risks of cardiovascular disease and other noncommunicable diseases, increased mental health, and weight control [Citation1]. However, despite these well-known benefits of physical activity (PA), 31% of the abled-bodied adults globally and 43% in Western countries are physically inactive [Citation2]. These numbers are even higher in people with spinal cord injury (SCI), who are 60% less physically active compared to able-bodied individuals [Citation3]. PA promotion is therefore needed and of great importance, especially in people with SCI.
To facilitate PA promotion, the World Health Organization (WHO) developed evidence-based PA guidelines based on studies on the dose-response relationship between frequency, duration, and intensity of physical activity and health outcomes [Citation4,Citation5]. Although the WHO states “the recommendation can be applied to adults with disabilities,” it is also mentioned that “they may need to be adjusted for each individual based on their exercise capacity and specific health risks or limitations” [Citation4]. Despite the effort to place more emphasis on people with chronic disabilities in the new 2020 WHO PA guidelines, limited evidence was presented on specific chronic conditions and disabilities [Citation5]. Therefore, the two recently developed and published exercise guidelines specifically for people with SCI to promote PA are relevant [Citation6,Citation7]. Both guidelines were specifically designed towards exercise, a subcategory of PA, which is considered as “physical activity that is planned, structured, repetitive, and purposive in the sense that improvement or maintenance of one or more components of physical fitness is an objective” [Citation8]. Therefore, the focus of the remaining of this paper will be on exercise specifically.
The recent exercise guidelines for people with SCI [Citation6,Citation7] are to a certain extent similar but seem to differ in recommended weekly aerobic exercise, as shown in . Martin Ginis et al. [Citation6] developed SCI-specific exercise guidelines for improving fitness with additional guidelines with more strenuous recommendations for improving cardiometabolic health. The guidelines developed by Tweedy et al. [Citation7] are based on the assumption that the recommendations for the general population also apply to people with SCI, as SCI-specific exercise evidence is consistent with those from the general population. Therefore, the Tweedy et al. [Citation7] guidelines resulted in a higher physical weekly load regarding frequency and time than the guidelines of Martin Ginis et al. [Citation6]. According to Tweedy et al. [Citation7], this higher load is “required in order for people with SCI to achieve good cardiometabolic health, physical fitness, and functioning.”
Table 1. Overview of different SCI exercise guidelines.
These differences in load between the exercise guidelines likely influence the proportion of the SCI community meeting them. Rauch et al. [Citation9] documented that sex, age, time since injury (TSI), severity of SCI, and type of locomotion are associated with meeting WHO exercise guidelines, and Rocchi et al. [Citation10] documented that type of locomotion and autonomous motivation are associated with meeting the guidelines of Martin Ginis. It remains unknown, however, if and how meeting different exercise guidelines and therefore weekly load, translates to additional fitness and health benefits [Citation11]. With increasing exercise levels, and therefore, increasing fitness levels, a curvilinear reduction in mortality has been well documented in able-bodied [Citation12]. As a consequence, it could be assumed that physical fitness and health are more likely to be better in people who meet the more strenuous guidelines of Tweedy et al. [Citation7], compared to people who only meet the fitness or cardiometabolic guidelines of Martin Ginis et al. [Citation6] or people not meeting any exercise guidelines at all.
Therefore, the aims of this study were: (1) to estimate the proportion of Dutch wheelchair users with chronic SCI (≥5 years after injury) meeting two different exercise guidelines; (2) to evaluate which demographic and lesion characteristics are associated with meeting these guidelines; and (3) whether meeting these guidelines is associated with better physical fitness and health.
Methods
Study design
A cross-sectional analysis was performed on merged data from two Dutch research programs, i.e., “Restoration of mobility in the rehabilitation of persons with SCI” (Umbrella project) [Citation13] and “Active LifestyLe Rehabilitation Interventions in aging Spinal Cord injury” (ALLRISC) [Citation14]. Participants were recruited from eight Dutch rehabilitation centers with a specialized SCI unit. All participants provided informed consent after being informed about the study. Approval was given by the local medical ethics committee of rehabilitation center Hoensbroek and the medical ethics committee of the University Medical Centre Utrecht for the Umbrella project and by the medical ethics committee of the University Medical Centre Utrecht for the ALLRISC project.
Participants
Individuals were eligible to participate in the Umbrella project if they had a recent SCI, classified as A-D on the American Spinal Injury Association (AISA) impairment scale [Citation15]; were aged between 18 and 65 years; and were wheelchair dependent for community use. Exclusion criteria to participate were: having an SCI due to malignancies; progressive disease; known cardiovascular disease or psychiatric problems; and insufficient command of the Dutch language. The data of the Umbrella project collected 5 years after the discharge of inpatient rehabilitation were analyzed for this study [Citation16].
Individuals were eligible to participate in the cross-sectional ALLRISC project if they had an SCI, age at injury between 18 and 35 years with at least a time since injury (TSI) of 10 years at inclusion; and were wheelchair dependent for longer distances (>500 m). Insufficient command of the Dutch language was an exclusion criterion to participate in this project [Citation14].
Data collection
The two datasets were prepared and merged on all available parameters relating to personal demographics, lesion characteristics, Physical Activity Scale for Individuals with Physical Disabilities (PASIPD) items, fitness, and health-related outcomes. All participants who did not complete items 4–6 from the PASIPD, needed to determine whether exercise guidelines were met or not, were excluded from the analysis.
Physical activity
Three items (items 4–6) from the PASIPD [Citation17], administered in both projects, were used to determine whether participants met the different SCI-specific exercise guidelines. These items determined the weekly amount of time spent in moderate (item 4) and strenuous (item 5) exercise intensity and on muscle strength exercises (item 6). For each item, the frequency (0, 1–2, 3–4, or 5–7 times a week) and duration (<1, 1–2, 2–4, >4 h) were reported. This could then be calculated into an average daily time spent (hours/day) on the aerobic exercise of moderate intensity, vigorous intensity, and strength exercise, based on the algorithm the PASIPD provided [Citation17], and converted into weekly average time spent on each activity. PASIPD outcomes were checked on outliers, by comparing the results to answers of other exercise-related available questions (e.g., hours per week spent on sports participation). When the PASIPD outcomes were not in line with the other exercise-related statements, the participant was excluded from the dataset due to unreliable PASIPD outcomes.
Based on the remaining PASIPD outcomes it was determined whether participants met any aerobic part of any SCI-specific exercise guidelines, with exercise frequency not taken into account. Participants whose weekly time spent on moderate exercise exceeded 150 min or on vigorous exercise exceeded 60 min, were categorized as meeting the exercise guidelines of Tweedy et al. [Citation7] (TW guidelines). A combination of time spent on moderate and vigorous exercise intensity was also allowed to meet the TW guidelines. Time spent on vigorous exercise multiplied by 2.5 was summed with time spent on moderate intensity and should have exceeded the recommended 150 min. Participants whose weekly time spent on moderate and/or vigorous exercise exceeded 90 min were categorized as meeting the cardiometabolic exercise guidelines of Martin Ginis et al. [Citation6] (MG cardiometabolic guidelines). Participants whose weekly time spent on moderate and/or vigorous exercise exceeded 40 min were categorized as meeting the fitness exercise guidelines of Martin Ginis et al. [Citation6] (MG fitness guidelines). If participants did not reach the recommended weekly 40 min, they were categorized as not meeting any guidelines.
Item 6 was used to determine whether individuals were involved in strength exercises at least once a week, as the questionnaire only allows to differentiate frequency into either never, 1–2 times, 3–4 times, or 5–7 times a week. Based on these outcomes, participants were categorized into either: (1) not involved in any strength exercise, or (2) involved in strength exercise at least once a week, which was also done in the study of Rauch et al. [Citation9].
Groups meeting guidelines or not
To test how meeting different exercise guidelines influences fitness and health, participants were allocated to one of the following four groups: (1) not meeting any exercise guidelines; (2) meeting the MG fitness guidelines; (3) meeting the MG cardiometabolic guidelines; or (4) meeting the TW guidelines. Allocation to the different guideline groups was done as described in . Participants meeting multiple exercise guidelines were only allocated to the most strenuous exercise guidelines in the order as described above with the TW guideline being the most strenuous.
Demographics
Personal and social demographics (sex, age, height, educational level) were collected. Educational level was categorized into three categories according to the Dutch central agency for statistics [Citation18]: (1) lower educational level (primary school, lower educational level), (2) middle educational level (high school, vocational education), and (3) higher educational level (applied-university or higher).
SCI characteristics
SCI characteristics (TSI, etiology, lesion level, motor, and sensory completeness) were collected and assessed according to the International Standards for Neurological Classification of Spinal Cord Injury [Citation15]. Neurological lesion level below T1 was considered as paraplegia and lesions at or above T1 as tetraplegia. The etiology of the SCI was dichotomized into either traumatic or non-traumatic.
Fitness
Respiratory function
Respiratory function was tested and measured according to a standardized protocol [Citation19] with the following outcomes: forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), forced inspiratory volume in 1 s (FIV1), forced expiratory flow (PEF) and forced inspiratory flow (PIF). All measurements were repeated until at least three measurements of each test within a range of ±5% were recorded. The highest measured outcome value of each test was used for analysis.
Exercise capacity
To test exercise capacity, a graded wheelchair exercise test was performed with the outcome measures peak oxygen uptake (VO2peak) expressed in L/min and L/kg/min and peak power output (POpeak) expressed in Watt (W) and W/kg. Participants were excluded from this test if they had (1) cardiovascular contraindications as stated by the American College of Sports Medicine guidelines [Citation20] or (2) severe musculoskeletal complaints in the upper extremities. The equipment and protocol used for this test have been described in detail elsewhere [Citation16,Citation21]. VO2peak was determined by using the highest recorded values of the average oxygen consumption during 30-s periods. POpeak was the power output measured during the highest treadmill inclination that was maintained by the participant for at least 30 s.
Health
Body mass (kg) and height (m) were measured and used to calculate the body mass index (BMI) (body mass/height2). In the ALLRISC project only, waist circumference (WC, in cm) was measured three times using a tape measure, with the average value being used for analysis.
Systolic (SBP) and diastolic blood pressure (DBP) were measured in mmHg in a seated position by a physician with an automatic (ALLRISC project) or manual sphygmomanometer (Umbrella project). Hypertension was defined as SBP of ≥140 mmHg and/or DBP of ≥90 mmHg [Citation22]. Mean arterial pressure (MAP) was calculated by the following formula: DBP + 1/3*(SBP − DBP).
Lipid profile was determined from blood samples taken in the morning in a fasting state. Concentrations (mmol/L) of total cholesterol (TC), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglycerides (TG) were determined, and TC/HDL calculated. Standardized laboratory protocols were used to obtain the concentrations.
Statistics
IBM SPSS software (Version 27, IBM Corporation, Armonk, NY, USA) was used for analyses. The total study population and the categorized groups based on meeting different SCI-specific exercise guidelines were described. Differences in personal, lesion, fitness, and health characteristics between selected groups were tested with a one-way ANOVA. If the assumptions were violated, the non-parametrical equivalent test was used. All categorical data were tested with the Kruskal-Wallis test. Dichotomous data were tested with the Chi-Square test. In the case of significance of the one-way ANOVA test, a post-hoc Bonferroni test was performed among all groups with the significance level set at p < 0.05. In the case of significance of the non-parametrical alternative, a corresponding post-hoc test was performed among all three groups, with a significance level set on p < 0.017 to adjust for alpha inflation (0.05/3–0.017).
Multiple regression analysis was performed to evaluate if meeting SCI-specific aerobic exercise guidelines affects fitness and health. Multiple regressions were performed twice on each fitness and health outcome variable. Once with the MG guidelines group and once with the inactive group as the reference category to allow for multiple comparisons. In the case of dichotomous outcomes, logistic regressions were performed. Outcomes were adjusted for the potential confounders age, sex, TSI, lesion level, lesion completeness, etiology of SCI, and educational level. Statistical significance was considered if one of the two group variables showed p < 0.05 compared to the reference category and confidence intervals are presented in Supplementary Appendix 1.
Results
A total of 358 participants were included for analysis after excluding 151 participants. The in-/exclusion of participants, and exercise guidelines allocation process, including when strength exercise was taken into account, is depicted in . The MG cardiometabolic group (n = 16) was merged with the MG fitness group (n = 43) during the group comparisons and regression analyses to ensure decent groups size and is from here onwards referred to as the MG guidelines (n = 59). Personal, lesion, fitness, and health characteristics, including the number of participants available for each variable and guidelines allocation, are shown in . Outcomes for each group separately and group comparisons after allocation based on meeting SCI aerobic exercise guidelines are presented in .
Figure 1. Flowchart of in- and exclusion of data and of group allocation of different SCI exercise guidelines. Bolded groups were used for group comparisons and multiple regression analysis.
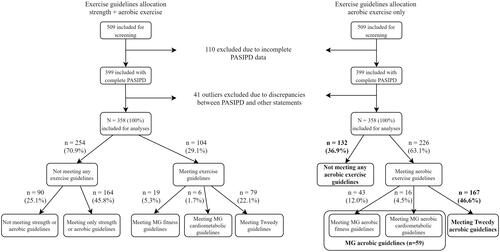
Table 2. Demographic, lesion, fitness, and health characteristics of all participants (N = 358).
Table 3. Differences in demographic and lesion characteristics, fitness, and health outcomes between groups meeting different aerobic exercise guidelines.
Several variables showed significant differences between the groups. Being female, older in age, having tetraplegia, and having a lower educational level was associated with a lower likelihood to meet any exercise guidelines (). All fitness variables showed more positive outcomes in individuals meeting exercise guidelines compared to inactive individuals, of which multiple variables showed a significant difference. However, no significant differences between groups were found for health-related variables except for waist circumference. TW guidelines group showed a significantly smaller waist circumference compared to the inactive group ().
Physical fitness
Respiratory function
In all multiple regressions, outcomes were adjusted for demographic and lesion characteristics. All respiratory parameters were significantly higher (p ≤ 0.005; ) in individuals meeting the MG guidelines compared to the inactive group, except for the PIF. The TW guidelines group showed significantly better scores (p < 0.001) on all respiratory parameters compared to the inactive group (). No significant differences in respiratory parameters were found between the MG and TW guidelines groups, except for PIF, which was higher in the TW guidelines group (p = 0.009; Table 4b, Supplementary Appendix 1).
Table 4. Multiple regression analysis on fitness and health outcomes with inactive as reference.
Exercise capacity
The TW guidelines group showed a significantly higher relative VO2peak (p = <0.001, ) and absolute VO2peak (p = 0.001, Table 5a, Supplementary Appendix 1) compared to the inactive group. Both the MG (p = 0.047) and the TW guidelines group (p = <0.001) scored significantly better on relative POpeak compared to the inactive group (). The TW guidelines group scored significantly higher (<0.001) on absolute POpeak compared to the inactive group (Table 5a, Supplementary Appendix 1). Additionally, the TW guidelines group scored significantly better on both absolute VO2peak (p = 0.022) and POpeak (p = 0.026) compared to the MG guidelines group (Table 5b, Supplementary Appendix 1).
Health
A significantly lower BMI was found (p = 0.039) in the MG guidelines group compared to the inactive group (). A significantly lower WC was found (p = 0.007) in the TW guidelines group compared to the inactive group (). The TW guidelines group showed significantly higher SBP (p = 0.005, Table 6a, Supplementary Appendix 1) and MAP (p = 0.026, ) compared to the inactive group. No significant differences in the prevalence of hypertension or in lipid profile outcomes were found among groups.
Discussion
The purpose of this study was to estimate the proportion of Dutch wheelchair users with SCI meeting different SCI exercise guidelines, which demographic and lesion characteristics are associated with meeting these guidelines, and whether meeting these guidelines is associated with better physical fitness and health. Results showed that only 29% of Dutch wheelchair users with SCI meet SCI-specific exercise recommendations if strength exercise is taken into account. When strength training is not taken into account, 63% meet either the MG or TW guidelines for aerobic exercise. When adjusted for demographic and lesion characteristics, a strong association was found between aerobic exercise activity levels and beneficial outcomes on physical fitness, with more strenuous guidelines showing better outcomes on exercise capacity. Additional benefits were found regarding body composition in more strenuous aerobic exercise activity levels, and therefore possibly health. These results clearly show the importance of regular exercise and that the SCI-specific exercise guidelines partly achieve what they were designed for.
As expected, older age, being female, having tetraplegia, and low educational level seem to negatively influence exercise behavior, and therefore physical fitness and health outcomes. In this study, only 29% of the participants met the least strenuous SCI-specific exercise guidelines (MG), and 22% of the TW guidelines, when strength exercise was taken into account. This result shows that combining aerobic and strength exercise is a challenge for most Dutch wheelchair users with SCI. Higher proportions were found in Switzerland in previous research of Rauch et al. [Citation9], who applied allocation to guidelines using a similar methodology. Rauch et al. found that 49% of persons with SCI fulfilled the WHO guidelines, including strength exercise, which are comparable guidelines to the TW guidelines. However, the WHO does not differentiate between moderate and vigorous activity levels like the TW guidelines. In contrast, a Canadian study showed much lower percentages, i.e., with only 12% meeting the MG exercise guidelines compared to 29% in this study [Citation10]. When only aerobic exercise was taken into account, 63% of our participants met the MG guidelines, compared to 36% of the participants in a study of Rocchi et al. [Citation10] who applied the Leisure Time Physical Activity Questionnaire for People with Spinal Cord Injury (LTPAQ-SCI). The use of a different questionnaire might have caused differences in allocating participants to meeting exercise guidelines or not, as the LTPAQ-SCI asks the exact number of days spent in different intensity levels while the PASIPD categorizes this question into: never, 1–2, 3–4, or 5–7 days. Therefore, it is more likely to overestimate the time spent in specific exercise intensities when using the PASIPD. Only 22% of our participants met the TW guidelines, which is much lower compared to the 44% of the general Dutch population who meets the comparable WHO guidelines [Citation23]. This emphasizes once more the necessity to facilitate and support exercise in individuals with SCI.
Results of the regression analyses showed beneficial associations between meeting exercise guidelines and respiratory function, as both the MG and TW guidelines group scored significantly better on almost all respiratory function tests compared to the inactive group, even after correction for lesion level and completeness, and age. Respiratory dysfunction can have a severe impact on daily life in individuals with SCI. Increased residual lung volumes, along with a reduced ability to cough, can cause increased accumulation of secretion, increasing the risk of pulmonary infections and other complications [Citation24]. No significant differences were found between the MG and TW guidelines group, suggesting respiratory function improvement already occurs at relatively low exercise activity levels.
Significantly higher outcomes in relative POpeak were found in the MG and TW guidelines groups compared to the inactive group. This is a valuable finding as most individuals with SCI depend on a manual wheelchair and those with a higher POpeak tend to experience a lower amount of strain in activities of daily living, are more likely to return to work, and experience a higher quality of life [Citation25–27]. The TW guidelines group scored also significantly better on POpeak and relative VO2peak compared to the inactive group. There may have been a positive selection bias as a higher proportion of individuals with tetraplegia was found in the inactive group (56.8%) compared to the MG (49.2%) and TW (39.0%) guidelines groups. This probably explains the relatively low number of inactive individuals who performed a peak exercise test (31.8%), compared to the MG group (67.8%) and TW group (71.3%). Thus, the actual differences in physical fitness between the inactive group and the MG and TW guidelines groups might be even larger. However, even after controlling for lesion level, a clear pattern was found showing increased benefits in physical fitness with increased exercise activity levels.
One of the main reasons exercise guidelines were developed, was to provide evidence-based recommendations to support behavior that leads to fitness and health benefits and reduce health risks and mortality [Citation5]. Obesity, high blood pressure, and high cholesterol are among the most critical risk factors [Citation28]. Despite the known positive relationship between exercise and these factors, results in the present paper are limited. The TW guidelines group showed a significantly lower WC compared to the inactive group suggesting additional health benefits as the guidelines were designed for. Surprisingly, participants who met the MG guidelines showed a significantly lower BMI compared to the inactive group while participants who met the TW guidelines did not. This could be explained by the fact that BMI does not take body composition, and therefore, muscle mass into account. Significantly higher SBP and MAP were found in the TW guidelines group compared to the inactive group, however, this did not translate into significantly different hypertension ratios compared to other groups. No significant differences were found in lipid profile outcomes, which could be attributed to their complex regulation which is controlled by many factors, of which some cannot be influenced by exercise, or can be influenced by medication use, which was not taken into account in the analyses.
Strengths and limitations
Merging two relatively large SCI datasets made it possible to perform analysis with a relatively large group of 358 participants. However, this study also has some limitations. The PASIPD was used to determine whether exercise guidelines were met, which is a self-administered outcome and a questionnaire not specifically designed to quantify exercise time and exercise intensity precisely. Therefore, the outcomes obtained from the participants might not fully reflect their actual situation. Previous research has shown that the PASIPD tends to overestimate time spent on physical activity, which might have caused biased group allocation [Citation29]. Additionally, answer options of the PASIPD for exercise frequency were in the ranges 0, 1–2, 3–4, or 5–7 times a week, as a result, exercising once a week could not be distinguished from exercising twice a week based on this item. Therefore, the classification of meeting or not meeting the aerobic exercise guidelines was based on total weekly time spent on exercise, leaving frequency (aerobic exercise at least twice a week) out of the process of allocation. The involvement of strength exercise could only be determined as at least once a week, like in the study of Rauch et al. [Citation9]. Therefore, the actual number of participants meeting any of the exercise guidelines including strength exercise could be even lower. Moreover, differentiation in moderate or vigorous intensity level was done subjectively by the participants based on the given PASIPD questions, which included examples of moderate or vigorous exercise activities. Due to the severity and level of their lesion the exercise capacity of individuals with tetraplegia can be severely reduced, putting them under relatively more strain in activities of similar intensity compared to individuals with paraplegia, making exercise intensity differentiation difficult and possibly unreliable.
Conclusion
With only 29% a small proportion of the Dutch wheelchair users with SCI seem to meet an SCI exercise guidelines. The exercise guidelines seem to at least partially achieve what they are designed for. Meeting the MG guidelines was associated with improved respiratory function and exercise capacity, which is achieved with relatively low exercise levels. Increased exercise levels, like in the TW guidelines, were associated with additional fitness and body composition benefits.
Ethical approval
Ethical approval was given by the local medical ethics committee of rehabilitation center Hoensbroek and the Medical Ethics Committee of the University Medical Centre Utrecht. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Author contributions
DH, JH, SdG, and TJ conceived and designed the research. LvdW and SdG organized and managed the data collection of both projects. KP was involved in the organization and data collection of the Umbrella project. DH cleaned and merged the datasets. DH analyzed the data with the supervision of JH, SdG, and TJ. DH wrote the paper and all authors read the paper, provided feedback, and approved the manuscript.
Appendix_1._Regression_analysis_of_all_outcomes_measures_including_CI_manuscript_ID_TIDS-09-2021.pdf
Download PDF (282.5 KB)Acknowledgments
We thank all involved researchers, physicians, and research assistants involved in data collection within the Umbrella and ALLRISC project.
Disclosure statement
The authors declare no conflict of interest.
Additional information
Funding
References
- World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization; 2009.
- Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257.
- Van Den Berg-Emons RJ, Bussmann JB, Stam HJ. Accelerometry-based activity spectrum in persons with chronic physical conditions. Arch Phys Med Rehabil. 2010;91(12):1856–1861.
- World Health Organization. Global recommendations on physical activity for health. Geneva: World Health Organization; 2010.
- Bull FC, Al-Ansari SS, Biddle S, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462.
- Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56(4):308–314.
- Tweedy SM, Beckman EM, Geraghty TJ, et al. Exercise and sports science Australia (ESSA) position statement on exercise and spinal cord injury. J Sci Med Sport. 2017;20(5):422–423.
- Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–131.
- Rauch A, Hinrichs T, Oberhauser C, Cieza A. Do people with spinal cord injury meet the WHO recommendations on physical activity? Int J Public Health. 2016;61(1):17–27.
- Rocchi M, Routhier F, Latimer-Cheung AE, et al. Are adults with spinal cord injury meeting the spinal cord injury-specific physical activity guidelines? A look at a sample from a Canadian province. Spinal Cord. 2017;55(5):454–459.
- Kressler J, Cowan RE, Bigford GE, et al. Reducing cardiometabolic disease in spinal cord injury. Phys Med Rehabil Clin N Am. 2014;25(3):573–604.
- Powell KE, Paluch AE, Blair SN. Physical activity for health: what kind? How much? How intense? On top of what? Annu Rev Public Health. 2011;32:349–365.
- De Groot S, Dallmeijer AJ, Post MWM, et al. Demographics of the Dutch multicenter prospective cohort study ‘restoration of mobility in spinal cord injury rehabilitation’. Spinal Cord. 2006;44(11):668–675.
- Adriaansen JJE, Van Asbeck FWA, Lindeman E, et al. Secondary health conditions in persons with a spinal cord injury for at least 10 years: design of a comprehensive long-term cross-sectional study. Disabil Rehabil. 2013;35(13):1104–1110.
- Maynard FM, Bracken MB, Creasey G, Ditunno JF, et al. International standards for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Spinal Cord. 1997;35(5):266–274.
- Van Koppenhagen CF, De Groot S, Post MWM, et al. Wheelchair exercise capacity in spinal cord injury up to five years after discharge from inpatient rehabilitation. J Rehabil Med. 2013;45(7):646–652.
- Washburn RA, Zhu W, McAuley E, et al. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83(2):193–200.
- Centraal Bureau voor de Statistiek. Standaard Onderwijsindeling 2017/2018; 2018.
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338.
- American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 6th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2000.
- de Groot S, van der Scheer JW, Bakkum AJT, et al. Wheelchair-specific fitness of persons with a long-term spinal cord injury: cross-sectional study on effects of time since injury and physical activity level. Disabil Rehabil. 2016;38(12):1180–1186.
- Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension. J Hypertens. 2018;36(12):2284–2309. 2018
- Health Council of the Netherlands. Dutch physical activity guidelines 2017. The Hague: Health Council of the Netherlands; 2017.
- Schilero GJ, Spungen AM, Bauman WA, et al. Pulmonary function and spinal cord injury. Respir Physiol Neurobiol. 2009;166(3):129–141.
- Janssen TWJ, Van Oers CAJM, Veeger HEJ, et al. Relationship between physical strain during standardised ADL tasks and physical capacity in men with spinal cord injuries. Paraplegia. 1994;32(12):844–859.
- Van Velzen JM, De Groot S, Post MWM, et al. Return to work after spinal cord injury: is it related to wheelchair capacity at discharge from clinical rehabilitation? Am J Phys Med Rehabil. 2009;88(1):47–56.
- Kouwijzer I, de Groot S, van Leeuwen CM, et al. Changes in quality of life during training for the HandbikeBattle and associations with cardiorespiratory fitness. Arch Phys Med Rehabil. 2020;101(6):1017–1024.
- Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285–292.
- Van Den Berg-Emons RJ, L’Ortye AA, Buffart LM, et al. Validation of the physical activity scale for individuals with physical disabilities. Arch Phys Med Rehabil. 2011;92(6):923–928.
